Abstract
Objective
Many maternal-fetal medicine (MFM) specialists provide dilation and evacuation (D&E) procedures for their patients with fetal or obstetrical complications. Our study describes the D&E training opportunities available to MFM trainees during their fellowship.
Study Design
National surveys of MFM fellows and fellowship program directors assessed the availability of D&E training in fellowship. Univariate and multivariate comparisons of correlates of D&E training and provision were performed.
Results
Of the 270 MFM fellows and 79 fellowship directors contacted, 92 (34%) and 44 (56%) responded, respectively. More than half of fellows (60/92) and almost half of fellowship programs (20/44) report organized training opportunities for D&E. Three-quarters of fellows surveyed believe that D&E training should be part of MFM fellowship, and a third of fellows who have not yet been trained would like training opportunities. Being at a fellowship that offers D&E training is associated with 7.5 times higher odds of intending to provide D&E after graduation. (p=0.005, 95% CI 1.8 – 30)
Conclusion
MFM physicians are in a unique position to provide termination services for their patients with pregnancy complications. Many MFMs provide D&E services during fellowship and plan to continue after graduation. MFM fellows express a strong interest in D&E training, and D&E training opportunities should be offered as a part of MFM fellowship.
Keywords: Dilation & Evacuation, Maternal-fetal medicine training, Second-trimester abortion
INTRODUCTION
Approximately 120,000 second-trimester abortions are done each year in the US (1, 2). Dilation and evacuation (D&E) is the most common method of second-trimester abortion but requires specialized training, which is not available at almost a third of all US obstetrics and gynecology (OB/GYN) residency programs (3). Due in part to limited availability of training in the procedure, D&E providers are scarce, with only 67% of self-identified abortion providers offering D&E services during the second trimester, and only 23% after 20 weeks (1). The downstream effect of this scarcity is that many women identify difficulty finding a provider as a major barrier to accessing D&E services and as a cause of delay in obtaining abortion services (4).
Maternal-fetal medicine (MFM) subspecialists can play a role in increasing access to D&E services; these subspecialists care for women with complicated pregnancies and fetal anomalies who may desire or require second-trimester termination. In addition, MFMs are located throughout the country and may be found in areas where there are no other second-trimester abortion providers (5). A recent survey of MFMs indicates that 31% of respondents provide at least one D&E per year, and that 33% of those who provide were trained after residency (6). Like OB/GYN residency programs, MFM fellowship programs require training in pregnancy termination, but do not specify the technique or gestational age. The American Board of Obstetrics and Gynecologists (ABOG) recognizes that performing D&E for second-trimester fetal death or lethal anomalies is within the scope of practice of maternal-fetal medicine, but unlike other procedures needed by women with pregnancy complications (amniocentesis, cerclage) only an understanding of the risks and indications, rather than actual clinical experience, is required for graduation (7).
While we know that many MFMs receive training in D&E during fellowship, little is known about MFM fellows’ interest in training, how frequently D&E training is offered, and what components are included in training. We surveyed MFM fellows and MFM fellowship program directors to describe fellows’ interest in and availability of D&E training during MFM fellowship.
MATERIALS AND METHODS
We recruited MFM fellows by contacting all associate members of the Society for Maternal Fetal Medicine (SMFM) as well as inviting fellows currently enrolled in one of the American Board of Obstetricians and Gynecologists (ABOG) approved Maternal-Fetal Medicine fellowship sites in 2010. The names were obtained from a purchased list available through the SMFM, the ABOG subspecialty handbook, and by searching the institutional websites of the fellowship sites. When we were able to obtain email addresses from the institutional websites or from PubMed, we sent an email invitation with a link to the online survey. Fellows for whom an email address was not available received a mailed invitation containing the survey as well as a link to the online version. If names of the fellows were not publicly available from institutional websites, we sent paper surveys addressed to “MFM Fellow” at their respective institutions. Those recruited via email received three separate email invitations, while those receiving the paper survey received a postcard reminder once after the original mailing. As an incentive, respondents were offered a $5 gift card that was not contingent upon completing the survey. To preserve anonymity, the respondent’s name and address were entered separately from the survey responses. All responses were entered into KeySurvey, an online software program.
