Abstract
Background
Adolescents and young adults (AYAs; aged 15–39 years) have inferior survival in comparison with younger (aged 0–14 years) cancer patients. Impact of care at specialized centers such as National Cancer Institute–designated Comprehensive Cancer Centers (NCICCC) for AYAs of all ages or the Children’s Oncology Group (COG) for AYAs aged 15 to 21 years with central nervous system (CNS) tumors remains unstudied.
Methods
We constructed a cohort of 560 children and 784 AYAs with CNS tumors reported to the Los Angeles cancer registry from 1998 to 2008. Cox and logistic regression models were used, with two-sided P values from Wald χ2 tests.
Results
In Cox regression analysis restricted to World Health Organization (WHO) grade II tumors, patients of all ages saw worse outcome if not treated at NCICCC/COG sites (non-NCICCC/COG vs NCICCC/COG: hazard ratio [HR] =1.73; 95% confidence interval [CI] = 1.09 to 2.72). Furthermore, the worse outcome for AYAs compared with children (HR = 1.90; 95% CI = 1.21 to 2.98; P = .005) was abrogated (HR = 1.35; 95% CI = 0.79 to 2.29; P = .27) by care at NCICCC/COGs. Those less likely to receive care at NCICCC/COG sites included young AYAs (aged 15–21 years vs children: odds ratio [OR] = 0.23; 95% CI = 0.11 to 0.48; P < .001) and older AYAs (aged 22–39 years) with low socioeconomic status (OR = 0.39; 95% CI = 0.17 to 0.89; P = .02), public/no insurance (OR = 0.30; 95% CI = 0.12 to 0.71; P < .01), and distance to care greater than 5 miles (OR = 0.29; 95% CI = 0.15 to 0.57; P < .001).
Conclusions
Population-based data reveal that care at NCICCC/COG sites mitigates inferior outcome in AYAs with WHO grade II CNS tumors compared with children. Compared with children, AYAs are less likely to receive care at NCICCC/COGs. Insurance, socioeconomic status, and distance serve as barriers to care at NCICCCs for older AYAs.
Cancer remains the leading cause of nonaccidental death in individuals aged 15 to 39 years (1,2), in part because these individuals have not benefited from the improvement in survival evidenced by the younger patients. Thus, although 5-year survival in children aged 14 years or younger improved over the past 25 years, survival rates improved minimally in those aged 15 to 24 years and not at all among those aged 25 to 34 years (3). Those aged 15 to 39 years constitute a vulnerable population and are therefore given special designation by the National Cancer Institute (NCI) as adolescents and young adults (AYAs), with a critical need to address the AYA gap (3,4).
Previous studies indicate better survival of AYA populations treated on pediatric therapeutic trials and at specialized centers (5–8), such as pediatric-centered facilities (9), with higher probability of enrollment on pediatric trials. However, AYAs (in particular, older AYAs) are more likely to receive care at adult community facilities (10) and, in this setting, are enrolled less often on therapeutic trials (11). NCI-designated Comprehensive Cancer Centers (NCICCC) are dedicated to developing effective approaches to prevent and treat cancer, meeting standards for breadth and depth in research while serving as models for translating discoveries from the bench to the bedside, including underserved populations (12). The impact of care at NCICCCs across the age range of the AYA population, including the older AYAs (aged 22–39 years), remains unstudied.
We tested the hypothesis that the AYA gap is, in part, due to disparities in access to quality cancer care experienced by AYAs. Thus, we aimed to study the impact of site of care for complex diseases with poor prognosis, such as central nervous system (CNS) tumors that require multidisciplinary, evidence-based care available at NCICCCs; we followed this by examining barriers to care at these centers in the AYA population.
Methods
The study included all patients newly diagnosed between 1998 and 2008 with primary CNS tumors at less than 40 years of age. Eligible patients resided in Los Angeles (LA) County and received care at facilities within LA County. We constructed a population-based cohort of children (aged 0–14 years at diagnosis) and AYAs (aged 15–39 years at diagnosis) using the LA County cancer registry (Cancer Surveillance Project; described in the Supplementary Materials, available online). This project was approved by the City of Hope institutional review board and the Committee for the Protection of Human Subjects of the State of California, both of which provided a waiver of informed consent.
Clinical Prognostic Variables
Clinical variables included age at diagnosis, year of diagnosis, sex, and primary diagnosis. Diagnoses were selected based on International Classification of Diseases for Oncology 3–based histology coding in the Cancer Surveillance Project using site codes consistent with brain or spinal cord locations. Using 2007 World Health Organization (WHO) guidelines, we assigned WHO grades to all patients (details provided in the Supplementary Materials, available online) (13–15).
Sociodemographic Predictors
A combined race/ethnicity variable yielded the following categories: non-Hispanic white, Hispanic, black, and Asian/Pacific Islander. Becauser of small numbers (n = 10) Alaskan Native/other patients and those with unknown/missing ethnicity were excluded. Payor was collapsed into three categories: public, private, and no insurance. Patients were excluded if insurance information was missing or unknown (n = 37). The socioeconomic status (SES) variable used 2000 Census block data, including education and median household income (16); Cancer Surveillance Project quintiles were consolidated into three levels (high, middle, low). Patients were excluded if SES was missing or unknown (n = 13).
