Abstract
AIM: To investigate the allelic and haplotypic association of reg1α gene with tropical calcific pancreatitis (TCP). Since TCP is known to have a variable genetic basis, we investigated the interaction between mutations in the susceptibility genes, SPINK1 and CTSB with reg1α polymorphisms.
METHODS: We analyzed the polymorphisms in the reg1α gene by sequencing the gene including its promoter region in 195 TCP patients and 150 ethnically matched controls, compared their allele and haplotype frequencies, and their association with the pathogenesis and pancreaticolithiasis in TCP and fibro-calculous pancreatic diabetes.
RESULTS: We found 8 reported and 2 novel polymo-rphisms including an insertion-deletion polymorphism in the promoter region of reg1α. None of the 5’ UTR variants altered any known transcription factor binding sites, neither did any show a statistically significant association with TCP. No association with any reg1α variants was observed on dichotomization of patients based on their N34S SPINK1 or L26V CTSB status.
CONCLUSION: Polymorphisms in reg1α gene, including the regulatory variants singly or in combination with the known mutations in SPINK1 and/or CTSB genes, are not associated with tropical calcific pancreatitis.
Keywords: Tropical calcific pancreatitis, Lithostathine, Stone formation, Polymorphism, Haplotype
INTRODUCTION
Chronic Pancreatitis (CP) is a continuing or relapsing inflammatory process of the pancreas resulting in exocrine and/or endocrine insufficiency. The cardinal manifestations of CP are pain, steatorrhoea, formation of pancreatic stones, and diabetes mellitus. Recently, mutations in cationic trypsinogen (PRSS1)[1], the serine protease inhibitor, Kazal type 1 (SPINK1)[2], and cystic fibrosis transmembrane regulator (CFTR)[3] genes have been found to be associated with chronic pancreatitis. Tropical calcific pancreatitis (TCP) is an idiopathic, juvenile, nonalcoholic form of chronic pancreatitis with a unique tropical distribution, while fibro-calculous pancreatic diabetes (FCPD) is a condition characterized by the development of diabetes secondary to TCP. A genetic etiology for TCP and FCPD was suggested by Pitchumoni et al[4] and confirmed by Mohan el al[5], who showed familial aggregation of FCPD with evidence of vertical transmission in some families. We previously reported evidence of its genetic nature, based on clustering of TCP in a few families and its association with SPINK1 mutations[6].
In a previous study we had shown that mutations in PRSS1 did not play a role in TCP, whereas mutations in SPINK1 gene were found in the majority of such patients[7]. Recently, we have demonstrated that mutations in pro-peptide region of cathepsin B (CTSB) gene are strongly associated with TCP[8]. Irrespective of mutations in different genes, premature intra-pancreatic activation of trypsinogen is believed to play a central role in the pathogenesis of chronic pancreatitis. However, the phenomenon of stone formation continues to be poorly understood. Although various hypotheses have been proposed for stone formation, the development of protein plugs appears to be an important initiating event[9]. It has been proposed that if concentration-dependent precipitation is the cause of protein plug formation, there should be an associated increase in the concentration of some proteins in the pancreatic juice[10].
Lithostathine C was initially isolated as a major proteic component of pancreatic stones in alcoholic calcifying chronic pancreatitis, and was consequently called pancreatic stone proteic (PSP)[9]. Human PSP or Reg protein is encoded by reg1α gene (regenerating gene)[11] as a 166 amino acid pre-proprotein with a 22-residue long signal sequence. A similar protein with 89% homology with PSP is coded by another gene reg1β belonging to the same type 1 subclass but has never been isolated and its expression in pancreas remains controversial[12]. Only the Reg1α protein is highly represented in the human pancreatic secretions[13] and is found to be 100% identical to a glycoprotein that is generated by trypsin cleavage resulting in a 133 aa polypeptide previously named pancreatic thread protein (PTP). The mature protein is a soluble glycoprotein existing under 11 isoforms (17-22 kDa)[14], generated by post-translational modification such as glycosylation. Of these isoforms, S2-S5 are believed to inhibit calcite crystal growth in vitro and thus stone formation[15,16]. PSP is highly susceptible to trypsin cleavage at Arg11-Ile12 bond resulting in PTP formation, which is known to form fibrilla at neutral pH and is found in protein plugs or stones extracted from pancreatic ducts of CP patients[9,17]. The exact function of Reg1α protein is not clear, but it could stimulate the regeneration and/or growth of pancreatic β-cell[18]. We hypothesized that mutations in the promoter region of reg1α may lead to altered expression of the protein. Alternatively, variants in the coding region could predispose the Reg1 protein to increased tryptic cleavage resulting in greater formation of PTP. This may cause precipitation of PTP and obstruction of the pancreatic duct secondary to protein plugs and calculi, resulting in pancreatitis. Since high levels of intrapancreatic trypsin produced both by known mechanisms like PRSS1 mutations or by as yet unknown mechanisms such as mutations in SPINK1 and CTSB genes is an established fact, it can be speculated that intrapancreatic trypsin may cleave the soluble lithostathine (PSP S2-S5) into insoluble PTP. FCPD is a condition characterized by the development of diabetes secondary to TCP, however, the etiology of diabetes in these patients is not clear, hence we investigated the role of these polymorphisms in the pathogenesis of FCPD. Since, N34S SPINK1 mutations occur in the majority of these patients and it is not clear whether pancreatitis is the cause or the effect of ductal obstruction, we attempted to investigate the interaction between N34S SPINK1 mutation and L26V CTSB mutations and reg1α gene polymorphisms. We also performed haplotype analysis to see if a particular reg1α haplotype is associated with the disease.
