Abstract
Purpose
To compare the resolution and optical quality of the ReSTOR® +3.0 D and ReSTOR +2.5 D multifocal intraocular lenses (IOLs) with the AT LISA® tri and FineVision® trifocal IOLs.
Methods
Resolution, image quality, and photic phenomena were evaluated in the AcrySof® IQ ReSTOR +3.0 D and +2.5 D multifocal IOLs and compared with the AT LISA tri 839MP and FineVision Micro F12 trifocal IOLs, using a Badal optometer and a Snellen visual acuity chart. Simulated headlight images were obtained using a modulation transfer function (MTF) bench and a 50 μm pinhole target. MTF values, using vertical and horizontal slits, were determined at far, intermediate, and near distances.
Results
Resolution at 20/40 Snellen visual acuity equivalence was attainable over nearly the entire viewing distance range with the AT LISA tri and FineVision IOLs, but background shadows were more prominent with the AT LISA tri and FineVision IOLs than with the ReSTOR IOLs. Distance MTF peaks at 20/20 Snellen–equivalent spatial frequency were greatest for ReSTOR +2.5 D and ReSTOR +3.0 D IOLs. The near MTF peak occurred at 53 cm with ReSTOR +2.5 D and had a 20/20 Snellen–equivalent value that was lower than the near peaks of the other models but higher than the intermediate foci of the trifocal IOLs.
Conclusion
AT LISA tri and FineVision trifocal IOLs achieved a useful third focus for intermediate vision but were associated with increased background halos and reduced distance visual quality compared with ReSTOR +2.5 D and +3.0 D multifocal IOLs.
Keywords: multifocal, trifocal, modulation transfer function, Badal image, visual acuity, resolution
Introduction
Cataract accounts for 33% of all incidences of visual impairment worldwide and is the leading cause of blindness globally.1 Phacoemulsification of the crystalline lens, followed by capsular bag implantation of an intraocular lens (IOL), is the current standard of care for patients with cataracts.2,3 The goal of cataract surgery and IOL implantation is to improve visual acuity for an optimal refractive target, with minimal complications;2 however, the perceived success of the procedure may vary according to patients’ visual demands and activities. Monofocal IOLs, which provide effective distance vision, currently account for the majority of IOL implantations.2 Depending on their visual demands, patients who have undergone cataract surgery with implantation of monofocal IOLs may require spectacles to perform near-distance (eg, reading) or intermediate-distance (eg, using a computer) tasks.2,4
Multifocal IOLs that maintain distance focus and improve near and intermediate vision have been developed to reduce spectacle dependence.4 Multifocal IOLs improve patient performance of near-vision tasks, such as reading, crafts, hobbies, and social activities, to a greater extent than do monofocal IOLs.5 However, halos and reduced contrast sensitivity have been associated with multifocal IOLs4,5 and are common reasons for patient dissatisfaction.6,7
Multifocal IOLs utilize a variety of optical designs to limit visual disturbances and enhance visual acuity at multiple distances. AcrySof® IQ ReSTOR® (Alcon Laboratories, Inc., Fort Worth, TX, USA) IOLs combine an apodized diffractive zone (for distance and near or intermediate vision) and refractive zone (for distance vision) to enhance visual acuity at multiple distances and direct light to near or distant focal points, according to lighting conditions and pupil diameter.8,9 The ReSTOR +3.0 D and +2.5 D multifocal IOLs provide effective near, intermediate, and distance vision, with the ReSTOR +2.5 D IOL having a near focal point shifted toward intermediate distances. Trifocal lenses, such as the AT LISA® tri 839MP (Carl Zeiss Meditec AG, Jena, Germany) and FineVision® Micro F12 (PhysIOL SA, Liège, Belgium) provide an intermediate focal point in addition to near and distance focal points. The AT LISA tri IOL uses a diffractive pattern that provides trifocal function over the central 4.34 mm region of the IOL, with a more conventional bifocal diffractive pattern extending from 4.34 mm to 6.0 mm diameter. The trifocal diffractive structure asymmetrically directs incident light to distant (50%), intermediate (20%), and near (30%) focal points, independent of pupil diameter (up to 4.5 mm).10 The FineVision IOL contains two overlapping diffractive zones (one for distance and near vision and one for distance and intermediate focus) of more than 30 optical steps that decrease in height from the center of the lens to the periphery.11 Although light allocation and the introduction of a third focal point with trifocal IOLs may be beneficial, these modifications could also possibly impact the quality of near and distant vision. This optical bench study compared the resolution, through-focus image quality, and photic phenomena of two multifocal IOLs (ReSTOR +3.0 D and ReSTOR +2.5 D) and two trifocal IOLs (AT LISA tri 839MP and FineVision Micro F12).
