Abstract
OBJECTIVE
To analyze the causes of delay in hospital discharge of patients admitted to internal medicine wards.
METHODS
We reviewed 395 medical records of consecutive patients admitted to internal medicine wards of two public teaching hospitals: Hospital das Clínicas of the Universidade Federal de Minas Gerais and Hospital Odilon Behrens. The Appropriateness Evaluation Protocol was used to define the moment at which notes in the medical records indicated hospital stay was no longer appropriate and patients could be discharged. The interval between this estimated time and actual discharge was defined as the total number of days of delay in hospital discharge. An instrument was used to systematically categorize reasons for delay in hospital discharge and frequencies were analyzed.
RESULTS
Delays in discharge occurred in 60.0% of 207 hospital admissions in the Hospital das Clínicas and in 58.0% of 188 hospital admissions in the Hospital Odilon Behrens. Mean delay per patient was 4.5 days in the former and 4.1 days in the latter, corresponding to 23.0% and 28.0% of occupancy rates in each hospital, respectively. The main reasons for delay in the two hospitals were, respectively, waiting for complementary tests (30.6% versus 34.7%) or for results of performed tests to be released (22.4% versus 11.9%) and medical-related accountability (36.2% versus 26.1%) which comprised delays in discussing the clinical case and in clinical decision making and difficulties in providing specialized consultation (20.4% versus 9.1%).
CONCLUSIONS
Both hospitals showed a high percentage of delay in hospital discharge. The delays were mainly related to processes that could be improved by interventions by care teams and managers. The impact on mean length of stay and hospital occupancy rates was significant and troubling in a scenario of relative shortage of beds and long waiting lists for hospital admission.
Keywords: Patient Discharge; Length of Stay; Bed Occupancy; Hospitals, Teaching
INTRODUCTION
Remaining in hospital beyond the necessary time has long been a concern, contributing, as it does, to reduced care quality and increased costs.13 Moreover, keeping the user within the health care system keeps them away from family and community life, as well as exposing them to avoidable risks such as hospital infection, depression, loss of physical conditioning, deep vein thrombosis and falls.
Delays in hospital discharge (HD) occur in the majority of hospitals (rates vary between 13.5% and 62.0%).2,4,17
Concern with the costs resulting from inappropriate use of hospital beds designated for acute care appeared at the end of the last century.25 A study in 199116 showed an increase in hospital stays in Canada and in the United States, attributed to the growing number of chronic patients dependent on non-hospital care occupying beds that should have been used for the care of acute patients.
There should be concern to discover the reasons for delayed HD for every hospitalization. Identifying the problem is the first stage in seeking a solution. Changes in work processes may result in decreased HD delays, with no need for financial investments in structure.5
Studies have identified causes and measured days of delay in HD4,16,20 and proposed methods for quantifying the number of unnecessary days of hospitalization.
The instrument that has been most widely tested and validated in various countries for measuring the appropriateness of hospitalizations and hospital stays is the Appropriateness Evaluation Protocol (AEP).8,17,27 This instrument has been shown to be reliable and to have good inter- and intra-observer concordance.17
Despite the importance of identifying and minimizing the factors that unnecessarily prolong hospital stays, there are few studies categorizing the factors that prevent the HD of patients with a stabilized clinical situation.4,22
The aim of this study was to analyze the causes of delays in hospital discharge for patients admitted to internal medicine wards.
METHODS
The study was conducted in two large public teaching hospitals that only treated patients from the Brazilian Unified Health System, in the city and metropolitan area of Belo Horizonte, MG Southeastern Brazil. The hospitals studied were: Hospital das Clínicas da Universidade Federal de Minas Gerais (HC), a university hospital which admits patients from its ER and, as it is a high complexity reference hospital with various specialties, it also takes patients from other institutions after evaluation by the central bed regulator; and the Hospital Odilon Behrens – HOB), which is a local authority hospital, the emergency services of which play an important role in the municipal network and which refers the majority of patients admitted. Both hospitals have specialist outpatient departments that provide continuity of care post-discharge.
