Abstract
Purpose
The purpose of this study was to evaluate the effects of age at onset of the first major depressive episode on the clinical features of individuals with major depressive disorder (MDD) in a large cohort of Korean depressed patients.
Materials and Methods
We recruited 419 MDD patients of age over 18 years from the Clinical Research Center for Depression study in South Korea. At the start of the study, the onset age of the first major depressive episode was self-reported by the subjects. The subjects were divided into four age-at-onset subgroups: childhood and adolescent onset (ages <18), early adult onset (ages 18-44), middle adult onset (ages 45-59), and late onset (ages 60+). Using analysis of covariance (ANCOVA) and ordinal logistic regression analysis with adjusting the effect of age, the relationships between clinical features and age at onset of MDD were evaluated.
Results
There was an apparent, but inconsistent correlation between clinical features and age at onset. Earlier onset MDD was significantly associated with higher proportion of female gender [adjusted odds ratio (AOR)=0.570, p=0.022], more previous suicide attempts (AOR=0.635, p=0.038), greater number of previous depressive episodes (F=3.475, p=0.016) and higher scores on the brief psychiatric rating scale (F=3.254, p=0.022), its negative symptom subscale (F=6.082, p<0.0001), and the alcohol use disorder identification test (F=7.061, p<0.0001).
Conclusion
Early age at onset may increase the likelihood of distinguishable MDD subtype, and age at onset of the first major depressive episode is a promising clinical indicator for the clinical presentation, course, and outcome of MDD.
Keywords: Major depressive disorder, age at onset, clinical indicator, subtype
INTRODUCTION
The clinical manifestations of major depressive disorder (MDD) are not limited to mood symptoms, but also include a wide range of cognitive and motor symptoms. Thus, MDD is considered a multifactorial and heterogeneous disorder which varies in terms of symptom severity, psychiatric comorbidity, and clinical course, including recurrence and response to treatment.1,2 Hence, MDD has classified by its clinical manifestation and progress, and its subtyping has no clear demarcation because of complex phenomena.3,4 Age at onset of the first major depressive episode can influence the symptoms and clinical course of depressive episodes, and has been proposed as a clinical indicator able to classify heterogeneous individuals diagnosed with MDD into more homogenous subgroups, and be useful in the subtyping or phenotyping of MDD.5,6 In previous studies, early-onset (or childhood and adolescent onset) MDD has been associated with a severe and chronic condition with a higher proportion of females, longer duration of illness, more episodes, more tendency to suicide, higher symptom severity, more psychiatric comorbidity, and more psychiatric symptoms,7,8 but fewer sleep, appetite and weight changes.9 Patients with early-onset MDD coupled with alcohol dependence had a more unfavorable response to escitalopram than those with late-onset MDD and alcohol dependence.10 In terms of immunology, it has been suggested that early-onset MDD involves a suppression of natural killer cell numbers and natural killer cell activity coupled with proinflammatory processes.11 Furthermore, based on the close relationship between early-onset mood disorder, high recurrence rate, and bipolarity, it has been proposed that age at onset is a more favorable clinical and genetic indicator than polarity in characterizing unipolar MDD and bipolar II disorder.12
There have been few studies in large cohorts of Korean MDD patients of the effect of age at onset of the first major depressive episode on the clinical features of MDD. The Clinical Research Center for Depression (CRESCEND) study of South Korea, which was the first large, prospective, observational, clinical study of a nationwide sample of Korean individuals diagnosed with depressive disorders, included epidemiological data using a number of psychometric scales to assess their clinical features.1 Hence, using the CRESCEND study, we aimed to evaluate the relationship between age at onset and the clinical features of MDD. More specifically, the purpose of this study was to answer the following questions:
How does age at onset of the first major depressive episode distribute?
Can the clinical features of the MDD of the different age-at-onset subgroups be distinguished?
MATERIALS AND METHODS
Study overview
A detailed description of the CRESCEND study has been presented elsewhere.13 In that study, 1183 depressed patients were recruited at one or other of 18 study centers consisting of 16 university-affiliated hospitals and two general hospitals across South Korea, from January 2006 to August 2008. The study protocols and consent forms were approved by all the relevant university and/or hospital Institutional Review Boards. The CRESEND study was performed over nine years. In phase I, the eligible subjects were assessed at baseline, followed by assessments in weeks 1, 2, 4, 8, 12, 24, and 52. In phase II, they were assessed annually over the course of eight years. The collection of data was managed and its quality monitored by the Department of Preventive Medicine of the Catholic University College of Medicine in Seoul. All the demographic and clinical data were collected by trained and certified clinical research coordinators, who were supervised by clinical psychiatrists at the regional centers. Using a preselected clinical report form, all data were recorded and stored on the website of the CRESCEND study (www.smileagain.or.kr).