Treatment Site
Treatment site was determined using the facility in which the patient was reported to have received all or part of their initial treatment. Patients were considered to have been treated at NCICCCs regardless of age if they were cared for at one of the three LA County NCICCCs (UCLA/Jonsson, Norris/Children’s Hospital Los Angeles, and City of Hope); of note, all three facilities are also Children’s Oncology Group (COG) member sites. Patients aged 21 years or younger were considered to have been treated at a COG site if they were treated at one of the three NCICCCs or at one of three additional sites with COG membership (Harbor/UCLA, Cedars-Sinai, Kaiser Permanente); patients treated at other sites were considered to have received care at a community site. Patients aged greater than 21 years not treated at an NCICCC were considered to have been treated at a community site.
Geography
Using Geographic Information Systems (ArcMap 10.1; esri, Redlands, CA), we measured straight-line distance between the residence and the nearest age-appropriate NCICCC/COG site (details provided in the Supplementary Materials, available online).
Statistical Analysis
Overall survival was calculated using Kaplan–Meier survival analysis, with log-rank tests used to detect differences between groups. Cox regression was used to model risk of mortality, determining hazard ratios (HRs) with associated 95% confidence intervals (CIs). The assumption of proportionality was verified through visualization of the Kaplan–Meier curves and inclusion of time-dependent variables; no violation was observed. Logistic regression was used to model the likelihood of receiving care at an NCICCC/COG site, determining odds ratios (ORs) with associated 95% CIs. Two-sided tests with P less than .05 were considered statistically significant. Analysis was performed using SAS 9.3 (SAS Institute, Cary, NC).
Results
Patients
Clinical and sociodemographic characteristics of the cohort are detailed in Table 1. The cohort included 560 children and 784 AYAs with newly diagnosed CNS tumors. Female patients comprised 43.0% of the cohort (n = 578); 36.2% (n = 486) of the cohort was non-Hispanic white, 47.5% (n = 638) was Hispanic, 9.4% (n = 127) was Asian/Pacific Islander, and 6.9% was black (n = 93). The majority of patients were privately insured (n = 832; 61.9%) and in either the high (n = 491; 36.5%) or low SES group (n = 590; 43.9%). Astrocytic/glial morphologies accounted for 60.3% (n = 810) of all tumors. There was an overrepresentation of WHO grade IV in children and WHO grade II in AYAs.
Table 1.
Sociodemographic and clinical characteristics of children and adolescents and young adults diagnosed with central nervous system tumors from 1998 to 2008 in Los Angeles County*
| Characteristics |
Entire cohort, aged 0–39 y
(n = 1344) |
Children, aged 0–14 y
(n = 560) |
Young AYAs, aged 15–21 y (n = 139) |
Older AYAs, aged 22–39 y
(n = 645) |
|||||
|---|---|---|---|---|---|---|---|---|---|
| No. (%) | No. (%) | No. (%) | No. (%) | ||||||
| Sex† | |||||||||
| Male | 766 (57.0) | 308 (55.0) | 82 (59.0) | 376 (58.3) | |||||
| Female | 578 (43.0) | 252 (45.0) | 57 (41.0) | 269 (41.7) | |||||
| Race/ethnicity‡ | |||||||||
| Non-Hispanic white | 486 (36.2) | 156 (27.9) | 40 (28.8) | 290 (44.9) | |||||
| Hispanic/Latino | 638 (47.5) | 313 (55.9) | 62 (44.6) | 263 (40.8) | |||||
| Black | 93 (6.9) | 43 (7.7) | 19 (13.6) | 31 (4.8) | |||||
| Asian/Pacific Islander | 127 (9.4) | 48 (8.5) | 18 (13.0) | 61 (9.5) | |||||
| Socioeconomic status‡ | |||||||||
| High | 491 (36.5) | 177 (31.6) | 43 (31.0) | 271 (42.0) | |||||
| Mid | 263 (19.6) | 111 (19.8) | 28 (20.1) | 124 (19.2) | |||||
| Low | 590 (43.9) | 272 (48.6) | 68 (48.9) | 250 (38.8) | |||||
| Insurance status‡ | |||||||||
| Private | 832 (61.9) | 326 (58.2) | 80 (57.5) | 426 (66.1) | |||||
| Public | 392 (29.2) | 226 (0.4) | 40 (28.8) | 126 (19.5) | |||||
| Uninsured | 120 (8.9) | 8 (1.4) | 19 (13.7) | 93 (14.4) | |||||
| WHO grade‡ | |||||||||
| I | 223 (16.6) | 157 (28.0) | 33 (23.7) | 33 (5.1) | |||||
| II | 507 (37.7) | 135 (24.1) | 49 (35.3) | 323 (50.1) | |||||
| III | 154 (11.5) | 57 (10.2) | 17 (12.2) | 80 (12.4) | |||||
| IV | 460 (34.2) | 211 (37.7) | 40 (28.8) | 209 (32.4) | |||||
| Morphology‡ | |||||||||
| Astrocytic/glial | 810 (60.3) | 214 (38.2) | 78 (56.1) | 518 (80.3) | |||||
| Embryonal | 205 (15.2) | 134 (23.9) | 19 (13.7) | 52 (8.1) | |||||
| Ependymal | 111 (8.3) | 59 (10.6) | 9 (6.5) | 43 (6.7) | |||||
| Generally cured with excision | 218 (16.2) | 153 (27.3) | 33 (23.7) | 32 (4.9) | |||||
| Distance to nearest National Cancer Institute–designated Comprehensive Cancer Center or Children’s Oncology Group site in miles§ | |||||||||
| WHO I–IV Median (IQR) Mean ± SD | |||||||||
| 7.56 (4.99–11.81) | 6.73 (4.21–9.62) | 7.08 (4.67–10.73) | 8.92 (5.69–13.80) | ||||||
| 9.52±7.37 | 8.18±6.68 | 9.20±7.85 | 10.75±7.62 | ||||||
| WHO II Median (IQR) Mean ± SD | |||||||||
| 8.11 (5.59–13.16) | 7.05 (4.56–9.31) | 7.79 (5.73–11.17) | 9.27 (5.80–14.33) | ||||||
| 10.08±7.35 | 8.27±6.94 | 10.03±8.47 | 10.84±7.22 | ||||||
* IQR = interquartile range; SD = standard deviation; WHO = World Health Organization.
