A tele-intensive care unit (tele-ICU) uses telemedicine, in an intensive care unit (ICU) setting, to care for critically ill patients by off-site clinical resources. This literature review examined a large number of studies of implementation in hospitals. The evidence supporting cost savings was mixed. Implementation of a tele-ICU system was associated with cost savings, shorter lengths of stay, and decreased mortality. However, two studies suggested increased hospital cost after implementation. Intensivists working these systems are able to more effectively treat ICU patients, providing better clinical outcomes for patients at lower costs compared with hospitals without a tele-ICU.
Abstract
Objectives:
A tele-intensive care unit (tele-ICU) uses telemedicine in an intensive care unit (ICU) setting, applying technology to provide care to critically ill patients by off-site clinical resources. The purpose of this review was to examine the implementation, adoption, and utilization of tele-ICU systems by hospitals to determine their efficiency and efficacy as identified by cost savings and patient outcomes.
Methods:
This literature review examined a large number of studies of implementation of tele-ICU systems in hospitals.
Results:
The evidence supporting cost savings was mixed. Implementation of a tele-ICU system was associated with cost savings, shorter lengths of stay, and decreased mortality. However, two studies suggested increased hospital cost after implementation of tele-ICUs is initially expensive but eventually results in cost savings and better clinical outcomes.
Conclusions:
Intensivists working these systems are able to more effectively treat ICU patients, providing better clinical outcomes for patients at lower costs compared with hospitals without a tele-ICU.
Introduction
Telemedicine is the use of medical information exchanged from one site to another via electronic communications to improve a patient’s clinical health status. Telemedicine includes a growing variety of applications and services using twoway video, smart phones, wireless tools, and other forms of telecommunications technology.1 A tele-intensive care unit (tele-ICU) involves the use of telemedicine in an intensive care unit (ICU), using technology to assist in providing care for critically ill patients by off-site clinical resources.2
In the US, more than 4 million patients are admitted to ICUs each year; treatment of these critically ill patients has been estimated to account for 30% of costs of acute care hospitals.3,4 Patient safety concerns persist in the ICU, and serious medication errors account for 78% of all errors in the ICU.5 Hospital costs for critically ill patients have been estimated to be about $67 billion annually, with mortality rates ranging from 10% to 28%, or approximately 540,000 deaths each year.6–8
Tele-ICUs may be effective by decreasing costs, decreasing ICU length of stay (LOS), decreasing medication errors, and increasing patient safety when adopted and implemented in hospitals. Two distinct types of tele-ICU have been identified. The decentralized tele-ICU is a medical facility or multiple medical facilities that can be accessed from remote sites such as office, home, or mobile. There is no distinct tele-ICU; rather there is a process of care having multiple sites of access to the patient, with intensivists monitoring the patients. A centralized tele-ICU program is often the tele-ICU system of choice. In the centralized system, one central ICU provides intensive care via telemedicine and remote monitoring to several satellite ICUs.
In the tele-ICU model, the tele-ICU is a definable entity providing continuous monitoring to sites with high levels of need via private, dedicated telecommunications lines.9 Networks of audiovisual communication and computer systems link hospital ICUs to intensivists and other critical care professionals, who are able to access patient data such as medical records, to conduct remote real-time monitoring of vital signs or chronic conditions, or to facilitate staff interactions via video, phone, or online computer. Video cameras located on the ceiling of an ICU patient room are situated to allow telemedicine practitioners to observe equipment and monitors in the patient’s room. Cameras often have an alert system to announce that the tele-ICU staff is in visual contact to share observations and care recommendations with bedside caregivers.10 These devices and elements are vital to the successful application of tele-ICUs. As has been noted, without appropriate electronic medical records and clinical decision support systems, or lacking patient-related data and information, clinicians may make inappropriate treatment recommendations.11
Studies have demonstrated both clinical and economic benefits associated with adoption of tele-ICUs, including decreased mortality rate, decreased frequency of ICU complications, decreased ICU LOS and decreased ICU costs after a 16-week implementation of technology-enabled remote care.12–14 Additionally, it has been found that tele-ICU use can decrease medication errors and improve patient safety.11 A meta-analysis of non-severity-adjusted data from 11 studies confirmed these results and found the decrease of ICU mortality and ICU LOS, as well as hospital mortality and hospital LOS to be statistically significant.15 These outcomes are particularly important because studies that reported results on the basis of both severity-adjusted data and non-severity-adjusted data have found that the level of statistical significance of these outcome variables when using non-severity-adjusted data was higher than when using severity-adjusted data.16,17 These findings indicate that the benefits of tele-ICU implementation reach all populations of patients, regardless of severity of illness.
It has been estimated that full implementation of the tele-ICU standard in community hospitals could prevent between 5400 and 13,400 deaths and could potentially save $5.4 billion annually.18,19
One of the main barriers to adoption of tele-ICUs has been adoption and implementation cost: the cost of construction, installation, and training. The “command center” for a tele-ICU system has been estimated to cost between $2 and $5 million, with each additional tele-ICU added to the system costing $250,000.20 Such substantial financial outlays can be a challenge for hospitals and health systems that lack significant financial funds or borrowing capacity, especially with annual operating costs of about $2 million, including maintenance costs, licenses, staffing expenses, and additional upgrades.21 If the tele-ICU system is not fully compatible with the hardware or software systems of the physical ICU, additional software, hardware, and infrastructure may be required, which would require additional cost to the hospital.
Regardless of the need for upgrades, staff must overcome additional barriers such as computer issues, including difficulty logging on, short battery life, frequent rebooting, and other technical issues with computers or software. Some of the possible solutions for these problems include ensuring computers remain plugged in, confirming that passwords are able to be used in multiple programs, and providing information technology (IT) assistance by phone and on-site as required.22
Although tele-ICUs are expensive to implement, with startup costs between $50,000 and $100,000 per bed, the benefits of tele-ICU utilization may far outweigh those costs for ICUs. Because ICU patients frequently have such complex medical and/or surgical conditions, intensive care provided via a tele-ICU system can provide this care and decrease hospital cost.23
The purpose of this review was to examine the implementation, adoption, and utilization of tele-ICU systems by hospitals to determine their efficiency and efficacy as identified by cost savings and patient outcomes.
Methods
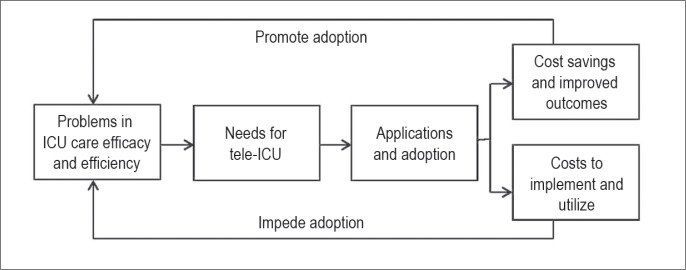
The methods employed for this study were a literature review and a review of case studies. The research approach for the examination of the promotion factors and barriers to adoption of tele-ICUs was customized to this study following the conceptual framework used by Yao et al24 (Figure 1). Figure 1 depicts the process of IT adoption in health care, in this case, the tele-ICU. To research how tele-ICU can help improve health care practices in the ICU, it is first necessary to recognize the existing problems in the ICU and issues that drive and impede adoption of this technology by the hospital industry; then different applications can be identified to solve or partially unravel these challenges. By analyzing the literature, the benefits and barriers of tele-ICU utilization in health care can be identified (Figure 1). The use of this framework in the current study is appropriate because the focus of this study, as in that by Yao et al,24 is to show how new technologies and IT systems can be applied to health care settings to enhance the care of patients. In addition, this conceptual approach has been successfully replicated in previous studies, including adoption of tele-ICU, radiofrequency identification, and electronic prescribing technologies, thus supporting its internal validity.25–27
Figure 1.