A pilot study was conducted to assess concordance in application of the AEP between researchers, using medical records of patients who had been discharged from January 1, 2010 onwards, consecutively, until the n calculated for this end (30 patients) was reached. These medical records were not used in the following stage of the study.
During the pilot project, there was concordance in the application of the AEP, with kappa of 0.53, 0.59 and 0.66.
In both hospitals, a rate of 20.0% delay in HD was considered when calculating the sample size. Thus, a sample of 174 medical records per hospital was calculated, with a 90% confidence level and 5% limits of confidence.
The consecutive medical records of patients discharged from hospital between January 1, 2010 and March 19, 2010 were evaluated by three researchers.
We selected the medical records of patients for whom internal medicine was the responsible medical specialty.
There were 207 medical records analyzed for patients admitted to the HC and 188 from the HOB, after exclusion of 21 and 9 medical records, respectively. The most common reasons for exclusion in the HC and the HOB were, respectively, the activities of internal medicine classified as consultation (28.6% and 55.5%), the same medical record being analyzed more than once, due to filing errors (47.6% and 11.1%) and the medical record being dated before the start period of the study (4.8% and 33.4%).
The instrument used to identify the moment at which delays in hospital discharge begin was the Portuguese version of the AEP, validated for Portugal.6,21,29,30
The AEP is a form divided into two parts. The first part assesses the patient’s clinical state (vital signs, neurological alterations with acute onset of paralysis in any part of the body, alterations in consciousness, vision or hearing). Changes in complementary tests such as electrocardiograms and ion determinations are also analyzed. The second part assesses need for clinical care, such as administering intravenous medication, monitoring vital data every two hours or administering intra-muscular medication every eight hours.
Exception criteria (criteria not included in the original AEP, but justifying hospitalization) were defined, considering the local situation. Such criteria are provided for in the instrument itself and should be used to avoid regional difficulties interfering with the application of the instrument.
The exception criteria were: dyspnea of unknown etiology with oxygen saturation < 92.0% in room air, need for micronebulization at ≤ 4 hour intervals or the presence of extensive skin lesions (Steven Johnson Syndrome and pressure ulcers).
Hospital stay was considered appropriate when any criteria from the AEP or in the exception criteria were present.
HD was deemed possible when the patient no longer met any of the AEP criteria or the exception criteria.
Discharge was deemed to take place on the day the patient left the hospital and the bed became available for occupation by another patient.
Deaths and transfers to other departments or hospitals were considered medical hospital discharge.
The days of delay in hospital discharge were calculated as the difference between the date of hospital discharge taking place and the day on which it had been deemed possible.
The form with the reasons for HD delays was completed based on the categories drawn up by Selker et al in 1989:22 patients awaiting complementary tests; patients awaiting the results of complementary tests; patients awaiting surgical procedures; patients awaiting specialist consultations; delays concerning medical-related accountability (patients hospitalized for complementary tests to be performed, HD depending on discussion with the care team/preceptor for a clinical decision to be made and the existence of outpatient care); delays related to poor planning for discharge or to awaiting extra-hospital care to be arranged; non-viable level of appropriate care or unavailable extra-hospital resources, including availability of long-term or palliative care beds or rehabilitation, patients awaiting transfer to intensive care or admission to another program or in-home care or awaiting transfer to other departments within the same hospital. This last category also included inadequate family support.
Pearson’s Chi-square test and Mann-Whitney and Kruskal-Wallis non-parametric tests were used in the statistical analysis.1,12,14,18
Bootstrap resampling7 was used to calculate the confidence intervals of days of delay in HD, mean hospital stay and occupation rate due to HD delays. The software programs used were Excel 2010, SPSS 15.0 and R 2.7.1.
The research project was approved by the Research Ethics Committees of the Universidade Federal de Minas Gerais and the HOB (HOB FR - 300143, on February 11, 2010; UFMG Record ETIC 0536.0.203.000-09, April 8, 2011).
