Abstract
The reported mortality rates in patients with cirrhosis undergoing various non-transplant surgical procedures range from 8.3% to 25%. This wide range of mortality rates is related to severity of liver disease, type of surgery, demographics of patient population, expertise of the surgical, anesthesia and intensive care unit team and finally, reporting bias. In this article, we will review the pathophysiology, morbidity and mortality associated with non-hepatic surgery in patients with cirrhosis, and then recommend an algorithm for risk assessment and evidence based management strategy to optimize post-surgical outcomes.
Keywords: Pre-operative risk assessment, Risk stratification, Cirrhosis, Model for end-stage liver disease, Non-transplant surgery, Outcomes
INTRODUCTION
The prevalence of chronic liver disease is increasing in the US and the rest of the world because of hepatitis C (HCV), hepatitis B (HBV), alcohol and non-alcoholic fatty liver disease (NAFLD)[1]. It has been estimated that about 10% of patients with cirrhosis will undergo surgery in the last 2 years of their life[2]. General anesthesia and surgery may lead to complications in a significant proportion of patients with well-compensated or occult cirrhosis, and these complications may result in considerable morbidity and mortality. The reported mortality rates in patients with cirrhosis undergoing various surgical procedures range from 8.3% to 25% (Table 1) in comparison to 1.1% in non-cirrhotic patients[3-6]. This wide range of mortality rates is related to severity of liver disease, type of surgery, demographics of patient population, expertise of the surgical, anesthesia and intensive care unit (ICU) team and finally, reporting bias. It is therefore, important to assess the risk in relation to the type of surgery that is performed; arbitrarily, the type of surgery could be categorized into high, moderate or low risk surgery (Table 2)[3]. In this article, we will review the morbidity and mortality associated with non-hepatic surgery in patients with cirrhosis, and then recommend a risk assessment and evidence based management strategy to optimize post-surgical outcomes[7,8].
Table 1.
Reported surgical mortality risk in patients with cirrhosis
| Surgery in patients with cirrhosis | n | Died (n) | % | Ref No. |
| Gastrointestinal | ||||
| Peptic ulcer surgery-elective | 20 | 2 | 10 | 34 |
| Peptic ulcer surgery-bleeding | 94 | 46 | 49 | 34 |
| Peptic ulcer surgery-perforation | 167 | 70 | 42 | 34 |
| Gastric bypass | 125 | 5 | 4 | 38 |
| Biliary tract surgery | 212 | 45 | 21 | 34, 39 |
| Small bowel surgeries | 9 | 6 | 67 | 34 |
| Colon surgeries | 87 | 36 | 41 | 34 |
| Open cholecystectomy | 110 | 8 | 7.7 | 40 |
| Laparoscopic cholecystectomy | 265 | 0 | 0 | 41 |
| Abdominal | ||||
| Abdominal surgery for trauma | 17 | 8 | 47 | 42 |
| Emergency abdominal surgery | 57 | 12 | ||
| Splenectomy | 7 | 0 | 0 | 43 |
| Umbilical herniorrhaphy | 24 | 2 | 8.3 | 6 |
| Inguinal herniorrhaphy | 1197 | 30 | 2.5 | 44 |
| Bone/Joint | ||||
| Hip surgery-elective | 14 | 0 | 0 | 45 |
| Hip surgery-emergent | 5 | 3 | 60 | 45 |
| Knee surgery | 42 | 0 | 0 | 46 |
| Cardiac | ||||
| Cardiac surgery-elective | 18 | 3 | 17 | 47 |
| Cardiac surgery-emergent | 5 | 4 | 80 | 48 |
| Genito-urinary | ||||
| TURP | 30 | 2 | 6.7 | 49 |
| Hysterectomy | 105 | 8 | 7.6 | 50 |
| Abdominal surgeries in various liver conditions | ||||
| Acute hepatitis | 11 | 11 | 100 | 51 |
| Hepatitis C | 34 | 0 | 0 | 52 |
| Chronic hepatitis | 20 | 0 | 0 | 36 |
| Obstructive jaundice | 5-60 | 53 |
TURP: Transurethral resection of the prostrate.
Table 2.
Surgical severity risk stratification[14]
| Low risk | Moderate risk | High risk |
| Eye | Intracranial surgery | Lung resection |
| ENT | Laminectomy/Disc surgery | Heart surgery |
| Dental | Thyroidectomy | AAA repair |
| Sinuses/Tonsils | Other endocrine surgery | Porto-systemic shunt |
| Chest tube/ Thoracentesis | Head and neck surgery | Splenectomy |
| Bronchoscopy | Major blood vessels surgery | Laparotomy |
| Laryngoscopy | Peripheral artery surgery | Esophagus/Stomach surgery |
| Tracheostomy | Embolectomy | Liver/Biliary surgery |
| Venous procedures | Carotid artery surgery | Small bowel/Large bowel/Pancreas surgery |
| Vein stripping | Rectal/Anal surgery | Renal surgery |
| Pacemaker insertion | Herniorrhaphy | Hip surgery |
| Lymph node biopsy/ resection | Bladder procedures | Back fusion |
| GI endoscopy | Prostate procedures | Long bone fractures |
| Laparoscopy | Hysterectomy ± oophorectomy | |
| GU endoscopy | Amputations | |
| Male GU procedures | Hand, foot, knee surgery | |
| Female GU procedures | Breast biopsy/ mastectomy | |
| D & C | ||
| Skin lesion excision | ||
| Superficial tumor excision | ||
| Other diagnostic/ therapeutic procedures | ||
ENT: Ear, nose and throat; GI: Gastrointestinal; GU: Genitourinary; D & C: Dilatation and curettage; AAA: Abdominal aortic aneurysm.
