The prevalence of diabetes has risen markedly over the past decade and is projected to increase substantially.1 Over 20 percent of hospitalized patients are estimated to have diabetes,2 and individuals with diabetes have historically suffered higher inpatient mortality than individuals without diabetes.3 Over the past decade, evidence from large clinical trials has prompted recommendations for tighter inpatient and outpatient glucose control as well as more stringent blood pressure and lipid management in order to improve outcomes for patients with diabetes.4–6 It is unclear whether the mortality impact of diabetes has changed as a consequence.
Methods
We examined 10-year trends in mortality among patients with and without diabetes hospitalized at Yale-New Haven Hospital (YNHH), a major urban medical center. We considered all adult, non-obstetric patients with an inpatient discharge between January 1, 2000 and December 31, 2010 in YNHH administrative billing data. The primary endpoint was in-hospital mortality. Diabetes status was defined as a diagnosis of diabetes during the index admission or in any hospital encounter in the year prior to the index admission. Time was measured as the difference between January 1, 2000 and patient admission date, in years. We additionally included an array of covariates based on established associations with in-hospital mortality.
We used a difference-in-differences approach comparing changes over time in in-hospital mortality in patients with versus without diabetes, in order to determine whether patients with diabetes had a different time trend in risk of in-hospital mortality. We constructed multivariate logistic regression models including time in years, diabetes status, and the interaction between time and diabetes status as well as an array of covariates. We calculated odds of death and confidence intervals for each additional year for patients with diabetes by exponentiating the sum of parameter estimates for time and the diabetes-time interaction term. We used a type I error of 5% (two-sided) to test for statistical significance and obtained point estimates and 95% confidence intervals via the bootstrap method. Institutional review board approval was obtained for the study.
Results
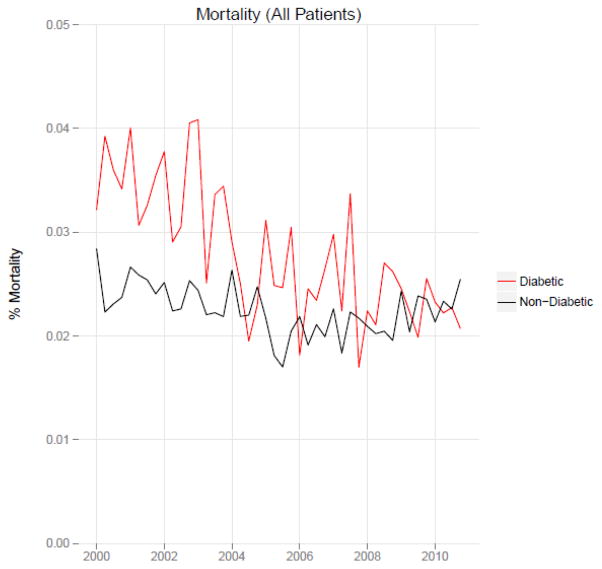
We included 322,938 patient admissions, of which 76,758 (23.8%) were from patients with diabetes. The overall mortality rate was 2.3%:2.7% of patients with diabetes and 2.2% of patients without diabetes. Unadjusted mortality among patients with diabetes decreased from 3.6% in 2000 to 2.2% in 2010 while mortality among patients without diabetes decreased from 2.4% in 2000 to 2.3% in 2010. Figure 1 shows quarterly in-hospital mortality for patients with and without diabetes from 2000 to 2010.
Figure 1.
Unadjusted mortality trends among patients with diabetes versus patients without diabetes, 2000–2010
Table 1 describes the difference-in-differences regression analyses. Each successive year was associated with a 4.5% reduction in the adjusted odds of mortality (OR=0.96, 95% CI: 0.95, 0.96) for patients without diabetes compared to a 8.7% reduction for those with diabetes (OR=0.91, 95% CI: 0.90, 0.93). Patients with diabetes compared to patients without diabetes had a significantly greater decline in risk of adjusted mortality of 4.4% per year (OR=0. 96, 95% CI: 0. 94, 0. 97). The adjusted odds of mortality among patients with versus without diabetes decreased from 1.20 in 2000 to 0.78 in 2010.
Table 1.