MATERIALS AND METHODS
Patients and controls
195 unrelated subjects belonging to Australoid ethnicity[19] (134 males and 61 females), diagnosed with tropical calcific pancreatitis at the Asian Institute of Gastroenterology, Hyderabad and 150 age and sex matched individuals (98 males and 52 females) of the same ethnicity but without any evidence of pancreatitis on imaging studies were included as patients and controls respectively[7]. Both the patients and the controls completed a detailed questionnaire and underwent similar investigations including imaging studies. Written informed consent was obtained from all the patients and controls, before the collection of blood samples. The Institutional Ethics Committee of both participating institutes approved the study as per the guidelines of the Indian Council of Medical Research for research on human subjects.
Genetic analysis
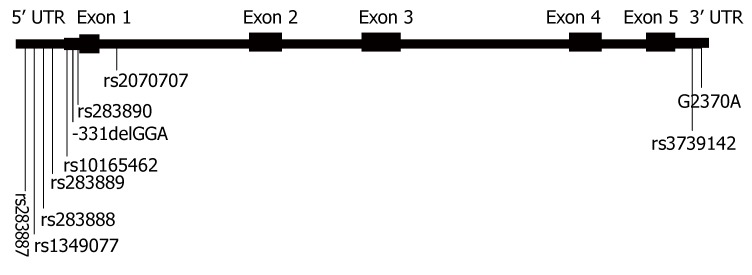
Genomic DNA was isolated from patients and healthy volunteers using salting out method[20]. The human reg1α gene is located on 2p12 with six exons (5 translated exons, Figure 1) spanning 2962 base pairs and is known to contain TATA and CCAAT box-like sequences that are located at 27 and 100 bp upstream from the transcriptional initiation site[21]. Using the software tool Transplorer (Biobase Biological Databases, Wolfenbuttel, Germany), we attempted to identify transcription factor binding sites in a sequence of about 1600 bases upstream of transcriptional start site, which included the above-mentioned sequence[22]. We screened the complete reg1α gene including its exons, introns and 5'- and 3'- untranslated regions by direct sequencing, using 4 sets of primers in 50 patients and 50 controls (Table 1). PCR products were purified and sequenced individually on both the strands using Big-dye terminator cycle sequencing ready kit (Applied Biosystems, Foster City, CA) on an ABI3730 Genetic Analyzer (Applied Biosystems). In case of unclear sequence data, we repeated sequencing under various conditions until the genotype was determined correctly. Six SNPs (Table 2) that exceeded allele frequency of 3% were screened in another 145 patients and 100 controls from the same ethnic background. N34S and L26V mutations in the SPINK1 and in CTSB genes respectively were analyzed using the methodology as described previously[7,8]. Ten percent of randomly chosen samples were re-genotyped for validation of the data, and no genotyping error was noted.
Figure 1.
Diagrammatic representation of the reg1α gene showing exons (translated), UTRs (untranslated regions) and the location of the polymorphisms studied (constructed on the lines of reg1α gene structure as on UCSC genome browser, figure not to scale).
Table 1.
