Abstract
Objectives:
The aim of this study was to assess female university students’ knowledge of breast cancer and its preventative measures and to identify their main misconceptions regarding breast cancer.
Methods:
This cross-sectional study was conducted between April 2011 and June 2012 and included female students from three large universities in Ajman, United Arab Emirates (UAE). A stratified random sampling procedure was used. Data were collected through a validated, pilot-tested, self-administered questionnaire. The questionnaire included 35 questions testing knowledge of risk factors, warning signs and methods for the early detection of breast cancer. Participants’ opinions regarding breast cancer misconceptions were also sought.
Results:
The participants (n = 392) were most frequently between 18 and 22 years old (63.5%), non-Emirati (90.1%) and never married (89%). A family history of breast cancer was reported by 36 (9.2%) of the students. The percentage of participants who had low/below average knowledge scores regarding risk factors, warning signs and methods for early detection of breast cancer was 40.6%, 45.9% and 86.5%, respectively. Significantly higher knowledge scores on risk factors were noticed among participants with a family history of breast cancer (P = 0.03). The misconception most frequently identified was that “treatment for breast cancer affects a woman’s femininity” (62.5%).
Conclusion:
A profound lack of knowledge about breast cancer was noted among female university students in the three UAE universities studied. The most prominent gaps in knowledge identified were those concerning breast cancer screening methods.
Keywords: Breast Cancer, Awareness, Students, United Arab Emirates
Advances in Knowledge
- This study found that female university students in the United Arab Emirates (UAE) showed a profound lack of knowledge about breast cancer. This was particularly the case with regards to knowledge about breast cancer screening methods.
- Given the lack of published data about female university students’ knowledge of breast cancer in the UAE, the results of this study could be used as a baseline for planning future breast cancer education programmes for young women. These programmes should reflect the specific needs of this population, taking into account all of the identified barriers and misconceptions noted in this study.
Application to Patient Care
- The findings of this study highlight the need to raise awareness of breast cancer among female university students. Self-awareness can help prevent the late detection of breast cancer and thereby improve survival rates.
- Students are an easily accessible target group for breast cancer education and it is important that they be included in educational programmes. Increased knowledge of breast cancer among female university students would be an asset in disseminating correct information among the community.
Breast cancer is the most common cancer in women; in 2004, it comprised 16% of all female cancers and was the cause of death for 519,000 women worldwide.1 Available data from the USA show that between 2005 and 2006 the highest incidence rate of breast cancer was among women aged 75–79 years and the median age at the time of diagnosis was 61 years.2 In the UK, approximately 80% of cases occur in women over the age of 50 years, with the peak ages being 50–64 years.3 In the Eastern Mediterranean region (EMR), breast cancer is the most commonly diagnosed cancer in women and the second leading cause of cancer-related deaths.4 In the United Arab Emirates (UAE), breast cancer is the most common female cancer, accounting for 22.8% of diagnosed cases.5 However, 12% of these patients were less than 35 years of age at their first diagnosis, while 74% were less than 54 years of age.5 This average age at first diagnosis is earlier than those observed in the USA and UK. These data suggest that it is necessary to raise breast cancer awareness among young women in the UAE.
In the UAE, there is a marked underutilisation of existing public screening services for breast cancer. In 2007, only 12% of the targeted female population underwent screening using a mammography.6 An inadequate awareness of and widespread misconceptions about breast cancer were identified as barriers that affect the utilisation of the existing public screening services.6 It has been suggested that the enhancement of knowledge and the correction of misconceptions among young women will stimulate positive attitudes towards breast cancer education and make them more ‘breast aware’, which in turn may promote the earlier detection of breast cancer.7
The present study aimed to assess the knowledge of female university students in the UAE regarding breast cancer and its preventive measures and to identify the main misconceptions regarding breast cancer among this population.
