Abstract
Objective
Using data from the community-based Johnston County Osteoarthritis Project (JoCo OA), we examined race and gender variations in willingness to undergo, and perceptions regarding, total joint replacement (TJR).
Methods
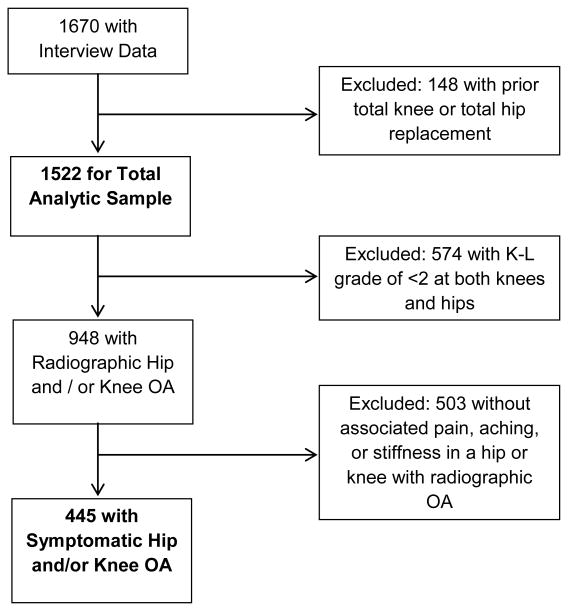
Analyses were conducted for the total sample who participated in a follow-up measurement period from 2006-2010 (n=1,522) and a subsample with symptomatic hip and / or knee osteoarthritis (sOA; n=445). Participants indicated how willing they would be to have TJR (hip or knee) if their doctor recommended it; responses were categorized as “definitely” or “probably” willing vs. “unsure,” “probably not” or “definitely not” willing, or “don't know.” Participants answered seven questions regarding perceptions of TJR outcomes. Multivariable logistic regression models of willingness included participant characteristics (including socioeconomic status) and TJR perception variables that were associated with willingness at the p<0.1 level in bivariate analyses.
Results
African Americans had lower odds of willingness to undergo TJR than Caucasians in the total sample (adjusted OR = 0.57, 95% CI = 0.44-0.74) and the sOA subsample (adjusted OR = 0.39, 95% CI = 0.25-0.62). There were no gender differences in willingness. African Americans expected poorer TJR outcomes than Caucasians, but gender differences were minimal; perceptions of TJR outcomes were not significantly associated with willingness.
Conclusions
In this community sample, racial differences in TJR willingness and perceptions were substantial, but gender differences were small. Perceptions of TJR did not appear to affect willingness or explain racial differences in willingness.
Introduction
Total joint replacement (TJR) surgery is an effective treatment option for end-stage hip and knee osteoarthritis (OA) (1, 2). These surgeries are among the most common elective procedures, and utilization rates are increasing (3). A number of studies have shown that African Americans undergo TJR at lower rates than Caucasians (4-9). These racial differences in use of TJR have not been attributed to clinical appropriateness (10, 11), nor do they seem to be driven primarily by provider referrals or communication about TJR (12, 13). Rather, prior studies report that African American patients expect poorer outcomes from TJR and are less willing to consider TJR if recommended (14-22). However, these studies have involved primarily clinic-based samples, and there is still a need to examine whether there are racial differences in willingness to undergo TJR among broader community-based samples that may vary more widely in care-seeking for OA, as well as health care options and experiences. There is also a need to examine whether racial differences in perceptions of TJR outcomes might explain any observed differences in willingness to consider TJR in these samples.
Similarly, there is evidence that women are less likely to undergo TJR than men (23), and when they do, they do so at later stages of disease and worse functional states (24-26). However, there has been relatively little research examining factors that may explain gender differences in the use of TJR (9). Although physicians report that patient gender makes no difference in whether they refer for or perform TJR (27, 28), one study showed that when performing blind evaluations of two standardized patients with moderate knee OA (one male, one female), physicians were more likely to recommend surgery for the male patient (29). Focus groups suggest women are less likely to choose TJR early in the disease process, expect poorer outcomes, have more concerns about recovery, are more willing to endure pain than risk surgery, and tend to avoid disruption of care giving roles (19, 30). Again, there is a need for broader community-based studies to examine whether there are gender differences in willingness to undergo TJR and whether differences in perceptions of specific TJR outcomes might explain any observed differences.
This study compared willingness to undergo TJR by race and gender among participants in the Johnston County Osteoarthritis Project (JoCo OA), as well as perceptions of TJR outcomes that might explain any differences observed. These analyses fill several gaps in our current understanding of TJR disparities. First, analysis of this community-based cohort expands generalizability of findings beyond the primarily clinic-based samples from prior studies in this area. Second, to our knowledge this is the first community-based study to evaluate factors that may be associated with gender differences in willingness to undergo TJR. Third, we examined racial differences in willingness to undergo TJR among men and women separately to assess whether there may be an interaction in the racial and gender differences in willingness that have been observed in prior studies. Fourth, we included both individual and community measures of socioeconomic status as covariates, which has not been done in prior studies.
Patients and Methods
This research was reviewed and approved by the Institutional Review Boards of the University of North Carolina, Chapel Hill and the Durham VA Medical Center.
Participants
This cross-sectional sample was composed of adults enrolled in JoCo OA, an ongoing community-based study of hip and knee OA in a rural, bi-racial population of North Carolina (NC), described in detail previously (31). Briefly, this study involved civilian, non-institutionalized adults aged 45 years and older who resided in six townships in Johnston County, NC. At baseline (1991-1997), participants were recruited with over-sampling of African Americans. A second wave of enrollment in 2003-2004 aimed to enrich the sample for African Americans and younger individuals. Participants from both waves of enrollment participated in another data collection period from 2006-2010; all data included in these analyses were from the 2006-2010 data collection period. For these analyses we excluded participants who had previously undergone TJR, based on self-report, resulting in a total analytic sample of n=1,522 (total sample, Figure 1). We also identified a sub-sample with symptomatic knee or hip OA (sOA subsample, n=445, Figure 1). Participants underwent posterior-anterior (PA) radiography of both knees with weight-bearing using a Synaflexer® positioning device. Supine A-P pelvis films were obtained women ≥ 50 years of age and all men. All radiographs were read for Kellgren-Lawrence (K-L) score by a single bone and joint radiologist (JBR) without regard to participant's clinical status. Intrarater reliability and interrater reliability, assessed with another trained radiologist, were both high (weighted kappas were 0.89 and 0.86, respectively) (31, 32). Radiographic knee and hip OA were defined as a K-L grade ≥2. To assess joint symptoms, participants were asked: “On most days, do you have pain, aching, or stiffness in your…right/left knee/hip.” Participants responding “yes” to this question for a joint with radiographic OA were considered to have symptomatic OA (n=445; Figure 1).