RESULTS
The characteristics of the samples from the two hospitals were similar. The age of the patients in HC ranged between 13 and 92. Mean age was 55.9 (SD: 19.2 years) with a median of 57 (age was not noted for five patients), 58.0% were female and 42.0% male. Thirty-two patients died, the mortality rate was 16.0% (95%CI 9.0;23.0). The mean and median ages at HOB were similar to those at HC (58.1, SD: 18.5 years and 58 years old, respectively), with ages ranging between 13 and 95; 37.5% were female and 62.5% male. Sixteen patients died, the mortality rate was 9.0% (95%CI 2.0;16.0).
Some patients were admitted more than once during the study period, which meant that the number of hospitalizations was greater than the number of patients.
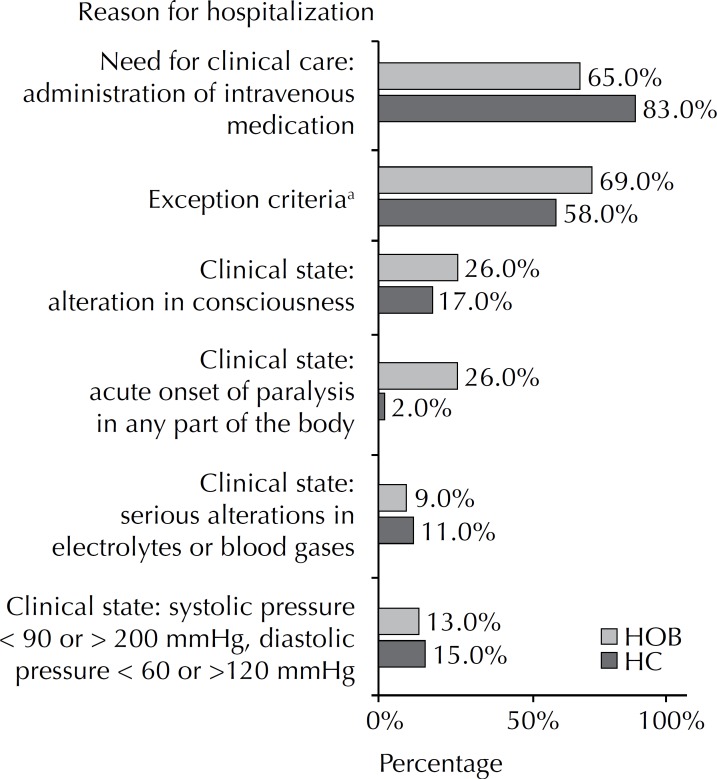
Some patients had more than one reason, according to the AEP, justifying their hospital stay (Figure 1).
Figure 1.
Reasons for hospital stay in internal medicine care wards in two public teaching hospitals. Minas Gerais, Southeastern Brazil, January to March 2010.
HC: Hospital das Clínicas da Universidade Federal de Minas Gerais
a Some patients met more than one criteria for hospitalization.
HD delays were found in 60.0% of HC hospitalizations (95%CI 53.0;67.0), corresponding to 23.0% (95%CI 18.0;27.0) of the occupation rate. This latter figure was estimated using bootstrap resampling,7 as the data (days of delay) did not have normal distribution. Of the 117 patients who experienced a delay in HD, there was one cause of delay in 33.4% cases, 46.1% had more than one cause and 20.5% between four and six causes. The 196 hospitalization analyzed corresponded to 190 patients, as six patients were hospitalized more than once during the period.
The total days of hospitalization in HC was 3,869, of which 22.3% were because of delays.
The mean hospital stay in HC was 20.4 days (95%CI 17.2;23.3), but would be 15.9 days (95%CI 12.9;18.5) if the mean delay of 4.5 days (95%CI 3.5;5.5) were discounted.
A 58.0% (95%CI 51.0;65.0) percentage of delay in HD was found in HOB, using binomial distribution of the patients, corresponding to a 28.0% occupation rate (95%CI 22.0;34.0), interval constructed using bootstrap resampling.7 Of the 102 patients who experienced a delay in HD, 34.3% had one cause, 55.9% more than one cause and 9.8% had four or five causes.
The total days of hospitalization of the HOB sample was 2,567 and HD delays were found in 28.35% of days.
Mean hospital stay in the HOB, without calculating delays, was 10.5 days (95%CI 8.4;12.9). A mean delay of 4.1 days (95%CI 3.2;5.1) was calculated and the mean stay increased to 14.6 days.
