Abstract
OBJECTIVES
To determine whether elderly people with different patterns of MRI findings have different long-term outcomes.
DESIGN
longitudinal cohort study.
SETTING
the Cardiovascular Health Study.
PARTICIPANTS
5,888 people over age 65 were recruited; 3,660 underwent MRI; and 3,230 without a stroke prior to the scan were included in these analyses.
MEASUREMENTS
Cluster analysis of brain MRI findings was previously used to define five clusters: Normal, Atrophy, Simple Infract, Leukoaraiosis, and Complex Infarct. Participates were subsequently classified as "healthy" if they rated their health as excellent, very good or good and as "able" if they did not report any limitations in activities of daily living (ADLs). Mean years of life (YoL), years of healthy life (YHL) and years of able life (YAL) were calculated over 16 years following the MRI and compared across clusters, using unadjusted and adjusted regression analyses.
RESULTS
Mean age of participants was 75.0 years. With 16 years of follow-up, mean YoL was 11.3 years; YHL, 8.0; and YAL, 8.4.Outcomes differed significantly across clusters. With or without adjustments, outcomes were all significantly better in the Normal than Complex Infarct cluster. The three remaining clusters had intermediate results, significantly different from the Normal and Complex Infarct clusters but not usually from one another. Over 16 years of follow-up, participants in the Complex Infarct cluster (n=368) spent the largest percentage of their 8.4 years alive being sick (38%) and not able (38%).
CONCLUSION
Findings on MRI scans in the elderly are associated not only with long-term survival but also with long-term self-rated health and limitation in ADLs. The combination of infarcts and leukoaraiosis carried the worst prognosis, presumably reflecting small vessel disease.
Keywords: magnetic resonance imaging, cohort study, prognosis, and outcome assessment
INTRODUCTION
In the Cardiovascular Health Study (CHS) -- a community-based, longitudinal study of the elderly -- cluster analysis was used to characterize patterns of findings on cranial magnetic resonance imaging (MRI) and to define five clusters: Normal, Atrophy, Simple Infarct, Leukoaraiosis, and Complex Infarct. 1Compared to the other clusters, the Complex Infarct cluster had the highest burden of disease combining both infarcts and leukoaraiosis. The frequency of vascular events about five years after the MRI scans was examined and found to be elevated with certain clusters compared to others, but especially with the Complex Infarct cluster.2 Although associations of the MRI findings, including the five clusters,1 with measures of health and activity in CHS have been examined in cross-sectional analyses, longitudinal analyses of these measures have not been examined. Besides the occurrence of vascular events and death, years of self-rated healthy life and self-rated active or able life expectancy have been used in analyses of other exposures such as obesity3 and physical activity.4 With now over two decade of follow-up, including 16 years since the MRI scan, the goal of the current work was to examine the associations of these different MRI-defined clusters with years of life (YoL), years of healthy life (YHL), and years of able life (YAL) without any limitations in activities of daily living (ADLs).3,4 We already knew from the original cluster analysis that participants differed significantly across the clusters on many variables,1 so the goal of this work was not to explore mechanisms for associations but to describe these outcomes. We hypothesize that the longitudinal measures of healthy life and able life would differ across the five clusters, being most preserved in those with the Normal cluster and least preserved in those with the Complex Infarct cluster.
METHODS
In brief, the CHS is a community-based longitudinal study of risk factors for vascular disease in 5,888 participants aged 65 and older at baseline.5,6 Participants were recruited from a random sample of Medicare eligible persons in four U.S. communities. The original cohort of 5,201 participants was recruited in1989 and 1990, and a second cohort of 687 African Americans was recruited in 1992 and 1993 from three of the original study communities. Extensive data were collected during annual clinic visits and telephone calls.