Methods
This cross-sectional study was conducted between April 2011 and June 2012 and included female students from three large universities in Ajman, UAE. These universities were the Gulf Medical University (U1), Ajman University of Science & Technology (U2) and Preston University Ajman (U3). One of the universities offers only medical/health-related programmes (U1), while the other two offer mainly science and technology programmes (U2 and U3). Female participants of 18 years of age or older, who were registered students in any of the three selected universities and who were available during the data collection period were included in the study. Students who were male or who were attending other universities were excluded from the study.
In order to overcome variability in the various curricula regarding health-related knowledge and obtain adequate representation from all programmes offered in the three universities, a stratified random sampling procedure was adopted to recruit the participants. A minimum of 10 samples were therefore selected from each programme taught in the three universities. An equal number of questionnaires (n = 150) were distributed among the three universities (n = 450) so as to have an equal representation of the female students from all three universities.
A validated, pilot-tested and self-administered questionnaire was used as a data collection tool. The questionnaire included knowledge questions in three subdomains: risk factors, signs of and methods for the early detection of breast cancer. The first subdomain, concerning knowledge of breast cancer risk factors, was based on guidelines and information published by the World Health Organization (WHO) Regional Office for the Eastern Mediterranean and the American Cancer Society.8,9 Using Cronbach’s alpha coefficient, the internal consistency and reliability of this subdomain was 0.85. The second and third knowledge subdomains were warning signs of breast cancer and methods for the early detection of breast cancer.10 A scoring system was used to analyse the students’ knowledge: a score of one was given for a correct response while a score of zero was given for an incorrect answer or if the participant responded ‘I don’t know’. To compare the participants’ knowledge in the three subdomains, quartiles of correct total scores in the subdomains were used to categorise participants’ scores as either low (quartile 1), below average (quartile 2), above average (quartile 3) or high (quartile 4). The frequency and percentage of correct answers in these categories for each subdomain was subsequently calculated. Knowledge scores were compared in relation to the participants’ demographic characteristics (age, nationality, university, marital status and family history of breast cancer). The questionnaire also aimed to determine the participants’ breast self-examination (BSE) practices, their main sources of breast cancer information and their opinions regarding breast cancer and its effect on women. These latter questions were based on misconceptions concerning breast cancer identified in a previous survey.7
Data were entered into an Excel spreadsheet, Version 2011 (Microsoft Corp., Redmond, Washington, USA) and analysed using the Statistical Package for the Social Sciences (SPSS), Version 19 (IBM, Corp., Chicago, Illinois, USA). The Kruskal-Wallis test for independent samples, Mann-Whitney U test and Pearson’s Chi-squared test were used to analyse the data.
This study was funded by the WHO and the research adhered to ethical conduct guidelines. The study was approved by the Ethics Review Committees of the Gulf Medical University and the WHO Regional Office for the Eastern Mediterranean. Informed consent was taken from the participants before their enrolment in the study and the confidentiality of information was respected.
Results
A total of 392 students took part in the study (response rate = 87%), with 142, 137 and 113 students from U1, U2 and U3, respectively. Participants were mostly between 18 and 22 years of age (63.5%), expatriates (90.1%) and never married (89%). The age of the participants ranged from 16–47 years, with a median age of 21 years and a mean of 21.2 ± 3.5 years. None of the participants reported currently having breast cancer, although a family history of breast cancer was reported by 36 students (9.2%), mostly in second-degree relatives (n = 23, 63.9%).
