Abstract
Mushrooms are a recognized component of the human diet, with versatile medicinal properties. Some mushrooms are popular worldwide for their nutritional and therapeutic properties. However, some species are dangerous because they cause toxicity. There are many reports explaining the medicinal and/or toxic effects of these fungal species. Cases of serious human poisoning generally caused by the improper identification of toxic mushroom species are reported every year. Different substances responsible for the fatal signs and symptoms of mushroom toxicity have been identified from various poisonous mushrooms. Toxicity studies of mushroom species have demonstrated that mushroom poisoning can cause adverse effects such as liver failure, bradycardia, chest pain, seizures, gastroenteritis, intestinal fibrosis, renal failure, erythromelalgia, and rhabdomyolysis. Correct categorization and better understanding are essential for the safe and healthy consumption of mushrooms as functional foods as well as for their medicinal use.
Keywords: Mushroom toxicity, Poisonous mushroom, Toxic compounds
Poisoning is an important global public health problem. It recently became the leading cause of injury death for the first time since at least 1980. According to a report of the Centers for Disease Control and Prevention (CDC), more than 41,000 people have died in 2008 because of unintentional poisoning, while the World Health Organization (WHO) has reported 0.346 million deaths since 2004 worldwide [1]. A significant portion of these global numbers is attributable to mushroom poisoning. There are numerous mushroom poisoning cases in different countries each year. In 1998, 1,675 mushroom poisoning cases were reported in France and approximately 8,000 to 10,000 cases are estimated to be on record.
Mushrooms have long attracted a great deal of interest in many areas of the food and biopharmaceutical industries. They are well known for their nutritional and medicinal values [2, 3]. The worldwide diversity of mushroom species is roughly accounted as 0.14 million. Of these, 14,000 are known and 7,000 are considered to have varying levels of edibility. More than 2,000 species are safe and 700 are documented to have considerable pharmacological properties [2, 4, 5, 6].
A series of species have been characterized as hazardous to health and defined as toxic species. Toxic substances are also found in some mushroom species with beneficial properties [7]. The ingestion of mushrooms containing toxins is accidental and often occurs through the misidentification of species [8, 9]. This accidental event frequently occurs due to insufficient available data on poisonous mushrooms, including information on potential toxicity [9, 10]. It is critical to characterize the toxicological profile of mushroom species before using them for human consumption. The aim of the current study is to review the poisonous substances present in different species of edible, medicinal, and poisonous mushrooms.
POISONOUS SUBSTANCES IN MUSHROOMS
Several exceptionally potent toxins have already been identified from a number of mushrooms (Table 1). Even consumption of a small amount can be dangerous for humans. Mushroom toxidromes are classified according to the toxins involved and clinical presentations (Table 1). Mushroom toxins have been divided into seven main categories: amatoxins (cyclopeptides), orellanus (Cortinarius species), gyromitrin (monomethylhydrazine), muscarine, ibotenic acid, psilocybin, and coprine [11]. A discussion of these toxins follows, including their sources, molecular properties, clinical manifestations, mechanisms, and potential toxicity (Table 1 and 2).
Table 1.
Clinical manifestations, sites of toxicity, and toxicity potential of various mushroom species

GI, gastrointestinal; GIT, gastrointestinal tract; CNS, central nervous system.
Table 2.
