Abstract
The JCVSD (Japan Cardiovascular Surgery Database) was organized in 2000 to improve the quality of cardiovascular surgery in Japan. Web-based data harvesting on adult cardiac surgery was started (Japan Adult Cardiovascular Surgery Database, JACVSD) in 2001, and on congenital heart surgery (Japan Congenital Cardiovascular Surgery Database, JCCVSD) in 2008. Both databases grew to become national databases by the end of 2013. This was influenced by the success of the Society for Thoracic Surgeons’ National Database, which contains comparable input items. In 2011, the Japanese Board of Cardiovascular Surgery announced that the JACVSD and JCCVSD data are to be used for board certification, which improved the quality of the first paperless and web-based board certification review undertaken in 2013. These changes led to a further step. In 2011, the National Clinical Database (NCD) was organized to investigate the feasibility of clinical databases in other medical fields, especially surgery. In the NCD, the board certification system of the Japan Surgical Society, the basic association of surgery was set as the first level in the hierarchy of specialties, and nine associations and six board certification systems were set at the second level as subspecialties. The NCD grew rapidly, and now covers 95% of total surgical procedures. The participating associations will release or have released risk models, and studies that use ‘big data’ from these databases have been published. The national databases have contributed to evidence-based medicine, to the accountability of medical professionals, and to quality assessment and quality improvement of surgery in Japan.
Keywords: Clinical database, Quality improvement, Medical board, Patient safety, Medical expenditure
INTRODUCTION: THE SOCIETY FOR THORACIC SURGEONS NATIONAL DATABASE
The first historical study of quality assessment in the medical field was reported by Ernest Amory Codman, MD, of Massachusetts General Hospital in 1920. To support his ‘end results theory,’ he made public the results of the review of his own hospital in a privately published book, “A study in hospital efficiency,” in which he emphasized the importance of patient follow-up and quality assessment. He helped to found the Hospital Standardization Program, which eventually became the Joint Commission on Accreditation of Healthcare Organizations in 1987, and the Joint Commission in 2007, with the motto ‘Helping Health Care Organizations Help Patients.’
From the 1970s through the 1980s, the rapid increase in medical lawsuits and the medical malpractice insurance crisis promoted risk management of medical practices in the United States. In 1989, the Society for Thoracic Surgeons (STS) started to establish national databases [1] as an initiative to improve quality and patient safety among cardiothoracic surgeons and to respond to strong public opinion about the importance of accountability. In 1997, an initiative was begun to improve data quality and auditing, and staff were hired to support these efforts. In the STS Congenital Heart Surgery Database data specification, (http://www.sts.org/sites/default/files/documents/CongenitalDataSpecsV3_22.pdf), the Patient National Identification (Social Security Number) is listed, but this field should be collected in compliance with state/local privacy laws. The STS National Database complies with the Health Insurance Portability and Accountability Act, and the federal government protects the STS National Database.
In 1998, the STS contracted with the Duke Clinical Research Institute (DCRI) for data warehousing and data analysis. In 1999, the Institute of Medicine published a report titled “To err is human: building a safe health system,” which stated that 44,000 to 98,000 persons die in hospitals as a result of medical errors that could have been prevented. This report led worldwide health policy organizations to introduce initiatives for patient safety.
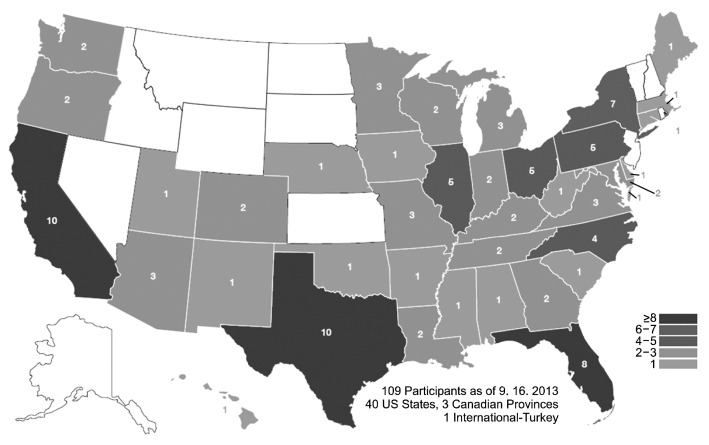
Today, the management of the National Database is one of the most important tasks of the STS. The database contains three components: adult cardiac surgery, general thoracic surgery and congenital heart surgery (Fig. 1).