Of the 5,888 original participants, 3660 (62%) underwent MRI between 1991 and 1994. An adjudication committee comprised of neurologists and a neuroradiologist evaluated all suspected vascular events and used all available information to decide whether or not the participant had experienced a transient ischemic attack or stroke. Those who experienced such events before the MRI were excluded from the cluster analysis. After excluding participants with transient ischemic attacks, strokes, or missing values for MRI findings, 3230 participants remained for cluster analyses.1 This statistical technique seeks to identify among a set of variables patterns or clusters that are data, not hypothesis, driven. Based upon the MRI findings of infarcts and the 10-point grades of white matter hyperintensities, sulcal size, and ventricular size, five distinctive clusters were defined (see figure in reference 1): Normal, Atrophy, Simple Infarct, Leukoaraiosis, and Complex Infarct. The Normal cluster and Atrophy cluster lacked infarcts and high white matter grade but differed on sulcal and ventricular grades. The Simple Infarct cluster had infarcts but lacked a high white matter grade; the Leukoaraiosis cluster had a high white matter grade but lacked infarcts; and the Complex Infarct cluster had both infarcts and a high white matter grade. These MRI findings were considered subclinical or covert since participants with symptoms of transient ischemic attack or stroke had been excluded.
With exceptions as detailed in the online Appendix, data were collected every six months on mortality, self-rated health (excellent, very good, good, fair, and poor)7,8 and self-rated limitations in ADLs (difficulty walking around at home, getting out of bed or a chair, dressing, eating, bathing or showering, or using the toilet). Data were also collected on participants' demographic information and history of hypertension around the time of the MRI scan. Hypertension was defined as systolic blood pressure 140 mm Hg or greater, diastolic blood pressure 90 mm Hg or greater, or history of hypertension with the participant on treatment.
Longitudinal, dichotomized outcomes were determined semiannually and included: alive versus dead, healthy versus sick, and able versus not able. "Healthy" was assigned to those who rated their health as excellent, very good, or good, while "sick", to those who rated their health as fair or poor. "Able" was assigned to those without any limitations in ADLs, while "not able, "to those with at least one limitation. At follow-up, each living CHS participant was classified for each of the five clusters into one of two health states: healthy or sick for YHL and able or not able for YAL. Because participants were followed over time, a third state was added for death. Thus three states were possible each half-year or semester for each cluster.
With the MRI scans having been done from 1991 to 1994, follow-up varied. We picked a common maximum number of 16 years of follow-up, so that number was the same for each participant regardless of the year in which the scan was done. Details of the imputation of missing data and the calculation of YoL, YHL, and YAL are given in the online Appendix. We compared the means across clusters using analysis of variance. We used multiple regression analyses to predict YoL, YHL, and YAL as a function of the five clusters, controlling for age, log age, sex, an age-by-sex interaction term, and race. In some analyses, we also adjusted for the participant's status around the time of the MRI scan with respect to being healthy, able and hypertensive. In all of these analyses, the cluster variable was represented by four dummy variables with the Normal cluster serving as the reference category. As a consequence, the coefficient for a dummy variable represented the years of the outcome for the particular cluster minus the years for the Normal cluster.
We also calculated an adjusted outcome measure for each person. For example, adjusted YoL were the participant's observed YoL minus expected YoL from the regression controlling for age, sex, and race plus the average YoL in the entire sample. These outcome measures were used to provide graphic illustrations of the adjusted means by cluster.
We first plotted the number of YHL, years of sick life (YSL),YAL, years of not-able life (YNAL), and years dead by cluster type. We next examined the relationship of the dependent and independent variables with cluster type. We regressed YoL, YHL, and YAL on the independent variables to determine whether the five MRI-defined clusters were significantly different after controlling for the independent variables. Finally, we graphed the adjusted means years by the five clusters.
