Abstract
AIM
To describe the clinical characters of rhegmatogenous retinal detachment (RRD) associated with massive spontaneous suprachoroidal hemorrhage (SSCH). To evaluate optimal timing and prognosis of pars plana vitrectomy.
METHODS
A retrospective review of 6 cases (6 eyes) of RRD and massive SSCH among 3772 cases of RRD was conducted. All of 6 patients were treated with twenty-gauge vitrectomy, suprachoroidal blood drainage, phacoemulsification (PHACO) or lensectomy and silicon oil tamponade. The clinical characters, intraoperative findings and treatment outcomes were reported.
RESULTS
In the 6 affected eyes of 6 patients (3 men and 3 women; mean age, 53.83y; range 34-61y), preoperative visual acuity ranged from faint light perception (LP) to counting finger (CF). The average interventional duration from visual decreased to surgery was 12.8 d (range 9-15d). All eyes were associated with high myopia and the mean ocular length was 30.32 mm (range 28.14-32.32 mm). Choroidal hemorrhage were successfully drained in the operation of all 6 eyes. Intraoperative findings showed there were multiple retinal breaks in all 6 eyes and in 4 eyes breaks were along supratemporal and/or infratemporal retinal vascular arcade, especially in the edge of chorioretinal atrophy areas. These patients were followed up from 6 to 34mo (Mean, 23.5mo). The best-corrected visual acuity after surgery varied from CF to 20/100, with improvement in 5 eyes (83.33%) and no change in 1 eye (16.67%). Ocular hypertension ocurred in 1 eye (16.67%), which was successfully treated by silicon oil removal combined with trabeculectomy. In 4 eyes, tractional retinal detachment caused by proliferative vitreoretinopathy (PVR) appeared and a secondary surgery of pre-retinal membrane peeling and silicon oil retained were performed. In 4 eyes, silicon oil cannot be removed. The initial and final reattachment rates were 33.33% and 66.67%, respectively.
CONCLUSION
RRD associated with massive SSCH is an extremely rare event. The most common risk factor is long axial length. Vitrectomy and choroidal blood drainage can effectively remove suprachoroidal hemorrhage and promote retinal reattachment in these eyes. However, silicon oil could not be removed in most eyes and final visual acuities are generally poor.
Keywords: rhegmatogenous retinal detachment, suprachoroidal hemorrhage, pars plana vitrectomy
INTRODUCTION
Rhegmatogenous retinal detachment (RRD) associated with massive spontaneous suprachoroidal hemorrhage (SSCH) is an extremely rare event. To the best of our knowledge, there hadn't any report about it. In this report, we presented a case series of RRD with SSCH, and reviewed their clinical characters, management, and surgical prognosis.
SUBJECTS AND METHODS
We conducted a retrospective case review of RRD with SSCH patients treated in the Second Xiangya Hospital in China from January 2009 to June 2011. The study was approved by the Institutional Review Board of the Second Xiangya Hospital and was carried out in accordance with the tenets of the Declaration of Helsinki. Patients' data were collected by using the diagnosis RRD and suprachoroidal hemorrhage, all of 37 patient records were retrieved from our hospital's database. After excluding patients during or immediately after surgery or trauma, a total of 6 patients' records were collected for this study. Patient data collected included age, sex, associated medical history, previous ocular history, anticoagulant use, laboratory findings, initial and final visual acuity, intraocular pressure, anterior and posterior segment abnormalities, fundus colorized photography, A-scan ultrasound, B-scan ultrasound, type of surgery, timing to surgical intervention, final ocular findings and anatomy, and duration to follow-up.
All of 6 patients were treated with twenty-gauge vitrectomy, suprachoroidal blood drainage, photocoagulation, phacoemulsification (PHACO) or lensectomy and silicon oil tamponade. Triamcinolone acetonide (TA) was used during surgery to visualize better the posterior cortical vitreous. To limit retinal damage secondary to surgical manipulation, special attention was given to separating the posterior hyaloid gently over tight adhesion areas. The internal limiting membrane (ILM) was removed in all 6 eyes. Face-down posturing was instructed in the following 2wk.
