Abstract
Objective:
In the ongoing absence of available trial data, a national survey was carried out to provide details on radiotherapy treatment strategy for non-melanoma skin cancer (NMSC).
Methods:
A survey of clinical oncologists treating NMSC was performed. The respondents were asked for basic information on workload as well as a proposed treatment strategy for various clinical scenarios for patients of varying fitness.
Results:
A total of 43 completed and 20 partially completed surveys were received. There was a wide variation in the workload and additional disease sites that respondents had responsibility for. Kilovoltage radiotherapy was available to 81% of responders. The respondents' approach was affected by the fitness of patients, with longer fractionation regimes proposed for younger, fitter patients and shorter or non-standard fractionations more likely for the infirm elderly. Four daily fractionation regimes (18–20 Gy in 1 fraction, 35 Gy in 5 fractions, 45 Gy in 10 fractions and 55 Gy in 20 fractions) were most commonly suggested. There was a large degree of variation in non-standard fractions proposed with significant potential differences in radiobiological effect. Concern over the use of kilovoltage photons on skin over cartilage was apparent, as was a reluctance to use radiotherapy in areas of increased risk of poor wound healing.
Conclusion:
The survey results largely showed practice to be in line with available published evidence. The variation seen in some areas, such as non-standard fractionation, would benefit from the publication of local outcomes to achieve a more consistent approach.
Advances in knowledge:
This study provides information on national practices and identifies variations, particularly within widespread use of non-standard fractionation.
Non-melanoma skin cancer (NMSC) is the most common malignancy in the UK. In 2010, around 100,000 people were diagnosed with NMSC, and there were 585 related deaths in 2011.1 The vast majority of these lesions are basal cell carcinomas (BCCs) or, less commonly, squamous cell carcinomas (SCCs). Various treatment modalities can be utilized to manage this condition, with a potential for excellent local control and cosmesis, including topical therapies, surgical excision, electrocautery, cryotherapy and radiotherapy. The choice of treatment approach is influenced by the stage and location of disease, patient fitness and preference. For patients who are not fit enough to be considered for surgery or for disease in locations where excision would be cosmetically undesirable, the use of radiotherapy is commonly recommended.
Various methods of radiotherapy delivery are available, including electron, kilovoltage and megavoltage external beam radiotherapy as well as brachytherapy, although there is variable access to these methods between centres in the UK. A lack of prospective trial data to guide treatment has led to the development of local practice regarding dose fractionation schedules, and it is unclear how much variation currently exists nationally. In the absence of likely forthcoming trials, there is little impetus for variable practice to change.
To potentially streamline clinical practice, details on the most commonly used strategies employed in various clinical scenarios would be of interest as a basis for harmonizing dose/fractionation schedules.
METHODS AND MATERIALS
An invitation to complete an anonymous online survey was sent to all 58 clinical heads of the Service and Clinical Oncology Audit Leads throughout the UK to pass on to consultants, with an interest in treating patients with NMSC. The survey was hosted via the online website Qualtrics and remained open for a period of 3 months. Basic information regarding the experience of the responder and the number of skin cases treated was requested as well as a proposed treatment strategy for various clinical scenarios. In each of these scenarios, a tissue diagnosis had been made, and the multi-disciplinary meeting decision was for management with primary radiotherapy. Owing to the wide diversity of both location and types of tumour that occur, this was intended to give a flavour of the current practice. For each scenario, a treatment strategy was requested for a healthy 65 year old, a relatively well 80 year old and an 85 year old nursing home resident with early dementia and significant comorbidity. Details of each scenario can be found in Figure 1. It was hoped that this would give some indication of actual practice in a “real world” environment, although obviously real clinical judgments would not be made on chronological age.