Materials and methods
Intraocular lenses
The resolution, through-focus image quality, and photopic phenomena of two diffractive trifocal IOLs were compared with two apodized diffractive multifocal IOLs. The two aspheric diffractive trifocal IOLs used in this study were AT LISA tri 839MP IOLs (with 21.0 D base power, +3.33 D near add power, and +1.66 D intermediate add power) and FineVision Micro F12 IOLs (with 20.0 D base power, +3.5 D near add power, and +1.75 D intermediate add power). The apodized diffractive multifocal IOLs used in this study were AcrySof IQ ReSTOR +3.0 D IOLs with 21.0 D base power (model SN6AD1) and AcrySof IQ ReSTOR +2.5 D IOLs with 21.0 D base power (model SV25T0). The IOLs were selected based on availability at the time of the study; a FineVision Micro F12 IOL with 21.0 D base power was not available for our assessment.
All IOLs tested had an aspherical design, with negative spherical aberration added to correct for corneal spherical aberration. The FineVision Micro F12 and the ReSTOR +3.0 D IOLs had spherical aberration correction of −0.1 μm. The spherical aberration correction of the AT LISA tri was −0.18 μm,12 and the ReSTOR +2.5 D had a spherical aberration correction of –0.2 μm. The model eye cornea with +0.2 μm spherical aberration was judged to be a reasonable match for all four IOLs.
Experimental design
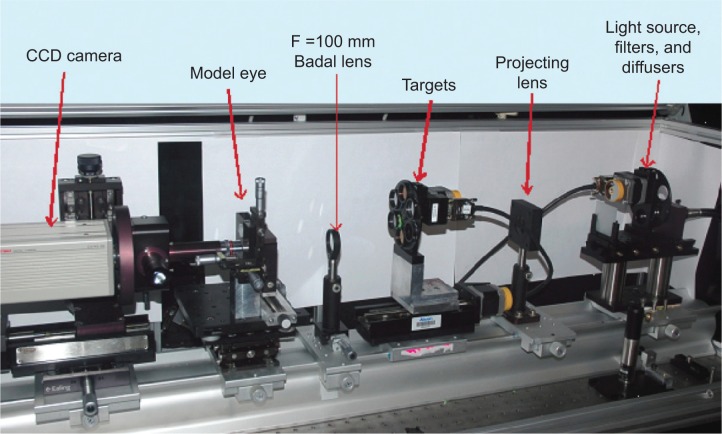
Badal imaging
A custom modulation transfer function (MTF) bench (Image Science Ltd., Chalgrove, UK) with a model eye was constructed as a Badal optometer, thereby allowing viewing of visual targets at near, intermediate, and infinite distances without affecting image magnification (Figure 1). The model eye was positioned at the front focus of a 100 mm focal length doublet, which served as the Badal lens. IOLs were positioned within a model eye containing deionized water and a convex plano lens with 0.2 μm of positive spherical aberration over a 6.0 mm aperture; the IOL was held on a paddle that contained a 3.0 mm pupil. The target was a chrome-on-glass, 25 mm diameter Snellen visual acuity chart that depicted nine rows, with the smallest row corresponding to 20/12 visual acuity (Figure 2). The light source was a Dolan-Jenner Fiber-Lite® LMI-6000 LED Fiber Optic Illuminator (Dolan-Jenner Industries, Boxborough, MA, USA), set so that a cooled scientific charge-coupled device (CCD) camera (model 4742; Hamamatsu Photonics KK, Hamamatsu City, Japan) imager was at the threshold of saturation with a monofocal IOL in the model eye. A narrow-band, 550 nm interference filter was used to limit the spectrum. Through-focus images were obtained at target positions simulating infinity, at the manufacturer’s labeled best near focus for each IOL, and at distances simulating 100, 80, 70, 60, 50, and 40 cm viewing distances.
Figure 1.
Badal optometry bench setup.
Abbreviations: CCD, charge-coupled device; F, focal length.
Figure 2.
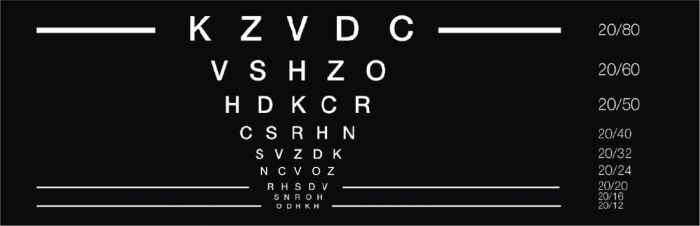
Schematic of the text chart used in the Badal optometer system.