Figure 1. Johnston County Osteoarthritis Project Participants Included in Two Analytic Samples.
Willingness to Undergo and Perceptions of TJR
All participants were asked, “If your hip or knee pain were ever to get severe, how willing would you be to have surgery to replace your hip or knee if your doctor recommended it.” We compared those who were “definitely” and “probably” willing with those who were “unsure,” “probably not” willing, “definitely not” willing or did not know; this is the same categorization used recently by Vina et al (9). Because responses of “unsure” or “don't know” may differ from “probably not” or “definitely not” willing, we also performed sensitivity analyses in which we included only those who indicated “probably not” or “definitely not” and only those who indicated “unsure” or “don't know.” Results showed very similar patterns with respect to racial and gender differences in odds of willingness to undergo TJR. Therefore, for simplicity we present the results using the most inclusive definition of “not willing.” All participants were also asked seven questions about their perceptions of TJR, shown in tables. For multivariable analyses, we created meaningful categories of response options, based on the distributions of responses.
Participant Characteristics
In addition to participant race (African American vs. Caucasian) and gender, 13 other participant characteristics included in these analyses were age, education (< 12 vs. ≥ 12 years), marital status (married or living with partner vs. never married, divorced, separated, or widowed), employment status (currently employed vs. unemployed, retired, or disabled), health insurance type ( Government Insurance Only (Medicare / Medicaid, VA / CHAMPUS), Non-Government Insurance Only (Work / Union, Grange / Farmer's Bureau, Direct Purchase, Other Plan), Government + Non-Government Insurance, No Insurance), community poverty (percentage of households in a participant's block group that fell below the Census Bureau measure of poverty line (33, 34), self-rated health (excellent, very good, or good vs. fair or poor), body mass index (BMI, kg/m2), depressive symptoms (Center for Epidemiologic Studies Depression Scale (CES-D), defined continuously (35)), social support (Strong Ties Measure of Social Support (36)), duration of OA symptoms (i.e. number of years with pain, aching, and stiffness on most days in hip/knee), number of hip and knee joints with OA (KL ≥ 2), KL grade of the worst hip or knee, and Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) score of the worst hip or knee.
Analyses
All analyses were conducted for the total sample and sOA sub-sample. In addition, we conducted separate analyses for those with symptomatic hip OA and those with symptomatic knee OA. For each set of analyses, we first compared participants' responses to each TJR willingness and perceptions question according to race and gender. Next, we examined bivariate associations of willingness to undergo TJR (binary variable) with the seven TJR perception questions and 12 participant characteristics. Chi square and t-tests were used to examine associations with categorical and continuous variables, respectively. We then completed multivariable logistic regression models of willingness to undergo TJR, which included any TJR perception questions and participant characteristics that were associated with willingness at the p<0.1 level in bivariate analyses. Finally, we stratified the total sample and sOA sub-sample by gender and evaluated racial differences in TJR variables within those gender groups, using the same series of analyses described above. We included this analysis because many prior studies in this area involved samples of male veterans (14-16, 21), and we were interested in specifically assessing racial differences among the women in this sample. All analyses were completed using SAS version 9.1 software (SAS Institute, Cary, NC).
Results
Participant Characteristics
The total sample included 66.6% women and 31.1% African Americans, and the sOA subsample included 74.0% women and 33.5% African Americans (Table 1). As expected, the sOA subsample was slightly older, more often female, and had worse pain and radiographic findings than the total sample. All participant characteristics differed significantly between the two samples except race and duration of arthritis symptoms. There were also some gender and race differences in other demographic and clinical variables. In the total sample, women were less likely to be married (p<0.001) and less likely to be employed (p<0.004); women also had higher community poverty (p<0.01), shorter symptom duration (p=0.01), greater depressive symptoms (p<0.001), greater social support (p<0.001), and worse WOMAC scores (p<0.001). In the total sample, African Americans were less likely to have ≥12 years of education (p<0.001), less likely to be married (p<0.001), more likely to have no health insurance and only government health insurance (p<0.001), and less likely to have “excellent, very good, or good” self-reported health (p<0.01); African Americans also had higher KL grades (p<0.001), younger age (p<0.01), greater community poverty (p<0.001), higher BMI (p<0.001), and greater depressive symptoms (p<0.02). In the symptomatic OA sample, women were less likely to be married (p<0.001), had a higher BMI (p<0.001), and had shorter symptom duration (p=0.02). In the symptomatic OA sample, African Americans were less likely to have ≥12 years of education (p<0.01), less likely to be married (p<0.001), more likely to have no health insurance and only government health insurance (p<0.001), and less likely to have “excellent, very good, or good” self-reported health (p=0.03); African Americans also had higher KL grades (p<0.01), greater community poverty (p<0.001), higher BMI (p<0.001), and higher WOMAC scores (p=0.03).