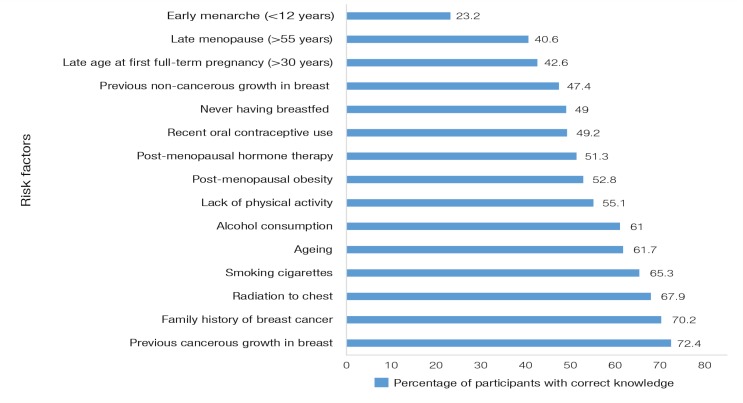
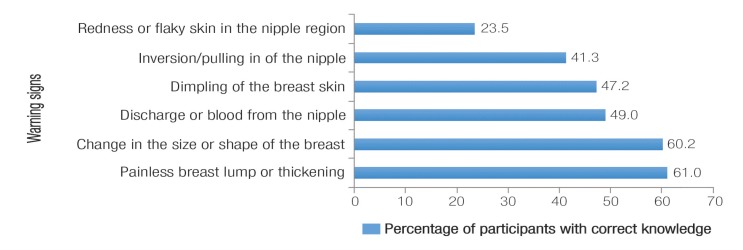
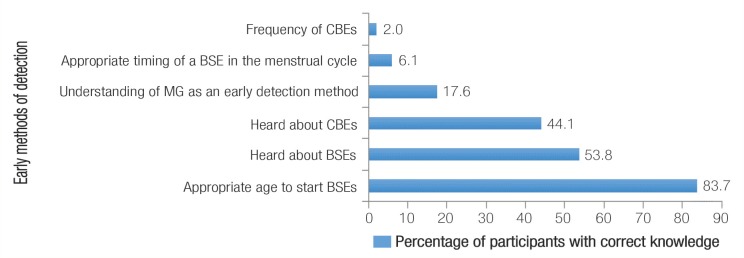
The percentage of participants who had scores indicating correct knowledge regarding risk factors and warning signs for breast cancer are shown in Figures 1 and 2. More than 50% of the participants did not have correct knowledge regarding the majority of the risk factors and warning signs. Only 49% knew that never breastfeeding could be a risk factor for breast cancer. The proportion of those who knew that obesity, cigarette smoking and a lack of physical activity increased the risk of breast cancer were 53%, 65% and 55%, respectively. Figure 3 shows the percentage of correct answers regarding methods for the early detection of breast cancer. Only 69 participants (17.6%) correctly identified mammography as a method for the early detection of breast cancer. Additionally, approximately half of the students had never heard of BSEs and clinical breast examinations (CBEs), at 46.2% and 55.9%, respectively. The vast majority of the participants did not have any knowledge regarding the recommended frequency of BSE (98%) or its timing in relation to their menstrual cycle (94%).
Figure 1:
The percentage of correct answers among participants regarding breast cancer risk factors (N = 392).
Figure 2:
The percentage of correct answers among participants regarding warning signs for breast cancer (N = 392).
Figure 3:
The percentage of correct answers among participants regarding methods for the early detection of breast cancer (N = 392).
CBE = clinical breast examination; BSE = breast self-examination; MG = mammography.
The median knowledge scores of participants by age, nationality, university, marital status and family history of breast cancer and the significance of these median differences are shown in Table 1. The variability between participants’ knowledge scores (as observed in the wide standard deviation) made the mean an unreliable measure in reflecting the knowledge of the group. In consequence, median scores were used for comparison [Table 1]. Significantly higher knowledge scores regarding risk factors for breast cancer were noted among participants from the university offering only medical/health-related programmes and those with a family history of breast cancer, compared to their respective counterparts. With regards to knowledge about methods for the early detection of breast cancer, significant differences by age and university were also observed.