MORBIDITY, MORTALITY AND RISK STRATIFICATION
The published evidence for the risk of surgery in patients with cirrhosis is mostly derived from retrospective studies. These have shown that the postoperative mortality and morbidity correlate well with Child-Turcotte-Pugh (CTP) class of cirrhosis (Table 3)[3,9]. Based on these reports, it has been suggested that elective surgery is tolerated in patients with CTP class A cirrhosis, permissible with preoperative preparation in patients with CTP class B cirrhosis (except those undergoing extensive hepatic resection or cardiac surgery) and contraindicated in patients with CTP class C cirrhosis (Table 4). In recent years, the model for end-stage liver disease (MELD) score has been utilized to prioritize organ allocation in patients awaiting liver transplant. This objective score has been shown to reflect the 90 d mortality in patients with cirrhosis. Unlike the CTP score which has subjective components (severity of hepatic encephalopathy and ascites), the MELD score is considered more objective as it relies only on serum bilirubin, creatinine and international normalized ratio (INR). More recent studies suggest that MELD could also be used to stratify risk in patients undergoing non-transplant surgery, and MELD score < 10, 10-14 and > 14 may correspond to CTP classes A, B and C respectively[9,10].
Table 3.
Modified Child Turcotte Pugh (CTP) score
| Feature | Points | ||
| 1 | 2 | 3 | |
| Albumin (g/dL) | > 3.5 | 2.8-3.5 | < 2.8 |
| Prothrombin time | |||
| -Seconds prolonged | < 4 | 4-6 | > 6 |
| -INR | < 1.7 | 1.7-2.3 | > 2.3 |
| Bilirubin (mg/dL) | < 2 | 2-3 | > 3 |
| (PBC/PSC)1 | < 4 | 4-10 | > 10 |
| Ascites | Absent | Slight-moderate | Tense |
| Encephalopathy | None | Grade I-II | Grade III-IV |
| CTP Class | Points | 2 yr patient survival (%) | |
| Class A | 5-6 | 85 | |
| Class B | 7-9 | 60 | |
| Class C | 10-15 | 35 | |
In primary biliary cirrhosis (PBC) and primary sclerosing cholangitis (PSC), the bilirubin references are changed to reflect the fact that these diseases feature high conjugated bilirubin levels.
Table 4.
Contraindications to elective surgery in patients with liver disease[11]
| Acute hepatitis | Chronic hepatitis |
| Alcoholic | Chronic severe hepatitis |
| Autoimmune | Class C cirrhosis |
| Uncontrolled Wilson’s disease | Uncontrolled portal hypertension with sequelae |
| Severe coagulopathy1 | |
| Systemic liver-related co-morbidities | |
| Hypoxia (POPH or HPS)2 | |
| Cardiac volume overload | |
| Hepatorenal syndrome |
Severe coagulopathy defined as platelets < 50 000/mm3 and prothrombin time prolonged beyond 3 s with no response to Vitamin K;
POPH: Porto-pulmonary hypertension; HPS: Hepatopulmonary syndrome.
Other proposed individual risk factors include the presence of jaundice, prolonged prothrombin time (> 2.5 s above control that does not correct with vitamin K), ascites, encephalopathy, hypoalbuminemia, portal hypertension, renal insufficiency, hyponatremia, infection, anemia and malnutrition. There is no evidence suggesting that these individual risk factors are better than either CTP or MELD scores. Semi-quantitative liver function tests including galactose elimination capacity, aminopyrine breath test, indocyanine green clearance, mono-ethylglycinexylidide test (MEGX) have also been proposed to risk-stratify patients with cirrhosis undergoing surgery, but these are not available universally and hence not used routinely in clinical practice[11].
The nature of the surgical procedure is an important determinant of postoperative complications. In general, emergency surgery is associated with a higher morbidity and mortality than elective surgery[12-14]. The morbidity and mortality risks are highest in patients undergoing cardiac and open abdominal surgeries including cholecystectomy, gastric resection, colectomy and hepatic resection[11]. Laparotomy causes a greater reduction in liver blood flow and increased hepatic ischemia than extra-abdominal surgery. Another contributing factor is increased risk of intra-operative bleeding in the presence of portal hypertension, especially in patients with previous abdominal surgery and adhesions.
Hemodynamic changes, characterized by increased cardiac output, splanchnic vasodilation and decreased systemic vascular resistance, are common in patients with portal hypertension, and these changes progress with worsening liver disease. Despite an increased cardiac output, perfusion may be impaired due to shunting of blood, and in addition, anesthetic agents may also reduce hepatic blood flow and decrease oxygen uptake by the liver and splanchnic organs[15,16]. Hypotension, hypoxemia, hemorrhage and use of vasoactive drugs may further reduce hepatic oxygenation. Hepatic blood flow and liver function may be further compromised by catecholamine release and other neurohormonal responses[17].
PREOPERATIVE EVALUATION AND RISK ESTIMATION
A thorough preoperative history and physical examination are keystones in the evaluation and management of patients with chronic liver disease prior to surgery. It is essential to assess for the presence and severity of liver disease. In addition to identifying the risk factors for liver disease (blood transfusions, tattoos, illicit drug use, sexual promiscuity, family history of liver disease, alcoholism, travel history, review of prescribed or over the counter medications), it is important to elicit any previous history of decompensation such as ascites, edema, or hepatic encephalopathy, variceal bleeding or anesthesia-related complications (Table 5). Stigmata of chronic liver disease such as jaundice, palmar erythema, spider nevi, gynecomastia, or testicular atrophy and portal hypertension such as splenomegaly, ascites, or asterixis should lead to a thorough evaluation of liver disease and its severity. Figure 1 shows general guidelines for preoperative evaluation of patients with liver disease.
Table 5.
