Abstract
We use hierarchical cross-classified random-effects models to simultaneously measure age, period, and cohort patterns of mortality risk between 1986 and 2006 for non-Hispanic white and non-Hispanic black men and women with less than a high school education, a high school education, and more than a high school education. We examine all-cause mortality risk and mortality risk from heart disease, lung cancer, and unpreventable cancers. Findings reveal that temporal reductions in black and white men’s and women’s mortality rates were driven entirely by cohort changes in mortality. Findings also demonstrate that disparate cohort effects between education groups widened the education gap in all-cause mortality risk and mortality risk from heart disease and lung cancer across this time period. Educational disparities in mortality risk from unpreventable cancers, however, did not change. This research uncovers widening educational differences in adult mortality and demonstrates that a cohort perspective provides valuable insights for understanding recent temporal changes in U.S. mortality risk.
Keywords: mortality, age-period-cohort, disparities, trends, education
Early in the twentieth century, scientists and doctors made tremendous achievements to improve health and reduce early death in the United States. Across the latter half of the century, steady gains in longevity were made by reducing mortality risk of degenerative diseases for middle and older adult age groups (Crimmins 1981; Cutler et al. 2010; Yang 2008). Research largely attributes more recent mortality declines to temporal changes in a handful of specific causes of death, chiefly heart disease, lung cancer, and other cancers (Cooper et al. 2000; Guyer et al. 2000; Jemal et al. 2005). These achievements are to be celebrated, but our understanding of factors behind mortality reductions remains limited. One problem is that many studies of U.S. mortality employ a period perspective to understand and analyze trends. In these cases, age-specific mortality risk at one time period is compared to age-specific mortality risk in a past time period, with little attention given to the cohort composition of populations at the respective times. As a result of this approach, improvements in health outcomes and survival may be misattributed to health inputs during that period (Fogel 2005; Healthy People 2000, 2010, 2020; Meara, Richards, and Cutler 2008).
This article addresses this shortcoming by analyzing how age, period, and cohort effects on U.S. adult mortality risk between 1986 and 2006 vary by educational attainment. To do so, we first bring together three perspectives of mortality risk: Link and Phelan’s (1995) fundamental cause theory, the life course perspective (Ben-Shlomo and Kuh 2002; Montez and Hayward 2011), and Riley’s (1987) principle of cohort differences in aging. We frame recent changes in educational disparities of U.S. adult mortality using these perspectives, and we develop hypotheses regarding age-, period-, and cohort-based differences in the education-mortality relationship. We further hypothesize that educational disparities in mortality, and cohort trends in these disparities, are stronger for causes of death under greater degree of human control, such as heart disease and lung cancer. We suspect that cohort changes in the education-mortality relationship are stronger among U.S. non-Hispanic whites (henceforth “whites”) than among U.S. non-Hispanic blacks (henceforth “blacks”). We employ new data and methods to simultaneously examine how age, period, and cohort (APC) effects on recent U.S. adult mortality risk differ by educational attainment. We do this separately for black and white women and men, as well as for major underlying causes of death. Our findings overwhelmingly support the contention that educational disparities in adult mortality risk are growing larger across cohorts, and that growth in these disparities is more pronounced for whites than for blacks. We conclude by advocating for the use of a cohort perspective of mortality change over the more commonly used period perspective (Finch and Crimmins 2004; Fogel 2005; Riley 1987; Ryder 1965; Yang 2008).
THEORETICAL BACKGROUND AND HYPOTHESES
Educational Attainment and U.S. Adult Mortality Risk
The association between educational attainment and mortality has been widely studied in the social and health sciences. In the United States, the education-mortality relationship was first comprehensively documented with national-level data by Kitagawa and Hauser (1973). Their findings demonstrated that educational differences in mortality were evident, were much wider at younger than at older ages, and were somewhat larger among women than among men. Since then, many studies have documented the education-mortality association and attempted to explain how education affects mortality risk (for a recent review, see Hummer and Lariscy 2011). In general, research shows that individuals with relatively low levels of education have a significantly higher annual risk of mortality than do those with more education. While it is widely acknowledged that a sizable portion of the education-mortality association is mediated by economic resources, social-psychological resources and health behaviors are also important mediators of this relationship (Denney et al. 2010; Lynch 2006; Mirowsky and Ross 2003; Ross and Wu 1995). Scholars also argue that education directly affects mortality risk via the knowledge and effective use of available health technologies (Glied and Lleras-Muney 2008; Phelan, Link, and Theranifar 2010) and the enhancement of cognitive skills (Baker et al. 2011). Despite continued declines in both all-cause and cause-specific death rates, as well as aggregate increases in educational attainment, education disparities in U.S. mortality risk have widened across time (Lauderdale 2001; Meara et al. 2008; Montez et al. 2011; Pappas et al. 1993). Widening educational disparities in mortality indicates fundamental socioeconomic stratification of a treasured resource—life itself—that must be better understood if efforts to close such a disparity are to succeed.
The strength of the relationship between education and mortality implies that education is a fundamental social cause of health and mortality risk (Link 2008; Link and Phelan 1995, 1996, 2002; Phelan et al. 2004; Phelan et al. 2010). This is because education shapes individual-level “resources like knowledge, money, power, prestige, and social connections that strongly influence people’s ability to avoid risks and to minimize the consequences of disease once it occurs” (Link and Phelan 1996:472). Additionally, education influences the broad contexts in which individuals live and work, as well as the social networks individuals belong to. These social contexts can also shape risk factors (e.g., poor housing, hazardous workplaces, and second-hand smoke) and the knowledge and lifestyles individuals are exposed to (Phelan et al. 2010). A central tenet of fundamental cause theory is the staying power of education. That is, despite changes in our understanding of disease, health behaviors, and treatment of disease and disability, the association between education and mortality persists. The well-educated continue to be the most likely to have access to, and to take advantage of, new knowledge, practices, and technologies that are related to morbidity and mortality risk (Glied and Lleras-Muney 2008; Link 2008; Link and Phelan 1995; Phelan et al. 2004). This implies that educational differences in mortality risk might grow wider during periods of rapid development of health technologies, especially for causes of death associated with such technologies (Chang and Lauderdale 2009; Miech et al. 2011). In general, though, fundamental cause theory is largely silent with regard to the patterns by which the education-mortality association differs by age and may change across birth cohorts or time periods. Our article adds to this literature by detailing education’s effects on mortality risk during a period of rapid development of health technologies (Chang and Lauderdale 2009; Glied and Lleras-Muney 2008; Lucas et al. 2006), rising socioeconomic inequality (Campbell et al. 2005; Pettit and Ewert 2009), and decreasing mortality risk (Xu et al. 2010).
Educational Attainment and Mortality Risk: Age Differences
Before turning to period and cohort differences in the education-mortality association, we briefly consider age differences in this relationship. Continued debate surrounds the manner by which education’s effect on mortality changes with age. Some research has found that educational differences in mortality risk converge at the oldest adult ages, which supports an age-as-leveler perspective (Beckett 2000). Other scholars, however, argue that effects of education on health and mortality increase with age. Lynch (2003), for example, found that the effect of education on self-rated health strengthens with age, and that this pattern has intensified across cohorts (see also Lauderdale 2001; Mirowsky and Ross 2008; Willson, Shuey, and Elder 2007). Such findings support a cumulative advantage perspective.
Most existing literature omits cohort effects in age-related analyses of education and mortality. This is problematic because no single “life course” exists. Instead, each cohort experiences a distinct life course shaped by the confluence of age effects and each cohort’s unique experience of history (Riley 1973, 1978, 1987; Riley and Riley 1986; Ryder 1965). Indeed, Riley (1987), in advancing her principle of cohort differences in aging persuasively argues that people in different cohorts age in unique ways due to the disparate sociohistorical conditions in which their life courses unfold. It follows, then, that the way by which age conditions the education-mortality association may be changing across cohorts, and analyses that omit cohort effects in the examination of the education-mortality relationship are thus biased (Ben-Shlomo and Kuh 2002; Masters forthcoming). While not the main focus of our article, we hypothesize the following:
Hypothesis 1: Educational differences in U.S. adult mortality are characteristic of all age groups once period and cohort effects are accounted for.
Educational Attainment and Period-Based Trends in Adult Mortality Risk
The literature on U.S. mortality trends generally concludes that the effect of socioeconomic status, education included, was quite strong at the beginning of the twentieth century, but that the relationship weakened by the middle of the century as the population underwent the epidemiologic transition (Lynch 2003; Manton, Stallard, and Corder 1997; Warren and Hernandez 2007). This is evidenced by the fact that the leading emerging degenerative diseases in the mid-twentieth-century United States—heart disease, cancers, and other undiagnosed or at the time untreatable diseases—affected all socioeconomic subpopulations similarly. In fact, researchers found a positive association between education and coronary heart disease among U.S. men during the 1940s and 1950s, due in large part to high levels of smoking and meat consumption among high status men (Manton et al. 1997).
Only after gaining greater knowledge of risk factors, and the development of medical technologies to prevent and treat degenerative diseases progressed, did researchers begin to note a protective educational effect on U.S. mortality risk due to heart disease, stroke, and some cancers. Recognizing this, a host of studies in the late 1980s and early 1990s compared socioeconomic mortality differentials in the mid-1980s with those found by Kitagawa and Hauser (1973), who utilized data from 1960. The later analyses showed that educational differences in adult mortality widened between 1960 and the mid-1980s (Feldman et al. 1989; Pappas et al. 1993), particularly among men (Preston and Elo 1995).
More recent evidence suggests that the education-mortality relationship continued to widen during the 1990s and into the early 2000s. Cutler and colleagues (2010), for example, found that the education gap in mortality risk widened modestly for men but especially so for women during the 1990s (see also Jemal et al. 2008; Meara et al. 2008). Most recently, Montez and colleagues (2011) showed that the educational gap in adult mortality widened among U.S. adults age 45 to 84 years between 1986 and 2006, with both women and men at the highest educational levels exhibiting sharp mortality declines over this period, while women at the lowest educational level actually exhibited a mortality risk increase. In all, this research documents a continuation of the trend of widening educational differences in U.S. adult mortality that began at least as early as the mid-twentieth century, despite major policy initiatives designed to the contrary (e.g., Healthy People 2000, 2010, and 2020 [National Center for Health Statistics 2001, 2011; Department of Health and Human Services 2010]). Thus, in general, we expect to find the following:
Hypothesis 2: The educational gap in U.S. adult mortality risk widened between 1986 and 2006.
Educational Attainment and Cohort-Based Trends in Adult Mortality Risk
A major limitation of existing literature on U.S. mortality trends is its overwhelming adherence to a period perspective. This practice is puzzling because cohort perspectives have been central to sociological theories of social change for some time (Ryder 1965). Indeed, Smith (2008:289) states that sociologists are “mad for cohorts” and the role cohort replacement plays in driving social change. Yet, despite this tradition, a cohort perspective is largely absent from recent sociological and epidemiological analyses of U.S. mortality disparities. In most studies of mortality trends, as well as official reports of U.S. death statistics (Xu et al. 2010), population-level mortality is perceived to be, measured as, and presented as a period phenomenon.
