Abstract
Corneal small aperture inlays provide extended depth of focus as a solution to presbyopia. As this procedure is becoming more popular, it is interesting to compare its performance with traditional approaches, such as monovision. Here, binocular visual acuity was measured as a function of object vergence in three subjects by using a binocular adaptive optics vision analyzer. Visual acuity was measured at two luminance levels (photopic and mesopic) under several optical conditions: 1) natural vision (4 mm pupils, best corrected distance vision), 2) pure-defocus monovision ( + 1.25 D add in the nondominant eye), 3) small aperture monovision (1.6 mm pupil in the nondominant eye), and 4) combined small aperture and defocus monovision (1.6 mm pupil and a + 0.75 D add in the nondominant eye). Visual simulations of a small aperture corneal inlay suggest that the device extends DOF as effectively as traditional monovision in photopic light, in both cases at the cost of binocular summation. However, individual factors, such as aperture centration or sensitivity to mesopic conditions should be considered to assure adequate visual outcomes.
OCIS codes: (330.1400) Vision - binocular and stereopsis, (110.1080) Active or adaptive optics, (330.4460) Ophthalmic optics and devices
1. Introduction
As the eye ages, it becomes affected by presbyopia [1]. Since the percentage of the elderly population is steadily growing, a constant search for the best solution to meet visual needs of presbyopic patients is going on. Although vision correction with synthetic intrastromal implants was already suggested in 1949 [2], it has only become a procedure of practical interest within the last years. Progress in refractive surgery techniques has significantly decreased the complexity of its implementation. Advances in the development of biocompatible materials have also reduced postoperative complications. A currently available corneal inlay to overcome presbyopia is the AcuFocus Corneal Inlay 7000 (ACI 7000, AcuFocus Inc., Irvine, CA). Based on small-aperture monovision, it extends depth of focus (DOF) of the eye it is implanted in [3]. Clinical studies support efficacy and safety of the device for presbyopia treatment with published data of up to three years [4–6]. The intrastromal corneal inlay is a 5 μm thick polyvinylidene fluoride ring opacified by carbon nanoparticles. Its outer diameter measures 3.8 mm and the central aperture 1.6 mm. The inlay is perforated with 5-11 μm holes, which are randomly arranged, allowing nutritional flow through the inlay to sustain stromal tissue. Average light transmission with an 8400-hole pattern is approximately 5%. Meant to be a binocular solution to presbyopia, the inlay is usually implanted in the patient’s nondominant eye, centered on the coaxially sighted corneal reflex and combined with a + 0.75 D micro-monovision. The + 0.75 D add was found to be the optimal value when simulating the corneal inlay for a set of real eyes with optical ray tracing software [7].
In spite of the commercial implantation of the inlay having been approved in Europe in 2005, some limitations and potential benefits of the corneal small aperture approach as compared to other existing techniques are still unknown. Although computer-based optical simulations with eye models can estimate monocular outcomes [7], it is still unclear how the mechanism of binocular summation behaves in such an unnatural condition of unequal pupils size. Under normal visual conditions, binocular vision is in general superior to monocular vision [8,9]. To quantify the advantage of binocular vision commonly the binocular summation ratio (BSR) is used. It is defined as the ratio between binocular decimal VA and monocular decimal VA of the better performing eye for according optical conditions. Binocular visual acuity (VA) exceeds monocular VA in the best eye by 11% [8] on average. However, it has also been shown that BSR increases as bilateral contrast decreases [10,11]. In line with these experiments are recent findings that BSR decreases as optical aberrations are corrected binocularly [12,13]. Furthermore, the binocular advantage can be decreased by increased interocular difference in visual quality [14–16], the amount of induced anisometropia [17,18], and unequal retinal illuminance [19].
Binocular adaptive optics vision simulators (BAOVS) are powerful tools to investigate and evaluate monovision approaches [20–22] given that the main optical parameters can be controlled. The use of a BAOVS as a pre-screening device could customize the inlay implantation and optimize postoperative outcomes. Furthermore, the instrument could provide general information about critical limits for reduced light levels or inlay-decentrations, complementary to the knowledge gained in clinical studies.
The purpose of this study was to compare binocular visual through-focus performance with the simulated inlay and pure-defocus monovision in the same group of subjects. Since binocular summation is expected to be reduced both with the corneal inlay and traditional monovision, another goal of this research was to quantify the decrease in BSR for both presbyopia correction methods. The study have been conducted under photopic and mesopic illumination conditions in order to understand the performance of the different corrections under realistic situations. Moreover, a case of practical interest was also studied: vision through a large pupil with an obscuring annulus. The latter is potentially induced in those patients implanted with the corneal inlay under low levels of illumination when their natural pupil exceeds the size of the outer diameter of the inlay.