Subjects
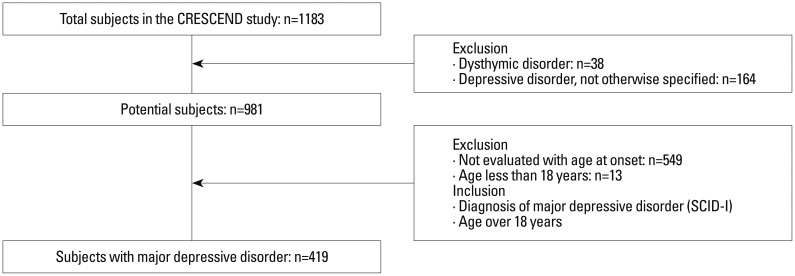
Broad inclusion and minimal exclusion criteria were adopted by the CRESCEND study, in order to closely reflect the real clinical situation. Psychiatric inpatients and outpatients who were beginning treatment for first-onset or recurrent depression were recruited. The inclusion criteria were as follows: 1) age over 7 years, and 2) current diagnosis of MDD without psychotic features, MDD with psychotic features, dysthymic disorder, and depressive disorders not otherwise specified, according to the fourth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) criteria.14 Diagnoses were confirmed within 2 weeks, using the Structured Clinical Interview for DSM-IV (SCID).15 The exclusion criteria were as follows: 1) current or lifetime diagnosis of schizophrenia, other psychotic disorders, bipolar disorder, psychotic disorders due to general medical condition or dementia, according to DSM-IV criteria; 2) a comorbid medical or neurological disease which interfered with the study evaluations and interviews; and/or 3) breastfeeding, pregnancy or intention to become pregnant within 9 months of enrollment. Written informed consent prior to participation was obtained from all the study participants or their authorized representatives. A psychiatric diagnosis confined to MDD without or with psychotic features was used as an inclusion criterion for the analysis described here, whereas it was not used to determine inclusion in the CRESCEND study. Hence, as shown in Fig. 1, 38 patients with dysthymic disorder and 164 patients with depressive disorder not otherwise specified were excluded from this study. Moreover, 549 depressed patients whose ages at onset were not clear, and 13 patients of age less than 18 years were also excluded. As a result, 419 MDD patients over 18 years were included in our investigation. Demographic data including age, sex, marital status (married or unmarried), educational status (below or above a college education), occupational status (employed or unemployed), religious affiliation (religious observance or not) and monthly income (below or above 2000 USD) were collected.
Fig. 1.
Process and criteria for selecting subjects. SCID, Structured Clinical Interview for DSM-IV.
Defining age at onset
The reliability of self-reported age at onset of first major depressive episode was generally good, as in previous studies.16,17 It has been suggested that younger MDD patients tend to report lower ages at onset than older patients,17 but this has been contested.16 In accord with DSM-IV, the first major depressive episode was defined by the first experience of a cluster of symptoms and signs of a major depressive episode, lasted at least 2 weeks, and was associated with clinically significant distress or functional impairment. Upon entry into the CRESCEND study, each depressed patient was asked about the age at onset and this was also estimated by the trained and certified clinical research coordinator. In cases of MDD superimposed on dysthymic disorder, the age at onset of MDD was regarded as the subject's best estimate of when the first major depressive episode had developed according to the definition used in previous studies.
The subjects were divided into four distinct age-at-onset categories, based on the designs of previous studies.7,8,18 To obtain clinically meaningful findings, the age-at-onset subgroups were defined in relation to the human life cycle. Thus, we divided the subjects into four age at onset subgroups as follows: child and adolescent onset (age <18), early adult onset (age 18-44), middle adult onset (age 45-59), and late adult onset (age 60+).
Assessments
Presence or absence of the symptoms corresponding to the specific diagnostic criteria for DSM-IV MDD was assessed. Total numbers of depressive symptoms, as defined by the DSM-IV diagnostic construct, were also counted. The following clinician-administered assessment scales were applied: the 17-item Hamilton Depression Rating Scale (HAMD),19 the Hamilton Anxiety Rating Scale (HAMA),20 the Brief Psychiatric Rating Scale (BPRS),21 the Clinical Global Impression item for severity (CGI-s),22 and the Social and Occupational Functioning Assessment Scale (SOFAS).23 Scores on the following self-administered assessment scales were also obtained: the Scale for Suicide ideation (SSI-Beck),24 the WHO quality of life assessment instrument-abbreviated version (WHOQOL-BREF),25 and the Alcohol Use Disorders Identification Test (AUDIT).26 All scales had been formally translated into the Korean language. In addition, their validity and reliability had been confirmed with acceptable levels in Korean setting.27,28,29 More severe symptoms or impacts were indicated by higher scores on the HAMD, the HAMA, the BPRS, the CGI-s, the SSI-Beck, and the AUDIT, and by lower scores on the SOFAS and the WHOQOL-BREF. In the HAMD and HAMA, each item is rated from 0 (not present) to 4 (severe). In the BPRS, each item is rated from 1 (absence of symptoms) to 7 (extremely severe). Positive symptoms were measured by the thinking disturbance subscale, namely the conceptual disorganization, hallucinatory behavior, and usual thought content items of the BPRS, and negative symptoms were measured by the emotional withdrawal, motor retardation, and blunted affect items.21 The score on the CGI-s is rated from 1 (not ill) to 7 (extremely severe),22 while the score on the SOFAS is rated from 1 to 10023 and the score on the AUDIT from 1 to 40.26 All the raters were trained twice a year, with a formal consensus meeting for applying the rater-administered assessment instruments.