Molecular properties and mechanism of toxicity of different toxins found in various mushroom species
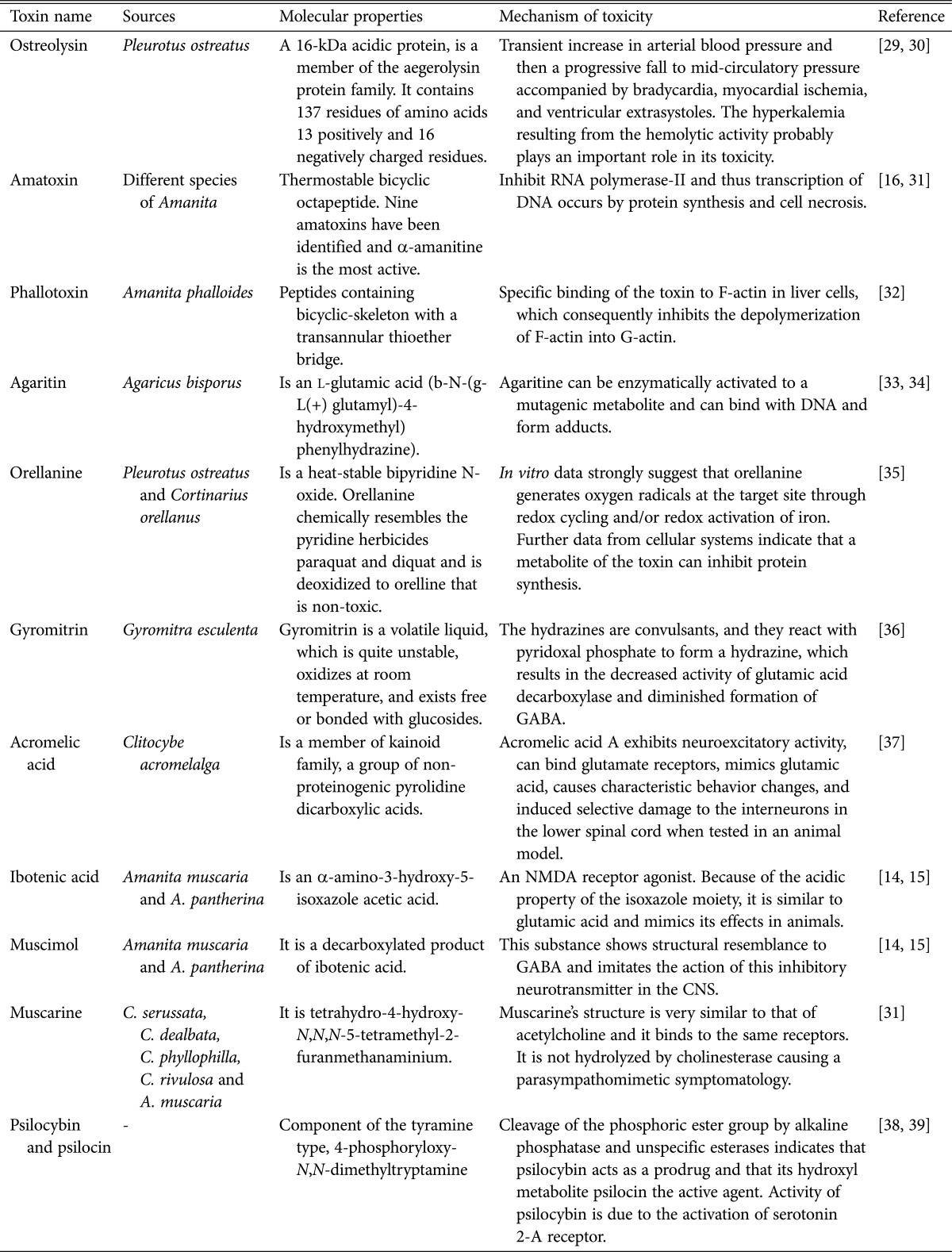
GABA, gamma-aminobutyric acid; NMDA, N-methyl-D-aspartate; CNS, central nervous system.
All amatoxin-containing fungi are found within the families Amanitaceae (genus Amanita), Agaricaceae (genus Lepiota), and Cortinariaceae (genus Galerina). Some species of Amanita such as Amanita virosa, A. phalloides, A. ocreata, A. verna, A. suballiacea, A. bisporigera, A. hygroscopica, and A. tenuifolia are abundant in amatoxins. Amatoxins are bicyclic octapeptides and powerful thermostable poisons [12]. The most potent amatoxin is α-amanitine, and is among the nine amatoxins that have been recognized. Ataxia, motor depression, euphoria, dizziness, gastrointestinal disturbances, drowsiness, muscle twitches, and changes in insight, feelings, and mood are common symptoms associated with amatoxin poisoning [13, 14, 15]. The molecular mechanism of amatoxin action is inhibition of DNA-dependent RNA polymerase-II (Table 2). Depletion of mRNA levels leads to reduced protein synthesis and ultimately the affected cells undergo necrosis or apoptosis [12, 16]. Symptomatic treatments are mainly recommended for this poisoning, including the use of phenobarbitone or benzodiazepines during seizures [17, 18]. Detoxification at the beginning of treatment is essential in amatoxin-intoxicated patients and they need careful monitoring. Liver transplantation may be required in cases of severe poisoning [12].