Table 1. Characteristics of Study Samples.
| Characteristic | Total Sample (N=1522) | Symptomatic OA Subsample (N=445) |
|---|---|---|
| Demographic | ||
| Mean (SD) Age in years* | 68.1 (9.0) | 69.9 (9.0) |
| % Women* | 66.6 | 74.0 |
| % African American | 31.1 | 33.5 |
| % With ≥12 Years Education* | 78.4 | 69.1 |
| % Married or Living with Partner* | 59.5 | 52.4 |
| % Currently Employed* | 32.9 | 23.7 |
| Mean (SD) of % Poverty Households in block group* | 16.2 (10.2) | 18.0 (10.6) |
| Health Insurance Type (%*) | ||
| No Health Insurance | 5.2 | 4.3 |
| Government Only | 29.9 | 35.3 |
| Non-Government Only | 26.1 | 15.7 |
| Government + Non-Government | 38.7 | 44.7 |
| Health-Related | ||
| % With Excellent, Very Good, Good Self-Rated Health* | 76.4 | 61.4 |
| Mean (SD) BMI* † | 31.3 (7.2) | 33.8 (8.4) |
| Median (IQR‡) Depressive Symptoms (CES-D§)* | 4 (1-9) | 6 (2-12) |
| Median (IQR) Social Support* ‖ | 19 (16-20) | 18 (16-20) |
| OA Related | ||
| Median (IQR) WOMAC¶ Score of Worst Knee or Hip* | 7 (0-31) | 34 (17-50) |
| Mean Symptom Duration (SD) (Longest number years for knee or hip) | 10.6 (10.6) | 11.6 (11.3) |
| % Distribution of the Number of Knee / Hip Joints with KL ≥ 2 OA * | ||
| 0 | 36.5 | 0 |
| 1 | 21.6 | 21.8 |
| 2 | 27.3 | 47.6 |
| 3 | 8.1 | 16.0 |
| 4 | 6.5 | 14.6 |
| % Distribution of the KL Grade of Worst Knee or Hip Joint * | ||
| 0-1 | 36.5 | N/A |
| 2 | 34.6 | 36.6 |
| 3 | 14.1 | 25.2 |
| 4 | 14.8 | 38.2 |
Statistically significant difference (p<0.05) between Total Sample and Symptomatic OA Subsample; Chi-square for categorical variables, t-test to compare means of continuous variables, Wilcoxon-Mann-Whitney to compare medians of continuous variables.
BMI=kg/m2; BMI≥30 in kg/m2 defined as obese
IQR = Interquartile Range
CES-D range 0-60; higher scores indicate presence of more depressive symptoms
Strong Ties Measure of Social Support range 0-20; higher scores indicate more social support
WOMAC range 0-96; higher scores indicate worse pain/function
Results for the Total Sample
Willingness to Have TJR by Race and Gender
African Americans were less willing to have TJR than Caucasians (49.8% vs. 69.9% “probably” or “definitely” willing), and women were less willing than men (61.8% vs. 67.4%; Table 2a). In bivariate analyses, African Americans had significantly lower odds of being willing than Caucasians (49.8% vs. 69.9%; OR = 0.43, 95% CI = 0.34-0.53), and women had significantly lower odds than men (OR = 0.79, 95% CI = 0.63-0.98).
Table 2a. Willingness and Perceptions of Total Joint Replacement, by Gender and Race: Total Sample (n=1522).
| Women (N=1014) % | Men (N=508) % | African American (N=473) % | Caucasian (N=1049) % | |
|---|---|---|---|---|
| Willing to have TJR | ||||
| Definitely Not | 5.0 | 3.5 | 6.6 | 3.5† |
| Probably Not | 7.1 | 6.3 | 10.6 | 5.2 |
| Unsure | 21.1 | 17.5 | 25.6 | 17.3 |
| Probably | 33.6 | 33.9 | 29.0 | 35.8 |
| Definitely | 28.2 | 33.5 | 20.8 | 34.1 |
| Don't Know | 5.0 | 5.3 | 7.4 | 4.1 |
| Perceptions of TJR | ||||
| Have you ever heard of surgery to replace a hip or knee that has become damaged by arthritis? | ||||
| Yes | 94.7 | 93.1* | 92.4 | 95.0 |
| No | 5.3 | 6.1 | 7.4 | 4.8 |
| Don't Know | 0.0 | 0.8 | 0.2 | 0.3 |
| Do you have any family members or friends that have had a hip or knee replaced by surgery? | ||||
| Yes | 76.2 | 76.0 | 69.3 | 79.2† |
| No | 23.1 | 22.8 | 29.0 | 20.3 |
| Don't Know | 0.7 | 1.2 | 1.7 | 0.5 |
| Do you have a good understanding of what happens to somebody when they undergo hip or knee replacement surgery? | ||||
| Yes | 62.0 | 65.9 | 51.1 | 68.9† |
| No | 25.5 | 20.5 | 32.6 | 19.8 |
| Don't Know | 12.4 | 13.6 | 16.3 | 11.3 |
| How long do you think someone who has hip or knee replacement surgery would be in the hospital or other health care facility? | ||||
| 1-3 days | 9.8 | 12.2 | 5.1 | 13.1† |
| 4-7 days | 28.9 | 33.3 | 23.1 | 33.6 |
| 1-2 weeks | 17.7 | 17.9 | 18.9 | 17.3 |
| >2 weeks | 18.2 | 13.8 | 17.6 | 16.3 |
| Don't know | 25.4 | 22.8 | 35.4 | 19.7 |
| How long do you think it would take someone to fully recover from hip or knee replacement surgery? | ||||
| <2 weeks | 0.1 | 0.2 | 0.2 | 0.1† |
| 2 weeks-1 month | 1.1 | 3.0 | 3.0 | 1.1 |
| 1-2 months | 10.7 | 10.0 | 7.6 | 11.7 |
| 2-6 months | 33.7 | 35.2 | 25.6 | 38.0 |
| 6-12 months | 17.8 | 17.7 | 16.1 | 18.5 |
| > 12 months | 7.8 | 6.9 | 8.3 | 7.3 |
| Don't know | 28.9 | 27.0 | 39.2 | 23.4 |
| Sometimes people who have extreme pain in their hip or knee choose to have joint replacement surgery. How much pain do you think people will still have after they have recovered from their surgery? | ||||