Statistical analysis
Logistic regression models and analyses of covariance (ANCOVA) were used with age at onset as an independent variable. Subjects in the childhood and adolescent onset group were younger than those in the early, middle, and late adult onset groups (27.2 years, SD=7.12 versus 48.5 years, SD=14.24; t=16.03, p<0.0001). Because of this, comparisons among the age at onset groups were adjusted for the effect of age. Binary logistic regression models were fitted after adjusting for the effect of age to detect any gradation in discrete variables. ANCOVA were conducted after adjusting for the effect of age to analyze group differences in continuous variables, and Tukey's post-hoc analyses were also used. Statistical significance was set at p<0.05 (two-tailed) in all tests. All statistical analyses were performed using SPSS 18.0 for Windows (SPSS Inc., Chicago, IL, USA).
RESULTS
General characteristics of the subjects
As shown in Table 1, a large proportion of the subjects were female (78.8%), unmarried (76.4%), and unemployed (67.5%), suffered from depressive mood (98.9%), markedly diminished pleasure (89.3%), insomnia or hypersomnia (78.3%), psychomotor retardation or agitation (68.3%), and fatigue or loss of energy (81.4%) according to the DSM-IV MDD diagnostic criteria, and reported histories of suicide attempts (69.9%). Mean age was 37.4 (SD=15.6), and mean number of education years was 10.5 (SD=4.4). The mean score on the HAMD was 19.9 (SD=6.3), followed by 20.4 (SD=9.3) on the HAMA, 22.2 (SD=9.1) on the BPRS, 13.0 (SD=8.8) on the SSI-Beck, 4.7 (SD=1.0) on the CGI-s, 57.2 (SD=11.9) on the SOFAS, 62.5 (SD=10.2) on the WHOQOL-BREF, and 10.8 (SD=9.5) on the AUDIT.
Table 1.
General Characteristics of Subjects (n=419)
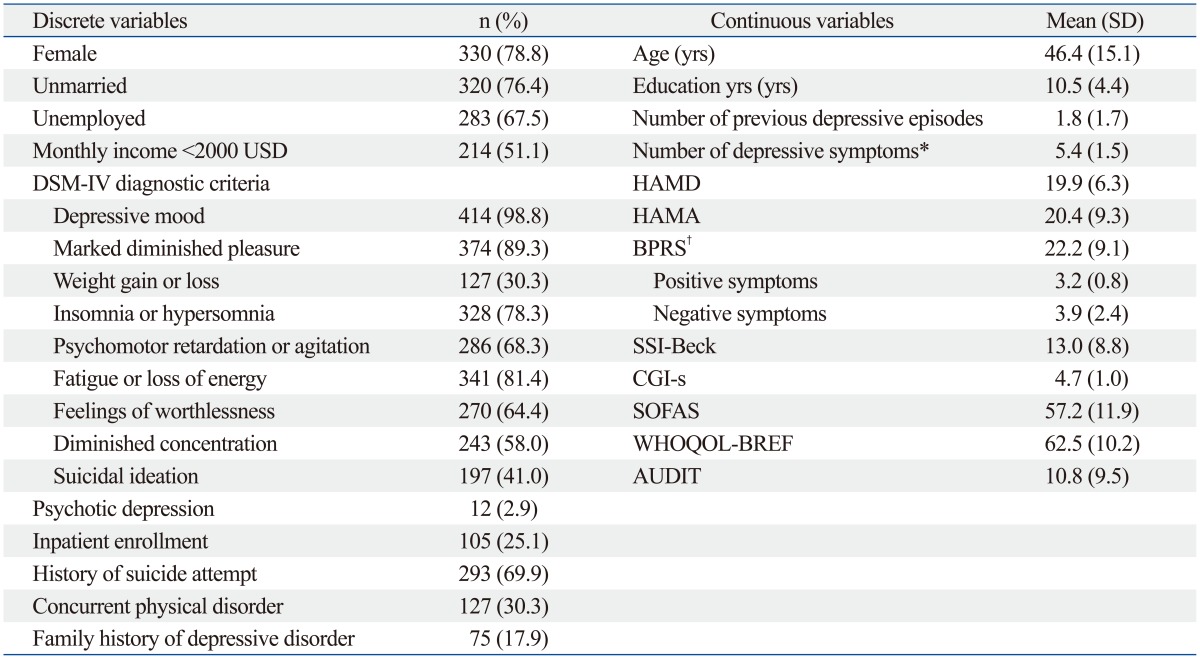
AUDIT, Alcohol Use Disorders Identification Test; BPRS, Brief Psychiatric Rating Scale; CGI-s, Clinical Global Impression item for severity; HAMA, Hamilton Anxiety Rating Scale; HAMD, Hamilton Depression Rating Scale; SSI-Beck, Scale for Suicide Ideation; SOFAS, Social and Occupational Functional Assessment Scale; WHOQOL-BREF, WHO quality of life assessment instrument-abbreviated version.
*Depressive symptoms were defined according to the diagnostic criteria for DSM-IV major depressive episode.
†n=320.