Note: Corresponding Snellen visual acuity is indicated on the right.
Simulated headlight imaging
IOLs were inserted into a modified ISO (International Standards Organization) model eye with 0.2 μm of positive spherical aberration over a 6.0 mm aperture and a paddle that contained a 5 mm pupil to simulate enlarged pupil size under mesopic light conditions. The target (a 50 μm pinhole formed in a metallic sheet) was imaged at infinity and illuminated on one side by a Fiber-Lite® DC-950 Fiber Optic Illuminator (Dolan-Jenner Industries). Images were captured with the CCD camera and recorded using an MTF bench (Optikos Corp, Wakefield, MA, USA) with OpTest™ software (version 5.2.2; Optikos Corp). To make the background more visible, the integration time of the detector was increased to saturate the central image. Light intensity and the imager’s integration time were constant for all measurements.
Modulation transfer function measurements
The IOLs were mounted in model eyes, as described for Badal imaging, and the MTF was measured using the custom Image Science MTF bench. The targets were vertical and horizontal slits, imaged at infinity and illuminated by a light source with a 550 nm narrow-band filter. The image of each slit was obtained from the IOL through a magnified external pupil simulating a 3.0-mm diameter and relayed to the CCD camera. Computer software (Matrix® version 13.8; Image Science Ltd.) was used to analyze the images, obtain average vertical-slit and horizontal-slit values, and generate MTF curves for each IOL. Best focus for distance and near were determined from the peak MTFs at 100 line pairs per millimeter (lp/mm) (equivalent to 20/20 Snellen acuity). Best focus for the intermediate foci was determined from the peak MTF at 50 lp/mm (equivalent to 20/40 Snellen acuity) because for some models, the MTF at 100 lp/mm for this focus was low, making it difficult to determine the best focus. Through-focus MTF was measured by moving the CCD camera and recording the MTF at 50 lp/mm, at 70 discrete points.
Results
Badal images
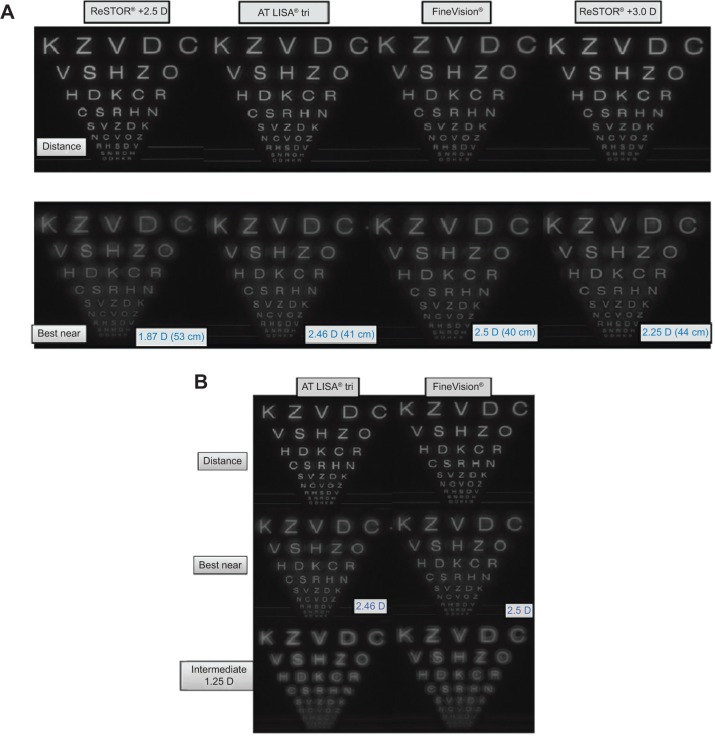
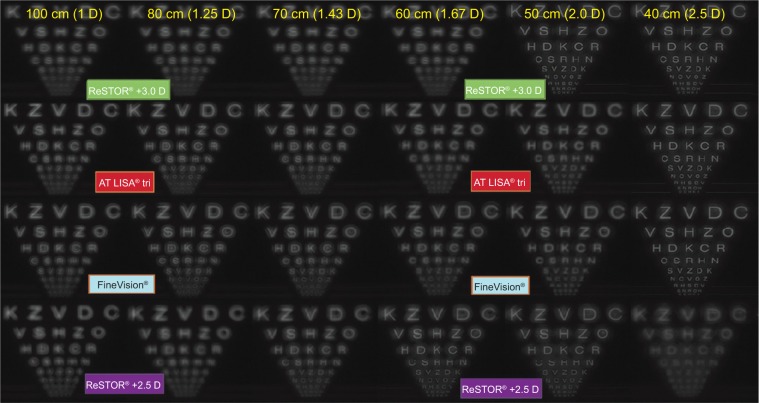
All IOLs resolved the 20/20 Snellen visual acuity line at their distance focal points, with the ReSTOR +2.5 D having the best-resolved distance image. Background shadows around letters were more evident with the FineVision versus the AT LISA tri or ReSTOR +3.0 D IOLs at distance (Figure 3A). Near vision was similar among the AT LISA tri, FineVision, and ReSTOR +3.0 D IOLs. At an intermediate focal distance, the