Abstract
AIM
To present the results of same-day topography-guided photorefractive keratectomy (TG-PRK) and corneal collagen crosslinking (CXL) after previous intrastromal corneal ring segment (ISCR) implantation for keratoconus.
METHODS
An experimental clinical study on twenty-one eyes of 19 patients aged 27.1±6.6y (range 19-43y), with low to moderate keratoconus who were selected to undergo customized TG-PRK immediately followed by same-day CXL, 9mo after ISCR implantation in a university ophthalmology clinic. Refraction, uncorrected distance visual acuities (UDVA) and corrected distance visual acuities (CDVA), keratometry (K) values, central corneal thickness (CCT) and coma were assessed 3mo after TG-PRK and CXL.
RESULTS
After TG-PRK/CXL: the mean UDVA (logMAR) improved significantly from 0.66±0.41 to 0.20±0.25 (P<0.05); Kflat value decreased from: 48.44±3.66 D to 43.71±1.95 D; Ksteep value decreased from 45.61±2.40 D to 41.56±2.05 D; Kaverage also decreased from 47.00±2.66 D to 42.42±2.07 D (P<0.05 for all). The mean sphere and cylinder decreased significantly post-surgery from, -3.10±2.99 D to -0.11±0.93 D and from -3.68±1.53 to -1.11±0.75 D respectively, while the CDVA, CCT and coma showed no significant changes. Compared to post-ISCR, significant reductions (P<0.05 or all) in all K values, sphere and cylinder were observed after TG-PRK/CXL.
CONCLUSION
Same-day combined topography-guided PRK and corneal crosslinking following placement of ISCR is a safe and potentially effective option in treating low-moderate keratoconus. It significantly improves all visual acuity, reduced keratometry, sphere and astigmatism, but causes no change in central corneal thickness and coma.
Keywords: keratoconus, astigmatism, photorefractive keratectomy, corneal collagen crosslinking, intrastromal corneal rings
INTRODUCTION
Keratoconus is a chronic non-inflammatory, asymmetric and usually bilateral cornea degeneration, characterized by localized corneal thinning, visual distortion, corneal steepening, and central corneal scarring[1],[2]. Its onset is usually in young adult hood but often becomes apparent during the second decade of life, progressing until the fourth decade of life, when it usually stabilizes[3]–[6]. Although, predicting the severity and time of progression of the disease is hard, progress is usually more rapid in the first affected eye and happens in a period of 3-8y[5],[7].
The ocular symptoms and signs of the disease vary widely with the disease severity[3]. At the earliest stage, unless corneal topography is assessed, keratoconus can go unnoticed by the practitioner, due to the absence of symptoms[8]. There is a significant loss of visual acuity (VA) which cannot be corrected with spectacles, and the appearance of a ‘scissor-like’ reflex motion on retinoscopy, suggesting the development of irregular astigmatism. Keratometer readings are commonly within the normal range but may have irregular mires. Corneal topography may reveal corneal thinning with the thinnest part of the cornea located outside the visual axis[1]. In the later (moderate to advanced) stage of the disease, Fleischer's ring, Vogt's striae, Rizzuti's sign, Munson's sign, and the increased visibility of cornea nerves become apparent[9]. Corneal scarring may eventually develop in the majority of contact lens wearers.
Treatment options comprise first: the use of spectacle or rigid gas permeable contact lenses at the early stages; second, restoring the integrity of the cornea by surgical techniques such as intracorneal ring segments and collagen crosslinking (CXL)[9],[10]. However, lamellar or penetrating keratoplasty are considerable options in the advanced stages of keratoconus, where the aim is often to improve patient's quality of life[11].
Collagen crosslinking treatment uses riboflavin and ultraviolet-A (UVA) irradiation to strengthen the cornea by augmenting the crosslinks between collagen fibrils, thereby stabilizing the condition[12]. Studies on CXL have reported stability in progression of the disorder, but with minimal improvement in vision quality of patients[13]–[15]. For this reason, combined procedures have been proposed to maximize the results from CXL: conductive keratoplasty followed by CXL; Intrastromal corneal ring (ISCR) implantation and subsequent photorefractive keratectomy (PRK)/CXL; and simultaneous wavefront-guided PRK combined with CXL[16]–[20]. Recent studies have reported promising results in the improvement of visual outcomes, and stability of the disease condition using a combined treatment of topography-guided photorefractive keratectomy (TG-PRK) and CXL[17]–[19],[21]–[24]. Kanellopoulos[23] showed that same-day simultaneous TG-PRK and CXL was superior to sequential CXL with later PRK in the visual rehabilitation of progressing keratoconus. In this study, we present the results of same-day topography-guided photokeratectomy combined with CXL, performed three months after ISCR implantation in the treatment of progressive keratoconus.