Case Reports
Case 1
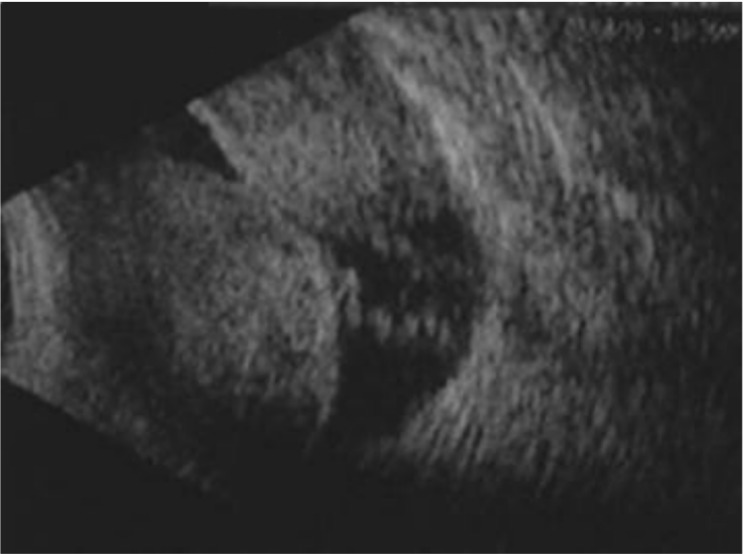
A 59-year-old woman with high myopia, presented with a 10d history of acute vision loss and severe pain in her right eye. On admission, her blood pressure was 160/100 mm Hg, but she did not feel any uncomfortable and denied history of taking any antihypertensive agents and anticoagulants. Three years earlier, she had PHACO with posterior chamber lens implantation in her left eye. Three months after, a vitrectomy and silicon oil tampernade was performed because of RRD in her left eye. On presentation, her visual acuity was weak light perception (LP) right and 20/500 left. The IOP was 3 mm Hg in the right and 4 mm Hg in the left. Ocular examination revealed mixed congestion, corneal edema, a deepen anterior chamber with Tyndall sign positive and lens opacification in her right eye. Dilated fundus examination (Figure 1) showed RRD associated with massive choroidal detachment. No vitreous hemorrhage was seen. B-Scan ultrasound confirmed retinal detachment and massive suprachoroidal hemorrhage (Figure 2). A-Scan ultrasound showed her axial length right was 30.73 mm. Routine blood tests, including a clotting screen, fasting glucose, liver and kidney functions, were entirely normal. Pred-Forte 1% Q2h, tropicarmide 0.5% three times a day and dexamethasone 10 mg intravenous drip once a day were prescribed. She was also treated for hypertension with oral nitrendipine tablets 10 mg TID. Over the next 3d, her blood pressure remained 110-130/70-90 mm Hg and the choroidal detachment was unchanged observed by ophthalmoscopy, but B scan ultrasound showed that multiple liquefied cavities of low to medium echogenicity in suprachoroidal hemorrhage began to appear. So a surgery of twenty-gauge vitrectomy, choroidal drainage, PHACO, photocoagulation and silicon oil tamponade was performed.
Figure 1. Fundus colour photograph of the right eye preoperative showing retinal detachment and massive choroidal detachment.