† χ2 tests yielded two-sided P values that were non-statistically significant between age groups (P > .05).
‡ χ2 tests yielded two-sided P values that were statistically significant between age groups (P ≤ .001).
§ Analysis of variance yielded P values that were statistically significant between age groups (P ≤ .001).
Overall Survival by Age and Site of Care
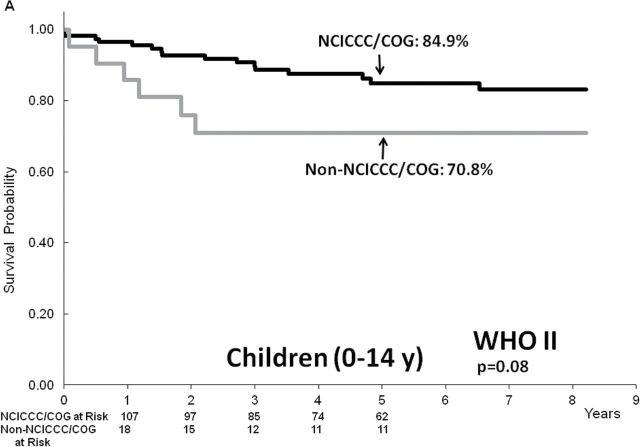
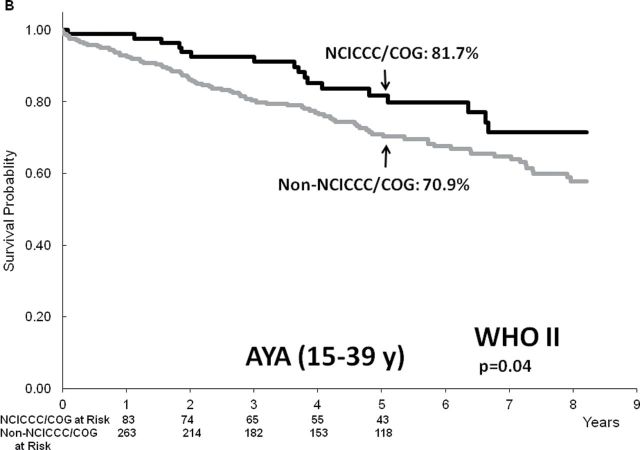
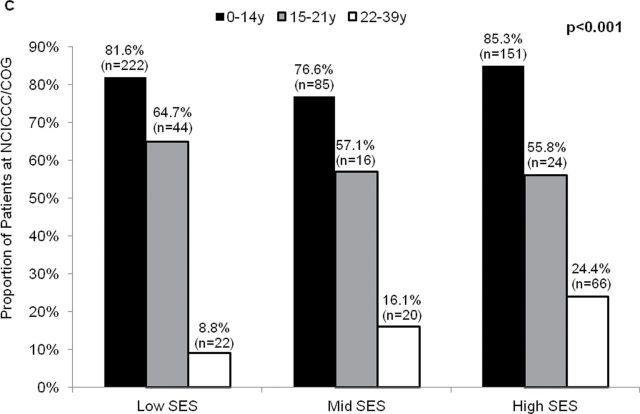
The 5-year overall survival varied by WHO grade (I: 94.0%, 95% CI = 90.6% to 97.1%; II: 76.0%, 95% CI = 71.9% to 80.1%; III: 40.6%, 95% CI = 32.0% to 49.2%; and IV: 43.1%, 95% CI = 38.3% to 47.9%; P < .001 for all comparisons between grades). We observed no difference in overall survival by age for WHO grade I (aged 0–14 years: 96.0%, 95% CI = 92.9% to 99.1%; aged 15 to 39 years: 89.0%, 95% CI = 80.5% to 97.5%; P = .15) or grades III or IV (aged 0–14 years: 42.7%, 95% CI = 36.4% to 49.0%; aged 15–39 years: 42.5%, 95% CI = 36.9% to 48.1%; P = .44) (Figure 1). However, among patients with WHO grade II tumors, 5-year overall survival was superior among those aged 0 to 14 years (82.7%; 95% CI = 75.9% to 89.5%) compared with those aged 15 to 39 years (73.4%; 95% CI = 68.4% to 78.4%; P = .006). With respect to site of care, no difference was observed in the overall survival for grade I (NCICCC/COG: 94.1%, 95% CI = 90.0% to 94.2%; community: 93.8%, 95% CI = 87.8% to 99.8%; P = .84) or grades III or IV tumors (NCICCC/COG: 45.0%, 95% CI = 39% to 51%; community: 40.4%, 95% CI = 34.6% to 46.2%; P = .65). On the other hand, among patients with grade II tumors, 5-year overall survival was superior among those treated at NCICCC/COG sites (83.5%; 95% CI = 77.8% to 89.2%) compared with those treated at community facilities (71.0%; 95% CI = 65.3% to 76.7%; P < .001). This differential persisted among children (NCICCC/COG: 84.9%, 95% CI = 77.7% to 92.1%; community: 70.8%, 95% CI = 51.1% to 90.5%; P = .08) and AYAs (NCICCC/COG: 81.7%, 95% CI = 72.5% to 90.9%; community: 70.9%, 95% CI = 65.0% to 76.8%; P = .04) with grade II tumors (Figure 2). In the setting of uniformly good outcomes in WHO grade I tumors and uniformly poor outcome in grades III and IV tumors (irrespective of age or site of care), subsequent analyses were restricted to patients with WHO grade II tumors.
