Abstract
Charting point-of-care results is generally not performed by the laboratory point-of-care team; however, the oversight of this activity remains the responsibility of the point-of-care program. Although point-of-care management and interfacing are not new, there remain a significant number of hospitals not yet utilizing automated electronic interfaces for charting of results to tests performed outside the clinical laboratory (also known as point of care). This article is designed to help quantify the costs associated with manual charting and help build the case for implementing an automated electronic interface through a return-on-investment method.
Key Words: manual charting, return on investment, automated electronic interface
Charting point-of-care results is generally not performed by the laboratory point-of-care team; however, the oversight of this activity remains the responsibility of the point-of-care program. Being intimately involved with the LifeScan exit from the hospital point-of-care glucose testing market has given me awareness into the number of programs where glucose results are still not automatically electronically interfaced to the laboratory information system/electronic medical record (LIS/EMR), and thus one can only assume there is a manual process for documentation of these and other point-of-care testing results. In this article, I will help to quantify the cost of manual charting, provide components for creating a return on investment (ROI) by investing in automated interfaces, and review the benefits of an electronic interface to the LIS/EMR for the point-of-care program, not just for bedside glucose testing, but for all point-of-care testing including those tests performed manually. Let’s begin with the cost of manual charting.
If results are not electronically interfaced, one can only assume they are either documented onto a paper chart or manually entered into the EMR’s nursing notes or flow sheet. Because charting of glucose results is very akin to other nurse charting activities, a very interesting study, “Enhancing Patient Safety Through Electronic Medical Record Documentation of Vital Signs,” studied both errors made manually charting into the EMR and onto a paper chart. The study found the error rate for manual entry into the EMR to be less than 5% compared with the paper chart, where the error rate was 10%. The types of errors were both errors of omission and transcription. For the sake of this article, we are going to assume bedside glucose results are being manually entered into the EMR’s nursing notes or flow sheet simply because I believe we all know the benefits of clinician access to electronic results as opposed to the single paper chart. Have you ever taken the time to quantify how much time is spent manually charting these results every day? All you really need to know is the number of patient tests being performed, using glucose as our example, and an estimate of the number of minutes used to chart results for these tests. Once you have determined the variables just mentioned, you can plug them into the simple formula below to calculate the amount of time spent performing this manual activity.
TABLE 1.
No caption available.
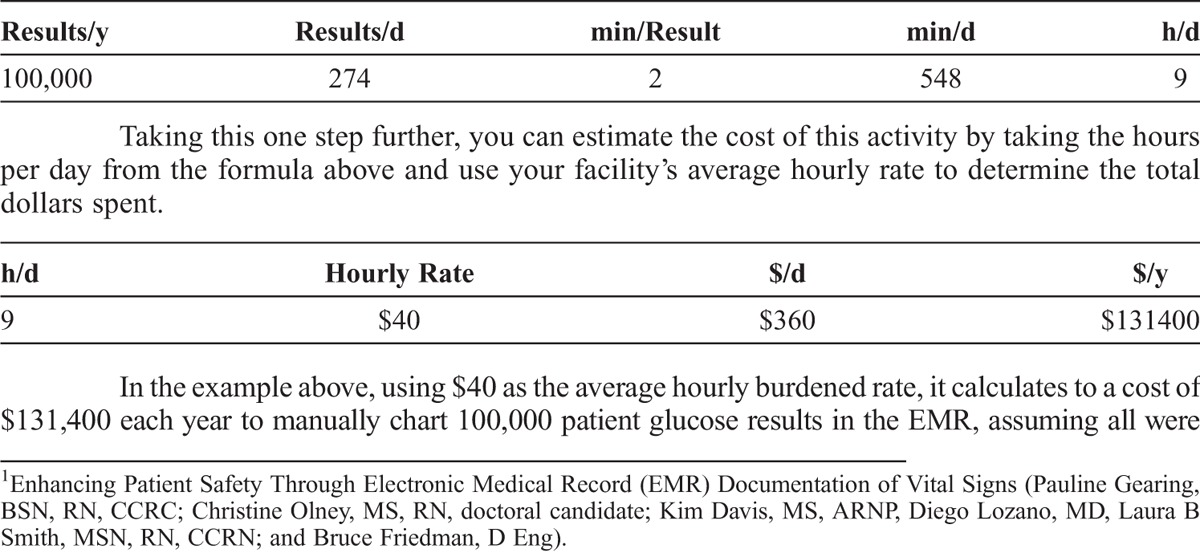
Taking this one step further, you can estimate the cost of this activity by taking the hours per day from the formula above and use your facility’s average hourly rate to determine the total dollars spent.
