Abstract
Surgical resection of a contralateral recurrence of non-small cell lung cancer (NSCLC) is indicated in patients without evidence of disseminated disease and considered functionally operable. General anesthesia and double-lumen intubation involves one lobe ventilation in a patient treated with a previous lobectomy, thus increasing the risks of ventilator-induced injuries and the morbidity. Awake procedures facilitate the surgery decreasing the anesthetic and surgical times, keeping the diaphragm motion and diminishing the ventilator-induced injuries into the remaining contralateral lobe. We present a 43-year-old woman with a previous left-lower lobectomy for a 3.1-cm mucinous adenocarcinoma 15 months before without nodal involvement, who presents a right-lower lobe 8-mm cavitated nodule, with evident radiological growth and fine-needle aspiration concordant with mucinous adenocarcinoma. We suggest an awake procedure with locoregional epidural anesthesia.
Keywords: Thoracoscopy/VATS, lung cancer surgery, anesthesia
A 43-year-old woman with past history of left-lower lobectomy for a mucinous adenocarcinoma pathologic stage IB without nodal involvement, presents in a follow-up CT scan a 6-mm nodule in the upper segment of the right-lower lobe, growing to 8 mm in a later control. A fine needle aspiration is performed with diagnosis of mucinous adenocarcinoma concordant with a contralateral recurrence. Pulmonary function tests with 85% FEV1 and 73% DLCO enable surgery. We are developing two clinical trials comparing the standard general anesthesia with double-lumen orotracheal intubation and the awake nonintubated with locoregional epidural anesthesia, for both pulmonary metastasis and interstitial lung disease. In this specific case, we proposed an awake procedure in order to avoid double-lumen intubation and deleterious adverse effects of mechanical ventilation in the remaining left-upper lobe during the surgery, that we hypothesized could adversely affect the postoperative course of the patient in terms of pulmonary complications. After the proposal explaining the advantages and disadvantages of both ways of proceeding, the patient accepted the nonintubated one, so she signed a written informed consent.
A thoracic epidural catheter was inserted at the T4-T5 level with a single injection of 15 mL of bupivacaine 0.5% and left in place during the procedure, until 24 hours after the operation. Pressure of carbon dioxide (PaCO2) and oxygen (PaO2) were measured during the surgery. Midazolam and fentanyl were administered intravenously to keep the patient calm but under conscious sedation throughout the procedure, so she could communicate with the anesthetist and the surgeon. She was placed in left lateral decubitus position and continued breathing spontaneously. An intranasal multiperforated catheter was inserted with local anesthesia and left above the vocal cords to elevate the oxygen concentration in the inspired air. This device was used because it is very easy to put, well tolerated and it doesn’t increase inspiratory flow. Before the incision, the O2 pressure in arterial blood was 400 mmHg, and the CO2 pressure was 44 mmHg.
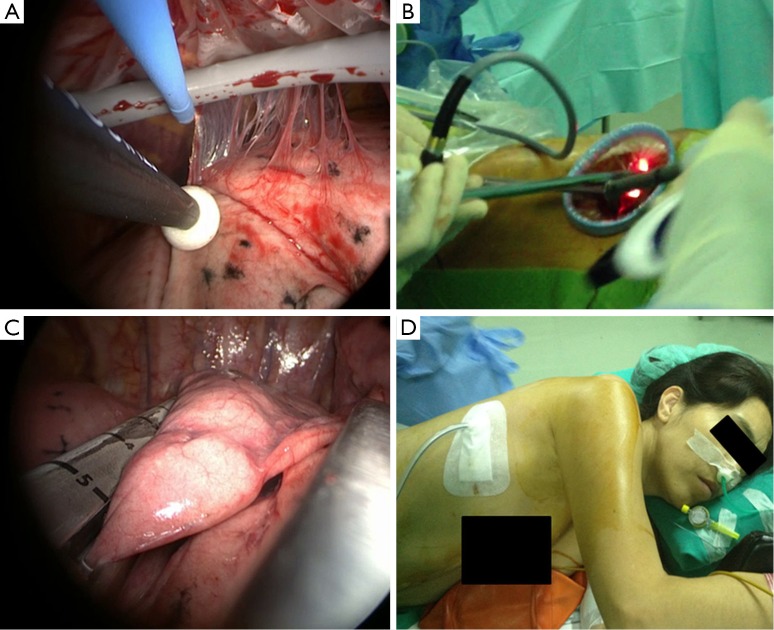
Then we performed a 4-cm single incision in the 5th intercostal space (uniportal VATS) resulting in a surgical pneumothorax with excellent lung collapse owing to the absence of underlying pathology in her lungs. There were adhesions from the right upper and middle lobes to the chest wall. Some of the adhesions were liberated with monopolar electrocautery and the adhesions in the most-upper part were left in place to keep the apex without complete collapse (Figure 1A). After the surgical pneumothorax the O2 pressure in arterial blood kept in 446 mmHg, and the CO2 pressure elevated to a moderate hypercapnia degree (56 mmHg) without clinical repercussion. There were no changes in the heart rate, blood pressure and respiratory rate (Table 1).