Table 1:
Knowledge scores of participants in the three breast cancer subdomains by age, nationality, marital status, university and family history of breast cancer (N = 392)
| Demographic variables | n | Knowledge scores, median (range) | |||||
|---|---|---|---|---|---|---|---|
| Risk factors | P value | Warning signs | P value | Early detection methods | P value | ||
| Age in years* | |||||||
| <18 | 57 | 10.0 (0–18) | 0.598 | 5 (0–8) | 0.421 | 3 (1–6) | 0.002 |
| 18–20 | 133 | 10.0 (0–18) | 5 (0–8) | 3 (0–6) | |||
| 20–22 | 116 | 11.0 (0–18) | 5 (0–8) | 3 (1–6) | |||
| 22–24 | 48 | 11.0 (0–18) | 5 (0–7) | 4 (2–7) | |||
| ≥25 | 38 | 10.5 (0–18) | 5 (0–8) | 4 (2–8) | |||
| Nationality** | |||||||
| Emirati | 39 | 11.0 (0–18) | 0.680 | 5 (0–8) | 0.502 | 3 (0–6) | 0.779 |
| Non-Emirati | 353 | 11.0 (0–18) | 5 (0–8) | 3 (1–8) | |||
| Marital status** | |||||||
| Never married | 349 | 11.0 (0–18) | 0.796 | 5 (0–8) | 0.994 | 3 (0–7) | 0.13 |
| Married or previously married | 43 | 11.0 (0–17) | 5 (0–8) | 4 (2–8) | |||
| University* | |||||||
| 1 | 142 | 12.0 (0–18) | <0.001 | 5 (0–8) | 0.01 | 3 (0–7) | 0.001 |
| 2 | 137 | 11.0 (0–18) | 5 (0–8) | 3 (1–8) | |||
| 3 | 113 | 8.0 (0–17) | 4 (0–8) | 3 (1–6) | |||
| Family history of breast cancer** | |||||||
| Yes | 36 | 12.5 (2–18) | 0.03 | 5 (0–8) | 0.629 | 3 (2–7) | 0.469 |
| No | 356 | 11.0 (0–18) | 5 (0–8) | 3 (0–8) | |||
Kruskal-Wallis test;
Mann-Whitney U test.
An analysis of the knowledge scores in the three subdomains is shown in Table 2. The percentage of students who had low or below average knowledge scores in the three knowledge subdomains was 40.6%, 45.9% and 86.5%, for the risk factors, warning signs and early detection methods domains, respectively. This demonstrated that the most evident gap in knowledge among the participants concerned methods for the early detection of breast cancer.
Table 2:
Participants’ scores in the three breast cancer knowledge subdomains by quartile (N = 392)
| Score | Knowledge subdomain | ||
|---|---|---|---|
| Risk factors | Warning signs | Early detection methods | |
| Quartile, n (%)* | |||
| 1 | 54 (13.8) | 120 (30.6) | 138 (35.2) |
| 2 | 105 (26.8) | 60 (15.3) | 201 (51.3) |
| 3 | 165 (42.1) | 140 (35.7) | 48 (12.2) |
| 4 | 68 (17.3) | 72 (18.4) | 5 (1.3) |
| Mean ± SD | 9.8 ± 4.8 | 3.9 ± 2.7 | 3.2 ± 1.2 |
| Median | 11.0 | 5.0 | 3.0 |
| Range | 0–18 | 0–8 | 0–8 |
SD = standard deviation.
Quartiles of correct total scores in the subdomains were used to categorise participants’ scores as either low (quartile 1), below average (quartile 2), above average (quartile 3) or high (quartile 4).
Table 3 shows the participants’ median knowledge scores when divided according to their BSE practice. Participants were asked how often they practiced BSE and were categorised according to their response: no practice, rarely, sometimes and every month. Only 89 participants (22.7%) admitted to having ever conducted a BSE and only 13 (3.3%) of the students practiced monthly BSEs. The median knowledge scores of participants who conducted BSEs were significantly higher in all three subdomains compared to those who indicated that they did not practise BSE.
Table 3:
Breast cancer knowledge scores of participants among breast self-examination practice groups (N = 392)
| BSE practice | n | Knowledge scores, median (range) | |||||
|---|---|---|---|---|---|---|---|
| Risk factors | P value | Warning signs | P value | Early detection methods | P value | ||
| None | 303 | 10.0 (0–18) | 4.0 (0–8) | 3.0 (0–6) | |||
| Rarely | 42 | 11.5 (0–18) | 0.02 | 6.0 (0–8) | <0.001 | 4.0 (2–7) | <0.001 |
| Sometimes | 34 | 11.0 (1–18) | 5.0 (0–7) | 4.0 (2–7) | |||
| Every month | 13 | 13.0 (0–18) | 6.0 (4–8) | 5.0 (3–8) | |||
BSE = breast self-examination.
