Abstract
Objective
The aim of this study is to evaluate the clinical course of intracranial aneurysm in patients aged 65 years and older and the immediate outcome after its aggressive management.
Materials and Methods
We performed a retrospective analysis using the medical records of 159 elderly patients managed at our institute from September 2008 to December 2013. Obtained clinical information included age, sex, Hunt and Hess grade (HHG), aneurysm location, Fisher grade (FG) and the treatment modality. Concomitant clinical data aside from cerebrovascular condition (hypertension, diabetes, previous medication) were evaluated to determine risk factors that might affect the functional outcomes.
Results
A total of 108 patients (67.9%) presented with subarachnoid hemorrhage (SAH), and 51 (32.1%) with unruptured intracranial aneurysms (UIAs). Coiling was performed in 101 patients and 58 patients underwent clipping. In the SAH population, 62 patients (57.4%) showed favorable outcomes, with a mortality rate of 11.3% (n = 18). In the UIAs population, 50 (98%) patients achieved 'excellent' and one (2%) achieved 'good' outcome. Factors including high-grade HHG (p < 0.001), advanced age (p = 0.014), and the presence of intraventricular hematoma (IVH) (p = 0.017) were significant predictors of poor outcome.
Conclusion
SAH patients with high grade HHG and IVH are associated with poor outcome with statistical significance, all the more prominent the older the patient is. Therefore, the indication for aggressive therapy should be considered more carefully in these patients. However, as the outcomes for elderly patients with UIAs were excellent regardless of the treatment modality, aggressive treatment could always be considered in UIAs cases.
Keywords: Elderly, Intracranial aneurysm, Subarachnoid hemorrhage, Outcome, Microsurgical clipping, Endovascular coiling
INTRODUCTION
The definition of 'elderly' may vary according to chronological, biological, psychological, and social aspects, however, most developed countries have accepted the chronological age of 65 years as a definition of 'elderly' or older person, as defined by the World Health Organization (WHO). Advances in medical science have led to an increase in life expectancy, and, consequently, the proportion of elderly people among the total population. In 2013, approximately 12.2% of the Korean population was aged over 65 years.11) With continued expansion of the aging population, and the development of less invasive and high-quality neuroimaging modalities, more elderly patients are expected to develop intracranial aneurysms.
As supportive intensive critical care and neurointerventional treatment options become more advanced, more aggressive treatment of elderly aneurysm patients is being encouraged.1) Aggressive treatment for many conditions is becoming more common, resulting in more positive outcomes.5),16),20) The aim of our study was to describe intracranial aneurysm treatments in all elderly patients treated in our institute and to observe their clinical course and immediate prognosis under aggressive therapy.
MATERIALS AND METHODS
This is a retrospective, cross-sectional study from a single institution. The medical records of all patients treated at our hospital from September 2008 to December 2013 were reviewed for selection of patients aged 65 years or older who underwent microsurgical clipping or endovascular management for treatment of an intracranial aneurysm. To reduce variability, a single vascular neurosurgeon performed all microsurgical clippings and endovascular coilings in these patients. Clinical information obtained included age, sex, Hunt and Hess grade (HHG), aneurysm location, Fisher grade (FG), and treatment (microsurgical clipping, endovascular coiling). To determine which risk factors affected the functional outcome, clinical data including hypertension, diabetes, and previous medication were evaluated as well.
All eligible patients were placed in the microsurgical clipping group or the endovascular coiling group. The HHG were evaluated at admission. Clinical outcome at the time of discharge was assessed for each patient using the Glasgow outcome scale (GOS) score: favorable outcome (good recovery, GOS 5; moderate disability, GOS 4) or poor outcome (severe disability, GOS 2-3; death, GOS 1).
Statistical analysis was performed using commercially available software (SPSS version 18, SPSS Inc., Chicago, IL, United States). Univariate comparison of continuous variables with a normal distribution was performed using two sample t-tests. All categorical data were assessed by χ2 test or Fisher's exact test. Logistic regression was used to test bivariate associations between variables of interest and good versus poor outcome. A p value < 0.05 was considered statistically significant.