2. Methods
2.1 Binocular adaptive optics instrument
The BAOVS used in this research [13] and previous versions of the setup [23,24] have been described in detail before. The instrument permits a subject to perform visual testing while his or her monochromatic aberrations can be measured and manipulated. Briefly, the main components of the system are a binocular Hartmann-Shack wavefront sensor, a binocular wavefront modulator based on liquid crystal on silicon (LCOS) (PLUTO-VIS, Holoeye, Berlin, Germany), and a second liquid crystal device to produce the artificial transmittance pupils (LC2002, Holoeye, Berlin, Germany). Visual stimuli were presented on a micro-display (MPro 120, 3M, USA) placed at optical infinity. Subjects’ pupil alignment was ensured continuously by means of a pupil monitoring channel. This channel consists of a CCD camera with enhanced sensitivity in the infrared (Manta G-145 NIR, Allied Vision Technologies GmbH, Stadtroda, Germany) that is focused on the subjects’ iris while their eyes are illuminated with a set of infrared LEDs. The alignment is based upon the image of the iris from an instrument axis that is coaxially with the primary line of sight. Custom-developed routines allow computerized control of all the devices.
In this particular study, the binocular wavefront modulator was used to correct the subjects’ refraction. Higher order aberrations were neither corrected nor manipulated.
2.2 Subjects
Three subjects familiar with the experiment with normal vision and eye health participated in the study. Their mean age at the time of the study was 43 ± 6 years. For two subjects, accommodation was paralyzed with 1% tropicamide solution. The other subject (PA) was a presbyope with pupil diameter large enough to conduct the experiments without pupil dilation. The three subjects were right-eye dominant when tested by the Miles test [25]. Natural defocus and astigmatism were corrected throughout the study, whereas higher order aberrations were not modified. The research followed the tenets of the Declaration of Helsinki. Informed consent was obtained from the subjects after explanation of the nature and possible consequences of the study.
2.3 Experimental procedure
Measurements were organized in several sessions lasting between one and two hours each. VA was assessed using the method of adjustment with a Tumbling E test. Monocular performance was assessed in the nondominant eye (NDE) of the subjects by means of VA measurements. As a first reference, the small aperture was centered on the primary line of sight by means of the pupil camera. Monocular through-focus performance was tested for a 1.6 mm small aperture pupil, a 4 mm pupil and a 5 mm pupil with an obscuring annulus. The latter case was set so that the inner and the outer diameters of the obscuring annulus were 1.6 mm and 3.8 mm, respectively. For clarity, the pupil shapes are depicted in Fig. 1. The 5 mm pupil imitates the situation when an eye is implanted with the small aperture corneal inlay but the natural pupil size becomes larger than the outer inlay diameter.
Fig. 1.
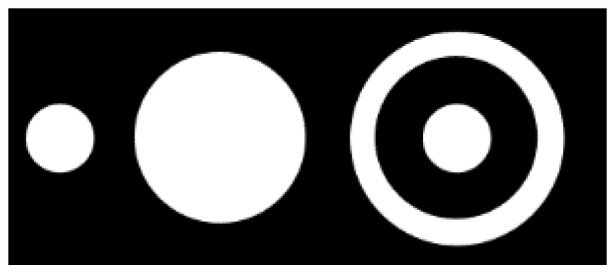
Pupils for which monocular through-focus visual acuity was measured: a 1.6 mm pupil, a 4 mm pupil, and a 5 mm pupil with obscuring annulus (inner inlay diameter 1.6 mm, outer inlay diameter 3.8 mm).
Optimum inlay centration was then tested at distance in polychromatic light. Therefore, the inlay was displaced with respect to the subject’s pupil center in the horizontal direction for testing the impact of implant positioning. Binocular performance was tested for natural vision and three different types of monovision. Figure 2 illustrates amplitude and phase of the pupil functions for unaberrated eyes in far vision when individual binocular optical conditions were simulated. Henceforth, these conditions are referred to as natural vision, traditional monovision, small aperture monovision, and combined monovision. Natural vision was simulated with artificial pupils of 4 mm in diameter and without any added phase. Traditional monovision was simulated with artificial pupils of 4 mm in both eyes and inducing + 1.25 D of pure defocus in the NDE. In case of simulating small aperture monovision, the artificial pupil conjugate to the NDE’s pupil plane was reduced to 1.6 mm in diameter. Combined monovision was simulated by reducing the artificial pupil to 1.6 mm in diameter and additionally inducing + 0.75 D of defocus in the NDE.
Fig. 2.
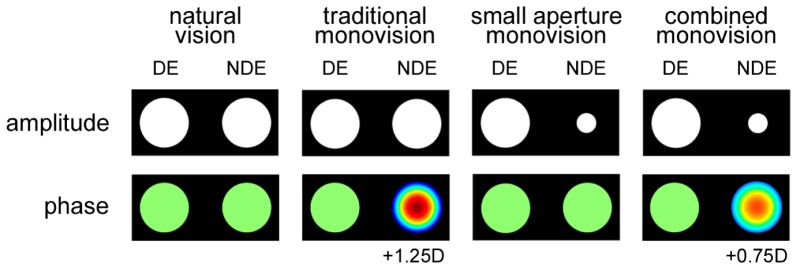
Overview of the binocular optical conditions for which through-focus visual acuity was assessed. The upper row shows the binary amplitude and the lower row shows the phase maps of the complex pupil functions for the dominant and nondominant eye (DE and NDE). Natural vision was simulated with 4mm pupils and best corrected distance vision in both eyes. For the different types of monovision, the optics of the NDE was modified as depicted in the Figure.
We would like to point out that the artificial pupil uses the magnified pupil dimensions in the corneal plane, not the original pupil dimensions. In clinical practice, the inlay is located very close to the corneal surface (~170 µm), so that the magnification is small (<1.01). Therefore, it is a good approximation to use the actual inlay diameter as artificial pupil diameter.
