Abstract
Pneumomediastinum (PM) is mainly an atypical finding among traumatic neck or thoracic injury patients. Moreover, PM secondary to isolated orbital floor fracture remains a rare event which is infrequently associated with severe complications such as mediastinitis, airway obstruction and pneumothorax. Herein, we report an atypical case of mediastinal emphysema consequent to orbital floor fracture along with review of the literature.
INTRODUCTION
Surgical or subcutaneous emphysema (presence and spread of air in subcutaneous or submucous tissues) is a common finding in maxillofacial practice. It is also a frequent complication of trauma, surgery, endoscopy, endotracheal intubation and multitude of other conditions [1]. Although different sources are described, chest trauma remains the most frequent cause of subcutaneous emphysema following blunt or penetrating injuries [1].
Associated pneumomediastinum (PM) or mediastinal emphysema usually denotes a primary perforation of visceral organ such as trachea, esophagus, bronchus or an intraabdominal hollow viscus injury [2]. Subcutaneous emphysema is caused by the upward movement of gas to the subcutaneous areas through fascial planes; the reverse pathway is very rare (occurrence of PM after maxillofacial trauma) [2]. Herein, we report an atypical case of mediastinal emphysema secondary to orbital floor fracture.
CASE REPORT
A 45-year-old Nepalese male presented to the trauma room after facial trauma assault. He has been hit mainly to his face 2 days prior to the index admission. The patient complained of left-sided facial swelling and pain with chest pain and progressive difficulty in swallowing.
Initial vital signs showed blood pressure of 120/80 mmHg, a pulse rate of 92 beats/min and a respiratory rate of 26 breaths/min. On physical examination, left periorbital swelling and tenderness were observed. Extraocular eye movements were intact in all directions and there was no sign of diplopia. Inspection of larynx revealed no sign of blunt or penetrating neck trauma. By palpation of larynx, laryngeal skeleton was intact and the endolaryngeal examination revealed normal mucosal integrity.
Palpation revealed tactile crepitus over the left orbit, cheek, neck and thoracic wall. By auscultation, heart sounds and bilateral breath sounds were normal. Laboratory investigations and electrocardiogram were within normal.
Chest X-ray and head, neck and chest computed tomography (CT) confirmed the diagnosis and extension of PM (Figs 1–3). CT revealed fracture of the floor of left orbit with soft tissue, fat herniation into left maxillary sinus roof, left orbital emphysema with no muscular entrapment. Gas was observed in periorbital tissues, left temporal scalp, infratemporal fossa, left parapharyngeal space and left cheek. Moreover, tissue planes in the neck revealed the presence of air particularly around the carotid vessels, in the posterior triangle and superior mediastinum (PM) around the thymus, trachea (middle), left side of the aorta and anterior to the sternum. However, on auscultation, lungs were clear with and the laryngeal passages and trachea looked normal.
Figure 2:
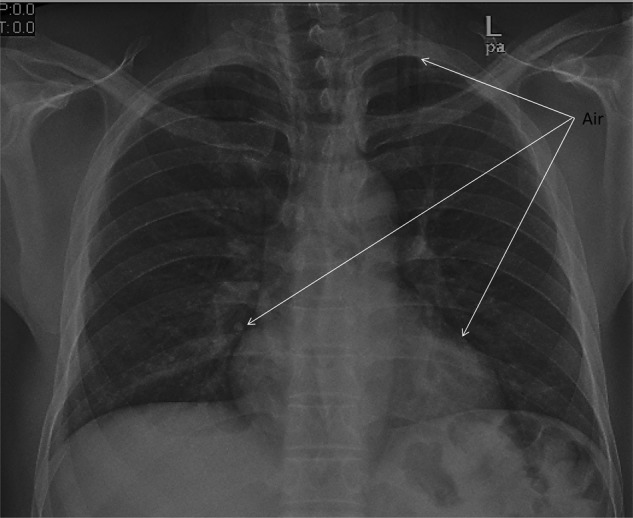
Chest X-ray shows the air extension in the chest.