AT LISA tri and FineVision IOLs resolved images at a Snellen visual acuity of 20/40, but strong background shadows were observed (Figure 3B). At distances of 50 and 60 cm, better resolution was observed with the ReSTOR +2.5 D and ReSTOR +3.0 D IOLs than with the AT LISA tri or FineVision IOLs (Figure 4). In through-focus images, the AT LISA tri and FineVision IOLs resolved 20/50 throughout the 100 to 40 cm range (Figure 4); however, strong, structured shadows were prominent with the AT LISA tri and FineVision IOLs, especially at 70 cm. For example, in the 20/60 line (with text “V S H Z O”) at 70 cm, both trifocal IOL images appeared to have a faint vertical line in the center of the letter “H”.
Figure 3.
Image quality of the AT LISA® tri, FineVision®, ReSTOR® +2.5 D, and ReSTOR® +3.0 D IOLs at various focal distances.
Notes: (A) Image quality through all IOLs at distance and best near focal distances. (B) Image quality through trifocal IOLs (AT LISA tri IOL and FineVision IOL) at intermediate focal distances. The smallest line on the chart corresponds with a visual acuity of 20/12. The third line (with the text “R H S D V”) and sixth line (with text “C S R H N”) from the bottom are equivalent to visual acuities of 20/20 and 20/40, respectively. AcrySof® IQ ReSTOR® IOLs, Alcon Laboratories, Fort Worth, TX, USA; AT LISA® tri 839MP IOLs, Carl Zeiss Meditec AG, Jena, Germany; FineVision® Micro F12 IOLs, PhysIOL SA, Liège, Belgium.
Abbreviation: IOL, intraocular lens.
Figure 4.
Through-focus image quality of the AT LISA® tri, FineVision®, ReSTOR® +2.5 D, and ReSTOR® +3.0 D IOLs at various simulated viewing distances.
Notes: The smallest line on the chart corresponds with a visual acuity of 20/12. The third line (with the text “R H S D V”) and sixth line (with text “C S R H N”) from the bottom are equivalent to visual acuities of 20/20 and 20/40, respectively. AcrySof® IQ ReSTOR® IOLs, Alcon Laboratories, Fort Worth, TX, USA; AT LISA® tri 839MP IOLs, Carl Zeiss Meditec AG, Jena, Germany; FineVision® Micro F12 IOLs, PhysIOL SA, Liège, Belgium.
Abbreviation: IOL, intraocular lens.
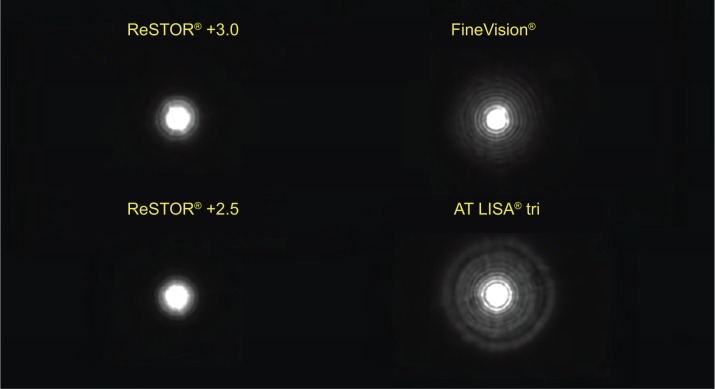
Headlight images
Halos surrounding the simulated headlight target were smaller with the ReSTOR +2.5 D and +3.0 D IOLs compared with the AT LISA tri and FineVision IOLs (Figure 5). Although large halos were observed with both trifocal IOLs, halos were more distinct with the AT LISA tri IOL, whereas those surrounding the FineVision IOL tended to diminish with increasing distance from the central focus point.
Figure 5.
