Abstract:
Rapid correction of severe hyponatremia carries the risk of osmotic demyelination. Two recently introduced methods of correction of hyponatremia have diametrically opposite effects on aquaresis. Inhibitors of vasopressin V2 receptor (vaptans) lead to the production of dilute urine, whereas infusion of desmopressin causes urinary concentration. Identification of the category of hyponatremia that will benefit from one or the other treatment is critical. In general, vaptans are effective in hyponatremias presenting with concentrated urine and, with the exception of hypovolemic hyponatremia, can be used as their primary treatment. Desmopressin is effective in hyponatremias presenting with dilute urine or developing urinary dilution after saline infusion. In this setting, desmopressin infusion helps prevent overcorrection of the hyponatremia. Monitoring of the changes in serum sodium concentration as a guide to treatment changes is imperative regardless of the initial treatment of severe hyponatremia.
Key Indexing Terms: Hyponatremia, Vaptans, Desmopressin
Hyponatremia is considered severe when serum sodium concentration ([Na]s) is <125 mmol/L1 and/or when hypertonic or isotonic saline is infused to correct severe neurological manifestations or symptomatic hypovolemia.2 In severe cases of hyponatremia, the rate of correction of [Na]s is critical for prevention of either prolonged brain edema or osmotic demyelination.2 The current standard is a controlled rate of rise in [Na]s. Although there is some debate about how rapid the initial increase in [Na]s should be in severe hyponatremia,3,4 there is strong evidence that the incidence of osmotic demyelination increases sharply if the correction exceeds 20 mEq/L in the first 24 hours.5 Based on these observations, most experts recommend slower rates of correction.3–6 Recent guidelines from an expert panel recommend a minimum rate of correction of [Na]s by 4 to 8 mEq/L per day, and a goal of 4 to 6 mEq/L per day if the risk of osmotic demyelination syndrome is high.7 The expert panel set also upper limits in the rate of correction. [Na]s should not rise by more than 8 mEq/L in any 24-hour period if the risk of osmotic myelinolysis is high and by no more than 10 to 12 mEq/L in any 24-hour period or 18 mEq/L in any 48-hour period if the risk of osmotic myelinolysis syndrome is not high.7
Achieving the desired rate of correction of [Na]s is a difficult task. In a recent report, the rise in [Na]s in the first 24 hours of treatment exceeded 12 mEq/L in 11% of the subjects admitted with severe hyponatremia.8 Saline infusion carries special risks of overcorrection of hyponatremia. The volume of infused saline is calculated by formulas that take into account the starting and target [Na]s values, the concentration of sodium in the infusate and the volume of body water before the start of saline infusion.2,9 Lack of precision, or inaccuracy, of the clinical estimates of body water entered in the formulas used to calculate the volume of infused saline required for a specific rise in [Na]s are important sources of error in the predictive formulas.2,10
The major source of error during treatment of hyponatremia with saline infusion, however, is not accounted for in the predictive formulas. The source of this error is the volume and the concentrations of sodium and potassium of the urine during the treatment period.2 Two recently proposed strategies addressed specifically the effect of urine volume and composition on [Na]s during treatment of severe hyponatremia. These strategies, which include use of V2 vasopressin receptor inhibitors (vaptans) and infusion of desmopressin along with saline, have diametrically opposite effects on urinary free water excretion. Vaptans increase water loss in the urine (aquaresis) without changing urinary excretion of sodium or potassium; in contrast, desmopressin promotes water reabsorption in the collecting ducts, thereby limiting urinary water loss.
It is therefore imperative to analyze the advantages, risks, indications and contraindications of these 2 treatments for the various categories of hyponatremia. The recent guidelines address some of the uses of vaptans and desmopressin in hyponatremia.7 The purpose of this report was to provide a rationale, based on the pathogenetic mechanism of each episode of severe hyponatremia, for choosing vaptans or desmopressin plus saline as the method of treatment of severe hyponatremia. We do not address alternative methods (eg, restriction of fluid intake, administration of other than vaptan medications blocking the effect of vasopressin on the urinary concentrating mechanism, urea infusion), all of which may have a role in the management of severe hyponatremia in particular individuals.
RELATIONSHIP BETWEEN URINE COMPOSITION, URINE FLOW RATE AND CORRECTION OF [Na]s
As we have previously discussed,2 the changes in [Na]s can be predicted based on various clinical parameters, including initial body water volume, urine flow rate and electrolyte composition, infusate volume and composition as well as dietary ingestion and extrarenal salt and water losses. If we ignore extrarenal losses, the final serum sodium concentration after infusion of saline ([Na]Fin) is predicted by the equation:
 |
where TBWIni is total body water before the infusion, [Na]Ini is the initial serum sodium concentration, 1.11 is an empiric correction term proposed by Edelman et al.11 VInf is the volume of the infusate, [Na]Inf is the sodium concentration in the infusate, VUrine is the volume of urine and [Na]Urine and [K]Urine are the concentrations of sodium and potassium in the urine, respectively.