Fig. 1.
The Society for Thoracic Surgeons National Database: the Congenital Heart Surgery Database participants (http://www.sts.org/sites/default/files/documents/congenitalMap.pdf).
The STS was the first professional organization to seek approval for its measures from the National Quality Forum (NQF), a multi-stakeholder health policy organization head-quartered in Washington, DC. In this manner, the STS has gained a positive reputation with the government and with health policy organizations. In addition, in 2010, the STS started to publicly report isolated coronary artery bypass grafting (CABG) composite star ratings not only on its own website but also on a consumer report website (www.consumerreportshealth.org) [2]. Later, public reporting of aortic valve surgery (AVR) and CABG+AVR began, and this year, will be extended to congenital heart surgery. The NQF has been releasing quality indicators in medical fields under the rubric of ‘NQF-Endorsed Standards’ (http://www.quality-forum.org/Home.aspx). For example, the standard measures of congenital heart surgery are ‘participation in the STS National Database,’ ‘operative mortality stratified by the five STS-EACTS (European Association for Cardiothoracic Surgery) Mortality Categories,’ and ‘Risk Adjustment in Congenital Heart Surgery (RACHS-1) Pediatric Heart Surgery Mortality [3].’ The STS states on its website that ‘STS believes the public has a right to know the quality of the surgical outcomes, and considers public reporting an ethical responsibility of the specialty [4,5].’
THE JAPAN CARDIOVASCULAR SURGERY DATABASE
In turn, in 1998, at the 7th Annual Meeting of the Asian Society for Cardiovascular and Thoracic Surgery in Singapore, the need for an Asian Cardiovascular Surgery Database was discussed. First, a database ad hoc committee was formed by the Japanese Society for Cardiovascular Surgery (JSCVS) and the Japanese Association for Thoracic Surgery (JATS) (Table 1).
Table 1.
Progress in quality improvement in medical fields worldwide and the Japan Cardiovascular Surgery Database
| Year | History |
|---|---|
| 1920 | Initial report of quality assessment by Codman, MD. |
| 1989 | Start of the Society for Thoracic Surgeons National Database |
| 1998 | Kick-off meeting for cardiovascular surgery database during the 7th annual meeting of the Asian Society of Thoracic and Cardiovascular Surgery in Singapore |
| 1999 | Report from the Institute of Medicine, ‘To err is human’ |
| 2000 | Database ad hoc committee started under the Japanese Society for Cardiovascular Surgery, and the Japanese Association for Thoracic Surgery |
| 2000 | Establishment of the Japan Cardiovascular Surgery Database |
| 2001 | The beginning of the data harvest on Japan adult cardiovascular surgery database, JACVSD, by 5 units |
| 2008 | The beginning of data harvest on Japan congenital cardiovascular surgery database, JCCVSD, by 7 units |
| 2011 | The JBCVS decided to adopt the reported data of the JACVSD and the JCCVSD for board certification |
| 2011 | Establishment of National Clinical Database |
| 2013 | The first “paper-less and web-based” board certification meeting of JBCVS |
| 2014 | A new organization for medical board certification in Japan |
JACVSD, Japan Adult Cardiovascular Surgery Database; JCCVSD, Japan Congenital Cardiovascular Surgery Database; JBCVS, Japanese Board of Cardiovascular Surgery.
Moreover, quality improvement of cardiovascular surgery has been discussed by the members of the board of JSCVS and JATS since early 2000. In pursuit of this goal, three committees were organized by the JSCVS and JATS among its academic groups: 1) a board certification committee, 2) a center aggregation committee, and 3) a nurse practitioner and physician assistant committee.