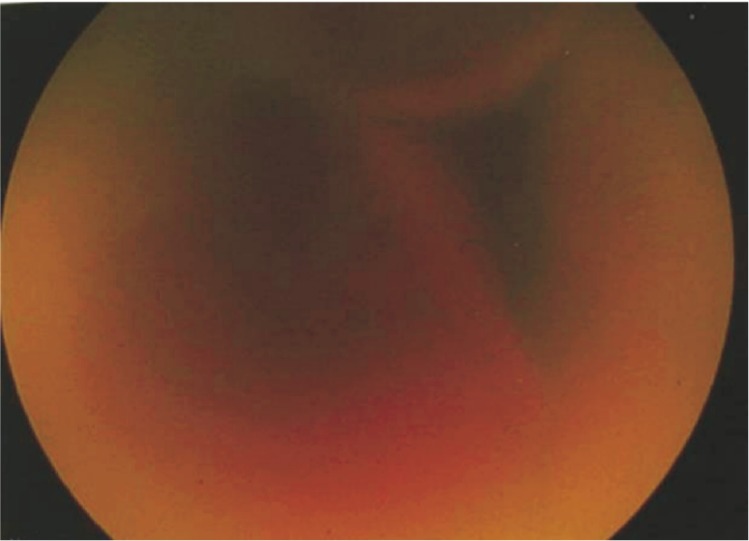
Figure 2. B-Scan ultrasound of case 1 confirming retinal detachment with massive suprachoroidal hemorrhage.
During the surgery, a infusion line with balanced salt solution (BSS) was placed in the anterior chamber through clear cornea and 3 scleral incisions were placed 3.5 mm posterior to the limbus to flow out the thick liquefied blood of suprachoroid until almost complete resolution of the choroidal detachment. Then, PHACO and vitrectomy were performed. It was found there were multiple areas of chorioretinal atrophy and 6 retinal breaks were along supratemporal and infratemporal retinal vascular arcade in the edge of atrophy areas. Some breaks could not be effectively closed by photocoagulation.
Her vision in right was CF, and the IOP was 6 mm Hg 45d after surgery. But there were tractional retinal detachment in the inferior temporal quadrant. Then the secondary surgery of peeling membrane and silicone oil retained was performed. Postoperatively, her retina in the right eye reattached and her vision remained CF in the following 26mo, but silicone oil could not be moved.
Case 2
A 61-year-old highly myopic woman presented with decreased vision in her right eye for 7d. She had not significant medical history. On presentation, her visual acuity was hand motion, and intraocular pressure was 5 mm Hg in the right eye. Examination showed a deep anterior chamber with iridodonesis, nuclear lens opacity with pigment remnants in the anterior capsule,and a prominent choroidal detachment with retinal detachment visible through the pupil. B-Scan ultrasound showed retinal detachment and massive suprachoroidal hemorrhage in her right eye (Figure 3). A-Scan showed her axial length in right was 30.31 mm. B scan ultrasound found that there were multiple liquefied cavities in her suprachoroidal space. Two days later, surgery of choroidal drainage, PHACO, twenty-gauge vitrectomy,photocoagulation and silicon oil tamponade was performed. There were 3 horseshoe tears in the superior and superotemporal mid-periphery retina. Four months after surgery, her retina in right reattached and vision was 20/200. A surgery of silicon oil remove was performed. After 2mo of follow up, her retina in right remained reattachment and visual acuity improved to 20/100.
Figure 3. B-Scan ultrasound of case 2 shows retinal detachment with massive suprachoroidal hemorrhage.
RESULTS
In 3772 patients of RRD treated in the second Xiangya Hospital in China from January 2009 to June 2011, 6 eyes of 6 patients (3 women and 3 men) with RRD and suprachoroidal hemorrhage were retrieved and reviewed (Table 1). The mean age was 53.83y (range 34-61y), and the mean follow-up time was 23.5mo (range 6-34mo). Only one patient was hypertensive. No patient had a history of anticoagulation use and other systemic disease. RRD and suprachoroidal hemorrhage were identified by indirect ophthalmoscope examination and B scan ultrasound. It occurred in the right eye in 5 patients, in the left eye in 1 patient. Initial visual acuity measurements ranged from faint LP to CF. Choroidal hemorrhage were successfully drained in all 6 eyes. The average interventional duration from visual decreased to surgery was 12.83d (range 9-15d). In most eyes, there were tight adhesion between the posterior vitreous membrane and retina, so it was very difficult to separate posterior vitreous cortex from inner surface of retina. Intraoperative findings also showed there were multiple retinal breaks in all 6 eyes. Retinal breaks lies in mid-periphery retina (n=2), along supratemporal or/and infratemporal retinal vascular arcade (n=4), especially in the edge of chorioretinal atrophy areas. Multiple retinal breaks associated with macular hole occurred in one case, whose retina can not reattached during follow-up period.