The survey included 75 questions on topics that included demographics and training opportunities available at their fellowship. Training opportunities were classified as “routine” (a required fellowship rotation), “opt-in” (available for interested fellows to arrange) or “not available”. We also asked questions about previous experience with D&E and about abortion attitudes with five questions with Likert scale responses. Abortion attitude scores ranged from 5 to 25, with higher scores reflecting attitudes more supportive of abortion. (8) This survey was completely anonymous, and asked only about geographic location but not about fellowship institution.
To complement the individual fellow's perspective, we then conducted a follow-up study directed at MFM fellowship program directors to confirm the availability of training opportunities. We sent a link to a 10-question online survey to the 79 ABOG-approved MFM fellowship program directors whose names and emails are publicly available on the SMFM website. Two reminder invitations were sent and a $5 gift card was offered as an incentive. These questions focused directly on the D&E training opportunities available to MFM fellows and the estimated proportion of fellows who participate. Fellowship directors were asked about the availability of formal routine or opt-in rotations (identical to the options given to the fellows themselves) but a third category capturing informal training opportunities (“no formal training, but fellows can participate in D&E when they occur”) was added based on feedback from the fellows’ survey. Both surveys were approved by the Committee on Human Research at the University of California, San Francisco.
We performed descriptive statistics with chi-square tests as well as multivariable logistic regression to identify correlates of D&E provision and training. We compared geographic characteristics with publicly available information about MFM and family planning fellowships. (9, 10) All analyses were performed with Stata 12 (StataCorp 2011, College Station, TX). Results with a p-value of less than 0.1 were examined for possible statistical significance due to our small sample size and our desire to avoid a Type II error of concluding no difference where one does truly exist.
RESULTS
Characteristics of Respondents
Of the 270 MFM fellows in 2010, we obtained the names of 190 and the email addresses of 156. A total of 126 paper surveys were mailed, 80 of which were addressed to “MFM Fellow” since names were not available. Ninety-two fellows responded to our survey for an overall response of 34%, with those invited by email more likely to respond (48%, 75/156). The majority of survey respondents were female (78%) and most lived either in the Northeast or the West (Table 1). Forty-four of the 79 MFM fellowship program directors completed our survey, for a response rate of 56%. These fellowship directors are at programs that train 168 fellows, 57% of all current MFM fellows. The majority of fellowship directors who responded to our survey were from the Northeast or South/Southwest (Table 1). Nationally, most fellows and fellowship programs are located in the Northeast (33%), followed by the South and the Midwest (23% each) and the West (18%) (9). However, there were no statistically significant differences between the geographic distribution of the fellows or the fellowship directors when compared with the national distribution of MFM fellowships (chi-square test p=0.358 and p=0.801, respectively).
Table 1.
Characteristics of Survey Respondents
| Characteristic | MFM fellows (n=92) | MFM fellowship directors (n=44) | All MFM fellowships* (n=79) |
|---|---|---|---|
| Region | |||
| Northeast | 37 (40%) | 16 (37%) | 26 (33%) |
| West | 22 (24%) | 6 (14%) | 14 (18%) |
| Midwest | 17 (18%) | 9 (21%) | 20 (25%) |
| South | 16 (17%) | 13 (30%) | 19 (24%) |
| Family Planning (FP) fellowship at institution | 59 (64%) ** | 15 (34%) | 24 (30%) |
MFM=Maternal-fetal medicine
Data from the Society for Maternal-Fetal Medicine (9) and the Fellowship in Family Planning (10)
p<0.001 for chi-square test of difference comparing prevalence of FP fellowship among MFM fellow respondents and the national prevalence. No other comparisons were statistically significant.
