Abstract
Background
Despite policies that recommend parasitological testing before treatment for malaria, presumptive treatment remains widespread in Nigeria. The majority of Nigerians obtain antimalarial drugs from two types of for-profit drug vendors—formal and informal medicine shops—but little is known about the quality of malaria care services provided at these shops.
Aims
This study seeks to (1) describe the profile of patients who seek treatment at different types of drug outlets, (2) document the types of drugs purchased for treating malaria, (3) assess which patients are purchasing recommended drugs, and (4) estimate the extent of malaria over-treatment.
Methods
In urban, peri-urban, and rural areas in Oyo State, customers exiting proprietary and patent medicine vendor (PPMV) shops or pharmacies having purchased anti-malarial drugs were surveyed and tested with malaria rapid diagnostic test. A follow-up phone survey was conducted four days after to assess self-reported drug administration. Bivariate and multivariate regression analysis was conducted to determine the correlates of patronizing a PPMV versus pharmacy, and the likelihood of purchasing an artemisinin-combination therapy (ACT) drug.
Results
Of the 457participants who sought malaria treatment in 49 enrolled outlets, nearly 92% had diagnosed their condition by themselves, a family member, or a friend. Nearly 60% pharmacy customers purchased an ACT compared to only 29% of PPMV customers, and pharmacy customers paid significantly more on average. Multivariate regression results show that patrons of PPMVs were younger, less wealthy, waited fewer days before seeking care, and were less likely to be diagnosed at a hospital, clinic, or laboratory. Only 3.9% of participants tested positive with a malaria rapid diagnostic test.
Conclusions
Poorer individuals seeking care at PPMVs are more likely to receive inappropriate malaria treatment when compared to those who go to pharmacies. Increasing accessibility to reliable diagnosis should be explored to reduce malaria over-treatment.
Introduction
Nigeria bears one of the world's highest burdens of malaria, accounting for a quarter of all cases in Africa [1]. It is estimated that over half of Nigeria's population experiences at least one episode of malaria each year, accounting for approximately 20% of all hospital admission, 30% of outpatient visits, and 10% of hospital deaths [2]. This burden of disease strains the resources of the health system as spending on malaria treatment and prevention accounts for nearly 50% of all health expenditures in Nigeria [3].
To effectively diagnose and treat malaria, the World Health Organization (WHO) currently recommends a confirmatory blood test for all suspected cases of malaria and prescription of artemisinin-based combination therapy (ACT) upon confirmation of malaria positivity [4]. ACTs are currently the most effective antimalarial treatment and are becoming more widely available in Nigeria [5]. However, many health care providers in Nigeria continue to prescribe less-effective drugs, such as chloroquine (CQ) and sulfadoxine-pyrimethamine (SP), for uncomplicated cases of malaria [6]. Despite the increased availability of malaria rapid diagnostic tests (RDTs) to facilitate point-of-care diagnosis elsewhere in sub-Saharan Africa [7]–[11], RDTs are not yet widely available in Nigeria [12] and presumptive diagnosis continues to be the most common method for determining a patient's malaria status [13].
This study aims to better characterize the practice of presumptive treatment of malaria in Nigeria and determine where interventions for malaria treatment delivery should be targeted. Nearly 60% of Nigerians seek treatment for malaria at drug shop outlets in the private healthcare sector [14]. Of these vendors, the minority is composed of licensed pharmacies, which are either owned or staffed by formally trained pharmacists, and which are mainly found in urban centers. The majority of vendors are informally trained, loosely regulated proprietary and patent medicine vendors (PPMVs), which are frequently the only source of drugs in rural areas [14]–[16]. While both types of vendors mainly operate as drug retailers, the quality of health services offered can vastly differ. PPMVs are legally permitted to only sell a number of medications over-the-counter, including antimalarial medications, but recent assessments show that they often do not stock ACTs, and have limited knowledge of malaria symptoms and recommended treatment guidelines [17]. In contrast, pharmacists are perceived to offer higher-quality malaria care services than PPMVs [18], although little empirical evidence exists to corroborate these views.
When choosing the type of facility at which to seek care, patients may prioritize convenience, availability of familiar drugs, and affordability [18]. While hospitals and clinics may provide higher quality care and testing, long wait and travel times often drive patients to accessible, nearby drug vendors. Similarly, there is little demand for confirmatory malaria microscopy testing, leading many people to bypass hospital/clinics or costly independent diagnostic laboratories [19].
Because private sector drug vendors are the source for such a large proportion of Nigeria's population seeking malaria care, it is important to understand the extent to which individuals seeking treatment for malaria are able to receive accurate diagnosis and treatment at pharmacies and PPMVs [20]. It is also important to understand what types of consumers may be at most risk for receiving poor quality services. Consequently, this study seeks to (1) describe and compare the profile of patients who seek treatment at PPMVs versus pharmacies, (2) document the types of drugs purchased for treating malaria, (3) assess which patients are purchasing recommended ACTs, and (4) estimate the extent of malaria over-treatment [21]. Implications of findings for targeting appropriate diagnostic and treatment interventions are discussed.
Materials and Methods
Ethical considerations
The Nigerian Health Research Ethical Review Committee (NHREC Approval Number NHREC/01/01/2007-30/08/2012) and the University of California, San Francisco's Committee for Human Research approved all study protocols. Data collectors obtained written informed consent from study participants and shop proprietors where the customers were recruited. Written consent was obtained from shop proprietors via signature and customers via signature or fingerprint for non-literate customers. The consent procedure was approved by the Nigerian Health Research Ethical Review Committee and the University of California, San Francisco's Committee for Human Research. Funding sponsors for the study did have any role in the study design, execution, or publication.
Study area and sample selection
The study was conducted in Oyo State, located in the Southwest geopolitical zone of Nigeria, comprised of about 4.5million people (predominantly of Yoruba descent) [13]. Four local government areas (LGAs) were purposefully selected for the study to include urban, semi-urban, and rural areas: Ibadan South East (urban) andEgbeda (semi-urban) in and around the Ibadancity area, whileOgbomosho South and OgoOluwa were selected in and around the Ogbomosho town area (rural). All PPMV and pharmaceutical shops were first enumerated within the four selected LGAs and a total number of 236 PPMVs and 24 pharmaceutical shops were identified during the enumeration exercise. Interviewers used a questionnaire that captured the names, addresses, location (urban, seri-urban, rural), LGA, GPS coordinates, notable landmarks, and size of outlets (‘small’ for outlets with two shelves of medicines; ‘medium’ for outlets with three to four shelves of medicine; ‘large’ for outlets with more than five shelves).
From the complete list of shops, a total of fifty pharmacies and PPMVs were randomly selected, stratified by the size of medicinal stock (i.e. small, medium, and large). Selected shops were visited to inform shop owners of the study aims and obtain permission to recruit exiting customers into the study. Enrolled study sites were later modified to exclude 24 small PPMV drug retailers in Ibadan whose main business was not medicinal sales (thus participants were not able to be recruited) and replaced with randomly selected PPMV shops in Ibadan North East LGA. Using a standard script, 49 out of 50 selected private sector retailers (42shop in/around Ibadan, 7shops in/around Ogbomosho) agreedto havetheir shop used for participant recruitment and were enrolled into the study; only one pharmacy declined to participatefor reasons not stated. The final roster of recruitment sites consisted of 21 pharmacies and 23 PPMVs. All seven shops enrolled in Ogbomosho were PPMVs as the city did not have any pharmacies during site enumeration.