Figure 1.
(A) Liberating adhesions through the incision with electrocautery; (B) working through the single incision of 4 cm with the camera, lung forceps and EndoGIA black load (Autosuture, Norwalk, CT); (C) performing the resection of the right-lower lobe nodule with oncologic margins after palpating the lesion; (D) the patient is mild-sedated with the intranasal multiperforated catheter breathing spontaneously.
Table 1. Operative and postoperative parameters.
| Parameters | Supine decubitus | Lateral decubitus | Surgical pneumothorax | Chest wall closed | 24 hours | Discharge |
|---|---|---|---|---|---|---|
| Heart rate (bpm) | 86 | 68 | 83 | 70 | 73 | 80 |
| Blood pressure (mmHg) | 96/72 | 112/74 | 120/80 | 110/82 | 116/75 | 120/70 |
| Respiratory rate (/min) | 12 | 12 | 12 | 13 | 15 | 16 |
| % O2 | 60 | 60 | 80 | 80 | 21 | 21 |
| PaO2 (mmHg) | 227 | 253 | 87 | 345 | 82 | 78 |
| PaCO2 (mmHg) | 53 | 53 | 60 | 60 | 42 | 44 |
| pH | 7.32 | 7.32 | 7.28 | 7.26 | 7.39 | 7.40 |
| PAS | – | – | – | – | 3 | 2 |
| Pain location | – | – | – | – | Drainage | Drainage |
bpm, beats per minute; % O2, oxygen inspired fraction; PaO2, oxygen blood partial pressure; PaCO2, carbon dioxide blood partial pressure; pain analogue scale [0-10].
After visualization and palpation of the nodule in the right-lower lobe, we performed a wide wedge resection of the lesion (EndoGIA black load, Autosuture, Norwalk, CT) and the specimen was removed with a specimen bag (Figure 1B,C). Intraoperative analysis showed an adenocarcinoma with more than 1-cm free margin. There were no other lesions and no lymph nodes enlarged. A 24 Fr chest drain was inserted through the single-port and connected to suction under 10 cm H2O while the patient was asked to breathe deeply and cough to completely reexpand the lung. Operative time was 30 minutes, and total anesthesia time was 40 minutes, with a global in-operation time of 70 minutes. Intranasal catheter was well tolerated (Figure 1D) and kept the oxygenation high, while hypercapnia was completely asymptomatic.
The patient stayed in an intermediate care unit for 24 hours, without evidence of air leak, and the chest X-ray showed complete lung reexpansion since 2 hours after the operation. In the 6 hours control heart rate, blood pressure and respiratory rate were kept in normal values. O2 pressure in arterial blood was kept in 87 mmHg with nasal cannula at 3 lpm, and CO2 pressure decreased to normal values immediately after the surgery (38 mmHg). There was no pain with the epidural catheter (visual analogue scale), and the patient resumed oral intake in the evening. A total of 24 hours after the procedure, she was moved into the hospitalization unit, the drainage was removed without air leak and epidural catheter was changed by oral analgesia, and with a chest X-ray showing complete lung reexpansion she was discharged 1 day after the surgery. In the late control she had O2 pressure in arterial blood of 94 mmHg without any device, and no changes in CO2 pressure (38 mmHg). We systematically quantify the satisfaction level according to a subjective four degree scale (excellent, good, tolerable, bad), and this patient expressed excellent tolerance without any complaint.
Final pathologic exam confirmed the recurrence nature of the lesion, with an 8-mm mucinous adenocarcinoma concordant to the former one, free margins of 1.3 cm.
In the postoperative visit to the clinic three weeks later she had no pain, and she expressed high level of satisfaction with the procedure, with radiological and clinical excellent parameters.
Discussion
Awake thoracic procedures have gained approval in the last years as an alternative to the standard procedures performed under general anesthesia and double-lumen intubation (1). Pioneers surgical teams as E. Pompeo and colleagues have shown feasible and safe to perform pulmonary biopsies, lung-volume reduction surgery of the emphysematous patient, sympathectomies for hyperhidrosis and pulmonary resections, as many other groups do. Even some groups have proved feasible to perform major pulmonary resections like lobectomies and also thymectomies in the awake patient (2).
Indications for awake procedures are getting elucidated after accumulating experience, but it is essential that the surgical and anesthetic team understand the physiologic changes occurring during the awake procedure in a spontaneously breathing patient, the changes in the operating maneuvers, and the potential complications of the procedure, and working with a skilled nursing team used to awake operations (3). An emergency protocol has to be well designed before venturing (Table 2). One of the main aspects of suggesting these procedures consists on strictly selecting the patient, because not all the patients are psychologically prepared and if the patient gets nervous and anxious the operation can be difficult (4).