| None | 12.4 | 12.3 | 7.9 | 14.4† |
| Mild | 37.4 | 42.7 | 29.4 | 43.5 |
| Moderate | 19.2 | 18.3 | 24.5 | 16.4 |
| Severe | 2.0 | 1.0 | 3.0 | 1.1 |
| Extreme | 0.4 | 0.2 | 0.9 | 0.1 |
| Don't know | 28.6 | 25.6 | 34.5 | 24.5 |
| Sometimes people who have extreme difficulty walking choose to have joint replacement surgery. How much difficulty walking do you think people will still have after they have recovered from their surgery? | ||||
| None | 15.1 | 16.5 | 10.0 | 18.0† |
| Mild | 38.4 | 41.1 | 31.1 | 43.0 |
| Moderate | 17.4 | 16.3 | 20.2 | 15.6 |
| Severe | 1.1 | 1.0 | 2.1 | 0.6 |
| Extreme | 0.5 | 0.4 | 0.9 | 0.3 |
| Don't know | 27.6 | 24.8 | 35.7 | 22.6 |
|
| ||||
| * Statistically significant different distributions (p<0.05) between women and men (across all response categories). †Statistically significant different distributions (p<0.05) between African Americans and Caucasians (across all response categories). Chi-squares when cells sizes reasonable; exact tests for variables with small sizes. Note: Missing data for one participant for pain still after TJR and two for difficulty walking after TJR | ||||
| Table 2b. Willingness and Perceptions of Total Joint Replacement, by Gender and Race: Symptomatic OA subsample (n=445) | ||||
|---|---|---|---|---|
|
| ||||
| Women (N=328) % | Men (N=117) % | African American (N=149) % | Caucasian (N=296) % | |
| Willing to have TJR | ||||
| Definitely Not | 8.5 | 6.0 | 10.7 | 6.4† |
| Probably Not | 8.5 | 12.0 | 16.1 | 6.1 |
| Unsure | 18.9 | 16.2 | 23.5 | 15.5 |
| Probably | 32.6 | 24.8 | 20.8 | 35.5 |
| Definitely | 26.8 | 33.3 | 20.1 | 32.8 |
| Don't Know | 4.6 | 7.7 | 8.7 | 3.7 |
| Perceptions of TJR | ||||
| Heard of TJR | ||||
| Yes | 95.7 | 92.3* | 92.6 | 96.0 |
| No | 4.3 | 6.0 | 6.7 | 3.7 |
| Don't Know | 0.0 | 1.7 | 0.7 | 0.3 |
| Friend / family member had TJR | ||||
| Yes | 79.0 | 77.8 | 77.8 | 79.1 |
| No | 20.7 | 19.7 | 20.1 | 20.6 |
| Don't Know | 0.30 | 2.6 | 2.0 | 0.3 |
| Good understanding of TJR | ||||
| Yes | 63.1 | 65.8 | 55.0 | 68.2† |
| No | 24.1 | 1830 | 28.2 | 19.6 |
| Don't Know | 12.8 | 16.2 | 16.8 | 12.2 |
| How long in hospital for TJR | ||||
| 1-3 days | 9.8 | 12.0 | 5.4 | 12.8† |
| 4-7 days | 29.3 | 32.5 | 26.2 | 32.1 |
| 1-2 weeks | 17.1 | 20.5 | 19.5 | 17.2 |
| >2 weeks | 18.0 | 13.7 | 19.5 | 15.5 |
| Don't know | 25.9 | 21.7 | 29.5 | 22.3 |
| How long to fully recover from TJR | ||||
| <2 weeks | 0.3 | 0.00 | 0.00 | 0.3† |
| 2 weeks-1 month | 2.1 | 2.6 | 4.7 | 1.0 |
| 1-2 months | 11.0 | 9.4 | 8.1 | 11.8 |
| 2-6 months | 33.8 | 29.9 | 22.8 | 37.8 |
| 6-12 months | 15.6 | 22.2 | 16.8 | 17.6 |
| > 12 months | 9.5 | 6.8 | 12.1 | 7.1 |
| Don't know | 27.7 | 29.1 | 35.6 | 24.3 |
| Pain after TJR recovery | ||||
| None | 11.3 | 6.9 | 10.1 | 10.2† |
| Mild | 35.4 | 44.0 | 30.2 | 41.4 |
| Moderate | 20.4 | 21.6 | 22.2 | 20.0 |
| Severe | 2.4 | 0.00 | 3.4 | 1.0 |
| Extreme | 0.9 | 0.00 | 2.0 | 0.00 |
| Don't know | 29.6 | 27.6 | 32.2 | 27.5 |
| Difficulty walking after TJR recovery | ||||
| None | 13.5 | 14.7 | 8.7 | 16.3† |
| Mild | 38.5 | 40.5 | 32.2 | 42.5 |
| Moderate | 17.7 | 18.1 | 22.8 | 15.3 |
| Severe | 1.2 | 2.6 | 3.4 | 0.7 |
| Extreme | 0.9 | 0.9 | 1.3 | 0.7 |
| Don't know | 28.1 | 23.3 | 31.5 | 24.5 |
Statistically significant difference (p<0.05) between women and men.
Statistically significant difference (p<0.05) between African Americans and Caucasians. Chi-squares when cells sizes reasonable; exact tests for variables with small sizes.
Note: Missing data for one participant for pain still after TJR and one for difficulty walking after TJR
Perceptions of TJR by Race and Gender
African Americans had poorer perceptions of TJR than Caucasians across all outcomes; only one item (“Have you heard..” of TJR) did not differ significantly by race (Table 2a). Higher proportions of African Americans than Caucasians reported “don't know” regarding expectations for many of the TJR outcomes. Women tended to perceive poorer outcomes from TJR outcomes than men, but only one item (“Have you heard..” of TJR) differed significantly by gender.
Models of TJR Willingness
All participant characteristics except social support were significantly associated with TJR willingness at the p<0.1 level and therefore included in the multivariable analysis. In the multivariable model (Table 3), African American participants still had lower odds of reporting willingness to undergo TJR than Caucasian participants (OR = 0.47, 95% CI = 0.31-0.72), but gender was not significantly associated with willingness.