In 2000, before this movement, the Japan Cardiovascular Surgery Database (JCVSD) was established with close ties to the JSCVS and JATS. The JCVSD and JSCVS invited the founder of the STS National Database to discuss starting the construction of the database. The JCVSD established input items comparable to those of the STS National Database. In the Congenital Heart Surgery Database, the common terminologies and the definitions of congenital heart diseases published in the “Annals of thoracic surgery [6]” were adopted, and 193 input items were established in the Japan Congenital Cardiovascular Surgery Database (JCCVSD).
Thus, the Congenital Heart Surgery Databases in the United States, Europe, and Japan were integrated by using common language in these databases. As a result, international comparisons became possible. Although the results were not reported, for example, the discharge mortality in the JCCVSD was 0.2%, 0.7%, 3.6%, 7%, and 17.6% for RACHS-1 categories 1, 2, 3, 4, and 5/6, respectively, during 2008 to 2010 (Fig. 2). This result is comparable to that reported from the STS Congenital Heart Surgery Database [7].
Fig. 2.
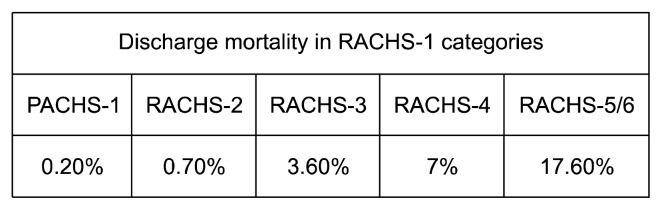
Discharge mortality in the Japan Congenital Cardiovascular Surgery Database according to the RACHS-1 categories. RACH-1, Risk Adjustment in Congenital Heart Surgery.
Unlike the STS National Database, the JCVSD employed web-based data collection. Data on adult cardiac surgery (Japan Adult Cardiovascular Surgery Database [JACVSD]) were collected beginning in 2001 by five participating units and data on congenital heart surgery (JCCVSD) were collected beginning in 2008 by seven units. JCVSD required informed consent from each patient according to the ‘opt-in rule’ to comply with the Private Information Protection Law. For Web-data transmission, high level secure socket layer was adopted for coding of the individual patient’s information.
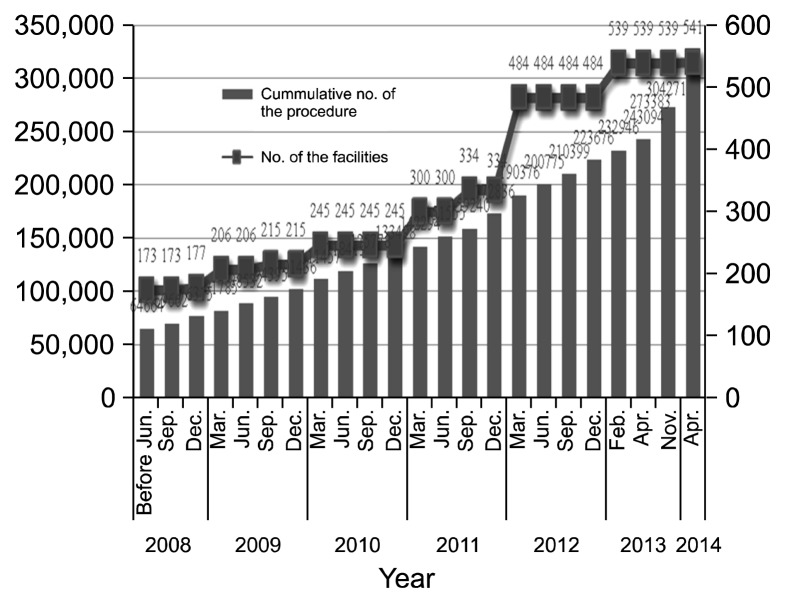
The JACVSD and JCCVSD grew to become national databases by the end of 2013 (Fig. 3). The most recent annual number of submitted procedures are 49,507 in JACVSD and 10,835 in JCCVSD. Twenty frequently cited papers dealing with topics such as risk models of isolated coronary bypass surgery [8], thoracic aortic surgery [9], and valve surgery [10] have been published in indexed international journals. The performance of the Congenital Heart Surgery risk model as measured by the C-index is over 0.8 [11].