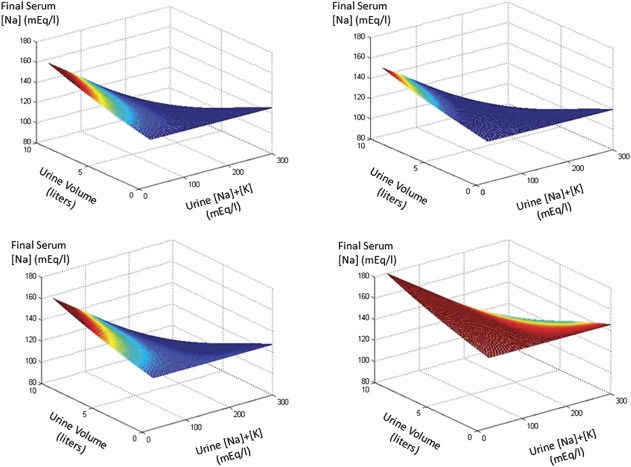
Using this formula and assuming starting points attributable to a 70-kg man with a serum sodium of 125 mEq/L, we performed simulations shown in Figure 1. Reviewing these figures, it seems very clear that infusion of substantial amounts of hypertonic saline would be associated with very high rates of rise in [Na]s unless the urine remained very concentrated. Ergo, it would be predicted that the combination of vaptan therapy, which would cause the elaboration of dilute urine, and hypertonic saline would likely result in too-rapid rates of correction. Vaptans or desmopressin are indicated in certain categories of hyponatremia and are contraindicated or ineffective in other categories.
FIGURE 1.
Simulations of the response of [Na]s depending on urine flow and electrolyte content as well as infusate composition and volume. We began with a 70-kg man (42 L TBWIni) and a [Na]Ini of 125 mEq/L. Simulations are shown in 4 circumstances. Top left panel: no infusate. Top right panel: 2 L of 5% dextrose in water. Bottom left panel: 2 L of 0.9% saline. Bottom right panel: 2 L of 3% saline. Urine volume and electrolyte content were allowed to range in the x and y axes between 0 and 10 L and 25 and 300 mEq/L, respectively. We present simulations as if these occurred after 24 hours and color-coded rates of correction exceeding 20 mEq/L per 24 hours as red with lesser rates of correction having hues moving toward the blue end of the color spectrum.
CATEGORIES OF HYPONATREMIA
One large group of hyponatremias is characterized by high serum vasopressin levels and urine osmolality levels that are higher than the levels that should normally accompany low [Na]s levels.6,8,10,12 High levels of serum vasopressin are the main cause of the inability to excrete water in this group, which consists of 3 categories, hypovolemic, euvolemic and hypervolemic hyponatremia.7,12
Characterization of volume status in hyponatremic patients with high levels of serum vasopressin is critical but encounters serious difficulties. Historical evidence, clinical examination and certain laboratory findings have traditionally been the cornerstone of this classification.2,7,9,10,12–14 Hypovolemic hyponatremia is characterized by history suggesting loss of volume through the gastrointestinal tract, the kidneys or the skin, clinical findings (recent weight loss, orthostatic hypotension, orthostatic tachycardia, absence of edema) and low sodium concentration in the urine except when sodium losses occur through the urine.7,12,13 Euvolemic hyponatremia is characterized by the absence of historical or clinical findings of volume deficit and, usually, by relatively high urine sodium concentration and low serum uric acid level.7,12,13 Hypervolemic hyponatremia is characterized by the presence of a disease causing sodium retention, absence of clinical signs of volume deficit, significant edema (≥0.5 cm of pressure-induced edema) and low urine sodium concentration.7,12,13
The sensitivity and specificity of clinical criteria in differentiating between hypovolemic and euvolemic hyponatremia are poor.14 Urine sodium concentration is low in hypovolemic hyponatremia except in patients with renal losses of sodium caused by disease or diuretics. Whereas, urine sodium is high in most patients with euvolemic hyponatremia except those who experience sodium losses in addition to the primary condition causing euvolemic hyponatremia.7,14 Serum levels of norepinephrine and renin, which are high in hypovolemic hyponatremia and low in euvolemic hyponatremia,14 provide better discrimination between the 2 states. If doubts persist, careful infusion of saline in relatively small volumes and monitoring of urinary water and sodium excretion and of [Na]s may provide useful information about the category of hyponatremia.2,7,14 The characterization of volume status in patients with severe hyponatremia may benefit from application of the specialized noninvasive and invasive techniques that are now available for assessment of intravascular volume in critically ill patients.15 However, we did not find any studies that investigated these techniques in hyponatremia.
The second group of hyponatremias is characterized by low serum vasopressin levels and typically low urine osmolality. Mechanisms other than vasopressin excess are primarily responsible for the water retention in this heterogeneous group, but vasopressin action may play a secondary role. This group includes hyponatremia in chronic renal failure,16 psychiatric disorders,17 potomania,18 low solute load excreted in the urine19 and the sick cell syndrome.20 Resetting of the osmostat may present with high or low urine osmolality (see below). It will be classified in this report in the category of hyponatremia secondary to high vasopressin level because patients with resetting of the osmostat have high vasopressin levels and high urine osmolality when they have hyponatremia.