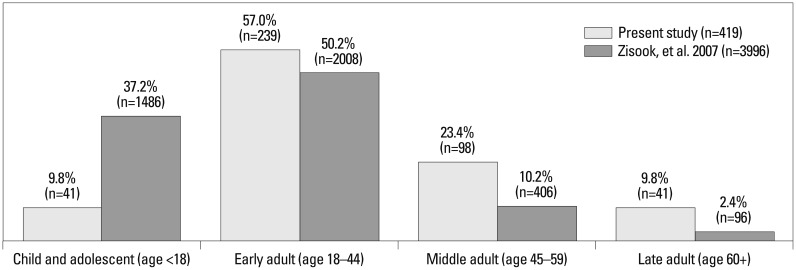
Subgroups in terms of age at onset of the first major depressive episode
As shown in Fig. 2, the mean age at onset of the first depressive episode was 37.4 years (SD=15.6; range=10-77). The distribution of ages at onset was positively skewed (skewness=0.30), and its kurtosis was -0.80. The mean age at onset was higher than its median (36.0 years) and mode (30.0 years). As shown in Fig. 3, about half (57.0%) of the subjects were first affected by MDD as young adults, followed by 23.4% as middle adults, and 9.8% each as children and adolescents, and as late adults.
Fig. 2.
Distribution of ages at onset of the first major depressive episode (n=419).
Fig. 3.
Subgroups in terms of age at onset of the first major depressive episode.
Clinical features associated with age at onset of the first major depressive episode
The clinical features (discrete variables) associated with age at onset are presented in Table 2. After adjustment for current age, logistic regression models showed that earlier age at onset was associated with female gender [odds ratio (OR)=0.570; 95% confidence interval (CI)=0.352-0.921; p=0.022] and more frequent previous suicide attempts (OR=0.635; 95% CI=0.413-0.975; p=0.038). After adjustment for age, there were no significant differences between the four subgroups with respect to unmarried status (OR=1.449; 95% CI=0.540-3.893; p=0.461), unemployed status (OR=1.146; 95% CI=0.747-1.757; p=0.533), monthly income <2000 USD (OR=1.039; 95% CI=0.719-1.499; p=0.840), current presence of depressed mood (OR=1.192; 95% CI=0.191-7.641; p=0.851), markedly diminished pleasure (OR=0.903; 95% CI=0.494-1.651; p=0.740), weight gain or loss (OR=1.098; 95% CI=0.738-1.633; p=0.645), insomnia or hypersomnia (OR=0.189; 95% CI=0.861-2.135; p=0.189), psychomotor retardation or agitation (OR=1.088; 95% CI=0.728-1.624; p=0.681), fatigue or loss of energy (OR=1.257; 95% CI=0.859-1.838; p=0.239), feelings of worthlessness (OR=0.921; 95% CI=0.635-1.334; p=0.662), or diminished concentration (OR=1.081; 95% CI=0.747-1.564; p=0.680), psychotic depression (OR=1.106; 95% CI=0.323-3.784; p=0.874), inpatient enrollment (OR=1.106; 95% CI=0.732-1.672; p=0.631), and family history of depressive disorder (OR=0.813; 95% CI=0.487-1.358; p=0.996).
Table 2.
Clinical Features Associated with Age at Onset of the First Major Depressive Episode (I): Discrete Variables (n=419)
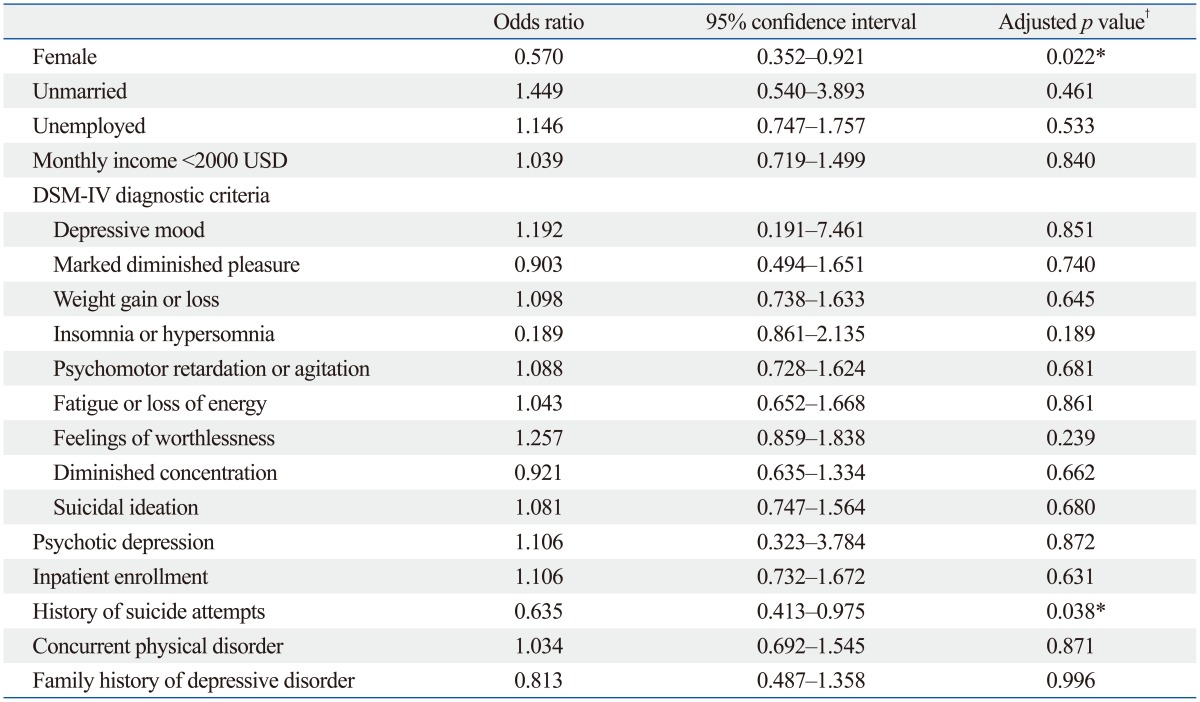
*p<0.05.