Gyromitrin is an oxidizable volatile liquid at room temperature, making it an unstable chemical. The toxin gyromitrin is present in some species of Gyromitra. Ingestion of Gyromitra, and even the inhalation of vapors produced during the cooking of this mushroom, can cause toxicity [9, 10]. Diarrhea, vomiting, fatigue, vertigo, ataxia, tremor, and nystagmus are the most common symptoms of this intoxication. Development of hemolysis and hepatic diseases of moderate severity may develop in some patents. Hydrazines, which have convulsant, cytotoxic, and irritating properties, can be formed by the hydrolysis of gyromitrin in the stomach after ingestion [9, 40]. Carcinogenesis is another adverse effect of gyromitrin. Symptoms of intoxication start 8~12 hr after ingestion. The antidote is pyridoxine.
Mushrooms containing coprine may cause addiction when taken with alcohol. This ingredient accumulates in the blood because of alcohol decomposition when alcohol ingestion occurs before, with, or after mushroom intake. Coprinus atramentarius mushrooms contain coprine. The antidote is not known. Some species of Clitocybe are responsible for causing muscarinic syndrome. Muscarine is abundant in C. rivulosa, C. dealbata, C. cerussata, C. phyllophila, and C. candicans. It is also present in Amanita muscaria and the Inocybe genus. Symptoms of muscarinic syndrome include increased pulse rate, headache, nausea, vomiting, dizziness, and rapid breathing. Affected patients may show hypersecretion, miosis, and gastrointestinal disturbance. Bradycardia and even collapse may occur in severe cases of intoxication with this poison [28].
The symptoms of muscarinic poisoning caused by ingestion of mushrooms are sweating, tearing, drooling, vomiting, diarrhea, blood pressure, and shortness of breath due to effects on the parasympathetic nervous system. Most patients recover within 24 hr, except in cases when the heart has stopped and the patient cannot be revived. Symptomatic treatment is recommended to treat this syndrome. Administration of atropine is recommended to neutralize the muscarinic effects [28]. Poisonous mushrooms also contain muscimol. It causes paralysis 20~22 min after ingestion by acting on the central nervous system. Muscimol can serve as an insecticide and can kill flies. The mushrooms containing muscimol are Amanita muscaria and Tricholoma muscarium. The antidote is physostigmine.
Psilocybin is found abundantly in the genus Psilocybe [41]. Common mushrooms that contain psylocibin include P. bohemica, P. mexicana, P. semilanceata, P. baeocystis, and P. cubensis [40]. The toxicity symptoms of psilocybin develop 30 min after ingestion of these mushrooms. Frequently reported symptoms of this intoxication include hypertension, tachycardia, visual problems, nausea, anxiety, asthenia, vertigo, mydriasis, motor incoordination, and disorientation. Psilocybin toxicity-associated problems resolve completely 4~12 hr after ingestion. Generally, hospitalization is not required and myocardial infarction in adults after intoxication with psilocybin-containing mushrooms is rare. Coma, hyperthermia, and seizures may occur in children [40].
Indole derivative-containing psilocin mushrooms are usually blue in color. Symptoms of psilocin toxicity include curly limbs, tongue anxiety, poor comprehension, colorful hallucinations, and auditory hallucinations. The mushrooms containing psilocin are Panaeolus papilionaceus, Panaeolus sphinctrinus, and Panaeolus subbalteatus. The antidote is chlorpromazine. An example of a lampterol-containing mushroom is Lampteromyces japonicus [42]. Symptoms of lampterol poisoning include vomiting, diarrhea, and abdominal pain. The symptoms of poisoning with fasciculol-containing mushrooms are vomiting, diarrhea, and nerve paralysis. The mushrooms containing fasciculol are Naematoloma fasciculare and Hypholoma fasciculare.
After ingestion, choline in poisonous mushrooms is converted into acetylcholine in the body. Symptoms of choline toxicity include increased blood pressure, decreased heart rate, pupil contraction, increased blood flow, and increased digestive system activity. The mushrooms containing choline are Rhodophyllus rhodopolius, Russula emetic, and Lactarius chrysorrheus. Symptoms of poisoning with glyzicin-containing mushrooms occur 4~5 days after ingestion, and last more than one month. An example glyzicin-containing poisonous mushroom is Clitocybe acromelalga. Severe pain in the hands and feet, caused by peripheral neuropathy, lasts for over a month, but is not fatal.