Research framework.
ICU = intensive care unit.
The review was conducted in stages, including: 1) determining the search strategy and establishing inclusion and exclusion criteria, 2) literature analysis, and 3) extracting and categorizing the findings.
Step 1: Determining the Search Strategy and Establishing Inclusion and Exclusion Criteria
When executing the search, the following terms were used: “tele-ICU” or “telemedicine ICU” or “virtual ICU” and “cost” or “benefits.” A mix of databases and online sources were used to compile a set of references covering both academic peer-reviewed research and practitioner literature. It was believed that this approach would help create the most comprehensive and up-to-date review. The following electronic databases and sources were used: PubMed, Academic Search Premier, Science Direct, ProQuest, and Google Scholar. The Web sites of the Society of Critical Care Medicine and the American Telemedicine Association also were searched.
Step 2: Literature Analysis
The literature review yielded 76 sources, which were assessed for information pertaining to this research project. Given the technology- and enterprise-oriented nature of the current study, literature was selected for review on the basis of financial, technological, and organizational impacts. References were reviewed and determined to have satisfied the inclusion criteria if the material provided accurate information about the tele-ICU with a particular focus on benefits and barriers to its implementation. Only articles that were written in English were included for review. Given the rapid changes in technology, studies that were published before 2001 were excluded from the search.
Step 3: Literature Categorization
In the third step, selected academic articles and practitioner health IT sources were analyzed, and relevant categories were identified. The findings are presented in the subsequent sections using the categories of cost of telemedicine technology in the ICU and several case studies. The use of brief case studies was thought to illustrate real cases of tele-ICU implementation.
Results
How Tele-ICUs Can Be Cost-Effective
According to the leading tele-ICU systems vendor, Philips VISICU in Baltimore, MD, tele-ICU implementation costs ranged from about $50,000 to $100,000 per bed, and the cost of equipping 100 beds was approximately $3 to $5 million.28,29 Annual operating costs (eg, overhead, maintenance, staffing) were estimated by Philips VISICU to be approximately 20% of the software costs, or about $300,000 for 100 beds.30 Staffing costs depended on hours in use and level of additional staff in the off-site center; typical staffing scenarios added approximately $1 to $2 million per year per 100 beds covered.31
Brief Case Study 1: Sentara Healthcare
Sentara Healthcare in Norfolk, VA, was the nation’s first health system to establish a tele-ICU program in 2000 through the vendor VISICU (now Philips VISICU).32 Implementation of the tele-ICU at Sentara Norfolk General Hospital and Sentara Hampton General Hospital took 5 months and cost more than $1 million. In 2002, Sentara reported a reduction in hospital mortality of 26%, with a 17% decrease in ICU LOS (Table 1).33
Table 1.
Tele-intensive care unit cases studied, implementation costs, and outcomes
| Institution | Setting | Implementation costs (US dollars) | Major results/outcomes |
|---|---|---|---|
| Sentara Healthcare | Sentara Healthcare,a academic tertiary care medical center with 5 ICUs, 103 critical care beds | 1 million | Decreased ICU LOS by 17%; decreased hospital mortality by 26.4%33,36 |
| New England Healthcare Institute and Massachusetts Technology Collaborative | University of Massachusetts Memorial Medical Center, academic hospital with 5 adult ICUs, 130 beds, 7000 ICU patients | 7.12 million | Decreased ICU LOS (from 13.3 to 9.8 days); decreased mortality from 13.6% to 11.8%; recovered costs of implementation; lowered rates of complications36 |
| Resurrection Health Care | Community hospitals with 14 ICUs, 182 critical care beds Pre- and postimplementation design; preimplementation: n = 2034 patients; postimplementation: n = 2134 |
7 million | 6 months after implementation: 38% decrease in ICU LOS, approximately $3 million in cost savings37,38 |
Includes both Sentara Norfolk General Hospital and Sentara Hampton General Hospital.
ICU = intensive care unit; LOS = length of stay.
Findings from an independent evaluation by Cap Gemini Ernst & Young, London, United Kingdom, suggested a $2 million tele-ICU cost that was offset by $3 million in net savings annually.33 It reported extra revenue, approximately $460,000 per month, because of increased patient turnover resulting from decreased LOS.34 Table 2 displays the findings of the patient cost reduction of $2150 per stay based on reduced patient expenses and increased ICU capacity as well.
Table 2.
Sentara Healthcare and Resurrection Health Care tele-intensive care unit implementation savings
| Hospital | Cost of implementation (US dollars) | Outcomes | Cost saving |
|---|---|---|---|
| Sentara Healthcare (savings from 2002 to 2010) | 1 million | Reduction in mortality by 27%; decreased LOS of 17% | Reduced patient cost of $2150; average case contribution margina increased by 55.6%33,36 |
| Resurrection Health Care (savings from 2007 to 2011) | 7 million | Decreased LOS of 38% | 7% reduction in blood transfusions ($11,200 in savings); estimated total cost savings of $11.5 million37,38 |
Average case contribution margin is the selling price per unit minus cost per unit. Contribution represents the portion of sales revenue that is not consumed by variable costs and so contributes to the coverage of fixed costs.
LOS = length of stay.
The centralized model has allowed optimization of time and services of intensivists without the requirement of staffing intensivists at multiple locations. The availability of intensivists in a single location also has given patients the opportunity to stay in location, instead of traveling and being transferred to a different hospital.35 As of 2010, more than 1 million ICU patients had been cared for using the strategy of frequent reassessment, alert-prompted evaluation, and rapid response to clinical needs.34
Brief Case Study 2: University of Massachusetts Memorial Medical Center
The University of Massachusetts Memorial Medical Center in Worcester, MA, installed a tele-ICU command center in 2005 and extended the tele-ICU coverage to 2 Massachusetts community hospitals in 2007 and 2008. Over 3 years, 1 tele-ICU command center extended coverage to 9 adult ICUs covering 116 ICU beds in central Massachusetts.36
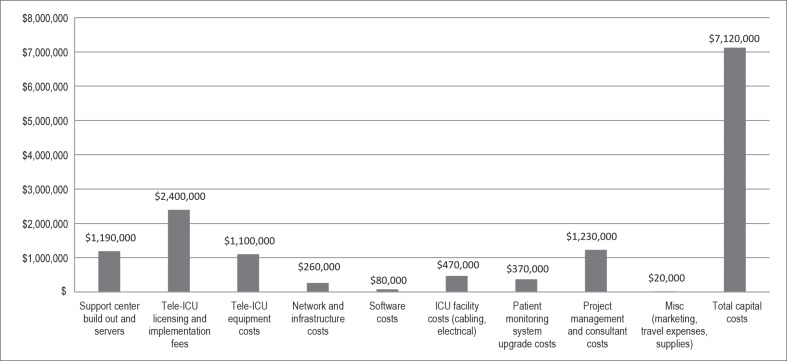
Figure 2 shows the initial expenses of implementation of a tele-ICU at the medical center. The total operating costs of $7.12 million also required an increment of annual operating cost of $3.15 million. Licensing and implementation fees accounted for 34% of the total expenses. Tele-ICU equipment costs and support center and servers accounted for $1.1 million and $1.19 million, respectively (Figure 2).