SUBJECTS AND METHODS
Study Population
Twenty-one eyes of 19 keratoconus patients [fifteen males (79%) and four females (21%)] of age 19-43y were recruited in this study. All patients underwent ISCR implantation followed by same-day TG-PRK and CXL. These patients were recruited randomly from patients already scheduled to undergo the surgery technique in our hospital after the research protocol was explained, and informed consent obtained, from each subject. The hospital research review board approved the study protocol and study procedures conformed to the tenets of the Declaration of Helsinki 1975 as revised in Fortaleza 2013.
Patients were included if: they were intolerant to contact lens wear, showed low-grade to moderate keratoconus, and progression in keratoconus observed over the previous 6mo; and excluded in the presence of any of the following conditions: central or paracentral corneal scarring; central pachymetry less than 400 µm, as measured by ultrasound pachymeter (DGH Technology Inc, Exon, PA, USA); pregnancy and lactation; severe dry-eye disease; systemic autoimmune disease; and/or a history of herpetic keratitis. Keratoconus was graded based on Amsler-Krumeich classification in accordance with the distribution area of the ectasia as has been described by Gómez-Miralles et al[25] There were eleven eyes (52.4%) with low keratoconus and ten eyes (47.6%) with moderate keratoconus.
However, progression of keratoconus (KC) was defined as one or more of the following changes over a period of 6mo: an increase of ≥1.00 D in K-max, an increase of ≥1.00 D manifest cylinder, or an increase of ≥0.50 D in manifest refraction spherical equivalent. All patients were seeking for relief from their refractive error.
Data Collection
Clinical evaluation of general and ocular health was performed pre-operatively. For all patients, the same optometrists also assessed the following visual parameters, at baseline, after ISCR, at last follow-up (average of 9mo) after ISCR but prior to TG-PRK/CXL, and three months after TG-PRK/CXL: uncorrected distance visual acuity [UDVA(logMAR)], corrected distance visual acuity [CDVA(logMAR)] were obtained by the Snellen projected eye chart; mean manifest cylinder and mean sphere by objective refraction were thrice obtained and averages recorded; topographical keratometry values (D) and Coma (µm) were once obtained by the Schwind Corneal wavefront Analyzer (Eye-tech-Solutions, GmbH & Co. Kleinostheim, Germany). All data were analyzed for normality. All data were entered into a Microsoft Excel 2007 spreadsheet (Microsoft, Inc, Redmond, Washington, USA). The mean, standard deviation, minimum and maximum values were calculated and presented descriptively in a table and figure where applicable. To study the differences in all tested parameters pre- and post-treatments, a Student's t-test analysis was conducted to compare the baseline with first-step; baseline with second step; first step with second step, post-surgical outcome values. All statistical analyses were conducted using the Graphpad Instat software (version 3.00-Graph pad Software Inc., San Diego, CA, USA). A P value <0.05 (α) was considered statistically significant, and with 20 eyes the study had a power of 80% as calculated using the G power software 3.1.3 version.
Surgical Procedures
All procedures-the first step (ISCR) and the second step (TG-PRK/CXL)-in all patients were performed in the University Ophthalmology clinic by the same ophthalmologist (WA) under sterile conditions. As a first step, all eyes underwent femtosecond laser-enabled (Intralase FS, Intralase Corp./Abbott Medical Optics, Inc. Abbott Park, Illinois, USA) placement of ISCR using the Keraring (Mediphacos, Brazil). Segment sizes were determined according to the nomogram provided by the manufacturer. Depth of the ring channels was set at 75%-80% of the thinnest pachymetry reading. At the end of the surgery, antibiotic and corticosteroid eye drops were administered, a bandage contact lens was fitted, and slit-lamp examination was conducted. About three to five days later, the bandage contact lens was removed after the epithelial defect at the site of incision had closed.
The patients were followed after ISCR implantation for at least 3mo and at most 24mo until stabilization of refraction was achieved. Subsequently, the patients underwent a second step TG-PRK followed by same-day riboflavin-UVA CXL during same session. De-epithelialization was performed in all cases by phototherapeutic keratectomy (PTK) using the Schwind Amaris laser platform (SCHWIND Eye-tech-Solutions, GmbH & Co. Kleinostheim, Germany), so as to smooth the anterior irregular cornea. The PTK ablation was performed to remove 50 µ of the central 6.5 mm of corneal epithelium prior to performing TG-PRK treatments with a 6 mm optical zone. The aim was to normalize the cornea by reducing irregular astigmatism while treating part of the refractive error. This depth was chosen to minimize tissue ablation and reduce the risk of iatrogenic ectasia as was reported in a previous study[10]. Mitomycin C 0.02 mg/mL was then applied for 30s for all TG-PRK procedures.