Orellanine is a heat-stable bipyridine N-oxide. The cyclopeptide orellanine is present in C. orellanus and C. speciosissimus and hence these two mushrooms are nephrotoxic. The quinone class of compounds may assemble in renal tissue due to the oxidation of orellanine, and covalent binding of biological structures with those quinones may cause cell damage [8]. Orellanine toxicity symptoms may arise 2~20 days after ingestion. Nausea, abdominal pain, and vomiting are symptoms in the early stages of toxicity. Chills, intense thirst, oliguria or polyuria, and probably anuria follow these. It is usually recommended to continue hemodialysis until there are gradual improvements in renal function [43]. It is evident from in vitro data that orellanine generates oxygen radicals at the target site through the redox activation of iron and/or redox cycling. It has also been demonstrated with advanced information on cellular systems that protein synthesis can be inhibited by a metabolite of orellanine [35].
CONCLUSION
There are a large number of mushroom poisoning cases reported every year in areas with high mushroom consumption. Insufficient knowledge and misidentification of species are the leading causes of mushroom intoxication. Some species contain hazardous toxins in varying proportions that cause diverse signs and syndromes. Not only toxic mushrooms but also some edible mushrooms contain poisonous compounds and the severity of intoxication is dependent on the amount consumed. Accidental ingestion of mushrooms is difficult to avoid when there is a lack of knowledge and awareness about mushroom poisoning. Accurate recognition of mushrooms is a fundamental step in avoiding toxicity and enabling successful treatment through the rapid detection of intoxication symptoms. Cases of fatal mushroom poisoning have been reported previously; however, the properties of toxins, syndromes, and mechanisms of toxicity have not been summarized. Thus, it is crucial to review information on mushroom toxins and their fatality. Careful experimental and clinical investigations are required to identify the possible side effects of edible and medicinal mushrooms and enable their safe consumption.
Fig. 1.
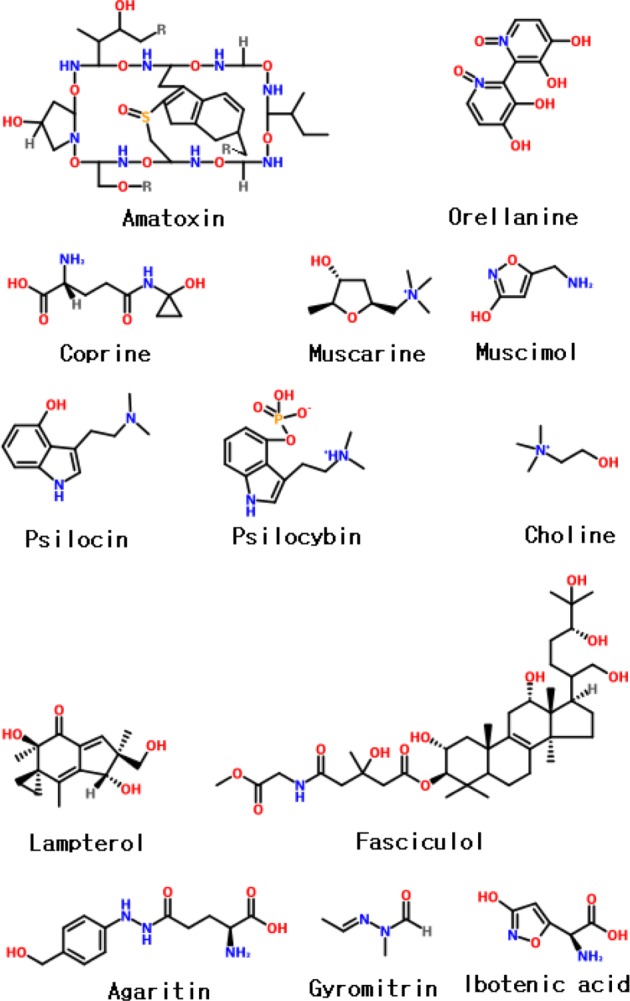
Chemical structures of various mushroom toxins.
ACKNOWLEDGEMENTS
This work was supported in part by the Technology Development Program for Agriculture and Forestry, Ministry for Food, Agriculture, Forestry and Fisheries and in part by a grant (no. PJ009007) from the Next-Generation BioGreen 21 Program, Rural Development, South Korea.
