Abstract
The occurrence of ectopic lingual thyroid tissue was first reported over 100 years ago. We report an unusual presentation of ectopic thyroid tissue occurring in the submental area. A 27-year-old female presented to the Sultan Qaboos University Hospital in Muscat, Oman, in October 2011 with an 8 × 6 cm mass which caused difficulty in talking and a feeling of heaviness in the jaw. She was clinically and biochemically euthyroid upon presentation. The clinical diagnosis was confirmed by a technetium-99m thyroid scan, magnetic resonance imaging and fine needle aspiration. A single dose of 976 megabecquerels of radioactive iodine-131 resulted in hypothyroidism after three months and the complete disappearance of the swelling and associated symptoms. At a two-year follow-up, the patient was healthy and continuing lifelong replacement therapy with thyroxine.
Keywords: Thyroid, abnormalities; Ectopic Thyroid; Iodine Radioisotopes, therapeutic use; Fine Needle Aspiration; Thyroglossal Cyst; Case Report; Oman
In 1869, hickman reported the first case of lingual ectopic thyroid, which is the most common type of thyroid ectopia and accounts for 90% of all reported cases.1 Thyroid tissue originates at the foramen caecum, which is situated in the midline of the tongue at the junction between the anterior two-thirds and posterior third. It grows downward, bifurcating to form the lateral lobes and isthmus of the normal thyroid gland. A failure to migrate from the foramen caecum may leave part or all of the thyroid tissue at the base of the tongue or along the thyroglossal duct.2–4
Of all ectopic thyroids, 90% are found in the lingual dorsum;1 these are known as lingual thyroid or ectopic lingual thyroid. In rare cases, parathyroid glands are associated with ectopic thyroid tissue.5 Other sites of ectopic thyroid deposition include the cervical lymph nodes, the submandibular glands and the trachea. Approximately two-thirds of patients with a lingual thyroid lack thyroid tissue in the neck.6 This paper presents a rare case of a large (8 × 6 cm) submental ectopic thyroid mass and includes a discussion of the clinical presentation, diagnosis and treatment of this condition.
Case Report
A 27-year-old female presented to the Sultan Qaboos University Hospital (SQUH) in Muscat, Oman, in October 2011 with a long-standing swelling at the base of the tongue, which had been gradually increasing in size over the past 11 years. Her speech was adversely affected and she reported a feeling of heaviness in the tongue. Over the previous four years, a submental mass had developed and was slowly increasing in size. There was no history of difficulty in swallowing or breathing and no history of palpitations, haemoptysis or changes in weight. The past medical history of the patient was insignificant and she was not currently taking any medication. She had two children and her youngest child was three years old.
A clinical examination revealed a large non-tender submental spherical swelling extending from the mental front of the trachea to the chin, approximately 8 × 6 cm in size. The swelling was firm in consistency, with a smooth regular surface and no bruit or thrill. It moved when the patient swallowed but not when she protruded her tongue. The overlying skin was scarred due to previous cautery attempts. There were no palpable lymph nodes [Figure 1].
Figure 1:
Lateral view of the patient’s face showing a large submental ectopic thyroid mass.
An oropharyngeal examination revealed a rounded mass at the base of the tongue, which was the result of the upward enlargement of the submental thyroid tissue. She was euthyroid on clinical examination, with a pulse rate of 72 beats per minute, sinus rhythm and blood pressure of 120/80 mmHg, with no palpable thyroid in the neck. The systemic examination was unremarkable. Due to these findings, a clinical diagnosis of ectopic thyroid tissue was suspected.