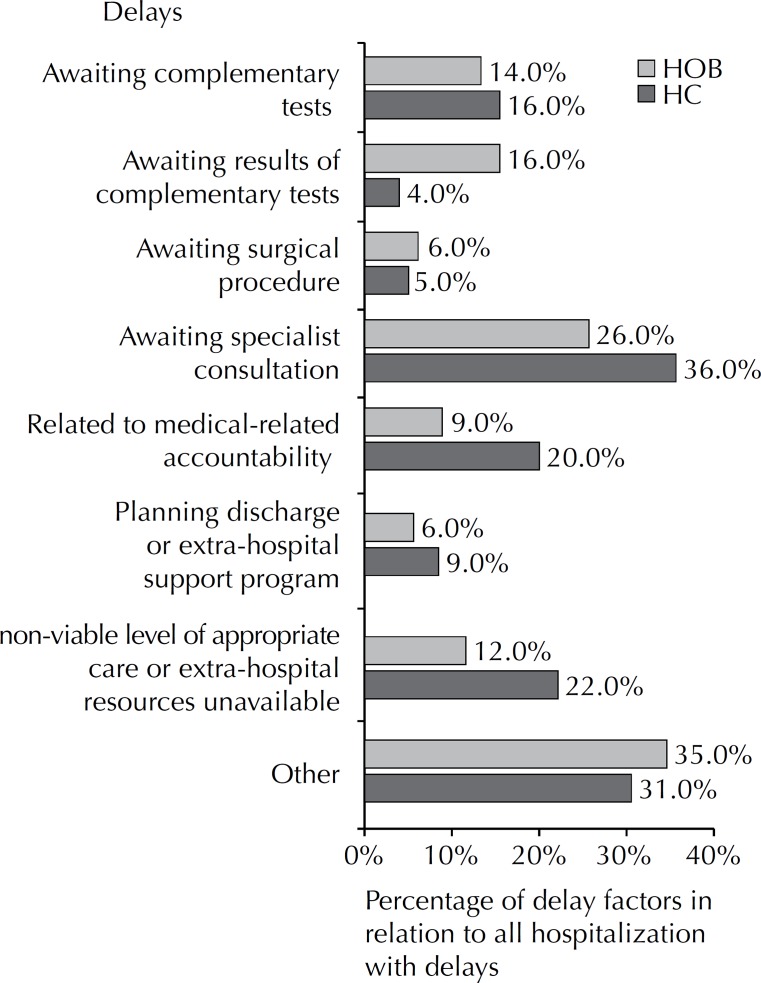
The causes for delays in HD are shown in Figure 2. It adds up to more than 100% because some patients experienced more than one cause of delay.
Figure 2.
Delay factors in hospital discharge in internal medicine wards of two public teaching hospitals. Minas Gerais, Southeastern Brazil, January to March 2010.
HOB: Hospital Odilon Behrens; HC: Hospital das Clínicas da Universidade Federal de Minas Gerais
There was no association between patient’s age and the number of days of delay in HD in either of the hospitals analyzed.
Figure 3 shows mean days of delay according to reason for delay.
Figure 3.
Mean days of delay in hospital discharge in internal medicine wards of two public teaching hospitals, according to cause of delay. Minas Gerais, Southeastern Brazil, January to March 2010.
HOB: Hospital Odilon Behrens; HC: Hospital das Clínicas da Universidade Federal de Minas Gerais
DISCUSSION
This study was the first time the AEP was used in this environment to analyze appropriateness of hospital stays, and it found a significant rate of HD delay (> 50.0%) in both of the hospitals analyzed. This delay was equivalent to 23.0% (HC) and 28.0% (HOB) of the occupation rate. These rates of delay are among the highest found in the literature.3-6,10,11,1 3,19,20
The main reason for hospital stays was prescription of intravenous medication. According to the guidelines for using the AEP,8 the use of intravenous infusions to maintain venous access was not considered criteria of appropriateness for hospital stay. However, it was observed that intravenous hydration was prescribed for hydrated, normotensive patients without electrolyte disturbances and with established oral or enteral routes. Such inappropriate recommendations for intravenous hydration were deemed appropriate criteria for hospital stay. The percentage of delays in HD in both hospitals would have been even higher if these situations were classified as inappropriate stay, which increases still more the relevance of this problem.