Table 2. Emergency protocol.
| Criteria for a conversion to thoracotomy or general anesthesia |
| Respiratory acidosis with pH <7.1, with taquipnea (higher than 30 rpm) |
| Hypoxemia (pO2 <60 mmHg) with no improvement despite high flow oxygenation nor non invasive-ventilation |
| Continuous cough with no improvement despite aerosolized lidocaine nor vagal blockade |
| Anxiety attack with no improvement with sedation |
| Moderate to major bleeding, uncontrollable with the single incision/awake procedure, which requires more important maneuvers (pulmonary artery clamp, primary suture, reconstruction) |
| Non adequate lung collapse which make lung mobilization and resection difficult |
| Adhesions in more than 50% of the lung surface which lengthens the procedure or makes the procedure difficult |
| Impossibility of nodule palpation through the single-incision or the awake fashion (small nodules, central location, excessive cough reflex without improvement with vagal blockade) |
| Pulmonary lesions requiring major lung resection (lobectomy, pneumonectomy) through the single-incision/awake procedure (relative criteria) |
| Patient voluntary desire of conversion |
| Conversion to general anesthesia/thoracotomy |
| Introduce thoracic drainage through the incision, connect it to water seal system and close the wound with a sterile transparent dressing around the drainage, to let the lung reexpand again and improve oxygen saturation or dyspnea |
| General anesthesia and orotracheal lateral decubitus intubation |
| Perform the thoracotomy or the additional ports and proceed |
The potential advantages of these procedures include minimizing the ventilator-induced injuries (barotraumas, atelectrauma, volutrauma) thus decreasing the risks of respiratory postoperative infections, special in patients with pulmonary underlying disease. Avoiding the effects of general anesthesia on the cellular and humoral immune response, can potentially diminish the incidence of postoperative infections and even it has been suggested the possibility of decreasing the chance of tumor progression (5). Uniportal VATS approach, in experienced hands, allows to perform the procedure without extending the operative time, and seems to reduce postoperative pain unless there is still a lack of clinical trials comparing with normal VATS approaches.
In this patient we suggested an awake surgery because she had been previously performed a contralateral lobectomy. We hypothesized that avoiding mechanical ventilation in the remaining lobe could prevent potential damages, so the remaining lobe was spontaneously ventilated with high oxygen concentration, keeping the diaphragm motion. It only appeared what has been called “permissive hypercapnia”, but the patient didn’t experience dyspnea. She could also resume normal activities like walking and oral intake the same day of the surgery, and the reexpansion was complete without air leak so she was discharged 24 hours after a lung resection without pain, so recovery of normal life can be fastened. Cardiovascular parameters remained without changes throughout all the process and CO2 pressure in arterial blood decreased to normal values immediately after the surgery (PaCO2 42 mmHg).
Intranasal multiperforated catheter has proved to be a very useful device and well tolerated with mild sedation, increasing the oxygen concentration just above the airway without elevating the flow neither the pressure in the airway, keeping the O2 pressure in arterial blood in excellent values.
Decreasing the need of general anesthesia and mechanical ventilation, the operative and anesthetic times, and the length of stay, also decreases the economical costs of the procedure (6).
We hypothesized that decreasing the interference with immune response with an awake procedure can potentially be beneficial in recurrent neoplastic disease in order to decrease the chance of reappearance of the tumor, but more evidence is needed showing that this benefit could potentially counteract the hypothetic stress related to surgical pneumothorax in an awake patient.
We conclude that awake uniportal limited pulmonary resections in recurrent non-small cell lung cancer (NSCLC), in the absence of high comorbidity and satisfactory functional tests, are feasible and have a safe pattern avoiding complications related to mechanical ventilation and general anesthesia, letting the patient resume his normal life sooner. Multiperforated intranasal catheter is a useful device in this purpose. Prospective randomized clinical trials are needed to confirm this hypothesis.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- 1.Galvez C, Bolufer S, Navarro-Martinez J, et al. Awake uniportal video-assisted thoracoscopic metastasectomy after a nasopharyngeal carcinoma. J Thorac Cardiovasc Surg 2014;147:e24-6. [DOI] [PubMed] [Google Scholar]
- 2.Pompeo E. eds. Awake thoracic surgery. Bentham Science Publishers, 2012:9-18. [Google Scholar]
- 3.Hung MH, Hsu HH, Cheng YJ, et al. Nonintubated thoracoscopic surgery: state of the art and future directions. J Thorac Dis 2014;6:2-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yang JT, Hung MH, Chen JS, et al. Anesthetic consideration for nonintubated VATS. J Thorac Dis 2014;6:10-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Walker WS, Leaver HA. Immunologic and stress responses following video-assisted thoracic surgery and open pulmonary lobectomy in early stage lung cancer. Thorac Surg Clin 2007;17:241-9, ix. [DOI] [PubMed] [Google Scholar]
- 6.Rocco G, Romano V, Accardo R, et al. Awake single-access (uniportal) video-assisted thoracoscopic surgery for peripheral pulmonary nodules in a complete ambulatory setting. Ann Thorac Surg 2010;89:1625-7. [DOI] [PubMed] [Google Scholar]