Shortly after PRK, the CXL treatment was initiated by instilling 0.1% riboflavin solution in the center of the cornea every 2 to 3min for 30min. Then UVA irradiation was performed at the central 8.0 mm diameter of the cornea using a UVX system (Peshke, Inc.) of wavelength 365 nm for 30min at irradiance of 3.0 mJ/cm2; during this time, riboflavin drops were instilled every 2min. After CXL, the corneal surface was irrigated with a cold balanced salt solution kept at 4°C, antibiotic and corticosteroid eye drops were administered, a bandage contact lens was fitted until full re-epithelialization, and the eyes were examined at the slitlamp. The bandage contact lens was removed when total epithelialization was observed (between 3d to 5d) and post-operative medication included: diclofenac sodium 0.1% (Voltaren) drops for 2d and tobramycin/dexamethasone drops 4 times daily until bandage contact lens was removed. In all cases, a silicon-hydrogel lens (Air Optix [Ciba Vision] of material lotrafilcon B, diameter 14.0 mm, base curve 8.6 mm, and Dk of 140 barrers, was used as bandage contact lens.
Safety index was calculated by the ratio: post-keraring placement CDVA/baseline CDVA (in logMAR). Efficacy index was calculated by the ratio: post-keraring placement UDVA/baseline CDVA (in logMAR).
RESULTS
The descriptive statistics of the mean±standard deviation values of the visual and refractive outcomes at baseline (pre-ISCR), after the first-step (post-ISCR), pre-2nd step (pre-TG-PRK/CXL) and at after the second step (post-TG-PRK/CXL), and the results of the paired t-test analysis has been shown in Table 1.
Table 1. Descriptive statistics and results of paired t-test conducted on mean±standard deviation (range) values obtained from 21 eyes with low-grade-moderate keratoconus pre-operatively (baseline), post-intracorneal ring segment implantation (1st step), and subsequent same-day topography-guided photorefractive keratectomy & corneal collagen cross linking (2nd step).
| Outcomes | Baseline | Post-1st step | 1P | Pre-2nd step | Post-2nd step | 2P | 3P |
| UDVA (logMAR) | 0.66±0.41 (0.05 to 1.30) | 0.31±0.18 (0.00 to 0.70) | 0.01 | 0.28±0.37 (0.00 to 1.00) | 0.20±0.25 (0.00 to 1.00) | 0.17 | 0.01 |
| CDVA (logMAR) | 0.21±0.22 (-0.10 to 0.70) | 0.28±0.73 (0.00 to 1.00) | >0.05 | 0.28±0.73 (0.00 to 1.00) | 0.03±0.04 (0.00 to 0.15) | 0.10 | 0.03 |
| Ksteep (D) | 48.44±3.66 (42.40 to 54.42) | 45.98±2.53 (43.42 to 51.30) | <0.0001 | 44.18±2.90 (40.66 to 50.58) | 43.71±1.95 (39.59 to 46.68) | 0.0007 | <0.05 |
| Kflat (D) | 45.61±2.40 (41.74 to 50.27) | 44.18±2.90 (40.66 to 50.58) | 0.0003 | 45.98±2.50 (43.54 to 51.30) | 41.56±2.05 (37.90 to 45.90) | 0.0005 | <0.05 |
| Kaverage (D) | 47.00±2.66 (41.57 to 52.35) | 45.01±2.34 (42.21 to 50.80) | 0.0001 | 47.00±2.66 (41.57 to 52.35) | 42.42±2.07 (39.18 to 46.29) | 0.0001 | <0.05 |
| Sphere (D) | -3.10±2.99 (-9 to +3) | -1.33±1.51 (-3.25 to +0.5) | 0.004 | -1.67±1.97 (-5.75 to +1.50) | -0.11±0.93 (-2.75 to 1.50) | 0.02 | <0.05 |
| Cylinder (D) | -3.68±1.53 (-6.0 to -1.25) | -1.81±1.49 (-0.5 to -6.0) | <0.0001 | -2.10±1.45 (-6.0 to -0.50) | -1.11±0.75 (-3.00 to 0.00) | 0.02 | <0.05 |
| Coma (µm) | 2.13±1.25 (1.40 to 4.54) | 1.65±0.97 (0.50 to 3.86) | >0.05 | 1.57±0.68 (0.70 to 2.90) | 1.58±0.75 (0.68 to 2.97) | >0.14 | >0.05 |
| CCT (µm) | 496.94±31.39 (443 to 565) | 492.90±15.02 (477 to 521) | 0.38 | 492.90±15.02 (477 to 521) | 469.82±33.60 (425 to 526) | 0.29 | 0.27 |
1,2,3P values of post-hoc analysis 1st step versus baseline, 1st step versus 2nd step, baseline versus 2nd step respectively. UDVA: Uncorrected distance visual acuity in logMAR; CDVA: Corrected distance visual acuity in logMAR; CCT: Central corneal thickness; D: Diopter; 1st step: Intrastromal corneal ring implantation; 2nd step: Topography-guided photorefractive keratectomy and collagen cross linking.