†Adjusted for the effect of age.
Table 3 presents the clinical features (continuous variables) associated with age at onset. After adjustment for current age, ANCOVA showed that earlier age at onset was associated with greater number of previous depressive episodes (F=3.475; p=0.016), higher scores on the BPRS (F=3.254; p=0.022), on its negative symptom subscale (F=6.082; p<0.0001), and on the AUDIT (F=7.061; p<0.001). According to Tukey's post-hoc analyses, subjects with childhood and adolescent onset MDD had significantly more previous depressive episodes, a higher score on the negative symptom subscale of the BPRS, and a higher total score on the AUDIT than those in the other subgroups. After adjustment for age, there were no significant differences between the four subgroups with respect to years of education (F=0.764; p=0.515), number of current depressive symptoms (F=1.643; p=0.179), scores on the HAMD (F=1.295; p=0.276), the HAMA (F=1.198; p=0.310), the SSI-Beck (F=1.733; p=0.160), the CGI-s (F=1.069; p=0.362), the SOFAS (F=1.036; p=0.376) and WHOQOL-BREF (F=0.207; p=0.892).
Table 3.
Clinical Features Associated with Age at Onset of the First Major Depressive Episode (II): Continuous Variables (n=419)
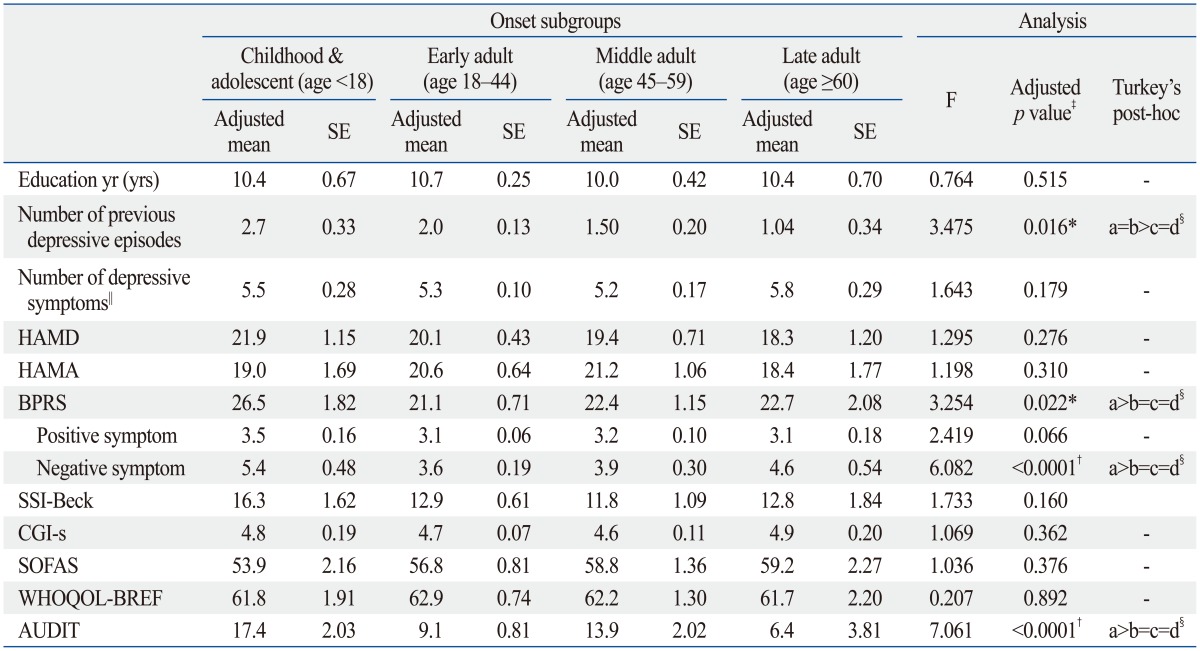
AUDIT, Alcohol Use Disorders Identification Test; BPRS, Brief Psychiatric Rating Scale; CGI-s, Clinical Global Impression item for severity; HAMA, Hamilton Anxiety Rating Scale; HAMD, Hamilton Depression Rating Scale; SSI-Beck, Scale for Suicide Ideation; SOFAS, Social and Occupational Functional Assessment Scale; WHOQOL-BREF, WHO quality of life assessment instrument-abbreviated version; SE, standard error; DSM-IV, fourth edition of the Diagnostic and Statistical Manual of Mental Disorders.
*p<0.05.
†p<0.01.
‡Adjusted for the effect of age.
§a, childhood and adolescent onset subgroup; b, early adult onset subgroup; c, middle adult onset subgroup; d, late adult onset subgroup.
∥Depressive symptoms were defined by diagnostic criteria for the DSM-IV major depressive episode.