There are very important reasons, though, to consider a cohort perspective of mortality change in addition to the more commonly measured period perspective. On empirical grounds, Yang (2008) used newly developed age-period-cohort (APC) methods to analyze U.S. vital statistics data from 1960 to 1999 and showed that temporal reductions in U.S. adult mortality rates across this time were almost exclusively attributable to cohort, not period, effects. Furthermore, research has found that race and sex gaps in life course trajectories of disability, depressive symptoms, and self-rated health in the U.S. population are significantly associated with cohort membership (Willson et al. 2007; Yang and Lee 2009). Scholars have also found significant cohort variation in socioeconomic disparities in health trajectories in the Chinese population (Chen, Yang, and Liu 2010).
On theoretical grounds, we point to the growing literature on life course effects on adult health and mortality risk. The idea that early-life conditions influence subsequent health and later-life mortality risk is not new, but life course studies of mortality risk have surged in recent years. Considered to be a “long arm of childhood” (Hayward and Gorman 2004), research shows that harsh conditions in early life have direct and indirect effects on adult self-rated health (Kestilä et al. 2006), morbidity (Blackwell, Hayward, and Crimmins 2001; Freedman et al. 2008; O’Rand and Hamil-Luker 2007), and mortality risk (Davey Smith et al. 1998; Hayward and Gorman 2004). In one set of studies, socioeconomic conditions during childhood (e.g., family size and parents’ education) are shown to influence susceptibility to childhood disease (Case and Paxson 2010) and significantly affect trajectories of socioeconomic attainment (Palloni 2006), which, in turn, affects adult mortality risk (Montez and Hayward 2011). In another set of studies, a poor uterine environment (Barker 2007), childhood malnourishment (Fogel 2005), and early bouts with infections and inflammation are shown to increase physical susceptibility to later-life disease and mortality by scarring vital organs (Crimmins and Finch 2006; Finch and Crimmins 2004), stunting growth (Case and Paxson 2010; Fogel 2004), and contributing to an immune risk phenotype (Gluckman et al. 2008; Simanek, Dowd, and Aiello 2008). Researchers continue to investigate the pathways by which childhood conditions affect later-life mortality, but evidence overwhelmingly suggests an association (for a recent review, see Montez and Hayward 2011).
Yet, the extent to which the association between early-life conditions and later-life mortality has changed across U.S. birth cohorts is unknown. Consistent with Riley’s (1987) principle of cohort differences in aging” researchers are recognizing the need to embed the life course in the sociohistorical contexts in which it unfolds (Ben-Shlomo and Kuh 2002; Masters forthcoming; Reither, Olshansky, and Yang 2011; Yang and Lee 2009). This suggests that the life course is, in fact, a cohort-specific phenomenon and can vary over time. Consistent with this, Finch and Crimmins (2004) propose that enduring effects of cohorts’ disparate exposures to early-life conditions produce distinct cohort morbidity phenotypes. Indeed, if cohorts vary in their exposures to early-life conditions then we should also expect cohort-specific variation in susceptibilities to later-life mortality risk. This perspective has profound implications for understanding and analyzing how the education-mortality association has changed over time in the United States. We illustrate this via the following four points.
First, early-life conditions have improved across U.S. birth cohorts. Early in the twentieth century, major efforts were undertaken to reduce infectious diseases (Centers for Disease Control 1999), improve nutrition (Fogel 2004; Manton et al. 1997), and expand public health services (Cutler and Miller 2005; Easterlin 1997). Mortality rates fell faster across the first third of the twentieth century than at any other time in U.S. history, and both maternal and childhood health dramatically improved (Case and Paxson 2010; Cutler and Miller 2005; Fogel 2004; Warren and Hernandez 2007). Living conditions changed in substantial ways too, as urbanization, compulsory schooling (Glied and Lleras-Muney 2008), reductions in fertility, and expansion of consumer goods reshaped families, increased household safety, and improved general standards of living (Easterlin 1997).1
As the prevalence and severity of harsh early-life conditions decreased across cohorts, as greater proportions of cohorts survived into adulthood, and as the leading causes of adult deaths changed over time, the relative degree to which early-life conditions shaped cohorts’ later-life mortality may have lessened (Crimmins and Finch 2006; Masters forthcoming; Montez and Hayward 2011; van den Berg et al. 2011). Thus, our second point is that, in absolute terms, the association between early-life conditions and later-life mortality has likely diminished across cohorts. This is not to argue that the individual-level strength of the association between early-life conditions and later-life mortality risk has waned. Rather, we are making the simple point that childhood conditions at the aggregate level are likely accounting for less variance in cohorts’ overall adult mortality levels. While certainly stemming from cohort improvements in early-life conditions, this also partly reflects disparate rates of cohort survival into adulthood. In fact, relative to women born between 1900 and 1904 , women born between 1960 and 1964 enjoyed 26.0 percent greater survival to age 25 years (Human Mortality Database 2011). Because childhood mortality accounted for a diminishing portion of overall mortality, and because early-life conditions improved across cohorts, the relative degree to which early-life conditions affected later-life mortality changed across cohorts.
Third, due to reductions in harsh infant and childhood conditions, mortality in adulthood accounts for a greater proportion of overall U.S. mortality, and the adult environment has grown relatively more important in shaping later-life mortality risk. Thus, on the one hand, personal behaviors such as exercise, diet, and cigarette smoking grew more important in shaping adult mortality risk (Rogers and Hackenberg 1987). On the other hand, knowledge of, access to, and use of preventative and curative health technologies such as physical examinations, statins, beta-blockers, chemotherapy, and corrective surgeries also grew increasingly important (Cutler et al. 2010).
Fourth, because the adult environment is growing relatively more important in shaping cohorts’ adult mortality risk, the role of resources used to navigate this environment, collect and understand health-related information, procure helpful technologies, and take advantage of new health-related ideas should be growing increasingly important as well. Consistent with fundamental cause theory, we argue that education is becoming an ever greater resource used to shape access to new health knowledge, beneficial technologies, and contexts that promote healthy behavior (Link 2008). Moreover, because the process of educational attainment and access to resources unfolds in a life course fashion, and differentially so across cohorts, education is becoming more strongly associated with U.S. adult mortality risk across cohorts. Thus, based on empirical and theoretical grounds, we hypothesize the following:
Hypothesis 3: The educational gap in U.S. adult mortality is widening across birth cohorts rather than across time periods.
Education and U.S. Adult Mortality Trends: Differences by Gender, Race, and Cause of Death
Because U.S. women and men experience significantly different adult mortality risk, we stratify all of our analyses by sex. Our hypotheses pertaining to age, period, and cohort differences in mortality equally apply to men and women, but gender differences in cohort patterns of educational attainment, lifestyle risk factors, and gender-stratified economic opportunities, among other factors, should be kept in mind. For instance, cohort differences in men’s and women’s smoking patterns will likely influence disparate patterns of heart disease and lung cancer mortality risk (Pampel 2003; Preston and Wang 2006).
U.S. health and mortality patterns also differ between blacks and whites in substantial and persistent ways (Hummer and Chinn 2011; Williams and Sternthal 2010). Differences in life expectancy between the U.S. white and black populations have modestly narrowed in recent years (Harper et al. 2007), but black-white gaps in chronic disease (Hayward et al. 2000) and mortality risk (Hummer and Chinn 2011) remain distressingly large. Evidence suggests that racial gaps in adult mortality reflect cumulative life course processes of health and socioeconomic disadvantages suffered by the black population (Hayward et al. 2000; Shuey and Willson 2008; Williams and Jackson 2005; Williams et al. 2010). Racial stratification of resources like educational attainment across the life course and across cohorts, combined with the persistent racial gap in U.S. health and mortality risk, suggests that cohort changes in the education-mortality relationship probably differ by race. On the one hand, black cohorts, on average, have endured higher prevalence and greater severity of early-life disadvantages than have white cohorts (see Figure S1 in the online supplement) (Hayward et al. 2000; Masters forthcoming). This implies that the extent to which adult mortality risk is influenced by the long arm of childhood may be greater among blacks than among whites (Hayward and Gorman 2004). Consequently, blacks’ ability to capitalize on education to improve adult health and reduce mortality risk may be hindered by persistent deleterious childhood effects. Indeed, research shows the relationship between educational attainment and U.S. adult mortality to be somewhat weaker among blacks than among whites (Zajacova and Hummer 2009). On the other hand, irrespective of education level, racial discrimination in employment, earnings, health care, housing, and other aspects of social life make the adult environment harsher for blacks (Colen 2011; Williams and Jackson 2005). Therefore, we hypothesize that education is growing increasingly important in shaping U.S. cohort mortality experiences, but we further hypothesize that race conditions this effect.
Hypothesis 4: Cohort changes in educational disparities in adult all-cause mortality are stronger in the white population than in the black population.
Finally, cohort changes in the education-mortality relationship should be strong for causes of death that are significantly associated with risk factors such as smoking (Link 2008; Preston and Wang 2006) or from diseases that are somewhat preventable or treatable with medical knowledge and technologies (Chang and Lauderdale 2009; Glied and Lleras-Muney 2008; Phelan et al. 2010). This is because educational attainment, as argued earlier, has become an increasingly important resource in shaping access to healthy lifestyles and health information and care. Consistent with this, we should see large and growing educational disparities across cohorts for causes of death such as heart disease and lung cancer; on the other hand, we should expect significantly smaller educational gradients in mortality from cancers that are less preventable or are difficult to treat. We therefore further test fundamental cause theory by analyzing age, period, and cohort patterns of adult mortality risk for heart disease, lung cancer, and unpreventable cancers between 1986 and 2006 (Phelan et al. 2004).2 Due to significantly smaller counts of cause-specific deaths among blacks, we test this cause-specific hypothesis only for the subsamples of white men and women.
Hypothesis 5: Educational differences in heart disease and lung cancer mortality are larger and widening across cohorts, more so than educational differences in mortality from unpreventable cancers.
DATA
We used data from 19 National Health Interview Surveys (NHIS), 1986 through 2004, linked to follow-up mortality information for each cross-section through December 31st, 2006 (NCHS 2010). This linked dataset was concatenated and made publicly available by the National Center for Health Statistics (NCHS) and the Integrated Health Interview Series (IHIS) project at the Minnesota Population Center (Ruggles 2011). The NHIS used a multistage probabilistic sampling design, and respondents of the NHIS were matched to the computerized mortality records of the National Death Index (NDI) using a 14-item identification scheme (NCHS 2010a). Respondents of the NHIS not eligible for matches to death records were dropped from the final sample. We used NCHS derived analytical weights to make results from this dataset representative of the noninstitutionalized white and black adult population. The resulting 1986 to 2006 National Health Interview Survey-Linked Mortality Files (NHIS-LMF) are a unique combination of repeated cross-sectional surveys coupled with longitudinal annual records of individual respondents’ survival status. These data have several advantages for studying trends in educational differences in mortality risk across cohorts and time. First, combining repeated cross-sections of the NHIS with individual-level longitudinal mortality histories allows us to employ methods that break the linear dependency of age, period, and cohort in our analyses of mortality (Yang 2006; Yang and Land 2006). Second, because links between the NHIS surveys and the NDI range from 1986 to 2006, there is sufficient overlap between age, period, and cohort to estimate stable and reliable effects of all three variables. Furthermore, unlike U.S. vital statistics data that rely on death certificate reports, NHIS respondents self-report their age, race, and educational attainment.