The most frequent breast cancer misconceptions reported by the study participants were that: treatment for breast cancer affects a woman’s femininity (62.5%); herbal remedies can treat breast cancer (56.4%); there is little that can be done to prevent cancer (49.7%); breast cancer inevitably results in death (44.4%); men do not get breast cancer (38%); they were too young to worry about breast cancer (35.5%); individuals can only get breast cancer if they have a family history of breast cancer (21.4%), and that breast cancer is the result of a curse or due to the ‘evil eye’ (19.4%). The reported sources of information for breast cancer were, in descending order, the media (72.4%), the internet (59.9%), doctors/nurses/health workers (37%), previous lectures in college/curriculum materials (31.6%), relatives (27%) and scientific journals/meetings (24.5%).
Discussion
In the UAE, breast cancer is the most common form of cancer in females among both citizens and non-citizens.3 The annual report of the UAE Ministry of Health in 2008 showed that 28% of deaths attributed to breast cancer occurred in women less than 45 years of age.11 Data regarding breast cancer knowledge and preventative practices among female university students in the UAE are limited. Several factors affect an individual’s risk of developing breast cancer, some of which are modifiable and largely related to lifestyle, social, economic and environmental factors.12 A study conducted in 2010 showed that 26.8% of breast cancer cases in the UK were attributable to lifestyle and environmental factors.13 It is essential for women to know about these factors early in life so they can make the right lifestyle choices concerning these risk factors, since an increase in women’s awareness can change their risk perceptions and behaviours.14 The current study found that there was a profound lack of knowledge regarding breast cancer among a group of female university students at three universities in the UAE.
In this study, many participants correctly identified that a personal and family history of breast cancer was a risk factor, which correlates with other researchers’ findings.15 However, a lack of knowledge was noted among a large proportion of the participants regarding modifiable risk factors for breast cancer, such as the risk of never breastfeeding. This is thought to be a risk factor because various physiopathological mechanisms are involved in the protective effect of breastfeeding: anovulation, cellular differentiation of the mammary cells and excretion in the milk of breast carcinogens.16 Obesity, cigarette smoking and a lack of physical activity also increase the risk of breast cancer; however, only 53%, 65% and 55% of participants, respectively, were aware of this. A similar study in Turkey reported that the percentage of their participants who were aware of these three risk factors was 23%, 64% and 43%, respectively.7 A study from Buraidah, Saudi Arabia, showed that the most frequently reported risk factors for breast cancer were not breastfeeding and the use of female sex hormones.17 It should be noted here that an increase in awareness about risk factors and risk-reducing strategies are important for the primary prevention of breast cancer.