Fig. 3.
The growth in the Japan Adult Cardiovascular Surgery Database, As of April 2014, the number of facilities were 541 and the cumulative number of procedures were 304,271.
On the basis of these risk models, a web-based risk calculator called JapanSCORE was released. With this tool, adult cardiac surgeons can estimate the 30-day mortality rate, in-hospital mortality rate, and major complication rate after inputting the patient’s covariates before the surgical procedure. The estimated mortality rate is much lower than that derived by using EuroScore [12]. JapanSCORE contributes to obtaining adequate informed consent from the patients and the families, leading to increased satisfaction. In addition, benchmark reports have been released as support tools for quality improvement of participating institutions. In Japan, many adult cardiac surgeons learn about the risks faced by their patients, as well as their own performance as a surgeon, through the risk-adjusted mortality and benchmark report.
To ensure fairness and transparency in evidence-based medicine (EBM), the JCVSD organized a data access and usage working group. This working group meets twice a year, and requests 100% of their data during at least for the immediate 2-years. After the working group accepts an application, the Department of Health Quality Assessment (HQA) of the University of Tokyo [13,14] analyzes the newly submitted data. The role of the HQA is similar to that of the DCRI for the STS National Database.
The JCVSD places importance on auditing the reported data. Site visits have been carried out since 2004. A site visit working group was established by the JACVSD. The members of the working group include two to three adult cardiac surgeons; visits to 70 sites have been carried out so far. Recently the HQA reported the details and outcomes of the site visits to the JCCVSD [15].
In 2011, the JCVSD started to collect a participation fee of 10,000 yen per year for each section in the JACVSD and the JCCVSD. The total number of sections was 658 (541 in the JACVSD, 117 in the JCCVSD) by the end of April 2014. This participation fee is much lower than that required by the STS National Database; however, it is an important financial resource, especially for site visits.
In 2011, the Japanese Board of Cardiovascular Surgery (JBCVS) decided to adopt the data of the JACVSD and the JCCVSD for board certification. In 2013, there were 162 new applicants and 1,003 renewals. The JBCVS held its first web-based and paperless review in September 2013. Compared with the previously employed review method that relied on the submission of operation records, the web-based and paperless review method had higher quality, lower cost, and required less time.
THE NATIONAL CLINICAL DATABASE
In 2010, the JCVSD served as the basis for the establishment of the National Clinical Database (NCD) in Japan, which includes clinician-initiated databases reflecting all surgical fields. The NCD adopted to “Web-based” data collection with the same security level of JCVSD as mentioned above to protect the individual patient’s information. Through the central institutional review board in the University of Tokyo, an ‘opt-out rule’ was adopted, and informed consent became unnecessary. The NCD is governed by a committee whose members are representatives of medical associations related to surgery, such as the Japan Surgical Society (JSS), JSCVS, JATS, the Japanese Association for Chest Surgery, the Japanese Society of Gastroenterological Surgery, the Japanese Society of Pediatric Surgeons, the Japanese Society of Vascular Surgery, the Japanese Society of Endocrine Surgery, the Japanese Society for Mammary Cancer, and the Japanese Thyroid Association. The NCD establishes the surgical board certification system for the JSS, which requires 13 input items at the first level in the hierarchy of specialties. Six board certification systems, including the JBCVS and the databases of nine academic associations, are set at the second level as subspecialties. The main server was transferred from the HQA to the University Hospital Medical Information Network (UMIN) with a mirror-image backup. The HQA focused on data analysis and site visits, whereas the UMIN is responsible for data warehousing. The NCD uses cutting-edge statistical techniques to detect any trace of data inconsistency. The participating associations have supported the NCD financially and the database has grown rapidly; the total number of participating hospitals is 4105, and the number of cumulative procedures was 4,138,000 at the end of April 2014. The NCD covers 95% of total surgical procedures. The participating associations will release, or have released, their own risk models [16–18], and papers have been published based on data from the NCD [16].