Binocular through-focus performance was assessed under photopic and mesopic luminance conditions in quasi-monochromatic green light. In addition, monocular through-focus VA was measured in both the dominant eye (DE) and the NDE under photopic conditions. VA decrease was determined by fitting linear functions to the averaged through-focus VAs. Regression or correlation coefficients of the fits were obtained, shown as R2-values. DOF was derived from linearly interpolating through-focus curves for individual subjects. In photopic light, a VA threshold of Jaeger score J2 (0.18 logMAR) was chosen, whereas in mesopic light the threshold was lowered to J3 (0.3 logMAR). The BSR was obtained as defined in the Introduction.
3. Results
3.1 Monocular visual performance
Average monocular through-focus VA measurements for the different pupils simulated with the BAOVS are shown in Fig. 3. For the small aperture pupil and the larger 4 mm pupil, distance VA is similar. However, with the small aperture inlay, the VA decrease rate is considerably reduced from 0.20 logMAR/D (R2 = 0.99) to 0.12 logMAR/D (R2 = 0.93). The through-focus curve measured with the 5 mm pupil runs approximately parallel to that measured with the small aperture pupil (R2 = 0.96), though average performance is reduced by about 0.07 logMAR. For vergences larger than 0.5 D, performance with the 5 mm pupil is noticeably better than with the 4 mm reference pupil.
Fig. 3.
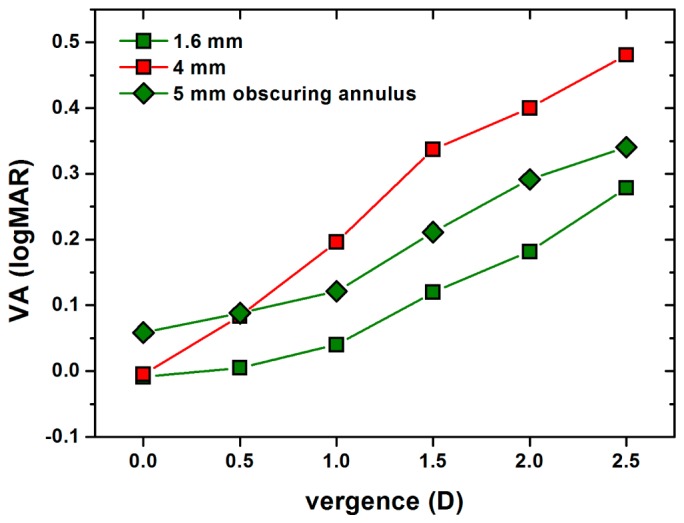
Monocular through-focus visual acuity (VA) for the 1.6 mm pupil (green squares), the 4 mm pupil (red squares), and the 5 mm pupil with obscuring annulus (green diamonds). When compared to performance with the 1.6 mm pupil, the 5 mm pupil with obscuring annulus decreases distance VA but increases performance at vergences greater than 1 D.
VA with the small aperture depended strongly on the centration of the inlay. Figure 4 shows the average VA as a function of inlay decentration with respect to the primary line of sight. Positive decentrations mean that the inlay was displaced in nasal direction whereas negative decentrations stand for temporal displacements. Standard deviations were around 0.2 logMAR. On average, best VA was achieved when the inlay was located between 0 and 0.5 mm nasally. VA decreased quickly when the inlay was decentered, although the course varied strongly among subjects.
Fig. 4.
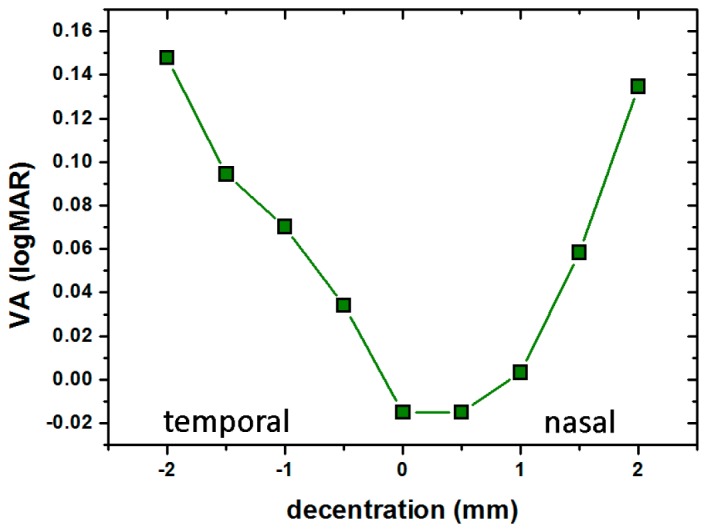
Visual acuity (VA) as a function of the small pupil inlay centration shows that correct centration is critical to achieve good VA.