Figure 2.
University of Massachusetts Memorial Medical Center: one-time costs for tele-intensive care unit implementation, 2010.36
ICU = intensive care unit; Misc = miscellaneous.
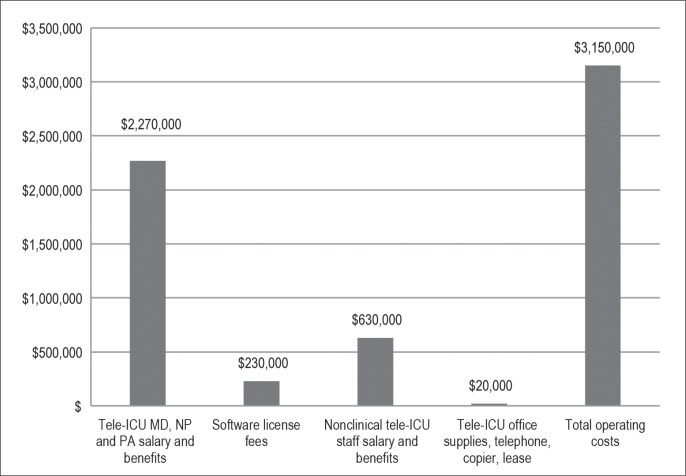
Figure 3 shows the operating costs and the continuous ongoing costs for the tele-ICU. The main ongoing cost was clinical salaries and benefits accounting for 72% or $2.27 million, followed by nonclinical salaries at 20% or $630,000 (Figure 3). The centralized tele-ICU program has been one of the most beneficial programs to the medical center. The positive net revenue produced a rapid payback such that total costs of implementation were recovered within 1 year.36
Figure 3.
University of Massachusetts Memorial Medical Center ongoing operating costs, 2010.36
ICU = intensive care unit; MD = physician; NP = nurse practitioner; PA = physician assistant.
Brief Case Study 3: Resurrection Health Care
Covering 7 acute care hospitals and a long-term care facility, Resurrection Health Care in Des Plaines, IL (now part of Presence Health), introduced telemedicine into its 14 ICUs in 2007. The tele-ICU command center in Resurrection’s Holy Family Medical Center (now Presence Holy Family Medical Center) promoted proactive intervention, including trended alerts, which showed incremental changes in such factors as blood pressure, oxygen levels, and drip rates.37
In the first 6 months after installation in 2007, a cost savings of $3 million was reported, including $11,200 from a 7% reduction in blood transfusions. The hospital found a 38% decrease in ICU LOS in 6 months, which totaled to approximately $3 million in savings (Table 2).
Resurrection Health Care leadership wanted to know how the system was going to prove its return on investment on the $7 million spent to set up all 14 ICU systems simultaneously. In 2011, it was reported that it had a $387,000 financial benefit: tele-ICU support for ICU patients across the health care system resulted in 9000 ICU days saved, for an estimated cost savings of $11.5 million. Also, it was reported that the reengineering of the existing tele-ICU infrastructure was expanded to support telestroke, telepsychiatry, telemedicine with skilled nursing facilities, and sepsis management initiatives.38
Brief Case Study 4: Six Intensive Care Units in Five Large Hospitals
A study by Franzini et al39 was conducted to determine the costs and cost-effectiveness of 6 ICUs in 5 large hospitals in the Gulf Coast region after the installation of a tele-ICU program. The sample included 4142 patients in the 6 different ICUs: 2034 patients were from the pretest period and 2108 were from the posttest period. Table 3 shows the ICU average daily cost before and after the tele-ICUs were implemented. The average daily costs and costs per case increased in all 6 ICUs after implementation (posttest period) from the period before implementation of the tele-ICU (pretest period). Overall, the daily average ICU cost increased from $2851 to $3653, or a 28% increase after tele-ICUs were installed, which was statistically significant. Two hospitals experienced cost increases greater than 30% (Table 3).39
Table 3.
Average daily costs (US dollars) before and after tele-ICU installation in six intensive care units in 201039
| Costs | Overall | ICU 1 | ICU 2 | ICU 3 | ICU 4 | ICU 5 | ICU 6 |
|---|---|---|---|---|---|---|---|
| Before tele-ICU period | 2851 | 2586 | 3647 | 4248 | 3155 | 2355 | 2370 |
| After tele-ICU period | 3653 | 3272 | 4307 | 4252 | 4131 | 3275 | 2746 |
| Change (%) | 802 (28) | 686 (27) | 660 (18) | 4 (0) | 976 (31) | 920 (39) | 376 (16) |
ICU = intensive care unit.
The floor daily average costs increased 16%, from $1451 to $1687, after tele-ICUs were installed. The overall ICU costs per case increased from $13,029 to $19,324 after tele-ICU installation.39
Costs per patient for hospitals increased, but the patient out-of-pocket expenses remained the same, causing the hospitals to need to find some way to absorb the financial losses of tele-ICU implementation. Average ICU hospital cost per patient was $20,231 in the pretest period and $25,846 in the posttest period, which was financially and statistically significant (Table 4). Overall, the installation of the tele-ICU programs in the 6 ICUs was associated with higher costs not attributable to medical inflation. These researchers did note that sicker patients exhibited lower mortality; thus ICUs with high volumes of severely ill patients may gain more financial benefit with the utilization of tele-ICU technology. The researchers also noted that about two-thirds of ICU physicians in the study chose only minimal participation in the tele-ICU intervention.
Table 4.
Intensive care unit costs per case (US dollars) before and after tele-ICU installation in six intensive care units in 201039
| Costs | Overall | ICU 1 | ICU 2 | ICU 3 | ICU 4 | ICU 5 | ICU 6 |
|---|---|---|---|---|---|---|---|
| Before tele-ICU period | 13,029 | 7422 | 12,912 | 26,296 | 8770 | 13,328 | 15,167 |
| After tele-ICU period | 19,324 | 10,797 | 18,519 | 33,594 | 19,002 | 15,392 | 18,947 |
| Change (%) | 6295 (48) | 3374 (45) | 5608 (43) | 7298 (28) | 10,232 (117) | 2065 (15) | 3780 (25) |
| Average cost: before tele-ICU period vs after tele-ICU period | 20,231 vs 25,846 |
ICU = intensive care unit.