Table 1. Clinical characteristics of the 6 patients.
| Cases | Eye | Sex | Age (a) | Initial VA | Final VA | Ocular complications | AL (mm) | Follow up (mo) | Interventional duration (d) | Preoperative IOP (mm Hg) | SIR |
| 1 | OD | F | 61 | HM | 20/100 | No | 30.31 | 6 | 9 | 5 | Y |
| 2 | OD | M | 53 | CF | 20/2000 | PVR and focal TRD | 30.39 | 34 | 14 | 2 | N |
| 3 | OD | F | 59 | Faint LP | CF | PVR and focal TRD | 30.73 | 26 | 13 | 3 | N |
| 4 | OS | M | 57 | HM | CF | PVR and TRD | 32.32 | 22 | 14 | 10 | N |
| 5 | OD | F | 34 | HM | 20/200 | PVR and focal TRD | 28.14 | 25 | 15 | 2 | N |
| 6 | OD | M | 59 | CF | CF | SG | 30.03 | 28 | 12 | 4 | Y |
VA: Visual acuity; AL: Axial length; OD: Right eye; OS: Left eye; HM: Handmove; CF: Counting finger; LP: Light perception; TRD: Tractional retinal detachment; PVR: Proliferative vitreoretinopathy; SIR: Silicon oil remove; SG: Secondary glaucoma; PPV: Pars plana vitrectomy; SOI: Silicon oil implantation; IOP: Intraocular pressure.
In all 6 eyes, best-corrected visual acuity after surgery varied from CF to 20/100, with improvement in 5 eyes (83.33%) and no change in 1 eye (16.67%). Complications included PVR and TRD (n=4), secondary glaucoma (n=1). In 4 eyes, recurrent focal TRD caused by PVR appeared and a secondary surgery of pre-retinal membrane peeling and silicon oil retained were performed. In the case of secondary glaucoma, ocular hypertension occurred 7wk after surgery, and finally it was successfully treated by silicon oil removal combined with trabeculectomy 65d after surgery. In 4 eyes, silicon oil can not be removed. The final rates of retinal reattachment were 66.67%.
DISCUSSION
Suprachoroidal hemorrhage is a vision-threatening complication associated with ocular trauma or certain surgical procedures, such as cataract extraction, glaucoma filtering surgery, penetrating keratoplasty, and vitreoretinal surgery[1]–[5]. But SSCH is uncommon and previously it has been described only in isolated case reports. The recognised risk factors of SSCH include systemic diseases with anticoagulants[6],[7] and age-related macular degeneration (ARMD) with anticoagulants[8]–[11]. While RRD associated with SSCH is even extremely rare. To the best of our knowledge, there have been no studies about SSCH in RRD patients. In our study, we reviewed 3772 patients of RRD treated in our hospital from January 2009 to June 2011, and retrieved 6 cases of RRD associated with SSCH, providing a rate for the incidence of 1 in 629 (0.159%).
