Abstract
This report describes a rare case of metastatic hepatocellular carcinoma (HCC) presenting a huge mass in the left external auditory canal (EAC). The patient was a 55-year-old man with hepatitis B virus-related HCC. He presented to our department with a three-month history of increasing left otalgia, and hearing loss with recent fresh aural bleeding. Histopathologic examination indicated that the tumor was secondary to HCC. Although external irradiation was not effective, the tumor was treated with surgical debulking and high dose rate 192 Ir remote afterloading system (RALS) for postoperative intracavitary irradiation. A review of the literature revealed only five other cases of HCC metastasis to the temporal bone, all of which mainly metastasized in the internal acoustic meatus. The present case is the first report of HCC metastasis to the EAC.
Keywords: Hepatocellular carcinoma, Metastasis, External auditory canal
INTRODUCTION
Hepatocellular carcinoma (HCC) is a very highly invasive tumor that metastasizes hematogenously and lymphogenously to distant sites. Most frequently affected sites are the lungs, regional lymph nodes, bones, and adrenal glands[1]. However, external auditory canal (EAC) metastases from HCC are extremely rare. A review of the literature revealed only five other cases of HCC metastasis to the temporal bone, all of which mainly metastasized in the internal acoustic meatus[2-4]. To the best of our knowledge, the present patient is the first case of HCC metastasis to the EAC.
We report here a rare case of bleeding due to EAC metastasis from HCC. The patient was treated with surgical debulking and high dose rate 192Ir remote afterloading system (RALS) for postoperative intracavitary irradiation.
CASE REPORT