Positive Outcomes of Tele-ICU Implementation
In terms of effectiveness, the literature on tele-ICUs demonstrated improved hospital financial performance, improved ICU financial performance, improved teamwork climate and safety climate, and improved patient care (Table 5).40–66 A tele-ICU program enhanced compliance to evidence-based practice bundles for severe sepsis. Between January 1, 2006, and December 31, 2008, antibiotic administration increased from 55% to 74%, serum lactate measurement increased from 50% to 66%, the initial fluid bolus of 20 mL/kg or greater increased from 23% to 70%, and central line placements increased from 33% to 50%.53 Higher rates of ICU staff adherence to critical care best practices, reduction of ICU LOS, and improved patient care were found in several studies (Table 5). Quality improvement and patient care have been improved by the implementation of the tele-ICU by increasing the use of evidence-based protocols for sepsis, ventilator-associated pneumonia, and blood transfusion (Table 5).67–70
Table 5.
Studies addressing tele-ICU implementation and utilization
| Author, year | Study design | Outcome |
|---|---|---|
| Aaronson et al, 200640 | Literature review | Higher rates of ICU staff adherence to critical care best practices |
| Badawi et al, 201041 | Pre/posttest of tele-ICU implementation | Higher rates of ICU staff adherence to critical care best practices |
| Badawi and Shemmeri, 200642 | Pre/posttest of tele-ICU implementation | Higher rates of ICU staff adherence to critical care best practices |
| Berenson et al, 200931 | Literature review | Improved patient care |
| Breslow et al, 200412 | Pre/posttest of tele-ICU implementation across several hospitals | Improved hospital financial performance, improved ICU financial performance, improved patient care |
| Chu-Weininger et al, 201043 | Pre/posttest of tele-ICU implementation and utilization in 3 ICUs | Improved teamwork and/or safety climate |
| Coletti et al, 200844 | Cross-sectional survey of residents in ICU and tele-ICUs | Improved teamwork and/or safety climate |
| Dickhaus, 200645 | Pre/posttest of tele-ICU implementation and utilization in a multistate hospital system | Lower ICU LOS |
| Giessel and Leedom, 200746 | Pre/posttest of tele-ICU implementation and utilization | Higher rates of ICU staff adherence to critical care best practices |
| Groves et al, 200813 | Literature review | Lower ICU LOS |
| Howell et al, 200747 | Pre/posttest of tele-ICU implementation and utilization | Lower ICU LOS |
| Howell et al, 200848 | Pre/posttest of tele-ICU implementation and utilization | Lower ICU LOS |
| Ikeda et al, 200967 | Pre/posttest of tele-ICU implementation and utilization | Lower ICU LOS |
| Kohl et al, 200749 | Pre/posttest of tele-ICU implementation and utilization | Lower ICU LOS |
| Kohl et al, 200750 | Pre/posttest of tele-ICU implementation and utilization | Improved ICU financial performance, lower ICU LOS |
| Kohl et al, 201216 | Pre/posttest of tele-ICU implementation and utilization | Lower ICU LOS |
| Kumar et al, 201351 | Literature review | Improved ICU financial performance |
| Khunlertkit and Carayon, 201311 | Qualitative study with semistructured interview of tele-ICU staff | Improved ICU staff adherence to evidence-based protocols for sepsis, ventilator-associated pneumonia, and blood transfusion |
| Lilly et al, 201117 | Pre/posttest of tele-ICU implementation and utilization | Higher rates of ICU staff adherence to critical care best practices, lower ICU LOS, improved patient care |
| Mora et al, 200752 | Survey of residents practicing in tele-ICUs | Improved patient care |
| Norman et al, 200953 | Literature review and meta-analysis | Improved ICU financial performance |
| Patel et al, 200754 | Pre/posttest of tele-ICU implementation and utilization of 6 tele-ICUs | Higher rates of ICU staff adherence to critical care best practices, lower ICU LOS |
| Rincon et al, 200755 | Pre/posttest of tele-ICU utilization in prevention of sepsis | Higher rates of ICU staff adherence to critical care best practices:
|
| Scales et al, 201156 | Literature review | Higher rates of ICU staff adherence to critical care best practices |
| Thomas et al, 200757 | Pre/posttest of tele-ICU implementation and utilization | Improved teamwork and/or safety climate |
| Vespa et al, 200758 | Pre/posttest of tele-ICU implementation and utilization | Improved ICU financial performance, lower ICU LOS, improved patient care |
| Wilcox and Adhikari, 201215 | Meta-analysis of 11 studies | Lower ICU LOS |
| Willmitch et al, 201259 | Pre/posttest of tele-ICU implementation and utilization over 3 years | Lower ICU LOS |
| Youn, 200660 | Literature review and meta-analysis | Higher rates of ICU staff adherence to critical care best practices |
| Young et al, 201161 | Meta-analysis of 11 studies | Lower ICU LOS |
| Zawada et al, 200662 | Survey of physicians practicing in remote areas using tele-ICU | Higher rates of ICU staff adherence to critical care best practices, lower ICU LOS |
| Zawada et al, 200763 | Pre/posttest of tele-ICU implementation and utilization | Improved ICU financial performance, lower ICU LOS |
| Zawada et al, 200864 | Pre/posttest of tele-ICU implementation and utilization in a rural health care system | Higher rates of ICU staff adherence to critical care best practices, improved ICU financial performance |
| Zawada and Herr, 200865 | Pre/posttest of tele-ICU implementation and utilization | Improved patient care |
| Zawada et al, 200966 | Pre/posttest of tele-ICU implementation and utilization | Improved hospital financial performance |
ICU = intensive care unit; LOS = length of stay.
In 2013, Kumar et al71 combined a systematic review with cost data from the implementation of a tele-ICU program in 7 ICUs (74 beds) in the Veterans Health Administration to measure the cost of tele-ICU programs. According to the authors, it was estimated that the first-year costs of implementation ranged between $70,000 and $87,000 per ICU bed. The Veterans Health Administration also projected cost for staffing and operating the monitoring site for the first year as $3300 or 27% of total cost. The researchers also reported that tele-ICU studies with vendor association presented cost savings of $2600 to $3000 per patient, whereas studies without vendor association suggested increased hospital cost after implementation. Hospital cost per patient ranged from a reduction of $3000 to an increase of $5600.71
Discussion
This research study has examined potential benefits of implementing a centralized tele-ICU system. The evidence supporting cost savings is mixed. The hospitals in the first three cases experienced some benefit in terms of cost reduction, a decreased ICU LOS, or an overall improved efficiency.
The return on investment for hospitals implementing a tele-ICU system depends on how the system is used, as well as the number of patients the hospital ICU treats. If a hospital system wants to use a tele-ICU system for safety reasons or to make their workforce more efficient, the tele-ICU is a tool that could help. Another benefit of tele-ICU implementation has been an expansion of markets; the tele-ICU allows health care facilities to take care of more patients, which decreases geographic barriers and allows the provision of ICU services into previously inaccessible markets, such as those in rural areas.
In hospital tele-ICU systems examined by Franzini et al39 and Morrison et al,72 hospital costs rose after implementation. Both studies noted that costs associated with physicians choosing a low or nonexistent involvement with tele-intensivists rose more quickly than those costs associated with physicians choosing a higher level of tele-intensivist involvement. Additionally, Franzini et al39 noted that the tele-ICU system used in their study was not fully integrated with the hospitals’ electronic health record system, which may also have contributed to increased cost.
The LOS decreased because intensivists had more time to spend with the patient and were able to provide adequate intensive care. Franzini et al39 and Morrison et al72 noticed patients were being served more effectively than before the implementation of a tele-ICU system.