Two members of the survey team, one trained nurse and one researcher, were stationed at enrolled PPMVs and pharmacies on randomly selected days of the week (excluding Sunday) and approached customers as they exited the drug store to assess eligibility. The inclusion criteria were as follows: the participant must be a non-pregnant adult having purchased treatment for malaria for him-or herself and be willing to complete a 15-minute survey. Malaria “treatment” was defined to mean any drug purchased by the customer that s/he intended to take for their current episode of suspected malaria, which may include inappropriate drugs for malaria and not necessarily an antimalarial drug. While seeking consent, the participant was informed that if they qualified, they would be offered a RDT and would be compensated for their time with a small mobile phone credit of 200 Naira (∼US$1.20) for participating in the interview.
Data collection
Two surveys were conducted, one at the time of enrollment and testing (i.e. baseline) and one after four days of the initial encounter via telephone call(i.e. follow-up). All data were collected concurrently. At baseline, the eligible participant was offered a RDT performed by a trained nurse at the beginning of the survey. While the RDT result was pending (about 15 minutes), a detailed survey was conducted designed to capture information on the background demographics and socioeconomic stats, symptoms experienced, and care-seeking actions taken for the current and past episodes of suspected malaria. Contact information was also collected during enrollment to facilitate later follow-up. At the end of the survey, the participant was provided with the result of his or her test.
Nurses were instructed to provide participants with standard advice according to their RDT results. If the participant tested positive for malaria, he/she was told that the positive result suggests the presence of malaria. Per ethical considerations to ensure that the participants testing positive had a quality-assured anti-malaria drug, a free course of ACTs was provided and participants were instructed to take it according to the recommended dosage protocol. If the test was negative, the participant was told that the negative result indicates the absence of malaria and that anti-malarial drugs they purchased were not needed. Regardless of the test result, all participants were referred to local clinics and hospitals where they could seek care if their condition was not malaria, or if their illness became worse. All participants were told to expect a short 5–10 minute follow up phone call in four days to check on the status of their illness and that they would be compensated with a small phone credit of 100 Naira (∼US$0.60)for taking the call.
Four days after the baseline survey, a nurse called the participants and conducted a phone survey to obtain information on the state of their health and the drugs they had used. A total of 465 adults were enrolled in the baseline survey, but eight were excluded due to survey numbering errors, and 424 participated in the follow-up phone survey—a follow-up retention rate of 92.8%. No differences in individual characteristics between attritted and retained participants were detected; detailed sample attrition are described elsewhere [22].
Data Analysis
Descriptive data analysis
Descriptive analysis was used for the study to review the sample for basic socio demographic characteristics, reasons for choosing the drug shop, and drugs purchased and taken. Wealth distribution was assessed using standard principal components analysis (PCA) [23] in two ways. First, to compare the representativeness of the study sample to the overall state and national sample, weights associated with PCA component items generated from the 2010 Nigeria Malaria Indicator Survey (MIS) were applied to comparable asset indicators collected in the study sample to compute a wealth index that reflected the national wealth distribution. This index was then converted to quintile categorical indicators for comparing external sample representativeness. A second wealth index was created using only the study sample via the same PCA technique and converted to quintile indicators to obtain an even, within-sample distribution of wealth.
Regression Analysis
Two types of regression analyses were conducted. First, we estimated bivariate and multivariate logistic regressions to assess differences in the types of individuals that patron different types of drug shops—PPMVs versus pharmacies. The likelihood that a PPMV was chosen was predicted by the individual's age, sex, educational attainment, marital status, and wealth. In addition to basic socio demographics, employment status (i.e. full-time wage worker, part-time wage worker, self-employed, and unemployed) was included as shop owners indicated that customers tend to stop at drug shops on their way to and from work. Self-reported symptoms felt for the current illness episode, the number of days waited before seeking care, and where the recognition of the illness as malaria came from (i.e. myself/relative/friend, a hospital/clinic/diagnostic laboratory, or at a drug retailer) were also included because these factors may influence the choice of drug shop type based on perceived severity, need for drug administration, or recommendations by diagnosticians. Second, the likelihood of buying an ACT was predicted using logistic regression analysis. In addition to individual characteristics described above, the type of shop (i.e. PPMV vs. pharmacy) was included as a risk factor for receiving the recommended first-line malaria drug. In both analyses, only statistically significant explanatory variables at the 5% level in bivariate analysis were included in the multivariate model. To account for autocorrelation between individuals recruited at the same shop, standard errors were clustered at the shop level. Odds ratios are reported.
Findings
Sample characteristics
Of the 457participants who sought malaria treatment from the 49enrolled shops, 71.1% (n = 325) were recruited in Ibadan, 55.6% (n = 254) were under the age of 40 (median = 37; range: 18–82), 50.8% were male (n = 232), and 68.1% (n = 311) were married. Only 22.5% (n = 103) had primary education or less; 39.8% (n = 182) completed secondary education and 37.6% (n = 172) had some tertiary level education. Among those interviewed, 31.3% (n = 143) were employed either on a full-time or part-time basis; 53.6% were self-employed (n = 245) and 15.1% were unemployed (n = 69). Participants reported feeling a variety of symptoms during their current episode of illness. Fever was most commonly reported (74.6%, n = 341), followed by body aches, chills, or convulsions (57.5%, n = 263), feeling weak, fatigued, or having little appetite (55.8%, n = 255). Nearly half of participants waited one day (18.7%, n = 79) or less (28.7%; n = 122) before seeking care; 34.3% (n = 146) waited three days or more. Nearly 92% (n = 423) of the participants reported that they had diagnosed the episode of malaria by themselves, a family member, or a friend. See Table 1 for a summary of the sample characteristics.
Table 1. Customer demographic and socioeconomic variables (N = 457).
| Variable | N | % | |
| Site | Ogbomosho | 132 | 28.9 |
| Ibadan | 325 | 71.1 | |
| Age of respondents | 18–29 | 127 | 27.8 |
| 30–39 | 127 | 27.8 | |
| 40–49 | 100 | 21.9 | |
| 50+ | 103 | 22.5 | |
| Sex | Male | 232 | 50.8 |
| Female | 227 | 49.2 | |
| Education | No education | 130 | 28.4 |
| Primary education | 13 | 2.8 | |
| Secondary education | 245 | 53.6 | |
| Higher education | 69 | 15.1 | |
| Marital status | Not married | 146 | 31.9 |
| Married | 311 | 68.1 | |
| Employment status | Employed full time | 130 | 28.4 |
| Employed part time | 13 | 2.8 | |
| Self-employed | 245 | 53.6 | |
| Unemployed | 69 | 15.1 | |
| Wealth quintile1 | Poorest | 90 | 19.7 |
| Second | 92 | 20.1 | |
| Third | 93 | 20.4 | |
| Fourth | 90 | 19.7 | |
| Richest | 92 | 20.1 | |
| Symptoms reported | |||
| Fever, headache, dizziness | Yes | 341 | 74.6 |
| No | 116 | 25.4 | |
| Body aches, chills, convulsions | Yes | 263 | 57.5 |
| No | 194 | 42.5 | |
| Weak, fatigue, no appetite | Yes | 255 | 55.8 |
| No | 202 | 44.2 | |
| Bitter taste in the mouth | Yes | 62 | 13.6 |
| No | 395 | 86.4 | |
| Congestion, shallow breathing | Yes | 58 | 12.7 |
| No | 399 | 87.3 | |
| Vomiting, diarrhea | Yes | 54 | 11.8 |
| No | 403 | 88.2 | |
| Other: blisters, dark urine, yellow eyes | Yes | 63 | 13.8 |
| No | 394 | 86.2 | |
| Number of days waited before seeking care2 | <1 day | 122 | 28.7 |
| 1 day | 79 | 18.7 | |
| 2 days | 77 | 18.2 | |
| 3–5 days | 104 | 24.5 | |
| 6 days or more | 42 | 9.8 | |
| Source of diagnosis | Self-diagnosis | 418 | 91.5 |
| Hospital/clinic/lab | 20 | 4.4 | |
| Pharmacy/PPMV | 19 | 4.2 |
Result of within-sample principle components analysis.