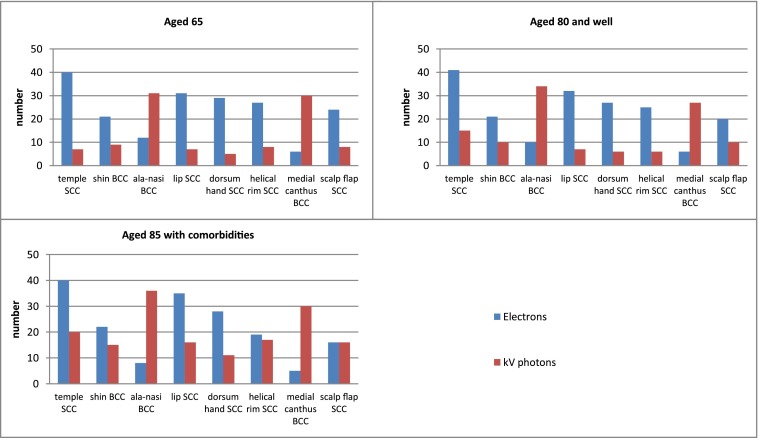
Figure 1.
Fractionation regimes employed for a given scenario in different patient groups. BCC, basal cell carcinomas; SCC, squamous cell carcinomas.
RESULTS
A total of 43 complete and 20 partially complete anonymous surveys were received. 91% of responders worked in centres with an identified clinical oncology team or individual to plan “complex” skin radiotherapy. The volume of skin cases seen varied nationally with 46.2% of respondents treating <5 cases per month; 21.1%, 5–10 cases; 25.0%, 11–20 cases; and 7.7%, >20 cases. The age of the patient seen also differed between centres with the proportion over the age of 80 years <10% in 3.9%, 10–25% in 27.5%, 25–50% in 33.3% and >50% in 35.3%.
81% of responders had access to kilovoltage radiotherapy for the treatment of skin cancers with varying energies available at different centres.
Almost all responders were expected to have expertise in more than one disease site. Only 2% treated skin cases exclusively, 24% treated two sites, 42% treated three sites, 20% treated four sites, 8% treated five sites and 4% treated six sites.
Response to the clinical scenarios posed was varied with multiple, albeit similar, fractionation regimes employed. This study mainly focused on the fractionation used and how this varied dependent on the age and fitness of patient and disease location. The results for each scenario are shown below (Figure 1). The various regimes proposed were divided into obvious groups: single fractions, 3–5 fractions, 8–10 fractions, ≥15 fractions, non-standard fractionation, brachytherapy and palliative treatments.
When treating disease at the inner canthus, a correction for stand off was made by 74% of respondents. When treating an area of recurrence within a previously grafted area, 40.6% would treat the whole graft, 50% would treat the area of recurrence with a margin and 9.4% would vary practice dependent on the graft size. The use of kilovoltage photon or electron radiotherapy varied according to the disease site and the status of the patient (Figure 2).
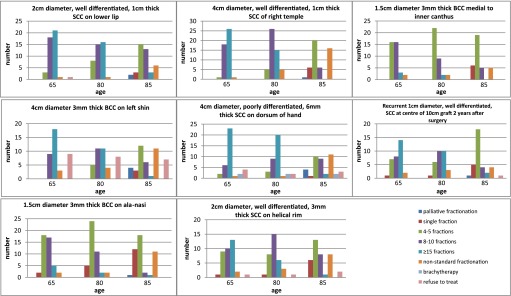
Figure 2.
Radiation modality employed for given scenario in different patient groups. BCC, basal cell carcinomas; kv, kilovoltage; SCC, squamous cell carcinomas.
An analysis of the fractionation regimes proposed in response to each scenario shows a large number of different dose fractionations employed, although several were, by far, the most likely to be used: 18–20 Gy/1#, 35 Gy/5#, 45 Gy/10# and 55 Gy/20#. A large degree of heterogeneity amongst non-standard (less than daily treatments) fractionation treatments was also shown with 24 different dose fractionations proposed. The total number of times that the more popular of these and the other standard dose fractionations were suggested is shown in Table 1.
Table 1.