Primer sequences and PCR conditions for the reg1α gene
| Primer | Sequence (5'-3') | Tann (°C) |
| 1F | TGTCCCAATTCATATACTTA | 50 |
| 1R | GCATGTTAGAGACGCCCTTC | |
| 2F | CGGGAAAAGGCTCGTACTGG | 60 |
| 2R | TCAGTTCTCCACCCCATTAG | |
| 3F | TAAAAGGGAAACTGGAGACT | 56 |
| 3R | CCTCCTTCTTACTTCTCAAA | |
| 4F | TGCACTGTAGATGATTGGAG | 62 |
| 4R | AAAGACTGGGGTAGGTAAAACT | |
| 4F-INT1 | TCTTGGTGGAATACAGTTAA | Seq |
| 4F-INT2 | AATGGATGTTTGGTTTTTGT | Seq |
F: Forward; R: Reverse; Tann: Annealing temperature; INT: Internal primer for sequencing.
Table 2.
Distribution of polymorphisms in reg1α gene in patients with tropical calcific pancreatitis and healthy controls
| Polymorphism2 | rs number | Position5 |
Minor allele frequency |
OR (95% CI) | P Value | |
| Patients (n = 195) | Controls (n = 150) | |||||
| G-974C4 | rs283887 | 79200522 | 0.01 | 0.02 | 0.49 (0.02-7.10) | 1.001 |
| G-938A | rs1349077 | 79200558 | 0.34 | 0.33 | 1.05 (0.56-1.96) | 0.88 |
| T-912G | rs283888 | 79200584 | 0.49 | 0.50 | 0.94 (0.54-1.78) | 0.84 |
| G-501A4 | rs283889 | 79200995 | 0.01 | 0.02 | 0.49 (0.02-7.10) | 1.001 |
| T-385C | rs10165462 | 79201111 | 0.32 | 0.29 | 1.15 (0.60-2.20) | 0.65 |
| -331delGGA3 | - | - | 0.01 | 0.01 | 1.00 | 1.001 |
| T-243G | rs283890 | 79201253 | 0.34 | 0.35 | 1.09 (0.75-1.58) | 0.63 |
| G209T | rs2070707 | 79201704 | 0.20 | 0.17 | 1.29 (0.78-2.12) | 0.29 |
| G2199A | rs3739142 | 79203694 | 0.34 | 0.34 | 1.01 (0.70-1.48) | 0.94 |
| G2370A34 | - | - | 0.01 | 0.03 | 0.33 (0.01-3.60) | 0.611 |
AA: Amino acid; OR: Odds ratio; CI: Confidence interval;
Yates corrected P value;
Nomenclature as per NCBI sequence Accession No. NT_022184;
Novel polymorphism;
Data from 50 patients & 50 controls;
Chromosomal location according to UCSC Genome Browser, March 2006 build (dbSNP build 126).
Statistical analysis
The allele and genotype frequencies were calculated for each polymorphism (Table 2) in the whole cohort as well as in TCP and FCPD patients separately (Table 3). We analyzed any deviation from the Hardy-Weinberg equilibrium, and observed the expected genotype frequencies by Markov simulation based goodness of fit test using Arlequin software version 2[23]. Pearson’s Chi-square and Yates corrected chi-square test were used to analyze the statistical significance of the difference in allelic distribution of polymorphisms in patients and controls. Haplotypes were generated with 6 polymorphisms having a minimum allele frequency greater than 3% with the accelerated Expectation-maximization algorithm using Haploview software (Version 3.2) and compared the results between patients and controls[24]. This study was 90% powered to detect a relative risk of 1.60 (http://www.dssresearch.com/). Unless indicated specifically, a P-value of 0.05 was considered significant in all the analyses. Chi-square, genotype relative risk, odds ratio and confidence interval were calculated using the PEPI (Programme for EPIdemiologists, ver 4.04) and DeFenetti programs (http://www.ihg.gsf.de/cgi-bin/hw/hwa1/).
Table 3.
Comparison of reg1α gene polymorphisms in FCPD and TCP patients, and controls
| SNP1 |
Minor allele frequency |
FCPD vs TCP |
FCPD vs Controls |
TCP vs Controls |
|||||
| FCPD (n = 94) | TCP (n = 101) | Controls (n = 150) | OR (95% CI) | P value | OR (95% CI) | P value | OR (95% CI) | P value | |
| G-938A | 0.36 | 0.32 | 0.33 | 1.20 (0.64-2.24) | 0.55 | 1.14 (0.61-2.13) | 0.66 | 0.96 (0.51-1.80) | 0.88 |
| T-912G | 0.47 | 0.51 | 0.50 | 0.85 (0.47-1.54) | 0.57 | 0.89 (0.49-1.60) | 0.67 | 1.04 (0.58-1.88) | 0.89 |
| T-385C | 0.31 | 0.30 | 0.29 | 1.05 (0.55-2.00) | 0.88 | 1.10 (0.57-2.11) | 0.76 | 1.05 (0.55-2.02) | 0.88 |
| T-243G | 0.33 | 0.35 | 0.35 | 0.91 (0.49-1.71) | 0.77 | 0.91 (0.49-1.71) | 0.77 | 1.00 | 1.00 |
| G209T | 0.24 | 0.17 | 0.17 | 1.54 (0.73-3.27) | 0.22 | 1.54 (0.73-3.27) | 0.22 | 1.00 | 1.00 |
| G2199A | 0.41 | 0.33 | 0.34 | 1.41 (0.76-2.62) | 0.24 | 1.35 (0.73-2.50) | 0.31 | 0.96 (0.51-1.79) | 0.88 |
SNP: Single nucleotide polymorphism; n: Number of individuals; OR: Odds ratio; CI: Confidence interval; TCP: Tropical calcific pancreatitis; FCPD: Fibrocalculous pancreatic diabetes;
Only SNPs with > 3% minor allele frequency have been presented; The minor allele frequency at each polymorphism was compared between the three groups and P value with OR and 95% CI were calculated.