N = 424.
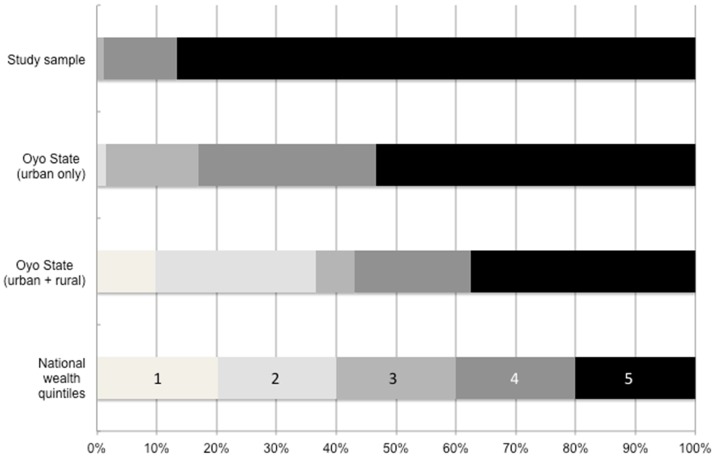
When comparing the wealth distribution between sampled individuals to that of the state and national populations captured by the 2010 MIS, those in the wealthiest quintile are disproportionately represented in the study sample. Based on the composite asset ownership measure, no individuals in the study sample were from the lowest two wealth quintiles of nation as seen in Figure 1. Although the population of Oyo State, and particularly in urban areas, is also comprised of households that are much wealthier than the nation as a whole, the study sample's wealth composition is even more concentrated among the wealthiest.
Figure 1. Wealth distribution of enrolled participants versus state and national populations.
When comparing the wealth distribution between sampled individuals to that of the state and national populations captured by the 2010 MIS, those in the wealthiest quintile are disproportionately represented in the study sample. Based on the composite asset ownership measure, no individuals in the study sample were from the lowest two wealth quintiles of nation. Although the population of Oyo State, and particularly in urban areas, is also comprised of households that are much wealthier than the nation as a whole, the study sample's wealth composition is even more concentrated among the wealthiest. Source: 2010 Nigeria Malaria Indicators Survey.
Types of medicines purchased for malaria treatment
Table 2 summarizes the types of drugs purchased at PPMVs and pharmacies for the current episode of suspected malaria among participants who agreed to have their drugs examined by the study nurse (n = 423). A significantly higher percentage of the patrons of pharmacies (57.4%, n = 132/230) purchased an ACT compared to only 28.5% (n = 55/193) of PPMV patrons (p<0.01). Of non-ACT antimalarials purchased, significantly more customers at PPMVs (47.7%; n = 92/230) purchased SP than customers of pharmacies (28.7%, n = 66/193; p<0.05). A higher percentage of PPMV customers also bought a non-malaria drug (70.1%, n = 136/194) compared to pharmacy customers (54.7%, n = 129/236). Significantly fewer analgesics (76.0%, n = 98/230), but more vitamins/supplements (85.3%, n = 110/230) and antibiotics (20.9%, n = 27/230) were purchased at pharmacies than at PPMVs (respectively: 92.6%, n = 126/193; 60.3%, n = 82/193; 5.9%, n = 8/193). More patrons of pharmacies bought only an antimalarial (45.3%, n = 107/230) compared to those at PPMVs (29.9%, n = 58/193). However, pharmacy customers paid significantly more for all of their drugs than those purchasing at PPMVs on average.
Table 2. Drugs purchased to treat malaria.
| Pharmacies | PPMVs | Total | |||||
| n | % | n | % | n | % | P-value | |
| Type of anti-malarial drug1 | |||||||
| ACT | 132 | 57.4 | 55 | 28.5 | 187 | 44.2 | 0.003 |
| SP | 66 | 28.7 | 92 | 47.7 | 158 | 37.4 | 0.022 |
| CQ | 46 | 20.0 | 33 | 17.1 | 79 | 18.7 | 0.545 |
| Other | 21 | 9.1 | 16 | 8.3 | 37 | 8.7 | 0.830 |
| Purchased non-malaria drug | |||||||
| Yes | 129 | 54.7 | 136 | 70.1 | 265 | 61.6 | 0.068 |
| No | 107 | 45.3 | 58 | 29.9 | 165 | 38.4 | |
| Type of non-malaria drugs | |||||||
| Analgesic | 98 | 76.0 | 126 | 92.6 | 224 | 84.5 | 0.003 |
| Vitamin/supplement | 110 | 85.3 | 82 | 60.3 | 192 | 72.5 | 0.007 |
| Antibiotic | 27 | 20.9 | 8 | 5.9 | 35 | 13.2 | 0.019 |
| Other | 16 | 12.4 | 11 | 8.1 | 27 | 10.2 | 0.251 |
| Purchase combinations | |||||||
| Anti-malarial only | 107 | 45.3 | 58 | 29.9 | 167 | 38.6 | 0.056 |
| Non-malaria drug only | 6 | 1.3 | 1 | 0.3 | 7 | 0.8 | |
| Both anti-malarial and non-malaria drug | 123 | 26.2 | 135 | 34.9 | 259 | 30.1 | |
| n | median | n | median | n | median | P-value | |
| Total amount paid (median) | 234 | 445 | 193 | 140 | 427 | 240 | 0.000 |
Pharmacies N = 230; PPMVs N = 193; Total N = 423. Not all participants purchased an anti-malarial drug.
Correlates of seeking care at a PPMV versus a pharmacy
Results of logistics regressions predicting the likelihood of going to a PPMV versus a pharmacy for malaria treatment are summarized in Table 3. In bivariate analyses, customers going to different shop types were significantly different in terms of their age, educational attainment, employment status, and wealth. Significant differences were also registered for a number of symptoms (i.e. fever, headache, or dizziness; feeling weak, fatigues, or no appetite; having congestion or shallow breathing; and other symptoms including blusters, dark urine, and yellow eyes), days waited before seeking care, and the source of diagnosis. In multivariate analyses, older individuals are about half as likely to patron a PPMV (age 30–39: OR = 0.416, 95% CI: 0.230–0.752; age 50+: OR = 0.461, 95% CI: 0.229–0.929) than those under age 30. A strong wealth gradient emerges with the individuals in progressively richer wealth quintiles increasingly less likely to go to a PPMV compared to those in the poorest quintile. Those reporting other types of symptoms (i.e. blisters, dark urine, yellow eyes) were more than three times as likely to go to a PPMV (OR = 3.138, 95% CI: 1.381–7.128) while those reporting fever, headache, or dizziness (OR = 2.589, 95% CI: 1.501–4.465) and weakness, fatigue, and lack of appetite (OR = 1.951, 95% CI: 1.043–3.649) were about twice as likely to go to a PPMV. When individuals waited one day before seeking care, they were twice as likely to go to a PPMV (OR = 2.070, 95% CI: 1.256–3.411) compared to those who sought treatment the same day; the likelihood of PPMV patronage progressively declined as the number of days waited increased, but these were not statistically significant. Diagnosis coming from a hospital, clinic, or laboratory was associated with a large and significantly lower likelihood of going to a PPMV (OR = 0.022, 95% CI: 0.137–1.311). Education and employment status were no longer statistically significant after adjusting for all confounders.