DISCUSSION
In terms of age at onset of first major depressive episode, the findings of this study were characterized by small proportion of child and adolescent subgroup and high proportions of adult subgroups (Fig. 3). The frequency distribution of onset groups is somewhat different from the distribution reported by Zisook, et al.18 The frequency of the childhood and adolescent onset MDD subgroup in this study is lower than that in the previous study, whereas the frequencies of the middle and late adult onset MDD subgroups in this study were higher. The mean age at onset of the first major depressive episode in this study (37.4 years) is markedly higher than in the previous study (26 years). Additionally, Yang, et al.9 reported that the mean age at onset of MDD in 1970 Han Chinese women was 35.9 years. Hence, there is a possibility that the difference in the mean age at onset of the recruited subjects between the two studies contributed to the different proportions of the subgroups in terms of first major depressive episode. However, comparison with the previous findings is difficult because of the variations between the studies, possibly due to differences between psychiatric inpatients and outpatients, ethnic effects on the age at onset of the first major depressive episode, and sample size.
Although there is no distinctively identifiable age-at-onset MDD subgroup in this study, subjects who have reported earlier age at onset are independently associated with higher proportion of female gender, more frequent history of suicide attempts, greater number of previous depressive episodes, more severe negative symptoms, and higher alcohol consumption. Moreover, those who reported later age at onset are associated with contradictory characteristics; thus, using the ordinal logistic regression and ANCOVA with Tukey's post-hoc analyses after adjusting for the effects of current age, the childhood and adolescent onset subgroup is more distinctive in terms of clinical features than the other subgroups in this study.
We now discuss each of these features in turn, within the context of the relevant previous ones. First, the subjects with earlier onset MDD are more likely to have a more troubled clinical course. Earlier onset MDD is associated with more frequent suicide attempts and a greater number of previous episodes in this study. Although we did not investigate the relationship between duration of illness and age-at-onset, these findings are partly in accordance with the previous finding that earlier onset of MDD was associated with more frequent recurrence, including a higher number of episodes, longer duration of illness, and more frequent attempted suicides.7,8,18
Second, patients with earlier onset MDD tends to have more atypical symptoms or other manifestations than the mood symptoms evident in the current depressive episodes in this study. Patients with earlier onset MDD have higher total scores on the BPRS. In particular, on the BPRS negative symptom subscale in this study, although there are no correlations among the subgroups with respect to the types and number of DSM-IV depressive symptoms, and scores on the CGI-s, HAMD, HAMA, and SSI-Beck. These findings are inconsistent with previous reports that earlier onset MDD is associated with greater severity of index depressive episode, more frequent current suicidal ideation9,18 and interpersonal rejection sensitivity.30 These contradictory findings may have been due to differences in sample size or composition, and methods of statistical analysis. Despite these differences, the possibility that dominantly negative symptoms of MDD in the index episode contributes to the separated and distinctive properties, unfavorable treatment response, and great burden of illness cannot be excluded.31,32
Third, subjects with earlier onset MDD were more likely to acknowledge more severe alcohol intake in this study. This finding is in accord with the trend towards a higher incidence of lifetime substance use disorders in earlier onset MDD patients, and an increasing body of evidence for an underpinning genetic linkage between MDD and addiction.33,34,35 Although higher numbers of lifetime comorbid psychiatric diagnoses (for example, panic disorder, posttraumatic stress disorder, obsessive-compulsive disorder, or hypochondriasis) in subjects with earlier onset MDD have been consistently observed in previous studies,9,18,30 the association between psychiatric comorbidity and age-at-onset subgroups has not been investigated in this study.
Fourth and finally, we have found no relationship between family history of depressive disorder and the age-at-onset subgroups. Although an association between earlier onset MDD and stronger genetic loading has been suggested in several previous studies,7,36,37 MDD can be the consequence of complex interactions between genetic and environmental variables.5 For example, Korten, et al.38 demonstrated that, based on the crude cutoff age of 40, there was a significant association between positive family history and early onset MDD. Differences in the cutoff age in terms of age-at-onset subgroups may contribute to the inconsistency between the findings of previous studies.
This study has several limitations. First, age at onset of first major depressive episode, which was estimated by self-report, is uncertain and arbitrary. Second, age at onset cannot directly allow conclusions concerning causal relationship between the clinical features of MDD. Third, we have not assessed duration of illness, duration of current episode, lifetime psychiatric comorbidity, cognitive symptom domains and other significant clinical characteristics. Findings concerning the association between clinical features and the age at onset subgroups are limited in this study. Fourth, the statistical differences between age at onset subgroups may be of limited clinical significance. Since these findings may be the result of the large sample size, or the broad inclusion criteria, their implications for clinical practice may be limited. Fifth, use of a modification of the Bonferroni's procedure for testing multiple hypotheses would have yielded more precise estimates of the association between the various variables and the age-at-onset subgroups. Sixth and finally, inter-rater reliability has not been examined in our study.
In spite of these limitations, this study has the virtue of expanding investigations of the relationship between clinical features and age at onset subgroups in a large Korean cohort with depressive disorders (the CRESCEND study). Based on the results of this study, the subjects with early onset MDD presented atypical manifestations with high alcohol intake, a greater tendency to recurrence, and poor clinical courses and/or outcomes. Thus, early age at onset may be a promising phenotyping indicator of MDD with a high clinical burden. Further studies refining the MDD clinical characteristics associated with age at onset in the Korean population are needed.