To ensure enough time for individuals to complete all measured levels of educational attainment, to focus on ages where mortality risk is high and death counts were most plentiful, and to limit the use of data where age is top coded, we restricted the NHIS-LMF to U.S.-born non-Hispanic black and white respondents age 25 to 84 years at time of survey who were 25 to 99 years of age during the follow-up period.3 Limiting the data in this way trimmed our starting analytic sample sizes to 368,356 white men; 407,371 white women; 54,236 black men; and 78,280 black women. After we calculated annual exposure times to death, the resulting person-period datasets consisted of 4,505,955 white men’s person-years; 5,103,764 white women’s person-years; 637,699 black men’s person-years; and 962,276 black women’s person-years.
We then collapsed these person-year samples into aggregated subsamples of age-period-cohort blocks.4 Birth cohort coding was composed of 16 five-year blocks ranging from 1900–1904 to 1975–1979. The coding for period was composed of five blocks ranging from 1986–1990 to 2003–2006; the earliest period block spans five years because it contains the fewest number of deaths, and the remaining four periods span four years each. Coding for age was in 15 five-year blocks ranging from 25 to 29 years up to 95 to 99 years. Each sex- and race-specific sample for all-cause mortality analyses was composed of 168 uniquely combined APC blocks. The cause-specific analyses were limited to person-periods ages 40 years and above and cohorts up through 1960 to 1964 because there were a limited number of cause-specific deaths among younger adults born in recent cohorts. Consequently, the sex-specific data for the cause of death analyses were each composed of 132 unique APC blocks.5 Table 1 presents descriptive statistics for individual-level data, person-period data, and sex- and race-specific APC blocks.
Table 1.
Descriptive Statistics of Non-Hispanic White and Black Men and Women, NHIS-LMF 1986 to 2004
| Men | Women | |||||||
|---|---|---|---|---|---|---|---|---|
|
|
||||||||
| Black | White | Black | White | |||||
|
|
||||||||
| Mean | sd | Mean | sd | Mean | sd | Mean | sd | |
| Person-Level Samplea | ||||||||
| Age | 46.49 | 14.9 | 47.88 | 15.2 | 46.66 | 15.3 | 49.06 | 16.0 |
| Year | 1994.26 | 5.4 | 1994.08 | 5.3 | 1994.17 | 5.4 | 1994.01 | 5.3 |
| Birth Year | 1947.77 | 15.8 | 1946.21 | 15.9 | 1947.51 | 16.1 | 1944.95 | 16.7 |
| % Less than High School | 29.52 | 45.6 | 15.50 | 36.2 | 28.15 | 45 | 15..15 | 35.9 |
| % High School Graduate | 37.86 | 48.5 | 35.13 | 47.7 | 37.12 | 48.3 | 39.79 | 49.0 |
| % Greater than High School |
32.61 | 46.9 | 49.37 | 50.0 | 34.73 | 47.6 | 45.05 | 49.8 |
| % Deceased | 19.98 | 40.0 | 16.64 | 37.2 | 14.93 | 35.6 | 14.34 | 35.1 |
| N | 54,236 | 368,356 | 78,280 | 407,371 | ||||
| Person-Period Sampleb | ||||||||
| Age | 49.70 | 13.2 | 52.21 | 15.0 | 50.82 | 13.0 | 54.00 | 15.8 |
| Year | 1999.46 | 4.9 | 1999.42 | 5.3 | 1999.54 | 4.5 | 1999.43 | 5.2 |
| Birth Year | 1949.76 | 13.4 | 1947.21 | 15.1 | 1948.72 | 13.2 | 1945.43 | 16.0 |
| % Less than High School | 26.43 | 41.5 | 14.29 | 35.8 | 26.16 | 38.5 | 14.39 | 35.4 |
| % High School Graduate | 39.09 | 45.9 | 35.56 | 49.0 | 38.02 | 42.5 | 40.61 | 49.5 |
| % Greater than High School | 34.48 | 44.7 | 50.15 | 51.2 | 35.82 | 42.0 | 45.00 | 50.1 |
| % Deceased | 1.48 | 11.3 | 1.29 | 11.6 | 1.09 | 9.08 | 1.10 | 10.5 |
| N | 637,699 | 4,505,955 | 962,276 | 5,103,764 | ||||
| 168 APC-Education Cellsc | ||||||||
| < High School Sample | ||||||||
| 5-Year Age Blockd | 6.09 | 3.1 | 6.44 | 3.3 | 6.38 | 3.3 | 7.19 | 3.4 |
| 4-Year Period Blocke | 2.49 | 1.3 | 2.48 | 1.3 | 2.53 | 1.3 | 2.47 | 1.3 |
| 5-Year Cohort Blockf | 8.82 | 3.2 | 8.47 | 3.4 | 8.57 | 3.3 | 7.70 | 3.4 |
| Cell Count Deceased | 61.59 | 58.6 | 219.19 | 243.1 | 67.13 | 70.1 | 242.25 | 284.4 |
| Cell Count N | 2132.30 | 1102.4 | 7505.02 | 3862.6 | 3025.10 | 1581.5 | 8357.18 | 4342.1 |
| High School Sample | ||||||||
| 5-Year Age Block | 4.02 | 2.6 | 4.92 | 2.9 | 4.39 | 2.7 | 5.59 | 3.1 |
| 4-Year Period Block | 2.73 | 1.2 | 2.67 | 1.3 | 2.71 | 1.2 | 2.64 | 1.3 |
| 5-Year Cohort Block | 11.10 | 2.5 | 10.14 | 2.9 | 10.71 | 2.7 | 9.46 | 3.1 |
| Cell Count Deceased | 32.00 | 27.6 | 184.64 | 202.2 | 33.64 | 30.7 | 211.84 | 280.9 |
| Cell Count N | 4329.34 | 2963.1 | 23492.76 | 16051.2 | 5919.2 | 3992.9 | 27194.0 | 16781.3 |
| > High School Sample | ||||||||
| 5-Year Age Block | 3.94 | 2.4 | 4.73 | 2.7 | 3.98 | 2.5 | 4.65 | 2.9 |
| 4-Year Period Block | 2.82 | 1.2 | 2.77 | 1.2 | 2.86 | 1.2 | 2.80 | 1.2 |
| 5-Year Cohort Block | 11.25 | 2.4 | 10.42 | 2.7 | 11.25 | 2.5 | 10.53 | 2.9 |
| Cell Count Deceased | 22.76 | 21.5 | 170.69 | 187.1 | 21.60 | 21.2 | 107.13 | 131.9 |
| Cell Count N | 3823.89 | 2687.0 | 35835.29 | 25354.7 | 5970.35 | 4287.7 | 36756.33 | 26942.9 |
Age 25 to 84 years at time of survey.
Age 25 to 99 years.
Age 25 to 99 years.
Ranges from 1 to 15.
Ranges from 1 to 5.
Ranges from 1 to 16.
We used three categories of educational attainment: less than high school (<HS), high school or equivalent (HS), and greater than high school (>HS). These categories each contained large numbers of individuals and a sufficient number of deaths across the age range of the study. Moreover, research shows these categories capture much of the differentiation in U.S. mortality risk by educational attainment (Montez, Hummer, and Hayward 2012). The educational composition of the U.S. population changed substantially across the twentieth century, with cohorts born early in the century being disproportionately composed of persons with less than a high school education. Conversely, cohorts born in the middle of the century experienced improved educational achievement, with the majority of cohorts born mid-century attaining a high school degree or higher. The aggregated change in educational attainment is thought to be a primary factor in the temporal decline of U.S. adult mortality (Baker et al. 2011; Lynch 2003; Yang 2008). Here, we stratified our analyses by educational attainment to allow for education-specific estimates of APC patterns of mortality. We tested educational differences in mortality by estimating and contrasting education-specific confidence intervals of age, period, and cohort effects on mortality.
ANALYTIC METHODS
We used hierarchical age-period-cohort (HAPC) models for repeated cross-sectional survey data for analyses of all-cause white men’s and women’s adult mortality rates (Yang and Land 2006, 2008). For cause-specific analyses and for black men’s and women’s mortality, we estimated Hierarchical Bayesian Models using Gibbs sampling (Gelman 2006; Gelman et al. 2004; Lynch 2007; Yang 2006). Both of these methods utilize a cross-classified random-effects model (CCREM) to embed each person-year observation within a shared time period and birth cohort at their given five-year age group. Goodness-of-fit statistics (see Table S1 in the online supplement) from fixed-effects models of APC analyses generally verify that all three effects should be included in the models for all race-sex subsamples. However, the more conservative BIC criterion, which penalizes models for numbers of parameters and sample size, indicates that period effects do not substantively improve model fit for black men and women.
Because the NHIS-LMF 1986 to 2006 data follow individual survival status as each respondent ages across periods, respondents can occupy several APC combinations. Also, each five-year age block is composed of multiple combinations of time periods and birth cohorts. Thus, while collinearity between the age, period, and cohort effects is high, these data do not suffer the identification problem induced by an absolute linear dependency between the three effects (Glenn 2005; Mason et al. 1973). The HAPC-CCREM modeling is an appropriate APC methodological tool, and research shows it is more efficient than a fixed-effects approach when data, such as the NHIS-LMF, are unbalanced (Yang and Land 2008).
The HAPC-CCREM estimates fixed effects of the five-year age groups, and random effects of the four-year period and five-year cohort groups as follows: Level-1 within-cell model:
| (1) |
where Dijk is the number of deaths occurring in the ith age group within the jth period and the kth cohort. Aijkl denotes a set of dummy variables corresponding to the five-year age groups, with fixed effects βl ; αjk is a random intercept indicating the log mortality rate in the reference age group (65 to 69 years) in period j and belonging to cohort k; and log(Rijk) is the natural log of the aggregated exposure time lived during each age-period-cohort cell.
Level-2 between-cell random intercept model:
| (2) |
in which αjk specifies that the fixed age effects vary from period to period and from cohort to cohort; π0 is the log mortality rate at the reference age (65 to 69 years) averaged over all periods and cohorts; t0j is the overall four-year period effect averaged over all five-year birth cohorts with variance σ2t0; and c0k is the overall five-year cohort effect averaged over all four-year periods with variance σ2c0.