Comparison of Baseline and Post-ISCR (1st step) and Post-TG-PRK/CXL (2nd step) Outcomes
Mean follow-up was 9.0±5.7mo (range 3-24mo) post-ISCR and 3mo post TG-PRK/CXL. From Table 1, it could be deduced that: compared to baseline (pre-ISCR), the mean UDVA, the mean K-values, the mean sphere, and the mean cylinder, all showed statistically significant improvements after the first step and after the second step (paired t-test: P<0.05, for both steps); the K values (Kmax, Kmin, Kaverage) showed significant decreases, so did the spherical and cylindrical refractive components, 3mo after PRK/CXL. The improvement in mean CDVA from baseline to post-ISCR was not statistically significant (paired t-test: P>0.05); however, the improvement post-TG-PRK/CXL was statistically significant (paired t-test: P=0.03). There was no significant change from baseline (pre-ISCR) to after treatment (post-ISCR and post-TG-PRK/CXL) in the mean CCT and in the mean coma, both of which decreased.
However, between the first step (post-ISCR) and the second step (post-TG-PRK/CXL), the improvements in mean UDVA, mean CDVA; the reductions in mean coma and mean CCT, were not statistically significant (paired t-test: P>0.05, for the four comparisons), while the decrease in K values, the decrease in mean spherical and mean cylindrical refractive components were all statistically significant (paired t-test: P<0.05, for the five comparisons) three months after TG-PRK/CXL (Table 1). Patient topographic improvements can be seen in the Schwind wavefront analyzer before, after ISCR and after TG-PRK/CXL (Figures 1A, 1B, 1C and Figure 2 respectively). There were no intraoperative or postoperative complications.
Figure 1. An example of a patient's right eye topographic maps (obtained by Schwind eye-tech-solutions, wavefront analyzer).
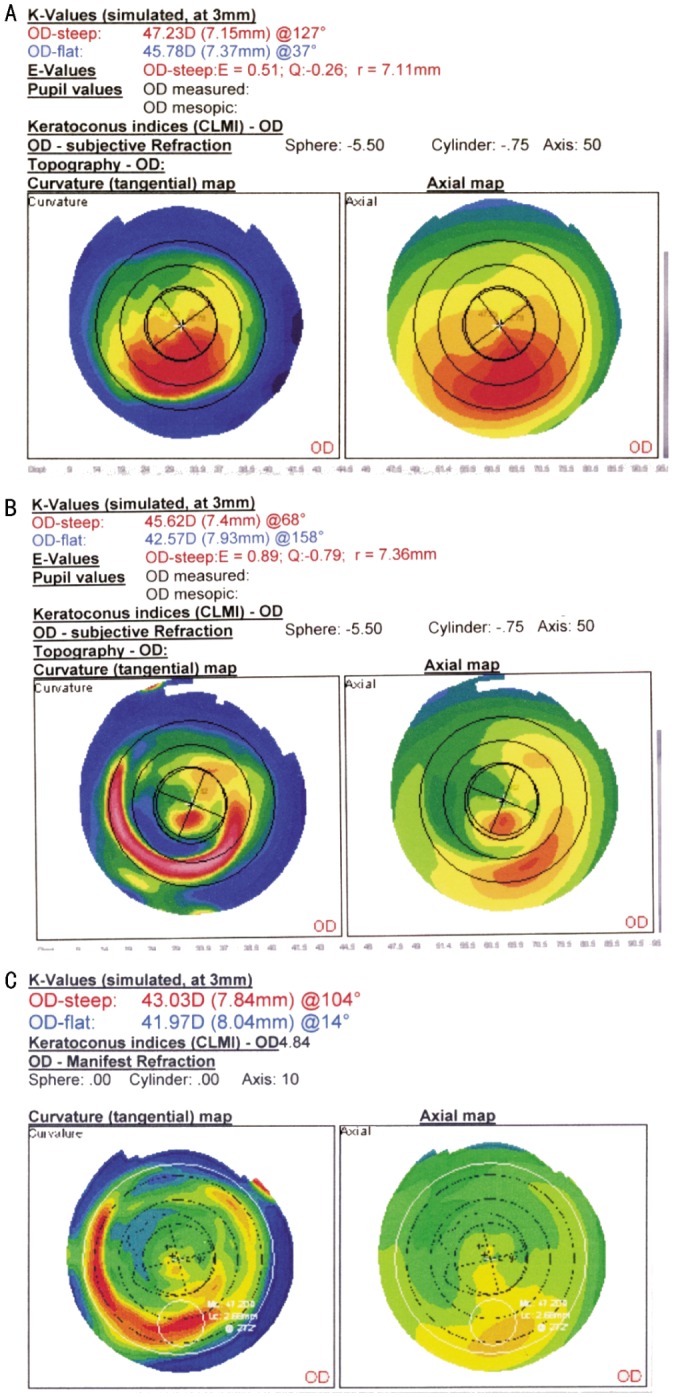
A: Before intra-stromal corneal ring implantation, (before 1st step-ISCR) treatment for keratoconus; B: After intra-stromal corneal ring implantation, (before 2nd step-ISCR) treatment for keratoconus, showing significant improvement; C: After TG-PRK/CXL, ( 2nd step-ISCR) treatment for keratoconus, showing significant improvement.