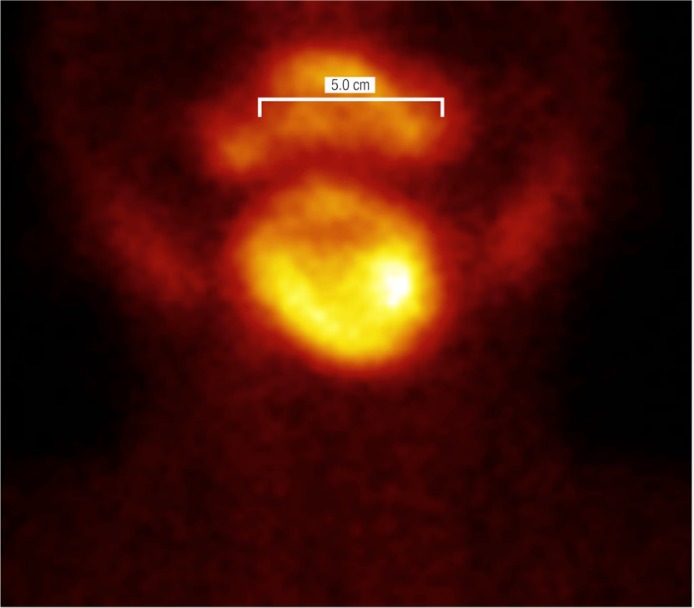
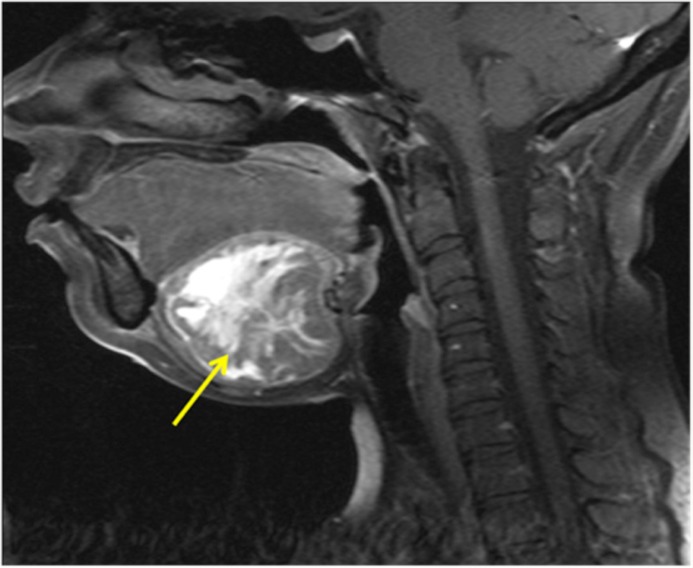
Laboratory investigations revealed a normal thyroid function test with the following results: free thyroxine (FT4) of 9.9 pmol/L (normal range: 7–14 pmol/L); thyroid stimulating hormone (TSH) of 2.27 mIU/L (normal range: 0.3–5.5 mIU/L), and thyroglobulin (TG) of 481 μg/L (normal range: 0–35 μg/L). In addition, thyroid peroxidase antibodies were negative. The technetium (Tc)-99m thyroid scan showed an uptake of 1.2% in the submental area; however, there was no uptake in the normal thyroid location, which is a feature consistent with a diagnosis of ectopic thyroid [Figure 2]. Magnetic resonance imaging (MRI) revealed a single distinct ectopic submental thyroid mass without any discrete nodules [Figure 3].
Figure 2:
Technetium-99m thyroid scan showing a large abnormal uptake of 1.2% at the submental area and no uptake in the normal thyroid location.
Figure 3:
Magnetic resonance image showing a single distinct submental ectopic thyroid mass.
An ultrasound-guided fine needle aspiration (FNA) revealed changes compatible with nodular hyperplasia without evidence of malignancy. The patient was treated with a single dose of iodine-131 (976 megabecquerels). Three months later she became hypothyroid with a TSH level of >100 mIU/L and an FT4 result of <3.2 pmol/L. Additionally, both the swellings at the base of the tongue and the submental area, as well all other associated symptoms, disappeared completely [Figure 4]. The patient was prescribed lifelong thyroxine replacement medication (100 mcg daily) and the adverse symptoms resulting from her hypothyroid state were soon resolved. At a two-year follow-up, she remained clinically and biochemically euthyroid, with undetectable TG levels, and was also referred to a dermatologist to treat her keloid scars.
Figure 4:
Lateral view of the patient’s face and neck three months after iodine-131 therapy. As can be observed, the swelling has completely disappeared.