RESULTS
Patients and characteristics
A comparison of the clinical characteristics of patients treated by endovascular coiling or microsurgical clipping is shown in Table 1. A total of 1010 aneurysms of 857 patients were treated during the study period. A total of 183 (18%) aneurysms were treated in 159 (18.6%) elderly patients, including 134 women (84.3%) and 25 men (15.7%) with a mean age of 71.6 years; 108 (67.9%) patients experienced subarachnoid hemorrhage (SAH) and 51 (32.1%) patients had unruptured intracranial aneurysms (UIA); 101 (63.5%) patients were treated by coiling and 58 (36.5%) patients were treated by microsurgical clipping. Fifty three patients presented with a high-grade SAH (HHG IV or V) and 55 patients presented with a SAH of HHG II or III.
Table 1.
A Comparison of the clinical characteristics of elderly patients with intracranial aneurysm
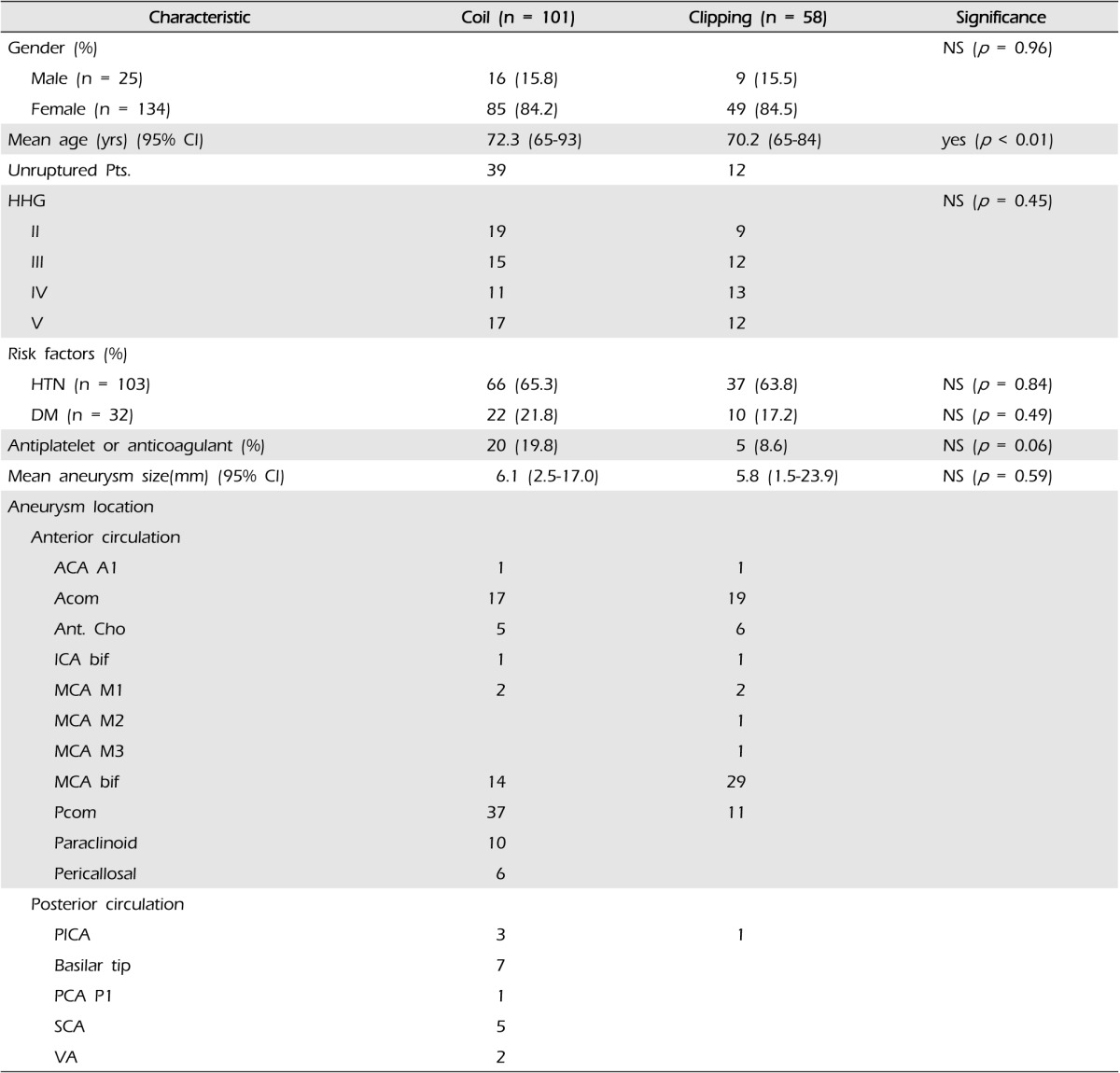
HHG = Hunt-Hess grade; HTN = Hypertension; DM = Diabetes Mellitus; ACA = anterior cerebral artery; Acom = anterior communicating artery; Ant.Cho = anterior choroidal artery; ICA bif= internal carotid artery bifurcation; MCA bif = middle cerebral artery bifurcation; Pcom = posterior communicating artery; PCA = posterior cerebral artery; PICA = posterior inferior cerebellar artery; SCA = superior cerebellar artery; VA = vertebral artery; yrs = years; CI = confidence interval; NS = not significant
The percentage of unruptured aneurysms treated by endovascular coiling was 76.5%. Age was the only significant difference between these two treatment groups. The average age of patients with aneurysms coiled and clipped was 72.3 (65-93) and 70.2 (65-84) years, respectively (p < 0.01). No significant differences based on gender, risk factors, HHG, and aneurysm size were observed between the coiling group and the clipping group.