ACKNOWLEDGEMENTS
This study was supported by a grant of the Korea Healthcare technology R&D Project, Ministry of Health and Welfare, Republic of Korea (HI10C2020). The Ministry of Health and Welfare had no further role in study design; in the collection, analysis, and interpretation of data; in the writing of the report; or in the decision to submit the paper for publication.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Seok JH, Lee KU, Kim W, Lee SH, Kang EH, Ham BJ, et al. Impact of early-life stress and resilience on patients with major depressive disorder. Yonsei Med J. 2012;53:1093–1098. doi: 10.3349/ymj.2012.53.6.1093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kendler KS, Kessler RC, Walters EE, MacLean C, Neale MC, Heath AC, et al. Stressful life events, genetic liability, and onset of an episode of major depression in women. Am J Psychiatry. 1995;152:833–842. doi: 10.1176/ajp.152.6.833. [DOI] [PubMed] [Google Scholar]
- 3.Paykel ES. Classification of depressed patients: a cluster analysis derived grouping. Br J Psychiatry. 1971;118:275–288. doi: 10.1192/bjp.118.544.275. [DOI] [PubMed] [Google Scholar]
- 4.Lichtenberg P, Belmaker RH. Subtyping major depressive disorder. Psychother Psychosom. 2010;79:131–135. doi: 10.1159/000286957. [DOI] [PubMed] [Google Scholar]
- 5.Zhu T, De Luca V, Gallaugher LA, Woldeyohannes HO, Soczynska JK, Szymkowicz S, et al. Admixture analysis of age at onset in major depressive disorder. Gen Hosp Psychiatry. 2012;34:686–691. doi: 10.1016/j.genhosppsych.2012.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jaffee SR, Moffitt TE, Caspi A, Fombonne E, Poulton R, Martin J. Differences in early childhood risk factors for juvenile-onset and adult-onset depression. Arch Gen Psychiatry. 2002;59:215–222. doi: 10.1001/archpsyc.59.3.215. [DOI] [PubMed] [Google Scholar]
- 7.Zisook S, Rush AJ, Albala A, Alpert J, Balasubramani GK, Fava M, et al. Factors that differentiate early vs. later onset of major depression disorder. Psychiatry Res. 2004;129:127–140. doi: 10.1016/j.psychres.2004.07.004. [DOI] [PubMed] [Google Scholar]
- 8.Zisook S, Rush AJ, Lesser I, Wisniewski SR, Trivedi M, Husain MM, et al. Preadult onset vs. adult onset of major depressive disorder: a replication study. Acta Psychiatr Scand. 2007;115:196–205. doi: 10.1111/j.1600-0447.2006.00868.x. [DOI] [PubMed] [Google Scholar]
- 9.Yang F, Li Y, Xie D, Shao C, Ren J, Wu W, et al. Age at onset of major depressive disorder in Han Chinese women: relationship with clinical features and family history. J Affect Disord. 2011;135:89–94. doi: 10.1016/j.jad.2011.06.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Muhonen LH, Lönnqvist J, Lahti J, Alho H. Age at onset of first depressive episode as a predictor for escitalopram treatment of major depression comorbid with alcohol dependence. Psychiatry Res. 2009;167:115–122. doi: 10.1016/j.psychres.2008.05.001. [DOI] [PubMed] [Google Scholar]
- 11.Frank MG, Wieseler Frank JL, Hendricks SE, Burke WJ, Johnson DR. Age at onset of major depressive disorder predicts reductions in NK cell number and activity. J Affect Disord. 2002;71:159–167. doi: 10.1016/s0165-0327(01)00395-0. [DOI] [PubMed] [Google Scholar]
- 12.Benazzi F. Classifying mood disorders by age-at-onset instead of polarity. Prog Neuropsychopharmacol Biol Psychiatry. 2009;33:86–93. doi: 10.1016/j.pnpbp.2008.10.007. [DOI] [PubMed] [Google Scholar]
- 13.Park SC, Kim JM, Jun TY, Lee MS, Kim JB, Jeong SH, et al. Prevalence and clinical correlates of insomnia in depressive disorders: The CRESCEND Study. Psychiatry Investig. 2013;10:373–381. doi: 10.4306/pi.2013.10.4.373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington DC: American Psychiatric Press; 1994. [Google Scholar]
- 15.First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders-Patient Edition (SCID-I/P, Version 2.0) New York: Biometrics Research Department, New York State Psychiatric Institute; 1995. [Google Scholar]
- 16.Farrer LA, Florio LP, Bruce ML, Leaf PJ, Weissman MM. Reliability of self-reported age at onset of major depression. J Psychiatr Res. 1989;23:35–47. doi: 10.1016/0022-3956(89)90015-0. [DOI] [PubMed] [Google Scholar]
- 17.Prusoff BA, Merikangas KR, Weissman MM. Lifetime prevalence and age of onset of psychiatric disorders: recall 4 years later. J Psychiatr Res. 1988;22:107–117. doi: 10.1016/0022-3956(88)90075-1. [DOI] [PubMed] [Google Scholar]
- 18.Zisook S, Lesser I, Stewart JW, Wisniewski SR, Balasubramani GK, Fava M, et al. Effect of age at onset on the course of major depressive disorder. Am J Psychiatry. 2007;164:1539–1546. doi: 10.1176/appi.ajp.2007.06101757. [DOI] [PubMed] [Google Scholar]