Popularity of commonly suggested dose fractionations
| Dose fractionation | Number of times suggested |
|---|---|
| 18 Gy/1# | 41 |
| 20 Gy/1# | 18 |
| 32 Gy/5# | 27 |
| 35 Gy/5# | 237 |
| 40.5 Gy/9# | 22 |
| 40 Gy/10# | 29 |
| 45 Gy/10# | 170 |
| 45 Gy/9# | 51 |
| 45 Gy/15# | 15 |
| 50 Gy/15# | 56 |
| 50 Gy/20# | 57 |
| 55 Gy/20# | 134 |
| 60 Gy/30# | 26 |
| 66 Gy/33# | 11 |
| 27 Gy/3# over 2 weeks | 20 |
| 28 Gy/2# over 6 weeks | 11 |
| 38 Gy/6# over 6 weeks | 11 |
| 45 Gy/9# over 3 weeks | 24 |
DISCUSSION
The survey was answered by 63 respondents from 58 centres in the UK. Of these respondents, 43 returned completed surveys, taking a median of 28 min to do so. It is possible that the proportion of respondents completing the survey may have been improved by reducing the number of given clinical scenarios. This would, however, have lost valuable clinical information. In addition, less than 1 min was spent reviewing the survey by almost all who failed to complete it, suggesting that the overall number of scenarios that they would have been unlikely to know was not the sole reason.
The survey has shown variation between clinicians regarding the best treatment approach for a given clinical scenario. As many responders identified, the decisions about the treatments are strongly influenced by seeing the patient in the clinic. The gestalt provided from this was not possible when answering this survey, and decisions had to be made on the basis of limited information from each scenario stem. This may have affected interpretation and response. Each question was devised to highlight differences in therapy approach for commonly encountered clinical scenarios.
The survey has shown that the proportion of clinical practice occupied by respondents to treat NMSC varies greatly with almost half treating less than one case per week. It is apparent that management decisions on some skin cancers are complex such that, where possible, a reasonable throughput of patients with a limited number of other subspecialist interests is to be recommended to engender expertise.
Standard daily fractionation
Owing to slight variation in practice between the centres, it is not possible to present exact dose/fractionation regimes. Responses did, however, divide naturally into various categories: palliative treatments, single fractions, 3–5 fraction regimes giving 27.5–35.0 Gy, 8–10 fraction regimes giving 32–45 Gy, 15–33 fraction regimes giving 45–66 Gy and non-standard alternate day, twice weekly or weekly regimes. These fractionation regimes are in line with published international approaches.2,3 The use of hypofractionated daily regimes has been shown in retrospective studies to be an effective treatment approach for NMSC with outcomes equivalent to 2–3 Gy per fraction regimes and with benefits in convenience for the patient and resource requirements;4,5 these two studies used hypofractionated regimes of 44–45 Gy given in ten daily fractions or 35 Gy in five daily fractions, both of which were commonly chosen by respondents to this current survey.
The survey responses also show wide variation in the use of electron or kilovoltage photon therapy and the energies employed. Many clinicians provided answers based both on actual and preferred practice, with almost one in five not having access to kilovoltage photon therapy. Again, the sheer heterogeneity of these answers has been simplified with the focus being on fractionation rather than the detail of technique. Electrons are more likely to be used with larger lesions and younger patients. This is supported by retrospective data that have shown electrons to be at least equivalent to kilovoltage photons in small series for local control and cosmesis.6–8
In the very elderly with significant comorbidity, the challenge of trying to offer radical therapy is evident in the variety of responses seen. Palliative treatments, single fractions and non-standard fractionation are more likely to be used and indeed, for some scenarios, make up the most commonly employed approach. Retrospective data have shown that a single fraction is an effective approach for the treatment of lesions <3 cm in diameter.9 Its appropriateness for lesions larger than this was not demonstrated in that study owing to limited patient numbers, but cosmesis was shown to be better with single fraction doses of 18 or 20 Gy compared with a higher dose of 22 Gy, which was associated with a significantly increased rate of necrosis. In our survey responses, reassuringly, the suggested dose was 18 or 20 Gy in 94% of radical single fraction treatments. We feel the use of a 22-Gy single fraction should no longer be considered acceptable practice unless correcting for stand-off. Single fraction therapy should generally be avoided for large lesions, even in the less fit when non-standard fractionation should be considered.