Results from Fellows’ Survey
Over two-thirds of MFM fellow respondents are in fellowships that offer D&E training (n=60, 65%), and three-quarters of those fellows have training that is opt-in rather than routine. Training is equally likely to be supervised by a MFM or a family planning subspecialist (45% vs 42%). D&E training is most likely to occur in the hospital operating room (60%) compared with labor and delivery (15%) or in an outpatient setting (22%).
When asked about their personal provision of second-trimester abortions, 87% of fellows provide either induction termination or D&E, while 37% of respondents perform D&E. Most fellows who provide D&E were trained in residency, but 22% report that they received training only during their fellowships. Just over one-third of fellows responding to the survey intend to provide D&E services for their patients after fellowship (37%). After adjusting for abortion attitude and having been trained in D&E, being at a fellowship that offers D&E training (either opt-in or routine) is associated with 7.5 times higher odds of intending to provide D&E later in their career. (p=0.005, 95% CI 1.8 – 30) (Table 2)
Table 2.
Correlates of fellows who intend to provide dilation and evacuation (D&E) after fellowship
| Correlate | Fellows who intend to provide D&E (n=36) | Fellows who don't intend to provide D&E (n=56) | Unadjusted OR (95% CI) | Adjusted OR (95% CI) |
|---|---|---|---|---|
| Age (±SD) | 34 (±3.6) | 34 (±3.5) | 0.99 (0.9 – 1.1)* | -- |
| Location (South vs other) | 5 (14%) | 11 (20%) | 0.65 (0.2 – 2.1) | -- |
| Male | 14 (39%) | 6 (11%) | 0.2 (0.06 – 0.6) | -- |
| FP fellowship at current institution | 26 (72%) | 33 (59%) | 1.8 (0.7 – 4.5) | -- |
| FP fellowship at past institution | 13 (36%) | 22 (41%) | 0.8 (0.3 – 1.9) | -- |
| D&E Training offered in fellowship | 32 (89%) | 28 (50%) | 8 (2.5 – 25) | 7.5 (1.8 – 30) |
| Abortion attitude score† (±SD) | 19 (±2.9) | 16 (±4.6) | 1.2 (1.1 – 1.4)‡ | 1.2 (1.0 – 1.4) |
| Trained in D&E (at any time) | 32 (89%) | 22 (39%) | 12.4 (3.9 – 39) | 7.6 (2.1 – 26) |
| Trained in residency | 20 (56%) | 20 (35%) | 2.3 (0.9 – 5.3) | -- |
Odds ratio for each increase in year
Abortion attitude scores can range from 5 to 25, with higher scores reflecting attitudes more supportive of abortion
Odds ratio for one point increase in abortion attitude score
FP=Family Planning
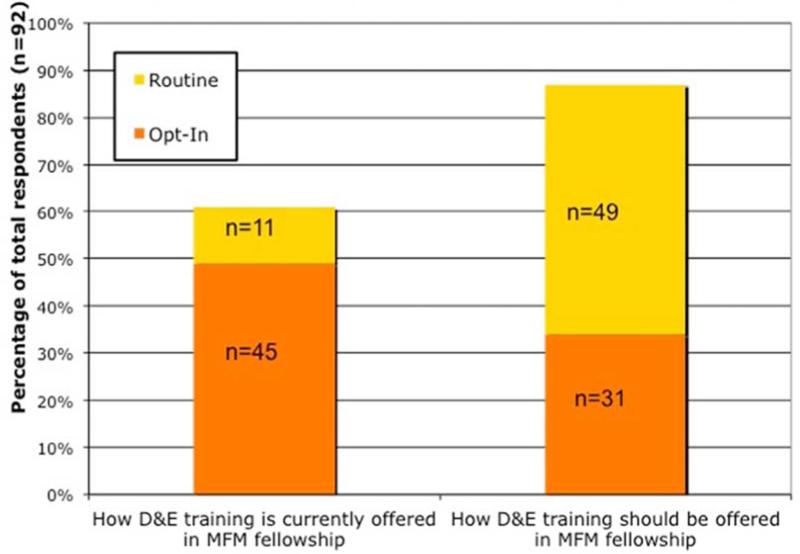
Of the 58 fellows who do not currently provide D&E, 31% report lack of training as the major barrier to provision, and 34% would like to provide D&E. Of the 38 fellows who have not been trained in D&E, nearly half desire training. Almost one-third of fellows currently at fellowships that do not offer D&E training would like to be trained (29%). The overwhelming majority of respondents think that D&E training should be offered during MFM fellowship (86%), with routine training identified as the preferred strategy of fellows at institutions both with and without D&E training (Figure 1).