RESULTS
We initially sequenced complete reg1α gene in 50 patients and an equal number of controls and subsequently, additional patients and controls were screened for six SNPs with rare allele frequency of > 3%. Sequencing results revealed the presence of 8 reported SNPs, one novel SNP and one insertion-deletion polymorphism in the promoter region of the gene (Table 4). We did not observe any significant deviation from Hardy-Weinberg equilibrium (P > 0.05) for any of the polymorphisms. The polymorphisms in the promoter region were of prime interest, since the levels of reg1α expression differ considerably between the pancreas of patients and controls. Transplorer predicted 3 transcription factor-binding sites (C-Rel, -1513 to -1609; NFκB2, -1527 to -1614; and Hesx1, -15 to -105) within the region +10 to -1600 bp of the putative promoter region[21]. We sequenced the upstream region flanking the 5'-UTR (about 1176 bp upstream of translation start site) along with putative promoter region and found four reported SNPs, G-938A, T-912G, T-385C, T-243G which were equally frequent in patients and controls. A novel insertion-deletion polymorphism at -331 position (-331 to -329) involving deletion of GGA (-331delGGA) in the 5'UTR was identified but the frequency of deletion allele was similar in cases and controls. None of the seven polymorphisms in the promoter region altered the transcription-binding site and hence neither any existing transcription binding site was destroyed nor was a new site created. Other SNPs included two in the intronic region and one in the 3’ UTR region of reg1α gene. All ten polymorphisms had comparable allele frequencies in patients and controls and the difference was statistically not significant (Table 2). Allelic odds ratio and confidence interval did not indicate an association with any of the polymorphisms identified in reg1α with TCP (Table 2). Haplotype analysis using the six reg1α polymorphisms with greater than 3% minor allele frequency supported the observations made from the allelic and genotypic data at different polymorphisms (Table 5). The patient population was divided into FCPD and TCP patients based on the presence or absence of diabetes, but we failed to observe any association between FCPD and polymorphisms in reg1α gene (Table 3). We also dichotomized the patient population based on the presence or absence of N34S mutation in the SPINK1 gene and L26V mutation in the cathepsin B gene and compared the allele frequency of 6 SNPs in reg1α gene of patients having at least one mutant allele with those with the wild type pattern at the above mentioned mutations (Table 6), but could not detect any interaction between them and the reg1α variants.
Table 4.
Genotype data of polymorphisms analyzed in reg1α gene
| Polymorphism |
Patients (n = 195) |
Controls (n = 150) |
||||
| AA | Aa | aa | AA | Aa | aa | |
| G-974C1 | 49 | 1 | 0 | 48 | 2 | 0 |
| G-938A | 92 | 73 | 30 | 74 | 52 | 24 |
| T-912G | 53 | 93 | 49 | 42 | 65 | 43 |
| G-501A1 | 49 | 1 | 0 | 48 | 2 | 0 |
| T-385C | 98 | 76 | 21 | 80 | 52 | 18 |
| -331delGGA | 193 | 2 | 0 | 148 | 2 | 0 |
| T-243G | 92 | 73 | 30 | 69 | 58 | 23 |
| G209T | 125 | 61 | 9 | 103 | 43 | 4 |
| G2199A | 94 | 68 | 33 | 72 | 54 | 24 |
| G2370A1 | 49 | 1 | 0 | 47 | 3 | 0 |
AA: Homozygous for major allele; Aa: Heterozygous; aa: Homozygous for minor allele.
Data from 50 patients & 50 controls.
Table 5.