3.2 Binocular visual performance in photopic light
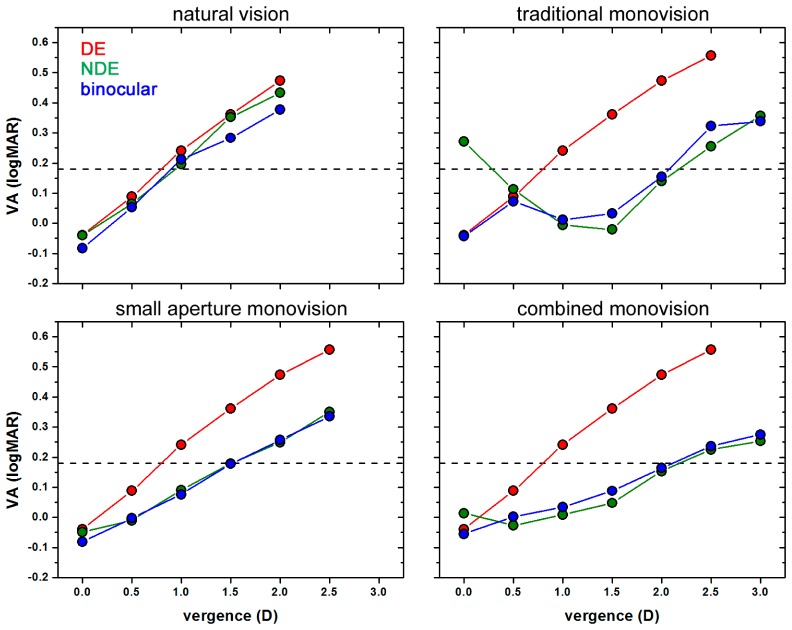
Figure 5 shows monocular VAs for DE and NDE, and binocular VAs as a function of object vergence averaged across subjects. Standard errors were in the range of 0.1 logMAR. Each panel stands for one binocular optical condition. In the upper row, conditions with equal pupil sizes are shown, whereas in the lower row, conditions with different pupil dimensions are illustrated. In the left and right column, results for conditions without and with unilaterally induced defocus are given.
Fig. 5.
Monocular (dominant eye: DE; nondominant eye: NDE) and binocular visual acuity (VA) as a function of object vergence in photopic light. In the upper row, conditions with equal pupil sizes are shown, whereas in the lower row, conditions with differently sized pupils are illustrated. In the left and right column, results for conditions without and with unilaterally induced defocus are given. Standard deviations were in the range of 0.1 logMAR.
For all simulated conditions, binocular VA closely followed monocular VA of the better performing eye. For natural vision, binocular VA decreased with increasing object vergence according to 0.23 logMAR/D (R2 = 0.97). For traditional monovision, the slope of binocular throughfocus VA was similar when considering vergences greater than 1 D (0.22 logMAR/D; R2 = 0.89).
The small aperture approach in the NDE had no significant effect on monocular distance VA. However, it reduced binocular VA decrease with object vergence to 0.169 logMAR/D (R2 = 0.99). Binocular through-focus VA with combined monovision did not show the typical double peak for unilaterally induced defocus. Instead, a linear regression resulted in accurate fitting (R2 = 0.99). Combined monovision further reduced binocular VA decrease to 0.113 logMAR/D.
The left panel of Fig. 6 directly compares binocular through-focus VA for the four simulated cases. Distance VA of −0.08 logMAR with natural vision was decreased to −0.04 logMAR with traditional monovision. Yet, according to a one-sided, paired student’s t-test this difference was not statistically significant (p = 0.055). Binocular distance VA was not sacrificed with the small aperture pupil. With combined monovision, distance performance decreased slightly less than with traditional monovision to −0.06 logMAR (p = 0.069). At vergences greater than 0.5 D, binocular VA was significantly better with traditional monovision and combined monovision than with natural vision.
Fig. 6.
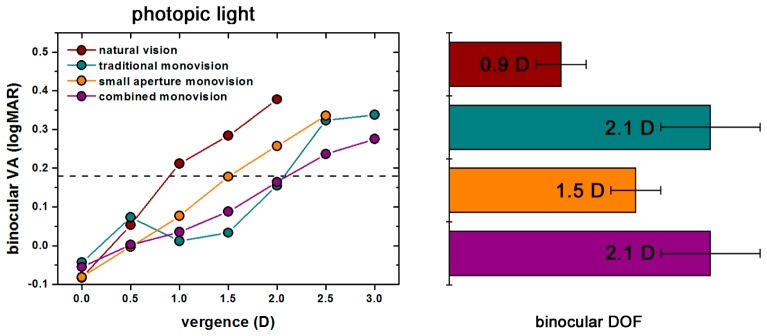
The left panel compares binocular through-focus visual acuities (VA) for the four optical conditions in photopic light. All types of monovision improve binocular VA for vergences greater than 0.5 D. In the right panel, binocular depth of focus (DOF) is shown when a threshold of 0.18 logMAR (J2) is set. The greatest DOF is achieved with traditional monovision and combined monovision.
Binocular DOF is presented in the right panel of Fig. 6. The threshold was set to J2 (0.18 logMAR). All types of monovision extended binocular DOF. Small aperture monovision increased binocular DOF from 0.9 ± 0.2 D to 1.5 ± 0.2 D (p = 0.046). The greatest DOF of 2.1 ± 0.4 D, however, was achieved with combined monovision and traditional monovision. Both increases with respect to natural vision were highly statistically significant (p = 0.003 and p<0.001).
The BSR was calculated for the four cases. Figure 7 shows the mean ratio versus object vergence. Averaged across subjects and object vergences, the ratio was 1.08 ± 0.05 for natural vision, 1.01 ± 0.02 for small aperture monovision and 0.99 ± 0.03 for both combined monovision and traditional monovision. The decrease in BSR from natural vision to either monovision condition was statistically significant (p = 0.007, 0.0009, and 0.015 for small aperture, combined, and pure-defocus monovision respectively). The differences in BSR between monovision conditions were very small and certainly not statistically significant.