We combined the level-1 and level-2 models to estimate the expected log mortality rate in each APC cell assuming that deaths follow a Poisson distribution. To produce results in the form of APC-specific log mortality rates, we offset the aggregated exposure time lived within the cells. Tests of significance of the models’ variance components used the criteria advanced by Yang, Frenk, and Land (2009). Data for black men and women and subsamples of specific causes of death contained small counts of death in some APC cells and required more robust modeling techniques, in which case we estimated Hierarchical Bayesian Models using Gibbs sampling (see Yang [2006] for a comparison of HAPC-CCREM and Hierarchical Bayesian Models). We assumed noninformative prior distributions for all model parameters (Gelman 2006; Lynch 2007). Models were robust to alternate prior distributions.6
RESULTS
Figure S2 in the online supplement presents graphed estimates of fixed-effects age coefficients and random-effects period and cohort coefficients from analyses of all-education/all-cause mortality rates of U.S. adult white and black men and women between 1986 and 2006. Figure S3 in the online supplement presents graphed estimates of APC patterns of white men’s and women’s mortality rates from heart disease, lung cancer, and unpreventable cancers. We first discuss estimates in Figures S2 and S3 to introduce the general APC patterns of U.S. adult mortality risk between 1986 and 2006. We then proceed to test our five hypotheses focusing on education-mortality trends.
Trends in All-Education/All-Cause and All-Education/Cause-Specific Mortality
Patterns of results from our HAPC-CCREM analyses of all-cause adult mortality rates between 1986 and 2006 for white and black men and women are consistent with findings from Yang (2008), who used vital statistics data for 1960 to 1999. As presented online in Figures S2 and S3, age effects on mortality follow the usual log-linear pattern, with slight tapering at the oldest-old age groups (85+). This is the case for all sex-race subsamples for all-cause mortality and also for most causes of death, with the exception of lung cancer mortality. The distinct age pattern of lung-cancer mortality risk has age effects rising much more steeply than other specific causes of death, but these taper off around age 65 and plateau thereafter.
Also consistent with Yang (2008), our HAPC-CCREM estimates of all-cause and cause-specific mortality suggest that temporal changes in U.S. mortality risk across 1986 and 2006 were largely driven by cohort reductions in mortality rates. We find little variation in estimated period effects of mortality, irrespective of race, sex, or cause of death, although we do find a slight increase in white men’s and women’s all-cause mortality across periods. Conversely, estimates of cohort effects illustrate significant and persistent cohort declines in men’s and women’s all-cause mortality rates and mortality rates from heart disease. Consistent with previous findings, cohort patterns of lung cancer mortality closely follow cohort patterns of adult smoking (Wang and Preston 2009). Finally, no cohort variation is visible for unpreventable cancers. These descriptive results support the idea that cohort processes drove temporal reductions in U.S. mortality risk between 1986 and 2006. At the same time, note that cohort reductions in black men’s and women’s mortality between 1986 and 2006 were less steep than cohort reductions in white men’s and women’s mortality. We now turn to our core examination of how age, period, and cohort patterns differ by educational attainment.
Educational Differences in Trends in U.S. Men’s and Women’s All-Cause Mortality Risk
Tables S2, S3, S4, and S5 in the online supplement present estimates of fixed-effects age coefficients and random-effects period and cohort coefficients from education-stratified HAPC-CCREM and Hierarchical Bayesian analyses of 1986 to 2006 all-cause adult mortality for black and white men, and black and white women, respectively. Taken together, the education-stratified models reveal tremendous educational variation in the size of age and cohort effects, but very little variation in period effects. Our subsequent discussion of these models relies on the graphed results in Figures 1 through 5.
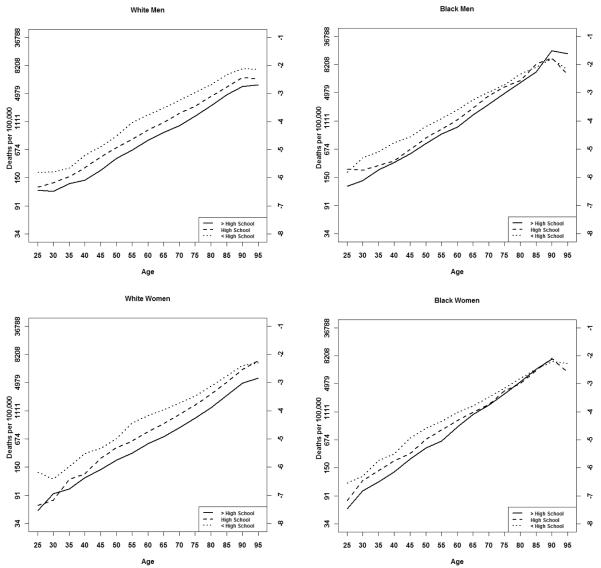
Figure 1.
Educational Differences in HAPC-CCREM Estimated Mortality Rates across Age, Black and White Men and Women, NHIS-LMF 1986 to 2004
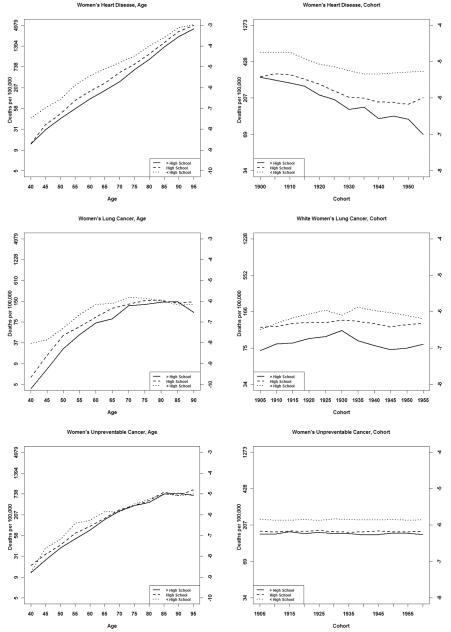
Figure 4.
Educational Differences in HAPC-CCREM Estimated Mortality Rates from Specific Causes of Death across Age and Cohort, White Women, NHIS-LMF 1986 to 2004
To test our first hypothesis, we present estimated age effects of men’s and women’s all-cause mortality rates, stratified by educational attainment, in Figure 1. For white men and women, the educational gap in age-specific mortality rates is preserved across all ages. That is, the difference in mortality between the <HS education group and the >HS education group is significant at all age-groups except 95 to 99 years, at which point large standard errors make the differences between the log mortality rates not significant. At no age group, however, do the point-estimates of all-cause logged mortality rates for the <HS population converge with the point-estimates of all-cause logged mortality rates for the >HS population. This evidence supports our first hypothesis. For black men and women, however, the educational gap in age-specific mortality is not significant in older adulthood. The estimated age effects of <HS all-cause mortality converge with the estimated age effects of >HS all-cause mortality for black men and black women; this evidence does not support our first hypothesis. These mixed results suggest the possible need for the age-as-leveler and cumulative disadvantage theories to incorporate race differences in the way education affects mortality risk across age. Indeed, race differences in educational returns, mortality selection, and life course processes of health and mortality can all affect how the education-mortality association changes with age (Hayward et al. 2000; Lynch, Brown, and Harmsen 2003).
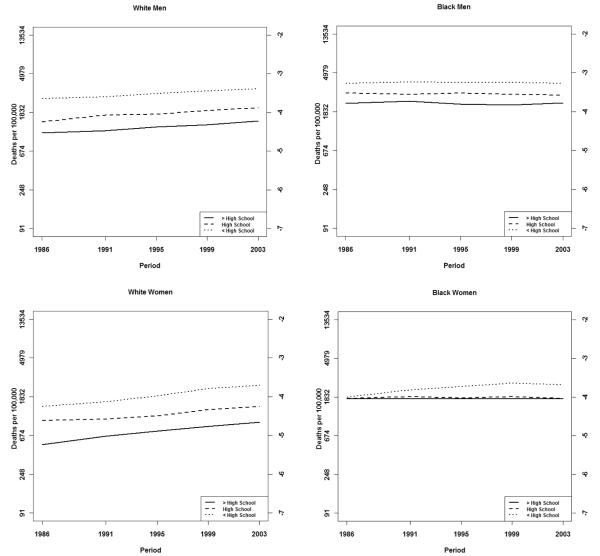
We next turn to Hypotheses 2, 3, and 4, in which we contrast the estimated period and cohort effects of all-cause mortality rates between 1986 and 2006 for black and white men and women in the United States. In reviewing the variance components of random cohort and period effects from models of black and white men’s and women’s all-cause mortality between 1986 and 2006 (Tables S2, S3, S4, and S5 in the online supplement), we draw three conclusions. In general, (1) cohort variance in mortality is significantly and sizably larger than period variance; (2) across all models, cohort variance is largest in the >HS education groups; and (3) race differences are evident in both of these patterns. Overall, this evidence supports Hypotheses 2, 3, and 4.7
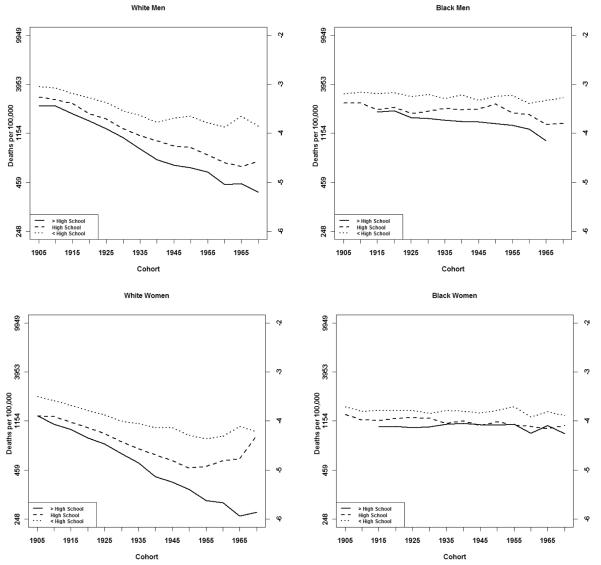
To best display results of these hypotheses tests, we refer to Figure 2, which presents education-specific estimates of log rates of all-cause mortality across cohorts for black and white men and women. We also turn to Figure 3, which illustrates the relatively negligible and not significant period variation in U.S. adult mortality. For white men, black men, and white women, we see strong evidence that educational differences in U.S. adult mortality grew across birth cohorts between 1986 and 2006. We observe significant and substantive declines in all-cause mortality for white men and women in the >HS education groups, yet much smaller reductions in mortality risk for the <HS groups. Among white women, we also note an increase in the HS education group’s mortality across recent cohorts. For black men, we see evidence of a small and stable educational gap in mortality, and a modest widening of this educational gap across cohorts. Small cell sizes preclude estimates of early cohort mortality patterns in the >HS education group for black men, but a steady cohort decline in mortality is evident from the 1915 to 1919 birth cohort through more recent cohorts. Because there is no cohort decline in black men’s mortality in the <HS education group, the education gap in black men’s mortality steadily widens across cohorts. These findings provide evidence that supports Hypotheses 2 and 3, in that educational differences in adult mortality grew from 1986 to 2006, and the educational gap grew across cohorts, not periods.
Figure 2.
Educational Differences in HAPC-CCREM Estimated Mortality Rates across Birth Cohort, Black and White Men and Women, NHIS-LMF 1986 to 2004
Figure 3.