Haplotype frequencies of reg1α gene in patients with tropical calcific pancreatitis and healthy controls
| S. No. | Haplotype |
Haplotype frequency (%) |
OR (95% CI) | P value | |
| Patients (n = 195) | Controls (n = 150) | ||||
| 1 | G G T G G G | 43.1 | 43.3 | ~1 | ~1 |
| 2 | A T C T G A | 30.3 | 31.3 | 0.95 (0.5-1.82) | 0.88 |
| 3 | G T T G T G | 19.0 | 17.3 | 1.15 (0.52-2.5) | 0.33 |
| 4 | G G T T G G | 2.1 | 2.0 | ~1 | ~1 |
OR: Odds ratio; 95% CI: 95% confidence interval; Haplotypes generated using six SNPs with minor allele frequency of > 3%, haplotypes with frequency > 2% are presented; Order of SNPs; G-938A, T-912G, T-385C, T-243G, G209T, G2199A in the reference sequence.
Table 6.
Distribution of reg1α gene polymorphisms in tropical calcific pancreatitis patients based on N34S SPINK1 and L26V CTSB status
| SNP |
SPINK1 mutation |
CTSB mutation |
||||||
|
Minor allele frequency1 |
OR (95% CI) | P value |
Minor allele frequency2 |
OR (95% CI) | P value | |||
| N34S (n = 48) | WILD (n = 82) | L26V (n = 105) | WILD (n = 73) | |||||
| G-938A | 0.33 | 0.34 | 0.96 (0.51-1.79) | 0.88 | 0.34 | 0.31 | 1.15 (0.61-2.16) | 0.65 |
| T-912G | 0.49 | 0.45 | 1.17 (0.65-2.13) | 0.57 | 0.43 | 0.54 | 0.64 (0.35-1.17)) | 0.12 |
| T-385C | 0.31 | 0.33 | 0.91 (0.48-1.73) | 0.76 | 0.31 | 0.26 | 1.28 (0.66-2.48) | 0.43 |
| T-243G | 0.33 | 0.39 | 0.77 (0.41-1.43) | 0.38 | 0.34 | 0.31 | 1.15 (0.61-2.16) | 0.65 |
| G209T | 0.18 | 0.21 | 0.83 (0.39-1.76) | 0.59 | 0.23 | 0.19 | 1.27 (0.61-2.66) | 0.49 |
| G2199A | 0.34 | 0.35 | 0.96 (0.51-1.79) | 0.88 | 0.38 | 0.27 | 1.66 (0.87-3.15) | 0.10 |
SNP: Single nucleotide polymorphism; n: Number of individuals; OR: Odds ratio; CI: Confidence interval;
Minor allele frequency based on N34S SPINK1 status;
Allele frequency based on L26V CTSB status.
DISCUSSION
TCP is associated with the presence of large calculi throughout the main pancreatic duct[25,26]. However, the mechanism of stone formation is not completely understood[26]. A decrease in tissular pancreatic stone protein mRNA concentration is associated with CCP[27,28]. The role of Reg proteins is debatable but they are known to be associated with pancreatic islet regeneration, diabetogenesis and amelioration of surgical diabetes in animal models[18]. Its role in pancreatic stone formation is not clear with suggestions that lithostathine could promote the nucleation of calcite crystals or may prevent pancreatic lithiasis by inhibiting calcite crystal nucleation and growth in the pancreatic juice[29]. Thus, mutations in reg1α gene could play an important role in the pathogenesis of TCP and FCPD.
A previous study, analyzed the exons of reg1α gene using a combination of Restriction fragment length polymorphism (RFLP), Single strand conformation polymorphism (SSCP) and sequencing techniques in 50 FCPD patients and controls, but did not identify any nucleotide substitutions and ruled out any contribution of mutations in the coding regions of reg1α gene[30]. However, these workers did speculate about a possible role of regulatory variants in reg1α gene. A subsequent study also analyzed only the coding region in 12 Thai FCPD patients and 22 controls and ruled out any association with the disease[31]. T-385C, a polymorphism in exon 1 (5’UTR) with a moderately high allele frequency (0.32 in patients and 0.29 in controls) could have been missed in these studies due to the inherent limitations of techniques like SSCP in detecting any sequence changes. Our study involving extensive analysis of the gene as well as of the promoter region detected several polymorphisms including the promoter variants but the results suggest that there may not be any allelic or haplotypic association between the polymorphisms in reg1α and TCP.