RESULTS
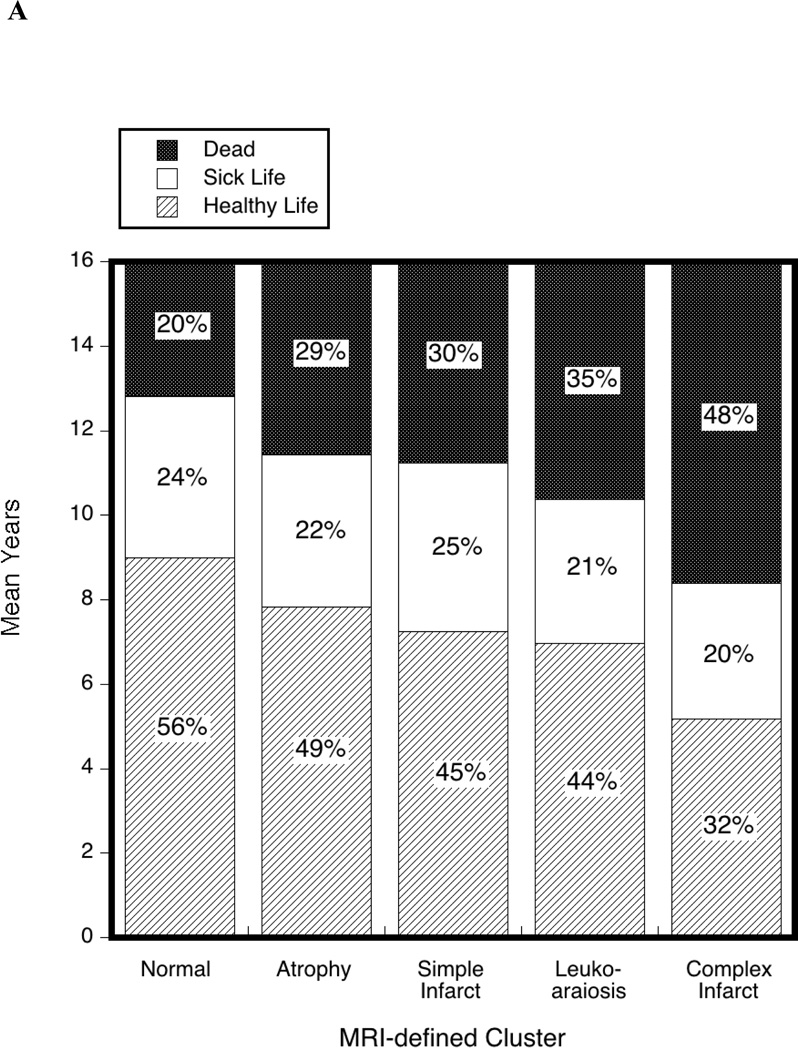
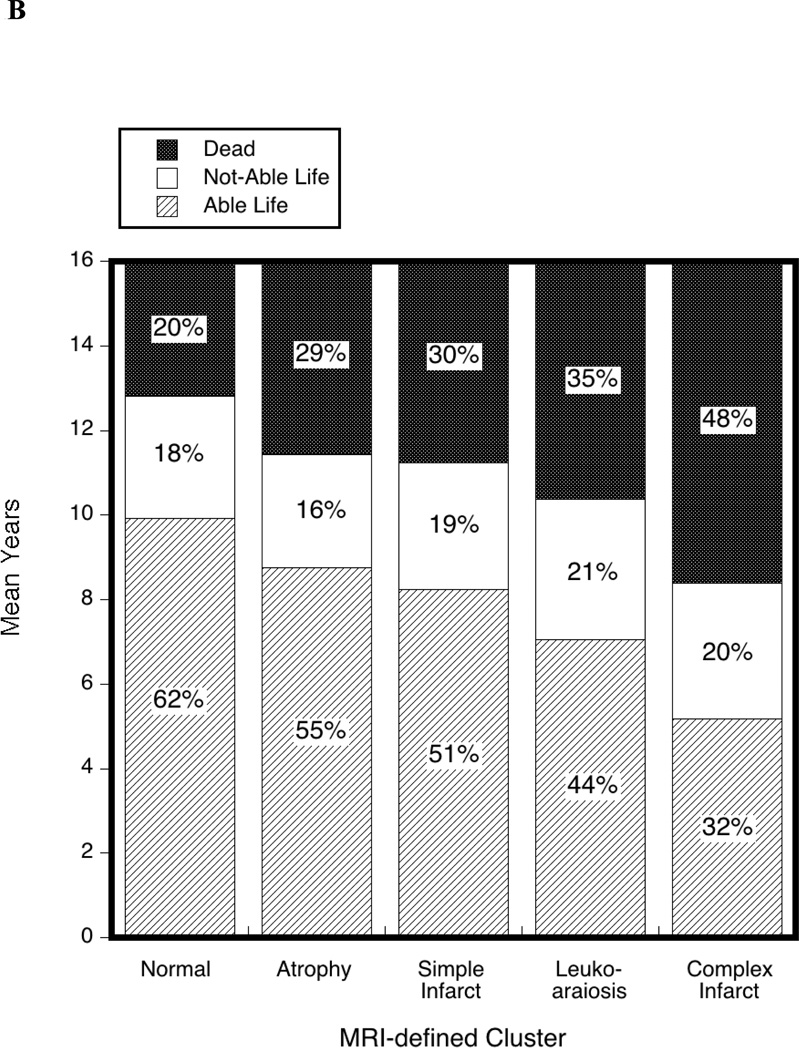
Figure 1A illustrates the unadjusted YHL, YSL, and years dead by the five clusters, and Figure 1B does the same for YAL, YNAL, and years dead. In both figures, the top section is the same and represents the average years lost to death, which increase going from the Normal cluster to the Complex Infarct cluster. A reverse pattern is seen with the bottom section, representing YHL and YAL, which decrease going from the Normal cluster to the Complex Infarct cluster. The bars for YSL and YNAL were similar across the five clusters being slightly larger in the Simple Infarct cluster for YSL and in Leukoaraiosis cluster for YNAL.