Figure 1:
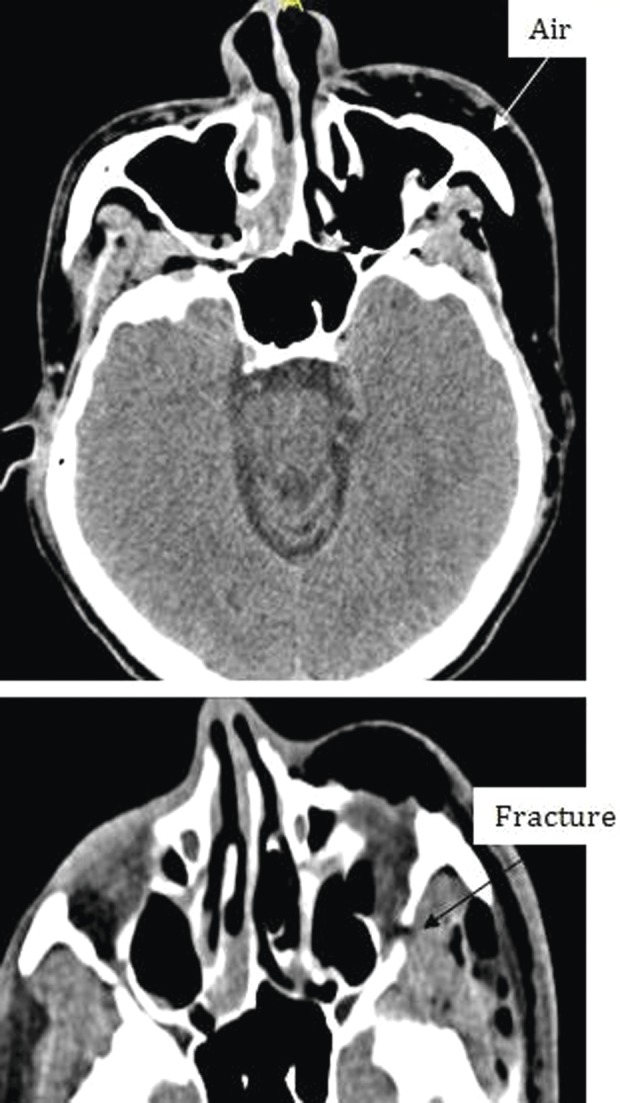
Different levels of head imagining showing fracture of the floor of the orbit and subcutaneous air.
Figure 3:
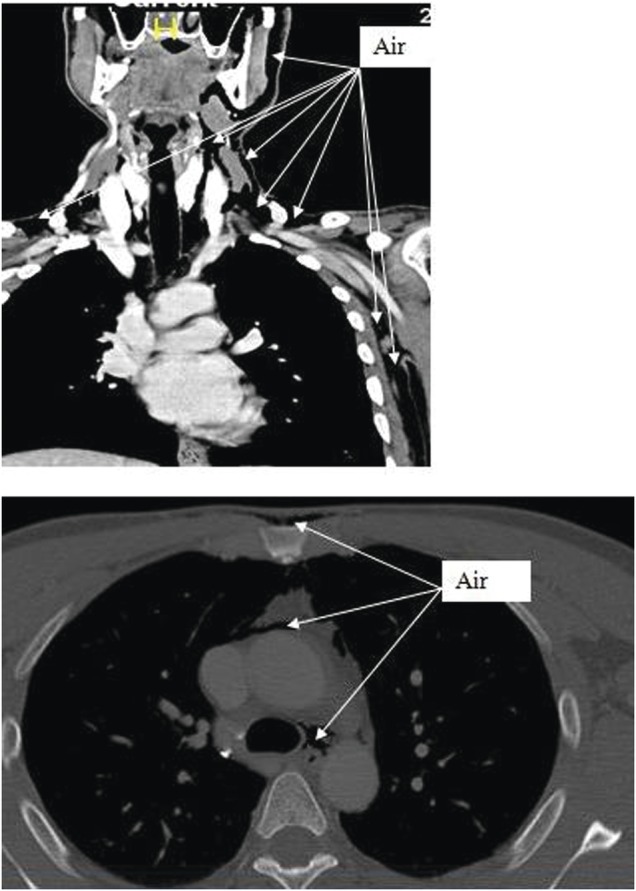
CT scan shows the extension of air from the face, neck and chest.
The patient was admitted for observation and started prophylactically on Co-AmoxiClav 1.2-g intravenously twice daily to avert potential mediastinitis. The patient was kept sitting and was instructed to avoid forceful blowing. The patient symptoms improved, while his emphysema initially increased, and follow-up CT with oral and IV contrast revealed no new changes. The fracture was treated conservatively; the patient tolerated full diet with uneventful hospital course and was discharged on the third hospital day with out-patient follow-up.
DISCUSSION
PM or the presence of air in the mediastinal space is a well-established event that might occur either spontaneously (rare) or due to severe post-traumatic thoracic-abdominal injury [2]. Moreover, procedures that involve trachea, bronchi, esophagus and natural facial planes might be involved in leakage of gas into the subcutaneous space of head and neck. Zylak et al. [3] described a path to the submandibular space via retropharyngeal space, and vascular sheaths within the neck to produce subcutaneous emphysema, pneumothorax and pneumopericardium. The authors also described the potential communication with peritoneum and retroperitoneal spaces to cause pneumoperitoneum and pneumoretroperitoneum.
PM itself does not signify a morbid condition (very rare linkage with airway compromise or tension), it is rather a marker of underlying illness or injuries [4]. Of note, tracheobronchial rupture, esophageal injury or perforation of a hollow abdominal viscus may cause free mediastinal air. So, the presence of PM particularly in the absence of associated lung injury and pneumothorax is taken as a red flag for these severe potentially lethal injuries.