INDICATIONS AND CONTRAINDICATIONS OF VAPTANS AND DESMOPRESSIN WITH SALINE FOR EACH CATEGORY OF SEVERE HYPONATREMIA
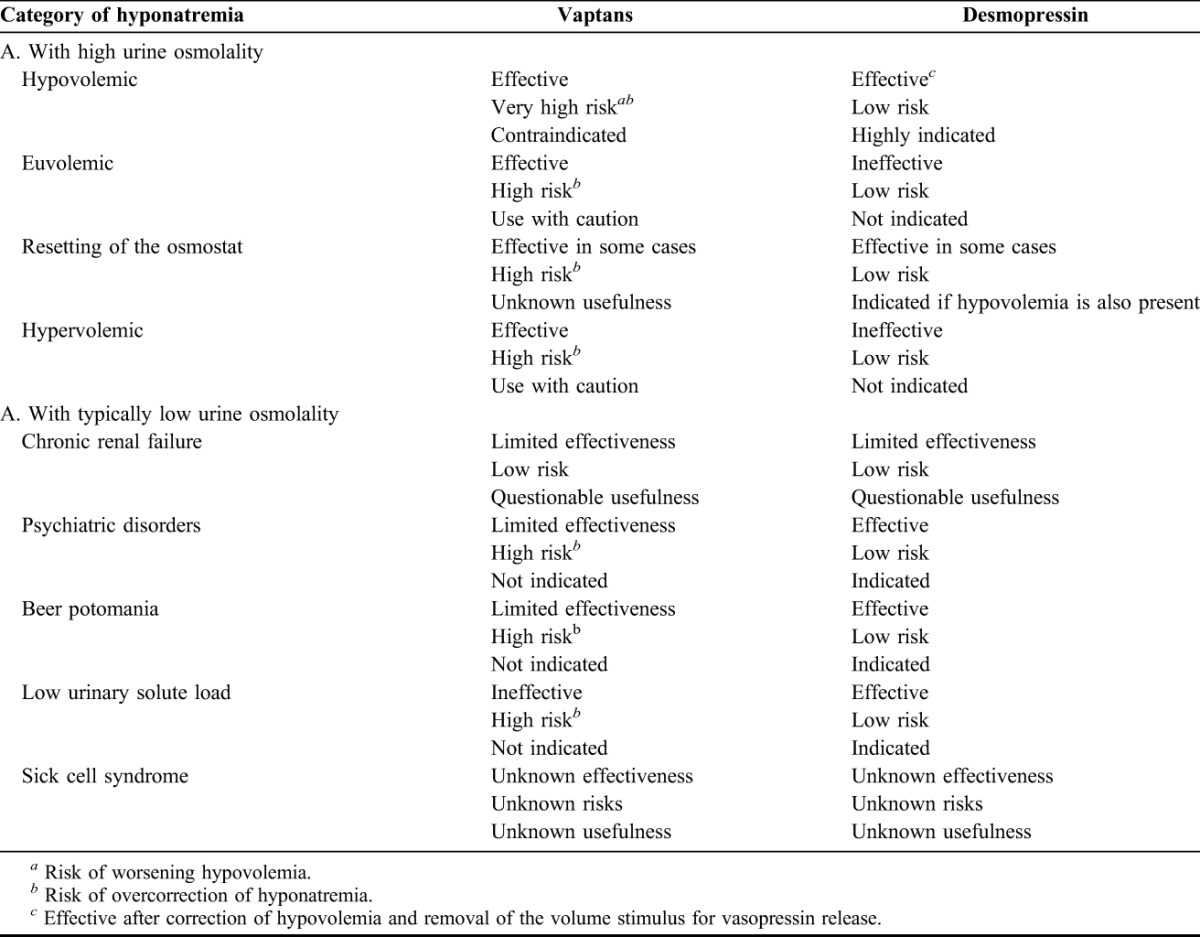
Several reports have analyzed the indications and contraindications of vaptan use in hyponatremia.7,21–23 Desmopressin infusion added to the infusion of hypertonic saline, the volume of which was calculated by the Adrogué-Madias formula,9 achieved the desired rise in [Na]s in 25 of 25 patients with severe hyponatremia.24 Overcorrection was not noted. The treatment with desmopressin infusion was provided to all the patients, regardless of the category of hyponatremia.24 Table 1 provides synoptic answers to the question whether vaptans and desmopressin are effective and safe initial treatments in each category of severe hyponatremia. The remaining text of this section provides the rationale for the statements in Table 1.
TABLE 1.
Vaptans and desmopressin in the treatment of severe hyponatremia (effectiveness, risks, indications and contraindications).
Hyponatremias Resulting Primarily From High Vasopressin Levels
Inhibition of vasopressin action by vaptans will cause aquaresis and increases in [Na]s in every category of hyponatremia in this group, whereas desmopressin, which is infused to prevent aquaresis and rapid increases in [Na]s, may be considered as ineffective given the known fact that increases in serum vasopressin levels above the level that cause maximal urine concentration physiologically (5 to 6 pg/mL) have no further effects on urine osmolality.25 However, there are differences between the 3 categories of hyponatremia in the indications and risks of these treatments. Each category is analyzed below.