Table 3. Logistic regression of the likelihood of buying drugs from a PPMV (versus a pharmacy).
| Pharmacy | PPMV | Bivariate | Multivariate | |||||||||
| n = 245 | % | n = 212 | % | P-value | OR1 | 95% CI | P-val | OR1 | 95% CI | P-val | ||
| Age of respondents | 18–29 (reference) | 52 | 21.2 | 74 | 34.9 | 0.005 | 1.000 | 1.000 | ||||
| 30–39 | 78 | 31.8 | 49 | 23.1 | 0.441*** | 0.275–0.709 | 0.001 | 0.416*** | 0.230–0.752 | 0.004 | ||
| 40–49 | 56 | 22.9 | 44 | 20.8 | 0.552 | 0.268–1.139 | 0.108 | 0.564 | 0.255–1.249 | 0.158 | ||
| 50+ | 59 | 24.1 | 45 | 21.2 | 0.524** | 0.292–0.939 | 0.030 | 0.461** | 0.229–0.929 | 0.030 | ||
| Sex | Male | 125 | 51.0 | 106 | 50.0 | 0.893 | 0.969 | 0.615–1.528 | 0.893 | |||
| Female (reference) | 120 | 49.0 | 106 | 50.0 | 1.000 | |||||||
| Education | No education (reference) | 10 | 4.1 | 28 | 13.2 | 0.012 | 1.000 | 1.000 | ||||
| Primary education | 24 | 9.8 | 42 | 19.8 | 0.610 | 0.247–1.504 | 0.283 | 0.984 | 0.319–3.033 | 0.977 | ||
| Secondary education | 102 | 41.6 | 79 | 37.3 | 0.277** | 0.102–0.749 | 0.012 | 0.470 | 0.157–1.407 | 0.177 | ||
| Higher education | 109 | 44.5 | 63 | 29.7 | 0.206*** | 0.064–0.667 | 0.008 | 0.607 | 0.136–2.712 | 0.514 | ||
| Marital status | Not married (reference) | 66 | 26.9 | 80 | 37.7 | 0.089 | 1.000 | |||||
| Married | 179 | 73.1 | 132 | 62.3 | 0.616* | 0.352–1.077 | 0.089 | |||||
| Employment status | Employed full time (reference) | 83 | 33.9 | 47 | 22.3 | 0.012 | 1.000 | 1.000 | ||||
| Employed part time | 8 | 3.3 | 5 | 2.4 | 1.104 | 0.240–5.078 | 0.899 | 0.463 | 0.085–2.520 | 0.373 | ||
| Self-employed | 111 | 45.3 | 134 | 63.0 | 2.116*** | 1.205–3.717 | 0.009 | 1.337 | 0.627–2.849 | 0.452 | ||
| Unemployed | 43 | 17.6 | 26 | 12.3 | 1.068 | 0.581–1.962 | 0.833 | 0.761 | 0.299–1.940 | 0.567 | ||
| Wealth quintile | Poorest (reference) | 21 | 8.6 | 68 | 32.1 | 0.000 | 1.000 | 1.000 | ||||
| Second | 38 | 15.5 | 54 | 25.5 | 0.439*** | 0.235–0.819 | 0.010 | 0.430** | 0.205–0.900 | 0.025 | ||
| Third | 53 | 21.6 | 40 | 18.9 | 0.233*** | 0.126–0.431 | 0.000 | 0.205*** | 0.087–0.487 | 0.000 | ||
| Fourth | 59 | 24.1 | 32 | 15.1 | 0.162*** | 0.072–0.368 | 0.000 | 0.152*** | 0.056–0.413 | 0.000 | ||
| Richest | 74 | 30.2 | 18 | 8.5 | 0.0751*** | 0.023–0.249 | 0.000 | 0.075*** | 0.018–0.318 | 0.000 | ||
| Symptoms reported | ||||||||||||
| Fever, headache, dizziness | Yes | 168 | 68.6 | 172 | 81.1 | 0.001 | 2.021*** | 1.317–3.101 | 0.001 | 2.589*** | 1.501–4.465 | 0.000 |
| No (reference) | 77 | 31.4 | 40 | 18.9 | 1.000 | 1.000 | ||||||
| Body aches, chills, convulsions | Yes | 130 | 53.1 | 133 | 62.7 | 0.096 | 1.508* | 0.929–2.448 | 0.096 | |||
| No (reference) | 115 | 46.9 | 79 | 37.3 | 1.000 | |||||||
| Weak, fatigue, no appetite | Yes | 120 | 49.0 | 134 | 63.2 | 0.011 | 1.813** | 1.144–2.872 | 0.011 | 1.951** | 1.043–3.649 | 0.036 |
| No (reference) | 125 | 51.0 | 78 | 36.8 | 1.000 | 1.000 | ||||||
| Bitter taste in the mouth | Yes | 29 | 11.8 | 33 | 15.6 | 0.241 | 1.381 | 0.806–2.367 | 0.240 | |||
| No (reference) | 216 | 88.2 | 179 | 84.4 | 1.000 | |||||||
| Congestion, shallow breathing | Yes | 38 | 15.5 | 20 | 9.4 | 0.016 | 0.570** | 0.361–0.902 | 0.016 | 0.619* | 0.372–1.030 | 0.065 |
| No (reference) | 207 | 84.5 | 192 | 90.6 | 1.000 | 1.000 | ||||||
| Vomiting, diarrhea | Yes | 30 | 12.2 | 24 | 11.3 | 0.752 | 0.920 | 0.548–1.545 | 0.752 | |||
| No (reference) | 215 | 87.8 | 188 | 88.7 | 1.000 | |||||||
| Other: blisters, dark urine, yellow eyes | Yes | 15 | 6.1 | 48 | 22.6 | 0.000 | 4.515*** | 2.345–8.696 | 0.000 | 3.138*** | 1.381–7.128 | 0.0063 |
| No (reference) | 230 | 93.9 | 164 | 77.4 | 1.000 | 1.000 | ||||||
| Number of days waited before seeking care2 | <1 day (reference) | 56 | 25.9 | 65 | 31.7 | 0.016 | 1.000 | 1.000 | ||||
| 1 day | 30 | 13.9 | 49 | 23.9 | 1.378 | 0.854–2.225 | 0.189 | 2.070*** | 1.256–3.411 | 0.004 | ||
| 2 days | 37 | 17.1 | 40 | 19.5 | 0.931 | 0.510–1.700 | 0.817 | 1.624 | 0.890–2.962 | 0.114 | ||
| 3–5 days | 66 | 30.6 | 37 | 18.0 | 0.483* | 0.220–1.058 | 0.069 | 0.659 | 0.289–1.504 | 0.322 | ||
| 6 days or more | 27 | 12.5 | 14 | 6.8 | 0.447* | 0.181–1.100 | 0.080 | 0.431 | 0.137–1.355 | 0.150 | ||
| Source of diagnosis | Myself/family/friend (reference) | 213 | 86.9 | 205 | 96.7 | 0.011 | 1.000 | 1.000 | ||||
| Hospital/clinic/lab | 19 | 7.8 | 1 | 0.5 | 0.055*** | 0.008–0.393 | 0.004 | 0.022** | 0.001–0.412 | 0.011 | ||
| Pharmacy/PPMV | 13 | 5.3 | 6 | 2.8 | 0.482 | 0.149–1.557 | 0.222 | 0.424 | 0.137–1.311 | 0.136 | ||
| Observations | 457 | 420 | ||||||||||
Odds ratios reported.