Non-standard fractionation
The survey has shown widespread usage of non-standard fractionations in patients who might otherwise struggle to complete treatment. There is some limited published evidence supporting this approach. A single centre review of 31 cases has previously shown that 24 Gy in 3 fractions over 3 weeks, treating predominantly SCC of a median size of 5 cm, achieved local control in 61.3% of tumours, with a further 25.8% unassessable, at a median follow-up of 17 weeks and with no severe late toxicity seen.10 A retrospective review of 42 BCCs treated with 30 Gy in 5 fractions over 4 weeks demonstrated local control in 95.2% with a median follow-up of 15 months and excellent or good cosmesis in all cases.11 There is, however, a wide variation in overall treatment times, and total doses suggested in survey responses, reflecting the paucity of trial data available to guide treatment and the consequent development of local practices. It would be of benefit to have more centres publish outcomes following these treatments to establish which are most efficacious and allow development of a more uniform approach, accepting that these schedules are often used for frail patients who are not regularly reviewed post treatment.
A comparison of various non-standard regimes can be performed by calculation of biological equivalent doses (BEDs), derived from the linear quadratic equation for cell kill following radiotherapy. Previous clinical studies have suggested an α/βtumour for skin cancer of 8.5 Gy, α/βlate effects of 3 Gy, the onset time (Tk) of 28 days, cell doubling time (Tp) of approximately 4 days and α value of 0.3:12–15
Applying this suggests that the three most commonly used non-standard regimes (45 Gy/9# over 3 weeks, 27 Gy/3# over 2 weeks and 38/6# over 3 weeks) have broadly similar radiobiological characteristics. Further assuming an α/β = 3 Gy for late effects demonstrates that some of the proposed non-standard regimes (28 Gy/2# 6 weeks apart, 32.4 Gy/3# weekly and 36 Gy/4# weekly) may have too high a risk of late effects if the equations are accurate and patients are living long enough to experience them. The adoption of another schedule in their place should be considered. In addition, some other regimes are clearly prescribed with a palliative intent (18 Gy/2# over 1 or 2 weeks, 25 Gy/5# over 4 weeks and 27 Gy/6# over 3 weeks), but, given the wide spread uses of non-standard regimes with radical intent, they should be appropriate in only limited circumstances.
Treatment of disease overlying cartilage
Historically, there has been concern about the use of kilovoltage radiation for skin lesions overlying cartilage owing to a perceived risk of dose build-up in cartilage and bone through the photoelectric effect.15 This theoretical concern has, however, been contested.16 The survey assessed how current practice when treating small tumours at the ali-nasi and helical rim is affected by this evolving debate and demonstrates a marked division in practice.
Skin overlying the nose cartilage is a frequent location of skin carcinoma, representing around 25% of disease occurring on the head and neck.17 It has been shown that treatment of the skin overlying cartilage of the nose using kilovoltage radiotherapy offers good or acceptable (mild skin atrophy or dyschromia) cosmesis in 96.8% of lesions in remission.18 When treating a small 1.5-cm ali-nasi BCC, >80% of respondents to the survey elect to use kilovoltage photons. The majority of these patients are offered a treatment of 35 Gy delivered in five fractions, in line with practice reported at other international centres.18,19
By contrast, kilovoltage photons are used by only around 25% of respondents for small (2 cm) SCCs of the helix of the ear, although this proportion does increase with elderly infirm patients. This is despite retrospective data showing kilovoltage photons to have good local control in this site with low risk of late complication for both SCC and BCC.20–22 It may be that kilovoltage photons would be more likely utilized for BCC in this location, which is not a given scenario, but concerns about increased late effects with kilovoltage photon treatments may still persist nationally. This is presumably a consequence of local experience of complications and may suggest that additional factors contribute to the poor tolerance of the ear cartilage to kilovoltage photons. Of note, it has been demonstrated that the frostbite of the ear occurs almost three times more frequently than those of the nose.23 This may imply that there are vascular causes contributing to late effects of radiotherapy to the ear.