Table 3. Multivariable Logistic Regression Models of Willingness to Undergo TJR, by 2 samples.
| Total Sample | sOA subsample | |||
|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | |
| Demographic Characteristics | ||||
| Older Age | 0.97 | 0.95-1.00 | N/A* | N/A |
| Women | 1.00 | 0.68-1.47 | N/A | N/A |
| African American | 0.47 | 0.31-0.72 | 0.42 | 0.25-0.69 |
| Education ≥ 12 years | 1.17 | 0.77-1.76 | 1.30 | 0.79-2.11 |
| Married or Living with Partner | 1.11 | 0.76-1.61 | 1.07 | 0.68-1.68 |
| Employed | 1.20 | 0.77-1.88 | N/A | N/A |
| Health Insurance | ||||
| No Health Insurance | 1.00 | 1.00 | ||
| Government Only | 1.43 | 0.63-3.23 | 1.07 | 0.42-2.70 |
| Non-Government Only | 0.91 | 0.39-2.10 | 0.88 | 0.32-2.45 |
| Government + Non-Government | 1.53 | 0.66-3.55 | 1.08 | 0.43-2.73 |
| Higher Community Poverty | 0.99 | 0.97-1.01 | 0.99 | 0.97-1.02 |
| Health Related Characteristics | ||||
| Excellent, Very Good, Good Self-Rated Health | 1.03 | 0.70-1.52 | 0.90 | 0.57-1.44 |
| Higher BMI | 0.99 | 0.97-1.01 | N/A | N/A |
| Higher CES-D | 1.00 | 0.97-1.02 | N/A | N/A |
| OA Related Characteristics | ||||
| Higher WOMAC Pain Score of Worst Knee or Hip | 1.04 | 0.97-1.11 | 1.03 | 0.95-1.12 |
| Higher WOMAC Function Score of Worst Knee or Hip | 0.99 | 0.97-1.01 | 0.97 | 0.95-1.00 |
| Longer Duration of Arthritis Symptoms | 0.99 | 0.68-1.01 | N/A | N/A |
| Greater Number of Knee / Hip Joints with KL ≥ 2 OA | 1.02 | 0.84-1.24 | N/A | N/A |
| Higher KL Grade of Worst Knee or Hip Joint | 0.92 | 0.75-1.13 | N/A | N/A |
| TJR Perceptions | ||||
| Heard of TJR | 1.27 | 0.57-2.85 | N/A | N/A |
| Family Member had TJR | 1.60 | 1.06-2.42 | N/A | N/A |
| Have a Good Understanding of TJR | 1.27 | 0.84-1.94 | 0.99 | 0.58-1.67 |
| Hospital Time | ||||
| 1-7 Days | 1.00 | 0.70-1.54 | 1.00 | |
| 1 week + | 1.04 | 0.55-1.99 | 0.95 | 0.58-1.55 |
| Don't Know | 1.04 | 1.03 | 0.48-2.22 | |
| Recovery Time | ||||
| < 2 months | 0.76 | 0.41-1.24 | 0.63 | 0.32-1.26 |
| 2-6 months | 1.00 | 1.00 | ||
| 6 + months | 0.75 | 0.49-1.17 | 0.78 | 0.45-1.35 |
| Don't Know | 0.95 | 0.51-1.79 | 0.97 | 0.45-2.08 |
| Pain Still after TJR | ||||
| None or Mild | 1.00 | 1.00 | ||
| Moderate to Extreme | 0.87 | 0.53-1.43 | 0.76 | 0.41-1.40 |
| Don't Know | 1.30 | 0.64-2.67 | 0.88 | 0.36-2.16 |
| Difficulty Walking Still after TJR | ||||
| None or Mild | 1.00 | 1.00 | ||
| Moderate to Extreme | 0.77 | 0.46-1.28 | 0.93 | 0.49-1.76 |
| Don't Know | 0.58 | 0.28-1.21 | 0.57 | 0.22-1.49 |
Not included in multivariable models because of lack of bivariate association p<0.1 with Willingness in this subsample.
Results for the sOA Subsample
Willingness to Have TJR by Race and Gender
African Americans were less willing to have TJR than Caucasians (40.9% vs. 73.3% “probably” or “definitely” willing), whereas willingness was similar for men and women (59.4% vs. 58.1%; Table 2b). In bivariate analyses, African Americans had significantly lower odds of being “probably” or “definitely” willing than Caucasians (OR = 0.32, 95% CI = 0.22-0.49), but women and men did not differ significantly in their odds (OR = 1.06, 95% CI = 0.69-1.62).
Perceptions of TJR by Race and Gender
Racial differences in expected TJR outcomes were statistically significant for all but two items (“Have you heard…” of TJR and “Do you have a family members or friends…” who have had TJR; Table 2b). African Americans expected worse outcomes than Caucasians and were more likely to report “don't know” for each of the outcomes. Gender differences in expected TJR outcomes in the sOA sample were less pronounced than in the total sample, and again only one item (“Have you heard..” of TJR) differed significantly by gender.
Models of TJR Willingness
Variables associated with TJR willingness in bivariate analyses of the sOA sample (p<0.1 level) are shown in Table 3. In the multivariable model (Table 3), African American participants still had lower odds of reporting willingness to undergo TJR than Caucasian participants (OR = 0.42, 95% CI = 0.25-0.69). Gender was not included in this model because it was not associated with willingness in the bivariate analysis. None of the TJR perception variables was significantly associated with willingness.
In the sample of participants with symptomatic hip OA (n=108; 25.9% African American, 74.1% women), African Americans were less likely to be willing to undergo TJR than Caucasians, but this difference was not statistically significant (OR = 0.44, 95% CI = 0.18-1.06); there was also no significant difference in willingness according to gender (OR = 1.86, 95% CI = 0.78-4.44). In the sample of participants with symptomatic knee OA (n=279; 37.6% African American, 74.2% women), African American participants were less likely to be willing to undergo TJR than Caucasians (OR = 0.25, 95% CI = 0.15-0.41), but there was no difference according to gender (OR = 0.81, 95% CI = 0.47-1.41). In the multivariable logistic regression model, African American race was still associated with lower odds of willingness to undergo TJR (OR = 0.5 95% CI = 0.22-0.54).