Pharmacy (n = 212), PPMV (n = 205), Total (n = 417).
Standard errors are clustered at the shop level;
***p<0.01,
**p<0.05,
*p<0.1.
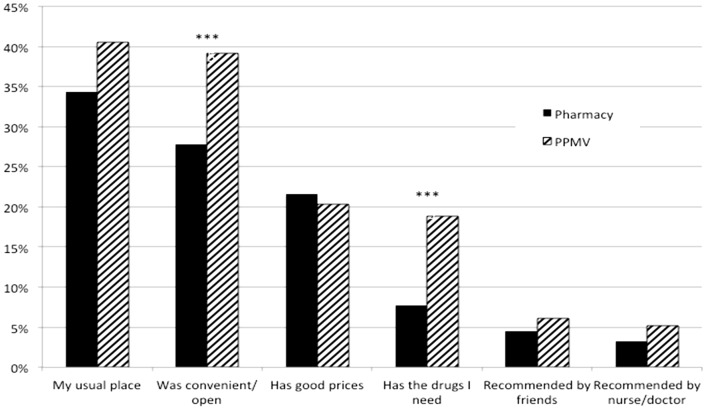
When asked for reasons why they chose the particular drug shop, most respondents stated reasons of habit and convenience (see Figure 2). A significantly higher percentage of participants at PPMVs said that the shop was convenient and had the drugs that s/he needed. In similar percentages, both types of outlets were cited for their prices.
Figure 2. Reasons for choosing a drug shop (N = 457).
When asked for reasons why they chose the particular drug shop, most respondents stated reasons of habit and convenience (see Figure 2). A significantly higher percentage of participants at PPMVs said that the shop was convenient and had the drugs that s/he needed. In similar percentages, both types of outlets were cited for their prices. Note: *** p<0.01, ** p<0.05, * p<0.1.
Predictors of purchasing an ACT
The logistic regression results predicting the likelihood of purchasing an ACT over other types of antimalarial drugs are listed in Table 4. In bivariate analyses, shop type, wealth, and the source of diagnoses were the only factors that were significantly associated with the likelihood of buying an ACT. In adjusted regressions, customers who went to PPMVs were significantly less likely to buy an ACT (OR = 0.371, 95% CI: 0.168-0.821). While having a diagnosis from a hospital, clinic, or laboratory was associated with increased likelihood of ACT purchase, this was only marginally significant at the 10% level. Differences in wealth were no longer significant in the multivariate specification, although a gradient was still observed.
Table 4. Logistic regression of the likelihood of buying an ACT (versus other anti-malarial drugs).
| ACT | Other anti-malarial | Bivariate | Multivariate | |||||||||
| n = 233 | % | n = 184 | % | P-value | OR1 | 95% CI | P-val | OR1 | 95% CI | P-val | ||
| Type of shop1 | PPMV | 136 | 58.4 | 136 | 29.3 | 0.002 | 0.296*** | 0.135–0.650 | 0.002 | 0.371** | 0.168–0.821 | 0.015 |
| Pharmacy | 97 | 41.6 | 97 | 70.7 | 1.000 | 1.000 | ||||||
| Age of respondents | 18–29 (reference) | 70 | 30.0 | 70 | 22.3 | 0.541 | 1.000 | |||||
| 30–39 | 64 | 27.5 | 64 | 29.3 | 1.441 | 0.800–2.595 | 0.224 | |||||
| 40–49 | 52 | 22.3 | 52 | 23.9 | 1.445 | 0.775–2.694 | 0.247 | |||||
| 50+ | 47 | 20.2 | 47 | 24.5 | 1.635 | 0.767–3.485 | 0.203 | |||||
| Sex | Male | 125 | 53.6 | 125 | 48.4 | 0.398 | 0.809 | 0.496–1.322 | 0.398 | |||
| Female (reference) | 108 | 46.4 | 108 | 51.6 | 1.000 | |||||||
| Education | No education (reference) | 18 | 7.7 | 18 | 6.5 | 0.182 | 1.000 | |||||
| Primary education | 36 | 15.5 | 36 | 9.8 | 0.750 | 0.300–1.873 | 0.538 | |||||
| Secondary education | 96 | 41.2 | 96 | 39.1 | 1.125 | 0.513–2.466 | 0.769 | |||||
| Higher education | 83 | 35.6 | 83 | 44.6 | 1.482 | 0.647–3.395 | 0.352 | |||||
| Marital status | Not married (reference) | 76 | 32.6 | 76 | 29.9 | 0.654 | 1.000 | |||||
| Married | 157 | 67.4 | 157 | 70.1 | 1.135 | 0.652–1.978 | 0.654 | |||||
| Employment status | Employed full time (reference) | 59 | 25.3 | 59 | 34.2 | 0.105 | 1.000 | |||||
| Employed part time | 6 | 2.6 | 6 | 2.7 | 0.780 | 0.174–3.499 | 0.746 | |||||
| Self-employed | 136 | 58.4 | 136 | 46.2 | 0.585** | 0.368–0.930 | 0.023 | |||||
| Unemployed | 32 | 13.7 | 32 | 16.8 | 0.907 | 0.541–1.522 | 0.712 | |||||
| Wealth quintile | Poorest (reference) | 50 | 21.5 | 50 | 14.7 | 0.008 | 1.000 | 1.000 | ||||
| Second | 59 | 25.3 | 59 | 14.1 | 0.816 | 0.454–1.466 | 0.497 | 0.652 | 0.357–1.192 | 0.165 | ||
| Third | 48 | 20.6 | 48 | 17.4 | 1.235 | 0.610–2.500 | 0.558 | 0.875 | 0.412–1.861 | 0.730 | ||
| Fourth | 44 | 18.9 | 44 | 23.9 | 1.852 | 0.870–3.943 | 0.110 | 1.234 | 0.615–2.477 | 0.554 | ||
| Richest | 32 | 13.7 | 32 | 29.9 | 3.183*** | 1.499–6.758 | 0.003 | 1.931 | 0.880–4.236 | 0.101 | ||
| Symptoms reported | ||||||||||||
| Fever, headache, dizziness | Yes | 171 | 73.4 | 171 | 73.4 | 0.996 | 0.999 | 0.635–1.571 | 0.996 | |||
| No (reference) | 62 | 26.6 | 62 | 26.6 | 1.000 | |||||||
| Body aches, chills, convulsions | Yes | 136 | 58.4 | 136 | 57.1 | 0.818 | 0.948 | 0.601–1.494 | 0.818 | |||
| No (reference) | 97 | 41.6 | 97 | 42.9 | 1.000 | |||||||
| Weak, fatigue, no appetite | Yes | 138 | 59.2 | 138 | 54.3 | 0.387 | 0.820 | 0.522–1.287 | 0.387 | |||
| No (reference) | 95 | 40.8 | 95 | 45.7 | 1.000 | |||||||
| Bitter taste in the mouth | Yes | 31 | 13.3 | 31 | 14.7 | 0.654 | 1.121 | 0.681–1.844 | 0.654 | |||
| No (reference) | 202 | 86.7 | 202 | 85.3 | 1.000 | |||||||
| Congestion, shallow breathing | Yes | 24 | 10.3 | 24 | 16.3 | 0.110 | 1.696 | 0.887–3.244 | 0.110 | |||
| No (reference) | 209 | 89.7 | 209 | 83.7 | 1.000 | |||||||
| Vomiting, diarrhea | Yes | 26 | 11.2 | 26 | 10.9 | 0.916 | 0.971 | 0.561–1.679 | 0.916 | |||
| No (reference) | 207 | 88.8 | 207 | 89.1 | 1.000 | |||||||
| Other: blisters, dark urine, yellow eyes | Yes | 33 | 14.2 | 33 | 11.4 | 0.448 | 0.781 | 0.412–1.480 | 0.448 | |||