Figure 1.
Dilation and evacuation (D&E) training opportunities according to maternal-fetal medicine (MFM) Fellows.
The figure displays the percentage of fellows who report routine or optional D&E training available at their fellowship and the percentage of fellows who think that routine or optional D&E training should be available.
Results from Fellowship Directors’ Survey
According to the fellowship directors who responded to our survey, 46% of programs offer some type of organized D&E training, with routine training as the least common training strategy, seen in only 18% of all programs (N=8). The most common training environment for MFM fellows is an informal one, where although there is no formalized training elective, fellows can participate in D&Es that are done on L&D or in the OR rather than in a dedicated family planning clinical location (N=18, 41%). Eleven percent (N=5) of MFM fellowships do not offer any type of D&E training, while the remainder of programs have optional training (N=13, 30%). Consistent with what was reported by the fellows, training most often occurs in the hospital operating room (52%) and is staffed by an MFM attending (51%).
Compared with programs that do not offer organized D&E training, programs that do offer training are more likely to be located in the West (24% vs 4%, p=0.06) and to collaborate with family planning subspecialists to provide training (43% vs 17%, p=0.06). Our data suggested that of those who responded to the survey, programs with informal training opportunities may be more likely to have the majority of fellows participate in D&E training (50% vs 23%, p=0.09) compared with programs with more formalized opportunities (Table 3). However, none of these results had a p-value less than 0.05 and so they may be due to chance alone.
Table 3.
Correlates of maternal-fetal medicine (MFM) fellowships that offer dilation and evacuation (D&E) training
| D&E training offered in routine or optional way (N=21) | No organized D&E training (N=23) | P value | |
|---|---|---|---|
| Western Region | 5 (24%) | 1 (4%) | 0.06 |
| Population > 1 million | 6 (29%) | 3 (13%) | 0.2 |
| Total number of fellows in fellowship (median) | 3 | 3 | 0.2 |
| Family planning fellowship | 9 (43%) | 6 (26%) | 0.2 |
| Training performed in hospital operating room | 13 (62%) | 10 (43%) | 0.2 |
| Trained by family planning specialist | 9 (43%) | 4 (17%) | 0.06 |
| Trained by MFM specialist | 10 (47%) | 10 (43%) | 0.8 |
| More than half of fellows pursue D&E training | 5 (23%) | 9 (50%) | 0.09 |
| Upper limit of gestational age of procedures performed (median) | 22 | 22 | 0.4 |
COMMENT
Although training in D&E is not required by the American Board of Obstetrics and Gynecology, the Maternal-Fetal Medicine fellowship governing body, 80% of MFM fellows responding to our survey believe that D&E training should be offered during fellowship. Currently, most fellow respondents are at fellowships that offer some type of training. However, a training gap still exists, with a substantial number of fellows desiring D&E training. In contrast to the informal training opportunities that are most commonly offered in MFM fellowships, MFM fellows responding to our survey desire routine, formal training electives. While the majority of MFMs nationwide do not provide D&Es, MFM attendings are the most common physicians to train MFM fellows.