NATIONAL CLINICAL DATABASES AND HEALTH SERVICES
The administrative database, diagnosis procedure combination (DPC)/par-diem payment system (PDPS) was introduced in Japan by the Japanese Ministry of Health, Labour and Welfare (MHLW, a government agency) in April 2003 to comprehensively assess fixed daily payments and to control medical expenditure in the acute setting based on the quality assessment. The number of participating hospitals by the end of April 2014 was 1,585, including all advanced-treatment hospitals, that is, university hospitals. In Japan, total health care expenditures have been increasing by 1 trillion yen annually, and health care expenditures make up 9.5% of the Gross Domestic Product, which puts Japan in the 16th position of the 34 member countries of the Organization for Economic Cooperation and Development. On the other hand, the population aging rate in Japan is over 24%, which is the highest rate in the world. Changes in population makeup and the growing proportion of elderly persons are the underlying issues relating to rising health care expenditures, and successive Cabinet office members and the MHLW have set policy directions to address this national issue. Quality improvement, quality assessment, and the pay-for-performance system provide methods to control medical expenditures. The Quality and Outcomes Framework (QOF), a system for the performance management and payment of genaral practitioners (GPs) in the National Health Service in England, Wales, Scotland and Northern Ireland was introduced as part of the new general medical services contract in April 2004. The QOF rewards GPs for implementing “good practice” in their medical practices. Participation in the QOF is voluntary for each partnership [19]. In contrast, in the United States, the Agency of Healthcare Research and Quality (AHRQ) has defined ‘never events’ or errors of medical care for which Medicare, the government healthcare insurance for aged and disabled persons, does not pay. In the C. Walton Lillehei Lecture of the 49th STS Annual Meeting, the director of the AHRQ emphasized that the federal government will pay for the quality, not for the volume.
In Japan, the NCD and DPC/PDPS could play complementary functions for quality assessment through adequate risk adjustment and the complete enumeration of procedures in various surgical fields. In the future, balancing professional autonomy and administrative leadership might be a recurrent issue for quality assessment and quality improvement in Japan.
PERSPECTIVES
Recently, the Japanese Association of Cardiovascular Intervention and Therapeutics proposed to the NCD a comparative study between percutaneous coronary intervention and CABG that would use well-tested statistical methods such as propensity score matching. Thus, the participation of units from nonsurgical fields, such as medical therapy, intervention, radiation therapy, and chemotherapy, will facilitate risk stratification of each treatment modality, and will contribute to the search for the best management of diseases and patients. A longitudinal follow-up database is needed for the design of such studies, and it is under construction.
Recently, the Pharmaceutical and Medical Device Agency (PMDA), a consultative organization of the MHLW, suggested to enroll in the JACVSD and perform follow-ups on the use of artificial valves for trans-aortic valve implantation. The PMDA recognized the completeness and reliability of the data of the JACVSD, and from a cost-performance point of view, the PMDA decided to outsource the post-market surveillance of newly covered medical devices in the cardiovascular surgical field. This demonstrates how the national database could contribute to the post-marketing surveillance of drugs and medical devices, and could help control randomized trials and multicenter studies.
The NCD will start to collect fees from participating hospitals according to the total number of enrolled surgical procedures. Clerical assistants have been widely employed throughout the country, which has gradually lightened the data input workload of young surgeons. Governmental support and some government funds are expected to be received for the continued maintenance of the national database.
CONCLUSION
Clinicians are responsible for patient safety and quality improvement, and the database will aid in achieving these goals.
As Reinertsen [20] stated, to truly improve quality, the system must, 1) eliminate unnecessary variation (standardize processes), and 2) achieve and document continuous improvement (in care processes and outcomes). In recent years, the importance of ‘certainty, not excellence’ of operations, and that of the concept of structure, process and outcome [21] have been emphasized, and multiple approaches, for instance, postgraduate education systems, reporting systems of malpractice to prevent recurrence, introduction of information technology, introduction of simulators, EBM, and other techniques, have been used for patient safety. The use of multiple strategies and teamwork are fundamental for patient safety.