Longer fractionations over 2 weeks or more are likely to be employed for treatment of the ear, which may further reflect concerns about toleration of treatment and the larger treatment volume that the use of electrons necessitates.
The use of longer treatment regimens for disease overlying cartilage is supported by outcomes from two retrospective series of dose-fractionation schedules. These demonstrate that using fraction sizes of <4–6 Gy is associated with a significant reduction in necrosis following radiotherapy over the pinna.20,22 Others have found a reduction in visible long-term cosmetic defect using schedules of 4 weeks or more over the nasal skin.19
Treatment of areas with impaired wound healing
Various areas of the body present significant clinical challenges owing to concerns over impaired tolerance of radiotherapy and an increased risk of late effects. This survey looked to identify what general approaches are employed in this setting.
NMSC of the hand is a problematic area to treat with definitive radiotherapy, and most would recommend surgical excision of the lesion as the preferred treatment modality. In various clinical scenarios, particularly with elderly infirm patients, this may not be possible and radiotherapy can have a role to play. There are few published data for outcomes of treatment to the hand. The local control rate with radiotherapy has been quoted up to 96%, in a case series of 50.24 Historical data identified a 6% incidence of radionecrosis following radiotherapy to the hand and concerns about cosmesis persist.25 A study of the use of brachytherapy for SCC of the hand using doses of 40–45 Gy have, however, shown minimal treatment-related morbidity.26 Most respondents, around 70%, would favour a longer fractionation regime (≥15 fractions) when treating a 4-cm SCC of the dorsum of the hand. Concerns about the use of kilovoltage photons owing to underlying bone, as in other areas, are reflected in respondents using electrons in >80% of treatments in fitter patients and around 70% of treatments of the infirm. The perceived problems of radiotherapy treatment are demonstrated by 7.7% of respondents, despite the scenario stating the patient was not suitable for surgery, declining to suggest any fractionation regime. Given the excellent published outcome data, the survey demonstrates very limited and, perhaps, suboptimal use of brachytherapy for this site.
This concern with effects of radiotherapy is even more pronounced in the treatment of carcinoma of the shin, with around 20% of respondents refusing to offer treatment, even in the infirm. Historical series have reported poor wound healing or failure to heal in 9–33% of patients treated with external beam radiotherapy to the lower leg, supporting clinician caution, with local control up to 94%.27–29 In younger patients, 60% of those offering treatment for a 4-cm BCC of the shin would treat over 3 weeks or longer. In the elderly and infirm, faced with the challenges of ensuring a patient completed treatment, 32% of respondents would give 3–5 daily treatments and 30% would offer non-standard fractionation.
Post-operative recurrent disease
There is a lack of published data on post-operative radiotherapy to an area containing a skin graft. However, several published articles on radiotherapy given to skin grafts either in a laboratory setting or single centre retrospective series have shown a good tolerance with low likelihood of graft breakdown.30–33 Responders to the survey are generally comfortable giving salvage radiotherapy to recurrent disease within grafts, presumably owing to local experience of good outcome. Only a small number refuse to offer any treatment when dealing with the elderly and infirm. The use of longer fractionations is preferred for younger fitter patients, as at other sites. The lack of good data on which to base treatment decisions is reflected in the almost equal split between clinicians who would treat the entire graft or the area of recurrence with a margin.
Treatment of anatomically challenging sites
Treatment of medial canthus NMSC, predominantly BCC, is demanding both owing to its concave location and because of underlying structures, which can be directly invaded by disease. Following surgical resection, there is a risk of significant post-operative defect. Primary kilovoltage radiotherapy can yield good cosmetic results and local control rates of 94% have been reported using 35–60 Gy in 5–30 daily fractions.34,35 There is, however, little detail reported on the radiotherapy technique employed.
In this current survey, around 80% of respondents would use kilovoltage photons to treat a 1.5–3.0-mm thick BCC at the inner canthus. Owing to the anatomy of this region, it is usually impossible to achieve apposition of an applicator to the tumour. A decision, therefore, has to be made whether to compensate for this stand-off distance in calculating the prescribed dose, termed stand-off correction, which 74% (26) of responders would do. Several comment that this correction is made if the gap is 5 mm or more. The most common fractionation regime suggested is 35 Gy in five fractions, in line with published data.