Aneurysm location
There were 164 (89.6%) anterior circulation aneurysms and 19 (10.4%) posterior circulation aneurysms. Forty eight (26.2%) aneurysms occurred in the posterior communicating artery, 43 (26.2%) in the middle cerebral artery bifurcation, and 36 (19.7%) in the anterior communicating artery. Multiple aneurysms occurred in 16 patients. Ninety three (56.7%) of the anterior circulation aneurysms and 18 (94.7%) of the posterior circulation aneurysms were treated by coiling. Seventy one (43.3%) anterior circulation aneurysms and one (5.3%) posterior circulation aneurysm were treated by microsurgical clipping.
Outcome
Of the 113 individuals with GOS scores of favorable outcome (i.e., independence in activities of daily living), 34 (58.6%) individuals belonged to the clipping group and 79 (78.2%) belonged to the coiling group (Fig. 1A). In the ruptured population, 62 (57.4%) patients achieved a favorable outcome. In the population with unruptured aneurysms, 50 (98%) and one (2%) patients achieved an excellent and good outcome, respectively. In the clipping group, there were 46 patients with SAH. Nine (19.6%) patients had an excellent outcome and 13 (28.3%) patients had a good outcome. Fifteen (32.6%) patients experienced moderate and severe disability. In the coiling group, there were 62 SAH patients. Twenty three (37.1%) patients were discharged in excellent status and 17 (27.4%) patients had a good outcome. Thirteen (21%) patients experienced moderate disability or required hospitalization (Tables 3, 4, Fig. 1B).
Fig. 1.
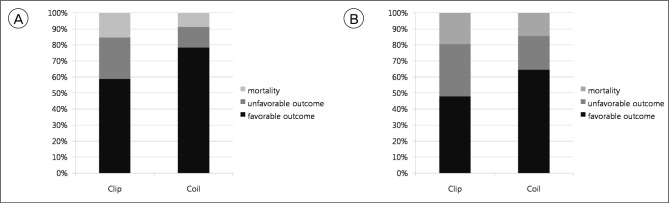
Clinical outcome of all patients with intracranial aneurysm according to treatment modality (A) and patients with subarachnoid hemorrhage (B).
Table 3.