Figure 2. Bar graph showing change in uncorrected distance visual acuity (UCVA), and corrected distance visual acuity (CDVA), before and after the second step procedure (TG-PRK/CXL) for low to moderate keratoconus. It shows that approximately 71% of eyes and 24% of eyes gained at least three lines of UCVA and CDVA respectively, at last follow-up examination.
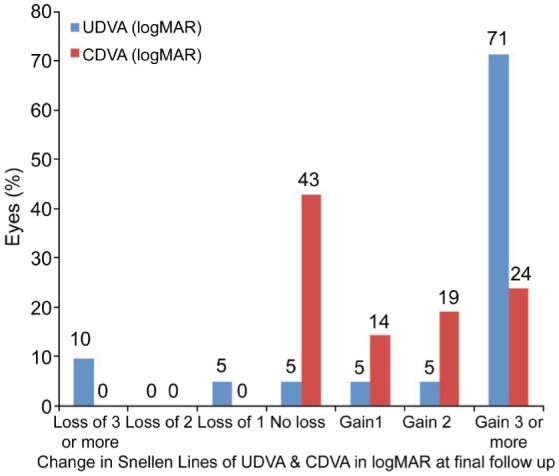
Regarding the method safety, 71% (15/21) of eyes gained three or more lines, 5% (1/21) each gained one and two lines respectively, while 10% (2/21) and 5% (1/21) of eyes each lost more than three lines and one line of UDVA respectively (which was corrected with spectacles), three months after PRK/CXL. Generally, UDVA was available in 17 out of 21 eyes at final follow-up (Figure 2) and an improvement in CDVA of at least one Snellen acuity line [57% (12/21) of eyes]. After the second step, the safety index was estimated to be 1.33 and efficacy index to be 0.46. As shown in Figure 2, at the last follow-up examination, 5% (1/21) eyes lost 1 line of BCVA.
DISCUSSION
Collagen crosslinking with riboflavin and UVA have been shown to be effective in stalling the progression of keratoconus and pellucid marginal degeneration, but with minimal improvement in visual quality, as a result of apical keratometry reduction and consequent corneal regularization[14],[26],[27]. Better results have been shown with a combination of CXL with techniques that improve visual acuity. TG-PRK in combination with CXL was found to yield improved topographic indices and improved UDVA and CDVA, in patients with mild to moderate keratoconus[18]–[20],[28],[29]. Iovieno et al[28] noted significant improvements in UDVA, CDVA, refraction, keratometry, and total aberrations, after six months of Intacs plus PRK/CXL in five eyes. In their study, neither a loss of lines of CDVA, nor a development of haze in any eye, was observed. Another study also reported significant improvements in mean UDVA and CDVA, no loss of lines of CDVA, a significant reduction in mean cylinder, mean apex K-value, and mild haze was observed in 11.1% of treated eyes, after 12mo of TG-PRK/CXL[20]. They[20] also observed that these visual outcomes did not differ significantly between 6 and 12mo after the procedure. In a more recent study[19] conducted on thirteen low-moderate keratoconic eyes, significant improvements were observed in UDVA, CDVA, mean sphere, mean astigmatism, average K, and coma, after six months of TG-PRK/CXL. Also, while no eyes lost lines of CDVA, 63% of eyes gained >2 lines of CDVA, and there was no change in CDVA in approximately 27% of the treated eyes[19]. Kanellopoulos[23] compared the visual functions of 325 eyes that underwent same-day simultaneous TG-PRK/CXL, to those who had sequential CXL with later PRK. They showed that, same-day simultaneous TG-PRK/CXL was superior to sequential CXL with later PRK, in the visual rehabilitation of progressing keratoconus[23]. In that study, the simultaneous group did better (P<0.05) in all fields evaluated: greater significant improvements in UCVA and best spectacle corrected visual acuity (BSCVA), greater mean reduction in spherical equivalent refraction and keratometry, and lesser corneal haze, after about 36mo of the performing the procedures[23]. While all these studies[9],[18]–[20],[23],[28],[29] have shown similar significant improvements in most of the visual functions examined in relation to the current study, they have either been conducted on a different population sample, and/or have not completely agreed in all findings, partly because of the variation in the surgical protocol, data collection/analysis method or follow-up duration.
