Figure 4.
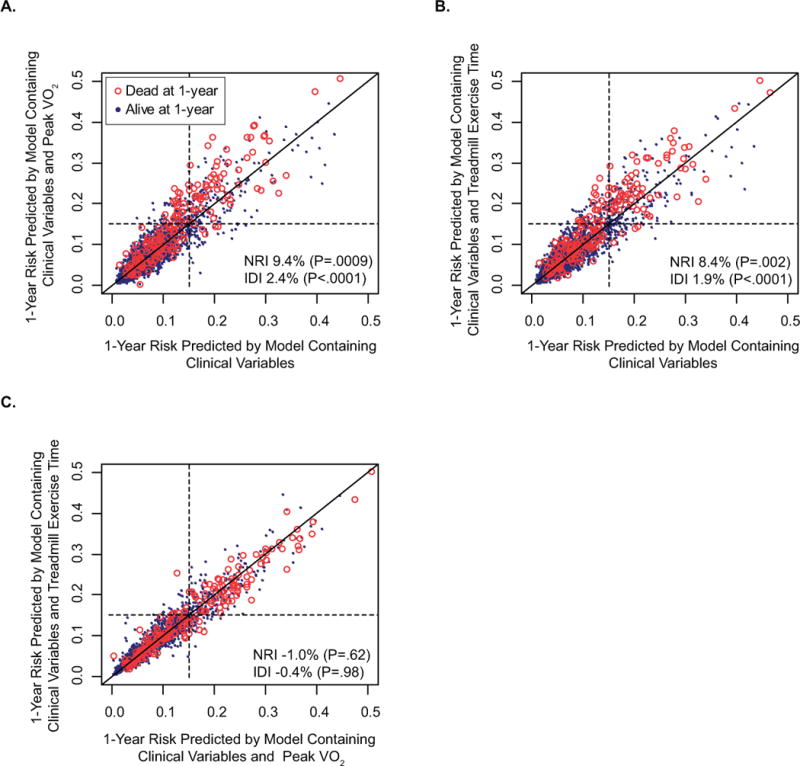
Reclassification: One year low-risk (<15%) and high-risk (≥15%) survival categories are cut-offs based on the observed national 1-year survival after heart transplantation. The endpoint is death and improvement of classification is expressed as net reclassification improvement (NRI) which is dependent on the pre-defined cut-offs and integrated discrimination improvement (IDI) which is not limited to pre-determined risk categories. If a variable adds no predictive value to the model, all points fall on the dark line of identity within each figure. Spread around the line indicates modulation of predicted risk; if the variable correctly modulates predicted risk, there should be a greater preponderance of events (red open circles) above the line of identify. A. Model with clinical variables and peak VO2 compared to model with only clinical variables. Peak VO2 with cardiac risk factors improved classification in 74 patients (23 who died, 51 who survived) but worsened it in 71 patients (4 who died, 67 who survived) with an IDI of 2.4% B. Model with clinical variables and treadmill exercise time compared to model with only clinical variables. Treadmill exercise time with cardiac risk factors improved classification in 70 patients (21 who died, 49 who survived) but worsened it in 68 patients (4 who died, 64 who survived) with an IDI of 1.9% C. Model with clinical variables and treadmill exercise time compared to model with clinical variables and Peak VO2 improved classification in 43 patients (6 who died, 37 who survived) but worsened it in 46 patients (8 who died, 38 who survived) with an IDI of −0.4% which was not statistically significant