Management outcome of aneurysm treated by clipping
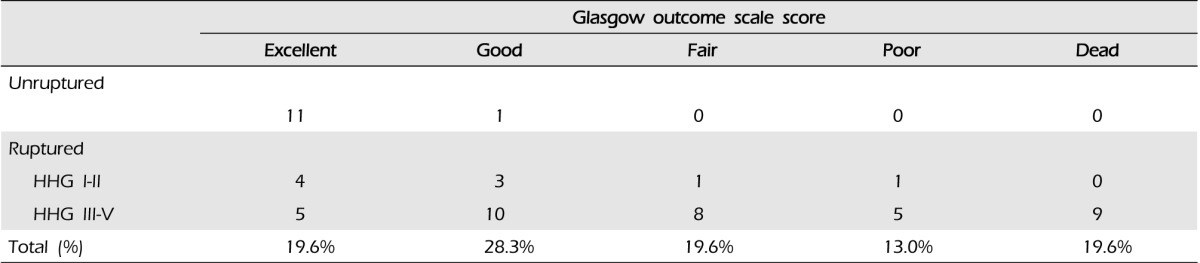
HHG = Hunt and Hess grade scale
Table 4.
Management outcome of aneurysm treated by coiling
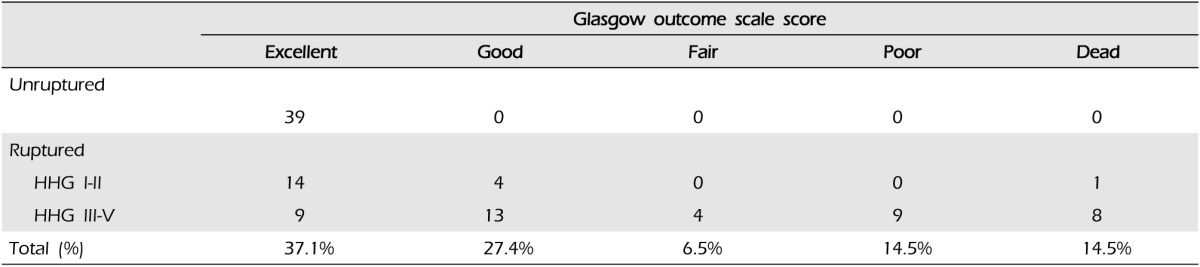
HHG = Hunt and Hess grade scale
Despite aggressive treatment, upon discharge, the overall mortality rate was 11.3% (n = 18). Statistical analysis using the binary outcome scale was performed for comparison of favorable outcome with poor outcome in terms of HHG. HHG was divided into binary variables as either good (HHG I, II, III) or not. Binary logistic regression analysis was performed. Analysis for other variables including age, co-existence of other medical diseases such as hypertension and diabetes mellitus, and medications taken such as antiplatelet or anticoagulants was performed using the same method. As shown in Table 2, high grade HHG, advanced age, and IVH were strong predictors of poor outcome. Table 5 shows the causes of mortality in patients with ruptured aneurysms, with the two most common causes being initial hemorrhage (52.6%; 10 of 19 deaths) and pneumonia (26.3%; five of 19 deaths). Sepsis/multiorgan failure (three deaths), myocardial infarction (one death) were other causes of death for patients who experienced ruptured aneurysms. There was no occurrence of death in the unruptured aneurysmal group.
Table 2.
Multivariate logistic regression analysis to identify factors predictive of a poor outcome as assessed by a Glasgow outcome scale
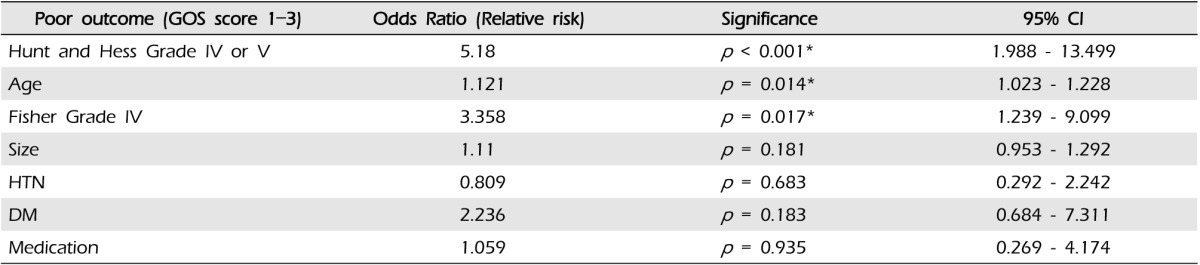
*indicates significance (p < 0.05)
GOS = Glasgow outcome Scale, HTN = hypertension, DM = diabetes mellitus
Table 5.