As the reg1α gene is believed to be involved in islet cell repair and regeneration[18], we examined the association of reg1α variants with TCP and FCPD. The etiology and relationship of diabetes mellitus in FCPD are not well understood. Some believe that diabetes in FCPD is secondary to TCP while others suggest there is selective β-cell impairment, the latter hypothesis is supported by the occurrence of FCPD in some patients at a very young age. Evidence showing a preserved pancreatic α-cell function in diabetics with advanced chronic pancreatitis of the tropics indicates the presence of two different pathogenic mechanisms, one causing chronic pancreatitis and the other selective pancreatic β-cell impairment and subsequently diabetes mellitus[32]. However, an independent analysis of the TCP and FCPD patients did not suggest any role for reg1α variants in FCPD patients. Although, nearly one-half of the TCP patients carry N34S SPINK1 mutation and the mutations in SPINK1 and CTSB are the only genetic changes known to be associated with TCP, we did not find any evidence of an interaction between them. Although the present study had limited power to analyse such an interaction, our preliminary observations did not find a statistically significant difference in allele frequency between these groups for any polymorphism, suggesting the lack of epistatic interaction between SPINK1 and/or CTSB with reg1α gene.
In conclusion, polymorphisms in reg1α gene, including those in the regulatory region are unlikely to contribute to the pathogenesis of pancreaticolithogenesis in tropical calcific pancreatitis. Other genes such as those involved in calcium signaling and regulation, either interacting with reg genes or functioning independently may play a role in stone formation in tropical calcific pancreatitis.
ACKNOWLEDGMENTS
The authors express their gratitude to all the patients and normal volunteers for participating in the study and especially for giving informed consent for genetic studies. The help of Dr. Ramakrishna, Asian Institute of Gastroenterology in recruitment of patients and the collection of blood samples is gratefully acknowledged. The financial support of Council of Scientific and Industrial Research, Ministry of Science and Technology, Government of India is gratefully acknowledged.
COMMENTS
Background
Chronic pancreatitis (CP), an inflammatory condition of the pancreas with diverse etiologies, is usually associated with parenchymal calcification and presence of stones in the pancreatic duct. The process of stone formation in chronic pancreatitis is not completely understood. Lithostathine (encoded by reg1α gene), identified as a major proteic component of pancreatic stones in patients with alcoholic calcifying chronic pancreatitis, is thought to play an important role in the inhibition of stone formation and its levels are known to correlate with disease severity and is possibly regulated by the reg1α variants.
Research frontiers
Tropical calcific pancreatitis (TCP) and fibrocalculous pancreatic diabetes (FCPD; TCP presenting with diabetes) is a type of chronic pancreatitis specific to tropical countries. One of the important features of this condition is formation of large and irregular intraductal stones. Currently, there is considerable interest in understanding the mechanism of stone formation, the factors that inhibit stones, the genes involved in the process of pancreaticolithiasis as well as the effect of various polymorphisms. An additional area of interest is the relationship between the pancreatic inflammation and pancreaticolithiasis as well as the influence of genetic variants that predict susceptibility to the development of chronic pancreatitis.
Innovations and breakthroughs
The present study attempted to open new frontiers in the area of molecular pathogenesis of stone formation in TCP and FCPD by ruling out the role of reg1α variants in pancreaticolithiasis.
Applications
The results of the present study propose a new assessment of the pathogenesis of stone formation in TCP and FCPD. Further studies should be designed to elucidate more information.
Terminology
The process of stone formation, lithogenesis, is believed to be initiated by calcite nucleation with the subsequent deposition of proteins leading to protein plug formation; Lithostathine C is known to influence this process.
Peer review
The authors of this manuscript screened the reg1α gene including the regulatory region by sequencing and examining the association of the polymorphisms in the gene with pancreaticolithiasis in TCP and FCPD. The authors conclude that neither the previously reported nor novel variants in the reg1α gene predict the susceptibility to pancreaticolithiasis in TCP and FCPD.