The large range of hospital costs per bed reported by Kumar et al71 stresses that each health care institution must do a careful cost-benefit analysis and should include vendors in the implementation process from the beginning. Many hospitals have demonstrated that a strong tele-ICU program can find payback in about a year, according to the New England Healthcare Institute (now the Network for Excellence in Health Innovation) in Cambridge, MA.36 In another study, with 10,000 patients, Advanced ICU Care in St Louis, MO, achieved a 40% reduction of mortality and a 25% reduction of ICU LOS.73 This finding concurred also with a study by Lilly et al74,75 of 28,000 patients across 8 states, supporting decreasing mortality and shorter LOS with increased cost savings for the hospitals implementing the tele-ICU programs.
Overall, hospitals have few research findings to help guide them when making a decision about whether to adopt and to use a tele-ICU program. The findings of this literature search suggest that the implementation of a centralized tele-ICU system can be cost-effective and can result in more efficient use of the hospital’s ICU staff, improvement in the quality of care provided, and a financial positive impact by the reduction of ICU LOS.
There were several limitations of this study review. Many articles documented the benefits of tele-ICUs but contained limited data on the actual financial savings or cost of implementing a tele-ICU. Other articles had cost data about the savings but did not have data on how much ICUs were costing them before a tele-ICU implementation. In addition, the excessively high fees presented may be peculiar to the location and hospital size, and so may not be as large elsewhere. This study also was limited by restrictions in the search strategy used, and publication and researcher’s bias may have limited the availability and quality of the research identified for review. Additionally, the review was limited to hospital organizations in the US, thus excluding many international providers of tele-ICU care.
The implication of this study is that the implementation of tele-ICU systems can be cost-effective and can improve patient outcomes. Future research should examine the results attributable to the implementation of a tele-ICU. A meta-analysis should be performed to have a more precise measurement of the effects (ie, cost and savings) of the implementation of a tele-ICU in practice. Other areas for study include how tele-ICUs affect different types of ICUs such as surgical vs nonsurgical ICUs, including tele-ICU vs a 24/7 in-house pulmonary model, and whether similar findings can be achieved in small and rural hospitals.
Conclusion
Although mixed results were found in the literature in terms of cost savings, the findings suggest that the implementation of tele-ICU systems have the potential to produce organizational change, with clinical and nonclinical ICU staff becoming more efficient and effective, and to decrease ICU LOS, hospital costs, and ICU mortality.
Acknowledgments
Katheleen Louden, ELS, of Louden Health Communications provided editorial assistance.
Footnotes
Disclosure Statement
The author(s) have no conflicts of interest to disclose.
Structure and Ability
The tasks assigned [to the physician] … are determined primarily by the social and economic structure of society and by the technical and scientific means available to medicine at the time.
— Medicine and Human Welfare, Henry E Sigerist, 1891–1957, Swiss medical historian
References
- 1.What is telemedicine? [Internet] Washington, DC: The American Telemedicine Association; p. c2012. [cited 2014 Feb 19]. Available from: www.americantelemed.org/learn/what-istelemedicine. [Google Scholar]
- 2.Aust MP. Intensive care unit telemedicine. Am J Crit Care. 2012 Jan;21(1):34. doi: 10.4037/ajcc2012416. DOI: http://dx.doi.org/10.4037/ajcc2012416. [DOI] [PubMed] [Google Scholar]
- 3.ICU outcomes (mortality and length of stay) methods, data collection tool and data [Internet] San Francisco, CA: Philip R Lee Institute for Health Policy Studies, University of California, San Francisco; 2012. [cited 2014 Apr 2]. Available from: http://healthpolicy.ucsf.edu/content/icu-outcomes. [Google Scholar]
- 4.Wenham T, Pittard A. Intensive care unit environment. Continuing Education in Anaesthesia, Critical Care & Pain. 2009 Dec;9(6):178–83. DOI: http://dx.doi.org/10.1093/bjaceaccp/mkp036. [Google Scholar]
- 5.Rothschild JM, Landrigan CP, Cronin JW, et al. The Critical Care Safety Study: the incidence and nature of adverse events and serious medical errors in intensive care. Crit Care Med. 2005 Aug;33(8):1694–700. doi: 10.1097/01.ccm.0000171609.91035.bd. DOI: http://dx.doi.org/10.1097/01.CCM.0000171609.91035.BD. [DOI] [PubMed] [Google Scholar]
- 6.Angus DC, Barnato AE, Linde-Zwirble WT, et al. Robert Wood Johnson Foundation ICU End-Of-Life Peer Group Use of intensive care at the end of life in the United States: an epidemiologic study. Crit Care Med. 2004 Mar;32(3):638–43. doi: 10.1097/01.ccm.0000114816.62331.08. DOI: http://dx.doi.org/10.1097/01.CCM.0000114816.62331.08. [DOI] [PubMed] [Google Scholar]
- 7.Kersten AE, Milbrandt EB, Rahim MT, et al. How big is critical care in the US? Crit Care Med. 2003;31(Suppl):A8. [Google Scholar]
- 8.Mayr VD, Dünser MW, Greil V, et al. Causes of death and determinants of outcome in critically ill patients. Crit Care. 2006;10(6):R154. doi: 10.1186/cc5086. DOI: http://dx.doi.org/10.1186/cc5086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Reynolds HN, Bander J, McCarthy M. Different systems and formats for tele-ICU coverage: designing a tele-ICU system to optimize functionality and investment. Crit Care Nurs Q. 2012 Oct-Dec;35(4):364–77. doi: 10.1097/CNQ.0b013e318266bc26. DOI: http://dx.doi.org/10.1097/CNQ.0b013e318266bc26. [DOI] [PubMed] [Google Scholar]
- 10.Myers MA, Reed KD. The virtual ICU (vICU): a new dimension for critical care nursing practice. Crit Care Nurs Clin North Am. 2008 Dec;20(4):435–9. doi: 10.1016/j.ccell.2008.08.003. DOI: http://dx.doi.org/10.1016/j.ccell.2008.08.003. [DOI] [PubMed] [Google Scholar]