Some causes of delays in HD, such as waiting for appropriate extra-hospital care to be set up, or for surgical procedures, were infrequent but, when they occurred, led to several days of delay. Inadequate coordination between points of the care network may explain these delays. Delays in performing complementary tests and in releasing test results led to small delays, but were very common. To decrease days of unnecessary hospitalization, the approach needs to cover not only internal work processes but also those related to other segments of the care network.
Some patients experienced various causes of delays in HD, making a multi-professional approach a priority.
Three causes of delays in HD, represented by time awaiting complementary tests, awaiting the results of tests and waiting for the preceptor/care team to make clinical decisions, were responsible for the majority of days of delay in HD. These results differ from those of studies conducted in other countries,3,4,9,11,17,20,23,24,26 in which the causes of delays in HD were most frequently related to difficulty in organizing continuity of care for the patient in an extra-hospital environment and to social problems such as lack of family support. This difference may be explained by more efficient infrastructure and processes for performing complementary tests in the institutions participating in the cited studies.
Brazil has serious social problems, a significant part of the population live in extreme poverty with limited access to health care services. Difficulties in providing post hospital discharge care may be a significant cause of HD delays. Inadequate recording of such situations on the medical record may have minimized the impact of social issues as a cause of HD delays.
Delays related to education, training or research are no longer adopted in Selker et al,22 guidelines setting out categories of HD delays. Researchers argue that such patients are no longer hospitalized due to current financial pressures. These situations are still found, above all in teaching hospitals, and may have been underestimated in this study, being included in the category of patients awaiting complementary tests.
Comparison between HOB and HC shows the importance of each institution being aware of its causes of HD delays. Despite the percentage of delays being similar in the two hospitals, the impact of each cause of HD delay was different, requiring the prioritization of different actions to be taken in each hospital.
The reality within a teaching hospital is different to that of other public and private hospitals in the country. The data from this study may not be applicable to other Brazilian health care institutions, although they do confirm the international fact that HD delays exist and that the causes differ from hospital to hospital.4,15,17,23,26-28 This means that this type of study is useful in supporting administrators’ decision making.
The AEP has not yet been validated for use in Brazil, which may be a limitation of this study. The use of the exception criteria minimize issues related to local peculiarities, but these criteria were also used for the first time in the hospitals analyzed and were based on the opinions of experienced doctors. The study was conducted in two teaching hospitals, which may imply selection bias.
Delays were mainly due to process-related factors (performing and releasing results of complementary tests) which could be improved by interventions by the care and management teams, without requiring significant financial investment. The desired results are increased care capacity and reduced costs and exposure of patients to risks related to unnecessary hospital stay.
HIGHLIGHTS
This article studied the reasons for hospitalized patients in stable clinical conditions remaining in hospital, increasing costs and the risk of adverse events related to unnecessary hospitalization.
In the two hospitals analyzed, delays in discharge were mainly due to process related factors (conducting complementary tests or releasing test results) which could be improved through care team or management interventions, with no need for significant financial investment. The desired results would be increased care capacity, reduced costs and decreased exposure of patients to risks related to unnecessary hospitalization.
Significant delays in hospital discharges (58.0% and 60.0%) were found. Mean delays were 4.1 days in one hospital and 4.5 days in the other.
The principle reasons for delays in both hospitals were: waiting for complementary tests to be done (30.6% x 34.7%) or for test results to be released (22.4% x 11.9%) and related to medical liability (36.2% x 26.1%), including delays discussing clinical cases and making clinical decisions and in providing specialized consultation (20.4% x 9.1%).
Professor Rita de Cássia Barradas Barata Scientific Editor
Footnotes
Article based on the master’s dissertation of Silva SA, entitled: “Fatores de atraso na alta hospitalar de dois hospitais públicos da cidade de Belo Horizonte, Minas Gerais”, presented to the Universidade Federal de Minas Gerais, in 2011.