References
- 1.Warner M, Chen LH, Makuc DM, Anderson RN, Miniño AM. Drug poisoning deaths in the United States, 1980-2008 [Internet] Atlanta: Centers for Disease Control and Prevention; 2011. [cited 2013 Feb 21]. Available from: http://www.cdc.gov/nchs/data/databriefs/db81.htm. [Google Scholar]
- 2.Wasser SP. Medicinal mushrooms as a source of antitumor and immunomodulating polysaccharides. Appl Microbiol Biotechnol. 2002;60:258–274. doi: 10.1007/s00253-002-1076-7. [DOI] [PubMed] [Google Scholar]
- 3.Gao Y, Chan E, Zhou S. Immunomodulating activities of Ganoderma, a mushroom with medicinal properties. Food Rev Int. 2004;20:123–161. [Google Scholar]
- 4.Chang R. Functional properties of edible mushrooms. Nutr Rev. 1996;54(11 Pt 2):S91–S93. doi: 10.1111/j.1753-4887.1996.tb03825.x. [DOI] [PubMed] [Google Scholar]
- 5.Wasser SP, Weis AL. Therapeutic effects of substances occurring in higher Basidiomycetes mushrooms: a modern perspective. Crit Rev Immunol. 1999;19:65–96. [PubMed] [Google Scholar]
- 6.Reshetnikov SV, Tan KK. Higher basidiomycota as a source of antitumor and immunostimulating polysaccharides (review) Int J Med Mushrooms. 2001;3:361–394. [Google Scholar]
- 7.Nieminen P, Kirsi M, Mustonen AM. Suspected myotoxicity of edible wild mushrooms. Exp Biol Med (Maywood) 2006;231:221–228. doi: 10.1177/153537020623100213. [DOI] [PubMed] [Google Scholar]
- 8.Karlson-Stiber C, Persson H. Cytotoxic fungi: an overview. Toxicon. 2003;42:339–349. doi: 10.1016/s0041-0101(03)00238-1. [DOI] [PubMed] [Google Scholar]
- 9.Flesch F, Saviuc P. Intoxications par les champignons: principaux syndromes et traitement. EMC Med. 2004;1:70–79. [Google Scholar]
- 10.White J, Warrell D, Eddleston M, Currie BJ, Whyte IM, Isbister GK. Clinical toxinology: where are we now? J Toxicol Clin Toxicol. 2003;41:263–276. doi: 10.1081/clt-120021112. [DOI] [PubMed] [Google Scholar]
- 11.Lin YM, Wang TL. Mushroom poisoning. Ann Disaster Med. 2004;3(Suppl 1):S8–S11. [Google Scholar]
- 12.Wong JH, Ng TB. Toxins from Basiodiomycete fungi (mushrooms): amatoxins, phallotoxins and virotoxins. In: Kastin AJ, editor. Handbook of biologically active peptides. San Diego: Elsevier; 2006. pp. 131–135. [Google Scholar]
- 13.Tsujikawa K, Mohri H, Kuwayama K, Miyaguchi H, Iwata Y, Gohda A, Fukushima S, Inoue H, Kishi T. Analysis of hallucinogenic constituents in Amanita mushrooms circulated in Japan. Forensic Sci Int. 2006;164:172–178. doi: 10.1016/j.forsciint.2006.01.004. [DOI] [PubMed] [Google Scholar]
- 14.Tsujikawa K, Kuwayama K, Miyaguchi H, Kanamori T, Iwata Y, Inoue H, Yoshida T, Kishi T. Determination of muscimol and ibotenic acid in Amanita mushrooms by high-performance liquid chromatography and liquid-chromatography-tandem mass spectrometry. J Chromatogr B Analyt Technol Biomed Life Sci. 2007;852:430–435. doi: 10.1016/j.jchromb.2007.01.046. [DOI] [PubMed] [Google Scholar]
- 15.Størmer FC, Koller GE, Janak K. Ibotenic acid in Amanita muscaria spores and caps. Mycologist. 2004;18:114–117. [Google Scholar]
- 16.Wieland T, Götzendörfer C, Zanotti G, Vaisius AC. The effect of the chemical nature of the side chains of amatoxins in the inhibition of eukaryotic RNA polymerase B. Eur J Biochem. 1981;117:161–164. doi: 10.1111/j.1432-1033.1981.tb06315.x. [DOI] [PubMed] [Google Scholar]