Hypovolemic Hyponatremia
In this category of hyponatremia, regardless of the mechanism of hypovolemia, vasopressin secretion is sustained by hypovolemia. Repletion of the extracellular volume by infusion of saline corrects the hypovolemia and removes the volume stimulus for vasopressin release in the circulation. Vasopressin release is then under the influence of osmolality, which is low. Thus, serum vasopressin levels become very low, resulting in profound aquaresis. Vaptans are unnecessary in this setting because production of dilute urine will inevitably follow volume repletion. In fact, vaptan use to treat severe hyponatremia is actually dangerous. Aquaresis preceding the correction of the volume deficit will aggravate this deficit and will also result in overcorrection of hyponatremia. Reversal of hypovolemia with hypertonic or isotonic saline infusion alone carries also the risk of overcorrection of hyponatremia because it will be followed by aquaresis and a rise in [Na]s exceeding that calculated using the predictive formulas.2 Maintenance of urine volume at the lowest rate that will allow solute excretion enhances the accuracy of the formulas that calculate the volume of infused saline and prevents overcorrection of the hyponatremia.2,6,24 Consequently, hypovolemic hyponatremia constitutes a prime indication for infusion of desmopressin along with saline.
Euvolemic Hyponatremias
This category consists of hyponatremias occurring in endocrine disorders, including the syndrome of inappropriate vasopressin secretion (SIADH), profound hypothyroidism and Addison's disease. SIADH can develop in certain disease states or can complicate the use of certain drugs.26 Vaptans are effective in correcting hyponatremia in this syndrome27 and can be used as initial treatment. Aquaresis resulting from the use of vaptans, however, is associated with the risk of overcorrection of hyponatremia. Monitoring of [Na]s and urine output is imperative in this setting. Infusion of hypertonic saline is the preferred initial step in the treatment of hyponatremia with profound neurological manifestations.22 Although not dangerous, desmopressin infusion in the setting of persistently elevated urine osmolality should be considered ineffective.
The nephrogenic syndrome of inappropriate diuresis is characterized by severe hyponatremia occurring early in life, undetectable (very low) serum vasopressin levels and urine with high osmolality. This syndrome is caused by a missense mutation in the gene of the sex-linked V2 receptor in the basolateral membrane of the principal cells of the collecting ducts.28 Whether there is any place for vaptans in the treatment of hyponatremia in patients with this syndrome is not known currently. Like in SIADH, desmopressin should be ineffective in this syndrome in which the high urine osmolality will not decrease during saline infusion.
Euvolemic hyponatremia is encountered in patients with severe hypothyroidism. The proper treatment for this condition is thyroid replacement, which corrects the hyponatremia. Because a vasopressin-mediated component is part of the inability to excrete water loads in this syndrome,29 it is expected that vaptans will be effective in correcting hyponatremia. However, information on the effectiveness of vaptans in this syndrome is lacking. Desmopressin and saline infusion may have a place in the early treatment of severe hyponatremia if thyroid hormone replacement promptly reverses the urinary diluting defect of hypothyroidism.
Secondary adrenal insufficiency is the third hormonal deficit leading to euvolemic hyponatremia. Glucocorticoids facilitate water excretion by the kidneys. Glucocorticoid deficit is associated with a vasopressin-mediated inability to excrete water loads that responds to vaptans.30 However, the primary treatment for this type of hyponatremia is glucocorticoid replacement. It is possible that desmopressin added to saline infusion may be useful in the treatment of severe hyponatremia if concomitant glucocorticoid administration causes an early reversal of the diluting defect. The hyponatremia of primary adrenal insufficiency with combined glucocorticoid and mineralocorticoid deficits has an important element of volume depletion. Desmopressin infusion has a role in the simultaneous correction of hyponatremia and volume defect by infusion of saline.
The concept of resetting of the osmostat has been applied to patients presenting with hyponatremia31 or hypernatremia32 who on formal testing of urinary dilution by water loading and concentration by water deprivation behave as if they have shifted their normal [Na]s downward or upward, respectively. The diagnosis of this syndrome requires exclusion of other types of hyponatremia. Resetting of the osmostat is usually seen in patients with chronic illness and can be combined with other mechanisms of water retention, such as low solute clearance.33 Measurement of urine osmolality and sodium concentration at presentation with hyponatremia should guide the choice of initial treatment. Hyponatremia resulting from resetting of the osmostat should respond to vaptans. However, early use of vaptans should be avoided. Desmopressin infusion is indicated if a component of hypovolemia or of low solute availability is suspected. In euvolemic hyponatremia treated with hypertonic saline, infusion of large loop diuretics promotes urinary water losses and can be used instead of vaptans. Frequent monitoring of the serum sodium concentration is imperative in this setting.
Hypervolemic Hyponatremias
This category of hyponatremias is characterized by conditions leading to progressive renal salt retention because of low effective intravascular volume in the absence of sodium salt deficit. Congestive heart failure, hepatic cirrhosis and the nephrotic syndrome are conditions that precipitate hypervolemic hyponatremia.9 In these conditions, water excretion by the kidneys is impaired by changes in renal hemodynamics, resulting in a low glomerular filtration rate, increased proximal fractional reabsorption values and by high serum levels of vasopressin released in the circulation by volume stimuli.34–36
The findings of high urine osmolality and low urine sodium concentration are indistinguishable between hypervolemic hyponatremia and hypovolemic hyponatremia of extrarenal origin.12 The characteristic difference between these 2 categories of hyponatremia is that saline infusion corrects the volume deficit and leads to aquaresis in hypovolemic hyponatremia but has no effect on the urinary defect in water excretion and aggravates the volume excess in hypervolemic hyponatremia. This difference guides the choice of treatment for hyponatremia. Vaptans are effective in all types of hypervolemic hyponatremias.37 Tolvaptan should not be used in patients with hepatic cirrhosis because of diminished effectiveness and a risk of hepatotoxicity.38 Vaptan use in patients with congestive heart failure and severe hyponatremia obviates the infusion of saline, which aggravates the heart failure, but should be accompanied by measurement of [Na]s every 3 hours to prevent overcorrection.21 Hypertonic saline should be the initial treatment of hypervolemic hyponatremia with profound neurological manifestations. Concomitant infusion of loop diuretics facilitates water diuresis but, like the vaptan use, should be accompanied by frequent measurements of [Na]s. Desmopressin should be ineffective in a setting of persistently high serum vasopressin levels and high urine osmolalities.