Clinically, PM might be asymptomatic or may be associated with chest or neck pain, cough, vomiting, voice change or stridor, low-grade fever, respiratory distress and mechanical shock (tension) [4]. Huon et al. [5] also reported neck pain, swelling and odynophagia to be the primary initial symptoms of spontaneous PM. Clinical signs may include subcutaneous emphysema, crepitations or murmur (precordial systolic crepitations and diminution of heart sounds) [4].
The diagnosis of occult PM and exclusion of associated aerodigestive injuries could be made by chest X-ray and CT scan [6]. Rezende-Neto et al. [7] reported occult PM in 6% of blunt chest trauma cases confirmed by chest CT scan. Although the investigators found higher injury severity score in occult PM cases, none of them had associated aerodigestive injuries.
Furthermore, in the case of suspected esophageal perforation, contrast studies are mandatory. Some authors recommended the use of a water-soluble contrast agent followed by a barium meal if the findings are normal in order to increase the sensitivity of the test [8]. Bronchoscopy is indicated if a tracheobronchial perforation is suspected, which may be observed occasionally following blunt chest trauma [9]. These patients should be observed very closely for evolving fever and signs of worsening respiratory distress or systemic sepsis. Moreover, mediastinitis is one of its known complications [2].
A recent case report presented facial subconjuctival and subcutaneous emphysema after an orbital floor fracture [10]. But, the occurrence of PM after facial trauma is extremely rare.
In conclusion, PM is a rare complication associated with blunt facial trauma. Intravenous antibiotic prophylaxis might be administered to avert mediastinitis and forceful blow to the nose should be avoided until complete recovery. In the absence of clear guidelines for the management of this rare entity clinical judgment and sound practices would be the guide for what is needed to do. This case report of mediastinal emphysema will be a basis for further clarification of this rare association and can guide future approach to similar cases regarding prognosis and management.
The authors thank all the trauma surgery staff for their cooperation. The authors have no conflict of interests and no financial issues to disclose. All authors read and approved the case report. This case report has been approved by the Medical Research Center (IRB no.13440/13), Hamad Medical Corporation.
CONFLICT OF INTEREST
The authors have no conflicts of interest to declare.
REFERENCES
- 1.Maunder RJ, Pierson DJ, Hudson LD. Subcutaneous and mediastinal emphysema. Pathophysiology, diagnosis, and management. Arch Intern Med. 1984;144:1447–53. [PubMed] [Google Scholar]
- 2.Naiboğlu Barıs. Extensive subcutaneous emphysema and pneumomediastinum associated with blowout fracture of the medial orbital wall. J Trauma. 2008;64:1366–9. doi: 10.1097/01.ta.0000235507.60878.3d. [DOI] [PubMed] [Google Scholar]
- 3.Zylak CM, Standen JR, Barnes GR, Zylak CJ. Pneumomediastinum revisited. Radiographics. 2000;20:1043–57. doi: 10.1148/radiographics.20.4.g00jl131043. [DOI] [PubMed] [Google Scholar]
- 4.Damore DT, Dayan PS. Medical causes of pneumomediastinum in children. Clin Pediatr (Phila) 2001;40:87–91. doi: 10.1177/000992280104000204. [DOI] [PubMed] [Google Scholar]
- 5.Huon LK, Chang YL, Wang PC, Chen PY. Head and neck manifestations of spontaneous pneumomediastinum. Otolaryngol Head Neck Surg. 2012;146:53–7. doi: 10.1177/0194599811421870. [DOI] [PubMed] [Google Scholar]
- 6.Dissanaike S, Shalhub S, Jurkovich GJ. The evaluation of pneumomediastinum in blunt trauma patients. J Trauma. 2008;65:1340–5. doi: 10.1097/TA.0b013e318169cd24. [DOI] [PubMed] [Google Scholar]
- 7.Rezende-Neto JB, Hoffmann J, Al Mahroos M, Tien H, Hsee LC, Spencer Netto F, et al. Occult pneumomediastinum in blunt chest trauma: clinical significance. Injury. 2010;41:40–3. doi: 10.1016/j.injury.2009.06.161. [DOI] [PubMed] [Google Scholar]
- 8.Demetriades D. Assessment and Management of Trauma. 5th edn. 2009. http://www.surgery.usc.edu/acutecare/downloads/redbook.pdf. accessed on 26 August 2013)
- 9.Neal MD, Sippey M, Gaines BA, Hackam DJ. Presence of pneumomediastinum after blunt trauma in children: what does it really mean? J Pediatr Surg. 2009;44:1322–7. doi: 10.1016/j.jpedsurg.2009.02.069. [DOI] [PubMed] [Google Scholar]
- 10.Ababneh OH. Orbital, subconjunctival, and subcutaneous emphysema after an orbital floor fracture. Clin Ophthalmol. 2013;7:1077–9. doi: 10.2147/OPTH.S44649. [DOI] [PMC free article] [PubMed] [Google Scholar]