Cause of mortality
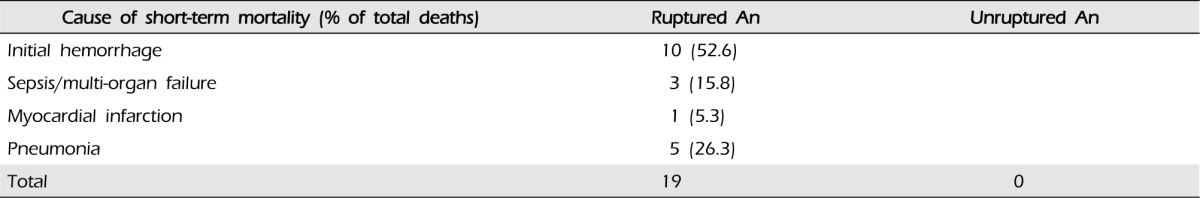
An = aneurysm
DISCUSSION
In this study, the primary finding was that patients with high grade HHG, increasing age, and intraventricular hematoma (IVH, FG4) had poor clinical outcomes as compared to patients without these factors, which were as follows. The initial clinical presentation of patients is the highest predictive power of the outcome. In our series, the final mortality rate and percentage of severely disabled patients with high grade HHG (HHG IV, V) was 28.3% and 24.5%, respectively. A favorable outcome was achieved in 31% of treated patients, higher than the result from previously published studies.5),7) In patients with a poor clinical grade with acute hydrocephalus and significant IVH (FG4), early placement of an external ventricular drainage (EVD) prior to aneurysm securing intervention improved the level of consciousness and short-term outcome.15),17),19) This study also demonstrated that placement of an EVD improved the clinical grade and outcome.
The secondary finding is that both microsurgical clipping and coiling yielded excellent results in elderly patients with unruptured aneurysm. The overall morbidity and mortality rates were 2% and 0% in each respective treatment modality, similar to those found in the literature.3),8),12),14) Currently, there are no established guidelines for ideal management of UIAs in elderly patients. In the distribution of aneurysm sizes, larger sized unruptured aneurysms were more common in the older age group and the annual incidence of SAH was noted to be three times higher.2),6),21) Thus, some researchers have suggested that elderly patients with UIAs should be considered for active surgical intervention to improve their outcomes. Advanced age alone has been reported to increase the risk of complications in elderly patients with unruptured aneurysm undergoing microsurgical clipping or endovascular coiling.4),10) In the current study, more patients with UIAs were treated by endovascular coiling (76.5%) and the mean age was significantly older than that of the microsurgical clipping group. To our surprise, favorable results have been obtained from both treatments along with our results. Our study supports the idea that surgical treatment of UIAs in the elderly should be advocated in making decisions on the optimal treatment strategy after careful assessment of each individual's circumstances.
In the ruptured aneurysm group, nine (47.4%) patients died from 'other' causes unrelated to SAH. Among the eight patients who died, five died of pneumonia and three died of sepsis and/or multiorgan failure. According to these results, more than one-third of the patients died within the acute period of the SAH, even if it was not due to the hemorrhage. Clinical care of elderly patients is challenging because of a greater chance of pharmacological complications, cardiopulmonary dysfunction, and so on. Elderly patients who survive SAH often face prolonged management in an intensive care unit (ICU), including treatment for multiple potential neurological and medical complications.13),18) Therefore, for proper co-management of these patients, in order to handle multiple issues, it is necessary to employ a more specialized neurointensivist dedicated to the ICU.9)
This study is limited by the fact that it was a retrospective review, with a limited number of patients at a single institution and no strictly defined selection criteria for the treatment procedure along with a lack of long-term follow up results. Lack of standard treatment guidelines and sufficient prognostic domestic data concerning treatment of aneurysms in the elderly make it difficult for clinicians when it comes to deciding on the proper treatment modality in such patients. We believe that our study may provide a valuable guide to help in decision making regarding treatment enrollment of elderly patients who could benefit from treatment, despite the known challenges in the management of this age group.