Simulated headlight images through the AT LISA® tri, FineVision®, ReSTOR® +2.5 D, and ReSTOR® +3.0 D IOLs.
Notes: Testing was performed with a 5 mm pupil size. AcrySof® IQ ReSTOR® IOLs, Alcon Laboratories, Fort Worth, TX, USA; AT LISA® tri 839MP IOLs, Carl Zeiss Meditec AG, Jena, Germany; FineVision® Micro F12 IOLs, PhysIOL SA, Liège, Belgium.
Abbreviation: IOL, intraocular lens.
MTF measurements
Distance-, intermediate-, and near-focus MTF results for 20/20 (100 lp/mm) and 20/40 (50 lp/mm) equivalent spatial frequencies are shown in Figure 6A and 6B, respectively. At 20/20 and 20/40 visual acuity equivalent, the ReSTOR +2.5 D had the highest distance MTF (49.2% and 54.8% at 20/20 and 20/40, respectively) followed by the ReSTOR +3.0 D (34.0% and 41.0%, respectively), the AT LISA tri (25.3% and 34.2%, respectively), and FineVision (23.9% and 33.0%, respectively). In contrast, near-focus MTFs were lowest with the ReSTOR +2.5 D IOL (13.5% for 20/20 and 20/40) but were similar among the ReSTOR +3.0 D (19.0% and 25.7%, respectively), AT LISA tri (17.8% and 21.3%, respectively), and FineVision (17.9% and 23.0%, respectively). At 20/40 visual acuity, the intermediate-focus MTF values of the AT LISA tri and FineVision IOLs were similar to each other (14.0% and 13.6% for FineVision and AT LISA tri, respectively) and to the near-focus MTF values of the ReSTOR +2.5 D IOL (13.5%); however, the AT LISA tri and FineVision IOLs had very low intermediate-focus MTF values at 20/20 visual acuity (5.7% and 6.3% for FineVision and AT LISA tri, respectively). The intermediate-focus MTF values of the ReSTOR +2.5 D IOL and the ReSTOR +3.0 D IOL at 20/20 visual acuity were also low (4.2% and 3.4%, respectively); at 20/40 visual acuity, the intermediate-focus MTF values were 5.0% for the ReSTOR +2.5 D IOL and 7.2% for the ReSTOR +3.0 D IOL.
Figure 6.
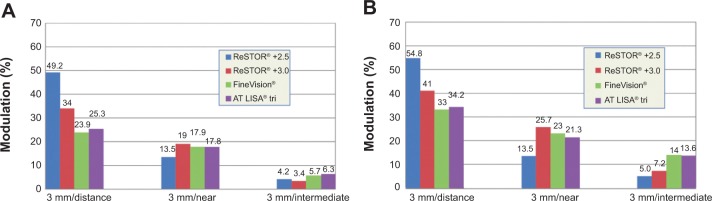
MTF values of the AT LISA® tri, FineVision®, ReSTOR® +2.5 D, and ReSTOR® +3.0 D IOLs at various focal distances.
Notes: (A) MTF values at 20/20 visual acuity equivalent (100 line pairs per mm). (B) MTF values at 20/40 visual acuity equivalent (50 line pairs per mm). AcrySof® IQ ReSTOR® IOLs, Alcon Laboratories, Fort Worth, TX, USA; AT LISA® tri 839MP IOLs, Carl Zeiss Meditec AG, Jena, Germany; FineVision® Micro F12 IOLs, PhysIOL SA, Liège, Belgium.
Abbreviations: IOL, intraocular lens; MTF, modulation transfer function.
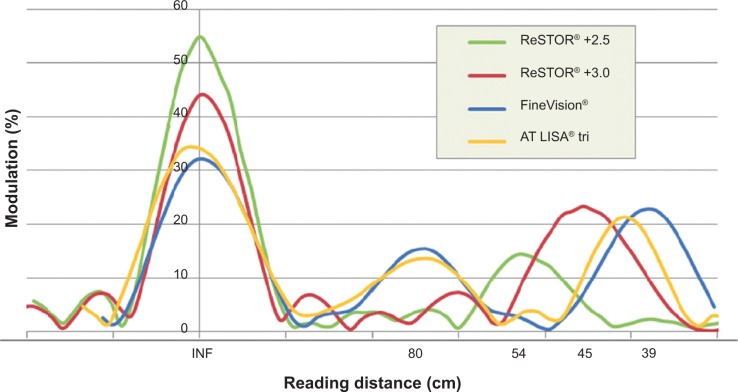
Figure 7 depicts the through-focus MTF curves at 20/40-equivalent spatial frequency, showing the in-focus positions corresponding to the peak MTFs presented in Figure 6B. Distance-focus MTF was greatest with ReSTOR +2.5 D and ReSTOR +3.0 D. Near-focus MTF values were similar for the ReSTOR +3.0 D, FineVision, and AT LISA tri IOLs but were lower with the ReSTOR +2.5 D IOLs. Near-focus MTF peaks occurred at different distances for each IOL (53 cm for the ReSTOR +2.5 D, 44 cm for ReSTOR +3.0 D, 38 cm for FineVision, and 40 cm for the AT LISA tri). The intermediate-focus MTF peaks occurred at a distance of approximately 80 cm for the FineVision and AT LISA tri IOLs.