Regression analysis of mortality trends
| Independent variables | OR (95% CI) |
|---|---|
| Diabetes | 1.21(1.08, 1.36) |
| Time (w/o diabetes) | 0.96(0.95, 0.96) |
| Time (w diabetes) | 0.91 (0.90, 0.93) |
| c-statistic | 0.92 |
| n | 322,935 |
Model controls for gender, age at time of admission, length of stay in days, race (defined by hospital registration), payer, Elixhauser comorbidity dummy variables (revised to exclude diabetes and to use only secondary diagnosis codes), whether a patient spent a night in the intensive care unit, primary discharge diagnosis grouped using the Clinical Classifications Software (CCS), and service assignment (medicine, neurology, and surgery, including orthopedics and neurosurgery). OR = odds ratio, CI = confidence interval.
Comment
In a decade with increasing emphasis and accountability for glycemic control and cardiovascular risk management among patients with diabetes, we found that patients with diabetes have experienced a disproportionate reduction in in-hospital mortality over time and a complete reversal in risk of mortality relative to patients without diabetes. This interesting trend warrants further study to elucidate its origins. Potential explanations include coincident improvements in inpatient glycemic control, improvements in outpatient glycemic control, improved non-glycemic cardiovascular risk management among patients with diabetes, and/or advances in therapies for diseases that disproportionately affect patients with diabetes.
Acknowledgments
The authors would like to acknowledge the Yale-New Haven Hospital diabetes management team: Gael Ulisse APRN, Helen Psarakis APRN, Anne Kaisen APRN, and the Yale Endocrine Fellows. We would additionally like to acknowledge Janis Bozzo, MSN, RN from Decision Support at the Yale-New Haven Health System. None of these individuals received compensation for this manuscript.
Funding sources: Dr. Horwitz is supported by the National Institute on Aging (K08 AG038336) and by the American Federation for Aging Research through the Paul B. Beeson Career Development Award Program. No funding source had any role in design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication.
Footnotes
Author contributions:
Design and conduct of the study: NB, JD, SI, TB, LH
Collection, management, analysis, and interpretation of the data: NB, BJ, JD, JR, SI, LH
Preparation, review, or approval of the manuscript: NB, BJ, JD, JR, SI, TB, LH
Dr. Inzucchi serves on a Data Safety Monitoring Board for Novo Nordisk, a manufacturer of insulin products used in the hospital setting. The remaining authors declare no conflicts of interest.
Leora Horwitz had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
References
- 1.Boyle JP, Honeycutt AA, Narayan K, et al. Projection of diabetes burden through 2050 impact of changing demography and disease prevalence in the US. Diabetes care. 2001;24(11):1936–1940. doi: 10.2337/diacare.24.11.1936. [DOI] [PubMed] [Google Scholar]
- 2.Healthcare Cost and Utilization Project. [Accessed November 12, 2013];Statistical Brief #93. 2010 http://www.hcup-us.ahrq.gov/reports/statbriefs/sb93.pdf.
- 3.Holman N, Hillson R, Young RJ. Excess mortality during hospital stays among patients with recorded diabetes compared with those without diabetes. Diabet Med. 2013 Jul 23; doi: 10.1111/dme.12282. [DOI] [PubMed]
- 4.Association AD. Standards of medical care in diabetes—2014. Diabetes care. 2014;37(Supplement 1):S14–S80. doi: 10.2337/dc14-S014. [DOI] [PubMed] [Google Scholar]
- 5.Cleeman J, Grundy S, Becker D, Clark L. Expert panel on Detection, Evaluation and Treatment of High blood Cholesterol in Adults. Executive Summary of the Third Report of the National Cholesterol Education Program (NCEP) Adult Treatment Panel (ATP III) JAMA : the journal of the American Medical Association. 2001;285(19):2486–2497. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 6.Patel A. Effects of a fixed combination of perindopril and indapamide on macrovascular and microvascular outcomes in patients with type 2 diabetes mellitus (the ADVANCE trial): a randomised controlled trial. The Lancet. 2007;370(9590):829–840. doi: 10.1016/S0140-6736(07)61303-8. [DOI] [PubMed] [Google Scholar]