CONCLUSION
According to our data, elderly patients with high grade HHG and IVH are truly associated with poor outcome, so that the indication for aggressive therapy should be considered carefully. To improve outcomes in elderly SAH patients, co-management by specialized neurointensivists who can handle patients with multiple conditions should be considered. According to our data, all elderly patients with UIAs had an excellent outcome, regardless of the treatment modality. Treatment of unruptured intracranial aneurysms can be considered in an optimistic way.
References
- 1.Brinjikji W, Rabinstein AA, Lanzino G, Kallmes DF, Cloft HJ. Effect of age on outcomes of treatment of unruptured cerebral aneurysms: a study of the national inpatient sample 2001-2008. Stroke. 2011 May;42(5):1320–1324. doi: 10.1161/STROKEAHA.110.607986. [DOI] [PubMed] [Google Scholar]
- 2.Carter BS, Sheth S, Chang E, Sethl M, Ogilvy CS. Epidemiology of the size distribution of intracranial bifurcation aneurysms: smaller size of distal aneurysms and increasing size of unruptured aneurysms with age. Neurosurgery. 2006 Feb;58(2):217–223. doi: 10.1227/01.NEU.0000194639.37803.F8. discussion 217-23. [DOI] [PubMed] [Google Scholar]
- 3.Higashida RT, Lahue BJ, Torbey MT, Hopkins LN, Leip E, Hanley DF. Treatment of unruptured intracranial aneurysms: a nationwide assessment of effectiveness. AJNR Am J Neuroradiol. 2007 Jan;28(1):146–151. [PMC free article] [PubMed] [Google Scholar]
- 4.Horiuchi T, Tanaka Y, Hongo K. Surgical treatment for aneurysmal subarachnoid hemorrhage in the 8th and 9th decades of life. Neurosurgery. 2005 Mar;56(3):469–475. doi: 10.1227/01.neu.0000153926.67713.b8. discussion 469-75. [DOI] [PubMed] [Google Scholar]
- 5.Hutchinson PJ, Power DM, Tripathi P, Kirkpatrick PJ. Outcome from poor grade aneurysmal subarachnoid haemorrhage-which poor grade subarachnoid haemorrhage patients benefit from aneurysm clipping? Br J Neurosurg. 2000 Apr;14(2):105–109. doi: 10.1080/02688690050004516. [DOI] [PubMed] [Google Scholar]
- 6.Inagawa T. Management outcome in the elderly patient following subarachnoid hemorrhage. J Neurosurg. 1993 Apr;78(4):554–561. doi: 10.3171/jns.1993.78.4.0554. [DOI] [PubMed] [Google Scholar]
- 7.Iosif C, Di Maria F, Sourour N, Degos V, Bonneville F, Biondi A, et al. Is a high initial World Federation of Neurosurgery (WFNS) grade really associated with a poor clinical outcome in elderly patients with ruptured intracranial aneurysms treated with coiling? J Neurointerv Surg. 2014 May 01;6(4):286–290. doi: 10.1136/neurintsurg-2013-010711. [DOI] [PubMed] [Google Scholar]
- 8.Jang EW, Jung JY, Hong CK, Joo JY. Benefits of surgical treatment for unruptured intracranial aneurysms in elderly patients. J Korean Neurosurg Soc. 2011 Jan;49(1):20–25. doi: 10.3340/jkns.2011.49.1.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Josephson SA, Douglas VC, Lawton MT, English JD, Smith WS, Ko NU. Improvement in intensive care unit outcomes in patients with subarachnoid hemorrhage after initiation of neurointensivist co-management. J Neurosurg. 2010 Mar;112(3):626–630. doi: 10.3171/2009.8.JNS09441. [DOI] [PubMed] [Google Scholar]