Hyponatremias Resulting Primarily From Mechanisms Other Than Vasopressin Release
Hyponatremia of Chronic Renal Failure
Hyponatremia in chronic renal failure is typically associated with hypervolemia and is often classified as hypervolemic hyponatremia. However, the mechanism of hyponatremia differs between chronic renal failure and the conditions listed in this report under hypervolemic hyponatremia. These conditions have high serum vasopressin levels and high osmolality values in the urine. The ability of the kidneys to produce urine with very low osmolality is preserved in chronic renal failure.39 In this syndrome, water loading leads to formation of dilute urine.39 Hyponatremia develops in this setting because the volume of water that the kidneys are capable to excrete is too low and can be less than even usual volumes of ingested water. Loop diuretics may increase water diuresis in hyponatremic patients with substantial residual renal function.
In contrast to urinary dilution, urine concentration is impaired in chronic renal failure. The concentrating defect is resistant to vasopressin infusion.40 Low levels of both the V2 receptor41 and aquaporin-242 have been found in renal failure. However, experimental animals with renal failure responded to water restriction with a weak increase in aquaporin-2, a decrease in urine volume and an increase in urine osmolality.43 Vaptan administration to patients with severe chronic renal failure and congestive heart failure increased urine volume and modestly decreased urine osmolality.44 Thus, vaptans may have a role in the management of hyponatremia of chronic renal failure. Desmopressin infusion will not be needed because of the limited ability of the kidneys to excrete free water.
Hyponatremia of Psychiatric Disorders
Several categories of drugs used to treat psychiatric disorders can cause SIADH.23 In addition, primary polydipsia with hyponatremia is encountered in large numbers of patients with various psychiatric diagnoses. Most patients with primary polydipsia have a dilute urine.45 In a number of patients, however, serum vasopressin was not suppressed adequately.46 Because the urine is not maximally diluted, hyponatremia in these patients may respond to vaptans.47 However, the main issue with the treatment of hyponatremia in the setting of excessive fluid intake is that cessation of water intake, which is the primary treatment, may lead to an inappropriately rapid rise in [Na]s because of a large volume of dilute urine. Desmopressin infusion is indicated, but with a note of caution. Impaired abundance of aquaporin-2 protein in this syndrome48 may limit the effectiveness of desmopressin.
Hyponatremia in Beer Potomania
Excessive fluid intake without any other abnormalities leads to a characteristic picture of very low to undetectable serum vasopressin concentration and a dilute urine, with an osmolality less than 100 mOsm/kg. However, beer drinkers developing hyponatremia exhibit a variety of biochemical profiles. Specifically, urine osmolality is >100 mOsm/kg in several subjects,49,50 whereas urine sodium concentration may be <20 mmol/L suggesting hypovolemia, >40 mmol/L suggesting SIADH, reset osmostat or salt wasting and between 20 and 40 mmol/L.49 In this last category, a large rise in [Na]s after infusion of a test volume of isotonic saline suggests the presence of hypovolemia.2,49 Low solute intake may contribute to the inability to excrete the ingested loads of fluid.50 The use of vaptans may assist in the elucidation of the mechanism of hyponatremia in patients with beer potomania51 but is associated with a risk of overcorrection of hyponatremia similar to the risk in hypovolemic hyponatremia. Saline infusion also carries a risk of overcorrection of hyponatremia, particularly in patients with hypovolemia.52 The indication for desmopressin infusion in this setting is strong.
Hyponatremia in Patients With Low Urinary Solute Load
These patients present with dilute urine.19 However, their ability to excrete water loads is severely limited even when their urine osmolality is at the lowest attainable level.52 Vaptans should have no effect on water excretion when urine dilution is maximal. Solute administration, in the form of saline infusion, rapidly increases free water excretion. Desmopressin infusion, along with saline, hypertonic or isotonic, is indicated in the initial phase of treatment of severe hyponatremia in this syndrome.
Hyponatremia in Patients With Sick Cells
The concept of sick cells refers to abnormalities in the function of transport processes of the cell membranes in patients with severe illnesses, with exit of low-molecular-weight organic solutes and water into the extracellular compartment.53 The characteristic biochemical picture is one of hyponatremia, normal serum osmolality and a large osmol gap, which is the difference between measured serum osmolality and osmolality calculated as the sum of the osmotic equivalents of serum sodium, glucose and urea.54 The concept of sick cell as a cause of hyponatremia has been disputed.55 Even if this syndrome causes hyponatremia, the changes in cell volume should be opposite in the sick cell syndrome, in which cells lose water, and other hyponatremias in which cells are swollen. The role of vaptans or desmopressin in the management of this syndrome is unclear.