The authors declare that there is no conflict of interest.
REFERENCES
- 1.Agresti A. Categorical Data Analisys. New Jersey: John Wiley and Sons; 2002. [Google Scholar]
- 2.Anderson P, Meara J, Brodhurst S, Attwood S, Timbrell M, Gatherer A. Use of hospital beds: a cohort study of admissions to a provincial teaching hospital. BMJ. 1998;297(6653):910–912. doi: 10.1136/bmj.297.6653.910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Apolone G, Fellin G, Tampieri A, Bonanoni E, Crosti PF, Lanzi E, et al. Appropriateness of hospital use. Report from an Italian study. Eur J Public Health. 1997;7(1):34–39. doi: 10.1093/eurpub/7.1.34. [DOI] [Google Scholar]
- 4.Carey MR, Sheth H, Braithwaite S. A prospective study of reasons for prolonged hospitalizations on a general medicine teaching service. J Gen Intern Med. 2005;20(2):108–115. doi: 10.1111/j.1525-1497.2005.40269.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chopard P, Perneger TV, Gaspoz JM, Lovis C, Gousset D, Rouillard C, et al. Predictors of inappropriate hospital days in a department of internal medicine. Int J Epidemiol. 1998;27(3):513–519. doi: 10.1093/ije/27.3.513. [DOI] [PubMed] [Google Scholar]
- 6.Cordero A, Áquila A, Massalana A, Escoto V, Susano R. Adequação dos internamentos num serviço de medicina-Aplicação da escala Appropriateness Evaluation Protocol. Acta Med Port. 2004;17(2):113–118. [PubMed] [Google Scholar]
- 7.Efron B. Booststrap methods:another look at the Jakkinife. Ann Stat. 1979;7(1):1–235. doi: 10.1214/aos/1176344552. [DOI] [Google Scholar]
- 8.Gertman PM, Restuccia JD. The appropriateness evaluation protocol: a technique for assessing unnecessary days of hospital care. Med Care. 1981;19(8):855–871. doi: 10.1097/00005650-198108000-00005. [DOI] [PubMed] [Google Scholar]
- 9.Jasinarachchi KH, Ibrahim IR, Keegan BC, Mathialagan R, McGourty JC, Phillips JRN, et al. Delayed transfer of care from NHS secondary care to primary care in England: its determinants, effect on hospital bed days, prevalence of acute medical conditions an deaths during delay, in older adults aged 65 years and over. BMC Geriatr. 2009;9:4. doi: 10.1186/1471-2318-4-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kossovsky MP, Chopard P, Bolla F, Sarasin P, Louis-Simonet M, Allaz AF, et al. Evaluation of quality improvement interventions to reduce inappropriate hospital use. Int J Qual Health Care. 2002;14(3):227–232. doi: 10.1093/oxfordjournals.intqhc.a002614. [DOI] [PubMed] [Google Scholar]
- 11.Lambert J, Panis GG, Verheggen FWSM, Pop P. To stay or not stay. The assessment of appropriate hospital stay: a Dutch report. Int J Qual Health Care. 2002;14(1):55–67. doi: 10.1093/intqhc/14.1.55. [DOI] [PubMed] [Google Scholar]
- 12.Lehmam EL, Abrera HJ. Nonparametrics: statistical methods based on ranks. New Jersey: Prentice Hall; 1998. [Google Scholar]
- 13.Lim SC, Doshi V, Castasus B, Lim JKH. Factors causing delay in discharge of elderly patients in a acute care hospital. Ann Acad Med Singapore. 2006;35(1):27–32. [PubMed] [Google Scholar]
- 14.Magalhães MN, Lima A. Noções de probabilidade e estatística. São Paulo: Edusp; 2002. [Google Scholar]
- 15.Maguire PA, Taylor IC, Stout R. Elderly patients in acute medical wards: factors predicting length of stay in hospital. Br Med J. 1986;292(6530):1251–1253. doi: 10.1136/bmj.292.6530.1251. Clin Res Ed. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McClaran J, Tover-Berglas R, Glass KC. Chronic status patients in a university hospital: bed-day utilization and length of stay. CMAJ. 1991;145(10):1259–1265. [PMC free article] [PubMed] [Google Scholar]