A 55-year-old man presented to our department with a three-month history of increasing left otalgia, and hearing loss with recent fresh aural bleeding, in April 2006. He denied any vertigo, and had no evidence of facial palsy. His past medical history revealed that hepatitis B virus-related HCC was diagnosed two years ago. Owing to the tumor’s inoperability and the presence of lung metastases, the patient began systemic chemotherapy with 5-fluorouracil and cisplatin, which was maintained for two years.
Physical examination did not find the left tympanic membrane, because the EAC was completely occupied by a tumor. Right-sided otoscopy was normal. Vestibular examination was unremarkable. There was no lymphade-nopathy, and the remainder of the head and neck and neurologic examinations was unremarkable.
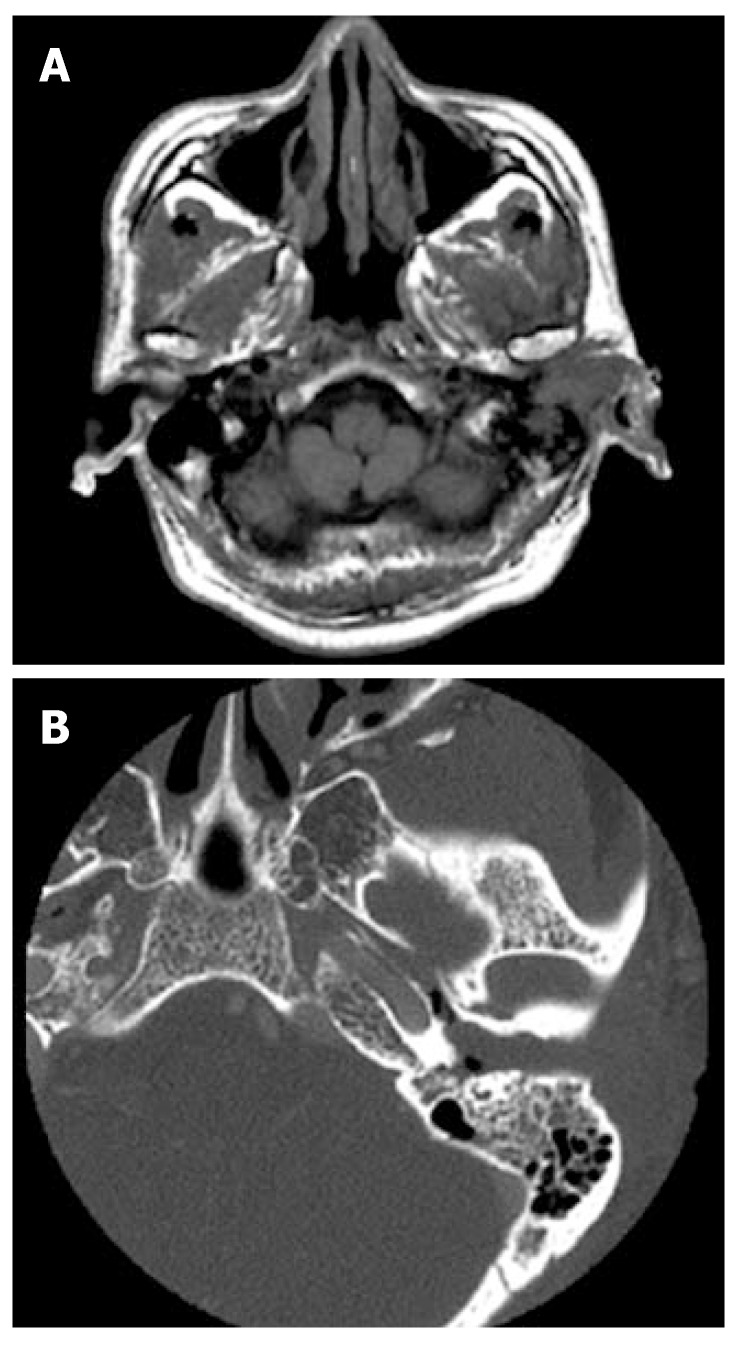
Magnetic resonance imaging showed a well-enhanced tumor lesion within the left EAC. T1- and T2- weighted images revealed that the EAC lesion exhibited a mixture of hypointensity and hyperintensity (Figure 1A). CT imaging showed tumor formation on the posterior wall of the EAC, and a shallow bony erosion (Figure 1B).
Figure 1.
Axial T1-weighted magnetic resonance image of the head showing a huge mass in the left EAC with extension of the lesion into the mastoid (A), and axial CT of the temporal bone demonstrating the mass occupying the left EAC (B).
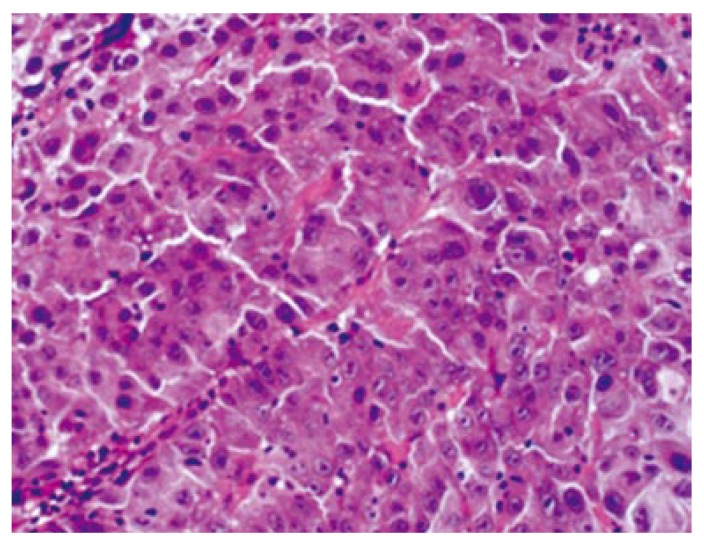
A biopsy was performed, and pathologic examination taken through the EAC suggested metastasis of HCC with histopathologic features similar to the primary lesion (Figure 2). The biopsy of the mass produced much bleeding, which was stopped with local pressure.
Figure 2.
Microscopically, the lesion in the external auditory canal is composed of proliferating atypical epithelial cells forming a solid and thick trabecular arrangement with necrosis, and a fibrous stroma (hematoxylin/eosin stain, x 400).