| No (reference) | 200 | 85.8 | 200 | 88.6 | 1.000 | |||||||
| Number of days waited before seeking care1 | <1 day (reference) | 68 | 30.8 | 68 | 24.8 | 0.140 | 1.000 | |||||
| 1 day | 46 | 20.8 | 46 | 15.5 | 0.924 | 0.455–1.875 | 0.827 | |||||
| 2 days | 42 | 19.0 | 42 | 18.6 | 1.214 | 0.691–2.135 | 0.500 | |||||
| 3–5 days | 45 | 20.4 | 45 | 29.2 | 1.776** | 1.038–3.039 | 0.0362 | |||||
| 6 days or more | 20 | 9.0 | 20 | 11.8 | 1.615 | 0.798–3.269 | 0.183 | |||||
| Source of diagnosis | Myself/family/friend (reference) | 219 | 94.0 | 219 | 89.1 | 0.019 | 1.000 | 1.000 | ||||
| Hospital/clinic/lab | 4 | 1.7 | 4 | 7.1 | 4.340** | 1.323–14.24 | 0.0155 | 3.124* | 0.987–9.894 | 0.053 | ||
| Pharmacy/PPMV | 10 | 4.3 | 10 | 3.8 | 0.935 | 0.345–2.530 | 0.894 | 0.758 | 0.301–1.909 | 0.557 | ||
| Observations | 417 | 417 | ||||||||||
Odds ratios reported.
Pharmacy (n = 221), PPMV (n = 161), Total (n = 382).
Standard errors are clustered at the shop level;
***p<0.01,
**p<0.05,
*p<0.1.
RDT results and self-reported drug administration
Of the 457 enrolled participants, 3.9% (n = 18) were RDT-positive as seen in Table 5. During the phone follow-up survey, 97.9% (n = 415/424) of those reached reported that they felt better than the day they were enrolled into the study and 5.9% (n = 25/422) had sought additional care. For those who were RDT-positive (and for whom drug information is available), 68.8% (n = 11/16) reported taking an ACT; none took a non-ACT anti-malarial and all took some type of non-anti-malarial drug that they had also purchased (n = 12). Among RDT-negative participants, 28.9% still used some form of anti-malarial medication: 9.7% (n = 39/402) took an ACT and 19.2% (n = 77/402) took a non-ACT anti-malarial. For those who also purchased a non-anti-malarial, 76.5% (n = 189/247) took these drugs. When asked which places could be trusted to provide RDTs, 77.4% (n = 328/425) indicated hospitals or clinics and 17.5% (n = 74) named a diagnostic laboratory; only 4.2% stated pharmacies, 1.2% (n = 5) named PPMVs, and 3.5% (n = 15) indicated a family or friend could be trusted.
Table 5. RDT result and self-reported drug administration.
| n | N | % | ||
| RDT result | Positive | 18 | 457 | 3.9 |
| Negative | 439 | 457 | 96.1 | |
| Generally feeling better since baseline | Yes | 415 | 424 | 97.9 |
| No | 9 | 424 | 2.1 | |
| Drugs taken | ||||
| RDT-positive | ||||
| ACT | Yes | 11 | 16 | 68.8 |
| No | 5 | 16 | 31.3 | |
| Non-ACT anti-malarial | Yes | 0 | 16 | 0 |
| No | 0 | 16 | 0 | |
| Non-anti-malarial | Yes | 12 | 12 | 100 |
| No | 0 | 12 | 0 | |
| RDT-negative | ||||
| ACT | Yes | 39 | 402 | 9.7 |
| No | 363 | 402 | 90.3 | |
| Non-ACT anti-malarial | Yes | 77 | 402 | 19.2 |
| No | 325 | 402 | 80.8 | |
| Non-anti-malarial | Yes | 189 | 247 | 76.5 |
| No | 58 | 247 | 23.5 | |
| Sought additional care | Yes | 25 | 422 | 5.9 |
| No | 397 | 422 | 94.1 | |
| Places trusted to provide RDTs | ||||
| Hospital/clinic | Yes | 328 | 424 | 77.4 |
| No | 96 | 424 | 22.6 | |
| Diagnostic lab | Yes | 74 | 424 | 17.5 |
| No | 350 | 424 | 82.5 | |
| Pharmacy | Yes | 18 | 424 | 4.2 |
| No | 406 | 424 | 95.8 | |
| PPMV | Yes | 5 | 424 | 1.2 |
| No | 419 | 424 | 98.8 | |
| Community health worker | Yes | 23 | 424 | 5.4 |
| No | 401 | 424 | 94.6 | |
| Traditional healer | Yes | 4 | 424 | 0.9 |
| No | 420 | 424 | 99.1 | |
| Family/friend | Yes | 15 | 424 | 3.5 |
| No | 409 | 424 | 96.5 | |
| Felt well at follow up and RDT positive | ||||
| Took ACTs | Yes | 9 | 16 | 56.3 |
| No | 7 | 16 | 43.7 | |
| Took non- ACT anti-malarial | Yes | 7 | 16 | 43.7 |
| No | 9 | 16 | 56.7 | |
| Non- antimalarial | Yes | 0 | 16 | 0 |
| No | 16 | 16 | 100 | |
| Felt well at follow up and RDT negative | ||||
| Took ACTs | Yes | 206 | 389 | 53.0 |
| No | 183 | 389 | 47.0 | |
| Took non- ACT anti-malarial | Yes | 181 | 389 | 46.5 |
| No | 208 | 389 | 53.5 | |
| Non- antimalarial | Yes | 2 | 389 | 0.5 |
| No | 387 | 389 | 99.5 | |
Discussion
Like elsewhere in sub-Saharan Africa [17], [24]–[26], medicine retailers in Nigeria are an important source of treatment for uncomplicated malaria even though the quality of care and knowledge among these providers is poorer compared to other types of health professionals. This study sought to better characterize the practice of presumptive treatment at drug outlets in Nigeria. Recruited as they exited drug shops, nearly all study participants reported that they had self-diagnosed their condition and chose to patron the particular shop because it was either their usual place to buy drugs or was convenient. Individuals who went to PPMVs were typically younger, poorer, waited fewer days before seeking care, and had not gone to a hospital/clinic for diagnosis. These results suggest that relatively poorer populations, and potentially less-educated, are disproportionately serviced by PPMVs, potentially motivated by a variety of factors, including proximity and accessibility [27], [28] and cost [29], [30].