Figure 7.
Through-focus MTF values of the AT LISA® tri, FineVision®, ReSTOR® +2.5 D, and ReSTOR® +3.0 D IOLs, at 20/40 Snellen visual acuity equivalent (50 line pairs per mm).
Notes: AcrySof® IQ ReSTOR® IOLs, Alcon Laboratories, Fort Worth, TX, USA; AT LISA® tri 839MP IOLs, Carl Zeiss Meditec AG, Jena, Germany; FineVision® Micro F12 IOLs, PhysIOL SA, Liège, Belgium.
Abbreviations: INF, infinity; IOL, intraocular lens; MTF, modulation transfer function.
Discussion
Both the AT LISA tri and FineVision trifocal IOLs demonstrated an intermediate focal point at approximately 80 cm. Near foci of the AT LISA tri, FineVision, and ReSTOR +3.0 D IOLs were in the range of 38 cm to 44 cm. The ReSTOR +2.5 D had a near focal distance at 53 cm, which is useful for intermediate-distance tasks, such as viewing computer monitors.13
The MTF values for all lenses were comparable to those previously reported using similar techniques14–16 and are consistent with the overall design of each IOL. In a bench study comparison of through-focus MTF curves with the ReSTOR +3.0 D and FineVision IOLs with a 3 mm pupil size, the FineVision provided better intermediate (67 cm) optical quality than did the ReSTOR +3.0 D, but optical quality at near (50 cm and 40 cm) and distant focal points was greater for the ReSTOR +3.0 D.15 In another optical bench study, the MTF values for a distant object with a 4.5 mm pupil diameter were greater for FineVision than for AT LISA tri IOLs.16 The authors attributed this difference to the apodized diffractive zone of the FineVision IOL, which directs a greater percentage of the available light to distance vision in mesopic conditions, versus the pupil size– independent allocation of light to the near focus in the AT LISA tri IOL.16 Similar results were obtained in the present study, with MTF values for the ReSTOR +3.0 D being slightly higher than those for the FineVision and AT LISA tri IOLs at near and distance focal points. The ReSTOR +2.5 D had the highest distance MTF, as expected from its more distance-dominant design.17 Near-focus MTF values were slightly reduced with the ReSTOR +2.5 D at its 53 cm near focal point compared with the ReSTOR +3.0 D, FineVision, and AT LISA tri IOLs, consistent with its greater light distribution to the distant focus.10,11,17 At 20/20 Snellen visual acuity equivalent, the MTF value at the near focal point of the ReSTOR +2.5 D was lower than the near MTF values of the other IOLs but higher than the intermediate foci of the two trifocal models.
Data on distance-vision MTF values for monofocal IOLs that were obtained using comparable bench methodology are limited. However, in a model eye with zero spherical aberration, equivalent to the model eye of the original ISO 11979-2, a 20.0 D aspheric monofocal AcrySof SN60WF (Alcon Laboratories, Inc.) had a peak MTF of 50 lp/mm of just under 70%, with a 3 mm pupil.14 Our measurements of the SN60WF IOL in the 0.2 μm spherical aberration model eye with a 3 mm pupil gave a peak MTF of 74% at 50 lp/mm and 54% at 100 lp/mm (Carson D, unpublished data, 2007).