In the current study, ISCR implantation with the aid of femtosecond laser was performed in 21 eyes of nineteen patients with low to moderate keratoconus, as a first-step procedure. Then, after a follow up period of nine months (when refraction and cornea regularity have stabilized), a second-step procedure was performed which involved a TG-PRK and CXL, performed on the same day, and in the same session. The satisfactory visual, keratometry and topography results obtained after 3mo of this triple procedure is an indication that, the 3 procedures complement one another.
The results showed a significant reduction in the pre-operative mean cylinder, mean sphere, steep K, flat K, and average K values three months after the second step procedure. Significant improvement in the UDVA was also observed in 71% (15/21) of eyes, and in the CDVA, 57% (12/21) of eyes showed improvement of at least one Snellen acuity line, 3mo after combined therapy. No change in CDVA was observed in 43% of eyes (Figure 2). Similar results have been recently reported[19]. However, the study[19] enrolled lesser number of eyes (13 eyes), and their follow-up period was longer (6mo), than that of the current study. From their observation[19] we can therefore deduce that, the improvements in visual functions observed in our subjects, will remain stable or even improve even after 6mo and beyond. In addition, in relation to the first step (post-ISCR) procedure, the current study observed that the second step combined therapy significantly reduced all keratometry values and refractive components, but no significant change in UDVA and CDVA, despite the slight improvement shown. Similarly, CCT and coma were further reduced by about 21 µm (P>0.05) and 2 µm (P>0.05) respectively (Table 1). Tuwairqi et al[18] and Kymionis et al[17] also observed non-statistically significant reductions in coma after treatment of keratoconus with similar procedure. Because the results of postoperative data varied significantly between ISCR and TG-PRK/CXL, we conclude that the same-day combined technique yielded better visual outcomes in patients with mild to moderate keratoconus (Figure 1B vs 1C). This also agrees with previous reports[17],[19],[23],[24],[28],[29].
The first combination of a TG-PRK treatment with CXL on patients with keratoconus was described by Kanellopoulos and Binder, and one study observed that, the technique was more effective when applied on the same day[22],[23]. Subsequently, studies[16],[22] have shown significant improvements in visual outcomes with simultaneous TG-PRK followed by CXL in patient series. Kymionis and cohorts[17] then reported even more improved visual outcomes on performing on the same day, a combination of PRK/CXL treatment after previous ISCR implantation on a patient with pellucid marginal degeneration. Although, the current study observed some loss of lines of UDVA, this was corrected with spectacles, three months after TG-PRK/CXL. Nevertheless, these eyes showed no post-surgical complications, and with a recent study reporting significant improvement of 2.7 lines in UDVA even after one year of paired ISCR combined with CXL, there is a greater tendency that these eyes will also improve in UDVA, few months after our data collection[30].
Even though the result of this study agrees well with previous studies[17],[19],[23],[24],[28]–[30] and provides additional information to encourage surgeons in this region owing to the observed significant visual improvements, which seem to be even more promising in the long term; it is limited by the relatively short period of follow up after the second step procedure. Studies with longer follow-up period are needed to further confirm these findings. Again, recruiting a control group may be necessary to better understand the cause of the changes observed in the current study.
In conclusion, the placement of intracorneal ring segments followed by same-day combined TG-PRK/CXL is a safe procedure that offers patients a functional vision. However, while this procedure appears to stabilize the cornea ecstasia in selected patients with keratoconus, there is also the need to monitor these eyes over a period of at least one year, in order to confirm this.
Acknowledgments
The authors extend their appreciation to the Research Centre, College of Applied Medical Sciences and the Deanship of Scientific Research at King Saud University for funding this research.
Conflicts of Interest: Zeraid FM, None; Jawkhab AA, None; Al-Tuwairqi WS, None; Osuagwu UL, None.