- 10.Khosla A, Brinjikji W, Cloft H, Lanzino G, Kallmes DF. Age-related complications following endovascular treatment of unruptured intracranial aneurysms. AJNR Am J Neuroradiol. 2012 May;33(5):953–957. doi: 10.3174/ajnr.A2881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kwon SC, Kwon OK. Endovascular coil embolization of unruptured intracranial aneurysms: a Korean multicenter study. Acta Neurochir (Wien) 2014 May;156(5):847–854. doi: 10.1007/s00701-014-2033-9. [DOI] [PubMed] [Google Scholar]
- 12.Moroi J, Hadeishi H, Suzuki A, Yasui N. Morbidity and mortality from surgical treatment of unruptured cerebral aneurysms at Research Institute for Brain and Blood Vessels-Akita. Neurosurgery. 2005 Feb;56(2):224–231. doi: 10.1227/01.neu.0000148897.28828.85. discussion 224-31. [DOI] [PubMed] [Google Scholar]
- 13.Naidech AM, Bendok BR, Tamul P, Bassin SL, Watts CM, Batjer HH, et al. Medical complications drive length of stay after brain hemorrhage: a cohort study. Neurocrit Care. 2009;10(1):11–19. doi: 10.1007/s12028-008-9148-x. [DOI] [PubMed] [Google Scholar]
- 14.Raja PV, Huang J, Germanwala AV, Gailloud P, Murphy KP, Tamargo RJ. Microsurgical clipping and endovascular coiling of intracranial aneurysms: a critical review of the literature. Neurosurgery. 2008 Jun;62(6):1187–1202. doi: 10.1227/01.neu.0000333291.67362.0b. discussion 1202-3. [DOI] [PubMed] [Google Scholar]
- 15.Ransom ER, Mocco J, Komotar RJ, Sahni D, Chang J, Hahn DK, et al. External ventricular drainage response in poor grade aneurysmal subarachnoid hemorrhage: effect on preoperative grading and prognosis. Neurocrit Care. 2007;6(3):174–180. doi: 10.1007/s12028-007-0019-7. [DOI] [PubMed] [Google Scholar]
- 16.Ryttlefors M, Enblad P, Kerr RS, Molyneux AJ. International subarachnoid aneurysm trial of neurosurgical clipping versus endovascular coiling: subgroup analysis of 278 elderly patients. Stroke. 2008 Oct;39(10):2720–2726. doi: 10.1161/STROKEAHA.107.506030. [DOI] [PubMed] [Google Scholar]
- 17.Sasaki T, Sato M, Oinuma M, Sakuma J, Suzuki K, Matsumoto M, et al. Management of poor-grade patients with aneurysmal subarachnoid hemorrhage in the acute stage: Importance of close monitoring for neurological grade changes. Surg Neurol. 2004 Dec;62(6):531–535. doi: 10.1016/j.surneu.2004.01.015. discussion 535-7. [DOI] [PubMed] [Google Scholar]
- 18.Smith M. Intensive care management of patients with subarachnoid haemorrhage. Curr Opin Anaesthesiol. 2007 Oct;20(5):400–407. doi: 10.1097/ACO.0b013e3282efa686. [DOI] [PubMed] [Google Scholar]
- 19.Suzuki M, Otawara Y, Doi M, Ogasawara K, Ogawa A. Neurological grades of patients with poor-grade subarachnoid hemorrhage improve after short-term pretreatment. Neurosurgery. 2000 Nov;47(5):1098–1104. doi: 10.1097/00006123-200011000-00014. discussion 1104-5. [DOI] [PubMed] [Google Scholar]
- 20.Wostrack M, Sandow N, Vajkoczy P, Schatlo B, Bijlenga P, Schaller K, et al. Subarachnoid haemorrhage WFNS grade V: is maximal treatment worthwhile? Acta Neurochir (Wien) 2013 Apr;155(4):579–586. doi: 10.1007/s00701-013-1634-z. [DOI] [PubMed] [Google Scholar]
- 21.Yamashita K, Kashiwagi S, Kato S, Takasago T, Ito H. Cerebral aneurysms in the elderly in Yamaguchi, Japan. Analysis of the Yamaguchi data bank of cerebral aneurysm from 1985 to 1995. Stroke. 1997 Oct;28(10):1926–1931. doi: 10.1161/01.str.28.10.1926. [DOI] [PubMed] [Google Scholar]