Gender Stratified Analyses of TJR Willingness and Perceptions
Total Sample
Among women in the total sample, 47.0% of African Americans and 69.2% of Caucasians reported being willing to have TJR (bivariate OR = 0.40, 95% CI = 0.30-0.52). In the multivariable model of TJR willingness, African American women remained less willing than Caucasian women (OR = 0.53, 95% CI = 0.35-0.79). Among men in the total sample, 56.6% of African Americans and 71.2% of Caucasians reported being willing to have TJR (bivariate OR = 0.53, 95% CI = 0.35-0.79). In the multivariable model of TJR willingness, there was a significant racial difference among men (OR = 0.42, 95% CI = 0.22-0.80).
sOA Sub-sample
Among women in the sOA subsample, 40.5% of African Americans and 69.8% of Caucasians reported being willing to have TJR (bivariate OR =0.30, 95% CI = 0.18-0.47). In the multivariable model of TJR willingness, African American women remained less likely to be willing than Caucasian women (OR = 0.41, 95% CI = 0.27-0.62). Among men in the sOA sub-sample, 42.4% of African Americans and 64.3% of Caucasians reported being willing to have TJR (bivariate OR = 0.41, 95% CI = 0.18-0.93). In the multivariable model of TJR willingness, there was a significant racial difference among men (OR = 0.42 95% CI = 0.19-0.97).
Discussion
In this community-based study we found important gender and racial differences in willingness to undergo TJR. In the total sample, women were less willing to undergo TJR than men. However, in the sOA subsample, for whom the question of TJR willingness is likely more salient, there was no gender difference. These results may reflect what seems to be an increase in the use of TJR among women with OA in the US (37). In contrast, in the sOA subsample, the racial difference in TJR willingness was more pronounced than in the total sample. These results follow several studies showing that African Americans with OA are less willing to consider or undergo TJR than whites (14, 16, 19).
We also observed gender and racial differences in perceptions of TJR outcomes, but the racial differences were more pronounced. Further, in the sOA subsample, gender differences were attenuated compared with the total sample, indicating some equalization among the group we would expect to have more information about TJR. However, substantial racial differences in TJR perceptions persisted in the sOA subsample, with African Americans expecting poorer outcomes. In addition, responses of “don't know” regarding TJR outcomes were more common among African Americans, even in the sOA subsample. These results concur with prior studies showing that African Americans with OA have less knowledge about TJR and expect poorer outcomes (15, 16, 18, 21).
In the multivariable model of TJR willingness in the total sample, African Americans still had lower odds of reporting willingness than whites (OR = 0.47), but there was no gender difference, and the TJR perception variables were generally not associated with willingness. In the multivariable model of TJR willingness in the sOA subsample, the racial difference also persisted and in fact was stronger than in the total sample; African Americans were less than half as likely as Caucasians to report willingness (OR = 0.42). Similar to the results for the total sample, none of the TJR perceptions variables was significantly associated with willingness in the multivariable model. These results differ from at least one other study that found TJR perceptions to mediate racial differences in willingness to undergo TJR among patients with moderate to severe hip or knee OA (16). The sample in that study differed substantially from this study, including elderly male patients at Department of Veterans Affairs outpatient clinics. It is unclear why TJR perceptions mediated willingness in that sample and not in the JoCo OA sample. Some research has shown that African Americans with OA are more likely to perceive prayer as helpful for treating arthritis, and this helps explain racial differences in consideration of TJR (14). Other research has shown that non-whites are more likely than whites to recognize barriers and risks to TJR (20, 21). Perceived efficacy of prayer and TJR risks were not assessed in this study, and these warrant further investigations of mediators of TJR willingness in community samples.
Racial differences in willingness to undergo TJR in this sample were somewhat more pronounced among women than men. In multivariable analyses, racial differences in willingness were only significant among women, both in the total sample and symptomatic OA sample. However, even among men, the odds of willingness were still somewhat lower among African Americans than Caucasians (OR=0.42). These results further emphasize the importance of exploring other factors that may help to explain racial differences in willingness to have TJR.
The racial difference in TJR willingness in the sOA subsample seemed to be largely explained by variation among patients with knee OA. Specifically, in an adjusted analysis there was no racial difference in TJR willingness among those with symptomatic hip OA, but among those with symptomatic knee OA, African Americans were only a third as likely to report willingness compared to Caucasians. Most other studies have jointly examined patients with hip and knee OA, and this study suggests that efforts to mitigate racial disparities in this area may be best targeted to patients with knee OA.
Strengths of this study include the large, community-based sample, ability to evaluate both racial and gender differences in TJR willingness and perceptions, and availability of information on key participant clinical and demographic characteristics that could affect these associations – particularly health insurance status and both individual and community measures of socioeconomic status. Although the community-based sample may enhance generalizability beyond a clinic-based sample, JoCo OA involves mostly rural participants over age 45, and this may limit generalizability to some other demographic groups. This study also did not include data on joint deformities, which, if severe, could affect patients' willingness to have TJR.
In summary, in a community-based sample there were substantial racial differences in perceptions of and willingness to undergo TJR, even after adjusting for important covariates. These results provide an important addition to prior studies that have involved clinic-based samples, in which results may not be as generalizable. Although some gender differences were also observed, they were smaller, particularly among the group with symptomatic OA. These findings support the need for continued efforts to reduce racial disparities particularly in knowledge about and perceptions of TJR. Patients' treatment choices are typically influenced by a host of beliefs and preferences, and the responsibility of the medical community is to support an informed decision. This includes providing patients with accurate, accessible information about treatment benefits and risks. In addition to fostering informed treatment choices, reducing racial disparities in TJR expectations is important because pre-surgical beliefs have been shown to influence post-surgical outcomes (38, 39). Work is still needed to determine the most effective methods and settings for delivering interventions to reduce racial disparities in this area.
Significance and Innovation.
In a community-based sample, African Americans were less willing to undergo total joint replacement (TJR) and perceived poorer outcomes than Caucasians; these results extend the generalizability of prior studies in clinic-based samples.