Figure 1.
Overall survival by age and site of care according to World Health Organization (WHO) grade of central nervous system tumors diagnosed and treated in Los Angeles County. A–C) Comparison of survival between children (aged 0–14 years) and adolescents and young adults (AYA; aged 15–39 years) in groups with WHO grade I (A), WHO grade II (B), and WHO grades III and IV (C). D–F) Comparison of survival between patients cared for at National Cancer Institute–designated Comprehensive Cancer Centers or Children’s Oncology Group member sites (NCICCC/COG) with those cared for at community facilities in groups with WHO grade I (D), WHO grade II (E), and WHO grades III and IV (F).
Figure 2.
Overall survival by site of care in World Health Organization grade II patients cared for at National Cancer Institute–designated Comprehensive Cancer Centers or Children’s Oncology Group member sites (NCICCC/COG), as compared with those cared for at community facilities. A) Comparison within children aged 0 to 14 years. B) Comparison within adolescents and young adults aged 15 to 39 years.
Risk of Mortality in Patients With WHO Grade II Tumors
In univariable analysis, AYAs with WHO grade II CNS tumors had an increased risk of mortality compared with children (HR = 1.90; 95% CI = 1.21 to 2.98; P = .005) (Table 2). Addition of sex and sociodemographics to the model did not modify this association appreciably (HR = 1.97; 95% CI = 1.25 to 3.11; P = .004). However, by including site of care in the model, the association was mitigated (HR = 1.35; 95% CI = 0.79 to 2.29; P = .27). Furthermore, site of care had an effect on mortality, with patients at community facilities experiencing an increased risk of mortality compared with patients cared for at NCICCC/COG sites (HR = 1.73; 95% CI = 1.09 to 2.72; P = .02). In a multivariable model that included age, sex, race/ethnicity, SES, insurance, distance to care, and site of care, older age (AYA) was not associated with increased risk of mortality (AYA: HR = 1.41; 95% CI = 0.82 to 2.43; P = .21); also sociodemographics (race/ethnicity, SES, insurance) had no effect on mortality, whereas care at community facilities continued to have a negative impact (HR = 1.69; 95% CI = 1.09 to 2.68; P = .03).
Table 2.
Risk of mortality in World Health Orgnaization grade II central nervous system tumors in children and adolescents and young adults*
| Parameter | Model 1† | Model 2† | Model 3† | Model 4† | Model 5† | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| HR (95% CI) | P | HR (95% CI) | P | HR (95% CI) | P | HR (95% CI) | P | HR (95% CI) | P | |
| Age group, y | ||||||||||
| 0–14 | 1.00 (referent) | __ | 1.00 (referent) | __ | 1.00 (referent) | __ | 1.00 (referent) | __ | 1.00 (referent) | __ |
| 15–39 | 1.90 (1.21 to 2.98)‡ | .005‡ | 1.89 (1.20 to 2.96)‡ | .006‡ | 1.97 (1.25 to 3.11)‡ | .004‡ | 1.35 (0.79 to 2.29) | .27 | 1.41 (0.82 to 2.43) | .21 |
| Sex | ||||||||||
| Female | 1.00 (referent) | __ | 1.00 (referent) | __ | 1.00 (referent) | __ | 1.00 (referent) | __ | ||
| Male | 1.31 (0.92 to 1.87) | .14 | 1.31 (0.92 to 1.88) | .14 | 1.31 (0.92 to 1.88) | .13 | 1.32 (0.92 to 1.88) | .13 | ||
| Site of care | ||||||||||
| NCI-designated Comprehensive Cancer Center | 1.00 (referent) | __ | 1.00 (referent) | __ | ||||||
| Community facility | 1.73 (1.09 to 2.72)‡ | .02‡ | 1.69 (1.07 to 2.68)‡ | .03‡ | ||||||
| Race/ethnicity | ||||||||||
| Non-Hispanic white | 1.00 (referent) | __ | 1.00 (referent) | __ | ||||||
| Other | 0.99 (0.83 to 1.19) | .96 | 1.00 (referent) (0.67 to 1.50) | 1.00 | ||||||
| Socioeconomic status | ||||||||||
| High/mid | 1.00 (referent) | __ | 1.00 (referent) | __ | ||||||
| Low | 1.27 (0.85 to 1.90) | .25 | 1.25 (0.84 to 1.87) | .27 | ||||||
| Payor | ||||||||||
| Private | 1.00 (referent) | __ | 1.00 (referent) | __ | ||||||
| Public/no insurance | 1.10 (0.74 to 1.64) | .65 | 1.08 (0.73 to 1.60) | .71 | ||||||
* CI = confidence interval; HR = hazard ratio; NCI = National Cancer Institute.