Fig. 7.
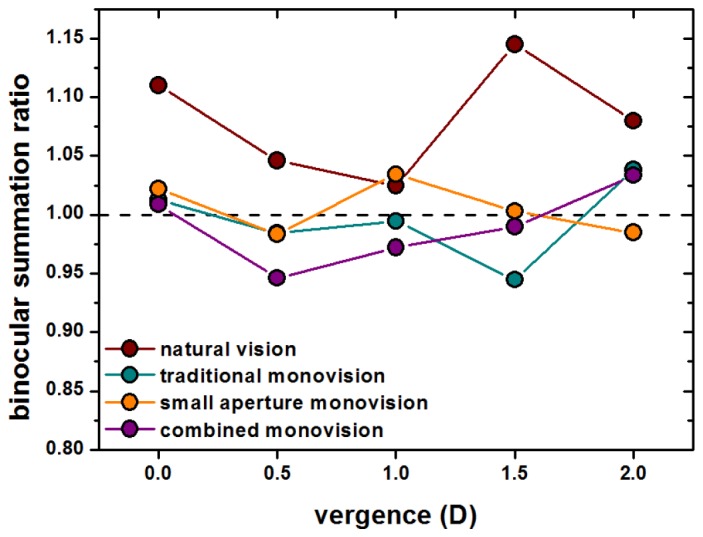
Binocular summation ratio versus object vergence for the four optical conditions in photopic light. The black dashed line marks a binocular summation ratio of one. All types of monovision caused a decrease in the binocular summation ratio.
3.3 Binocular visual performance in mesopic light
In the left panel of Fig. 8, binocular VA under mesopic light levels of illumination versus object vergence is compared for the four optical conditions. The dashed black line marks the J3-line (0.3 logMAR). Visual performance in mesopic light was reduced with respect to performance in photopic light, however, mesopic and photopic curves showed very similar decreases for the same optical conditions. Averaged across vergences, VA with natural vision was 0.15 logMAR worse than under photopic luminance conditions. With monovision, no matter of what type, mesopic VA was reduced more drastically. Binocular VA with traditional monovision, small aperture monovision, and combined monovision resulted 0.23, 0.26, and 0.25 logMAR worse than when measured under photopic luminance conditions. For natural vision, distance VA was −0.01 logMAR. With all types of monovision, distance VA was significantly reduced. Traditional monovision caused a distance VA of 0.05 logMAR (p = 0.026), whereas simulating small aperture monovision and combined monovision, decreased distance VA to 0.06 logMAR (p = 0.003 and p = 0.047). However, for object vergences of 1.5 D and 2 D, binocular VA with monovision was significantly better than for natural vision in all cases. Binocular VA for traditional monovision and combined monovision only differed significantly at the object vergence of 1.5 D (p = 0.038).
Fig. 8.
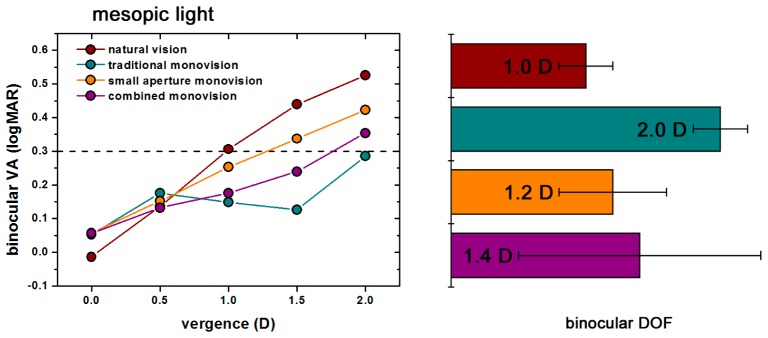
The left panel compares binocular through-focus visual acuities (VA) for the four optical conditions in mesopic light. All types of monovision improve binocular VA for vergences greater than 0.5 D, just as in photopic light. In the right panel, binocular depth of focus (DOF) is shown when a threshold of 0.18 logMAR (J2) is set. The greatest DOF is achieved with traditional monovision.
The right panel of Fig. 8 compares binocular DOF for natural vision with binocular DOF with monovision in mesopic light. Binocular DOF with natural vision averaged across the three subjects was 1.0 ± 0.2 D. Binocular DOF resulted largest for traditional monovision (2.0 ± 0.2 D). With small aperture monovision and combined monovision, average binocular DOF was 1.2 ± 0.4 D and 1.4 ± 0.9 D. Error bars were comparatively large here, because the small aperture inlay had no effect in mesopic light for Subject 3. When only considering Subject 1 and 2, binocular DOF averaged 1.4 ± 0.1 D with small aperture monovision and 2.0 ± 0.1 D with combined monovision.