Cancer of the vermillion border is the most common cancer of the head and neck after skin cancer. >90% of cases are SCCs and the vast majority involve the lower lip. Radiotherapy generally offers better cosmetic and functional results than does surgery, particularly, with larger tumours. Retrospective review has shown good local control, up to 99%, for early SCC treated with electron or kilovoltage modalities.36–40 Suggested dose fractionations used in these series varied from 40 Gy in 8 fractions to 55 Gy in 22 fractions. The survey scenario requested treatment strategy for a 1-cm thick SCC. A large majority of respondents would use electron treatments in this setting and would use longer fractionation regimes in fitter patients, similar to published data.
CONCLUSIONS
Overall, this survey has produced reassuring results. In most scenarios, the majority of clinicians would offer treatment that is in line with what published evidence is available. There is a large degree of heterogeneity is some areas, particularly, in non-standard fractionation treatments and the treatment of recurrent disease within skin grafts. With the number of dose fractionation schedules available, it should be possible to harmonize UK practice. Any attempt to achieve a more consistent approach would benefit from the publication of local outcomes of differing techniques, and this should be encouraged.
REFERENCES
- 1.Cancer Research UK. Skin Cancer statistics report August 2013. [Cited March 2014.] Available from: http://publications.cancerresearchuk.org/downloads/Product/CS_CS_SKIN.pdf
- 2.Halperin EC, Perez CA, Brady LW. Perez and Brady's principles and practice of radiation oncology. London, UK: Lippincott Williams & Wilkins; 2008. pp. 694. [Google Scholar]
- 3.Wong JR, Wang CC. Radiation therapy in the management of cutaneous malignancies. Clin Dermatol 2001; 19: 348–53. [DOI] [PubMed] [Google Scholar]
- 4.Van Hezewijk M, Creutzberg CL, Putter H, Chin A, Schneider I, Hoogeveen M, et al. Efficacy of hypofractionated schedule of electron beam radiotherapy for epithelial skin cancer: analysis of 434 cases. Radiother Oncol 2010; 95: 245–9. doi: 10.1016/j.radonc.2010.02.024 [DOI] [PubMed] [Google Scholar]
- 5.Kwan W, Wilson D, Moravan V. Radiotherapy for locally advanced BCC and SCC of skin. Int J Radiat Oncol Biol Phys 2004; 60: 406–11. [DOI] [PubMed] [Google Scholar]
- 6.Lovett RD, Perez CA, Shapiro SJ, Garcia DM. External irradiation of epithelial skin cancer. Int J Radiat Oncol Biol Phys 1990; 19: 235–42. [DOI] [PubMed] [Google Scholar]
- 7.Griep C, Davelaar J, Scholten AN, Chin A, Leer JW. Electron beam therapy is not inferior to superficial X-ray therapy in the treatment of skin carcinoma. Int J Radiat Oncol Biol Phys 1995; 32: 1347–50. [DOI] [PubMed] [Google Scholar]
- 8.Locke J, Karimpour S, Young G, Lockett MA, Perez CA. Radiotherapy for epithelial skin cancer. Int J Radiat Oncol Biol Phys 2001; 51: 748–55. [DOI] [PubMed] [Google Scholar]
- 9.Chan S, Dhadda AS, Swindell R. Single fraction radiotherapy for small superficial carcinoma of the skin. Clin Oncol (R Coll Radiol) 2007; 19: 256–9. [DOI] [PubMed] [Google Scholar]