† All models calculated using Cox proportional hazards regression analysis. Wald χ2 tests were used to calculate all two-sided P values.
‡ Values indicate statistical significance with P < .05.
Likelihood of Care at NCICCC
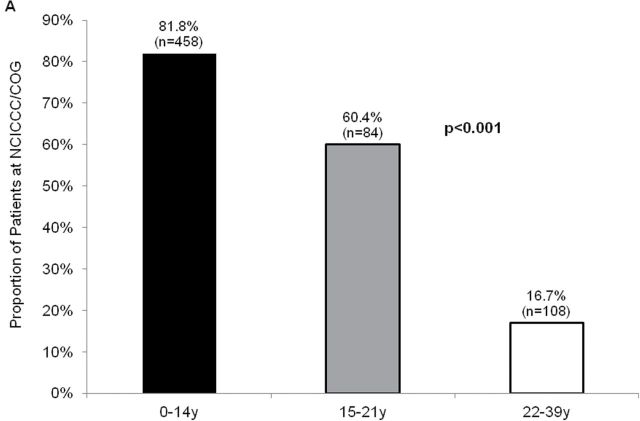
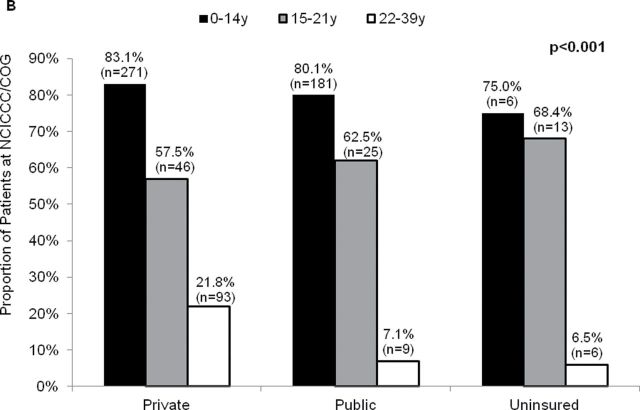
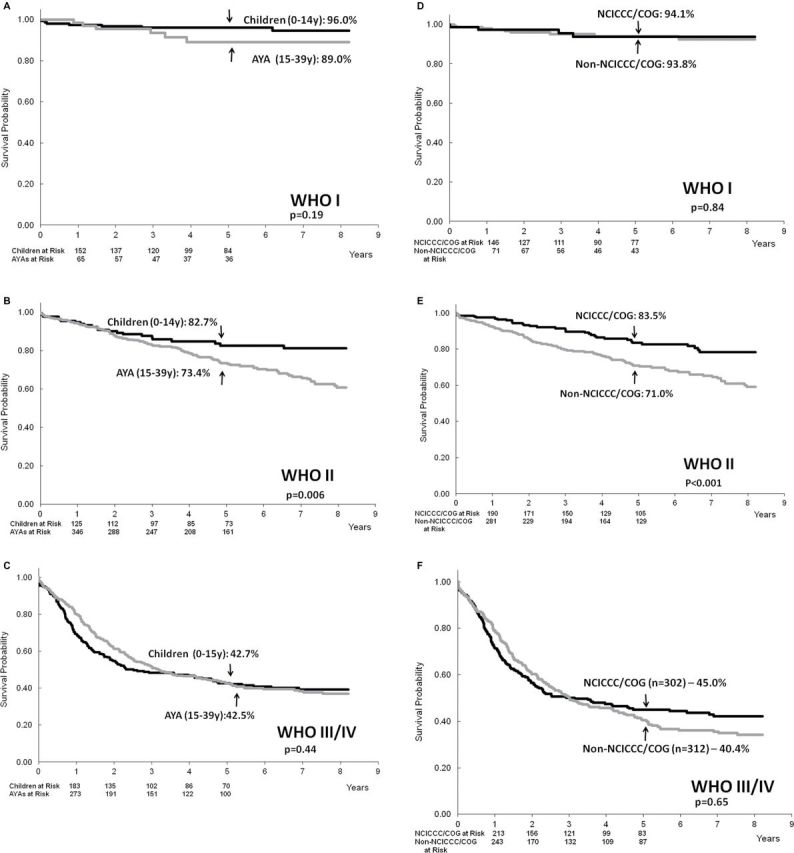
The proportion of patients receiving care at NCICCC/COG sites varied by age at diagnosis (aged 0–14 years: 81.8%; aged 15–21 years: 60.4%; aged 22–39 years: 16.7%; P < .001). This trend was observed regardless of SES, insurance status, and race/ethnicity (Figure 3).
Figure 3.
Proportion of children and adolescents and young adults (AYA) cared for at National Cancer Institute–designated Comprehensive Cancer Centers (NCICCC)/Children’s Oncology Group (COG) member sites. A) Proportion of patients cared for at NCICCC/COG member sites in each age group. B) Proportion of patients cared for at NCICCC/COG member sites according to insurance status by age group. C) Proportion of patients cared for at NCICCC/COG member sites according to socioeconomic status (SES) by age group.