The exact cause of SSCH development in RRD patients is still unclear. Speaker et al[12] were the first to publish a report in 1991 on that increased axial length is a significant independent risk factor for suprachoroidal hemorrhage in introcular surgery because the longer axial length causes choroidal vascular fragility increasing. It has been widely reported that hypertension, arteriosclerosis and advanced age are systemic risk factors for suprachoroidal haemorrhage in a surgical setting, but the association with these risk factors in spontaneous haemorrhage is unknown[13]. In 2003, Chak and Williamson[14] reported a case of SSCH with high myopia and aspirin and suggested that high myopia and using anticoagulants may be the risk factors for SSCH. In our study, except one patient was indistinct for hypertension, all other patients were no history of systemic disease, but all 6 patients were associated with increased axial length, and in 5 eyes, the axial length were more than 30 mm. Therefore, the risk factor that is suspected of predisposing to massive SSCH in RRD patients may be long axial length. The increased axial length may be related to choroidal vascular fragility increasing. At the meantime, when retinal detachment appeared, a dramatic drop in IOP is experienced. It increases the risk of developing SSCH in RRD patients.
Surgical drainage of suprachoroidal hemorrhage without RRD has been reported in a few isolated papers, but the clinical effects and optimal timing of surgical intervention remained uncertain[15]–[19]. Yang et al[15] reported 5 eyes from 4 patients with massive spontaneous choroidal hemorrhage. In these 4 patients, 3 were on anticoagulation therapy with warfarin, 3 were hypertensive, and also 3 had been diagnosed with ARMD. And eventually 4 of the 5 eyes underwent surgical intervention for evacuation of the hemorrhage through a posterior sclerotomy with simultaneous anterior chamber infusion using BSS plus via a 25-gauge needle. But in the 4 eyes which underwent surgical drainage had vision of no LP at the final follow-up, while the vision for the remaining patient who did not undergo surgical drainage was handmove (HM) at the follow-up. So, they thought surgical intervention may have value in the relief of pain and elevated IOP, but has not been shown to be beneficial in visual outcomes. But in our series, the best-corrected visual acuity after surgery varied from CF to 20/100, with improvement in 5 eyes (83.33%) and no change in 1 eye (16.67%), even 2 eyes (33.33%) reached or excessed 20/200. The difference of vision prognosis may be related to basic lesions of these patients. In Yang et al's[15] 4 patients, 3 cases (4 eyes) were associated with AMD. And in the 4 eyes with AMD, 3 demonstrated choroidal neovascular membranes; 2 were associated with a disciform process; and 1 was associated with a pigment epithelial detachment. Furthermore, 2 patients (3 eyes) presented with narrow-angle glaucoma on presentation. These basic lesions itself can also cause vision loss. While in our study, all of the patients were associated with RRD and high myopia. After twenty-gauge vitrectomy, suprachoroidal blood drainage, photocoagulation, PHACO or lensectomy and silicon oil tamponade, retina reattached in 4 eyes. We found that in our cases, vitreoretinal proliferation after surgery was easy to occur. We hypothesized that it is caused by 2 reasons. Firstly, tight adhesion between the posterior vitreous membrane and retina cause posterior vitreous cortex cannot be thoroughly clear. And secondly, massive suprachoroidal hemorrhage also can stimulate PVR development. In 4 of the 6 eyes, recurrent tractional retinal detachment caused by PVR appeared and a secondary surgery of pre-retinal membrane peeling were performed. The initial and final reattachment rates in the 6 eyes were 33.33% and 66.67%, respectively.
Scott et al[20] showed that patients with surgically induced suprachoroidal hemorrhage of longer than 14d had worse visual outcomes than did those of fewer than 14d. In our review, B-scan ultrasound was used to monitor lytic state of suprachoroidal space, and we found the average interventional duration from hemorrhage to hemorrhagic clot liquefaction was 12.83d (range 9-15d). It was analogous to the report of Lambrou et al[21], who suggested that time for surgical drainage was 10-14d. During the operations, we successfully drained suprachoroidal hemorrhage in all 6 eyes. It also confirmed that B-scan ultrasound was an effective means to decide surgical timing by monitoring lytic state of suprachoroidal hemorrhage.