We were surprised to see that fellowships with formalized rotations are less likely than those with informal training opportunities to engage more than half of fellows in D&E training according to the fellowship directors’ survey, although this result was not statistically significant and may be due to chance alone. Studies of ob-gyn residency training have found the opposite – that routine, integrated training is associated with a higher resident participation level. (3) It is possible that the directors at sites with informal training who responded to our survey were in MFM divisions that were very supportive of fellows’ training in D&E and may not be representative of programs with informal training that did not respond. Another explanation is that fellows who had training in residency may not choose to participate in a formalized rotation, but would participate in the occasional D&E to maintain skills. Our finding highlights that fellowships without formal D&E training electives can still engage fellows in D&E provision, and that informal training opportunities are likely important for previously trained fellows who do not desire a formal rotation. It is unknown whether this informal training is sufficient to ensure competency among those without prior training. Data from the fellows’ survey suggest that fellows are not satisfied with these informal opportunities, since three-quarters of MFM fellows at programs without formal electives desire formal training opportunities.
Consistent with recent data from our group on the practice patterns of practicing MFMs (6), over one-third of MFM fellows already provide D&E services for their patients and intend to provide after graduation from fellowship. The finding that fellows at sites that offer D&E training are more likely to report an intention to provide D&Es after graduation raises the question whether the training itself provoked the intention or whether the intention to provide shaped the decision of where to attend fellowship. Due to our cross-sectional survey design, we are unable to answer this question.
An important limitation of our survey is the relatively low response rate of the fellows. Although we attempted to contact all MFM fellows, we only invited 190 fellows by name. Due to the anonymity of the survey, we cannot report the number of respondents who were not personally invited, but we can guess that it would be very low. If we assume that all of the respondents were personally invited by email or mail survey, our response rate would be 48%, on par with other published surveys of physicians. The response rate among the fellowship directors exceeded 50%. Respondents to both surveys have a geographic distribution that is similar to the distribution of all MFM fellowships, but the fellows who responded are more likely to be at institutions with family planning fellowships, which may indicate that their responses are less generalizable. As with all surveys, selection bias occurs by including only those who chose to respond. In a survey that deals with the controversial topic of abortion, it is possible that those who responded had strong feelings about the subject, either in favor or against.
Maternal-fetal medicine subspecialists are most often the physicians who diagnose a fetal anomaly or pregnancy complication, and often participate in clinical decision-making during which termination of pregnancy is an option (12). There is evidence that women diagnosed with fetal anomalies prefer having the same provider throughout their pregnancy (13) and many women would likely value if their obstetrician could also provide their termination. As legal restrictions limiting access to abortions after 20 weeks of gestation increase, it may be even more important for women to have increased access to providers, since many anatomic anomalies are not diagnosed until 18-20 weeks of gestation. (14) MFM fellowships that provide D&E training and services may play a particularly important role in the South and Midwest, where almost one-half of all fellowships are located but where there are fewer abortion providers (1)
Much of the public rhetoric surrounding abortion focuses on decreasing the incidence of abortion by decreasing the number of unplanned pregnancies. However, this neglects the important role that abortion providers play in offering termination services to women carrying pregnancies complicated by congenital fetal anomalies, severe maternal disease, or inevitable pregnancy loss. Recognizing MFM fellows’ desire for training opportunities and incorporating both routine and informal D&E training into MFM fellowship could have a strong impact on expanding access to patient-centered care and reducing the impression of a divide between doctors who deliver babies and those who provide abortions.
CONDENSATION.
Maternal-fetal medicine fellows express a strong interest in dilation and evacuation training opportunities during their fellowship.
Acknowledgments
Funding for this work was provided by the University of California, San Francisco Clinical and Translational Science Institute Resident Research Grant.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The authors report no conflict of interest.