Distance to care was measured using Geographic Information Systems. The prevalences of patients with CNS diagnoses by Census tract and all treatment sites are shown in Supplementary Figure 1 (available online). In WHO grade II disease, the median distance from a patient’s residence to the nearest NCICCC/COG site was 7.05 miles (interquartile range [IQR] = 4.56–9.31) among those aged 0 to 14 years, 7.79 miles (IQR = 5.73–11.17) among those aged 15–21 years, and 9.27 miles (IQR = 5.80–14.33) among those aged 22 to 39 years (P < .001) (Table 1).
Multivariable logistic regression analyses were stratified into two groups (aged 0–21 years and aged 22–39 years) to account for receipt of care at COG member sites that is unique to the younger age group (Table 3). Among patients aged 21 years and younger at diagnosis, those aged 15 to 21 years were less likely to receive care at an NCICCC/COG site (OR = 0.23; 95% CI = 0.11 to 0.48; P < .001) after adjusting for sociodemographic characteristics and distance to care. Furthermore, sociodemographics and distance were not associated with likelihood of care at NCICCC/COG sites. On the other hand, in the analysis restricted to those aged 22 to 39 years, patients with public or no insurance (OR = 0.30; 95% CI = 0.12 to 0.71; P = .006), patients in the low SES group (OR = 0.39; 95% CI = 0.17 to 0.89; P = .03), and patients who lived further than 5 miles from the nearest NCICCC (OR = 0.29; 95% CI = 0.15 to 0.57; P < .001) were less likely to use NCICCCs.
Table 3.
Likelihood of care at National Cancer Institute–designated Comprehensive Cancer Centers/ Children’s Oncology Group Sites in World Health Organization grade II central nervous system tumors in children and adolescents and young adults in Los Angeles County*
| Characteristics | Odds ratio (95% CI) † | P |
|---|---|---|
| Aged ≤21 y‡ | ||
| Age group | ||
| 0–14 y | 1.00 (referent) | __ |
| 15–21 y | 0.23 (0.11 to 0.48)§ | <.001§ |
| Race/ethnicity | ||
| Non-Hispanic white | 1.00 (referent) | __ |
| Other | 0.47 (0.18 to 1.25) | .13 |
| Socioeconomic status | ||
| High/mid | 1.00 (referent) | __ |
| Low | 1.36 (0.59 to 3.13) | .47 |
| Insurance | ||
| Private insurance | 1.00 (referent) | __ |
| Public/no insurance | 1.33 (0.57 to 3.09) | .51 |
| Distance from NCI-designated Comprehensive Cancer Centers/COG sites, miles | ||
| 0–5 | 1.00 (referent) | __ |
| >5 | 0.90 (0.38 to 2.09) | .80 |
| Aged 22–39 y‡ | ||
| Race/ethnicity | ||
| Non-Hispanic whites | 1.00 (referent) | __ |
| Others | 0.70 (0.36 to 1.36) | .29 |
| Socioeconomic status | ||
| High/mid | 1.00 (referent) | __ |
| Low | 0.39 (0.17 to 0.89)§ | .03§ |
| Insurance | ||
| Private insurance | 1.00 (referent) | __ |
| Public/no insurance | 0.30 (0.12 to 0.71)§ | .006§ |
| Distance from NCI-designated Comprehensive Cancer Centers, miles | ||
| 0–5 | 1.00 (referent) | __ |
| >5 | 0.29 (0.15 to 0.57)§ | <.001§ |
* CI = confidence Interval; COG = Children’s Oncology Group; NCI = National Cancer Institute.
† Odds Ratios were calculated using multivariable logistic regression analysis.
‡ Separate multivariable models were used for those aged 0 to 21 years and those aged 22 to 39 years. Wald χ2 tests were used to calculate all two-sided P values.
§ Values indicate clinical significance with P < .05.
Discussion
Our findings indicate that AYAs with WHO grade II CNS tumors in need of complex, evidence-based care face poor survival compared with children and that receiving care at an NCICCC or COG facility mitigates this difference. We also demonstrate barriers to receipt of care at NCICCC/COG sites for AYAs with this diagnosis in LA County, especially in the older age group.
AYAs have not seen the same improvement in survival evidenced by young children despite shared diagnoses, leaving an AYA gap (3,4). This is especially true for older AYAs (3,17). Evidence suggests that in children (5,6) and young AYAs (9), in general, survival is superior at COG sites with specialized services, including access to clinical trials; however the impact of care at NCICCCs had not been explored among older AYAs. We hypothesized that a noteworthy portion of the AYA gap is due to disparities in quality cancer care. Recent findings in Canadian and US patients with acute lymphoblastic leukemia are consistent with the notion that health-care access may play a role in the AYA gap in light of Canadian universal coverage; despite consistent improvement in survival in patients aged less than 18 in both countries, only Canadian aged 20 to 29 years saw improvement in survival through time, whereas US counterparts did not (17). Our study is the first to assess the impact of treatment at NCICCC/COG sites on survival in AYAs through the age of 39 years.