Having adequate knowledge of the warning signs and symptoms of breast cancer, and being able to report any noticed abnormalities to healthcare providers, is part of what is known as “breast awareness”. This self-awareness can help in preventing the late detection of breast cancer and thereby improve survival rates.18 In this study, the percentage of participants who had correct knowledge scores regarding breast cancer warning signs was <60% for the majority of the signs mentioned in the questionnaire. Low levels of knowledge about breast cancer warning signs were also reported in a study of university students in Saudi Arabia.19 In Nigeria, only 70.7% of observed undergraduate females knew that there were warning signs of breast cancer.20
With regards to knowledge regarding measures for the early detection of breast cancer, it was worrying to find that most of the participants (86.5%) in the current study had low or below average knowledge regarding methods for early detection of breast cancer. A greater emphasis is required to address this knowledge gap in future educational campaigns directed at the female university population. Specifically, the majority of the participants were unaware that mammography is a useful method for the early detection of breast cancer. Additionally, approximately half of the students had never heard of BSE and CBE practices. In contrast, a study among female health workers in Nigeria reported that 81% of the participants mentioned mammography as a breast cancer diagnostic method, although only 46% mentioned BSE and CBE as diagnostic techniques.21 In Saudi Arabia, only 51.8% of the female university students studied by Habib et al. knew of mammography as a screening tool for breast cancer.19 The vast majority of the current study’s participants were unaware of the recommended frequency of BSE (98%) or its timing in relation to their menstrual cycle (94%). This finding is in agreement with data from Saudi Arabia, where approximately 86% of the female university students questioned did not know about the recommended frequency of BSE.19
In this study, age was found to be a significant determinant of knowledge related to methods for the early detection of breast cancer. It was found that younger participants had significantly lower knowledge scores in comparison to older participants. This finding is similar to that of a study from Australia.22 It should be noted that the confounding effect of maturity cannot be excluded in this study and that the observed improvement in the knowledge scores of older female students may not be related to the effect of the curriculum; especially as only 31% of the students considered the curriculum to be the main source of their information. Concerning nationality, no significant differences between knowledge scores were noted between Emirati and non-Emirati participants, which may indicate the possibility that cultural and ethnic factors have no significant effect on breast cancer awareness. However, a study in Singapore by Sim et al. found that that race was a significant independent factor affecting breast cancer knowledge.23 Another explanation, therefore, could be that the participants of the current study all had similar levels of education, likely diminishing the effect of cultural and ethnic factors.
The difference in the knowledge scores of participants from different universities may be attributed to the types of courses or programmes offered at each university and their basic curriculums. A similar observation was made in another study of university students from Angola.24 However, basic information about breast cancer should be provided to all young female students, irrespective of their educational programmes, in order to enhance overall awareness and influence positive behaviours related to breast cancer screening and prevention.
A family history of breast cancer was reported by 9% of the participants, which is very close to findings from a Saudi Arabian study by Sait et al. (9.8%) and from the Lebanese National Mammography Campaign in 2009 (8.9%).25,26 Interestingly, participants with a family history of breast cancer had significantly higher knowledge scores on breast cancer risk factors. This is consistent with a logistic regression model from another Saudi Arabian study among adult women in a primary healthcare setting.27
Researchers have identified misconceptions as an independent factor associated with a delay in seeking healthcare.28 Misconceptions also affect how women assess screening efficacy and make decisions about pursuing breast cancer screening.28 There were many misconceptions reported by the participants of the current study. For example, just over 44% of the participants thought that developing breast cancer inevitably resulted in death. A study from Pennsylvania in the USA showed that a fatalistic attitude influenced the breast cancer knowledge and screening practices of the participants since it led them to believe that there was little they could do to prevent cancer and death.29
Communication channels for health information have changed greatly in recent years. Selecting the right channels and materials based on the required behavioural change and knowledge of the target audience is essential in influencing health behaviours. In this study, the media was the major contributor to the participants’ knowledge of breast cancer. Other researchers have reported similar findings from Lebanon,26 Saudi Arabia17 and Iran.30 Greater attention should be directed to this medium to ensure that correct information regarding breast cancer reaches the target population.
Female university students are an easily accessible target group that should be included in breast cancer educational programmes. In addition, female university students may help in disseminating correct information and developing positive attitudes towards breast cancer detection among relatives, family members and friends. This approach would amplify the benefits of breast cancer education in the community as a whole.
Conclusion
A high proportion of female university students in the UAE have inadequate knowledge about breast cancer. In this study, the percentage of students who had low or below average knowledge scores in the three knowledge subdomains was similar to the percentages reported in similar studies conducted in the region. This suggests that a lack of knowledge regarding breast cancer is a regional issue and is not limited to Ajman or the UAE. More than half of the participants falsely believed that the treatment for breast cancer affects a woman’s femininity and held inaccurate beliefs regarding treatment and prevention. In light of this study’s findings, female university students in Ajman should be targeted for educational campaigns that take into consideration specific and relevant gaps in breast cancer knowledge.