American Society of Anesthesiologists (ASA) Classification of preoperative risk
| ASA Class | Systemic disturbance | Mortality (%) |
| 1 | Healthy patient with no disease outside of the surgical process | < 0.03 |
| 2 | Mild to moderate systemic disease caused by the surgical condition or by other pathological processes, medically well-controlled | 0.2 |
| 3 | Severe disease process which limits activity but is not incapacitating | 1.2 |
| 4 | Severe incapacitating disease process that is a constant threat to life | 8 |
| 5 | Moribund patient not expected to survive 24 h with or without an operation | 34 |
| E | Suffix to indicate emergency surgery for any class | Increased |
bP < 0.01 vs group B and control group; aP < 0.05 vs control group; dP < 0.01 vs group B and control.
Figure 1.
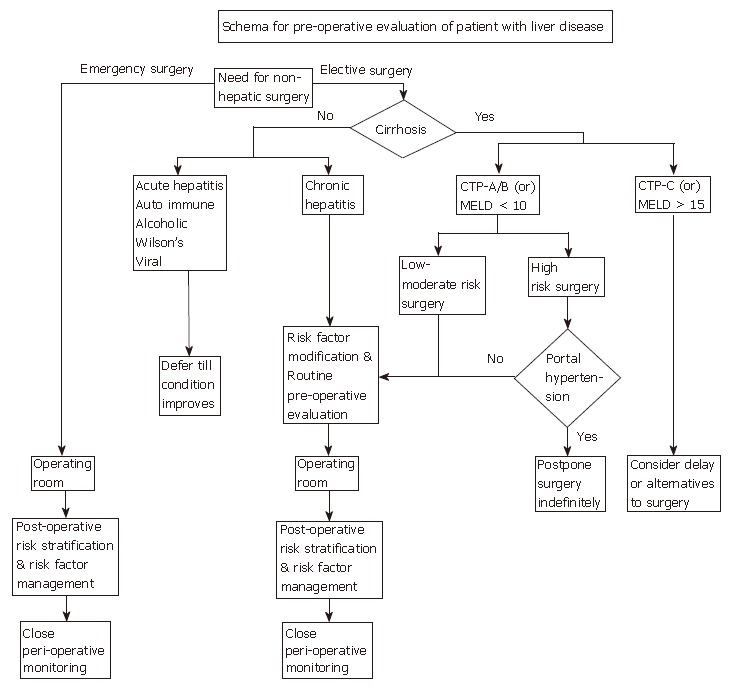
An algorithm for evaluation and management of patients with liver disease prior to surgery.
A preoperative evaluation should comprise laboratory tests such as comprehensive metabolic profile, complete blood counts and prothrombin time. Elevated bilirubin, low albumin, elevated liver enzymes, low platelets and elevated prothrombin time may suggest the presence of chronic liver disease. A medical history suggestive of liver disease, clinical signs of chronic liver disease or abnormal laboratory tests should prompt further evaluation to assess severity of liver disease.
PREOPERATIVE MANAGEMENT
The outcomes of patients with cirrhosis who undergo surgery could be improved by optimizing the following premorbid conditions.
Coagulopathy
Even in urgent surgical situations, management of coagulopathy is beneficial. While peripheral vascular surgery can be performed with significant coagulopathy, neurosurgery usually requires an INR below 1.2, platelets > 100 × 109/L, and fibrinogen > 100 mg/dL. A thromboelastogram, which is a graphic representation of the interaction of plasma coagulation proteins with platelets and fibrinogen, is a useful tool to help guide the administration of coagulation factors in the operating room.
Coagulopathy in liver disease could be due to hepatic synthetic dysfunction or vitamin K deficiency usually caused by malabsorption secondary to prolonged cholestasis. Though hepatic synthetic dysfunction cannot be corrected by vitamin K administration, it may be worthwhile to administer a trial of parenteral vitamin K in elective surgery cases in case malabsorption is a contributing factor. In emergency situations or cases in which there is inadequate response to vitamin K, fresh frozen plasma can be administered. If patients do not respond to fresh frozen plasma, Cryoprecipitate, which contains large amount of fibrinogen and von Willebrand factor, may be given intravenously preoperatively. DDAVP 0.3 μg/kg, which contains endogenous von Willebrand factor and factor VIIa infusion are other novel agents that could be used to correct clotting abnormalities. In most refractory cases, plasma exchange may be necessary. In addition to the correction of coagulopathy, prophylactic platelet transfusions may be considered for severe thrombocytopenia (< 50 000/mL).
Ascites
The presence of ascites may increase the risk of abdominal wound dehiscence, abdominal wall herniation, and respiratory compromise. Ascites could be managed by a combination of low sodium diet and administration of diuretics such as furosemide and spironolactone with careful monitoring of creatinine and electrolyte levels. If ascites is uncontrolled prior to surgery, large volume paracentesis could be performed either preoperatively or intra operatively. Replacement with albumin (8 g for each liter of ascites drained) is important to maintain intravascular volume and to reduce the risk of hepatorenal syndrome.
Patients with ascites could present with abdominal pain from spontaneous bacterial peritonitis (SBP) or secondary bacterial peritonitis. In such situations, it is important to analyze the ascites fluid for differential white cell counts. If absolute ascites neutrophil counts exceed 250 neutrophils/mL, the patient should be treated for SBP with a third generation cephalosporin such as ceftriaxone or a fluoroquinolone such as ciprofloxacin as the common pathogens are usually Escherichia coli and Klebsiella pneumoniae. If multiple organisms are grown, secondary bacterial peritonitis should be suspected.
Since ascites may reaccumulate rapidly with administration of normal saline, it is advisable to use colloids or blood perioperatively. The role of pre-operative transjugular portosystemic shunt (TIPS) to control refractory ascites is poorly defined and is not currently recommended[18].