Footnotes
Supported by the Council of Scientific and Industrial Research, Ministry of Science and Technology, Government of India
S- Editor Liu Y L- Editor Anand BS E- Editor Ma WH
References
- 1.Whitcomb DC, Gorry MC, Preston RA, Furey W, Sossenheimer MJ, Ulrich CD, Martin SP, Gates LK, Amann ST, Toskes PP, et al. Hereditary pancreatitis is caused by a mutation in the cationic trypsinogen gene. Nat Genet. 1996;14:141–145. doi: 10.1038/ng1096-141. [DOI] [PubMed] [Google Scholar]
- 2.Witt H, Luck W, Hennies HC, Classen M, Kage A, Lass U, Landt O, Becker M. Mutations in the gene encoding the serine protease inhibitor, Kazal type 1 are associated with chronic pancreatitis. Nat Genet. 2000;25:213–216. doi: 10.1038/76088. [DOI] [PubMed] [Google Scholar]
- 3.Sharer N, Schwarz M, Malone G, Howarth A, Painter J, Super M, Braganza J. Mutations of the cystic fibrosis gene in patients with chronic pancreatitis. N Engl J Med. 1998;339:645–652. doi: 10.1056/NEJM199809033391001. [DOI] [PubMed] [Google Scholar]
- 4.Pitchumoni CS. Familial pancreatitis. In: Pai KN, Suman CR, Varghese R, editors. Pancreatic diabetes. Geoprinters: Trivandrum; 1970. pp. 46–48. [Google Scholar]
- 5.Mohan V, Chari ST, Hitman GA, Suresh S, Madanagopalan N, Ramachandran A, Viswanathan M. Familial aggregation in tropical fibrocalculous pancreatic diabetes. Pancreas. 1989;4:690–693. doi: 10.1097/00006676-198912000-00006. [DOI] [PubMed] [Google Scholar]
- 6.Chandak GR, Idris MM, Reddy DN, Mani KR, Bhaskar S, Rao GV, Singh L. Absence of PRSS1 mutations and association of SPINK1 trypsin inhibitor mutations in hereditary and non-hereditary chronic pancreatitis. Gut. 2004;53:723–728. doi: 10.1136/gut.2003.026526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chandak GR, Idris MM, Reddy DN, Bhaskar S, Sriram PV, Singh L. Mutations in the pancreatic secretory trypsin inhibitor gene (PSTI/SPINK1) rather than the cationic trypsinogen gene (PRSS1) are significantly associated with tropical calcific pancreatitis. J Med Genet. 2002;39:347–351. doi: 10.1136/jmg.39.5.347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mahurkar S, Idris MM, Reddy DN, Bhaskar S, Rao GV, Thomas V, Singh L, Chandak GR. Association of cathepsin B gene polymorphisms with tropical calcific pancreatitis. Gut. 2006;55:1270–1275. doi: 10.1136/gut.2005.087403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.De Caro A, Lohse J, Sarles H. Characterization of a protein isolated from pancreatic calculi of men suffering from chronic calcifying pancreatitis. Biochem Biophys Res Commun. 1979;87:1176–1182. doi: 10.1016/s0006-291x(79)80031-5. [DOI] [PubMed] [Google Scholar]
- 10.Jin CX, Naruse S, Kitagawa M, Ishiguro H, Kondo T, Hayakawa S, Hayakawa T. Pancreatic stone protein of pancreatic calculi in chronic calcified pancreatitis in man. JOP. 2002;3:54–61. [PubMed] [Google Scholar]
- 11.Stewart TA. The human reg gene encodes pancreatic stone protein. Biochem J. 1989;260:622–623. doi: 10.1042/bj2600622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sanchez D, Figarella C, Marchand-Pinatel S, Bruneau N, Guy-Crotte O. Preferential expression of reg I beta gene in human adult pancreas. Biochem Biophys Res Commun. 2001;284:729–737. doi: 10.1006/bbrc.2001.5033. [DOI] [PubMed] [Google Scholar]
- 13.Carrère J, Guy-Crotte O, Gaia E, Figarella C. Immunoreactive pancreatic Reg protein in sera from cystic fibrosis patients with and without pancreatic insufficiency. Gut. 1999;44:545–551. doi: 10.1136/gut.44.4.545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.De Reggi M, Capon C, Gharib B, Wieruszeski JM, Michel R, Fournet B. The glycan moiety of human pancreatic lithostathine. Structure characterization and possible pathophysiological implications. Eur J Biochem. 1995;230:503–510. doi: 10.1111/j.1432-1033.1995.tb20589.x. [DOI] [PubMed] [Google Scholar]
- 15.Bernard JP, Adrich Z, Montalto G, De Caro A, De Reggi M, Sarles H, Dagorn JC. Inhibition of nucleation and crystal growth of calcium carbonate by human lithostathine. Gastroenterology. 1992;103:1277–1284. doi: 10.1016/0016-5085(92)91516-7. [DOI] [PubMed] [Google Scholar]