- 10.Barnes E, Bren D, Culleton S, Zhang L, Tsao M, Balogh J. Palliative radiotherapy for non-melanoma skin cancer. Clin Oncol 2010; 22: 844–9. [DOI] [PubMed] [Google Scholar]
- 11.Kouloulias V, Kouvaris J, Mosa E, Georgakopoulos J, Platoni K, Papadopoulos O, et al. Efficacy, cosmesis and skin toxicity in a hypofractionated irradiation schedule for cutaneous basal cell carcinoma of the head and neck area. Head Neck Oncol 2012; 4: 88. [Google Scholar]
- 12.Thames HD, Bentzen SM, Turesson I, Overgaard M, Van den Bogaert W. Time dose factors in radiotherapy: a review of the human data. Radiother Oncol 1990; 19: 219–35. [DOI] [PubMed] [Google Scholar]
- 13.Maciejewski BA, Skates S, Zajusz A, Lange D. Importance of tumour size and repopulation for radiocurability of skin cancer. Neoplasma 1993; 40: 51–4. [PubMed] [Google Scholar]
- 14.Bentzen SM, Thames HD. Clinical evidence for tumour clonogen regeneration: interpretations of the data. Radiother Oncol 1991; 22: 161–6. [DOI] [PubMed] [Google Scholar]
- 15.Allan E, Stanton A, Pye D, Collins C, Perry L, Filby M, et al. Fractionated high dose rate brachytherapy moulds—a precise treatment for carcinoma of the pinna. Radiother Oncol 1998; 48: 277–81. [DOI] [PubMed] [Google Scholar]
- 16.Atherton P, Townley J, Glaholm J. Cartilage: the “F”-factor fallacy. J Clin Oncol (R Coll Radiol) 1993; 5: 391–2. [DOI] [PubMed] [Google Scholar]
- 17.Koplin L, Zarem HA. Recurrent basal cell carcinoma: a review concerning the incidence, behaviour and management of recurrent basal cell carcinoma, with emphasis in the incompletely excised lesions. Plast Reconstr Surg 1980; 65: 656–63. [PubMed] [Google Scholar]
- 18.Caccialanza M, Piccinno R, Percivalle S, Rozza M. Radiotherapy of carcinoma of the skin overlying the cartilage of the nose: our experience in 671 lesions. J Eur Acad Dermatol Venereol 2009; 23: 1044–9. doi: 10.1111/j.1468-3083.2009.03247.x [DOI] [PubMed] [Google Scholar]
- 19.Tsao MN, Tsang RW, Liu FF, Panzarella T, Rotstein L. Radiotherapy management for squamous cell carcinoma of the nasal skin: the Princess Margaret Hospital experience. Int J Radiat Oncol Biol Phys 2002; 52: 973–9. [DOI] [PubMed] [Google Scholar]
- 20.Hayter CR, Lee KH, Brundage MD. Necrosis following radiotherapy for carcinoma of the pinna. Int J Radiat Oncol Biol Phys 1996; 36: 1033–7. [DOI] [PubMed] [Google Scholar]
- 21.Lim JT. Irradiation of the pinna with superficial kilovoltage radiotherapy. Clin Oncol (R Coll Radiol) 1992; 4: 236–9. [DOI] [PubMed] [Google Scholar]
- 22.Silva JJ, Tsang RW, Panzarella T, Levin W, Wells W. Results of radiotherapy for epithelial skin cancer of the pinna: the Princess Margaret Hospital experience 1982–1993. Int J Radiat Oncol Biol Phys 2000; 47: 451–9. [DOI] [PubMed] [Google Scholar]
- 23.Lehmuskallio E, Lindholm H, Koskenvuo K, Sarna K, Friberg O, Viljanen A. Frostbite of the face and ears: epidemiological study of risk factors in Finnish conscripts. BMJ 1995; 311: 1661–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Szabo P. Radiotherapy of carcinomas of the dorsum manus. [In German.] Strahlentherapie 1981; 157: 242–4. [PubMed] [Google Scholar]
- 25.Raynor CR. The results of treatment of two hundred and seventy three carcinomas of the hand. Hand 1981; 13: 183–6. [DOI] [PubMed] [Google Scholar]