Renal dysfunction
In advanced liver disease, patients may present with renal insufficiency from a variety of etiologies including iatrogenic causes such as medications [diuretics, non-steroidal anti-inflammatory drugs (NSAID) or other nephrotoxic agents] or large volume paracentesis (often performed without albumin replacement), infections (SBP and urinary tract infections are most common), gastrointestinal bleeding or hepatorenal syndrome (HRS). HRS occurs in the setting of advanced portal hypertension and associated profound splanchnic vasodilation. These changes result in a cascade of events leading to decreased renal perfusion and renal insufficiency. From a practical point of view, HRS is defined by a plasma creatinine > 1.5 mg/dL, in the absence of any iatrogenic causes, bleeding or intrinsic renal diseases, that is not improved by fluid (1.5 liters of isotonic saline) or colloids (albumin 1 g/kg body weight for 3 d) administration[19]. HRS may present in two different ways; rapidly progressive (type 1) where creatinine doubles (100% increase) over a period of 2 wk and slowly progressive (type II) where creatinine is ≥ 1.5 mg/dL, and then progresses slowly. Type 1 HRS has a dismal outcome without liver transplantation. However, HRS that is precipitated by SBP and the intravascular fluid shifts associated with anesthesia or surgery is potentially reversible. Combination treatments with midodrine and octreotide, or terlipressin and albumin have shown promising results, but there is a paucity of controlled data with adequate sample size on these treatment modalities[20,21]. Hemodialysis or continuous veno-venous hemodialysis (CVVHD) is often used as a bridge to liver transplantation; again there are no controlled studies proving its efficacy.
Hyponatremia
Hyponatremia is common in advanced liver disease. Severe hyponatremia may lead to seizures and worsening of hepatic encephalopathy. Rapid correction (> 10 meq/L per 24 h) of sodium, especially in malnourished patients, could lead to fatal central pontine myelinolysis. Hyponatremia is usually corrected by fluid restriction (< 1000 mL/d) and discontinuation of all diuretics. In symptomatic patients, intravenous 3% sodium chloride may be used judiciously[22].
Hepatic encephalopathy
It is important to recognize sub-clinical encephalopathy preoperatively. Many conditions including constipation, alkalosis, central nervous system depressants, hypoxia, infection, azotemia and gastrointestinal bleeding may precipitate overt hepatic encephalopathy (HE). In patients with cirrhosis, especially in those with clinical or sub-clinical HE, many of these precipitating factors could be avoided or treated early to prevent significant HE. HE may complicate the post-operative course resulting in immobility, lack of cooperation with nursing procedures, unnecessary investigations (if not diagnosed clinically or suspected) and aspiration pneumonia. Encephalopathy is treated with lactulose 30 mL orally every 6 h, titrated to 2 or 3 soft bowel movements daily. Metronidazole, rifaximin and low dose neomycin could be used in combination with lactulose, but it is important to avoid neomycin in patients with renal insufficiency[23-25].
Malnutrition
Malnutrition can result in hypoalbuminemia, low oncotic pressure and intravascular hypovolemia. Muscle wasting may result in patient immobility and respiratory muscle dysfunction, leading to prolonged mechanical ventilation postoperatively. When hospitalized with malnutrition, a nutritionist consultation should be obtained. Patients with advanced liver disease should receive nutritional supplementation, both enteral and parenteral in the perioperative period. Consideration should be given to starting the supplementation preoperatively, and this may reduce the short-term mortality and postoperative complications, but the impact of nutritional supplementation on long-term mortality remains unclear[26,27]. The supplementation should be high in carbohydrate/lipid content and low in amino acid content to prevent worsening of preexisting hepatic encephalopathy. Nutritional supplementation is particularly important in alcoholics and should include vitamin B1.
Pulmonary conditions
Common conditions include hydrothorax, hepatopulmonary syndrome, portopulmonary hypertension, immune mediated lung diseases (especially in autoimmune diseases) and emphysema (in smokers and alpha-1 antitrypsin deficiency). Hepatic hydrothorax occurs, usually on the right side, in about 5% of patients with cirrhosis. Preoperative thoracentesis is not usually recommended as the resulting hypoxemia is not very severe[7]. Use of an incentive spirometer postoperatively may prevent atelectasis. Hepatopulmonary syndrome includes the presence of systemic-to-pulmonary vascular shunts and intrapulmonary arteriovenous shunts, both of which result in systemic arterial desaturation. It is marked by orthodeoxia and platypnea and can be diagnosed by contrast echocardiography or a Technetium 99 m-labelled albumin scan. This could be further confirmed by pulmonary angiography. Type 1 HPS is a pattern, which responds well to 100% oxygen supplementation. Type 2 HPS does not respond to oxygen and is considered a contraindication to general anesthesia. Portopulmonary hypertension occurs in 2%-4% of patients with cirrhosis and portal hypertension. It is defined as a mean pulmonary artery pressure (MPAP) greater than 24 mmHg with a normal pulmonary capillary wedge pressure and a pulmonary vascular resistance greater than 120 dynes/s per cm5. When the MPAP is > 50 mmHg, the condition becomes life threatening and can lead to right ventricular failure and hypoxemia. If surgery is contemplated, pulmonary pressures must be optimized usually with intravenous epoprostenol[28], but sildenafil or bosentan have also been tried perioperatively.
Cardiac conditions
Dobutamine stress echocardiography has been advocated as a screening modality for coronary artery disease in patients with cirrhosis. However, its predictive value in patients with advanced cirrhosis is quite variable. In general, the American College of Cardiology and American Heart Association guidelines are useful to assess the suitability of patients with liver disease for non-cardiac surgery. Beta-blockers must be used in the perioperative period if no contraindications exist. They are not only useful in reducing the incidence of perioperative myocardial ischemia and adverse cardiac events, but also help to decrease the portal pressure. In patients with advanced cirrhosis and cardiac disease, less invasive procedures such as angioplasty, valvuloplasty and newer off-pump procedures may prove to be beneficial[29,30].