Figure 1. Distribution of healthy years (A)and able years (B) by the five MRI clusters.
Distribution of healthy years (A) and able years (B)in the 16 years following the MRI scan used to define the five clusters. Parts of columns representing years of healthy life (YHL) and years of able life (YAL) are lightly stripped; years of sick life (YSL) and years of not-able life (YNAL) are white; and years dead are darkly stippled. Percentages for each cluster total 100.
For each of the five MRI-defined clusters, the unadjusted means of YoL, YAL, and YHL used to create Figures 1A and B are presented in the first part of Table 1, and demographics, in the second part. As reported previously, the most common cluster was Normal (N=981), and the least common cluster was Complex Infarct (N=368).1 As illustrated in Figures 1A and B, the mean YoL, YHL, and YAL were highest in the Normal cluster and lowest in the complex cluster. Although the differences across the clusters for YSL and YNAL were significant, likely reflecting the large number of participants included in these analyses, the associations were not nearly as strong as for YoL, YHL, and YAL as reflected in the F-statistic in the analysis of variance (Table 1). Interestingly, YSL was smallest for the Complex Infarct cluster in absolute terms, suggesting that some of the YoL gained by the other clusters were spent sick rather than healthy. Nonetheless, in relative terms, those in the Complex Infarct cluster spent the largest percentage of their 8.4 years alive being sick (38%) and not able (38%). For contrast, those in the Normal cluster spent the smallest percentage of their 12.8 years alive being sick (30%) and not able (23%).
Table 1.
Outcomes and Demographics by the Five Magnetic Resonance Imaging-defined Clusters.1
| Clusters defined by cluster analysis of MRI findings |
||||||||
|---|---|---|---|---|---|---|---|---|
| In 16 years after MRI scan | Normal | Atrophy | Simple Infarct |
Leuko- araiosis |
Complex Infarct |
Total | Analysis of Variance |
|
| N=981 | N=891 | N=530 | N=460 | N=368 | N=3230 | F | p-value | |
| Years of Life | 12.8 | 11.4 | 11.2 | 10.4 | 8.4 | 11.3 | 71.5 | <0.0005 |
| Years Dead | 3.2 | 4.6 | 4.8 | 5.6 | 7.6 | 4.7 | 68.1 | <0.0005 |
| Years of Healthy Life | 9.0 | 7.8 | 7.2 | 7.0 | 5.2 | 8.0 | 47.5 | <0.0005 |
| Years of Sick Life | 3.8 | 3.6 | 4.0 | 3.4 | 3.2 | 3.7 | 4.2 | 0.002 |
| Years of Able Life | 9.9 | 8.8 | 8.2 | 7.1 | 5.2 | 8.4 | 68.0 | <0.0005 |
| Years of Not-able Life | 2.9 | 2.7 | 3.0 | 3.3 | 3.2 | 2.9 | 4.5 | 0.001 |
| Around time of MRI scan | ||||||||
| Age (y) | 73.0 | 75.3 | 74.6 | 76.4 | 78.1 | 75.0 | 94.9 | <0.0005 |
| Men (%) | 31 | 52 | 36 | 37 | 47 | 40 | 26.0 | <0.0005 |
| White (%) | 81 | 88 | 83 | 85 | 85 | 84 | 4.4 | 0.002 |
| Healthy (%) | 83 | 84 | 84 | 80 | 76 | 82 | 4.5 | 0.001 |
| Able (%) | 90 | 91 | 89 | 87 | 86 | 89 | 3.2 | 0.012 |
| Hypertension history (%) | 51 | 53 | 61 | 61 | 66 | 56 | 9.4 | <0.0005 |
MRI means magnetic resonance imaging; Healthy, self-reported health as excellent, very good or good; and Able, without any limitations with activities of daily living.