First, the patient received external irradiation (total dose, 30 Gy) to treat the EAC lesion. Despite the external irradiation therapy, the tumor increased in size, and was continuously bleeding. Therefore, it was decided to change the treatment from external irradiation to surgical debulking and 192Ir RALS. We planned to proceed with the debulking surgery for the progressive disease followed by transcatheter arterial embolization by means of superselective catherization.
Angiography was performed to delineate blood supply to the mass, and to embolize any feeding vessels. The external carotid artery was cannulated via the femoral artery, using the Seldinger technique. Evidence of vascular blush in the region of the left EAC was observed, and the posterior auricular artery was identified for embolization (Figure 3).
Figure 3.
Angiography showing hypervascula-rity in the left external auditory canal supplied by the posterior auricular artery (the arrow indica-tes the tumor stain).
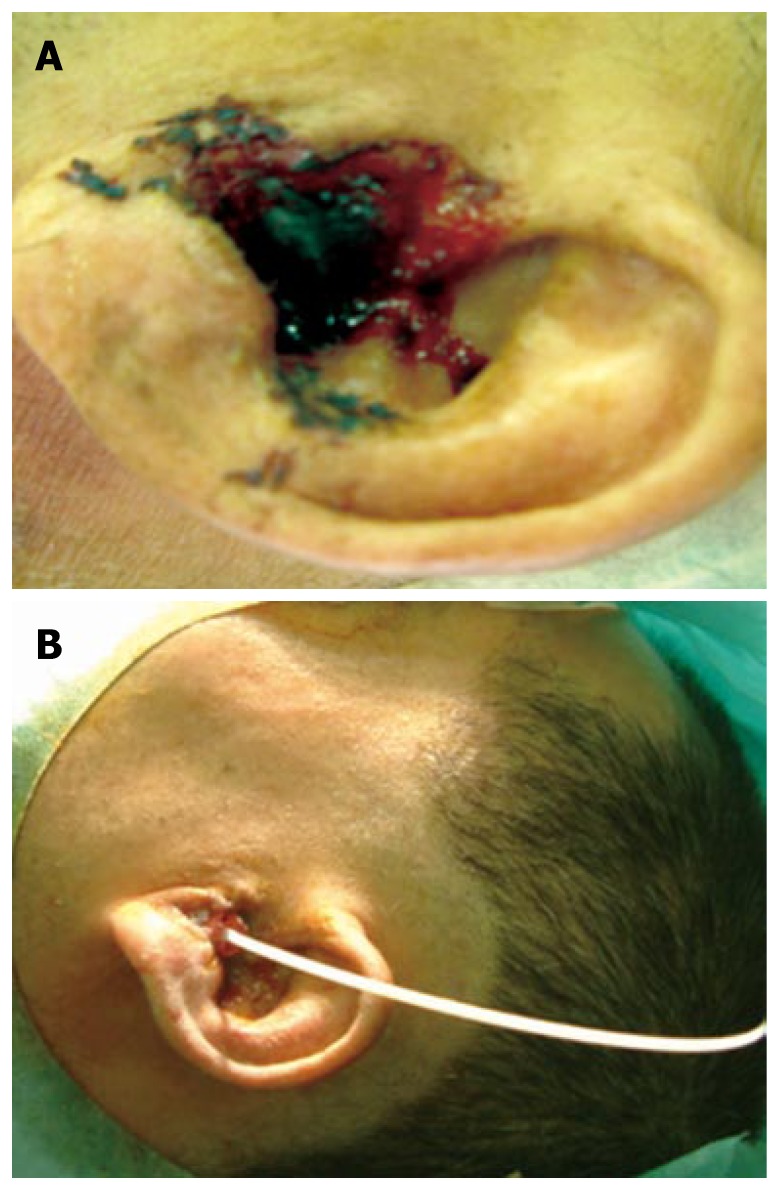
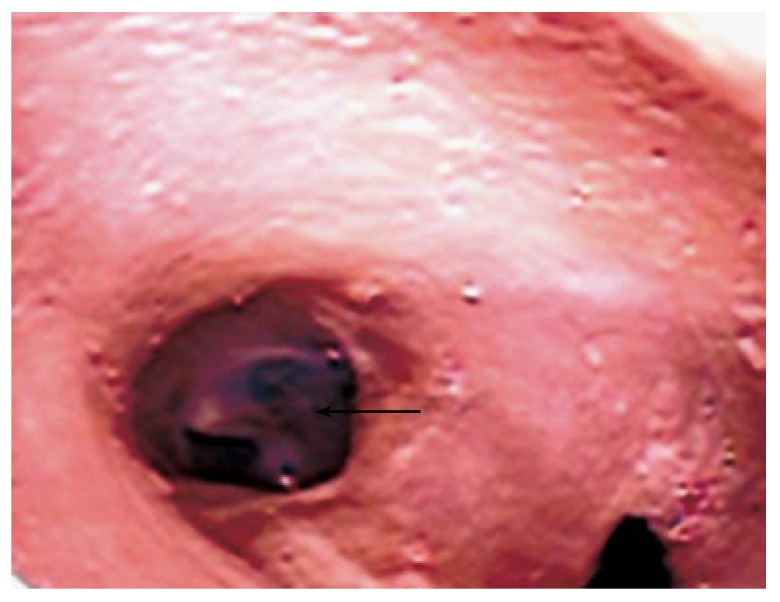
Following angiography, surgical debulking was performed under general anesthesia and a 6-Fr catheter for the 192Ir remote afterloader system was inserted into the left EAC (Figure 4A and B). A total dose of 15 Gy (10 Gy/Fr/wk) was given over a one-week period. When the irradiation treatment was completed in May 2006, otoscopy revealed tumor remission. Neither radiation-induced dermatitis nor otitis media with effusion was observed. Although the patient remained clinically free of disease in his left EAC (Figure 5), he died of progressive liver failure and lung metastases from HCC 9 mo after the treatment.
Figure 4.
Metastatic hepatocellular carcinoma protruding from the left external auditory canal (A) and inserted and fixed catheter for the 192Ir remote afterloader system in the left external auditory canal after debulking surgery (B).
Figure 5.
Fiberscopy of the external auditory canal 6 mo after treatment showing no evidence of residual tumor (the arrow indicates the left tympanic membrane).