Educational Differences in HAPC-CCREM Estimated Mortality Rates across Time Periods, Black and White Men and Women, NHIS-LMF 1986 to 2004
Findings for black women’s period and cohort trends exhibit several patterns that differ from the findings for the other race-sex groups. First, consistent with Hypothesis 4 and with findings for black men’s mortality, we find evidence that the education gap in black women’s mortality is significantly smaller than the respective education gap in white men’s and women’s adult mortality. Second, and also consistent with Hypothesis 4, cohort changes in the educational gap are more modest among black women and men than among white women and men. In fact, for black women, we find no evidence of significant cohort change in the education-mortality relationship. Conversely, we find growing, yet not significant, educational disparities in black women’s adult mortality across periods. Beyond age and cohort effects, black women with <HS education exhibited rising mortality rates across the 1986 to 2006 time period, whereas black women with higher levels of education exhibited no significant temporal change in mortality. Although not significant, the period trend could reflect a number of processes across this time period that disproportionately affected the mortality risk of low-educated black women. Changing labor market opportunities, for example, have produced absolute and relative loss of earnings for low-educated black women (Pettit and Ewert 2009). Moreover, research shows that the obesity epidemic is both a cohort and a period phenomenon that has disproportionately affected less educated black women (Ogden et al. 2006; Reither, Hauser, and Yang 2009). Finally, the nonsignificant cohort change in U.S. black women’s educational disparities in mortality might also reflect data sparseness issues in the NHIS-LMF. Small cell sizes are common in many early cohorts, irrespective of education, while counts of death are quite small, or nonexistent, in many of the more recent APC cells of the black women subsample.
Our general findings show that, first, reductions in U.S. adult all-cause mortality between 1986 and 2006 were driven overwhelmingly by cohort processes. Second, these reductions in mortality risk were significantly conditioned by educational attainment. And third, the way educational differences in mortality changed across cohorts was conditioned by race and gender. As such, we find evidence supporting our second, third, and fourth hypotheses. Indeed, evidence overwhelmingly suggests that the education gap in U.S. adult mortality risk grew substantially across this period, supporting Hypothesis 2. Furthermore, the growth in educational disparities in white men’s, black men’s, and white women’s mortality is a cohort trend, not a period trend, supporting Hypothesis 3. And finally, cohort changes in educational disparities in mortality differ significantly by race, supporting Hypothesis 4.
Trends in Educational Differences in Cause-Specific Mortality
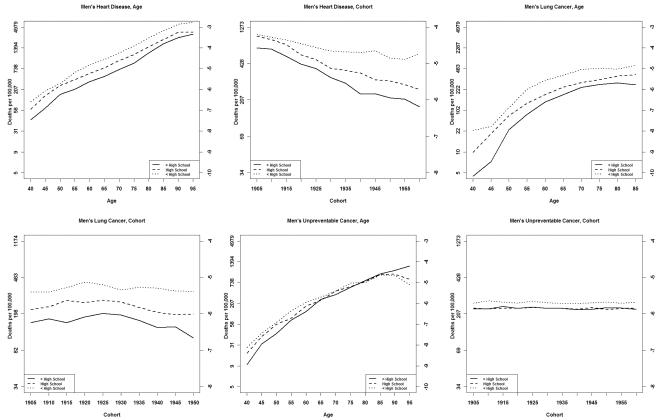
We next review results that test our fifth hypothesis, in which we contend that cohort changes in educational disparities in mortality are stronger for heart disease and lung cancer mortality than for unpreventable cancers. Figure 4 presents education-specific estimates of mortality from heart disease, lung cancer, and unpreventable cancer across age and cohorts for white men. Figure 5 presents these findings for white women.
Figure 4.
Educational Differences in HAPC-CCREM Estimated Mortality Rates from Specific Causes of Death across Age and Cohort, White Men, NHIS-LMF 1986 to 2004
Educational differences in men’s heart disease and lung cancer mortality rates across age are similar to the age patterns of educational differences in all-cause mortality. In each case, the education gap in mortality is large and observed at all age groups. Contrasted with these findings are the estimated age patterns of educational disparities in white men’s mortality rates from unpreventable cancers. In this case, we observe a much smaller educational gap that exists only among middle-aged adults. In short, the educational gap in white men’s mortality from unpreventable cancers is small and becomes nonsignificant relatively early in the life course. Results from APC analyses of white women’s heart disease and lung cancer mortality are similar to men’s, in that the educational gaps in age patterns of mortality are larger for heart disease and lung cancer mortality than for mortality from unpreventable cancers. However, whereas we see estimated educational differences in heart disease and lung cancer mortality at all ages for white men, evidence suggests that educational differences in mortality from these causes of death might converge at older ages for white women. Results from APC analyses of white women’s mortality from unpreventable cancers are also similar to men’s, in that the educational gap in mortality risk is small and becomes nonsignificant at early ages.
Regarding cohort changes in cause-specific mortality, our results provide evidence that strongly supports Hypothesis 5. In white men’s and women’s heart disease mortality, we observe a significant and substantial difference between respondents with a >HS education and those with a <HS education. Educational differences in cohort changes in heart disease mortality significantly widened the educational gap for both men and women. For men, we observe a flattening cohort trend for the <HS group’s heart disease mortality, whereas we observe significant and sizable cohort reductions in the >HS group’s heart disease mortality. For women, we see similar flattening and possibly increasing cohort trends in heart disease mortality for the <HS and HS education groups, but continued cohort reductions in the >HS group.
Educational disparities in men’s and women’s lung cancer mortality across cohorts follow a striking resemblance to cohort and educational patterns of smoking (Pampel 2003; Preston and Wang 2006; Wang and Preston 2009). Also, like educational disparities in heart disease mortality, men’s and women’s lung cancer mortality for respondents with a <HS education exhibits very little cohort variation, with lung cancer mortality rates essentially remaining the same across cohorts born in the 1930s through the 1950s. Conversely, men and women with a >HS education experienced substantive reductions in lung cancer mortality across recent cohorts.
Contrasted with the large and growing educational gaps in heart disease and lung cancer mortality in U.S. white men and women are cohort patterns of unpreventable cancer mortality. For both men and women, we observe much smaller and far more stable educational disparities in mortality. Indeed, estimates of cohort and period variance are not significant, and Figures 4 and 5 reveal no temporal change in educational differences in men’s and women’s unpreventable cancer mortality.
Our overall APC estimates of U.S. white men’s and women’s mortality rates between 1986 and 2006 from heart disease, lung cancer, and unpreventable cancer support Hypothesis 5. In short, educational disparities in heart disease and lung cancer mortality are significantly larger than educational disparities in unpreventable cancer mortality. Moreover, educational disparities in heart disease and lung cancer mortality grew significantly wider across birth cohorts between 1986 and 2006. Contrasted with these patterns, we find no evidence of temporal changes in educational disparities in unpreventable cancer mortality.
DISCUSSION
The cohort is an essential unit of analysis in studies of social change. Ryder (1965:845) rightly stressed that a cohort’s “distinctive composition and character reflect[s] the circumstances of its unique origination and history.” Importantly, he advised sociologists to focus on a cohort’s unique “flow of person-years” across history to best understand the effects that diffusing social norms and changing environments have on society. Riley (1973, 1978, 1987) advanced this line of thinking with her principle of cohort differences in aging, urging social researchers to recognize that cohorts age in distinct ways. Unfortunately, the cohort perspective has been underutilized in studies of U.S. mortality trends. Some life course researchers, however, have recently pushed the field in this direction and have empirically demonstrated that cohorts exhibit differential morbidity and mortality as a product of their unique exposures to early-life conditions (Crimmins and Finch 2006; Finch and Crimmins 2004; Fogel 2005; Fogel and Costa 1997). However, life course and cohort processes are not limited to childhood environments but likely extend into adult environments as well. As childhood conditions improve, cohorts’ varying exposures to subsequent advances in health-enhancing or health-protecting knowledge, practices, and technology produce disparate health and mortality outcomes across the life course.
In this study, we argued that education has played an increasingly important role in cohort processes related to life course patterns of mortality. As the United States underwent the epidemiologic transition during the early- and mid-twentieth century, disease patterns and causes of death shifted from infectious and communicable diseases that largely affected infants and children, to chronic and degenerative diseases that overwhelmingly affected the aged (Olshansky and Ault 1986; Omran [1971] 2005). Research shows that beyond the immediate effects of these changing disease patterns in childhood, the transition has slowly uncovered cohort effects on chronic disease susceptibility at older ages as well (Costa 2002; Finch and Crimmins 2004; Fogel 2004, 2005; Fogel and Costa 1997; Manton et al. 1997; Masters forthcoming). Thus, cohorts born in the later stages or after the epidemiologic transition have likely endured fewer and less harsh insults as they have aged, and are therefore increasingly composed of a more robust cohort morbidity phenotype. As effects of early-life environment on later-life mortality lessened across U.S. cohorts, advantages and disadvantages during adulthood increased in importance.
Our results provide evidence consistent with Link and Phelan’s (1995) fundamental cause theory, but with special attention given to the cohort-based effects of education. Specifically, our investigation yields the following five findings about adult mortality trends and disparities. First, we found empirical evidence consistent with previous findings that recent temporal changes in U.S. adult all-cause and cause-specific mortality risk were driven overwhelmingly by cohort processes (Yang 2008). Second, consistent with past research (Meara et al. 2008; Montez et al. 2011), we found that educational disparities in U.S. adult mortality have grown over the past two decades. Third, we demonstrated that these changes in educational disparities in adult mortality operated on a cohort, rather than a period, basis. That is, we showed that cohorts with <HS education did not experience the same reductions in all-cause mortality risk between 1986 and 2006 as cohorts with >HS education. However, the education-mortality relationship for black women in these data exhibits a pattern inconsistent with those found in the white men’s, white women’s, and black men’s samples. The unique patterns of black women’s cohort and period patterns of mortality change beg for further research. Fourth, we showed that cohort changes in the U.S. education-mortality relationship were conditioned by gender and race. And fifth, consistent with fundamental cause theory, we found that cohort changes in the education-mortality relationship were especially strong for deaths from heart disease and lung cancer. In contrast, we found a smaller and more stable educational gradient in mortality from unpreventable cancers.
Our analyses are not without limitations. First, the NHIS-LMF 1986 to 2006 captures a recent and short period of time. Although the lack of demonstrated period effects could be influenced by this data structure, we are encouraged by the similarities between our overall trend results and Yang’s (2008) trend results from a different dataset spanning the time period 1960 to 1999. Second, due to small cell sizes for certain combinations of education levels and specific causes of death, we were forced to measure educational attainment with only three levels. It would be useful, for example, to separate the greater than high school education group into a some college group and a bachelor’s degree or higher group to explore differential effects of accreditation on mortality risk. Future analyses of all-cause mortality should be able to do so because more recent birth cohorts are characterized by higher and higher levels of education. Third, our article tested important foundational hypotheses of mortality change but did not focus on the specific mechanisms responsible for the cohort effects we uncovered. Future work in this area should aim to append cohort- and period-based measures of social change onto datasets like the NHIS-LMF to better understand such mechanisms.