The higher intensity of bench-measured background halos surrounding simulated headlights with the AT LISA tri and FineVision IOLs compared with the ReSTOR +2.5 D and +3.0 D IOLs may relate to differences in the design features of the IOLs. The AT LISA tri IOL has a trifocal center, switching to bifocal at the lens periphery, but lacks apodization.18 FineVision has a trifocal diffractive pattern across the entire optic but is apodized.11 In contrast, the ReSTOR +3.0 D IOLs contain a central apodized diffractive zone ending at a 3.6-mm diameter with a refractive outer zone;8 this design makes these IOLs more strongly distance dominant at large pupil size. The ReSTOR +2.5 D has a similar 3.6 mm apodized diffractive zone that directs more energy to the distance focus and less to the near focus than the ReSTOR +3.0 IOL.17
In addition to the differences in energy distribution with pupil size between the trifocal and ReSTOR IOLs, the addition of a third focus may itself increase halos; this may be a subject for future study. Lower add power also contributes to brighter halos if the energy balance is not adjusted.9 The bright artifacts seen in the intermediate Badal optometer images with the AT LISA tri and FineVision IOLs are of a type that may be caused by reversals of the phase of the optical transfer function. In a simultaneous vision IOL, each focused image has a halo created by the out-of-focus images. The presence of two out-of-focus images is expected to broaden the halo more than a single out-of-focus image, unless two of the out-of-focus images are combined constructively.
The current study was limited by its laboratory nature, which may make generalization to clinical practice difficult. Given that there is normal variation in patient-reported outcomes with any IOL, bench testing of various IOLs may be more useful for comparison of different designs than for predicting exactly what a given patient will see. Although the image at the retina is the foundation of vision, it is not identical to the image perceived by the patient. For example, the Badal optometer images in this study do not take binocular effects into account. Of the four IOLs tested, the ReSTOR +3.0 D, which is designed for distance and near vision, produced the poorest quality intermediate vision; however, this was a bench evaluation, and clinical experience may differ from these findings. Only one corneal spherical aberration value was used, but spherical aberration correction is a small effect for a 3 mm pupil. Imaging was performed only with the 3.0 mm pupil at the IOL (equivalent to 3.6 mm at the corneal plane) because this pupil size is generally considered average for photopic conditions.19 However, the energy distribution of the AT LISA tri is pupil-independent up to 4.5 mm in diameter,18 so the results should not have been affected by omitting pupil sizes other than 3.0 mm from the study. The two ReSTOR designs and to a lesser extent, FineVision design, are known to be increasingly distance-dominant with increasing pupil size;9,11 therefore, MTF values at larger pupil sizes would be expected to provide better distance image quality with reduced intermediate and near focus.
Conclusion
In summary, the occurrence of background halos and overall visual quality were different among the tested IOLs, according to their design features. Based on this laboratory simulation, the ReSTOR +3.0 D is expected to provide high-quality distance and near vision, with a low propensity for halos. The ReSTOR +2.5 D is expected to provide the best distance vision, with low halo intensity and intermediate vision around 50 to 60 cm. The two trifocal IOLs provide improved intermediate vision in the 70 to 80 cm range, although this benefit may come at the expense of increased nighttime halos.
Acknowledgments
This study was funded by Alcon Research, Ltd. (Fort Worth, TX, USA). The authors would like to thank Zaiwei Xu, ME, and Elsinore Alexander, BS, for assistance with data collection. Medical writing assistance was provided by Jillian Gee, PhD, CMPP, of Complete Healthcare Communications, Inc. (Chadds Ford, PA, USA) and was funded by Alcon.
Footnotes
Disclosure
DC, XH, and MK are employees of Alcon Research, Ltd., Fort Worth, TX. WH has no proprietary interest in any of the products listed; he has consulted for Alcon Laboratories, Inc. The authors report no other conflicts of interest in this work.