Acknowledgments
The authors would like to thank the WHO for funding this study and the Centre for Advanced Biomedical Research and Innovation and the Statistical Support Unit of the Gulf Medical University in Ajman for their help and support. The authors would also like to thank the participants and their universities for their cooperation during the study.
References
- 1.World Health Organization The Global Burden of Disease: 2004 update. From: www.who.int/healthinfo/global_burden_disease/GBD_report_2004update_full.pdf Accessed: Jan 2014.
- 2.American Cancer Society Breast Cancer Facts & Figures, 2005–2006. From: www.cancer.org/acs/groups/content/@nho/documents/document/caff2005brfacspdf2005pdf.pdf Accessed: Jan 2014.
- 3.Office for National Statistics Cancer Statistics Registrations: Registrations of cancer diagnosed in 2006, England. From: www.ons.gov.uk/ons/rel/vsob1/cancer-statistics-registrations--england--series-mb1-/no--37--2006/index.html Accessed: Jan 2014.
- 4.World Health Organization Global Status Report on Noncommunicable Diseases 2010. From: www.who.int/nmh/publications/ncd_report_full_en.pdf?ua=1 Accessed: Jan 2014.
- 5.United Arab Emirates Ministry of Health Cancer Incidence Report: UAE 1998–2001. From: www.tawamhospital.ae/ccr/reports/Annual/CancerIncidenceReportUAE19982001.pdf Accessed: Aug 2014.
- 6.Global Initiative for Breast Cancer Awareness Team Abu Dhabi Community Profile: Summary of Findings. 2008. From: www.haad.ae/HAAD/Portals/0/CP-28-1-2009_Jalaa[1].pdf Accessed: Jan 2014.
- 7.Karayurt O, Ozmen D, Cetinkaya A. Awareness of breast cancer risk factors and practice of breast self examination among high school students in Turkey. BMC Public Health. 2008;8:359. doi: 10.1186/1471-2458-8-359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.World Health Organization Regional Office for the Eastern Mediterranean. Guidelines for the early detection and screening of breast cancer. From: www.emro.who.int/dsaf/dsa696.pdf Accessed: Jan 2014.
- 9.American Cancer Society Breast Cancer Facts & Figures, 2007–2008. From: www.bcdcofalaska.org/pdf/ACA%20Breast%20Cancer%20Facts%202009.pdf Accessed: Jan 2014.
- 10.Osteen RT. Breast Cancer. In: Lenhard RE Jr, Osteen RT, Gansler T, editors. Clinical Oncology. Atlanta, Georgia: American Cancer Society; 2001. pp. 251–68. [Google Scholar]
- 11.Abu Dhabi Ministry of Health . Annual Report of Health Policy Sector. Abu Dhabi: Ministry of Health; 2008. [Google Scholar]
- 12.World Cancer Research Fund and the American Institute for Cancer Research Policy and Action for Cancer Prevention: Food, nutrition and physical activity, with an added US perspective. From: www.aicr.org/assets/docs/pdf/advocacypapers/WCRF_Policy_US_Summary_final.pdf Accessed: Jan 2014.