We find that a higher proportion of those aged 15 to 21 years (60.4%) were treated at NCICCC/COG sites than older AYAs (16.7%). This can possibly be explained by health-care structures that likely impact access for the younger population: 1) in California, adolescents are eligible for federally mandated insurance coverage for life-threatening illnesses until their 21st birthday, negating the impact that insurance status would have on a referral pattern; 2) in LA County, there are six NCICCCs and/or COG sites treating this age group, as compared with three for older AYA, despite smaller absolute and relative numbers of treating oncologists (pediatric vs medical). However, examination of access to care at NCICCC/COG sites among patients aged 15 to 21 years (compared with those aged 0–14 years) revealed that the only characteristic that decreased likelihood of care at NCICCC/COG sites was status as an AYA (aged 15–21 years). The role played by referral patterns is undeniable. Adolescents may not have regular primary care (18); if they do, they are often under the care of family practitioners or internists who refer to community surgeons or oncologists with whom they maintain a working relationship.
Only 16.7% of those aged 22 to 39 years were referred to NCICCCs in LA County. In this age group, SES, insurance status, and distance to care served as barriers to quality cancer care. It is conceivable that insurance plays a role in this disparity because this age group is more likely to be underinsured; previous reports indicate that 34% of all those aged 21 to 24 years and 31% of all those aged 18 to 24 years were uninsured in the early 2000s as compared to 13% of all those aged 12 to 17 years and 11% of all those aged 10 to 14 years during the same era (19). Insurance coverage options afforded by the Affordable Care Act have increased coverage in this population in the current era. Particularly among sick young adults, the ability to remain on parents’ policies has already increased coverage in this age group (20). Additionally, temporary Medicaid expansion and initiation of health-care exchanges will provide more affordable coverage for this underinsured population. SES likely impacts insurance options, but given that SES remained an independent predictor of use of an NCICCC, it may impact access through issues such as awareness/education and thus the ability to navigate the complex world of health care and advocate for appropriate services, placing low SES patients at a distinct disadvantage.
Unlike those aged 0 to 21 years, the distance that a patient aged 22 to 39 years must travel does play a role in whether or not that young adult obtains care at an NCICCC. We explored this question at a granular level using Geographic Information Systems techniques with institution-related data. Others found no impact of distance to the nearest pediatric cancer center (10) or academic medical center (21) but were limited by analysis using groups of counties rather than patient distance, zip code centroid rather than individual address, or inability to include adult centers. These findings are particularly salient in this group in which there is no appreciable difference between the distance that children and AYAs would need to travel to obtain care at NCICCC/COG sites. Nevertheless, the distance that a patient aged 22 to 39 years must travel plays a statistically significant role in where (s)he seeks care; this implies that more factors are at play in the travel distance, likely transportation. Younger patients are likely transported by parents/guardians, whereas older AYAs need to be more self-reliant. They may face limited access to cars, long trips on public transportation, and high travel costs, restricting their movements and thus access. Also, older AYAs have a greater average distance to NCICCCs as compared with younger AYAs. For the purposes of this discussion, the younger group has access to COG sites and NCICCC/COG sites, thus there are six facilities to which distance has been calculated; on the other hand, the older group only has access to NCICCCs, and thus distance has been calculated to three sites.
We explored patients with CNS tumors because their management requires complex, evidence-based care. Uniformly, there were good outcomes in WHO grade I patients and poor outcomes in WHO grades III and IV patients regardless of age or treatment site. We found statistically significant differences by both age and treatment site in patients with WHO grade II tumors. Diagnoses in the WHO grade II category likely required coordination of complex, multidisciplinary care and benefitted from the availability of services at NCICCC/COG sites.
Study limitations stem from the nature of registry data. Despite using a homogeneous diagnostic group to minimize prognostic differences, the absence of data on disease biology or lead time to diagnosis is limiting. Although a lack of treatment data cannot be completely overcome given the nature of registry data, we addressed this by including WHO grade in the analysis, with the assumption that patients within each grade received generally similar treatments. It is difficult to identify whether pediatric or adult services are caring for the patient; at COG member sites without NCICC designation for the adult service, it is ambiguous to which service an AYA aged 15 to 21 years would be assigned. To minimize bias in this situation, we assigned patients aged 21 years and younger to COG sites, whereas patients aged 22 years and older were considered to have received community care. For equanimity, we limited our cohort to patients living and receiving treatment within the borders of the LA County; an out-of-county NCICCC/COG site location may be closer to some patients in a border area of the county, but examination of the map indicates this is a small proportion of the cohort. The number of sites available to each age group likely contributes to the impact of distance to care as well. There are more NCICCC/COG sites when compared with adult NCICCC sites, but overall there are fewer pediatric sites and practitioners; thus children are more likely to have to travel regardless of what type of facility they use. Although the definition of care in our model was systematic, use of registry data limits the ability to account for the continuum of care that occurs over time and could possibly involve more than one site. Finally, designation as uninsured is heterogeneous and ranges from poor patients not eligible for Medicaid to AYAs with part-time school/employment or those who risk remaining uninsured simply in the spirit of invincibility.
In summary, AYAs with WHO grade II CNS tumors have increased mortality when compared with children. This difference is mitigated by receipt of care at an NCICCC/COG site. Barriers to care at NCICCC/COG sites for those aged 15 to 21 years in LA County with WHO grade II CNS tumors include age alone; sociodemographic factors do not contribute to their likelihood of receiving care at these centers. Barriers to care at NCICCC sites for those aged 22 to 39 years include SES, insurance status, and distance to care at an NCICCC. Future work focusing on targeted interventional strategies to mitigate the disparities in outcome in AYAs should incorporate exploration at the individual level of both barriers and facilitators to care. In addition, future work should track access to care in AYA oncology as health-care delivery evolves, given the major changes currently underway in insurance options that may impact access to care for AYAs.