Since it is methodologically based on the JCVSD, the NCD represents an interface between medical databases and board certification systems, which is its point of difference from the STS National Database. In 2014, a new organization for medical board certification was established in Japan that, beginning in 2017, will certify all medical boards in close collaboration with medical associations. This new organization will adopt the standards of the JCVSD and the NCD for evaluating the clinical practices of applicants. For the assessment of medical outcomes and quality, the JCVSD and the NCD will continue to be the sole reliable data source for surgical fields in Japan, where medical system reform will be implemented quickly and based on professional autonomy.
The national database is fundamental for quality improvement, patient safety, and the adequate control of medical expenditures in the country.
ACKNOWLEDGMENTS
This paper was presented at the 45th Fall Meeting of the Korean Society for Thoracic and Cardiovascular Surgery on November 8, 2013, in Seoul. I appreciate the hospitality of the members of the society and Prof. Woong-Han Kim of Seoul National University, who invited me to this outstanding meeting.
Footnotes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
REFERENCES
- 1.Grover FL, Shroyer AL, Hammermeister K, et al. A decade’s experience with quality improvement in cardiac surgery using the Veterans Affairs and Society of Thoracic Surgeons national databases. Ann Surg. 2001;234:464–72. doi: 10.1097/00000658-200110000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ferris TG, Torchiana DF. Public release of clinical outcomes data: online CABG report cards. N Engl J Med. 2010;363:1593–5. doi: 10.1056/NEJMp1009423. [DOI] [PubMed] [Google Scholar]
- 3.Jenkins KJ, Gauvreau K, Newburger JW, Spray TL, Moller JH, Iezzoni LI. Consensus-based method for risk adjustment for surgery for congenital heart disease. J Thorac Cardio-vasc Surg. 2002;123:110–8. doi: 10.1067/mtc.2002.119064. [DOI] [PubMed] [Google Scholar]
- 4.Shahian DM, Edwards FH, Jacobs JP, et al. Public reporting of cardiac surgery performance: part 1--history, rationale, consequences. Ann Thorac Surg. 2011;92(3 Suppl):S2–11. doi: 10.1016/j.athoracsur.2011.06.100. [DOI] [PubMed] [Google Scholar]
- 5.Shahian DM, Edwards FH, Jacobs JP, et al. Public reporting of cardiac surgery performance: part 2--implementation. Ann Thorac Surg. 2011;92(3 Suppl):S12–23. doi: 10.1016/j.athoracsur.2011.06.101. [DOI] [PubMed] [Google Scholar]
- 6.Mavroudis C, Jacobs JP. Congenital Heart Surgery Nomenclature and Database Project: overview and minimum dataset. Ann Thorac Surg. 2000 Apr;69(4 Suppl):S2–17. doi: 10.1016/s0003-4975(99)01321-1. [DOI] [PubMed] [Google Scholar]
- 7.Jacobs JP, Jacobs ML, Lacour-Gayet FG, et al. Stratification of complexity improves the utility and accuracy of outcomes analysis in a Multi-Institutional Congenital Heart Surgery Database: Application of the Risk Adjustment in Congenital Heart Surgery (RACHS-1) and Aristotle Systems in the Society of Thoracic Surgeons (STS) Congenital Heart Surgery Database. Pediatr Cardiol. 2009;30:1117–30. doi: 10.1007/s00246-009-9496-0. [DOI] [PubMed] [Google Scholar]
- 8.Motomura N, Miyata H, Tsukihara H, Okada M, Takamoto S Japan Cardiovascular Surgery Database Organization. First report on 30-day and operative mortality in risk model of isolated coronary artery bypass grafting in Japan. Ann Thorac Surg. 2008;86:1866–72. doi: 10.1016/j.athoracsur.2008.08.001. [DOI] [PubMed] [Google Scholar]