The YoL, YHL, and YAL varied monotonically across the clusters. Such was also the case for some demographics, such as age, but not for others, such as sex. For example, women were more common than men in the Normal cluster, while the opposite was true for the Atrophy cluster. All of the variables listed in Table 1 were significantly different across the five clusters, suggesting that these covariates should be controlled when comparing clusters.
Table 2 shows the results of the regression analyses for the three outcomes -- YoL, YHL, and YAL -- without any adjustments in Model 1, with adjustment for demographics in Model 2, and with additional adjustment for the participant's status around the time of the MRI scan with respect to being healthy, able and hypertensive in Model 3. The cells contain the regression coefficients (B), their standard errors (SE), and their significance level. The regression coefficients can be interpreted as the difference in years between the Normal cluster and the other clusters of interest controlling for the other variables in the regression. Thus in Model 1, compared to the Normal cluster, the Atrophy cluster has 1.40 fewer years of life (SE=0.21, p<0.005), 1.16 fewer years of healthy life (SE=0.22, p<0.005), and 1.18 fewer years of able life (SE=0.23, p<0.005).The coefficients diminish in size as more covariates are controlled for but are always significantly different from zero. Specifically, the largest changes in the coefficients occurred when age, sex, and race were added, namely results for Model 1 differed from Model 2. The coefficients were not very sensitive to a participant's status around the time of the MRI scan with respect to being healthy, able and hypertensive, namely results for Model 2 were similar to Model 3.The Normal cluster has significantly higher years than the other clusters, with one exception; the Normal and Atrophy clusters were not significantly different on YAL in Model 2. In general, in Models 2 and 3, the differences between the Normal and Atrophy cluster were less dramatic than for the other clusters.
Table 2.
Adjusted regression coefficients (B) for differences in years between the Normal and four other clusters.
| Years of Life (YoL) | Years of Healthy Life (YHL) | Year of Able Life (YAL) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| B | SE | p-value | B | SE | p-value | B | SE | p-value | |
| Model 1 | |||||||||
| Normal | 0 | -- | -- | 0 | -- | -- | 0 | -- | -- |
| Atrophy | −1.40 | 0.21 | <0.005 | −1.16 | 0.22 | <0.005 | −1.18 | 0.23 | <0.005 |
| Simple | −1.58 | 0.25 | <0.005 | −1.75 | 0.26 | <0.005 | −1.69 | 0.27 | <0.005 |
| Leuko | −2.45 | 0.26 | <0.005 | −2.03 | 0.27 | <0.005 | −2.87 | 0.28 | <0.005 |
| Complex | −4.43 | 0.28 | <0.005 | −3.82 | 0.29 | <0.005 | −4.76 | 0.30 | <0.005 |
| Model 2 | |||||||||
| Normal | 0 | -- | -- | 0 | -- | -- | 0 | -- | -- |
| Atrophy | −0.44 | 0.21 | 0.03 | −0.58 | 0.22 | 0.01 | −0.36 | 0.22 | 0.10 |
| Simple | −1.02 | 0.23 | <0.005 | −1.31 | 0.25 | <0.005 | −1.08 | 0.25 | <0.005 |
| Leuko | −1.33 | 0.25 | <0.005 | −1.18 | 0.27 | <0.005 | −1.62 | 0.27 | <0.005 |
| Complex | −2.63 | 0.28 | <0.005 | −2.49 | 0.30 | <0.005 | −2.89 | 0.30 | <0.005 |
| Model 3 | |||||||||
| Normal | 0 | -- | -- | 0 | -- | -- | 0 | -- | -- |
| Atrophy | −0.46 | 0.20 | 0.02 | −0.62 | 0.20 | <0.005 | −0.41 | 0.21 | 0.04 |
| Simple | −1.00 | 0.23 | <0.005 | −1.32 | 0.22 | <0.005 | −1.05 | 0.23 | <0.005 |
| Leuko | −1.22 | 0.25 | <0.005 | −0.98 | 0.24 | <0.005 | −1.43 | 0.25 | <0.005 |
| Complex | −2.44 | 0.27 | <0.005 | −2.12 | 0.27 | <0.005 | −2.61 | 0.28 | <0.005 |
Five MRI-defined clusters: Normal, Atrophy, Simple Infarct, Leukoaraiosis, Complex Infarct.1
B is the regression coefficient representing differences of years for a particular cluster minus years for the Normal, which was the reference category. SE is the standard error for the regression coefficient.