- 17.McDonagh SM, Smith DH, Goddard M. Measuring appropriate use of acute beds: a systematic review of methods and results. Health Policy. 2000;53(3):157–184. doi: 10.1016/S0168-8510(00)00092-0. [DOI] [PubMed] [Google Scholar]
- 18.Montgomery DC. Design and analysis of experiments. New York: John Wiley & Sons; 2001. [Google Scholar]
- 19.Navarro G, Prat-Marin A, Asenjo MA, Menacho A, Trilla A, Salleras LL. Review of utilization of a university hospital in Barcelona (Spain): evolution 1992-1996. Eur J Epidemiol. 2001;17(7):679–684. doi: 10.1023/A:1015563618836. [DOI] [PubMed] [Google Scholar]
- 20.Panis LJGG, Gooskens M, Verheggen FWSM, Pop P, Prins MH. Predictors of inappropriate hospital stay: a clinical case study. Int J Qual Health Care. 2003;15(1):57–65. doi: 10.1093/intqhc/15.1.57. [DOI] [PubMed] [Google Scholar]
- 21.Rodriquez-Vera J. Appropriateness Evaluation Protocol 1997-2007: experiência em dois países. Barvalento Med. 2008;1(1):8–18. [Google Scholar]
- 22.Selker HP, Beshansky JR, Pauker SG, Kassirer JP. The epidemiology of delays in a teaching hospital. The development and use of a tool that detects unnecessary hospital days. Med Care. 1989;27(2):112–129. doi: 10.1097/00005650-198902000-00003. [DOI] [PubMed] [Google Scholar]
- 23.Semke J, VanDer Weele T, Weatherley R. Delayed discharge for medical and surgical patients in an acute care hospital. Soc Work Health Care. 1989;14(1):15–31. doi: 10.1300/J010v14n01_02. [DOI] [PubMed] [Google Scholar]
- 24.Simonet ML, Kossovsky MP, Chopard P, Siud P, Perneg TV, Gospoz JM. A predictive score to identify hospitalized patients risk of discharge to a post-acute care facility. BMC Health Serv Res. 2008;8:154. doi: 10.1186/1472-6963-8-154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Smeets PMJH, Verheggen FWSM, Pop P, Panis LJGG, Carpay JJ. Assessing the necessity of hospital stay by means of Appropriateness Evaluation Protocol: how strong is the evidence to proceed? Int J Qual Health Care. 2000;12(6):483–493. doi: 10.1093/intqhc/12.6.483. [DOI] [PubMed] [Google Scholar]
- 26.VanStraten A, van der Meulen JHP, van der Bos GAM. Lenght of hospital stay and discharge delay in stroke patients. Stroke. 1997;28(1):137–140. doi: 10.1161/01.STR.28.1.137. [DOI] [PubMed] [Google Scholar]
- 27.Vetter N. Inappropriately delayed discharge from hospital: What do we know? BMJ. 2003;326(7395):927–928. doi: 10.1136/bmj.326.7395.927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Victor CR, Healy J, Thomas A, Seargeant J. Older patients and delayed discharge from hospital. Health Soc Care. 2000;8(6):443–452. doi: 10.1046/j.1365-2524.2000.00270.x. [DOI] [PubMed] [Google Scholar]
- 29.Vieira NB, Rodriguez-Vera J, Ferrão E, Taveira T, Monteiro L, Grade MJ, et al. Adequação do internamento num serviço de medicina interna utilizando o Appropriateness Evaluation Protocol (AEP) Acta Med Port. 2006;19(1):67–70. [PubMed] [Google Scholar]
- 30.Vieira NB, Rodriguez-Vera J, Grade MJ, Arez L, Santos RTC. Adequação das admissões hospitalares num serviço de medicina interna utilizando o Appropriateness Evaluation Protocol (AEP) durante o ano de 2004. Med Interna. 2006;131(41):235–240. [Google Scholar]