REFERENCES
- 1.Romero-Jiménez M, Santodomingo-Rubido J, Wolffsohn JS. Keratoconus: a review. Cont Lens Anterior Eye. 2010;33(4):157–166. doi: 10.1016/j.clae.2010.04.006. [DOI] [PubMed] [Google Scholar]
- 2.Wagner H, Barr JT, Zadnik K. Collaborative Longitudinal Evaluation of Keratoconus (CLEK) Study: methods and findings to date. Cont Lens Anterior Eye. 2007;30(4):223–232. doi: 10.1016/j.clae.2007.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Robinowitz YS. Keratoconus. Surv Ophthalmol. 1998;42(4):297–319. doi: 10.1016/s0039-6257(97)00119-7. [DOI] [PubMed] [Google Scholar]
- 4.Kennedy RH, Bourne WM, Dyer JA. A 48-year clinical and epidemiologic study of keratoconus. Am J Ophthalmol. 1986;101(3):267–273. doi: 10.1016/0002-9394(86)90817-2. [DOI] [PubMed] [Google Scholar]
- 5.Woodward EG. Keratoconus-epidemiology. J Br Contact Lens Assoc. 1984;7:64–76. [Google Scholar]
- 6.Duke-Elder S, Leigh AG. Keratoconus. In: Duke-Elder S, editor. System of Ophthalmology. Vol. 8. St Louis: Mosby; 1965. pp. 964–976. [Google Scholar]
- 7.Bilgin LK, Yilmaz S, Araz B, Yüksel SB, Sezen T. 30 years of contact lens prescribing for keratoconic patients in Turkey. Cont Lens Anterior Eye. 2009;32(1):16–21. doi: 10.1016/j.clae.2008.07.001. [DOI] [PubMed] [Google Scholar]
- 8.Arntz A, Durán JA, Pijoán JI. Subclinical keratoconus diagnosis by elevation topography. Arch Soc Esp Oftalmol. 2003;78(12):659–664. [PubMed] [Google Scholar]
- 9.Kymionis GD, Siganos CS, Tsiklis NS, Anastasakis A, Yoo SH, Pallikaris AI, Astyrakakis N, Pallikaris IG. Long-term follow-up of Intacs in keratoconus. Am J Ophthalmol. 2007;143(2):236–244. doi: 10.1016/j.ajo.2006.10.041. [DOI] [PubMed] [Google Scholar]
- 10.Tan DT, Por YM. Current treatment options for corneal ectasia. Curr Opin Ophthalmol. 2007;18(4):284–289. doi: 10.1097/ICU.0b013e3281a7ecaa. [DOI] [PubMed] [Google Scholar]
- 11.Yildiz EH, Cohen EJ, Virdi AS, Hammersmith KM, Laibson PR, Rapuano CJ. Quality of life in keratoconus patients after penetrating keratoplasty. Am J Ophthalmol. 2010;149(3):416–422.e1-2. doi: 10.1016/j.ajo.2009.10.005. [DOI] [PubMed] [Google Scholar]
- 12.Wollensak G. Crosslinking treatment of progressive keratoconus: new hope. Curr Opin Ophthalmol. 2006;17(4):356–360. doi: 10.1097/01.icu.0000233954.86723.25. [DOI] [PubMed] [Google Scholar]
- 13.Wittig-Silva C, Whiting M, Lamoureux E, Lindsay RG, Sullivan LJ, Snibson GR. A randomized controlled trial of corneal collagen cross-linking in progressive keratoconus: preliminary results. J Refract Surg. 2008;24(7):S720–725. doi: 10.3928/1081597X-20080901-15. [DOI] [PubMed] [Google Scholar]
- 14.Raiskup-Wolf F, Hoyer A, Spoerl E, Pillunat LE. Collagen crosslinking with riboflavin and ultraviolet-A light in keratoconus: long-term results. J Cataract Refract Surg. 2008;34(5):796–801. doi: 10.1016/j.jcrs.2007.12.039. [DOI] [PubMed] [Google Scholar]
- 15.Coskunseven E, Jankov MR, 2nd, Hafezi F. Contralateral eye study of corneal collagen cross-linking with riboflavin and UVA irradiation in patients with keratoconus. J Refract Surg. 2009;25(4):371–376. doi: 10.3928/1081597X-20090401-02. [DOI] [PubMed] [Google Scholar]
- 16.Kymionis GD, Karavitaki AE, Kounis GA, Portaliou DM, Yoo SH, Pallikaris IG. Management of pellucid marginal corneal degeneration with simultaneous customized photorefractive keratectomy and collagen crosslinking. J Cataract Refract Surg. 2009;35(7):1298–1301. doi: 10.1016/j.jcrs.2009.03.025. [DOI] [PubMed] [Google Scholar]
- 17.Kymionis GD, Grentzelos MA, Portaliou DM, Karavitaki AE, Krasia MS, Dranidis GK, Kozobolis VP. Photorefractive keratectomy followed by same-day corneal collagen crosslinking after intrastromal corneal ring segment implantation for pellucid marginal degeneration. J Cataract Refract Surg. 2010;36(10):1783–1785. doi: 10.1016/j.jcrs.2010.06.044. [DOI] [PubMed] [Google Scholar]