Miscellaneous
Anemia must be managed aggressively with early and sufficient substitution of clotting factors and blood products. Glucose intolerance and diabetes are common in patients with liver disease. Insulin infusion is beneficial to maintain good control perioperatively. However, caution is warranted as patients with cirrhosis are also at risk for hypoglycemia[31]. Deficiency in 25-hydroxyvitamin D can occur in cirrhosis and if associated with nutritional deficiencies will lead to osteomalacia and will require Vitamin D and Calcitriol supplementation. Screening for varices should be performed in cirrhotic patients and those receiving beta blockade for prophylaxis of variceal bleeding and should continue to do so in the perioperative period[32,33]. Preoperative antibiotic prophylaxis is mandatory due to high rates of septic complications in patients with cirrhosis. In an emergency situation, especially after resectional procedures, selective bowel decontamination and prolonged course of antibiotics must be considered. In patients with peptic ulcer disease, long-term maintenance therapy with proton pump inhibitors may be recommended[34].
Strategies for specific liver conditions
Stress-dose steroids should be administered preoperatively in patients with autoimmune hepatitis who are on steroid therapy. Patients treated with D-pencillamine for Wilson’s disease can suffer from poor wound healing and thereby, the dosage should be decreased preoperatively and for one to two weeks postoperatively.
OPERATIVE AND POSTOPERATIVE MANAGEMENT
Liver dysfunction may result in prolonged duration of action of anesthetic and neuromuscular blocking agents because of altered metabolism or clearance rates. Isoflurane is the preferred anesthetic agent for patients with cirrhosis, while methoxyflurane, chloroform and halothane should be avoided if possible. In addition, the actions of neuromuscular blocking agents may be prolonged due to increased biliary excretion and decreased pseudocholinesterase activity. Therefore, atracurium is the drug of choice in patients with liver disease or biliary obstruction, and doxacurium is recommended for prolonged surgeries. Oxazepam and lorazepam are the most suitable anxiolytic sedatives, whereas fentanyl and sufentanyl should be the first-line narcotics. In contrast, morphine, meperidine and barbiturates can precipitate hepatic encephalopathy and should be avoided[35].
Postoperative complications in patients undergoing surgery include (1) cirrhosis related complications: worsening or new onset ascites, worsening or new onset hepatic encephalopathy (Grade 1-4), upper gastrointestinal bleeding, worsening or new onset acute renal failure/new need for dialysis, hepatorenal syndrome (acute renal failure in the setting of decreasing liver function with no other clinical, laboratory or anatomic cause for the renal failure), liver failure, and coagulopathy [disseminated intravascular coagulation (DIC), increased prothrombin time, increased activated partial thromboplastin time, decreased fibrinogen concentration, decreased platelet count]; (2) surgical wound complications: infection, dehiscence, eventration, fistula, abscess, surgical site bleeding; and (3) general complications: pneumonia/Acute Respiratory Distress Syndrome (ARDS), ventilation dependence, chronic obstructive pulmonary diseases (COPD) exacerbation, chronic heart failure/arrhythmia/myocardial infarction, urinary tract infections, paralytic ileus, phlebitis/PE, and death.
The common complications of surgery in patients with cirrhosis are hemorrhage, sepsis, liver failure, fluid overload and hepatorenal syndrome. Patients with cholestatic jaundice are at an increased risk of postoperative renal failure. Increased postoperative bilirubin levels (> 3 mg/dL), creatinine levels and a decreased albumin level are associated with greater mortality[36].
Pre-operative strategies, which has been discussed earlier to minimize complications, should be continued in the post-transplant period. In addition, in the post-operative period, one needs to closely monitor fluid balance and nutrition, identify and correct electrolyte abnormalities, coagulopathy, encephalopathy and infection. Non-steroidal anti-inflammatory drugs and nephrotoxic drugs should be avoided, and caution should be exercised with use of narcotics.
CONCLUSION
The mortality from abdominal surgeries in patients with cirrhosis is unacceptably high. Preoperative assessment can predict survival to some extent in cirrhotic patients requiring abdominal procedures. Furthermore, optimization of premorbid factors may reduce perioperative mortality and morbidity. However, better predictive models for risk-stratification are necessary to predict and improve post-operative outcomes of patients with cirrhosis[37].
ACKNOWLEDGMENTS
We thank Murtuza Balasinorwala for his help with the preparation of the illustrations.
COMMENTS
Background
In patients with cirrhosis, the surgical mortality is as high as 25%. Pre-operative risk stratification in such patients and optimization of medical care prior to surgery are essential to prevent adverse outcomes after surgery.
Research frontiers
Studies with better predictive models for risk-stratification are necessary to predict and improve post-operative outcomes of patients with cirrhosis.
Innovations and breakthroughs
The recent adoption of the MELD score by UNOS to risk stratify patients prior to transplant surgery has improved our ability to better characterize the severity of liver disease objectively in liver transplant population. Similar models are necessary to risk-stratify patients prior to any other surgery in patients with cirrhosis.
Applications
CTP score, MELD score, age, and American Society of Anesthesiologists class are factors that can quantify the risk of mortality postoperatively in patients with cirrhosis, independent of the procedure performed. These factors can be used in determining operative mortality risk, and to decide whether elective surgical procedures can be delayed until after liver transplantation.
Terminology
MELD score is a numerical score obtained by inserting the values of serum total bilirubin, INR and serum creatinine into a logarithmic formula. It is a disease severity index score and helps determine the mortality without liver transplantation in patients with advanced cirrhosis.