- 17.Michelot D, Melendez-Howell LM. Amanita muscaria: chemistry, biology, toxicology and ethnomycology. Mycol Res. 2003;107:131–146. doi: 10.1017/s0953756203007305. [DOI] [PubMed] [Google Scholar]
- 18.Satora L, Pach D, Ciszowski K, Winnik L. Panther cap Amanita pantherina poisoning case report and review. Toxicon. 2006;47:605–607. doi: 10.1016/j.toxicon.2006.01.008. [DOI] [PubMed] [Google Scholar]
- 19.Rumack BH, Spoerke DG. Handbook of mushroom poisoning: diagnosis and treatment. Boca Raton: CRC Press; 1994. p. 330. [Google Scholar]
- 20.Goldfrank LR. Mushrooms. In: Nelson LS, Lewin NA, Howland MA, Hoffman RS, Goldfrank LR, Flomenbaum NE, editors. Goldfrank's toxicologic emergencies. 9th ed. New York: McGraw-Hill; 2011. p. 1522. [Google Scholar]
- 21.Brent J, Palmer RB. Mushrooms. In: Shannon MW, Borron SW, Burns MJ, editors. Haddad and Winchester's clinical management of poisoning and drug overdose. 4th ed. Philadelphia: Saunders Elsevier; 2007. pp. 455–472. [Google Scholar]
- 22.Curtis DR, Lodge D, McLennan H. The excitation and depression of spinal neurones by ibotenic acid. J Physiol. 1979;291:19–28. doi: 10.1113/jphysiol.1979.sp012796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ennecker-Jans AS, Van Daele PL, Blonk MI, Varin DS, Van Laar JA. Amatoxin poisoning due to soup from personally picked deathcap mushrooms (Amanita phalloides) Ned Tijdschr Geneeskd. 2007;151:764–768. [PubMed] [Google Scholar]
- 24.Aygul N, Duzenli MA, Ozdemir K, Altunkeser BB. A case report of unusual complication of Amanita phalloides poisoning: development of cardiogenic shock and its successful treatment with intra-aortic balloon counterpulsation. Toxicon. 2010;55:630–632. doi: 10.1016/j.toxicon.2009.10.022. [DOI] [PubMed] [Google Scholar]
- 25.Mount P, Harris G, Sinclair R, Finlay M, Becker GJ. Acute renal failure following ingestion of wild mushrooms. Intern Med J. 2002;32:187–190. doi: 10.1046/j.1444-0903.2001.00199.x. [DOI] [PubMed] [Google Scholar]
- 26.Bedry R, Baudrimont I, Deffieux G, Creppy EE, Pomies JP, Ragnaud JM, Dupon M, Neau D, Gabinski C, De Witte S, et al. Wild-mushroom intoxication as a cause of rhabdomyolysis. N Engl J Med. 2001;345:798–802. doi: 10.1056/NEJMoa010581. [DOI] [PubMed] [Google Scholar]
- 27.Saviuc PF, Danel VC, Moreau PA, Claustre AM, Ducluzeau R, Carpentier PH. Acute erythermalgia: look for mushroons. Rev Med Interne. 2002;23:394–399. doi: 10.1016/s0248-8663(02)00576-3. [DOI] [PubMed] [Google Scholar]
- 28.Dehay MH, de Sainte Mareville F, Assez N, Dherbecourt V, Goldstein P. Syndrome muscarinique par ingestion de champignon: à propos de deux cas dont un mortel. Eur J Emerg. 2009;22:18–23. [Google Scholar]
- 29.Zuzek MC, Macek P, Sepcić K, Cestnik V, Frangez R. Toxic and lethal effects of ostreolysin, a cytolytic protein from edible oyster mushroom (Pleurotus ostreatus), in rodents. Toxicon. 2006;48:264–271. doi: 10.1016/j.toxicon.2006.05.011. [DOI] [PubMed] [Google Scholar]
- 30.Berne S, Sepcić K, Anderluh G, Turk T, Macek P, Poklar Ulrih N. Effect of pH on the pore forming activity and conformational stability of ostreolysin, a lipid raft-binding protein from the edible mushroom Pleurotus ostreatus. Biochemistry. 2005;44:11137–11147. doi: 10.1021/bi051013y. [DOI] [PubMed] [Google Scholar]