In the example above, using $40 as the average hourly burdened rate, it calculates to a cost of $131,400 each year to manually chart 100,000 patient glucose results in the EMR, assuming all were charted and charted correctly. Automated electronic interfaces remove this labor component. Not only will they remove this labor component, but they also provide the following other benefits:
Eliminate omissions and transcription errors discussed in the previously referenced article
Provide timely reporting to the LIS/EMR for clinician access
Provide timely oversight by the laboratory
Consolidate laboratory reporting
Automate charge capture
So why not implement an automated electronic interface for charting of these glucose results? Some may say it is just too expensive, but when you examine the cost to implement this type of interface, it really does pay for itself in just the first year.
When looking at the cost for acquisition and implementation of an automated electronic interface, you will need to account for the following components. These components should reflect a 1-time initial cost, and if any have been bundled into a cost-per-strip price, the glucose vendors would need to provide a detailed accounting to accurately reflect initial acquisition costs.
Point-of-care system hardware acquisition and installation
Point-of-care system acquisition
Point-of-care system result interface
Point-of-care system ADT interface
Point-of-care system vendor implementation resource time
Point-of-care system customer implementation resource time
LIS/EMR result interface acquisition and installation
LIS/EMR ADT interface acquisition and installation
LIS/EMR interface testing resource time
Once you have assigned a value to each of these items, the total can then be subtracted from the annual cost of manual charting to determine the ROI from eliminating manual charting. To calculate each subsequent year’s cost for the automated electronic interface, you will need to consider the following components:
Point-of-care system hardware maintenance
Point-of-care system and interface software maintenance
LIS/EMR result and ADT interface software maintenance
With an automated electronic interface, the errors of omission and result transcription have been eliminated. However, it is fair to say that some results will fail to post to the LIS/EMR because of an invalid patient ID entered on the device at test time, and time will now be required of the laboratory point-of-care team for the oversight and correction of these results. The amount of time spent performing just this task can also be determined by using the exact same formula used to calculate the time spent manually charting simply by substituting the number of results each day that require patient ID correction, the average amount of time required to address each result, and the average hourly rate for the individuals addressing this activity. For example, using an average of a 5% daily error rate, 15 minutes per result, and $40 per hour, the annual cost to address invalid patient ID errors on these results would be $50,000. However, with bar-code scanning and positive patient ID on the meters at the time of testing, hopefully the number of results falling into this category can be decreased from the 5% used in this example.
Let’s step away from glucose for the moment and look at manual results that do not have an electronic output from the “device.” It is probably fair to say that the majority of hospitals perform manual testing and that these results are being charted in one of the following ways:
(1) Manually entered onto the patient’s paper chart
(2) Manually entered into the EMR’s nursing notes or flow sheet
(3) Manually written on log sheets, which the laboratory in turn enters into the LIS/EMR
(4) Manually written on log sheets and not entered into the LIS/EMR
I will refer you back to the same article referenced in the beginning that addresses charting in the first 2 options above. There is an inherent delay with the third option and omission from the patient’s record in the fourth option. Wouldn’t it make more sense to provide a mechanism for the charting of manual results that provides the following benefits?
Discrete results that can be queried
Charting of both patient and liquid/aqueous quality control results
Operator certification management
Consistent reporting to the LIS/EMR
Automated opportunities for charge/cost capture
Timely laboratory oversight
Complete customization to satisfy both laboratory and nursing
There are such mechanisms provided by a couple of bedside glucose testing manufacturers and Web applications provided by point-of-care middleware vendors.
As you take a moment to consider the inefficiencies of manual charting, it is important for you to take a step back and look at the bigger picture of your organization’s current processes. You can do that by following these steps:
(1) Gain a full understanding of what manual charting is being done. Think beyond glucose. What other point-of-care devices are being used that can be interfaced? What other departments (ie, respiratory) are using bedside or near-patient testing? How are you electronically charting (or are you) results from manual tests? How accessible are your point-of-care results data?
(2) Evaluate the costs associated with manual charting. When looking at this, consider both the actual financial costs and the value associated with having more timely and accurate access to the results, having the ability to run more timely and accurate reports, and providing patients with more complete electronic records.
(3) Evaluate the costs associated with adding a solution that allows you to electronically interface the point-of-care testing results to the LIS/EMR, taking into account both the 1-time costs and the annual maintenance costs.
(4) Determine what your organization’s ROI would be. How long would it take to “break even?” How much would you continue to save in subsequent years? By using the formulas discussed in this article, you can evaluate each of your point-of-care devices and see how the cost savings could add up over time in terms of actual staff productivity as well as the point-of-care data management efficiency, accuracy, and accessibility.
Maintaining accurate electronic records is an important way for you to provide quality care to your patients in a timely manner. By eliminating as much manual labor as possible through automatic electronic interfaces and having the ability to have manually entered results interfaced to the LIS/EMR, you can not only save time and money, but also ultimately enhance the patient experience. This article focused on the single aspect of manual charting and the ROI with automated electronic interfaces. However, there are also other significant benefits from centralized operator management and oversight that can contribute to the ROI and support accreditation compliance for operators performing manual charting.
Footnotes
Becky Clarke is one of the co-founders and EVP of TELCOR Inc.
The author declares no conflict of interest.