Portions of this work were presented in poster form at the North American Forum on Family Planning in Washington, DC, October 22-24, 2011 and at the Society of Maternal-Fetal Medicine 33rd Annual Meeting in San Francisco, CA, February 11-16, 2013
References
- 1.Jones RK, Kooistra K. Abortion incidence and access to services in the United States, 2008. Perspect Sex Reprod Health. 2011 Mar;43(1):41–50. doi: 10.1363/4304111. [DOI] [PubMed] [Google Scholar]
- 2.Pazol K, Zane SB, Parker WY, Hall LR, Berg C, Cook DA, et al. Abortion surveillance-- United States, 2008. MMWR Surveill Summ. 2011 Nov 25;60(15):1–41. [PubMed] [Google Scholar]
- 3.Eastwood KL, Kacmar JE, Steinauer J, Weitzen S, Boardman LA. Abortion training in United States obstetrics and gynecology residency programs. Obstet Gynecol. 2006 Aug;108(2):303–8. doi: 10.1097/01.AOG.0000224705.79818.c9. [DOI] [PubMed] [Google Scholar]
- 4.Drey EA, Foster DG, Jackson RA, Lee SJ, Cardenas LH, Darney PD. Risk factors associated with presenting for abortion in the second trimester. Obstet Gynecol. 2006 Jan;107(1):128–35. doi: 10.1097/01.AOG.0000189095.32382.d0. [DOI] [PubMed] [Google Scholar]
- 5.Rayburn WF, Klagholz JC, Elwell EC, Strunk AL. Maternal-fetal medicine workforce in the United States. Am J Perinatol. 2012 Oct;29(9):741–6. doi: 10.1055/s-0032-1316445. [DOI] [PubMed] [Google Scholar]
- 6.Kerns JL, Steinauer JE, Rosenstein MG, Turk JK, Caughey AB, D'Alton M. Maternal-fetal medicine subspecialists' provision of second-trimester termination services. Am J Perinatol. 2012 Oct;29(9):709–16. doi: 10.1055/s-0032-1314893. [DOI] [PubMed] [Google Scholar]
- 7.American Board of Obstetrics and Gynecology . Guide to learning in maternal-fetal medicine. American Board of Obstetrics and Gynecology; Dallas, TX: 2013. [Google Scholar]
- 8.Aiyer AN, Ruiz G, Steinman A, Ho GY. Influence of physician attitudes on willingness to perform abortion. Obstet Gynecol. 1999 Apr;93(4):576–80. doi: 10.1016/s0029-7844(98)00467-0. [DOI] [PubMed] [Google Scholar]
- 9.Maternal-fetal medicine fellowship directory [Internet] Society for Maternal-Fetal Medicine; Washington, DC: [June 1, 2012]. Available from: https://www.smfm.org/act_FellowshipDirectoryPage.cfm. [Google Scholar]
- 10. [June 1, 2012];Where are the fellowships located? [Internet].: Fellowship in Family Planning. Available from: http://www.familyplanningfellowship.org/fellowship-locations.
- 11.Steinauer J, Landy U, Filippone H, Laube D, Darney PD, Jackson RA. Predictors of abortion provision among practicing obstetrician-gynecologists: A national survey. Am J Obstet Gynecol. 2008 Jan;198(1):39.e1,39.e6. doi: 10.1016/j.ajog.2007.06.002. [DOI] [PubMed] [Google Scholar]
- 12.Ogunyemi D, Buskye S. Prenatal diagnosis of fetal anomalies in a regional tertiary center: The role of a maternal fetal medicine unit--a review of 6,877 deliveries. J Matern Fetal Med. 2000 Jul-Aug;9(4):219–23. doi: 10.1002/1520-6661(200007/08)9:4<219::AID-MFM6>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 13.Lalor JG, Devane D, Begley CM. Unexpected diagnosis of fetal abnormality: Women's encounters with caregivers. Birth. 2007 Mar;34(1):80–8. doi: 10.1111/j.1523-536X.2006.00148.x. [DOI] [PubMed] [Google Scholar]
- 14.McCarthy M. Abortion restrictions increase at state level in US. BMJ. 2013 Jan 7;346:f98. doi: 10.1136/bmj.f98. [DOI] [PubMed] [Google Scholar]