Model 1 was without adjustments.
Model 2 was adjusted for age, sex, and race.
Model 3 was additional adjusted for the participant's status around the time of the MRI scan with respect to being healthy, able and hypertensive.
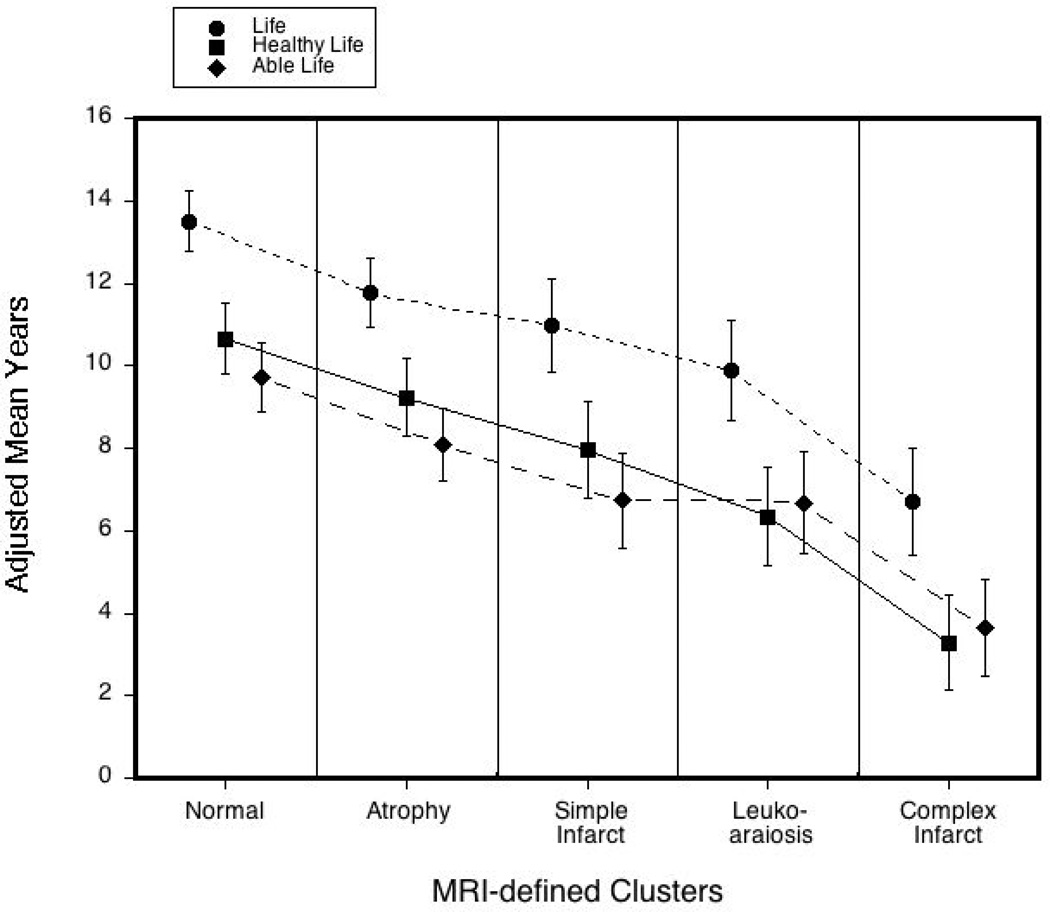
Figure 2 illustrates the adjusted mean years of life, healthy life, and able life when age, sex and race are held the same for each of the five clusters. The bars indicate the 99.5% confidence intervals, which are used to account for the multiple comparisons by the Bonferroni method. Bars that do not overlap approximate significantly different adjusted means. The bars for the Normal and Complex Infarct clusters do not overlap, indicating that the adjusted means were significantly different from each other as well as from the three other clusters. The three intermediate clusters -- Atrophy, Simple Infarct, and Leukoaraiosis -- were mostly not significantly different from one another after controlling for age, sex, and race. As with the unadjusted data in Figure 1, compared to participants in any of the other clusters, those in the Complex Infarct cluster spent the largest percentage of their 6.7 years alive being sick (51%) and not able (45%). For contrast, those in the Normal cluster spent the smallest percentage of their 13.5 years alive being sick (21%) and not able (28%).