In this study, even though patrons of PPMVs spent less on their drug purchases on average, they were also more likely to purchase sub-standard, non-ACT anti-malarials. Going to a PPMV was the largest risk factor for not buying an ACT, indicating that PPMVs continue to sell non-recommended drugs for malaria. Studies show that receiving ACTs is highly associated with consumer demand [6], and that PPMVs in particular tend to sell what customers demand and avoid referring patients for confirmatory blood tests because they fear losing customers due to added inconvenience or cost [18]. Thus, consumer preferences for presumptive treatment and non-recommended drugs may drive individuals to patron PPMVs rather than pharmacies, even both types of outlets are generally perceived to provider lower quality services than hospitals or clinics [31]. Profit motives may further constrain proper dispensing behavior due to strong consumer demand for substandard drugs [26].
In addition to fever, many participants attributed a wide variety of symptoms to malaria, and those going to PPMVs were especially likely to name symptoms unrelated to malaria. Further, only 3.9% of sick adults seeking care for malaria were found to be positive for malaria using an RDT. This corroborates qualitative evidence that malaria is identified as the illness for a large swath of conditions in Nigeria [18], and that malaria is over-diagnosed and over-treated, similar to other urban areas of Nigeria [32] and elsewhere in sub-Saharan malaria-endemic countries [33]–[36]. There is also an entrenched perception that malaria is rampant and many people have been regaled with the need to treat malaria promptly by public health messages in the past aimed at increasing awareness. This highlights the importance of malaria behavior change messages that inform people that not all fever cases can be attributed to malaria and the need for individuals to seek out malaria diagnosis.
Although the study did not have a comparison control group, it is assumed that most sick individuals who purchased malaria drugs in this study were intending to take their purchased drugs to presumptively treatment him/herself. Over 44% of participants bought ACTs and the median amount spent on purchasing anti-malarial drugs was 240 Naira (∼US$1.50). This level of overtreatment suggests that large quantities of ACTs may be wasted if reliable testing is not first carried out. It is therefore imperative to train all health workers as well as the populace on malaria symptoms and the need for a diagnostic test has become vital in health communications and education. Since PPMVs and pharmacies serve the majority of the population seeking treatment for malaria, standard diagnostic testing prior to treatment should be considered as part of a concerted strategy for malaria control. Some countries, including Tanzania, Senegal, and Zambia have successfully implemented RDTs in the public health sector and provider acceptability has improved over time, resulting in sizable cost-savings [7]–[10]. Further, this is the first study to assess patient adherence to test results (rather than provider prescription behavior) showing that simply providing diagnostic information to sick individuals can result in high rates of appropriate treatment behavior [22].
In addition, this also underscores the need to provide alternative means of management of non-malaria febrile illness. There is currently not a good understanding of the etiology of non-malaria febrile illnesses and only a handful of studies have documented the variety of causes of pediatric illnesses in select countries [33], [37]. Such information is vital for developing more comprehensive treatment guidelines for childhood illnesses that are country-relevant and should be the focus of future studies.
Limitations of the study
Populations in Southwest Nigeria are likely to be from higher socioeconomic status than populations in other areas of the country and consequently likely to be healthier overall [14]. A sample of adults as carried out in the study may not necessarily be representative of children under five who are yet to develop immunity to malaria. Further studies will be needed to look at the incidence of malaria in this group as well as in other parts of Nigeria to determine if this picture is consistent nationwide. Characteristics of the shop and its workers may also be important determinants of shop patronage and buying drugs which the current study was not able to capture, but which future studies will aim to include in the assessment of care-seeking behavior for malaria.
The study could not look at counterfeit or substandard drugs purchased at the medicine shops. However, quality-assured ACTs were given free of charge in order to address the risk of participants taking substandard drugs. Although shop workers did not participate in the recruitment or screening of customer participants, they may have altered their sales or prescriptive behavior in ways that we cannot account for.
Acknowledgments
The authors wish to acknowledge Exxon Mobil and the Global Fund to Fight AIDS, Tuberculosis and Malaria. Our appreciation also goes to the drug stores and PPMVs shops where the study was implemented, as well as the participants who agreed to receive an RDT and answer survey questions. Many thanks to Adetunji Ilori for excellent assistance in field work management and surveyor training, Tunde Ogunbenro for facilitating and supporting project management, and Alana Schwartz at San Francisco General Hospital for lab assistance. We are grateful for the comments and feedback from seminar participants at the UCSF Global Health Sciences and Infectious Diseases Group, the 6th MIM (Multilateral Initiative on Malaria) Pan-African Malaria Conference, the Population Association of America Annual Meeting, the International Health Economics Association Conference, Stanford School of Medicine's General Medical Disciplines Departmental Seminar, and the World Social Marketing Conference.
Funding Statement
The authors wish to acknowledge ExxonMobil for financial support of this study as well as the Global Fund to Fight AIDS, Tuberculosis and Malaria for provision of RDTs and ACTs for the study. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.WHO World Malaria Report 2008. Available: http://www.who.int/malaria/publications/world_malaria_report_2008/en/index.html. Accessed 2014 Feb 20.
- 2. Okeke TA, Uzochukwu BSC, Okafor HU (2006) An in-depth study of patent medicine sellers' perspectives on malaria in a rural Nigerian community. Malaria Journal 2006 5: 97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Onwujekwe O, Chima R, Okonkwo P (2000) Economic burden of malaria illness versus that of a combination of all other illnesses. A study in five malaria holo-endemic communities. Health Policy 54: 143–159. [DOI] [PubMed] [Google Scholar]
- 4.WHO World Malaria Report 2010. Available: http://www.who.int/malaria/publications/atoz/9789241547925/en/index.html. Accessed 2014 Feb 20.
- 5.AMFm Independent Evaluation Team (2012) Independent Evaluation of Phase 1 of the Affordable Medicines Facility - malaria (AMFm), Multi-Country Independent Evaluation Report: Final Report. Calverton, Maryland and London: ICF International and London School of Hygiene and Tropical Medicine.
- 6.Mangham LJ, Cundill B, Ezeoke O, Nwala E, Uzochukwu BS, et al. (2011) Treatment of uncomplicated malaria at public health facilities and medicine retailers in south-eastern Nigeria. Malar J 10(1): : 155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hamer DH, Ndhlovu M, Zurovac D, Fox M, Yeboah-Antwi K, et al. (2007) Improved diagnostic testing and malaria treatment practices in Zambia. JAMA: the journal of the American Medical Association 297(20): 2227–2231. [DOI] [PMC free article] [PubMed]
- 8.Masanja MI, McMorrow M, Kahigwa E, Kachur SP, McElroy PD (2010) Health workers' use of malaria rapid diagnostic tests (RDTs) to guide clinical decision making in rural dispensaries, Tanzania. The American journal of tropical medicine and hygiene 83(6): : 1238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Thiam S, Thior M, Faye B, Ndiop M, Diouf ML, et al. (2011) Major reduction in anti-malarial drug consumption in Senegal after nation-wide introduction of malaria rapid diagnostic tests. PLOS One 6(4): : 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yukich J, D'Acremont V, Kahama J, Swai M, Lengeler C (2010) Cost savings with rapid diagnostic tests for malaria in low-transmission areas: evidence from Dar es Salaam, Tanzania. American Journal of Tropical Hygiene and Medicine 83(1): : 61–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Cohen J, Fink G, Berg K, Aber F, Jordan M (2012) Feasibility of distributing rapid diagnostic tests for malaria in the retail sector Evidence from an implementation study in Uganda. PLOS One 7(11): 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Retail prices of ACTs co-paid by the AMFm and other antimalarial medicines: Ghana, Kenya, Madagascar, Nigeria, Tanzania and Uganda Report of price tracking surveys. August 2013. Available: http://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=4&ved=0CDcQFjAD&url=http%3A%2F%2Fwww.theglobalfund.org%2Fdocuments%2Famfm%2FAMFm_PriceTrackingByHAIAugust2013Survey_Report_en%2F&ei=ZdwDU9-eDJfYoASto4G4DQ&usg=AFQjCNHk61FW85C0QSf2L2qG8CEnvGc7Xw&bvm=bv.61535280, d.cGU&cad = rja. Accessed 2014 Feb 20.