4. Discussion
The efficacy of small aperture monovision [4,5,21,22,26] and traditional monovision [20,27–29] has been investigated in several studies. However, no direct comparison has been performed so far. Here, we compared binocular through-focus visual acuity performance with different types of monovision in a group of subjects. Our results show that the small aperture inlay in combination with micro-monovision of 0.75 D and traditional monovision of 1.25 D have comparable effects on binocular depth of focus and binocular summation in photopic light. Our measurements show that both the small aperture in one eye and induced anisometropia lead to a comparable, though non-significant, decrease in binocular summation with respect to natural vision. As a consequence, both types of monovision present a benefit for binocular DOF which is extended from 0.9 D to 2.1 D in both cases.
Monovision can be regarded as successful if interocular blur suppression is effective, but inhibition does not occur [30]. For high spatial frequencies, this can be quantified by the binocular visual acuity summation ratio. We found that, in photopic light, all types of monovision tested here reduced binocular summation from baseline (natural vision) to a similar extent. The ratio was not significantly different from one, meaning that neither summation nor inhibition occurred.
For two of the subjects, a benefit in binocular DOF with combined monovision could also be found under mesopic lighting conditions. Especially the result that visual performance in mesopic light was more subject-dependent with combined monovision, which can be deduced from the greater error, suggests that preliminary VA measurements in reduced light levels prior to implantation of the inlay may be important.
While small apertures in general increase DOF, this does not necessarily implicate that binocular DOF will be extended in case only one of the pupils is reduced. In case of keeping a constant light-source level, the smaller pupil investigated here reduced retinal illuminance about 6-fold. Unequal monocular illuminances are known to have a detrimental effect on BSR [19]. Although it is possible to estimate monocular optical outcomes with customized ray tracing, it is more difficult to predict binocular outcomes in such an unnatural case of different pupil sizes. Visual simulators could be used in screenings prior to presbyopia surgery in order to customize and optimize visual outcomes.
The study demonstrated that the BAOVS is appropriate to explore the potential and the limitations of different presbyopia correction methods. Without the need of a real implantation, the instrument realistically simulates different aspects of monocular and binocular visual conditions with the small aperture approach. When comparing visual performance with the simulated small aperture with clinical results [4,6], both monocular and binocular distance VA are in good agreement. However, near VAs are lower in this study by about 1-2 lines.
Artificial pupil generation with liquid-crystal spatial light modulators reveals advantages [23] as compared to other approaches when simulating vision. The current setup permits to control diameter and centration of artificial pupils, of even complex shape, with high spatial resolution (~1/30 mm). Furthermore, the liquid-crystal device makes pupil generation convenient and highly flexible. With a simple button press, the operator can change between different types of pupils. The impact of pinhole decentrations and a large pupil with obscuring annulus could be explored. Distance VA was found to be strongly dependent on inlay centration and the course of the curve was in turn strongly subject-dependent. Here, maximum VA was measured when the small aperture was located between 0 and 0.5 mm nasal to the pupil center. Tabernero and Artal [7] determined the average optimum position of the inlay to maximize Strehl ratios for personalized eye models to be located 0.4 mm nasal from the center of the pupil. Our results are in accordance with the aforementioned theoretical predictions. In clinical practice, the inlay is centered on the corneal reflex which is located about 0.5 mm nasal to the center of the pupil in a normal patient.
In contrast to the small aperture pupil, the 5 mm pupil reduced visual performance at distance. For closer objects, however, VA was better with the 5 mm pupil than with the natural 4 mm pupil. Yet, how subjects perform with the 5 mm pupil in lower light levels still lacks investigation.
A previous study with a monocular AO instrument demonstrated the efficacy of a small aperture pupil for monocular vision in photopic conditions [31]. Although distance VA with corrected HOA decreased when visual testing was performed through an artificial pupil of 2 mm compared with vision through 5 mm pupils, average through-focus VA was improved with the smaller pupil. In our measurements, monocular distance VA with the small aperture was not found to differ from that with the larger 4 mm pupil, but was comparable to small aperture distance VA in the study named above. The same observation was made by Atchison et al [32]. This can be attributed to the fact that, in contrast to the previous study, HOA were not corrected here. While HOA correction should have a minor impact on visual performance at best focus with small pupils, visual performance with larger pupils would improve noticeably [33]. A second consequence would be a steeper slope in through-focus curves measured with equal pupil diameters due to reduced DOF [34].
A limitation of the current study was the use of the natural pupil as reference for the visual axis. Centration on the achromatic axis would have been preferable as visual outcomes can be expected to be superior [7]. By implementing a two color Vernier alignment test and moving the simulated inlay horizontally and vertically, subjects could be asked to determine this location subjectively, similar to the procedure presented by Manzanera et al. [35]. Since this requires some modifications to the binocular adaptive optics visual simulator used here, such measurements could be performed in a future study.
Although binocular visual acuity and depth of focus are important measures characterizing visual performance, other aspects, such as binocular contrast sensitivity and stereoacuity are also relevant for patients to judge a vision correction as acceptable. A companion study investating stereoacuity for traditional monovision, small aperture monovision and combined monovision has been published [21]. While traditional monovision reduced stereoacuity, subjects performed similar with natural vision and the small aperture.
In conclusion, a small aperture in combination with micro-monovision is a simple and effective approach for some patients in order to correct for presbyopia. However, individual factors, such as aperture centration or sensitivity to mesopic conditions should be considered to assure optimum visual outcomes. Adaptive optics-based instruments may help to find the adequate parameters for every patient prior to clinical surgery.