Peer review
The authors reviewed the pathophysiology, morbidity and mortality associated with non-hepatic surgery in patients with cirrhosis, and then recommend an algorithm for risk assessment and evidence based management strategy to optimize post-surgical outcomes. They concluded that better predictive models for risk-stratification are necessary to predict and improve post-operative outcomes of patients with cirrhosis
Footnotes
S- Editor Zhu LH L-Editor Zhu LH E-Editor Li JL
References
- 1.Noble JA, Caces MF, Steffens RA, Stinson FS. Cirrhosis hospitalization and mortality trends, 1970-87. Public Health Rep. 1993;108:192–197. [PMC free article] [PubMed] [Google Scholar]
- 2.Jackson FC, Christophersen EB, Peternel WW, Kirimli B. Preoperative management of patients with liver disease. Surg Clin North Am. 1968;48:907–930. doi: 10.1016/s0039-6109(16)38591-7. [DOI] [PubMed] [Google Scholar]
- 3.Ziser A, Plevak DJ, Wiesner RH, Rakela J, Offord KP, Brown DL. Morbidity and mortality in cirrhotic patients undergoing anesthesia and surgery. Anesthesiology. 1999;90:42–53. doi: 10.1097/00000542-199901000-00008. [DOI] [PubMed] [Google Scholar]
- 4.Aranha GV, Sontag SJ, Greenlee HB. Cholecystectomy in cirrhotic patients: a formidable operation. Am J Surg. 1982;143:55–60. doi: 10.1016/0002-9610(82)90129-5. [DOI] [PubMed] [Google Scholar]
- 5.del Olmo JA, Flor-Lorente B, Flor-Civera B, Rodriguez F, Serra MA, Escudero A, Lledó S, Rodrigo JM. Risk factors for nonhepatic surgery in patients with cirrhosis. World J Surg. 2003;27:647–652. doi: 10.1007/s00268-003-6794-1. [DOI] [PubMed] [Google Scholar]
- 6.Leonetti JP, Aranha GV, Wilkinson WA, Stanley M, Greenlee HB. Umbilical herniorrhaphy in cirrhotic patients. Arch Surg. 1984;119:442–445. doi: 10.1001/archsurg.1984.01390160072014. [DOI] [PubMed] [Google Scholar]
- 7.Keegan MT, Plevak DJ. Preoperative assessment of the patient with liver disease. Am J Gastroenterol. 2005;100:2116–2127. doi: 10.1111/j.1572-0241.2005.41453.x. [DOI] [PubMed] [Google Scholar]
- 8.Wiklund RA. Preoperative preparation of patients with advanced liver disease. Crit Care Med. 2004;32:S106–S115. doi: 10.1097/01.ccm.0000115624.13479.e6. [DOI] [PubMed] [Google Scholar]
- 9.Northup PG, Wanamaker RC, Lee VD, Adams RB, Berg CL. Model for End-Stage Liver Disease (MELD) predicts nontransplant surgical mortality in patients with cirrhosis. Ann Surg. 2005;242:244–251. doi: 10.1097/01.sla.0000171327.29262.e0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Befeler AS, Palmer DE, Hoffman M, Longo W, Solomon H, Di Bisceglie AM. The safety of intra-abdominal surgery in patients with cirrhosis: model for end-stage liver disease score is superior to Child-Turcotte-Pugh classification in predicting outcome. Arch Surg. 2005;140:650–64; discussion 655. doi: 10.1001/archsurg.140.7.650. [DOI] [PubMed] [Google Scholar]
- 11.Friedman LS. The risk of surgery in patients with liver disease. Hepatology. 1999;29:1617–1623. doi: 10.1002/hep.510290639. [DOI] [PubMed] [Google Scholar]
- 12.Mansour A, Watson W, Shayani V, Pickleman J. Abdominal operations in patients with cirrhosis: still a major surgical challenge. Surgery. 1997;122:730–735; discussion 735 -736. doi: 10.1016/s0039-6060(97)90080-5. [DOI] [PubMed] [Google Scholar]
- 13.Farnsworth N, Fagan SP, Berger DH, Awad SS. Child-Turcotte-Pugh versus MELD score as a predictor of outcome after elective and emergent surgery in cirrhotic patients. Am J Surg. 2004;188:580–583. doi: 10.1016/j.amjsurg.2004.07.034. [DOI] [PubMed] [Google Scholar]
- 14.Garrison RN, Cryer HM, Howard DA, Polk HC. Clarification of risk factors for abdominal operations in patients with hepatic cirrhosis. Ann Surg. 1984;199:648–655. doi: 10.1097/00000658-198406000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Friedman LS, Maddrey WC. Surgery in the patient with liver disease. Med Clin North Am. 1987;71:453–476. doi: 10.1016/s0025-7125(16)30851-3. [DOI] [PubMed] [Google Scholar]
- 16.Gholson CF, Provenza JM, Bacon BR. Hepatologic considerations in patients with parenchymal liver disease undergoing surgery. Am J Gastroenterol. 1990;85:487–496. [PubMed] [Google Scholar]
- 17.Kowalski HJ, Abelmann WH. The cardiac output at rest in Laennec's cirrhosis. J Clin Invest. 1953;32:1025–1033. doi: 10.1172/JCI102813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vinet E, Perreault P, Bouchard L, Bernard D, Wassef R, Richard C, Létourneau R, Pomier-Layrargues G. Transjugular intrahepatic portosystemic shunt before abdominal surgery in cirrhotic patients: a retrospective, comparative study. Can J Gastroenterol. 2006;20:401–404. doi: 10.1155/2006/245082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Arroyo V, Ginès P, Gerbes AL, Dudley FJ, Gentilini P, Laffi G, Reynolds TB, Ring-Larsen H, Schölmerich J. Definition and diagnostic criteria of refractory ascites and hepatorenal syndrome in cirrhosis. International Ascites Club. Hepatology. 1996;23:164–176. doi: 10.1002/hep.510230122. [DOI] [PubMed] [Google Scholar]