Despite these limitations, the present study provides clear findings regarding the nature of temporal changes in educational differences in U.S. adult mortality risk. Consistent with both a cohort perspective of mortality change and fundamental cause theory, we found that cohort processes are driving temporal changes in adult mortality risk and that educational differences in adult mortality risk are growing across birth cohorts. While the cohort patterns driving the growing educational divide in mortality differ by gender, race, and cause of death, the overall change is directly counter to the major U.S. goal of eliminating disparities in health across socioeconomic groups (Healthy People 2010 [National Center for Health Statistics 2011]). These important findings emphasize the need for researchers to integrate a sociological understanding of cohort change into analyses of individual- and group-level mortality trends. Understanding sociohistorical contexts is central to understanding temporal changes in mortality risk, and a cohort perspective rooted in rich sociological theory is well-suited for understanding these contexts.
Furthermore, our findings should be useful in advancing effective policies that address the fundamental causes of health disparities. Our results clearly show not only wide U.S. mortality differences by education, but also that this is especially the case among more recent U.S. birth cohorts. In other words, our most highly educated individuals are better positioned than ever to live long lives, while less educated individuals are becoming increasingly distanced, at least in terms of mortality rates, from the most highly educated. Such findings provide strong evidence that policies that help shift more and more people out of the lowest levels of education to higher levels will not only improve overall population health but will also reduce the impact of disparities. Indeed, as Schoeni and colleagues (2008:10) affirm, “health research and policy in the United States must move towards models” that “consistently evaluate the impact of all policy—not just health policy.” Unfortunately, 13.1 percent of current U.S. adults age 25 to 34 years do not have a high school diploma (U.S. Census Bureau 2012), illustrating that we have much continued room for improvement along these lines. And while a compositional shift toward higher levels of educational attainment would, in and of itself, have no impact on relative educational differences in adult mortality, it would clearly expose many fewer individuals to the heightened risks of mortality due to low education that are particularly characteristic of recent birth cohorts of U.S. adults. Such fundamental, long-term thinking and policy action is necessary if we are to achieve success in improving U.S. population health.
Supplementary Material
Acknowledgments
We thank Mark Hayward, Tom Pullum, the Education-Mortality Working Group at the PRC, and the anonymous reviewers and ASR editors for very helpful comments and advice on this draft.
Biographies
Ryan K. Masters is a postdoctoral researcher and Robert Wood Johnson Foundation Health & Society Scholar at Columbia University. He received his PhD in sociology and demography from the University of Texas at Austin in 2011.
Robert A. Hummer is Centennial Commission Professor of Liberal Arts in the Department of Sociology and Population Research Center at the University of Texas at Austin. His research focuses on the careful documentation and understanding of health and mortality disparities in the United States. Together with Richard Rogers and Charles Nam, he published Living and Dying in the USA: Health, Behavioral, and Social Differentials of Adult Mortality (Academic Press, 2000), which won the Otis Dudley Duncan Award from the Population Section of the American Sociological Association for its contribution to the field of social demography.
Daniel A. Powers is a Professor of Sociology and a research associate at the Population Research Center at the University of Texas at Austin. He specializes in statistical methods in the context of health disparities, with a particular focus on infant mortality in the United States. He has published a second edition of his book with Yu Xie, Statistical Methods for Categorical Data Analysis, London: Emerald Books (2008). In addition to teaching UT courses he regularly gives short courses and workshops on specific methods.
Footnotes
We gratefully acknowledge support provided by a grant (1 R01-HD053696, PI Robert A. Hummer) from the Eunice Kennedy Shriver National Institute of Child Health Research and Human Development and by an NICHD infrastructure grant (5 R24 HD042849) awarded to the Population Research Center (PRC) at the University of Texas at Austin. We also gratefully acknowledge support provided by a research grant from the National Institute for Minority Health Disparities (1 R01MD00425, PI Brian K. Finch). We also thank the Robert Wood Johnson Foundation Health and Society Scholars Program for its financial support. We further thank Mark Hayward, Tom Pullum, the Education-Mortality Working Group at the PRC, and the anonymous reviewers and ASR editors for very helpful comments and advice on this draft. Please address any correspondence to: Ryan K. Masters, Columbia University, International Affairs Building, 420 West 118th St., 8th Floor, Mail Code 3355, New York, NY 10027.
Figure S1 in the online supplement (http://asr.sagepub.com/supplemental) presents cohort-level changes in the percent of U.S. infants born into large families (defined as having six or more members), the percent of infants born into farming households, the percent of infants born in southern states, and sex- and race-specific infant mortality rates. These measures serve as proxies of the drastic improvements in living and health conditions that unfolded across U.S. birth cohorts during the twentieth century. We present these cohort changes by race to illustrate the significant role race has played in shaping cohort changes in U.S. early-life conditions. In every measure, black (or non-white) cohorts endured higher levels of disadvantage and slower rates of improvement across time. We must consider these racial differences when we think about cohort changes in the education-mortality relationship.
Furthermore, in APC analyses of U.S. adult mortality rates between 1986 and 2006 (not shown), these measures of early-life conditions, as well as cohorts’ smoking patterns, accounted for nearly all variance in cohort-level mortality. In a reduced model, smoking alone accounted for large amounts of cohort variance in mortality, but only for cohorts born after the 1930s. Cohorts born between 1900 and 1935 were not substantively affected by cohorts’ smoking prevalence. Also, individual-level educational attainment accounted for only a small reduction in cohort variance in adult mortality between 1986 and 2006. These findings illustrate two key points. One, although indicators of the adult environment (i.e., education and smoking) explain some variance in cohort mortality risk, substantial cohort variance was not explained. Two, the variance explained by indicators associated with the adult environment was largely confined to cohorts born in the latter half of the twentieth century. Thus, both early-life and adult conditions appear to be associated with cohort variation in U.S. adult mortality risk.
We classified a cause of death as an “unpreventable” cancer by using the NCHS’s 113 Selected Causes of Death (NHCS 2010b) and Phelan and colleagues’ (2004) Appendix A. We classified deaths due to any cancer with a preventability rating lower than 4.0 as unpreventable cancers and coded them as 1; all other deaths or censored cases were coded as 0.
Individuals older than 99 years were censored from the sample because cell sizes and counts of death for the five-year age range 100 to 104 years were very small.
We attempted to analyze educational differences in U.S. adult mortality using HAPC discrete-time survival models. We estimated these models using the individual-level person-period data with a binomial family (1/0) and a complimentary-log-log link function, but convergence was achieved only for analyses of all-education/all-cause mortality of white men and women. To estimate effects of education, and to analyze these effects by race and cause of death, we had to aggregate the data.
Aggregated data did not always amount to 168 cells for all-cause mortality or to 132 cells for cause-specific mortality. The sample of black men with a HS education amounted to only 160 APC cells, and the sample of black men with a >HS education amounted to only 164 APC cells. Black women with a >HS education contained only 167 APC cells. Also, we limited the models of lung cancer mortality to ages 25–29 to 90–94 years due to small cell sizes at the oldest age group. As a result of this, the white men’s and women’s samples used to analyze lung cancer mortality, irrespective of educational attainment, all contained 126 APC cells.
To facilitate estimation, we set hyperpriors on variances of black men’s and women’s random period and cohort effects to narrower limits than (.001,.001). All programs and data are available upon request.
Due to limited space, we do not show statistical tests of the cohort and period variance components. We conducted significant tests of random-effects cohort and period coefficients following Yang and colleagues’ (2009) four-step guide to assessing significance in CCREMs. These are available upon request.
Contributor Information
Ryan K. Masters, Columbia University
Robert A. Hummer, The University of Texas at Austin
Daniel A. Powers, The University of Texas at Austin
References
- Baker David P., Juan Leon, Greenway Emily G. Smith, John Collins, Marcela Movit. The Education Effect on Population Health: A Reassessment. Population Development and Review. 2011;37:307–332. doi: 10.1111/j.1728-4457.2011.00412.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barker DJP. The Origins of the Developmental Origins Theory. Journal of Internal Medicine. 2007;261:412–17. doi: 10.1111/j.1365-2796.2007.01809.x. [DOI] [PubMed] [Google Scholar]
- Beckett Megan. Converging Health Inequalities in Later Life: An Artifact of Mortality Selection? Journal of Health and Social Behavior. 2000;41:106–119. [PubMed] [Google Scholar]
- Ben-Shlomo Yoav, Diana Kuh. A Life Course Approach to Chronic Disease Epidemiology: Conceptual Models, Empirical Challenges, and Interdisciplinary Perspectives. International Journal of Epidemiology. 2002;31:285–93. [PubMed] [Google Scholar]
- Blackwell Debra, Mark Hayward, Eileen Crimmins. Does Childhood Health Affect Chronic Morbidity in Later Life? Social Science and Medicine. 2001;52:1269–84. doi: 10.1016/s0277-9536(00)00230-6. [DOI] [PubMed] [Google Scholar]
- Case Anne, Christina Paxson. Causes and Consequences of Early-Life Health. Demography. 2010;47:S65–S85. doi: 10.1353/dem.2010.0007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell Mary, Haveman Robert, Sandefur Gary, Barbara Wolfe. Economic Inequality and Educational Attainment across a Generation. Focus. 2005;23:11–15. [Google Scholar]