Funding
This work was supported by the National Institutes of Health (K12 CA001727 to JAW) and the St. Baldrick’s Foundation (St. Baldrick’s Scholar Career Development Award to JAW). Research reported in this publication included work performed in the Survey Research Core supported by the National Cancer Institute of the National Institutes of Health under award number P30CA33572. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Supplementary Material
The study sponsors had no role in design of the study; the collection, analysis, and interpretation of the data; the writing of the manuscript; and the decision to submit the manuscript for publication.
Expert opinion in the categorization of CNS tumors was provided by Jana Portnow, MD, from the Department of Medical Oncology at City of Hope.
References
- 1. Horner M, Ries L, Krapcho M, et al. , (eds.). SEER Cancer Statistics Review, 1975–2006. Bethesda, MD: National Institutes of Health; http://seer.cancer.gov/csr/1975_2006/, based on November 2008 SEER data submission, posted to the SEER web site, 2009. [Google Scholar]
- 2. Newacheck PW, Park MJ, Brindis CD, et al. Trends in private and public health insurance for adolescents. JAMA. 2004;291(10):1231–1237. [DOI] [PubMed] [Google Scholar]
- 3. Bleyer A, Choi M, Fuller CD, et al. Relative lack of conditional survival improvement in young adults with cancer. Semin Oncol. 2009;36(5):460–467. [DOI] [PubMed] [Google Scholar]
- 4. Bleyer A, Budd T, Montello M. Adolescents and young adults with cancer: the scope of the problem and criticality of clinical trials. Cancer. 2006;107(7 Suppl):1645–1655. [DOI] [PubMed] [Google Scholar]
- 5. Kramer S, Meadows A, Pastore G, et al. Influence of place of treatment on diagnosis, treatment, and survival in three pediatric solid tumors. J Clin Oncol. 1984;2(8):917–923. [DOI] [PubMed] [Google Scholar]
- 6. Meadows AT, Kramer S, Hopson R, et al. Survival in childhood acute lymphocytic leukemia: effect of protocol and place of treatment. Cancer Invest. 1983;1(1):49–55. [DOI] [PubMed] [Google Scholar]
- 7. Pediatric Oncology Group. Progress against childhood cancer: the Pediatric Oncology Group experience. Pediatrics. 1992;89(4):597–600. [PubMed] [Google Scholar]
- 8. Wagner HP, Dingeldein-Bettler I, Berchthold W, et al. Childhood NHL in Switzerland: incidence and survival of 120 study and 42 non-study patients. Med Pediatr Oncol. 1995;24(5):281–286. [DOI] [PubMed] [Google Scholar]
- 9. Howell DL, Ward KC, Austin HD, et al. Access to pediatric cancer care by age, race, and diagnosis, and outcomes of cancer treatment in pediatric and adolescent patients in the state of Georgia. J Clin Oncol. 2007;25(29):4610–4615. [DOI] [PubMed] [Google Scholar]
- 10. Albritton KH, Wiggins CH, Nelson HE, et al. Site of oncologic specialty care for older adolescents in Utah. J Clin Oncol. 2007;25(29):4616–4621. [DOI] [PubMed] [Google Scholar]
- 11. Liu L, Krailo M, Reaman GH, et al. Childhood cancer patients’ access to cooperative group cancer programs: a population-based study. Cancer. 2003;97(5):1339–1345. [DOI] [PubMed] [Google Scholar]
- 12. National Cancer Institute. Cancer Centers http://cancercenters.cancer.gov/cancer_centers/index.html Accessed May 27, 2014.
- 13. Finlay J, Carroll W. Cancer in Children and Adolescents. Sudbury, MA: Jones and Bartlett Publishers; 2010. [Google Scholar]
- 14. Louis D, Ohgaki H, Wiestler OD, et al. The 2007 WHO classification of tumours of the central nervous system. Acta Neuropathol. 2007;114(2):97–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Mehta M, Vogelbaum MA, Chang S, et al. Principles & Practice of Oncology. 9th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2011. [Google Scholar]
- 16. Treadgold CL, Kuperberg A. Been there, done that, wrote the blog: the choices and challenges of supporting adolescents and young adults with cancer. J Clin Oncol. 2010;28(32):4842–4849. [DOI] [PubMed] [Google Scholar]
- 17. Pole JD, Darmawikarta D, Alibhai SMH, et al. Differential survival improvement for patients 20–29 years of age with acute lymphoblastic leukemia. Leukemia Res. 2013;37(10):1258–1264. [DOI] [PubMed] [Google Scholar]
- 18. Data Resource Center for Child & Adolescent Health. National Survey of Children’s Health 2011/2012. Data query from the Child and Adolescent Health Measurement Initiative http://www.childhealthdata.org Accessed May 27, 2014.
- 19. Fishman E. Aging out of coverage: young adults with special health needs. Health Aff (Millwood). 2001;20(6):254–266. [DOI] [PubMed] [Google Scholar]
- 20. Sommers BD, Buchmueller T, Decker SL, et al. The Affordable Care Act has led to significant gains in health insurance and access to care for young adults. Health Affairs. 2013;32(1):165–174. [DOI] [PubMed] [Google Scholar]
- 21. Yeager N, Hoshaw-Woodard S, Ruymann F, et al. Patterns of care among adolescents with malignancy in Ohio. J Pediatr Hematol Oncol. 2006;28(1):17–22. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.