Discussion
Thyroid ectopia is defined as functioning thyroid tissue found anywhere other than the usual anatomic location of the thyroid gland. Ectopic thyroid is usually located along the normal path of the thyroid gland descent; however, on rare occasions it can also be found in the mediastinum, heart, oesophagus or diaphragm. Ectopic thyroid tissue is derived from abnormalities in the migration of the medial anlage and it therefore does not typically contain parafollicular cells.7,8
A failure of the thyroid gland to descend correctly from the foramen caecum occurs in approximately one in 200,000 normal subjects and one in 6,000 patients with thyroid disease.7,8 It is four times more prevalent among females. The true incidence of thyroid ectopia is not known due to the asymptomatic nature of some cases of ectopic thyroid tissue.7,8
In patients with ectopic thyroid tissue, 70% will present with hypothyroidism, due to an enlargement of the ectopic tissue resulting from the elevated TSH levels.6 Many of these patients will respond to thyroxine suppression treatment, which results in the shrinkage of the tumour as the TSH levels return to normal. The patient in the current case report was considered unusual in that her tumour continued to grow despite normal FT4 and TSH levels. Fortunately, she had relatively few associated symptoms. However, the patient reported experiencing a rapid increase in the submental swelling during her last pregnancy; as a result she became symptomatic, experiencing a change in speech and a feeling of heaviness in the jaw. The gland became hypertropic as a response to the increased demand for the thyroid hormone during pregnancy. A similar response can occur during other conditions of metabolic stress, such as puberty, upper respiratory infections (due to the associated lymphoid tissue), trauma or menopause.1,7–9 This may then lead to regional symptoms such as dysphagia, dysphonia, dyspnoea or haemoptysis.2,7,10,11
In patients presenting with a lingual thyroid, over 70% have no thyroid tissue in the normal location.1,7–9 In the present case, the patient’s Tc-99m thyroid scan revealed that there was no thyroid uptake in the normal location. In situations where a Tc-99m thyroid scan is not available, ectopic lingual thyroid tissue can be demonstrated using computed tomographic scanning. Normal thyroid tissue gives the appearance of enhancement without a contrast injection due to the presence of iodine in the thyroid.2,10,11
The treatment of ectopic thyroid tissue depends on the size of the tissue as well as the presence or absence of symptoms and complicating factors such as ulceration, haemorrhage or malignancy. The recommendation for asymptomatic lingual thyroid patients is to prescribe lifelong thyroxine suppression treatment in order to prevent subsequent enlargement of the tissue, diminish the risk of malignancy and prevent the onset of hypothyroidism.2 Fortunately, carcinoma in ectopic thyroid tissue is rare, with fewer than 30 cases reported in the literature.12
Before iodine-131 therapy was established as a viable treatment option for such cases, surgery was the only option available for severely symptomatic patients who failed to respond to T4 suppression. In the current case, there was concern regarding the potential for further growth of the tumour and whether T4 suppression alone would result in a complete regression of the ectopic tissue. This was doubted because the tumour had continued to grow despite normal TSH levels and because the FNA had revealed nodular hyperplasia. Following discussions with the surgical team at SQUH, a surgical approach was deemed too risky in view of the extensive exposure required to remove such a large vascular mass. It was therefore decided that the best course of action would be to use iodine-131 therapy, which had previously proven to be extremely effective.2,13–17 However, surgery is still the preferred treatment option in many countries today. In view of the current case, the authors recommend that patients with ectopic thyroid tissue who are unlikely to respond to thyroxine suppression treatment should be prescribed iodine-131 therapy, except in cases where the patient has developed cancer in the ectopic thyroid tissue.17
Conclusion
This case report presents a patient with a large vascular ectopic submental thyroid tissue and associated symptoms. This case was unusual as the tissue continued to increase in size despite normal FT4 and TSH levels. The patient was subsequently treated with iodine-131 therapy which successfully resulted in the disappearance of both swellings and all associated symptoms. The authors therefore suggest that any patient requiring therapy who is unlikely to respond to thyroxine suppression treatment should initially be treated with iodine-131, unless the ectopic thyroid tissue is determined to be cancerous.