DISCUSSION
HCC is the most common malignant tumor of the liver. Intrahepatic metastases occur early in the disease, and more than half of these tumors metastasize to extrahepatic sites[5]. Autopsy and surgical series have suggested the presence of metastases from HCC in the lungs (18.1%-49.2%), lymph nodes (26.5%-41.7%), bones (4.2%-16.3%), and adrenal glands (8.4%-15.4%)[6-8]. However, reports on metastases from distant primary malignancies to different sites in the ear including EAC, are uncommon. The temporal bones are among the more common sites of the ear to develop metastases from distant malignancies[9]. Gloria-Cruz et al[4] reviewed the autopsy records of 864 cases, and reported that 47 of 212 patients (22%) with primary non-disseminated neoplasms had metastatic diseases involving the temporal bones. The primary site of the majority of metastases to the temporal bones is the breast (21%), followed by the lungs (12%), kidneys, and prostate, and only three patients (6%) showed histologic features consistent with HCC[4]. No other study has reported HCC metastasis to the EAC. To the best of our knowledge, the present patient is the first case of HCC metastasis to the EAC.
To treat metastatic tumors including HCC of the EAC, curative surgical resection is sometimes impossible, radiation therapy and chemotherapy can be considered as palliative therapies. Although external irradiation was performed in the present case, it was not effective, and the tumor was continuously bleeding. Therefore, we attempted surgical debulking and 192Ir RALS as postoperative irradiation. As a result, fiberscopy after treatment confirmed the effectiveness and safety of this combined procedure. In general, side effects of conventional external irradiation to the auditory canal include many complications such as external canal stenosis, otitis media with effusion, cholesteatoma, sensorineural hearing loss, vestibular impairment, facial nerve paralysis, and osteoradionecrosis. However, none of these complications was observed in this case.