- 11.Khunlertkit A, Carayon P. Contributions of tele-intensive care unit (Tele-ICU) technology to quality of care and patient safety. J Crit Care. 2013 Jun;28(3):315.e1–12. doi: 10.1016/j.jcrc.2012.10.005. DOI: http://dx.doi.org/10.1016/j.jcrc.2012.10.005. [DOI] [PubMed] [Google Scholar]
- 12.Breslow MJ, Rosenfeld BA, Doerfler M, et al. Effect of a multiple-site intensive care unit telemedicine program on clinical and economic outcomes: an alternative paradigm for intensivist staffing. Crit Care Med. 2004 Jan;32(1):31–8. doi: 10.1097/01.CCM.0000104204.61296.41. DOI: http://dx.doi.org/10.1097/01.CCM.0000104204.61296.41. [DOI] [PubMed] [Google Scholar]
- 13.Groves RH, Jr, Holcomb BW, Jr, Smith ML. Intensive care telemedicine: evaluating a model for proactive remote monitoring and intervention in the critical care setting. Stud Health Technol Inform. 2008;131:131–46. [PubMed] [Google Scholar]
- 14.Rosenfeld BA, Dorman T, Breslow MJ, et al. Intensive care unit telemedicine: alternate paradigm for providing continuous intensivist care. Crit Care Med. 2000 Dec;28(12):3925–31. doi: 10.1097/00003246-200012000-00034. DOI: http://dx.doi.org/10.1097/00003246-200012000-00034. [DOI] [PubMed] [Google Scholar]
- 15.Wilcox ME, Adhikari NK. The effect of telemedicine in critically ill patients: systematic review and meta-analysis. Crit Care. 2012 Jul 8;16(4):R127. doi: 10.1186/cc11429. DOI: http://dx.doi.org/10.1186/cc11429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kohl BA, Fortino-Mullen M, Praestgaard A, et al. The effect of ICU telemedicine on mortality and length of stay. J Telemed Telecare. 2012 Jul;18(5):282–6. doi: 10.1258/jtt.2012.120208. DOI: http://dx.doi.org/10.1258/jtt.2012.120208. [DOI] [PubMed] [Google Scholar]
- 17.Lilly CM, Cody S, Zhao H, et al. University of Massachusetts Memorial Critical Care Operations Group Hospital mortality, length of stay, and preventable complications among critically ill patients before and after tele-ICU reengineering of critical care processes. JAMA. 2011 Jun 1;305(21):2175–83. doi: 10.1001/jama.2011.697. DOI: http://dx.doi.org/10.1001/jama.2011.697. [DOI] [PubMed] [Google Scholar]
- 18.Venditti A, Ronk C, Kopenhaver T, Fetterman S. Tele-ICU “myth busters.”. AACN Adv Crit Care. 2012 Jul-Sep;23(3):302–11. doi: 10.1097/NCI.0b013e31825dfee2. DOI: http://dx.doi.org/10.1097/NCI.0b013e31825dfee2. [DOI] [PubMed] [Google Scholar]
- 19.Pronovost PJ, Waters H, Dorman T. Impact of critical care physician workforce for intensive care unit physician staffing. Curr Opin Crit Care. 2001 Dec;7(6):456–9. doi: 10.1097/00075198-200112000-00015. DOI: http://dx.doi.org/10.1097/00075198-200112000-00015. [DOI] [PubMed] [Google Scholar]
- 20.Tele-ICUs: remote management in intensive care units [Internet] Cambridge, MA: New England Healthcare Institute, Massachusetts Technology Collaborative, Health Technology Center; 2007. Mar, [cited 2013 Nov 17]. Available from: www.nehi.net/writable/publication_files/file/tele_icu_final.pdf. [Google Scholar]
- 21.Nielsen M, Saracino J. Telemedicine in the intensive care unit. Crit Care Nurs Clin North Am. 2012 Sep;24(3):491–500. doi: 10.1016/j.ccell.2012.06.002. DOI: http://dx.doi.org/10.1016/j.ccell.2012.06.002. [DOI] [PubMed] [Google Scholar]
- 22.Lyden C. From paper to computer documentation: one easy step? Online Journal of Nursing Informatics [Internet] 2008. Oct, [cited 2013 Nov 14];12(3):[about 20 p]. Available from: http://ojni.org/12_3/Lyden.pdf.
- 23.Zapatochny Rufo RJ. Virtual ICUs, lower operational costs. Nurs Manage. 2008 Dec;39(12):20, 22, 24. doi: 10.1097/01.NUMA.0000342685.95139.b6. DOI: http://dx.doi.org/10.1097/01.NUMA.0000342685.95139.b6. [DOI] [PubMed] [Google Scholar]
- 24.Yao W, Chu CH, Li Z. The use of RFID in healthcare: benefits and barriers. Proceedings of the 2010 IEEE International Conference on RFID-Technology and Applications (RFID-TA); 2010 Jun 17–19. Guangzhou, China. New York, NY: IEEE; 2010. pp. 128–34. DOI: http://dx.doi.org/10.1109/RFID-TA.2010.5529874. [Google Scholar]
- 25.Deslich S, Coustasse A. Expanding technology in the ICU: the case for the utilization of telemedicine. Telemedicine and e-Health. 2014 May;20(5):485–92. doi: 10.1089/tmj.2013.0102. DOI: http://dx.doi.org/10.1089/tmj.2013.0102. [DOI] [PubMed] [Google Scholar]
- 26.Coustasse A, Tomblin S, Slack C. Impact of radio-frequency identification (RFID) technologies on the hospital supply chain: a literature review. Perspect Health Inf Manag. 2013 Oct 1;10:1d. [PMC free article] [PubMed] [Google Scholar]
- 27.Porterfield A, Engelbert K, Coustasse A. Electronic prescribing: improving the efficiency and accuracy of prescribing in the ambulatory care setting. Perspect Health Inf Manag. 2014 Apr 1;11:1g. [PMC free article] [PubMed] [Google Scholar]
- 28.Goran SF. A second set of eyes: an introduction to Tele-ICU. Crit Care Nurse. 2010 Aug;30(4):46–55. doi: 10.4037/ccn2010283. DOI: http://dx.doi.org/10.4037/ccn2010283. [DOI] [PubMed] [Google Scholar]
- 29.Becker C. Remote control. Specialists are running intensive-care units from remote sites via computers, and at least one health system with the e-ICU is reaping financial rewards—and saving lives. Mod Healthc. 2002 Feb 25;32(8):40–2. 44, 46. [PubMed] [Google Scholar]
- 30.Cummings J, Krsek C, Vermoch K, Matuszewski K, University HealthSystem Consortium ICU Telemedicine Task Force Intensive care unit telemedicine: review and consensus recommendations. Am J Med Qual. 2007 Jul-Aug;22(4):239–50. doi: 10.1177/1062860607302777. DOI: http://dx.doi.org/10.1177/1062860607302777. [DOI] [PubMed] [Google Scholar]
- 31.Berenson RA, Grossman JM, November EA. Does telemonitoring of patients—the eICU—improve intensive care? Health Aff. 2009 Aug;28(5):w937–47. doi: 10.1377/hlthaff.28.5.w937. DOI: http://dx.doi.org/10.1377/hlthaff.28.5.w937. [DOI] [PubMed] [Google Scholar]
- 32.Sentara Healthcare to have nation’s first telemedicine intensive care unit contract signed for new round-the-clock intensive care coverage [Internet] Norfolk, VA: Sentara; 2000. Apr 18, [cited 2015 Jan 25]. Available from: www.sentara.com/News/NewsArchives/2000/Pages/ic_usa.aspx. [Google Scholar]