Acknowledgments
This research has been supported by the European Research Council Advanced Grant ERC-2013-AdG-339228 (SEECAT) and the “Ministerio de Ciencia e Innovación”, Spain, grant FIS2010-14926.
References and links
- 1.Duane A., “Normal Values of the Accommodation at all Ages,” J. Amercian Med. Assoc. 59(12), 1010–1013 (1912). 10.1001/jama.1912.04270090254042 [DOI] [Google Scholar]
- 2.Barraquer J., “Queratoplastia refractiva,” Estud. E. Inf. Oftalmológicas 2, 10–30 (1949). [Google Scholar]
- 3.Yilmaz O. F., Bayraktar S., Agca A., Yilmaz B., McDonald M. B., van de Pol C., “Intracorneal inlay for the surgical correction of presbyopia,” J. Cataract Refract. Surg. 34(11), 1921–1927 (2008). 10.1016/j.jcrs.2008.07.015 [DOI] [PubMed] [Google Scholar]
- 4.Seyeddain O., Riha W., Hohensinn M., Nix G., Dexl A. K., Grabner G., “Refractive surgical correction of presbyopia with the AcuFocus small aperture corneal inlay: two-year follow-up,” J. Refract. Surg. 26(10), 707–715 (2010). 10.3928/1081597X-20100408-01 [DOI] [PubMed] [Google Scholar]
- 5.Seyeddain O., Hohensinn M., Riha W., Nix G., Rückl T., Grabner G., Dexl A. K., “Small-aperture corneal inlay for the correction of presbyopia: 3-year follow-up,” J. Cataract Refract. Surg. 38(1), 35–45 (2012). 10.1016/j.jcrs.2011.07.027 [DOI] [PubMed] [Google Scholar]
- 6.Dexl A. K., Seyeddain O., Riha W., Rückl T., Bachernegg A., Emesz M., Ruckhofer J., Grabner G., “Reading performance and patient satisfaction after corneal inlay implantation for presbyopia correction: two-year follow-up,” J. Cataract Refract. Surg. 38(10), 1808–1816 (2012). 10.1016/j.jcrs.2012.06.047 [DOI] [PubMed] [Google Scholar]
- 7.Tabernero J., Artal P., “Optical modeling of a corneal inlay in real eyes to increase depth of focus: optimum centration and residual defocus,” J. Cataract Refract. Surg. 38(2), 270–277 (2012). 10.1016/j.jcrs.2011.07.040 [DOI] [PubMed] [Google Scholar]
- 8.Cagenello R., Arditi A., Halpern D. L., “Binocular enhancement of visual acuity,” J. Opt. Soc. Am. A 10(8), 1841–1848 (1993). 10.1364/JOSAA.10.001841 [DOI] [PubMed] [Google Scholar]
- 9.Campbell F. W., Green D. G., “Monocular versus binocular visual acuity,” Nature 208(5006), 191–192 (1965). 10.1038/208191a0 [DOI] [PubMed] [Google Scholar]
- 10.Banton T., Levi D. M., “Binocular summation in vernier acuity,” J. Opt. Soc. Am. A 8(4), 673–680 (1991). 10.1364/JOSAA.8.000673 [DOI] [PubMed] [Google Scholar]
- 11.Plainis S., Petratou D., Giannakopoulou T., Atchison D. A., Tsilimbaris M. K., “Binocular summation improves performance to defocus-induced blur,” Invest. Ophthalmol. Vis. Sci. 52(5), 2784–2789 (2011). 10.1167/iovs.10-6545 [DOI] [PubMed] [Google Scholar]
- 12.Sabesan R., Zheleznyak L., Yoon G., “Binocular visual performance and summation after correcting higher order aberrations,” Biomed. Opt. Express 3(12), 3176–3189 (2012). 10.1364/BOE.3.003176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schwarz C., Cánovas C., Manzanera S., Weeber H., Prieto P. M., Piers P., Artal P., “Binocular visual acuity for the correction of spherical aberration in polychromatic and monochromatic light,” J. Vis. 14(2), 1–11 (2014). [DOI] [PubMed] [Google Scholar]
- 14.Castro J. J., Jiménez J. R., Hita E., Ortiz C., “Influence of interocular differences in the Strehl ratio on binocular summation,” Ophthalmic Physiol. Opt. 29(3), 370–374 (2009). 10.1111/j.1475-1313.2009.00643.x [DOI] [PubMed] [Google Scholar]
- 15.Cuesta J. R. J., Anera R. G., Jiménez R., Salas C., “Impact of interocular differences in corneal asphericity on binocular summation,” Am. J. Ophthalmol. 135(3), 279–284 (2003). 10.1016/S0002-9394(02)01968-2 [DOI] [PubMed] [Google Scholar]
- 16.Jiménez J. R., Castro J. J., Jiménez R., Hita E., “Interocular differences in higher-order aberrations on binocular visual performance,” Optom. Vis. Sci. 85(3), 174–179 (2008). 10.1097/OPX.0b013e31816445a7 [DOI] [PubMed] [Google Scholar]
- 17.Legras R., Hornain V., Monot A., Chateau N., “Effect of induced anisometropia on binocular through-focus contrast sensitivity,” Optom. Vis. Sci. 78(7), 503–509 (2001). 10.1097/00006324-200107000-00013 [DOI] [PubMed] [Google Scholar]