- 13.Parkin DM, Boyd L, Walker LC. The fraction of cancer attributable to lifestyle and environmental factors in the UK in 2010. Br J Cancer. 2011;105:S77–81. doi: 10.1038/bjc.2011.489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Spector D, Mishel M, Skinner CS, Deroo LA, Vanriper M, Sandler DP. Breast cancer risk perception and lifestyle behaviors among white and black women with a family history of the disease. Cancer Nurs. 2009;32:299–308. doi: 10.1097/NCC.0b013e31819deab0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pöhls UG, Renner SP, Fasching PA, Lux MP, Kreis H, Ackermann S, et al. Awareness of breast cancer incidence and risk factors among healthy women. Eur J Cancer Prev. 2004;13:249–56. doi: 10.1097/01.cej.0000136718.03089.a5. [DOI] [PubMed] [Google Scholar]
- 16.Freund C, Mirabel L, Annane K, Mathelin C. [Breastfeeding and breast cancer] Gynecol Obstet Fertil. 2005;33:739–44. doi: 10.1016/j.gyobfe.2005.07.030. [DOI] [PubMed] [Google Scholar]
- 17.Dandash KF, Al-Mohaimeed A. Knowledge, attitudes, and practices surrounding breast cancer and screening in female teachers of Buraidah, Saudi Arabia. Int J Health Sci (Qassim) 2007;1:61–71. [PMC free article] [PubMed] [Google Scholar]
- 18.Sharma K, Costas A, Damuse R, Hamiltong-Pierre J, Pyda J, Ong CT, et al. The Haiti Breast Cancer Initiative: Initial findings and analysis of barriers-to-care delaying patient presentation. J Oncol. 2013;2013:206367. doi: 10.1155/2013/206367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Habib F, Salman S, Safwat M, Shalaby S. Awareness and knowledge of breast cancer among university students in Al Madina Al Munawara region. Mid East J Cancer. 2010;1:159–66. [Google Scholar]
- 20.Salaudeen AG, Akande TM, Musa OI. Knowledge and attitudes to breast cancer and breast self examination among female undergraduates in a state in Nigeria. Eur J Soc Sci. 2009;7:157–65. [Google Scholar]
- 21.Akhigbe AO, Omuemu VO. Knowledge, attitudes and practice of breast cancer screening among female health workers in a Nigerian urban city. BMC Cancer. 2009;9:203. doi: 10.1186/1471-2407-9-203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Johnson N, Dickson-Swift V. ‘It usually happens in older women’: Young women’s perceptions about breast cancer. Health Educ J. 2008;67:243–57. doi: 10.1177/0017896908097068. [DOI] [Google Scholar]
- 23.Sim HL, Seah M, Tan SM. Breast cancer knowledge and screening practices: A survey of 1,000 Asian women. Singapore Med J. 2009;50:132–8. [PubMed] [Google Scholar]
- 24.Sambanje MN, Mafuvadze B. Breast cancer knowledge and awareness among university students in Angola. Pan Afr Med J. 2012;11:70. [PMC free article] [PubMed] [Google Scholar]
- 25.Sait WA, Al-Amoudi SM, Tawtai DA, Abduljabbar HS. The knowledge of breast cancer among young Saudi females. Saudi Med J. 2010;31:1242–4. [PubMed] [Google Scholar]
- 26.Kobeissi L, Hamra R, Samari G, Koleilat L, Khalifeh M. The 2009 Lebanese National Mammography Campaign: Results and assessment using a survey design. Epidemiol. 2012;2:112. doi: 10.4172/2161-1165.1000112. [DOI] [Google Scholar]
- 27.Amin TT, Al Mulhim AR, Al Meqihwi A. Breast cancer knowledge, risk factors and screening among adult Saudi women in a primary health care setting. Asian Pac J Cancer Prev. 2009;10:133–8. [PubMed] [Google Scholar]
- 28.Rauscher GH, Ferrans CE, Kaiser K, Campbell RT, Calhoun EE, Warnecke RB. Misconceptions about breast lumps and delayed medical presentation in urban breast cancer patients. Cancer Epidemiol Biomarkers Prev. 2010;19:640–7. doi: 10.1158/1055-9965.EPI-09-0997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Luquis RR, Villanueva Cruz IJ. Knowledge, attitudes, and perceptions about breast cancer and breast cancer screening among Hispanic women residing in South Central Pennsylvania. J Community Health. 2006;31:25–42. doi: 10.1007/s10900-005-8187-x. [DOI] [PubMed] [Google Scholar]
- 30.Montazeri A, Vahdaninia M, Harirchi I, Harirchi AM, Sajadian A, Khaleghi F, et al. Breast cancer in Iran: Need for greater women awareness of warning signs and effective screening methods. Asia Pac Fam Med. 2008;7:6. doi: 10.1186/1447-056X-7-6. [DOI] [PMC free article] [PubMed] [Google Scholar]