- 31.Bédry R, Saviuc P. Severe mushroom poisoning excluding Amanita phalloides syndrome. Reánimation. 2002;11:524–532. [Google Scholar]
- 32.Kobayashi N, Endo S, Kobayashi H, Faulstich H, Wieland T, Munekata E. Comparative study on the formation of phalloidin, viroisin and related derivatives in aqueous solution. Eur J Biochem. 1995;232:726–736. [PubMed] [Google Scholar]
- 33.Walton K, Coombs MM, Walker R, Ioannides C. The metabolism and bioactivation of agaritine and of other mushroom hydrazines by whole mushroom homogenate and by mushroom tyrosinase. Toxicology. 2001;161:165–177. doi: 10.1016/s0300-483x(00)00430-3. [DOI] [PubMed] [Google Scholar]
- 34.Kondo K, Watanabe A, Akiyama H, Maitani T. The metabolisms of agaritine, a mushroom hydrazine in mice. Food Chem Toxicol. 2008;46:854–862. doi: 10.1016/j.fct.2007.10.022. [DOI] [PubMed] [Google Scholar]
- 35.Nilsson UA, Nyström J, Buvall L, Ebefors K, Björnson-Granqvist A, Holmdahl J, Haraldsson B. The fungal nephrotoxin orellanine simultaneously increases oxidative stress and down-regulates cellular defenses. Free Radic Biol Med. 2008;44:1562–1569. doi: 10.1016/j.freeradbiomed.2008.01.017. [DOI] [PubMed] [Google Scholar]
- 36.Arshadi M, Nilsson C, Magnusson B. Gas chromatographymass spectrometry determination of the pentafluorobenzoyl derivative of methylhydrazine in false morel (Gyromitra esculenta) as a monitor for the content of the toxin gyromitrin. J Chromatogr A. 2006;1125:229–233. doi: 10.1016/j.chroma.2006.05.040. [DOI] [PubMed] [Google Scholar]
- 37.Taguchi T, Tomotoshi K, Mizumura K. Excitatory actions of mushroom poison (acromelic acid) on unmyelinated muscular afferents in the rat. Neurosci Lett. 2009;456:69–73. doi: 10.1016/j.neulet.2009.03.102. [DOI] [PubMed] [Google Scholar]
- 38.Musshoff F, Madea B, Beike J. Hallucinogenic mushrooms on the German market: simple instructions for examination and identification. Forensic Sci Int. 2000;113:389–395. doi: 10.1016/s0379-0738(00)00211-5. [DOI] [PubMed] [Google Scholar]
- 39.Vollenweider FX, Vollenweider-Scherpenhuyzen MF, Bäbler A, Vogel H, Hell D. Psilocybin induces schizophrenia-like psychosis in human via serotonin-2 agonist action. Neuroreport. 1998;9:3897–3902. doi: 10.1097/00001756-199812010-00024. [DOI] [PubMed] [Google Scholar]
- 40.Berger KJ, Guss DA. Mycotoxins revisited: part II. J Emerg Med. 2005;28:175–183. doi: 10.1016/j.jemermed.2004.08.019. [DOI] [PubMed] [Google Scholar]
- 41.Keller T, Schneider A, Regenscheit P, Dirnhofer R, Rücker T, Jaspers J, Kisser W. Analysis of psilocybin and psilocin in Psilocybe subcubensis Guzmán by ion mobility spectrometry and gas chromatography-mass spectrometry. Forensic Sci Int. 1999;99:93–105. doi: 10.1016/s0379-0738(98)00168-6. [DOI] [PubMed] [Google Scholar]
- 42.Nakanishi K, Ohashi M, Tada M, Yamada Y. Illudins (Lampterol) Tetrahedron. 1965;21:1231–1246. doi: 10.1016/0040-4020(65)80065-5. [DOI] [PubMed] [Google Scholar]
- 43.Tegzes JH, Puschner B. Toxic mushrooms. Vet Clin North Am Small Anim Pract. 2002;32:397–407. doi: 10.1016/s0195-5616(01)00012-2. [DOI] [PubMed] [Google Scholar]