In contrast, there was no gender difference in willingness to undergo TJR, and perceptions of TJR outcomes were similar by gender.
These findings support the need for continued efforts to reduce racial disparities in knowledge about and perceptions of TJR.
Acknowledgments
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention or the Department of Veterans Affairs.
Grant Funding: Funding was made possible (in part) by: cooperative agreements S1734 and S3486 from the Centers for Disease Control and Prevention / Association of Schools of Public Health, the NIAMS Multipurpose Arthritis and Musculoskeletal Disease Center grant 5-P60-AR30701, the NIAMS Multidisciplinary Clinical Research Center grant 5 P60 AR49465-03, and an Arthritis Foundation Postdoctoral Fellowship Award (Golightly). Dr. Ibrahim is supported by a K24 Award (1K24AR055259-01) from the National Institutes of Musculoskeletal and Skin Disorders.
References
- 1.Callahan CM, Drake BG, Heck DA, Dittus RS. Patient outcomes following tricompartmental total knee replacement: A meta-analysis. JAMA. 1994;271(17):1349–57. [PubMed] [Google Scholar]
- 2.Chang RW, Pellisser JM, Hazen GB. A cost-effectiveness analysis of total hip arthroplasty for osteoarthritis of the hip. JAMA. 1996;275(11):858–65. [PubMed] [Google Scholar]
- 3.Singh JA. Epidemiology of knee and hip arthroplasty: a systematic review. Open Orthopaedics Journal. 2011;5:80–5. doi: 10.2174/1874325001105010080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Skinner J, Weinstein JN, Sporer SM, Wennberg JE. Racial, ethnic, and geographic disparities in rates of knee arthroplasty among Medicare patients. N Engl J Med. 2003;349(14):1350–9. doi: 10.1056/NEJMsa021569. [DOI] [PubMed] [Google Scholar]
- 5.Dunlop DD, Manheim LM, Song J, Sohn MW, Feinglass JM, Chang HJ, et al. Age and racial / ethnic disparities in arthritis-related hip and knee surgeries. Med Care. 2008;46(2):200–8. doi: 10.1097/MLR.0b013e31815cecd8. [DOI] [PubMed] [Google Scholar]
- 6.Hoaglund FT, Oishi CS, Gialamas GG. Extreme variations in racial rates of total hip arthroplasty for primary coxarthrosis: a population-based study in San Francisco. Ann Rheum Dis. 1995;54:107–10. doi: 10.1136/ard.54.2.107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention. Racial disparities in total knee replacement among Medicare enrollees--United States, 2000- 2006. MMWR - Morbidity & Mortality Weekly Report. 2009;58:133–8. [PubMed] [Google Scholar]
- 8.Mahomed NN, Barrett J, Katz JN, Baron JA, Wright J, Losina E. Epidemiology of total knee replacement in the United States Medicare population. J Bone Joint Surg Am. 2005;87(6):1222–8. doi: 10.2106/JBJS.D.02546. [DOI] [PubMed] [Google Scholar]
- 9.Vina ER, Cloonan YK, Ibrahim SA, Hannon MJ, Boudreau RM, Kwoh CK. Race, sex, and total knee replacement consideration: role of social support. Arthritis care & research. 2013;65(7):1103–11. doi: 10.1002/acr.21925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ang DC, Tahir N, Hanif H, Tong Y, Ibrahim SA. African Americans and whites are equally appropriate to be considered for total joint arthroplasty. J Rheumatol. 2009;36:1971–6. doi: 10.3899/jrheum.081214. [DOI] [PubMed] [Google Scholar]
- 11.Ang DC, James G, Stump TE. Clinical appropriateness and not race predicted referral for joint arthroplasty. Arthritis Care Res. 2009;61(12):1677–85. doi: 10.1002/art.24944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hausmann LR, Hanusa BH, Hresevic DM, Zickmund S, Ling BS, Gordon HS, et al. Orthopedic communication about osteoarthritis treatment: Does patient race matter? Arthritis Care Res. 2011;63(5):635–42. doi: 10.1002/acr.20429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hausmann LRM, Mor M, Hanusa BH, Zickmund S, Cohen PZ, Grant R, et al. The effect of patient race on total joint replacement recommendations and utilization in the orthopedic setting. J Gen Intern Med. 2010;25(9):982–8. doi: 10.1007/s11606-010-1399-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ang DC, Ibrahim SA, Burant CJ, Siminoff LA, Kwoh CK. Ethnic differences in the perception of prayer and consideration of joint arthroplasty. Med Care. 2002;40(6):471–6. doi: 10.1097/00005650-200206000-00004. [DOI] [PubMed] [Google Scholar]
- 15.Groeneveld PW, Kwoh CK, Mor MK, Appelt CJ, Geng M, Gutierrez JC, et al. Racial differences in expectations of joint replacement surgery outcomes. Arthritis Rheum. 2008;59(5):730–7. doi: 10.1002/art.23565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ibrahim SA, Siminoff LA, Burant CJ, Kwoh CK. Differences in expectations of outcome mediate African American/white patient differences in “willingness” to consider joint replacement. Arthritis Rheum. 2002;46(9):2429–35. doi: 10.1002/art.10494. [DOI] [PubMed] [Google Scholar]
- 17.Kroll TL, Richardson M, Sharf BF, Suarez-Almazor M. “Keep on truckin” or “It's got you in this little vacuum”: race-based perceptions in decision-making for total knee arthroplasty. J Rheumatol. 2007;34:1069–75. [PubMed] [Google Scholar]
- 18.Suarez-Almazor ME, Souchek J, Kelly PA, O'Malley K, Byrne M, Richardson M, et al. Ethnic variation in knee replacement: Patient preferences or uninformed disparity? Arch Intern Med. 2005;165:1117–24. doi: 10.1001/archinte.165.10.1117. [DOI] [PubMed] [Google Scholar]