In addition, intraoperative findings showed there were multiple retinal breaks in all 6 eyes. Retinal breaks lies in mid-periphery retina (n=2), along supratemporal and infratemporal retinal vascular arcade (n=4), especially in the edge of chorioretinal atrophy areas. These breaks in chorioretinal atrophy areas could not be effectively closed by laser photocoagulation. So in 4 eyes, silicon oil can not be removed.
In all, RRD associated with massive SSCH is an extremely rare event. The most common risk factor is long axial length. Vitrectomy and choroidal blood drainage can effectively remove suprachoroidal hemorrhage and promote retinal reattachment in these eyes. However, silicon oil could not be removed in most eyes and final visual acuities are generally poor.
Acknowledgments
Conflicts of Interest: Zhang J, None; Zhu XH, None; Tang LS, None.
REFERENCES
- 1.Pollack AL, McDonald HR, Ai E, Johnson RN, Dugel PU, Folk J, Grand MG, Lambert HM, Schwartz S, Miller RD. Massive suprachoroidal hemorrhage during pars plana vitrectomy associated with Valsalva maneuver. Am J Ophthalmol. 2001;132(3):383–387. doi: 10.1016/s0002-9394(01)01049-2. [DOI] [PubMed] [Google Scholar]
- 2.Tabandeh H, Sullivan PM, Smahliuk P, Flynn HW, Jr, Schiffman J. Suprachoroidal hemorrhage during pars plana vitrectomy. Risk factors and outcomes. Ophthalmology. 1999;106(2):236–242. doi: 10.1016/S0161-6420(99)90062-3. [DOI] [PubMed] [Google Scholar]
- 3.Wang LC, Yang CM, Yang CH, Huang JS, Ho TC, Lin CP, Chen MS. Clinical characteristics and visual outcome of non-traumatic suprachoroidal haemorrhage in Taiwan. Acta Ophthalmol. 2008;86(8):908–912. doi: 10.1111/j.1755-3768.2008.01266.x. [DOI] [PubMed] [Google Scholar]
- 4.Chandra A, Xing W, Kadhim MR, Williamson TH. Suprachoroidal hemorrhage in pars plana vitrectomy: risk factors and outcomes over 10 years. Ophthalmology. 2014;121(1):311–317. doi: 10.1016/j.ophtha.2013.06.021. [DOI] [PubMed] [Google Scholar]
- 5.Mei H, Xing Y, Yang A, Wang J, Xu Y, Heiligenhaus A. Suprachoroidal hemorrhage during pars plana vitrectomy in traumatized eyes. Retina. 2009;29(4):473–476. doi: 10.1097/IAE.0b013e318196b189. [DOI] [PubMed] [Google Scholar]
- 6.Nguyen HN, Nork TM. Massive spontaneous suprachoroidal hemorrhage in a young woman with cystic fibrosis and diabetes mellitus on anticoagulants. Retin Cases Brief Rep. 2012;6(2):216–218. doi: 10.1097/ICB.0b013e3182378c1a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.De Marco R, Aurilia P, Mele A. Massive spontaneous choroidal hemorrhage in a patient with chronic renal failure and coronary artery disease treated with Plavix. Eur J Ophthalmol. 2009;19(5):883–886. doi: 10.1177/112067210901900534. [DOI] [PubMed] [Google Scholar]
- 8.Lewis H, Sloan SH, Foos RY. Massive intraocular hemorrhage associated with anticoagulation and age-related macular degeneration. Graefes Arch Clin Exp Ophthalmol. 1988;226(1):59–64. doi: 10.1007/BF02172720. [DOI] [PubMed] [Google Scholar]