Figure 2. Adjusted years of life, healthy life, and able life.
Adjusted years of life (YoL), healthy life (YHL), and able life (YAL).Bars indicate99.5% confidence intervals to account for the multiple comparisons by the Bonferroni method, when age, sex and race are held the same for each of the five clusters. The short-dashed line is for YoL, the solid line is for YHL, and the long-dashed line is for YAL.
DISCUSSION
In this large, well characterized cohort of elderly people with a mean age of 75 years old without a history of transient ischemic attack or stroke, findings on MRI scans were associated over the subsequent 16 years of follow-up not only with mortality but with self-rated health status and ADLs in those who survived. Outcomes differed across the five previously defined clusters,1 always being best in the Normal cluster and worst in the Complex Infarct cluster, which combined both infarcts and high white matter grade. Outcomes for the three other clusters -- Atrophy, Leukoaraiosis, and Simple Infarct -- differed significantly from the Normal and Complex Infarct clusters but did not differ as much amongst themselves. Years lost to death differed across clusters more than years lost to sickness or to not being able to perform ADLs. Adjustment for demographics weakened associations somewhat, but adjustment for status around the time of the MRI scan with respect to being healthy, able and hypertensive did not make a substantive change in the results.
Importantly, this work does not explain the mechanism by which the MRI findings could have affected health status. In mostly cross-sectional studies, imaging-defined infarcts and leukoaraiosis have been associated with neurologic dysfunction and vascular events that could be disabling and life threatening.1,2,9,10 In the current work, other variables not considered in the multivariable models could have either confounded or mediated the associations, including cognition and depression, although the small changes that occurred in model 3 suggest that the changes due to additional covariates would not be large. So these MRI findings in the elderly may be markers for subsequent health status, but the associations may not necessarily be mediated through the vascular brain injury suggested by these MRI findings of infarcts and leukoaraiosis.9,10
In addition, the MRI findings at baseline may not be static over time. In the CHS, MRI scans were repeated about five years after the initial scans. In one study, participants whose initial MRI showed infarcts were excluded, and predictors were sought for developing an incident infarct on the follow-up MRI.11 One of the strongest predictors was the white matter grade on the initial scan. These findings suggest that the Leukoaraiosis cluster evolves over time to become the Complex Infarct cluster. A follow-up study concerning worsening of white matter grade suggests a similar evolution of the Simple Infarct cluster to the Complex Infarct cluster over time.12 The Complex Infarct cluster was associated with the worst prognosis. In the fully adjusted model, participants in the Complex Infarct cluster at baseline lost 2 to 3 years of life, healthy life, and able life relative to those in the Normal cluster.
Despite many strengths in the CHS, especially the larger number of elderly participants followed for 16 years, weaknesses exist. Participants in the CHS who underwent brain imaging were healthier than those who did not.1 Perhaps results may have been different if all of the participants had been scanned, although the inclusion of sicker participants may well have strengthened associations. The outcomes of YHL and YAL were based on self-report and other measures of these concepts may have given different results. Nonetheless, long-term follow-up of a large cohort of elderly participants demanded simple, reliable measures. Finally, perhaps results would have differed if no information had been missing, as detailed in the online Appendix.
These MRI findings and patterns are common in the elderly and often create anxiety in patients when they learn about the uncertain importance of the findings. The Normal and Atrophy clusters were the most similar with respect to outcomes. Those with isolated infarcts or isolated leukoaraiosis had significantly better outcomes than when these findings were combined but not as good as when all these findings were lacking. The findings on MRI scan of the combination of infarcts and leukoaraiosis portends a poor prognosis compared to the other clusters and should serve as a reminder to the clinician to identify and control vascular risk factors.