- 19.Byrne MM, Souchek J, Richardson R, Suarez-Almazor M. Racial/ethnic differences in preference for total knee replacement surgery. J Clin Epidemiol. 2006;59:1078–86. doi: 10.1016/j.jclinepi.2006.01.010. [DOI] [PubMed] [Google Scholar]
- 20.Gandhi R, Razak F, Davey JR, Mahomed NN. Ethnicity and patient's perception of risk in joint replacement surgery. J Rheumatol. 2008;35:1664–7. [PubMed] [Google Scholar]
- 21.Ang DC, Monahan PO, Cronan TA. Understanding ethnic disparities in the use of total joint arthroplasty: application of the Health Belief Model. Arthritis Care Res. 2008;59(1):102–8. doi: 10.1002/art.23243. [DOI] [PubMed] [Google Scholar]
- 22.Blum MA, Ibrahim SA. Race/ethnicity and use of elective joint replacement in the management of end-stage knee/hip osteoarthritis: a review of the literature. Clin Geriatr Med. 2012;28(3):521–32. doi: 10.1016/j.cger.2012.05.002. [DOI] [PubMed] [Google Scholar]
- 23.Hawker GA, Wright JG, Coyte PC, Williams JI, Harvey B, Glazier R, et al. Differences between men and women in the rate of use of hip and knee arthroplasty. N Engl J Med. 2000;342(14):1016–22. doi: 10.1056/NEJM200004063421405. [DOI] [PubMed] [Google Scholar]
- 24.Parsley BS, Bertolusso R, Harrington M, Brekke A, Noble PC. Influence of gender on age of treatment with TKA and functional outcome. Clin Orthop Relat Res. 468(7):1759–64. doi: 10.1007/s11999-010-1348-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Katz JN, Wright EA, Guadagnoli E, Liang MH, Karlson EW, Cleary PD. Differences between men and women undergoing major orthopedic surgery for degenerative arthritis. Arthritis Rheum. 1994;37(5):687–94. doi: 10.1002/art.1780370512. [DOI] [PubMed] [Google Scholar]
- 26.Fortin P, Clarke A, Joseph L, Liang M, Tanzer M, Ferland D, et al. Outcomes of total hip and knee replacement: preoperative functional status predicts outcomes at six months after surgery. Arthritis Rheum. 1999;42(8):1722–278. doi: 10.1002/1529-0131(199908)42:8<1722::AID-ANR22>3.0.CO;2-R. [DOI] [PubMed] [Google Scholar]
- 27.Coyte PC, Hawker G, Croxford R, Attard C, Wright JG. Variation in rheumatologists' and family physicians' perceptions of the indications for and outcomes of knee replacement surgery. J Rheumatol. 1996;23(4):730–8. [PubMed] [Google Scholar]
- 28.Wright JG, Coyte PC, Hawker GA, Bomardier C, Cooke D, Heck D, et al. Variation in orthopedic surgeons' perceptions of the indications for and outcomes of knee replacement. Can Med Assoc J. 1995;152(5):687–97. [PMC free article] [PubMed] [Google Scholar]
- 29.Borkhoff CM, Hawker GA, Kreder HJ, Glazier RH, Mahomed NN, Wright JG. The effect of patients' sex on physicians' recommendations for total knee arthroplasty. CMAJ Canadian Medical Association Journal. 2008;178(6):681–7. doi: 10.1503/cmaj.071168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Karlson EW, Daltroy LH, Liang MH, Eaton HE, Katz JN. Gender differences in patient preferences may underlie differential utilization in elective surgery. Am J Med. 1997;102:524–30. doi: 10.1016/s0002-9343(97)00050-8. [DOI] [PubMed] [Google Scholar]
- 31.Jordan JM, Helmick CG, Renner JB, Luta G, Dragomir AD, Woodard J, et al. Prevalence of knee symptoms and radiographic and symptomatic knee osteoarthritis in African Americans and Caucasians: the Johnston County Osteoarthritis Project. J Rheumatol. 2007;31(4):172–80. [PubMed] [Google Scholar]
- 32.Jordan JM, Linder GF, Renner JB, Fryer JG. The impact of arthritis in rural populations. Arthritis Care Res. 1995;8:242–50. doi: 10.1002/art.1790080407. [DOI] [PubMed] [Google Scholar]
- 33.Diez Roux AV, Merkin SS, Arnett D, Chambless L, Massing M, Nieto FJ, et al. Neighborhood of residence and incidence of coronary heart disease. N Engl J Med. 2001;345(2):99–106. doi: 10.1056/NEJM200107123450205. [DOI] [PubMed] [Google Scholar]
- 34.Krieger N, Zierler S, Hogan JW, Waterman P, Chen J, Lelmieux K, et al. Geocoding and measurement of neighborhood socioeconomic position: a US perspective. In: Kawachi I, Berkman LF, editors. Neighborhoods and Health. New York: Oxford University Press; 2003. pp. 149–79. [Google Scholar]
- 35.Radloff LS. Th CES-D Scale: a self-report depression scale for research in the general population. Appl Psychol Measurement. 1977;1:385–401. [Google Scholar]
- 36.Dean AE, Lin N. The stress buffering role of social support. J Nerv Ment Dis. 1977;165:403–17. doi: 10.1097/00005053-197712000-00006. [DOI] [PubMed] [Google Scholar]
- 37.Wier LM, Pfunger A, Maeda J, Stranges E, Ryan K, Jagadish P, et al. HCUP Facts and Figures: Statistics on Hospital-based Care in the United States, 2009. Rockvill, MD: Agency for Healthcare Research and QUality; 2011. [PubMed] [Google Scholar]
- 38.Gandhi R, Davey JR, Mahomed N. Patient expectations predict greater pain relief with joint arthroplasty. J Arthroplasty. 2009;24(5):716–21. doi: 10.1016/j.arth.2008.05.016. [DOI] [PubMed] [Google Scholar]
- 39.Mahomed NN, Liang MH, Cook EF, Daltroy LH, Fortin PR, Fossel AH, et al. The importance of patient expectations in predicting functional outcomes after total joint arthroplasty. J Rheumatol. 2002;29(6):1273–9. [PubMed] [Google Scholar]