- 20.Angeli P, Volpin R, Gerunda G, Craighero R, Roner P, Merenda R, Amodio P, Sticca A, Caregaro L, Maffei-Faccioli A, et al. Reversal of type 1 hepatorenal syndrome with the administration of midodrine and octreotide. Hepatology. 1999;29:1690–1697. doi: 10.1002/hep.510290629. [DOI] [PubMed] [Google Scholar]
- 21.Ortega R, Ginès P, Uriz J, Cárdenas A, Calahorra B, De Las Heras D, Guevara M, Bataller R, Jiménez W, Arroyo V, et al. Terlipressin therapy with and without albumin for patients with hepatorenal syndrome: results of a prospective, nonrandomized study. Hepatology. 2002;36:941–948. doi: 10.1053/jhep.2002.35819. [DOI] [PubMed] [Google Scholar]
- 22.Soupart A, Decaux G. Therapeutic recommendations for management of severe hyponatremia: current concepts on pathogenesis and prevention of neurologic complications. Clin Nephrol. 1996;46:149–169. [PubMed] [Google Scholar]
- 23.Williams R, James OF, Warnes TW, Morgan MY. Evaluation of the efficacy and safety of rifaximin in the treatment of hepatic encephalopathy: a double-blind, randomized, dose-finding multi-centre study. Eur J Gastroenterol Hepatol. 2000;12:203–208. doi: 10.1097/00042737-200012020-00012. [DOI] [PubMed] [Google Scholar]
- 24.Bucci L, Palmieri GC. Double-blind, double-dummy comparison between treatment with rifaximin and lactulose in patients with medium to severe degree hepatic encephalopathy. Curr Med Res Opin. 1993;13:109–118. doi: 10.1185/03007999309111539. [DOI] [PubMed] [Google Scholar]
- 25.Tarao K, Ikeda T, Hayashi K, Sakurai A, Okada T, Ito T, Karube H, Nomoto T, Mizuno T, Shindo K. Successful use of vancomycin hydrochloride in the treatment of lactulose resistant chronic hepatic encephalopathy. Gut. 1990;31:702–706. doi: 10.1136/gut.31.6.702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fan ST, Lo CM, Lai EC, Chu KM, Liu CL, Wong J. Perioperative nutritional support in patients undergoing hepatectomy for hepatocellular carcinoma. N Engl J Med. 1994;331:1547–1552. doi: 10.1056/NEJM199412083312303. [DOI] [PubMed] [Google Scholar]
- 27.Nompleggi DJ, Bonkovsky HL. Nutritional supplementation in chronic liver disease: an analytical review. Hepatology. 1994;19:518–533. [PubMed] [Google Scholar]
- 28.Kuo PC, Plotkin JS, Gaine S, Schroeder RA, Rustgi VK, Rubin LJ, Johnson LB. Portopulmonary hypertension and the liver transplant candidate. Transplantation. 1999;67:1087–1093. doi: 10.1097/00007890-199904270-00001. [DOI] [PubMed] [Google Scholar]
- 29.Khan NE, De Souza A, Mister R, Flather M, Clague J, Davies S, Collins P, Wang D, Sigwart U, Pepper J. A randomized comparison of off-pump and on-pump multivessel coronary-artery bypass surgery. N Engl J Med. 2004;350:21–28. doi: 10.1056/NEJMoa031282. [DOI] [PubMed] [Google Scholar]
- 30.Gaudino M, Santarelli P, Bruno P, Piancone FL, Possati G. Palliative coronary artery surgery in patients with severe noncardiac diseases. Am J Cardiol. 1997;80:1351–1352. doi: 10.1016/s0002-9149(97)00681-4. [DOI] [PubMed] [Google Scholar]
- 31.van den Berghe G, Wouters P, Weekers F, Verwaest C, Bruyninckx F, Schetz M, Vlasselaers D, Ferdinande P, Lauwers P, Bouillon R. Intensive insulin therapy in critically ill patients. N Engl J Med. 2001;345:1359–1367. doi: 10.1056/NEJMoa011300. [DOI] [PubMed] [Google Scholar]
- 32.Poldermans D, Boersma E, Bax JJ, Thomson IR, van de Ven LL, Blankensteijn JD, Baars HF, Yo TI, Trocino G, Vigna C, et al. The effect of bisoprolol on perioperative mortality and myocardial infarction in high-risk patients undergoing vascular surgery. Dutch Echocardiographic Cardiac Risk Evaluation Applying Stress Echocardiography Study Group. N Engl J Med. 1999;341:1789–1794. doi: 10.1056/NEJM199912093412402. [DOI] [PubMed] [Google Scholar]
- 33.Wallace A, Layug B, Tateo I, Li J, Hollenberg M, Browner W, Miller D, Mangano DT. Prophylactic atenolol reduces postoperative myocardial ischemia. McSPI Research Group. Anesthesiology. 1998;88:7–17. doi: 10.1097/00000542-199801000-00005. [DOI] [PubMed] [Google Scholar]
- 34.Lehnert T, Herfarth C. Peptic ulcer surgery in patients with liver cirrhosis. Ann Surg. 1993;217:338–346. doi: 10.1097/00000658-199304000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Maze M. Anesthesia and the liver. In: Anesthesia , editor. 4th ed. Miller RD, editor. Edinburgh: Churchill Livingstone; 1994. pp. 1969–1980. [Google Scholar]