References
- 1.Mussak EN, Kacker A. Surgical and medical management of midline ectopic thyroid. Otolaryngol Head Neck Surg. 2007;136:870–2. doi: 10.1016/j.otohns.2007.01.008. [DOI] [PubMed] [Google Scholar]
- 2.Kansal P, Sakati N, Rifai A, Woodhouse N. Lingual thyroid: Diagnosis and treatment. Arch Intern Med. 1987;147:2046–8. doi: 10.1001/archinte.1987.00370110174028. [DOI] [PubMed] [Google Scholar]
- 3.Aalaa M, Mohajeri-Tehrani MR. Images in clinical medicine: Ectopic thyroid gland. N Engl J Med. 2012;366:943. doi: 10.1056/NEJMicm1106077. [DOI] [PubMed] [Google Scholar]
- 4.Yu TY, Chang TC. Images in clinical medicine: Lingual thyroid. N Engl J Med. 2012;366:e15. doi: 10.1056/NEJMicm1112306. [DOI] [PubMed] [Google Scholar]
- 5.Salain S, Rodrigues G, Kumar S. Sublingual thyroid: A case report with literature review. Internet J Surgery. 2006;11:1. [Google Scholar]
- 6.Basaria S. Images in medicine: Lingual thyroid. Postgrad Med J. 2000;76:419. doi: 10.1136/pmj.76.897.419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Amani Mel A, Benabadji N, Benzian Z, Amani S. Ectopic lingual thyroid. Indian J Nucl Med. 2012;27:124–6. doi: 10.4103/0972-3919.110718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Di Benedetto V. Ectopic thyroid gland in the submandibular region simulating a thyroglossal duct cyst: A case report. J Pediatr Surg. 1997;32:1745–6. doi: 10.1016/S0022-3468(97)90522-4. [DOI] [PubMed] [Google Scholar]
- 9.Leung AK. Ectopic thyroid gland and thyroxine-binding globulin excess. Acta Paediatr Scand. 1986;75:872–4. doi: 10.1111/j.1651-2227.1986.tb10308.x. [DOI] [PubMed] [Google Scholar]
- 10.Wolf BS, Nakagawa H, Yeh HC. Visualization of the thyroid gland with computed tomography. Radiology. 1977;123:368. doi: 10.1148/123.2.368. [DOI] [PubMed] [Google Scholar]
- 11.Al-Hindawi AY, Mohammed KH, Baba WI, Al-Hiti T. The clinical presentation of ectopic thyroid gland with results of radioiodine studies. Br J Clin Pract. 1969;23:372–3. [PubMed] [Google Scholar]
- 12.Massine RE, Durning SJ, Koroscil TM. Lingual thyroid carcinoma: A case report and review of the literature. Thyroid. 2001;11:1191–6. doi: 10.1089/10507250152741055. [DOI] [PubMed] [Google Scholar]
- 13.Schilling JA, Karr JW, Hursh JB. The treatment of a lingual thyroid with radioactive iodine. Surgery. 1950;27:130–8. doi: 10.1016/0030-4220(51)90557-9. [DOI] [PubMed] [Google Scholar]
- 14.Danner C, Bodenner D, Breau R. Lingual thyroid: Iodine 131: A viable treatment modality revisited. Am J Otolaryngol. 2001;22:276–81. doi: 10.1053/ajot.2001.24819. [DOI] [PubMed] [Google Scholar]
- 15.Ibrahim NA, Fadeyibi IO. Ectopic thyroid: Etiology, pathology and management. Hormones (Athens) 2011;10:261–9. doi: 10.14310/horm.2002.1317. [DOI] [PubMed] [Google Scholar]
- 16.Patel Z, Johnson L. Iodine 131 ablation of an obstructive lingual thyroid. J Radiol Case Rep. 2009;3:3–6. doi: 10.3941/jrcr.v3i2.70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Noussios G, Anagnostis P, Goulis DG, Lappas D, Natsis K. Ectopic thyroid tissue: Anatomical, clinical, and surgical implications of a rare entity. Eur J Endocrinol. 2011;165:375–82. doi: 10.1530/EJE-11-0461. [DOI] [PubMed] [Google Scholar]