- 19.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hamilton M. The assessment of anxiety states by rating. Br J Med Psychol. 1959;32:50–55. doi: 10.1111/j.2044-8341.1959.tb00467.x. [DOI] [PubMed] [Google Scholar]
- 21.Overall JE, Gorham DR. The brief psychiatric rating scale. Psychol Rep. 1962;10:779–812. [Google Scholar]
- 22.Guy W U.S. Department of Health, Education, and Welfare Publication. ECDEU Assessment Manual for Psychopharmacology. Washington DC: National Institute of Mental Health; 1976. [Google Scholar]
- 23.Goldman HH, Skodol AE, Lave TR. Revising axis V for DSM-IV: a review of measures of social functioning. Am J Psychiatry. 1992;149:1148–1156. doi: 10.1176/ajp.149.9.1148. [DOI] [PubMed] [Google Scholar]
- 24.Beck AT, Kovacs M, Weissman A. Assessment of suicidal intention: the Scale for Suicide Ideation. J Consult Clin Psychol. 1979;47:343–352. doi: 10.1037//0022-006x.47.2.343. [DOI] [PubMed] [Google Scholar]
- 25.The WHOQOL Group. Development of the World Health Organization WHOQOL-BREF quality of life assessment. Psychol Med. 1998;28:551–558. doi: 10.1017/s0033291798006667. [DOI] [PubMed] [Google Scholar]
- 26.Saunders JB, Aasland OG, Babor TF, de la Fuente JR, Grant M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on Early Detection of Persons with Harmful Alcohol Consumption--II. Addiction. 1993;88:791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- 27.Yi JS, Bae SO, Ahn YM, Park DB, Noh KS, Shin HK, et al. Validity and reliability of the Korean Version of the Hamilton Depression Rating Scale(K-HDRS) J Korean Neuropsychiatr Assoc. 2005;44:456–465. [Google Scholar]
- 28.Lee JY, Cho MJ, Kwon JS. Global Assessment of Functioning Scale and Social and Occupational Functioning Scale. Korean J Psychopharmacol. 2006;17:122–127. [Google Scholar]
- 29.Joe KH, Chai SH, Park A, Lee HK, Shin IH, Min SH. Optimum cut-off score for screening of hazardous drinking using the Korean version of Alcohol Use Disorder Identification Test (AUDIT-K) J Korean Academy of Addiction Psychiatry. 2009;13:34–40. [Google Scholar]
- 30.Wilkowska-Chmielewska J, Szelenberger W, Wojnar M. Age-dependent symptomatology of depression in hospitalized patients and its implications for DSM-5. J Affect Disord. 2013;150:142–145. doi: 10.1016/j.jad.2012.12.012. [DOI] [PubMed] [Google Scholar]
- 31.Galynker II, Cai J, Ongseng F, Finestone H, Dutta E, Serseni D. Hypofrontality and negative symptoms in major depressive disorder. J Nucl Med. 1998;39:608–612. [PubMed] [Google Scholar]
- 32.Galynker II, Cohen LJ, Cai J. Negative symptoms in patients with major depressive disorder: a preliminary report. Neuropsychiatry Neuropsychol Behav Neurol. 2000;13:171–176. [PubMed] [Google Scholar]
- 33.Nurnberger JI, Jr, Foroud T, Flury L, Su J, Meyer ET, Hu K, et al. Evidence for a locus on chromosome 1 that influences vulnerability to alcoholism and affective disorder. Am J Psychiatry. 2001;158:718–724. doi: 10.1176/appi.ajp.158.5.718. [DOI] [PubMed] [Google Scholar]
- 34.Lyons MJ, Schultz M, Neale M, Brady K, Eisen S, Toomey R, et al. Specificity of familial vulnerability for alcoholism versus major depression in men. J Nerv Ment Dis. 2006;194:809–817. doi: 10.1097/01.nmd.0000244480.78431.49. [DOI] [PubMed] [Google Scholar]
- 35.Gokturk C, Schultze S, Nilsson KW, von Knorring L, Oreland L, Hallman J. Serotonin transporter (5-HTTLPR) and monoamine oxidase (MAOA) promoter polymorphisms in women with severe alcoholism. Arch Womens Ment Health. 2008;11:347–355. doi: 10.1007/s00737-008-0033-6. [DOI] [PubMed] [Google Scholar]
- 36.Alpert JE, Fava M, Uebelacker LA, Nierenberg AA, Pava JA, Worthington JJ, 3rd, et al. Patterns of axis I comorbidity in early-onset versus late-onset major depressive disorder. Biol Psychiatry. 1999;46:202–211. doi: 10.1016/s0006-3223(99)00017-7. [DOI] [PubMed] [Google Scholar]
- 37.Klein DN, Schatzberg AF, McCullough JP, Dowling F, Goodman D, Howland RH, et al. Age of onset in chronic major depression: relation to demographic and clinical variables, family history, and treatment response. J Affect Disord. 1999;55:149–157. doi: 10.1016/s0165-0327(99)00020-8. [DOI] [PubMed] [Google Scholar]
- 38.Korten NC, Comijs HC, Lamers F, Penninx BW. Early and late onset depression in young and middle aged adults: differential symptomatology, characteristics and risk factors? J Affect Disord. 2012;138:259–267. doi: 10.1016/j.jad.2012.01.042. [DOI] [PubMed] [Google Scholar]