- 33.Sentara’s eICU chosen as model for nation’s hospitals [Internet] Washington DC: Sentara; 2002. Sep 12, [cited 2014 Jan 25]. Available from: www.sentara.com/News/NewsArchives/2002/Pages/eicu_model_for_icu_care.aspx. [Google Scholar]
- 34.Sentara marks 10-year anniversary of groundbreaking eICU system [Internet] Norfolk, VA: Sentara; 2010. Jun 23, [cited 2014 Jan 25]. Available from: www.sentara.com/News/NewsArchives/2010/Pages/Sentara-marks-10-year-anniversary-of-groundbreaking-eICU-system.aspx. [Google Scholar]
- 35.Goran SF. A second set of eyes: An introduction to tele-ICU. Crit Care Nurse. 2010;30:46–55 D. doi: 10.4037/ccn2010283. OI: http://dx.doi.org/10.4037/ccn2010283. [DOI] [PubMed] [Google Scholar]
- 36.New England Healthcare Institute, Massachusetts Technology Collaborative . Critical care, critical choices: the case for tele-ICUs in intensive care [Internet] Westborough, MA: Massachusetts Technology Park Corporation; 2010. Dec, [cited 2014 Jan 25]. Available from: www.masstech.org/sites/mtc/files/documents/2010%20TeleICU%20Report.pdf. [Google Scholar]
- 37.All eyes on the ICU–telemedicine [Internet] Mount Prospect, IL: Society of Critical Care Medicine; 2010. Feb 1, [cited 2014 Feb 21]. Available from: www.sccm.org/Communications/Critical-Connections/Archives/Pages/All-Eyes-on-the-ICU---Telemedicine.aspx. [Google Scholar]
- 38.Shaw G. Virtual ICUs: bigger investment, bigger returns [Internet] Danvers, MA: HealthLeaders Media; 2010. Sep 15, [cited 2014 Apr 25]. Available from: www.healthleadersmedia.com/page-3/MAG-256507/Virtual-ICUs-Big-Investment-Bigger-Returns. [Google Scholar]
- 39.Franzini L, Sail KR, Thomas EJ, Wueste L. Costs and cost-effectiveness of a telemedicine intensive care unit program in 6 intensive care units in a large health care system. J Crit Care. 2011 Jun;26(3):329.e1–6. doi: 10.1016/j.jcrc.2010.12.004. DOI: http://dx.doi.org/10.1016/j.jcrc.2010.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Aaronson ML, Zawada ET, Jr, Herr P, Avera ICU Research Group Role of a telemedicine intensive care unit program (TISP) on glycemic control (GC) in seriously ill patients in a rural health system [abstract] Chest. 2006 Oct;130(4_MeetingAbstracts):226S. DOI: http://dx.doi.org/10.1378/chest.130.4_MeetingAbstracts.226S-a. [Google Scholar]
- 41.Badawi O, Breslow M, Jaber H, Hassan E. Trends in best practice adherence in a large cohort of ICUs: 2005–2010 [abstract no. 814] Crit Care Med. 2010 Dec;38(12 Suppl) DOI: http://dx.doi.org/10.1097/01.ccm.0000390903.16849.8c. [Google Scholar]
- 42.Badawi O, Shemmeri E. Greater collaboration between remote intensivists and on-site clinicians improves best practice compliance [abstract] Crit Care Med. 2006 Dec;34(12 Abstract suppl):A20. DOI: http://dx.doi.org/10.1097/00003246-200612002-00079. [Google Scholar]
- 43.Chu-Weininger MY, Wueste L, Lucke JF, Weavind L, Mazabob J, Thomas EJ. The impact of a tele-ICU on provider attitudes about teamwork and safety climate. Qual Saf Health Care. 2010 Dec;19(6):e39. doi: 10.1136/qshc.2007.024992. DOI: http://dx.doi.org/10.1136/qshc.2007.024992. [DOI] [PubMed] [Google Scholar]
- 44.Coletti C, Elliott D, Zubrow M. Resident perceptions of an integrated remote ICU monitoring system [abstract] Crit Care Med. 2008 Dec;36(12 Suppl):A71. DOI: http://dx.doi.org/10.1097/01.ccm.0000341823.62097.1d. [Google Scholar]
- 45.Dickhaus D. Delivering intensivist services to patients in multiple states using telemedicine [abstract] Crit Care Med. 2006 Dec;34(12 Abstract suppl):A24. DOI: http://dx.doi.org/10.1097/00003246-200612002-00092. [Google Scholar]
- 46.Giessel GM, Leedom B. Centralized, remote ICU intervention improves best practices compliance [abstract] Chest. 2007 Oct;132(4_MeetingAbstracts):444a. DOI: http://dx.doi.org/10.1378/chest.132.4_MeetingAbstracts.444a. [Google Scholar]
- 47.Howell GH, Lem VM, Ball JM. Remote ICU care correlates with reduced health system mortality and length of stay outcomes [abstract] Chest. 2007 Oct;132(4_MeetingAbstracts):443b–4b. DOI: http://dx.doi.org/10.1378/chest.132.4_MeetingAbstracts.443b. [Google Scholar]
- 48.Howell G, Ardilles T, Bonham AJ. Implementation of a remote intensive care unit monitoring system correlates with improvements in patient outcomes [abstract] Chest. 2008 Oct;134(4_MeetingAbstracts):s58003. DOI: http://dx.doi.org/10.1378/chest.134.4_MeetingAbstracts.s58003. [Google Scholar]
- 49.Kohl BA, Gutsche JT, Kim P, Sites FD, Ochroch EA. Effect of telemedicine on mortality and length of stay in a university ICU [abstract] Crit Care Med. 2007 Dec;35(12 Suppl):A22. DOI: http://dx.doi.org/10.1097/01.ccm.0000301049.77714.a1. [Google Scholar]
- 50.Kohl BA, Sites FD, Gutsche JT, Kim P. Economic impact of eICU implementation in an academic surgical ICU [abstract] Crit Care Med. 2007 Dec;35(12 Suppl):A26. DOI: http://dx.doi.org/10.1097/01.ccm.0000301049.77714.a1. [Google Scholar]
- 51.Kumar S, Merchant S, Reynolds R. Tele-ICU: efficacy and cost-effectiveness of remotely managing critical care. Perspect Health Inf Manag. 2013 Apr 1;10:1f. DOI: http://dx.doi.org/10.2174/1874431101307010024. [PMC free article] [PubMed] [Google Scholar]
- 52.Mora A, Faiz SA, Kelly T, Castriotta RJ, Patel B. Resident perception of the educational and patient care value from remote telemonitoring in a medical intensive care unit [abstract] Chest. 2007 Oct;132(4_MeetingAbstracts):443a. DOI: http://dx.doi.org/10.1378/chest.132.4_MeetingAbstracts.443a. [Google Scholar]
- 53.Norman V, French R, Hassan E, et al. Effect of a telemedicine facilitated program on ICU length of stay (LOS) and financial performance [abstract] Crit Care Med. 2009 Dec;37(12 Suppl):A2. DOI: http://dx.doi.org/10.1097/01.ccm.0000365439.11849.a2. [Google Scholar]
- 54.Patel B, Kao L, Thomas E, Campos T. Improving compliance with surviving sepsis campaign guidelines via remote electronic ICU monitoring [abstract] Crit Care Med. 2007 Dec;35(12 Suppl):A275. DOI: http://dx.doi.org/10.1097/01.ccm.0000301049.77714.a1. [Google Scholar]