Figure 2 shows a flow chart of treatment of hyponatremias with a focus on the use of vaptans or desmopressin.
FIGURE 2.
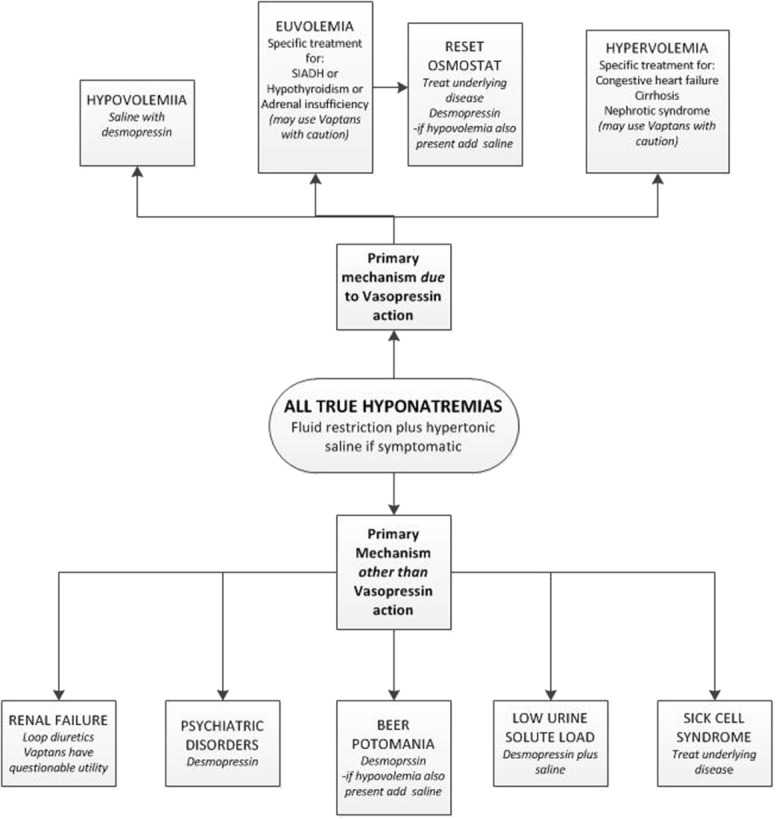
Initial management of severe hyponatremia.
CONCLUSIONS
The use of vaptans for initial treatment of severe hyponatremia is associated with serious risks and is ineffective in certain categories of hyponatremia. The risks of desmopressin infusion are not significant. However, this compound will be ineffective in hyponatremia with persistently elevated urine osmolality. Cost and side effects of each treatment should also be taken into account if alternative treatments are available. Vaptans are effective in correcting hyponatremia with high levels of serum vasopressin and high urine osmolality values. They can be used as initial treatment of hyponatremias with urine osmolality that is persistently elevated but should never be used simultaneously with hypertonic saline. The risk of overcorrection of [Na]s is very high in this case. Vaptans are contraindicated in hyponatremias with urine osmolality that is high initially but is lowered after saline infusion and they are ineffective in hyponatremia with dilute urine. Desmopressin infusion is ineffective for hyponatremias with persistently high urine osmolality but offers the best option for preventing overcorrection of severe hyponatremia with urine that is initially concentrated but responds to saline infusion with dilution. Desmopressin infusion is also indicated for most categories of severe hyponatremia with dilute urine. Characterization of the volume status is critical for the choice of treatment. Hypovolemia in hyponatremic patients may not be detectable by clinical means. Use of desmopressin as initial treatment of hyponatremia if there are doubts about the presence of hypovolemia is prudent. Monitoring of [Na]s, urine flow rate and, in selected cases, urine sodium and potassium concentration is critical during treatment of severe hyponatremia regardless of the method of treatment. Monitoring should be intensified if vaptans are used. The use of vaptans or desmopressin in certain types of hyponatremia will require further studies.
Footnotes
The authors have no financial or other conflicts of interest to disclose.