- 18.Pardhan S., Gilchrist J., “The effect of monocular defocus on binocular contrast sensitivity,” Ophthalmic Physiol. Opt. 10(1), 33–36 (1990). 10.1111/j.1475-1313.1990.tb01103.x [DOI] [PubMed] [Google Scholar]
- 19.Gilchrist J., Pardhan S., “Binocular contrast detection with unequal monocular illuminance,” Ophthalmic Physiol. Opt. 7(4), 373–377 (1987). 10.1111/j.1475-1313.1987.tb00763.x [DOI] [PubMed] [Google Scholar]
- 20.Zheleznyak L., Sabesan R., Oh J.-S., MacRae S., Yoon G., “Modified monovision with spherical aberration to improve presbyopic through-focus visual performance,” Invest. Ophthalmol. Vis. Sci. 54(5), 3157–3165 (2013). 10.1167/iovs.12-11050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fernández E. J., Schwarz C., Prieto P. M., Manzanera S., Artal P., “Impact on stereo-acuity of two presbyopia correction approaches: monovision and small aperture inlay,” Biomed. Opt. Express 4(6), 822–830 (2013). 10.1364/BOE.4.000822 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tabernero J., Schwarz C., Artal P., Fernandez E. J., “Binocular visual simulation of a corneal inlay to increase depth of focus,” Invest. Ophthalmol. Vis. Sci. 52(8), 5273–5277 (2011). 10.1167/iovs.10-6436 [DOI] [PubMed] [Google Scholar]
- 23.Schwarz C., Prieto P. M., Fernández E. J., Artal P., “Binocular adaptive optics vision analyzer with full control over the complex pupil functions,” Opt. Lett. 36(24), 4779–4781 (2011). 10.1364/OL.36.004779 [DOI] [PubMed] [Google Scholar]
- 24.Fernández E. J., Prieto P. M., Artal P., “Binocular adaptive optics visual simulator,” Opt. Lett. 34(17), 2628–2630 (2009). 10.1364/OL.34.002628 [DOI] [PubMed] [Google Scholar]
- 25.Miles W., “Ocular dominance demonstrated by unconscious sighting,” J. Exp. Psychol. 12(2), 113–126 (1929). 10.1037/h0075694 [DOI] [Google Scholar]
- 26.Dexl A. K., Seyeddain O., Riha W., Rückl T., Bachernegg A., Emesz M., Ruckhofer J., Grabner G., “Reading performance and patient satisfaction after corneal inlay implantation for presbyopia correction: two-year follow-up,” J. Cataract Refract. Surg. 38(10), 1808–1816 (2012). 10.1016/j.jcrs.2012.06.047 [DOI] [PubMed] [Google Scholar]
- 27.Collins M., Goode A., Brown B., “Distance Visual Acuity and Monovision,” Optom. Vis. Sci. 70(9), 723–728 (1993). 10.1097/00006324-199309000-00007 [DOI] [PubMed] [Google Scholar]
- 28.Evans B. J. W., “Monovision: a review,” Ophthalmic Physiol. Opt. 27(5), 417–439 (2007). 10.1111/j.1475-1313.2007.00488.x [DOI] [PubMed] [Google Scholar]
- 29.Legras R., Hornain V., Monot A., Chateau N., “Effect of induced anisometropia on binocular through-focus contrast sensitivity,” Optom. Vis. Sci. 78(7), 503–509 (2001). 10.1097/00006324-200107000-00013 [DOI] [PubMed] [Google Scholar]
- 30.Schor C., Landsman L., Erickson P., “Ocular dominance and the interocular suppression of blur in monovision,” Am. J. Optom. Physiol. Opt. 64(10), 723–730 (1987). 10.1097/00006324-198710000-00002 [DOI] [PubMed] [Google Scholar]
- 31.Hickenbotham A., Tiruveedhula P., Roorda A., “Comparison of spherical aberration and small-pupil profiles in improving depth of focus for presbyopic corrections,” J. Cataract Refract. Surg. 38(12), 2071–2079 (2012). 10.1016/j.jcrs.2012.07.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Atchison D. A., Smith G., Efron N., “The effect of pupil size on visual acuity in uncorrected and corrected myopia,” Am. J. Optom. Physiol. Opt. 56(5), 315–323 (1979). 10.1097/00006324-197905000-00006 [DOI] [PubMed] [Google Scholar]
- 33.Yoon G.-Y., Williams D. R., “Visual performance after correcting the monochromatic and chromatic aberrations of the eye,” J. Opt. Soc. Am. A 19(2), 266–275 (2002). 10.1364/JOSAA.19.000266 [DOI] [PubMed] [Google Scholar]
- 34.Guirao A., Porter J., Williams D. R., Cox I. G., “Calculated impact of higher-order monochromatic aberrations on retinal image quality in a population of human eyes: erratum,” J. Opt. Soc. Am. A 19(3), 620–627 (2002). 10.1364/JOSAA.19.000620 [DOI] [PubMed] [Google Scholar]
- 35.Manzanera S., Tabernero J., Benito A., Vilupuru A. S., Prieto P. M., Artal P., “Distribution of Achromatizing Pupil Positions and First Purkinje Reflections in a Normal Population,” Invest. Ophthalmol. Vis. Sci. 54, E–Abstract 4281 (2013). [DOI] [PubMed] [Google Scholar]