- 55.Rincon T, Bourke G, Ikeda D, Seiver A. Screening for severe sepsis: an incidence analysis [abstract] Crit Care Med. 2007 Dec;35(12 Suppl):A257. DOI: http://dx.doi.org/10.1097/01.ccm.0000301049.77714.a1. [Google Scholar]
- 56.Scales DC, Dainty K, Hales B, et al. A multifaceted intervention for quality improvement in a network of intensive care units: a cluster randomized trial. JAMA. 2011 Jan 26;305(4):363–72. doi: 10.1001/jama.2010.2000. DOI: http://dx.doi.org/10.1001/jama.2010.2000. [DOI] [PubMed] [Google Scholar]
- 57.Thomas EJ, Chu-Weininger MYL, Lucke J, Wueste L, Weavind L, Mazabob J. The impact of a tele-ICU on provider attitudes about teamwork and safety climate [abstract] Crit Care Med. 2007 Dec;35(12 Suppl):A145. doi: 10.1136/qshc.2007.024992. DOI: http://dx.doi.org/10.1097/01.ccm.0000301049.77714.a1. [DOI] [PubMed] [Google Scholar]
- 58.Vespa PM, Miller C, Hu X, Nenov V, Buxey F, Martin NA. Intensive care unit robotic telepresence facilitates rapid physician response to unstable patients and decreased cost in neurointensive care. Surg Neurol. 2007 Apr;67(4):331–7. doi: 10.1016/j.surneu.2006.12.042. DOI: http://dx.doi.org/10.1016/j.surneu.2006.12.042. [DOI] [PubMed] [Google Scholar]
- 59.Willmitch B, Golembeski S, Kim SS, Nelson LD, Gidel L. Clinical outcomes after telemedicine intensive care unit implementation. Crit Care Med. 2012 Feb;40(2):450–4. doi: 10.1097/CCM.0b013e318232d694. DOI: http://dx.doi.org/10.1097/CCM.0b013e318232d694. [DOI] [PubMed] [Google Scholar]
- 60.Youn BA. ICU process improvement: using telemedicine to enhance compliance and documentation for the ventilator bundle [abstract] Chest. 2006 Oct;130(4_MeetingAbstracts):226S. DOI: http://dx.doi.org/10.1378/chest.130.4_MeetingAbstracts.226S-c. [Google Scholar]
- 61.Young LB, Chan PS, Lu X, Nallamothu BK, Sasson C, Cram PM. Impact of telemedicine intensive care unit coverage on patient outcomes: a systematic review and meta-analysis. Arch Intern Med. 2011 Mar 28;171(6):498–506. doi: 10.1001/archinternmed.2011.61. DOI: http://dx.doi.org/10.1001/archinternmed.2011.61. [DOI] [PubMed] [Google Scholar]
- 62.Zawada ET, Jr, Aaronson ML, Herr P, Erickson DK, Avera ICU Research Group Relationship between levels of consultative management and outcomes in a telemedicine intensivist staffing program (TISP) in a rural health system [abstract] Chest. 2006 Oct;130(4_MeetingAbstracts):226S. DOI: http://dx.doi.org/10.1378/chest.130.4_MeetingAbstracts.226S-b. [Google Scholar]
- 63.Zawada ET, Herr P, Erickson D, Hitt J. Financial benefit of a tele-intensivist program to a rural health system [abstract] Chest. 2007 Oct;132(4_MeetingAbstracts):444. DOI: http://dx.doi.org/10.1378/chest.132.4_MeetingAbstracts.444. [Google Scholar]
- 64.Zawada ET, Herr P, Lindgren L. Clinical and fiscal impact of a rural tele-intensivist staffing program on transfer of patients from their community to a tertiary care hospital [abstract] Crit Care Med. 2008 Dec;36(12 Suppl):A86. DOI: http://dx.doi.org/10.1097/01.ccm.0000341823.62097.1d. [Google Scholar]
- 65.Zawada ET, Herr P. ICU telemedicine improves care to rural hospitals reducing costly transports [abstract] Crit Care Med. 2008 Dec;36(12 Suppl):A172. DOI: http://dx.doi.org/10.1097/01.ccm.0000341823.62097.1d. [Google Scholar]
- 66.Zawada ET, Jr, Herr P, Larson D, Fromm R, Kapaska D, Erickson D. Impact of an intensive care unit telemedicine program on a rural health care system. Postgrad Med. 2009 May;121(3):160–70. doi: 10.3810/pgm.2009.05.2016. DOI: http://dx.doi.org/10.3810/pgm.2009.05.2016. [DOI] [PubMed] [Google Scholar]
- 67.Ikeda D, Hayatdavoudi S, Winchell J, Rincon T, Yee A. The impact of using a standard protocol for the surviving sepsis 6 and 24 hr bundles in septic patients on total ICU risk adjusted mortality [abstract] Crit Care Med. 2006 Dec;34(Abstract suppl 12):A108. [Google Scholar]
- 68.Ries M. Tele-ICU: a new paradigm in critical care. Int Anesthesiol Clin. 2009 Winter;47(1):153–70. doi: 10.1097/AIA.0b013e3181950078. DOI: http://dx.doi.org/10.1097/AIA.0b013e3181950078. [DOI] [PubMed] [Google Scholar]
- 69.Groves RH, Jr, Holcomb BW, Jr, Smith ML. Intensive care telemedicine: evaluating a model for proactive remote monitoring and intervention in the critical care setting. Stud Health Technol Inform. 2008;131:131–46. [PubMed] [Google Scholar]
- 70.Ploetz JM, Badawi O, Rosenfeld BA. Adoption rate of blood transfusion evidence in the intensive care unit [abstract] Chest. 2008;135(4_MeetingAbstracts):p60004. DOI: http://dx.doi/org/10.1378/chest.134.4_MeetingAbstracts.p60004. [Google Scholar]
- 71.Kumar G, Falk D, Bonello R, Kahn JM, Perencevich E, Cram P. The costs of critical care telemedicine programs: a systematic review and analysis. Chest. 2013 Jan;143(1):19–29. doi: 10.1378/chest.11-3031. DOI: http://dx.doi.org/10.1378/chest.11.3031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Morrison JL, Cai Q, Davis N, et al. Clinical and economic outcomes of the electronic intensive care unit: results from two community hospitals. Crit Care Med. 2010;38(1):2–8. doi: 10.1097/CCM.0b013e3181b78fa8. DOI: http://dx.doi.org/10.1097/CCM.0b013e3181b78fa8. [DOI] [PubMed] [Google Scholar]
- 73.Gorman MJ. Driving best practices with tele-ICU [Internet] Chicago, IL: National Association for Healthcare Quality; 2012. [cited 2014 April 24]. Available from: www.nahq.org/annualconference/2012/401-404.html. [Google Scholar]
- 74.Lilly CM, Thomas EJ. Tele-ICU: experience to date. J Intensive Care Med. 2010 Jan-Feb;25(1):16–22. doi: 10.1177/0885066609349216. DOI: http://dx.doi.org/10.1177/0885066609349216. [DOI] [PubMed] [Google Scholar]
- 75.Lilly CM, Cody S, Zhao H, et al. University of Massachusetts Memorial Critical Care Operations Group Hospital mortality, length of stay, and preventable complications among critically ill patients before and after tele-ICU reengineering of critical care processes. JAMA. 2011 Jun 1;305(21):2175–83. doi: 10.1001/jama.2011.697. DOI: http://dx.doi.org/10.1001/jama.2011.697. [DOI] [PubMed] [Google Scholar]