References
- 1.Pascolini D, Mariotti SP. Global estimates of visual impairment: 2010. Br J Ophthalmol. 2012;96(5):614–618. doi: 10.1136/bjophthalmol-2011-300539. [DOI] [PubMed] [Google Scholar]
- 2.Lundström M, Barry P, Henry Y, Rosen P, Stenevi U. Evidence-based guidelines for cataract surgery: guidelines based on data in the European Registry of Quality Outcomes for Cataract and Refractive Surgery database. J Cataract Refract Surg. 2012;38(6):1086–1093. doi: 10.1016/j.jcrs.2012.03.006. [DOI] [PubMed] [Google Scholar]
- 3.American Academy of Ophthalmology Glaucoma Panel . Preferred Practice Pattern® Guidelines. Cataract in the Adult Eye. San Francisco, CA: American Academy of Ophthalmology; 2011. [Google Scholar]
- 4.Calladine D, Evans JR, Shah S, Leyland M. Multifocal versus monofocal intraocular lenses after cataract extraction. Cochrane Database Syst Rev. 2012;9:CD003169. doi: 10.1002/14651858.CD003169.pub3. [DOI] [PubMed] [Google Scholar]
- 5.Javitt J, Brauweiler HP, Jacobi KW, et al. Cataract extraction with multifocal intraocular lens implantation: clinical, functional, and quality-of-life outcomes. Multicenter clinical trial in Germany and Austria. J Cataract Refract Surg. 2000;26(9):1356–1366. doi: 10.1016/s0886-3350(00)00636-2. [DOI] [PubMed] [Google Scholar]
- 6.de Vries NE, Nuijts RM. Multifocal intraocular lenses in cataract surgery: literature review of benefits and side effects. J Cataract Refract Surg. 2013;39(2):268–278. doi: 10.1016/j.jcrs.2012.12.002. [DOI] [PubMed] [Google Scholar]
- 7.de Vries NE, Webers CA, Touwslager WR, et al. Dissatisfaction after implantation of multifocal intraocular lenses. J Cataract Refract Surg. 2011;37(5):859–865. doi: 10.1016/j.jcrs.2010.11.032. [DOI] [PubMed] [Google Scholar]
- 8.Fisher BL. Presbyopia-correcting intraocular lenses in cataract surgery – a focus on ReSTOR® intraocular lenses. US Ophthalmic Review. 2011;4(1):44–48. [Google Scholar]
- 9.Davison JA, Simpson MJ. History and development of the apodized diffractive intraocular lens. J Cataract Refract Surg. 2006;32(5):849–858. doi: 10.1016/j.jcrs.2006.02.006. [DOI] [PubMed] [Google Scholar]
- 10.Pietrini D. Cataract and Refractive Surgery Today Europe [serial on the Internet] 2012. Mar, [Accessed July 11, 2014]. Introducing a new generation of the AT LISA; pp. 1–16. [cited September 9, 2013] Available from: http://bmctoday.net/crstodayeurope/pdfs/0312_supp.pdf. [Google Scholar]
- 11.Roach L, Shaw J. Eyes on Europe: New options in multifocal IOLs. Eye Net Magazine [serial on the Internet] 2012. May, [Accessed July 11, 2014]. pp. 48–55. [cited August 12, 2013] Available from: http://www.aao.org/publications/eyenet/201205/feature.cfm.
- 12.Mojzis P, Peña-García P, Liehneova I, Ziak P, Alió JL. Outcomes of a new diffractive trifocal intraocular lens. J Cataract Refract Surg. 2014;40(1):60–69. doi: 10.1016/j.jcrs.2013.06.025. [DOI] [PubMed] [Google Scholar]
- 13.Charness N, Dijkstra K, Jastrzembski T, Weaver S, Champion M. Monitor viewing distance for younger and older workers. Proc Hum Factors Ergon Soc Annu Meet. 2008;52(19):1614–1617. [Google Scholar]
- 14.Gatinel D, Houbrechts Y. Comparison of bifocal and trifocal diffractive and refractive intraocular lenses using an optical bench. J Cataract Refract Surg. 2013;39(7):1093–1099. doi: 10.1016/j.jcrs.2013.01.048. [DOI] [PubMed] [Google Scholar]
- 15.Montés-Micó R, Madrid-Costa D, Ruiz-Alcocer J, Ferrer-Blasco T, Pons AM. In vitro optical quality differences between multifocal apodized diffractive intraocular lenses. J Cataract Refract Surg. 2013;39(6):928–936. doi: 10.1016/j.jcrs.2012.12.038. [DOI] [PubMed] [Google Scholar]
- 16.Ruiz-Alcocer J, Madrid-Costa D, García-Lázaro S, Ferrer-Blasco T, Montés-Micó R. Optical performance of two new trifocal intraocular lenses: through-focus modulation transfer function and influence of pupil size. Clin Experiment Ophthalmol. 2014;42(3):271–276. doi: 10.1111/ceo.12181. [DOI] [PubMed] [Google Scholar]
- 17.Alcon Laboratories, Inc . AcrySof® IQ ReSTOR® 2.5 D IOL [webpage on the internet] Alcon Laboratories, Inc; 2013. [Accessed June 20, 2014]. [cited September 9, 2013]. Available from: http://www.alconsurgical.co.za/acrysof-iq-restor-2-5-d-iol.aspx. [Google Scholar]
- 18.Carl Zeiss, Meditec AG. Trifocal MICS IOLs. Jena, Germany: Carl Zeiss Meditec AG; 2013. [Accessed February 6, 2014]. Available from: http://meditec.zeiss.com/content/dam/Meditec/downloads/pdf/ESCRS/czm_ATLISA.pdf. [Google Scholar]
- 19.Smith G, Atchison DA. The Eye and Visual Optical Instruments. New York, NY: Cambridge University Press; 1997. [Google Scholar]