- 18.Tuwairqi WS, Sinjab MM. Safety and efficacy of simultaneous corneal collagen cross-linking with topography-guided PRK in managing low-grade keratoconus: 1-year follow-up. J Refract Surg. 2012;28(5):341–345. doi: 10.3928/1081597X-20120316-01. [DOI] [PubMed] [Google Scholar]
- 19.Al-Tuwairqi W, Sinjab MM. Intracorneal ring segments implantation followed by same-day topography-guided PRK and corneal collagen CXL in low to moderate keratoconus. J Refract Surg. 2013;29(1):59–64. doi: 10.3928/1081597X-20121228-04. [DOI] [PubMed] [Google Scholar]
- 20.Kremer I, Aizenman I, Lichter H, Shayer S, Levinger S. Simultaneous wavefront-guided photorefractive keratectomy and corneal collagen crosslinking after intrastromal corneal ring segment implantation for keratoconus. J Cataract Refract Surg. 2012;38(10):1802–1807. doi: 10.1016/j.jcrs.2012.05.033. [DOI] [PubMed] [Google Scholar]
- 21.Krueger RR, Kanellopoulos AJ. Stability of simultaneous topography-guided photorefractive keratectomy and riboflavin/UVA cross-linking for progressive keratoconus: case reports. J Refract Surg. 2010;26(10):S827–832. doi: 10.3928/1081597X-20100921-11. [DOI] [PubMed] [Google Scholar]
- 22.Kanellopoulos AJ, Binder PS. Collagen cross-linking (CCL) with sequential topography-guided PRK: a temporizing alternative for keratoconus to penetrating keratoplasty. Cornea. 2007;26(7):891–895. doi: 10.1097/ICO.0b013e318074e424. [DOI] [PubMed] [Google Scholar]
- 23.Kanellopoulos AJ. Comparison of sequential vs same-day simultaneous collagen cross-linking and topography-guided PRK for treatment of keratoconus. J Refract Surg. 2009;25(9):812–818. doi: 10.3928/1081597X-20090813-10. [DOI] [PubMed] [Google Scholar]
- 24.Kanellopoulos AJ, Binder PS. Management of corneal ectasia after LASIK with combined, same-day, topography-guided partial transepithelial PRK and collagen cross-linking: the athens protocol. J Refract Surg. 2011;27(5):323–331. doi: 10.3928/1081597X-20101105-01. [DOI] [PubMed] [Google Scholar]
- 25.Gómez-Miralles M, Peris-Martínez C, Pastor-Pascual F. Biomechanical corneal response measurement after manual insertion of intrastromal rings in patients with keratoconus. J Emmetropia. 2010;1(4):206–212. [Google Scholar]
- 26.Spadea L. Corneal collagen cross-linking with riboflavin and UVA irradiation in pellucid marginal degeneration. J Refract Surg. 2010;26(5):375–377. doi: 10.3928/1081597X-20100114-03. [DOI] [PubMed] [Google Scholar]
- 27.Vinciguerra P, Albè E, Trazza S, Seiler T, Epstein D. Intraoperative and postoperative effects of corneal collagen cross-linking on progressive keratoconus. Arch Ophthalmol. 2009;127(10):1258–1265. doi: 10.1001/archophthalmol.2009.205. [DOI] [PubMed] [Google Scholar]
- 28.Iovieno A, Légaré ME, Rootman DB, Yeung SN, Kim P, Rootman DS. Intracorneal ring segments implantation followed by same-day photorefractive keratectomy and corneal collagen cross linking in keratoconus. J Refract Surg. 2011;27(12):915–918. doi: 10.3928/1081597X-20111103-03. [DOI] [PubMed] [Google Scholar]
- 29.Kanellopoulos AJ. The management of cornea blindness from severe corneal scarring, with the Athens Protocol (transepithelial topography-guided PRK therapeutic remodeling, combined with same-day, collagen cross-linking) Clin Ophthalmol. 2012;6:87–90. doi: 10.2147/OPTH.S27175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Yeung SN, Ku JY, Lichtinger A, Low SA, Kim P, Rootman DS. Efficacy of single or paired intrastromal corneal ring segment implantation combined with collagen crosslinking in keratoconus J Cataract Refract Surg` 2013. 39 8 1146 1151 [DOI] [PubMed] [Google Scholar]