- 9.Motomura N, Miyata H, Tsukihara H, Takamoto S Japan Cardiovascular Surgery Database Organization. Risk model of valve surgery in Japan using the Japan Adult Cardiovascular Surgery Database. J Heart Valve Dis. 2010;19:684–91. [PubMed] [Google Scholar]
- 10.Motomura N, Miyata H, Tsukihara H, Takamoto S Japan Cardiovascular Surgery Database Organization. Risk model of thoracic aortic surgery in 4707 cases from a nationwide single-race population through a web-based data entry system: the first report of 30-day and 30-day operative outcome risk models for thoracic aortic surgery. Circulation. 2008;118(14 Suppl):S153–9. doi: 10.1161/CIRCULATIONAHA.107.756684. [DOI] [PubMed] [Google Scholar]
- 11.Miyata H, Murakami A. The first report on risk models based on the Japan Congenital Cardiovascular Surgery Database. J Thorac Cardiovasc Surg. 2014 Jan 15; doi: 10.1016/j.jtcvs.2013.01.053. [In press] [DOI] [PubMed] [Google Scholar]
- 12.Roques F, Nashef SA, Michel P EuroSCORE study group. Risk factors for early mortality after valve surgery in Europe in the 1990s: lessons from the EuroSCORE pilot program. J Heart Valve Dis. 2001;10:572–7. [PubMed] [Google Scholar]
- 13.Miyata H, Motomura N, Kondo MJ, Fushimi K, Ishikawa KB, Takamoto S. Toward quality improvement of cardiovascular surgery in Japan: an estimation of regionalization effects from a nationwide survey. Health Policy. 2009;91:246–51. doi: 10.1016/j.healthpol.2008.11.003. [DOI] [PubMed] [Google Scholar]
- 14.Miyata H, Motomura N, Ueda Y, Tsukihara H, Tabayashi K, Takamoto S. Toward quality improvement of thoracic aortic surgery: estimating volume-outcome effect from nationwide survey. Eur J Cardiothorac Surg. 2009;36:517–21. doi: 10.1016/j.ejcts.2009.03.020. [DOI] [PubMed] [Google Scholar]
- 15.Tomotaki A, Miyata H, Hashimoto H, Murakami A, Ono M. Results of data verification of the Japan congenital cardiovascular database, 2008 to 2009. World J Pediatr Congenit Heart Surg. 2014;5:47–53. doi: 10.1177/2150135113508794. [DOI] [PubMed] [Google Scholar]
- 16.Miyata H, Gotoh M, Hashimoto H, et al. Challenges and prospects of a clinical database linked to the board certification system. Surg Today. 2014 May 23; doi: 10.1007/s00595-013-0802-3. [Epub] [DOI] [PubMed] [Google Scholar]
- 17.Kenjo A, Miyata H, Gotoh M, et al. Risk stratification of 7,732 hepatectomy cases in 2011 from the National Clinical Database for Japan. J Am Coll Surg. 2014;218:412–22. doi: 10.1016/j.jamcollsurg.2013.11.007. [DOI] [PubMed] [Google Scholar]
- 18.Kobayashi H, Miyata H, Gotoh M, et al. Risk model for right hemicolectomy based on 19,070 Japanese patients in the National Clinical Database. J Gastroenterol. 2014;49:1047–55. doi: 10.1007/s00535-013-0860-8. [DOI] [PubMed] [Google Scholar]
- 19.Roland M. Linking physician’s pay to the quality of care – a major experiment in the United Kingdom. N Engl J Med. 2004;351:1448–54. doi: 10.1056/NEJMhpr041294. [DOI] [PubMed] [Google Scholar]
- 20.Reinertsen JL. Zen and the art of physician autonomy maintenance. Ann Intern Med. 2003;138:992–5. doi: 10.7326/0003-4819-138-12-200306170-00011. [DOI] [PubMed] [Google Scholar]
- 21.Donabedian A. Evaluating the quality of medical care. Milbank Mem Fund Q. 1966;44(Suppl):166–206. [PubMed] [Google Scholar]