- Centers for Disease Control Achievements in Public Health 1900–1999: Control of Infectious Diseases. Morbidity and Mortality Weekly Report. 1999;48:621–29. [Google Scholar]
- Chang Virginia W., Lauderdale Diane S. Fundamental Cause Theory, Technological Innovation, and Health Disparities: The Case of Cholesterol in the Era of Statins. Journal of Health and Social Behavior. 2009;50:245–60. doi: 10.1177/002214650905000301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Feinian, Yang Yang, Guangya Liu. Social Change and Socioeconomic Disparities in Health over the Life Course in China: A Cohort Analysis. American Sociological Review. 2010;75:126–50. doi: 10.1177/0003122409359165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colen Cynthia G. Addressing Racial Disparities in Health Using Life Course Perspectives. Du Bois Review. 2011;8:79–94. [Google Scholar]
- Cooper R, Cutler J, Desvigne-Nickens P, Fortmann SP, Friedman L, Havlik R, Hogelin G, Marler J, McGovern P, Morosco G, Mosca L, Pearson T, Stamler J, Stryer D, Thom T. Trends and Disparities in Coronary Heart Disease, Stroke, and Other Cardiovascular Disease in the United States: Findings of the National Conference on Cardiovascular Disease Prevention. Circulation. 2000;102:3137–47. doi: 10.1161/01.cir.102.25.3137. [DOI] [PubMed] [Google Scholar]
- Costa Dora L. Changing Chronic Disease Rates and Long-Term Declines in Functional Limitation among Older Men. Demography. 2002;39:119–37. doi: 10.1353/dem.2002.0003. [DOI] [PubMed] [Google Scholar]
- Crimmins Eileen M. The Changing Pattern of American Mortality Decline, 1940–1977, and Its Implications for the Future. Demography. 1981;7:229–54. [Google Scholar]
- Crimmins Eileen M., Finch Caleb E. Infection, Inflammation, Height, and Longevity. Proceedings of the National Academy of Sciences. 2006;103:498–503. doi: 10.1073/pnas.0501470103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cutler David, Fabian Lange, Ellen Meara, Seth Richards, Ruhm Christopher J. Explaining the Rise in Educational Gradients in Mortality. National Bureau of Economic Research. 2010 Working Paper Series, Working Paper 15678. [Google Scholar]
- Cutler David, Miller Grant. The Role of Public Health Improvements in Health Advances: The Twentieth Century United States. Demography. 2005;42:1–22. doi: 10.1353/dem.2005.0002. [DOI] [PubMed] [Google Scholar]
- Davey Smith, George, Carole Hart, David Blane, Hole David. Adverse Socioeconomic Conditions in Childhood and Cause Specific Adult Mortality: Prospective Observational Study. British Medical Journal. 1998;316:1631–35. doi: 10.1136/bmj.316.7145.1631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Denney Justin T., Rogers Richard G., Hummer Robert A., Pampel Fred C. Educational Inequality in Mortality: The Age and Gender Specific Mediating Effects of Cigarette Smoking. Social Science Research. 2010;39:662–73. doi: 10.1016/j.ssresearch.2010.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Department of Health and Human Services . Healthy People 2020. Office of Disease Prevention and Health Promotion; Washington, DC: 2010. [Google Scholar]
- Easterlin Richard A. Growth Triumphant: The Twenty-first Century in Historical Perspective. University of Michigan Press; Ann Arbor: 1997. [Google Scholar]
- Feldman Jacob J., Makuc Diane M., Kleinman Joel C., Cornoni-Huntley Joan. National Trends in Educational Differentials in Mortality. American Journal of Epidemiology. 1989;129:919–33. doi: 10.1093/oxfordjournals.aje.a115225. [DOI] [PubMed] [Google Scholar]
- Finch Caleb E., Crimmins Eileen M. Inflammatory Exposure and Historical Changes in Human Life-Spans. Science. 2004;305:1736–39. doi: 10.1126/science.1092556. [DOI] [PubMed] [Google Scholar]
- Fogel Robert W. The Escape from Hunger and Premature Death, 1700–2100: Europe, America, and the Third World. Cambridge University Press; New York: 2004. [Google Scholar]
- Fogel Robert W. Changes in the Disparities in Chronic Diseases during the Course of the 20th Century. Perspectives in Biology and Medicine. 2005;48(1S):S150–S165. [PubMed] [Google Scholar]
- Fogel Robert W., Costa Dora L. A Theory of Technophysio Evolution, With Some Implications for Forecasting Population, Health Care Costs, and Pension Costs. Demography. 1997;34:49–66. [PubMed] [Google Scholar]
- Freedman Vicki A., Martin Linda G., Schoeni Robert F., Corman Jennifer C. Declines in Late-life Disability: The Role of Early- and Mid-life Factors. Social Science and Medicine. 2008;66:1588–1602. doi: 10.1016/j.socscimed.2007.11.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gelman Andrew. Prior Distributions for Variance Parameters in Hierarchical Models. Bayesian Analysis. 2006;1:515–33. [Google Scholar]
- Gelman Andrew, Carlin John B., Stern Hal S., Rubin Donald B. Bayesian Data Analysis. 2nd Chapman & Hall/CRC; Boca Raton, FL: 2004. [Google Scholar]
- Glenn Norval D. Cohort Analysis. 2nd Sage Publications; Thousand Oaks, CA: 2005. [Google Scholar]
- Glied Sherry, Lleras-Muney Adriana. Technological Innovation and Inequality in Health. Demography. 2008;45:741–61. doi: 10.1353/dem.0.0017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gluckman Peter D., Hanson Mark A., Cyrus Cooper, Thornburg Kent L. Effect of In Utero and Early-life Conditions on Adult Health and Disease. New England Journal of Medicine. 2008;359:61–73. doi: 10.1056/NEJMra0708473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guyer Bernard, Freedman Mary Anne, Strobino Donna M., Sondik Edward J. Annual Summary of Vital Statistics: Trends in the Health of Americans during the 20th Century. Pediatrics. 2000;106:1307–1317. doi: 10.1542/peds.106.6.1307. [DOI] [PubMed] [Google Scholar]
- Harper Sam, John Lynch, Scott Burris, Smith George Davey. Trends in the Black-White Life Expectancy Gap in the United States, 1983–2003. Journal of the American Medical Association. 2007;297:1224–32. doi: 10.1001/jama.297.11.1224. [DOI] [PubMed] [Google Scholar]
- Hayward Mark D., Crimmins Eileen M., Miles Toni P., Yang Yu. The Significance of Socioeconomic Status in Explaining the Racial Gap in Chronic Health Conditions. American Sociological Review. 2000;65:910–930. [Google Scholar]
- Hayward Mark D., Gorman Bridget K. The Long Arm of Childhood: The Influence of Early-Life Social Conditions on Men’s Mortality. Demography. 2004;41:87–107. doi: 10.1353/dem.2004.0005. [DOI] [PubMed] [Google Scholar]
- Human Mortality Database University of California, Berkeley (USA), and Max Planck Institute for Demographic Research. 2011 Retrieved ( http://www.mortality.org) [Google Scholar]
- Hummer Robert A., Chinn Juanita J. Race/Ethnicity and U.S. Adult Mortality: Progress, Prospects, and New Analyses. Du Bois Review. 2011;8:5–24. doi: 10.1017/S1742058X11000051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hummer Robert A., Lariscy Joseph T., Crimmins EM. Educational Attainment and Adult Mortality. In: Rogers RG, editor. Chapter 12 in International Handbook of Adult Mortality. Springer; New York: 2011. [Google Scholar]
- Integrated Health Interview Series (IHIS) Minnesota Population Center and State Health Access Data Assistance Center, Integrated Health Interview Series: Version 3.0. University of Minnesota; Minneapolis: 2011. [Google Scholar]
- Jemal Ahmedin, Thun Michael J., Ward Elizabeth E., Henley S. Jane, Cokkinides Vilma E., Murray Taylor E. Mortality from Leading Causes by Education and Race in the United States, 2001. American Journal of Preventative Medicine. 2008;34:1–8. doi: 10.1016/j.amepre.2007.09.017. [DOI] [PubMed] [Google Scholar]
- Jemal Ahmedin, Elizabeth Ward, Yongping Hao, Michael Thun. Trends in the Leading Causes of Death in the United States, 1970–2002. Journal of the American Medical Association. 2005;294:1255–59. [Google Scholar]
- Kestilä L, Koskinen S, Martelin T, Rahkonen O, Pensola T, Aro H, Aromaa A. Determinants of Health in Early Adulthood: What Is the Role of Parental Education, Childhood Adversities, and Own Education? European Journal of Public Health. 2006;16:306–315. doi: 10.1093/eurpub/cki164. [DOI] [PubMed] [Google Scholar]
- Kitagawa Evelyn M., Hauser Phillip M. Differential Mortality in the United States: A Study in Socioeconomic Epidemiology. Harvard University Press; Cambridge, MA: 1973. [Google Scholar]
- Lauderdale Diane S. Education and Survival: Birth Cohort, Age and Period Effects. Demography. 2001;38:551–61. doi: 10.1353/dem.2001.0035. [DOI] [PubMed] [Google Scholar]
- Link Bruce G. Epidemiological Sociology and the Social Shaping of Population Health. Journal of Health and Social Behavior. 2008;49:367–84. doi: 10.1177/002214650804900401. [DOI] [PubMed] [Google Scholar]
- Link Bruce G., Phelan Jo C. Social Conditions as Fundamental Causes of Disease. Journal of Health and Social Behavior. 1995;35:80–94. [PubMed] [Google Scholar]
- Link Bruce G., Phelan Jo C. Editorial: Understanding Sociodemographic Differences in Health: The Role of Fundamental Social Causes. American Journal of Public Health. 1996;86:471–73. doi: 10.2105/ajph.86.4.471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Link Bruce G., Phelan Jo C. McKeown and the Idea That Social Conditions Are Fundamental Causes of Disease. American Journal of Public Health. 2002;92:730–32. doi: 10.2105/ajph.92.5.730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lucas FL, DeLorenzo Michael A., Siewers Andrea E., Wennberg David E. Temporal Trends in the Utilization of Diagnostic Testing and Treatments for Cardiovascular Disease in the United States, 1993–2001. Circulation. 2006;113:374–79. doi: 10.1161/CIRCULATIONAHA.105.560433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lynch Scott M. Cohort and Life-Course Patterns in the Relationship between Education and Health: A Hierarchical Approach. Demography. 2003;40:309–331. doi: 10.1353/dem.2003.0016. [DOI] [PubMed] [Google Scholar]
- Lynch Scott M. Explaining Life Course and Cohort Variation in the Relationship between Education and Health: The Role of Income. Journal of Health and Social Behavior. 2006;47:324–38. doi: 10.1177/002214650604700402. [DOI] [PubMed] [Google Scholar]
- Lynch Scott M. Introduction to Applied Bayesian Statistics and Estimation for Social Scientists. Springer; New York: 2007. [Google Scholar]
- Lynch Scott M., Brown J. Scott, Harmsen Katherine G. Black-White Differences in Mortality Compression and Deceleration and the Mortality Crossover Reconsidered. Research on Aging. 2003;25:456–83. [Google Scholar]
- Manton Kenneth G., Eric Stallard, Corder Larry. Changes in the Age Dependence of Mortality and Disability: Cohort and Other Determinants. Demography. 1997;34:135–57. [PubMed] [Google Scholar]
- Mason Karen O., Mason William H., Winsborough HH, Poole W. Kenneth. Some Methodological Issues in Cohort Analysis of Archival Data. American Sociological Review. 1973;32:242–58. [Google Scholar]
- Masters Ryan K. Uncrossing the U.S. Black-White Mortality Crossover: The Role of Cohort Forces in Life Course Mortality Risk. Demography. doi: 10.1007/s13524-012-0107-y. Forthcoming. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meara Ellen, Seth Richards, Cutler David. The Gap Gets Bigger: Changes in Mortality and Life Expectancy, by Education. Health Affairs. 2008;27:350–60. doi: 10.1377/hlthaff.27.2.350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miech Richard, Fred Pampel, Jinyoung Kim, Rogers Richard G. The Enduring Association between Education and Mortality: The Role of Widening and Narrowing Disparities. American Sociological Review. 2011;76:913–34. doi: 10.1177/0003122411411276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mirowsky John, Ross Catherine E. Education, Social Status and Health. Aldine de Gruyter; New York: 2003. [Google Scholar]