REFERENCES
- 1.Lien YH. Are we ignoring dysnatremia? Am J Med 2012;125:1045–6 [DOI] [PubMed] [Google Scholar]
- 2.Tzamaloukas AH, Malhotra D, Rosen BH, et al. Principles of management of severe hyponatremia. J Am Heart Assoc 2013;2:e005199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kokko JP. Symptomatic hyponatremia with hypoxia is a medical emergency. Kidney Int 2006;69:1291–3 [DOI] [PubMed] [Google Scholar]
- 4.Sterns RH, Hix JK, Silver S. Treatment of hyponatremia. Curr Opin Nephrol Hypertens 2010;19:493–8 [DOI] [PubMed] [Google Scholar]
- 5.Sonnenblick M, Friedlander Y, Rosin AJ. Diuretic-induced severe hyponatremia. Review and analysis of 129 reported patients. Chest 1993;103:601–6 [DOI] [PubMed] [Google Scholar]
- 6.Adrogué HJ, Madias NE. The challenge of hyponatremia. J Am Soc Nephrol 2012;23:1140–8 [DOI] [PubMed] [Google Scholar]
- 7.Verbalis JG, Goldsmith SR, Greenberg A, et al. Diagnosis, evaluation, and treatment of hyponatremia: expert panel recommendations, Am J Med 2013;126:S1–42 [DOI] [PubMed] [Google Scholar]
- 8.Arampatzis S, Frauchiger B, Fiedler GM, et al. Characteristics, symptoms and outcome of severe dysnatremias present on hospital admission. Am J Med 2012;125:1125.e1–e7 [DOI] [PubMed] [Google Scholar]
- 9.Adrogué HJ, Madias NE. Hyponatremia. N Engl J Med 2000;342:1581–9 [DOI] [PubMed] [Google Scholar]
- 10.Lien YH, Shapiro JI. Hyponatremia: clinical diagnosis and management. Am J Med 2007;120:653–8 [DOI] [PubMed] [Google Scholar]
- 11.Edelman IS, Leibman J, O'Meara MP, et al. Interrelations between serum sodium concentration, serum osmolarity and total exchangeable sodium, total exchangeable potassium and total body water. J Clin Invest 1958;37:1236–56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schrier RW, Bansal S. Diagnosis and management of hyponatremia in acute illness. Curr Opin Crit Care 2008;14:627–34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Anderson RJ, Chung HM, Kluge R, et al. Hyponatremia: a prospective analysis of its epidemiology and the pathogenetic role of vasopressin. Ann Intern Med 1985;102:164–8 [DOI] [PubMed] [Google Scholar]
- 14.Chung HM, Kluge R, Schrier RW, et al. Clinical assessment of extracellular fluid volume in hyponatremia. Am J Med 1987;83:905–8 [DOI] [PubMed] [Google Scholar]
- 15.Kalantari K, Chang JN, Ronco C, et al. Assessment of intravascular volume status and volume responsiveness in critically ill patients. Kidney Int 2013;83:1017–28 [DOI] [PubMed] [Google Scholar]
- 16.Gross P, Rascher W. Vasopressin and hyponatremia in renal insufficiency. Contrib Nephrol 1986;50:54–63 [DOI] [PubMed] [Google Scholar]
- 17.de Leon J, Verghese C, Tracy JI, et al. Polydipsia and water intoxication in psychiatric patients: a review of the epidemiological literature. Biol Psychiatry 1994;35:408–19 [DOI] [PubMed] [Google Scholar]
- 18.Demanet JC, Bonnyns M, Bleiberg H, et al. Coma due to water intoxication in beer drinkers. Lancet 1971;2:1115–7 [DOI] [PubMed] [Google Scholar]
- 19.Thaler SM, Teitelbaum I, Berl T. “Beer potomania” in non-beer drinkers: effect of low dietary solute intake. Am J Kidney Dis 1998;31:1028–31 [DOI] [PubMed] [Google Scholar]
- 20.Gill GV, Osypiw JC, Shearer E, et al. Critical illness with hyponatraemia and impaired cell membrane integrity—the “sick cell syndrome” revisited. Clin Biochem 2005;38:1045–48 [DOI] [PubMed] [Google Scholar]
- 21.Jovanovich AJ, Berl T. Where vaptans do and do not fit in the treatment of hyponatremia. Kidney Int 2013;83:563–7 [DOI] [PubMed] [Google Scholar]
- 22.Lehrich RW, Ortiz-Melo DI, Patel MB, et al. Role of vaptans in the management of hyponatremia. Am J Kidney Dis 2013;62:364–76 [DOI] [PubMed] [Google Scholar]
- 23.Palmer BF. The role of v2 receptor antagonists in the treatment of hyponatremia. Electrolyte Blood Press 2013;11:1–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sood L, Sterns RH, Hix JK, et al. Hypertonic saline and desmopressin: a simple strategy for safe correction of severe hyponatremia. Am J Kidney Dis 2013;61:571–8 [DOI] [PubMed] [Google Scholar]
- 25.Robertson GL. Thirst and vasopressin function in normal and disordered states of water balance. J Lab Clin Med 1983;101:351–71 [PubMed] [Google Scholar]
- 26.Ellison DH, Berl T. Clinical practice. The syndrome of inappropriate antidiuresis. N Engl J Med 2007;356:2064–72 [DOI] [PubMed] [Google Scholar]
- 27.Verbalis JG, Adler S, Schrier RW, et al. Efficacy and safety of oral tolvaptan therapy in patients with the syndrome of inappropriate antidiuretic hormone secretion. Eur J Endocrinol 2011;164:725–32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Feldman BJ, Rosenthal SM, Vargas GA, et al. Nephrogenic syndrome of inappropriate antidiuresis. N Engl J Med 2005;352:1884–90 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chen YC, Cadnapaphornchai MA, Yang J, et al. Nonosmotic release of vasopressin and renal aquaporins in impaired urinary dilution in hypothyroidism. Am J Physiol Renal Physiol 2005;289:F672–8 [DOI] [PubMed] [Google Scholar]