Supplementary Material
ACKNOWLEDGMENTS
This research was supported by contracts HHSN268201200036C, HHSN268200800007C, N01HC15103, N01HC55222, N01HC85079, N01HC85080, N01HC85081, N01HC85082, N01HC85083, N01HC85086, and grant HL080295 from the National Heart, Lung, and Blood Institute (NHLBI), with additional contribution from the National Institute of Neurological Disorders and Stroke (NINDS). Additional support was provided by AG023629 from the National Institute on Aging (NIA). A full list of principal CHS investigators and institutions can be found at https://chs-nhlbi.org/CHS-NHLBI.org. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Sponsor's role: None.
Footnotes
Conflict of interest: The authors report none related to this paper.
Authors’ contributions: Study concept and design: Longstreth and Diehr Acquisition of data: Beauchamp. Statistical analysis: Diehr and Yee. Interpretation of data: Beauchamp, Diehr, Longstreth, Newman, and Yee. Drafting of the manuscript: Longstreth. Critical revision of the manuscript for content: Beauchamp, Diehr, Longstreth, Newman, and Yee. Study supervision: Beauchamp, Diehr, Longstreth, and Newman.
REFERENCES
- 1.Longstreth WT, Jr, Diehr P, Manolio TA, et al. Cluster analysis and patterns of findings on cranial magnetic resonance imaging of the elderly: The Cardiovascular Health Study. Arch Neurol. 2001;58:635–640. doi: 10.1001/archneur.58.4.635. [DOI] [PubMed] [Google Scholar]
- 2.Longstreth WT, Jr, Diehr P, Beauchamp NJ, et al. Patterns on cranial magnetic resonance imaging in elderly people and vascular disease outcomes. Arch Neurol. 2001;58:2074. doi: 10.1001/archneur.58.12.2074. [DOI] [PubMed] [Google Scholar]
- 3.Diehr P, Thielke S, O'Meara E, et al. Comparing years of healthy life, measured in 16 ways, for normal weight and overweight older adults. J Obes. 2012;2012:894894. doi: 10.1155/2012/894894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hirsch CH, Diehr P, Newman AB, et al. Physical activity and years of healthy life in older adults: results from the Cardiovascular Health Study. J Aging Phys Act. 2010;18:313–334. doi: 10.1123/japa.18.3.313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fried LP, Borhani NO, Enright P, et al. The Cardiovascular Health Study: Design and rationale. Ann Epidemiol. 1991;1:263–276. doi: 10.1016/1047-2797(91)90005-w. [DOI] [PubMed] [Google Scholar]
- 6.Tell GS, Fried LP, Hermanson B, et al. Recruitment of adults 65 years and older as participants in the Cardiovascular Health Study. Ann Epidemiol. 1993;3:358–366. doi: 10.1016/1047-2797(93)90062-9. [DOI] [PubMed] [Google Scholar]
- 7.Krause NM, Jay GM. What do global self-rated health items measure? Med Care. 1994;32:930–942. doi: 10.1097/00005650-199409000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Idler EL, Benyamini Y. Self-rated health and mortality: A review of twenty-seven community studies. J Health Soc Behav. 1997;38:21–37. [PubMed] [Google Scholar]
- 9.Vermeer SE, Longstreth WT, Jr, Koudstaal PJ. Silent brain infarcts: A systematic review. Lancet Neurol. 2007;6:611–619. doi: 10.1016/S1474-4422(07)70170-9. [DOI] [PubMed] [Google Scholar]
- 10.Debette S, Markus HS. The clinical importance of white matter hyperintensities on brain magnetic resonance imaging: Systematic review and meta-analysis. BMJ. 2010;341:c3666. doi: 10.1136/bmj.c3666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Longstreth WT, Jr, Dulberg C, Manolio TA, et al. Incidence, manifestations, and predictors of brain infarcts defined by serial cranial magnetic resonance imaging in the elderly: The Cardiovascular Health Study. Stroke. 2002;33:2376–2382. doi: 10.1161/01.str.0000032241.58727.49. [DOI] [PubMed] [Google Scholar]
- 12.Longstreth WT, Jr, Arnold AM, Beauchamp NJ, Jr, et al. Incidence, manifestations, and predictors of worsening white matter on serial cranial magnetic resonance imaging in the elderly: The Cardiovascular Health Study. Stroke. 2005;36:56–61. doi: 10.1161/01.STR.0000149625.99732.69. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.