- 16.Sarles H, Dagorn JC, Giorgi D, Bernard JP. Renaming pancreatic stone protein as 'lithostathine'. Gastroenterology. 1990;99:900–901. doi: 10.1016/0016-5085(90)90999-h. [DOI] [PubMed] [Google Scholar]
- 17.Multigner L, De Caro A, Lombardo D, Campese D, Sarles H. Pancreatic stone protein, a phosphoprotein which inhibits calcium carbonate precipitation from human pancreatic juice. Biochem Biophys Res Commun. 1983;110:69–74. doi: 10.1016/0006-291x(83)91261-5. [DOI] [PubMed] [Google Scholar]
- 18.Watanabe T, Yonemura Y, Yonekura H, Suzuki Y, Miyashita H, Sugiyama K, Moriizumi S, Unno M, Tanaka O, Kondo H. Pancreatic beta-cell replication and amelioration of surgical diabetes by Reg protein. Proc Natl Acad Sci USA. 1994;91:3589–3592. doi: 10.1073/pnas.91.9.3589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.The Indian Genome Variation database (IGVdb): a project overview. Hum Genet. 2005;118:1–11. doi: 10.1007/s00439-005-0009-9. [DOI] [PubMed] [Google Scholar]
- 20.Miller SA, Dykes DD, Polesky HF. A simple salting out procedure for extracting DNA from human nucleated cells. Nucleic Acids Res. 1988;16:1215. doi: 10.1093/nar/16.3.1215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Watanabe T, Yonekura H, Terazono K, Yamamoto H, Okamoto H. Complete nucleotide sequence of human reg gene and its expression in normal and tumoral tissues. The reg protein, pancreatic stone protein, and pancreatic thread protein are one and the same product of the gene. J Biol Chem. 1990;265:7432–7439. [PubMed] [Google Scholar]
- 22.Matys V, Fricke E, Geffers R, Gössling E, Haubrock M, Hehl R, Hornischer K, Karas D, Kel AE, Kel-Margoulis OV, et al. TRANSFAC: transcriptional regulation, from patterns to profiles. Nucleic Acids Res. 2003;31:374–378. doi: 10.1093/nar/gkg108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schaid DJ, Rowland CM, Tines DE, Jacobson RM, Poland GA. Score tests for association between traits and haplotypes when linkage phase is ambiguous. Am J Hum Genet. 2002;70:425–434. doi: 10.1086/338688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Barrett JC, Fry B, Maller J, Daly MJ. Haploview: analysis and visualization of LD and haplotype maps. Bioinformatics. 2005;21:263–265. doi: 10.1093/bioinformatics/bth457. [DOI] [PubMed] [Google Scholar]
- 25.Balakrishnan V. Chronic calcific pancreatitis in the tropics. Indian J Gastroenterol. 1984;3:65–67. [PubMed] [Google Scholar]
- 26.Pitchumoni CS, Viswanathan KV, Gee Varghese PJ, Banks PA. Ultrastructure and elemental composition of human pancreatic calculi. Pancreas. 1987;2:152–158. doi: 10.1097/00006676-198703000-00005. [DOI] [PubMed] [Google Scholar]
- 27.Montalto G, Bonicel J, Multigner L, Rovery M, Sarles H, De Caro A. Partial amino acid sequence of human pancreatic stone protein, a novel pancreatic secretory protein. Biochem J. 1986;238:227–232. doi: 10.1042/bj2380227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Giorgi D, Bernard JP, Rouquier S, Iovanna J, Sarles H, Dagorn JC. Secretory pancreatic stone protein messenger RNA. Nucleotide sequence and expression in chronic calcifying pancreatitis. J Clin Invest. 1989;84:100–106. doi: 10.1172/JCI114128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sarles H, Bernard JP. Lithogenesis. Gastroenterol Int Ed. 1991;4:130–134. [Google Scholar]
- 30.Hawrami K, Mohan V, Bone A, Hitman GA. Analysis of islet regenerating (reg) gene polymorphisms in fibrocalculous pancreatic diabetes. Pancreas. 1997;14:122–125. doi: 10.1097/00006676-199703000-00003. [DOI] [PubMed] [Google Scholar]
- 31.Boonyasrisawat W, Pulsawat P, Yenchitsomanus PT, Vannasaeng S, Pramukkul P, Deerochanawong C, Sriussadaporn S, Ploybutr S, Pasurakul T, Banchuin N. Analysis of the reg1alpha and reg1beta gene transcripts in patients with fibrocalculous pancreatopathy. Southeast Asian J Trop Med Public Health. 2002;33:365–372. [PubMed] [Google Scholar]
- 32.Rossi L, Parvin S, Hassan Z, Hildebrand P, Keller U, Ali L, Beglinger C, Azad Khan AK, Whitcomb DC, Gyr N. Diabetes mellitus in Tropical Chronic Pancreatitis Is Not Just a Secondary Type of Diabetes. Pancreatology. 2004;4:461–467. doi: 10.1159/000079849. [DOI] [PubMed] [Google Scholar]