- 30.Olchovsky D, Ezra D, Vered I, et al. Symptomatic hyponatremia as a presenting sign of hypothalamic-pituitary disease: a syndrome of inappropriate secretion of antidiuretic hormone (SIADH)-like glucocorticosteroid responsive condition. J Endocrinol Invest 2005;28:151–6 [DOI] [PubMed] [Google Scholar]
- 31.De Fronzo RA, Goldberg M, Agus ZS. Normal diluting capacity in hyponatremic patients. Reset osmostat or a variant of the syndrome of inappropriate antidiuretic hormone secretion. Ann Intern Med 1976;84:538–42 [DOI] [PubMed] [Google Scholar]
- 32.Gill G, Baylis P, Burn J. A case of “essential” hypernatraemia due to resetting of the osmostat. Clin Endocrinol (Oxf) 1985;22:545–51 [DOI] [PubMed] [Google Scholar]
- 33.Leehey DJ, Picache AA, Robertson GL. Hyponatraemia in quadriplegic patients. Clin Sci (Lond) 1988;75:441–4 [DOI] [PubMed] [Google Scholar]
- 34.Schrier RW. Pathogenesis of sodium and water retention in high-output and low-output cardiac failure, nephrotic syndrome, cirrhosis, and pregnancy (1). N Engl J Med 1988;319:1065–72 [DOI] [PubMed] [Google Scholar]
- 35.Schrier RW. Pathogenesis of sodium and water retention in high-output and low-output cardiac failure, nephrotic syndrome, cirrhosis, and pregnancy (2). N Engl J Med 1988;319:1127–34 [DOI] [PubMed] [Google Scholar]
- 36.Schrier RW. Body fluid volume regulation in health and disease: a unifying hypothesis. Ann Intern Med 1990;113:155–9 [DOI] [PubMed] [Google Scholar]
- 37.Schrier RW, Gross P, Georghiade M, et al. , SALT Investigators. Tolvaptan, a selective oral vasopressin V2-receptor antagonist, for hyponatremia. N Engl J Med 2006;355:2099–112 [DOI] [PubMed] [Google Scholar]
- 38.Torres VE, Chapman AB, Devuyst O, et al. , TEMPO 3:4 Trial Investigators. Tolvaptan in patients with autosomal dominant polycystic kidney disease. N Engl J Med 2012;367:2407–18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bricker NS, Dewey RR, Lubowitz H, et al. Observations on the concentrating and diluting mechanisms of the diseased kidney. J Clin Invest 1959;38:516–23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tannen RL, Regal EM, Dunn MJ, et al. Vasopressin-resistant hyposthenuria in advanced chronic renal disease. N Engl J Med 1969;280:1135–41 [DOI] [PubMed] [Google Scholar]
- 41.Teitelbaum I, McGuinness S. Vasopressin resistance in chronic renal failure. Evidence for the role of decreased V2 receptor mRNA. J Clin Invest 1995;96:378–85 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Nielsen S, Kwon TH, Christensen BM, et al. Physiology and pathophysiology of renal aquaporins. J Am Soc Nephrol 1999;10:647–63 [DOI] [PubMed] [Google Scholar]
- 43.Suzuki K, Hatano R, Michimata M, et al. Residual urinary concentrating ability and AQP2 expression in a rat model for chronic renal failure. Nephron Physiol 2005;99:p16–22 [DOI] [PubMed] [Google Scholar]
- 44.Otsuka T, Sakai Y, Ohno D, et al. The effects of tolvaptan on patients with severe chronic kidney disease complicated by congestive heart failure. Clin Exp Nephrol 2013;17:834–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hariprasad MK, Eisinger RP, Nadler IM, et al. Hyponatremia in psychogenic polydipsia. Arch Intern Med 1980;140:1639–42 [PubMed] [Google Scholar]
- 46.Goldman MB, Luchins DJ, Robertson GL. Mechanisms of altered water metabolism in psychotic patients with polydipsia and hyponatremia. N Engl J Med 1988;318:397–403 [DOI] [PubMed] [Google Scholar]
- 47.Bhardwaj SB, Motiwala FB, Morais M, et al. Vaptans for hyponatremia induced by psychogenic polydipsia. Prim Care Companion CNS Disord 2013;15 10.4088/PCC.12I01444 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Cadnapaphornchai MA, Summer SN, Falk S, et al. Effect of primary polydipsia on aquaporin and sodium transporter abundance. Am J Physiol Renal Physiol 2003;285:F965–71 [DOI] [PubMed] [Google Scholar]
- 49.Liamis GL, Milionis HJ, Rizos EC, et al. Mechanisms of hyponatraemia in alcohol patients. Alcohol Alcohol 2000;35:612–6 [DOI] [PubMed] [Google Scholar]
- 50.Sanghvi SR, Kellerman PS, Nanovic L. Beer potomania: an unusual cause of hyponatremia at high risk of complications from rapid correction. Am J Kidney Dis 2007;50:673–80 [DOI] [PubMed] [Google Scholar]
- 51.Steiner RW. Physiology of beer or non-beer potomania. Am J Kidney Dis 1998;32:1123. [DOI] [PubMed] [Google Scholar]
- 52.Berl T. Impact of solute intake on urine flow and water excretion. J Am Soc Nephrol 2008;19:1076–8 [DOI] [PubMed] [Google Scholar]
- 53.Flear CT, Singh CM. Hyponatraemia and sick cells. Br J Anaesth 1973;45:976–94 [DOI] [PubMed] [Google Scholar]
- 54.Guglielminotti J, Pernet P, Maury E, et al. Osmolar gap hyponatremia in critically ill patients: evidence for the sick cell syndrome? Crit Care Med 2002;30:1051–5 [DOI] [PubMed] [Google Scholar]
- 55.Bichet D, Schrier RW. Evidence against concept of hyponatraemia and “sick cells”. Lancet 1982;1:742. [DOI] [PubMed] [Google Scholar]