- 26.Somanchi BV, Stanton A, Webb M, Loncaster J, Allen E, Muir LT. Hand function after high dose rate brachytherapy for squamous cell carcinoma of the skin of the hand. Clinical Oncol (R Coll Radiol) 2008; 20: 691–7. [DOI] [PubMed] [Google Scholar]
- 27.Cox NH, Dyson P. Wound healing on the lower leg after radiotherapy or cryotherapy of Bowen's disease and other malignant lesions. Br J Dermatol 1995; 133: 60–5. [DOI] [PubMed] [Google Scholar]
- 28.Dupree MT, Kiteley RA, Weismantle K, Panos R, Johnstone PA. Radiation therapy for Bowen's disease: lessons for lesions of the lower extremity. J Am Acad Dermatol 2001; 45: 401–4. [DOI] [PubMed] [Google Scholar]
- 29.Podd TJ. Treatment of lower limb basal cell and squamous cell carcinomas with radiotherapy. Clin Oncol (R Coll Radiol) 1992; 4: 44–5. [DOI] [PubMed] [Google Scholar]
- 30.Lawrence WT, Zabell A, McDonald HD. The tolerance of skin grafts to postoperative radiation in patients with soft-tissue sarcoma. Ann Plast Surg 1986; 16: 204–10. [DOI] [PubMed] [Google Scholar]
- 31.Sumi Y, Ueda M, Kaneda T, Eto K. Effects of irradiation on grafted skin. J Oral Maxillofac Surg 1983; 41: 586–91. [DOI] [PubMed] [Google Scholar]
- 32.Bui DT, Chunilal A, Mehrara BJ, Disa JJ, Alektiar KM, Cordeiro PG. Outcome of split-thickness skin grafts after external beam radiotherapy. Ann Plast Surg 2004; 52: 551–6. [DOI] [PubMed] [Google Scholar]
- 33.Kulahci Y, Duman H, Zor F, Bozkurt M, Guden M, Gunhan O, et al. The effect of external beam irradiation timing on skin graft survival. Eur Surg Res 2010; 44: 142–51. doi: 10.1159/00027698 [DOI] [PubMed] [Google Scholar]
- 34.Krema H, Herrmann E, Albert-Green A, Payne D, Laperriere N, Chung C. Orthovoltage radiotherapy in the management of medial canthus basal cell carcinoma. Br J Ophthalmol 2013; 97: 730–4. doi: 10.1136/bjophthalmol-2012-302991 [DOI] [PubMed] [Google Scholar]
- 35.Swanson EL, Amdur RJ, Mendenhall WM, Morris CG, Kirwan JM, Flowers F. Radiotherapy for basal cell carcinoma of the medial canthus region. Laryngoscope 2009; 119: 2366–8. doi: 10.1002/lary.20658 [DOI] [PubMed] [Google Scholar]
- 36.de Visscher JG, Grond AJ, Botke G, van der Waal I. Results of radiotherapy for squamous cell carcinoma of the vermilion border of the lower lip: a retrospective analysis of 108 patients. Radiother Oncol 1996; 39: 9–14. [DOI] [PubMed] [Google Scholar]
- 37.Cerezo L, Lui FF, Tsang R, Payne D. Squamous cell carcinoma of the lip: analysis of the Princess Margaret Hospital experience. Radiother Oncol 1993; 28: 142–7. [DOI] [PubMed] [Google Scholar]
- 38.Petrovich Z, Parker RG, Luxton G, Kuisk H, Jepson J. Carcinoma of the lip and selected sites of the head and neck skin. A clinical study of 896 patients. Radiother Oncol 1987; 8: 11–17. [DOI] [PubMed] [Google Scholar]
- 39.Sykes J, Allen E, Irwin C. Squamous cell carcinoma of the lip: the role of electron treatment. Clin Oncol (R Coll Radiol) 1996; 8: 384–6. [DOI] [PubMed] [Google Scholar]
- 40.Mccombe D, Macgill K, Ainslie J, Beresford J, Matthews J. Squamous cell carcinoma of the lip: a retrospective review of the Peter, M McCallum Cancer Institute experience 1979–1988. Aust N Z J Surg 2000; 70: 358–61. [DOI] [PubMed] [Google Scholar]