- 36.Runyon BA. Surgical procedures are well tolerated by patients with asymptomatic chronic hepatitis. J Clin Gastroenterol. 1986;8:542–544. doi: 10.1097/00004836-198610000-00010. [DOI] [PubMed] [Google Scholar]
- 37.Goldman L, Caldera DL, Nussbaum SR, Southwick FS, Krogstad D, Murray B, Burke DS, O'Malley TA, Goroll AH, Caplan CH, et al. Multifactorial index of cardiac risk in noncardiac surgical procedures. N Engl J Med. 1977;297:845–850. doi: 10.1056/NEJM197710202971601. [DOI] [PubMed] [Google Scholar]
- 38.Brolin RE, Bradley LJ, Taliwal RV. Unsuspected cirrhosis discovered during elective obesity operations. Arch Surg. 1998;133:84–88. doi: 10.1001/archsurg.133.1.84. [DOI] [PubMed] [Google Scholar]
- 39.Cryer HM, Howard DA, Garrison RN. Liver cirrhosis and biliary surgery: assessment of risk. South Med J. 1985;78:138–141. doi: 10.1097/00007611-198502000-00005. [DOI] [PubMed] [Google Scholar]
- 40.Thulstrup AM, Sørensen HT, Vilstrup H. Mortality after open cholecystectomy in patients with cirrhosis of the liver: a population-based study in Denmark. Eur J Surg. 2001;167:679–683. doi: 10.1080/11024150152619327. [DOI] [PubMed] [Google Scholar]
- 41.Palanivelu C, Rajan PS, Jani K, Shetty AR, Sendhilkumar K, Senthilnathan P, Parthasarthi R. Laparoscopic cholecystectomy in cirrhotic patients: the role of subtotal cholecystectomy and its variants. J Am Coll Surg. 2006;203:145–151. doi: 10.1016/j.jamcollsurg.2006.04.019. [DOI] [PubMed] [Google Scholar]
- 42.Wahlstrom K, Ney AL, Jacobson S, Odland MD, Van Camp JM, Rodriguez JL, West MA. Trauma in cirrhotics: survival and hospital sequelae in patients requiring abdominal exploration. Am Surg. 2000;66:1071–1076. [PubMed] [Google Scholar]
- 43.Hayashi PH, Mehia C, Joachim Reimers H, Solomon HS, Bacon BR. Splenectomy for thrombocytopenia in patients with hepatitis C cirrhosis. J Clin Gastroenterol. 2006;40:740–744. doi: 10.1097/00004836-200609000-00015. [DOI] [PubMed] [Google Scholar]
- 44.Carbonell AM, Wolfe LG, DeMaria EJ. Poor outcomes in cirrhosis-associated hernia repair: a nationwide cohort study of 32,033 patients. Hernia. 2005;9:353–357. doi: 10.1007/s10029-005-0022-x. [DOI] [PubMed] [Google Scholar]
- 45.Cohen SM, Te HS, Levitsky J. Operative risk of total hip and knee arthroplasty in cirrhotic patients. J Arthroplasty. 2005;20:460–466. doi: 10.1016/j.arth.2004.05.004. [DOI] [PubMed] [Google Scholar]
- 46.Shih LY, Cheng CY, Chang CH, Hsu KY, Hsu RW, Shih HN. Total knee arthroplasty in patients with liver cirrhosis. J Bone Joint Surg Am. 2004;86-A:335–341. doi: 10.2106/00004623-200402000-00017. [DOI] [PubMed] [Google Scholar]
- 47.Hayashida N, Shoujima T, Teshima H, Yokokura Y, Takagi K, Tomoeda H, Aoyagi S. Clinical outcome after cardiac operations in patients with cirrhosis. Ann Thorac Surg. 2004;77:500–505. doi: 10.1016/j.athoracsur.2003.06.021. [DOI] [PubMed] [Google Scholar]
- 48.Klemperer JD, Ko W, Krieger KH, Connolly M, Rosengart TK, Altorki NK, Lang S, Isom OW. Cardiac operations in patients with cirrhosis. Ann Thorac Surg. 1998;65:85–87. doi: 10.1016/s0003-4975(97)00931-4. [DOI] [PubMed] [Google Scholar]
- 49.Nielsen SS, Thulstrup AM, Lund L, Vilstrup H, Sørensen HT. Postoperative mortality in patients with liver cirrhosis undergoing transurethral resection of the prostate: a Danish nationwide cohort study. BJU Int. 2001;87:183–186. doi: 10.1046/j.1464-410x.2001.02048.x. [DOI] [PubMed] [Google Scholar]
- 50.Nielsen IL, Thulstrup AM, Nielsen GL, Larsen H, Vilstrup H, Sørensen HT. Thirty-day postoperative mortality after hysterectomy in women with liver cirrhosis: a Danish population-based cohort study. Eur J Obstet Gynecol Reprod Biol. 2002;102:202–205. doi: 10.1016/s0301-2115(01)00603-0. [DOI] [PubMed] [Google Scholar]
- 51.Powell-Jackson P, Greenway B, Williams R. Adverse effects of exploratory laparotomy in patients with unsuspected liver disease. Br J Surg. 1982;69:449–451. doi: 10.1002/bjs.1800690805. [DOI] [PubMed] [Google Scholar]
- 52.O'Sullivan MJ, Evoy D, O'Donnell C, Rajpal PK, Cannon B, Kenny-Walsh L, Whelton MJ, Redmond HP, Kirwan WO. Gallstones and laparoscopic cholecystectomy in hepatitis C patients. Ir Med J. 2001;94:114–117. [PubMed] [Google Scholar]
- 53.Dixon JM, Armstrong CP, Duffy SW, Davies GC. Factors affecting morbidity and mortality after surgery for obstructive jaundice: a review of 373 patients. Gut. 1983;24:845–852. doi: 10.1136/gut.24.9.845. [DOI] [PMC free article] [PubMed] [Google Scholar]