- 13. Uzochukwu BSC, Onwujekwe E, Ezuma NN, Ezeoke OP, Ajuba MO, et al. (2011) Improving rational treatment of malaria: perceptions and influence of RDTs on prescribing behaviour of health workers in southeast Nigeria. PLOS One 6: e14627.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.National Population Commission (NPC), National Malaria Control Programme (NMCP), ICF International (2012) Nigeria Malaria Indicator Survey 2010. Abuja, Nigeria: NPC, NMCP, and ICF International.
- 15. Salako LA, Brieger WR, Afolabi BM, Umeh RE, Agomo PU, et al. (2001) Treatment of childhood fevers and other illnesses in three rural Nigerian communities. Tropical Pediatrics 47: 38–46. [DOI] [PubMed] [Google Scholar]
- 16. Oladepo O, Kabiru S, Adeoye BW, Oshiname F, Ofi B, et al. (2008) Malaria treatment in Nigeria: the role of patent medicine vendors. The Future Health Systems, Innovations and knowledge for future health systems for the poor. Policy Brief March 2008: 01.. [Google Scholar]
- 17. Goodman C, Brieger W, Unwin A, Mills A, Meek S, et al. (2007) Medicine sellers and malaria treatment in sub-Saharan Africa: what do they do and how can their practice be improved? Am J Trop Med Hyg 77: 203–218.. [PMC free article] [PubMed] [Google Scholar]
- 18. De La Cruz A, Liu J, Schatzkin E, Modrek S, Oladepo O, et al. (2012) The Influence of policy, hierarcy, and competition on malaria case management among retail providers in Nigeria. Poster #342 presented at the American Society for Tropical Medicine and Hygiene 62nd Annual Meeting, Atlanta GA [Google Scholar]
- 19. Ezeoke OP, Ezumah NN, Chandler CC, Mangham-Jefferies LJ, Onwujekwe OE, et al. (2012) Exploring health providers' and community perceptions and experiences with malaria tests in South-East Nigeria: a critical step towards appropriate treatment. Malar J 11: 368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Bastiaens GJH, Bousema T, Leslie T (2014) Scale-up of Malaria Rapid Diagnostic Tests and Artemisinin Based Combination Therapy: Challenges and Perspectives in Sub-Saharan Africa. PLOS Med 11(1): e1001590 doi:10.1371/journal.pmed.1001590 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Basu S, Modrek S, Bendavid E (2014) Comparing decisions for malaria testing and presumptive treatment: a net health benefit analysis. Med Decis Making 2014 May 14. pii: 0272989X14533609. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 22. Modrek S, Schatzkin E, De La Cruz A, Isiguzo C, Nwokolo E, et al. (2014) Malaria Journal 2014. 13: 69.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Filmer D, Pritchett LH (2001) Estimating Wealth Effects without Expenditure Data—Or Tears: An Application to Educational Enrollments in States of India. Demography Volume 38 (Issue 1) 115–132. [DOI] [PubMed] [Google Scholar]
- 24. Nshakira N, Kristensen M, Ssali F, Reynolds Whyte S (2002) Appropriate treatment of malaria? Use of antimalarial drugs for children's fevers in district medical units, drug shops and homes in eastern Uganda. Tropical Medicine & International Health 7(4): 309–316. [DOI] [PubMed] [Google Scholar]
- 25. Hetzel MW, Dillip A, Lengeler C, Obrist B, Msechu JJ, et al. (2008) Malaria treatment in the retail sector: knowledge and practices of drug sellers in rural Tanzania. BMC public health 8(1): 157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wafula FN, Goodman CA (2010) Are interventions for improving the quality of services provided by specialized drug shops effective in sub-Saharan Africa? A systematic review of the literature. International Journal for Quality in Health Care 22(4): : 316–323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Snow RW, Peshu N, Forster D, Mwenesi H, Marsh K (1992) The role of shops in the treatment and prevention of childhood malaria on the coast of Kenya. Transactions of the Royal Society of Tropical Medicine and Hygiene 86(3): 237–239. [DOI] [PubMed] [Google Scholar]
- 28. Van Der Geest S (1987) Self-care and the informal sale of drugs in South Cameroon. Social science & medicine 25(3): 293–305. [DOI] [PubMed] [Google Scholar]
- 29. Amin AA, Marsh V, Noor AM, Ochola SA, Snow RW (2003) The use of formal and informal curative services in the management of paediatric fevers in four districts in Kenya. Tropical Medicine & International Health 8(12): 1143–1152. [DOI] [PubMed] [Google Scholar]
- 30.Brieger WR, Sesay HR, Adesina H, Mosanya ME, Ogunlade PB, et al. (2000) Urban malaria treatment behaviour in the context of low levels of malaria transmission in Lagos, Nigeria. African journal of medicine and medical sciences 30: : 7–15. [PubMed] [Google Scholar]
- 31. Onwujekwe O, Onoka C, Uguru N, Nnenna T, Uzochukwu B, et al. (2010) Preferences for benefit packages for community-based health insurance: an exploratory study in Nigeria BMC Health Services Research. 10: 162.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Oyibo WA (2013) Overdiagnosis and Overtreatment of Malaria in Children That Presented with Fever in Lagos, Nigeria. ISRN Infectious Diseases, 2013 [Google Scholar]
- 33. Crump JA, Morrissey AB, Nicholson WL, Massung RF, Stoddard RA, et al. (2013) Etiology of severe non-malaria febrile illness in northern Tanzania: a prospective cohort study. PLOS neglected tropical diseases 7(7): e2324.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Reyburn H, Mbatia R, Drakeley C, Carneiro I, Mwakasungula E, et al. (2004) Overdiagnosis of malaria in patients with severe febrile illness in Tanzania: a prospective study. : British Medical Journal; 329(7476): 1212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Okebe JU, Walther B, Bojang K, Drammeh S, Schellenberg D, et al. (2010) Prescribing practice for malaria following introduction of artemether-lumefantrine in an urban area with declining endemicity in West Africa. Malaria journal 9(1): 180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Mangham LJ, Cundill B, Achonduh OA, Ambebila JN, Lele AK, et al. (2012) Malaria prevalence and treatment of febrile patients at health facilities and medicine retailers in Cameroon. Tropical Medicine & International Health 17(3): 330–342.. [DOI] [PubMed] [Google Scholar]
- 37. Acestor N, Cooksey R, Newton PN, Menard D, Guerin PJ, et al. (2012) Mapping the aetiology of non-malarial febrile illness in Southeast Asia through a systematic review—terra incognita impairing treatment policies. PLOS one 7(9): e44269.. [DOI] [PMC free article] [PubMed] [Google Scholar]