- 9.Chen YY, Chen YY, Sheu SJ. Spontaneous suprachoroidal hemorrhage associated with age-related macular degeneration and anticoagulation therapy. J Chin Med Assoc. 2009;72(7):385–387. doi: 10.1016/S1726-4901(09)70393-4. [DOI] [PubMed] [Google Scholar]
- 10.Garrott HM, Haynes RJ. Blindness from suprachoroidal haemorrhage in two patients with age-related macular degeneration on systemic anticoagulation therapy or an antiplatelet agent. Med J Aust. 2010;192(6):346–347. doi: 10.5694/j.1326-5377.2010.tb03536.x. [DOI] [PubMed] [Google Scholar]
- 11.Kuhli-Hattenbach C, Fischer IB, Schalnus R, Hattenbach LO. Subretinal hemorrhages associated with age-related macular degeneration in patients receiving anticoagulation or antiplatelet therapy. Am J Ophthalmol. 2010;149(2):316–321. doi: 10.1016/j.ajo.2009.08.033. [DOI] [PubMed] [Google Scholar]
- 12.Speaker MG, Guerriero PN, Met JA, Coad CT, Berger A, Marmor M. A case-control study of risk factors for intraoperative suprachoroidal expulsive hemorrhage. Ophthalmology. 1991;98(2):202–209. doi: 10.1016/s0161-6420(91)32316-9. [DOI] [PubMed] [Google Scholar]
- 13.Chu TG, Green RL. Suprachoroidal hemorrhage. Surv phthalmol. 1999;43(6):471–486. doi: 10.1016/s0039-6257(99)00037-5. [DOI] [PubMed] [Google Scholar]
- 14.Chak M, Williamson TH. Spontaneous suprachoroidal haemorrhage associated with high myopia and aspirin. Eye (Lond) 2003;17(4):525–527. doi: 10.1038/sj.eye.6700388. [DOI] [PubMed] [Google Scholar]
- 15.Yang SS, Fu AD, McDonald HR, Johnson RN, Ai E, Jumper JM. Massive spontaneous choroidal hemorrhage. Retina. 2003;23(2):139–144. doi: 10.1097/00006982-200304000-00001. [DOI] [PubMed] [Google Scholar]
- 16.Jin W, Xing Y, Xu Y, Wang W, Yang A. Management of delayed suprachoriodal haemorrhage after intraocular surgery and trauma. Graefes Arch Clin Exp Ophthalmol. 2014;252(8):1189–1193. doi: 10.1007/s00417-013-2550-x. [DOI] [PubMed] [Google Scholar]
- 17.Mandelcorn ED, Kitchens JW, Fijalkowski N, Moshfeghi DM. Active aspiration of suprachoroidal hemorrhage using a guarded needle. Ophthalmic Surg Lasers Imaging Retina. 2014;45(2):150–152. doi: 10.3928/23258160-20140306-09. [DOI] [PubMed] [Google Scholar]
- 18.Nadarajah S, Kon C, Rassam S. Early controlled drainage of massive suprachoroidal hemorrhage with the aid of an expanding gas bubble and risk factors. Retina. 2012;32(3):543–548. doi: 10.1097/IAE.0b013e31822058e9. [DOI] [PubMed] [Google Scholar]
- 19.Kunjukunju N, Gonzales CR, Rodden WS. Recombinant tissue plasminogen activator in the treatment of suprachoroidal hemorrhage. Clin Ophthalmol. 2011;5:155–157. doi: 10.2147/OPTH.S16134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Scott IU, Flynn HW, Jr, Schiffman J, Smiddy WE, Murray TG, Ehlies F. Visual acuity outcomes among patients with appositional suprachoroidal hemorrhage. Ophthalmology. 1997;104(12):2039–2046. doi: 10.1016/s0161-6420(97)30042-6. [DOI] [PubMed] [Google Scholar]
- 21.Lambrou FH, Jr, Meredith TA, Kaplan HJ. Secondary surgical management of expulsive choroidal hemorrhage. Arch Ophthalmol. 1987;105(9):1195–1198. doi: 10.1001/archopht.1987.01060090053025. [DOI] [PubMed] [Google Scholar]