192Ir RALS is the best choice of treatment to ensure decreased doses to other important organs such as the tympanic membrane, temporal bone, and carotid artery while providing a curable dose to a target volume in EAC tumors[10]. In addition, this treatment can be performed in a short period, without any invasive procedure, and may become a choice of modality for its efficacy and less severe side effects.
In conclusion, a rare patient with EAC metastasis from HCC can be treated with surgical debulking and high dose rate 192Ir RALS for postoperative intracavitary irradiation. This combined treatment can be used as a palliative modality for such patients.
Footnotes
S- Editor Liu Y L- Editor Wang XL E- Editor Ma WH
References
- 1.Kim HS, Shin JW, Kim GY, Kim YM, Cha HJ, Jeong YK, Jeong ID, Bang SJ, Kim do H, Park NH. Metastasis of hepatocellular carcinoma to the small bowel manifested by intussusception. World J Gastroenterol. 2006;12:1969–1971. doi: 10.3748/wjg.v12.i12.1969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nagai M, Yamada H, Kitamoto M, Ikeda J, Mori Y, Monzen Y, Fukuhara T. Facial nerve palsy due to temporal bone metastasis from hepatocellular carcinoma. J Gastroenterol Hepatol. 2005;20:1131–1132. doi: 10.1111/j.1440-1746.2005.03911.x. [DOI] [PubMed] [Google Scholar]
- 3.Brown NE, O'Brien DA, Megerian CA. Metastatic hepatocellular carcinoma to the temporal bone in a post-liver transplant patient. Otolaryngol Head Neck Surg. 2004;130:370–371. doi: 10.1016/j.otohns.2003.08.020. [DOI] [PubMed] [Google Scholar]
- 4.Gloria-Cruz TI, Schachern PA, Paparella MM, Adams GL, Fulton SE. Metastases to temporal bones from primary nonsystemic malignant neoplasms. Arch Otolaryngol Head Neck Surg. 2000;126:209–214. doi: 10.1001/archotol.126.2.209. [DOI] [PubMed] [Google Scholar]
- 5.Okada H, Kamino Y, Shimo M, Kitamura E, Katoh T, Nishimura H, Akimoto Y, Kaneda T, Hinata M, Yamamoto H. Metastatic hepatocellular carcinoma of the maxillary sinus: a rare autopsy case without lung metastasis and a review. Int J Oral Maxillofac Surg. 2003;32:97–100. doi: 10.1054/ijom.2002.0242. [DOI] [PubMed] [Google Scholar]
- 6.Kaczynski J, Hansson G, Wallerstedt S. Metastases in cases with hepatocellular carcinoma in relation to clinicopathologic features of the tumor. An autopsy study from a low endemic area. Acta Oncol. 1995;34:43–48. doi: 10.3109/02841869509093637. [DOI] [PubMed] [Google Scholar]
- 7.Yuki K, Hirohashi S, Sakamoto M, Kanai T, Shimosato Y. Growth and spread of hepatocellular carcinoma. A review of 240 consecutive autopsy cases. Cancer. 1990;66:2174–2179. doi: 10.1002/1097-0142(19901115)66:10<2174::aid-cncr2820661022>3.0.co;2-a. [DOI] [PubMed] [Google Scholar]
- 8.Ho J, Wu PC, Kung TM. An autopsy study of hepatocellular carcinoma in Hong Kong. Pathology. 1981;13:409–416. doi: 10.3109/00313028109059059. [DOI] [PubMed] [Google Scholar]
- 9.Hill BA, Kohut RI. Metastatic adenocarcinoma of the temporal bone. Arch Otolaryngol. 1976;102:568–571. doi: 10.1001/archotol.1976.00780140100015. [DOI] [PubMed] [Google Scholar]
- 10.Uchida N, Kuroda S, Kushima T, Moriyama M, Sugimura K, Kawauchi H, Shirakawa R. Squamous cell carcinoma of the external auditory canal: two cases treated with high dose rate 192Ir remote afterloading system (RALS) Radiat Med. 1999;17:443–446. [PubMed] [Google Scholar]