- Mirowsky John, Ross Catherine E. Education and Self-Rated Health: Cumulative Advantage and Its Rising Importance. Research on Aging. 2008;30:93–122. [Google Scholar]
- Montez Jennifer K., Hayward Mark D. Early Life Conditions and Later Life Mortality. Chapter Nine in International Handbook of Adult Mortality. 2011;2(2):187–206. [Google Scholar]
- Montez Jennifer K., Hummer Robert A., Hayward Mark D. Educational Attainment and Adult Mortality in the United States: A Systematic Analysis of Functional Form. Demography. 2012;48:315–336. doi: 10.1007/s13524-011-0082-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montez Jennifer K., Hummer Robert A., Hayward Mark D., Hyeyoung Woo, Rogers Richard G. Trends in the Educational Gradient of U.S. Adult Mortality from 1986 through 2006 by Race, Gender, and Age Group. Research on Aging. 2011;33:145–71. doi: 10.1177/0164027510392388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Center for Health Statistics . Healthy People 2000 Final Review. Public Health Service; Hyattsville, Maryland: 2001. [Google Scholar]
- National Center for Health Statistics National Health Interview Survey (1986-2004) Linked Mortality Files: Analytic Guidelines. 2010a Analytic Support, Data Linkage Team, Office of Analysis and Epidemiology: http://www.cdc.gov/nchs/data_access/data_linkage/mortality/nhis_linkage.htm#description. [Google Scholar]
- National Center for Health Statistics The National Health Interview Survey 1986-2004 Linked Mortality Files Public-use File Layout. 2010b Analytic Support, Data Linkage Team, Office of Analysis and Epidemiology: http://www.cdc.gov/nchs/data/datalinkage/nhis_file_layout_public_2010.pdf. [Google Scholar]
- National Center for Health Statistics . Healthy People 2010 Final Review. Public Health Service; Hyattsville, Maryland: 2011. [Google Scholar]
- Ogden Cynthia, Margaret Carrol, Lester Curtin, Margaret McDowell, Carolyn Tabak, Katherine Flegal. Prevalence of Overweight and Obesity in the United States, 1999–2004. Journal of the American Medical Association. 2006;295:1549–55. [Google Scholar]
- Olshansky S. Jay, Ault Brian. The Fourth Stage of the Epidemiologic Transition: The Age of Delayed Degenerative Diseases. Milbank Quarterly. 1986;64:355–91. [PubMed] [Google Scholar]
- Omran Abdel R. The Epidemiological Transition: A Theory of the Epidemiology of Population Change. Milbank Quarterly. 2005;83:731–57. doi: 10.1111/j.1468-0009.2005.00398.x. 1971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Rand Angela M., Hamil-Luker Jenifer. Processes of Cumulative Adversity: Childhood Disadvantage and Increased Risk of Heart Attack across the Life Course. Journals of Gerontology Series B:Psychological Sciences and Social Sciences. 2007;60:S117–S124. doi: 10.1093/geronb/60.special_issue_2.s117. Special Issue 2. [DOI] [PubMed] [Google Scholar]
- Palloni Alberto. Reproducing Inequalities: Luck, Wallets, and the Enduring Effects of Childhood Health. Demography. 2006;43:587–615. doi: 10.1353/dem.2006.0036. [DOI] [PubMed] [Google Scholar]
- Pampel Fred C. Age and Education Patterns of Smoking among Women in High-Income Nations. Social Science and Medicine. 2003;57:1505–1514. doi: 10.1016/s0277-9536(02)00543-9. [DOI] [PubMed] [Google Scholar]
- Pappas Gregory, Susan Queen, Wilbur Hadden, Fisher Gail. The Increasing Disparity in Mortality between Socioeconomic Groups in the United States, 1960 and 1986. New England Journal of Medicine. 1993;329:103–109. doi: 10.1056/NEJM199307083290207. [DOI] [PubMed] [Google Scholar]
- Pettit Becky, Ewert Stephanie. Employment Gains and Wage Declines: The Erosion of Black Women’s Relative Wages since 1980. Demography. 2009;46:469–92. doi: 10.1353/dem.0.0061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phelan Jo C., Link Bruce G., Ana Diz-Roux, Ichiro Kawachi, Levin Bruce. ‘Fundamental Causes’ of Social Inequalities in Mortality: A Test of the Theory. Journal of Health and Social Behavior. 2004;45:265–85. doi: 10.1177/002214650404500303. [DOI] [PubMed] [Google Scholar]
- Phelan Jo C., Link Bruce G., Tehranifar Parisa. Social Conditions as Fundamental Causes of Health Inequalities: Theory, Evidence, and Policy Implications. Journal of Health and Social Behavior. 2010;51:S28–S40. doi: 10.1177/0022146510383498. [DOI] [PubMed] [Google Scholar]
- Preston Samuel H., Elo Irma T. Are Educational Differentials in Adult Mortality Increasing in the United States? Journal of Aging and Health. 1995;7:476–96. doi: 10.1177/089826439500700402. [DOI] [PubMed] [Google Scholar]
- Preston Samuel H., Wang Haidong. Sex Mortality Differences in the United States: The Role of Cohort Smoking Patterns. Demography. 2006;43:631–46. doi: 10.1353/dem.2006.0037. [DOI] [PubMed] [Google Scholar]
- Reither Eric S., Robert Hauser, Yang Yang. Do Birth Cohorts Matter? Age-Period-Cohort Analyses of the Obesity Epidemic in the United States. Social Science and Medicine. 2009;69:1439–48. doi: 10.1016/j.socscimed.2009.08.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reither Eric S., Olshansky S. Jay, Yang Yang. New Forcasting Methodology Inidicates More Disease and Earlier Mortality Ahead for Today’s Younger Americans. Health Affairs. 2011;30(8):1562–1568. doi: 10.1377/hlthaff.2011.0092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riley Matilda White. Aging and Cohort Succession: Interpretation and Misinterpretations. Public Opinion Quarterly. 1973;37:35–49. [Google Scholar]
- Riley Matilda White. Aging, Social Change, and the Power of Ideas. Daedalus. 1978;107:39–52. [PubMed] [Google Scholar]
- Riley Matilda White. On the Significance of Age in Sociology. American Sociological Review. 1987;52:1–14. [Google Scholar]
- Riley Matilda White, Riley John W., Jr. Longevity and Social Structure: The Potential of the Added Years. In: Pifer A, Bronte L, editors. Our Aging Society: Paradox and Promise. W.W. Norton & Company; New York: 1986. pp. 53–77. [Google Scholar]
- Rogers Richard G., Hackenberg Robert. Extending Epidemiologic Transition Theory: A New Stage. Social Biology. 1987;34:234–43. doi: 10.1080/19485565.1987.9988678. [DOI] [PubMed] [Google Scholar]
- Ross Catherine E., Chia-ling Wu. The Links between Education and Health. American Sociological Review. 1995;60:719–45. [Google Scholar]
- Steven Ruggles, Alexander J. Trent, Katie Genadek, Ronald Goeken, Schroeder Matthew B., Sobek Matthew. Integrated Public Use Microdata Series: Version 5.0 [Machine-readable database] University of Minnesota; Minneapolis: 2011. [Google Scholar]
- Ryder Norman B. The Cohort as a Concept in the Study of Social Change. American Sociological Review. 1965;30:843–61. [PubMed] [Google Scholar]
- Schoeni Robert F., House James S., Kaplan George A., Pollack Harold., editors. Making Americans Healthier: Social and Economic Policy as Health Policy. Russell Sage Foundation; New York: 2008. [Google Scholar]
- Shuey Kim M., Willson Andrea E. Cumulative Disadvantage and Black-White Trajectories in Life-Course Health Trajectories. Research on Aging. 2008;30:200–225. [Google Scholar]
- Simanek Amanda, Jennifer Beam Dowd, Aiello Allison. Persistent Pathogens Linking Socioeconomic Position and Cardiovascular Disease in the U.S. International Journal of Epidemiology. 2008;38:775–87. doi: 10.1093/ije/dyn273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith Herb. Advances in Age-Period-Cohort Analysis. Sociological Methods and Research. 2008;36:287–96. [Google Scholar]
- U.S. Census Bureau Educational Attainment. American Community Survey. 20092005–2007 Table S1501. Retrieved September 14, 2011 ( http:factfinder.census.gov) [Google Scholar]
- U.S. Department of Health and Human Services . Healthy People 2010: Understanding and Improving Health. Second USGPO; Washington, DC: 2000. [Google Scholar]
- van den Berg Gerard J., Doblhammer-Reiter Gabriele, Christensen Kaare. Being Born Under Adverse Economic Conditions Leads to a Higher Cardiovascular Mortality Rate Later in Life: Evidence Based on Individuals Born at Different Stages of the Business Cycle. Demography. 2011;48(2):507–530. doi: 10.1007/s13524-011-0021-8. [DOI] [PubMed] [Google Scholar]
- Wang Haidong, Preston Samuel H. Forecasting United States Mortality Using Cohort Smoking Histories. Proceedings of the National Academy of Sciences. 2009;106:393–98. doi: 10.1073/pnas.0811809106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warren John Robert, Hernandez Elaine M. Did Socioeconomic Inequalities in Morbidity and Mortality Change in the United States over the Course of the Twentieth Century? Journal of Health and Social Behavior. 2007;48:335–51. doi: 10.1177/002214650704800401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams David R., Jackson Pamela Braboy. Social Sources of Racial Disparities in Health. Health Affairs. 2005;24:325–34. doi: 10.1377/hlthaff.24.2.325. [DOI] [PubMed] [Google Scholar]
- Williams David R., Mohammed Selina A., Jacinta Leavell, Collins Chiquita. Race, Socioeconomic Status, and Health: Complexities, Ongoing Challenges, and Research Opportunities. Annals of the New York Academy of Sciences. 2010;1186:69–101. doi: 10.1111/j.1749-6632.2009.05339.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams David R., Sternthal Michelle. Understanding Racial-Ethnic Disparities in Health: Sociological Contributions. Journal of Health and Social Behavior. 2010;51:S15–S27. doi: 10.1177/0022146510383838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willson Andrea E., Shuey Kim M., Elder Glen H., Jr. Cumulative Advantage Processes as Mechanisms of Inequality in Life Course Health. American Journal of Sociology. 2007;112:1886–1924. [Google Scholar]
- Xu Jiaquan, Kochanek Kenneth D., Murphy Sherry L., Tejada-Vera Betzaida. National Vital Statistics Reports. 19. Vol. 58. Hyattsville, MD: 2010. Deaths: Final Data for 2007. [PubMed] [Google Scholar]
- Yang Yang. Bayesian Inference for Hierarchical Age-Period-Cohort Models of Repeated Cross-Section Survey Data. Sociological Methodology. 2006;36:39–74. [Google Scholar]
- Yang Yang. Trends in U.S. Adult Chronic Disease Mortality, 1960–1999: Age, Period, and Cohort Variations. Demography. 2008;45:387–416. doi: 10.1353/dem.0.0000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Yang, Steven Frenk, Land Kenneth. Assessing the Significance of Cohort and Period Effects in Hierarchical Age-Period-Cohort Models. Presented at the annual meeting of the American Sociological Association; San Francisco, CA. August 8; 2009. http://www.allacademic.com/meta/p307398_index.html. [Google Scholar]
- Yang Yang, Land Kenneth C. A Mixed Models Approach to the Age-Period-Cohort Analysis of Repeated Cross-Section Surveys, with an Application on Trends in Verbal Test Score. Sociological Methodology. 2006;36:75–97. [Google Scholar]
- Yang Yang, Land Kenneth C. Age-Period-Cohort Analysis of Repeated Cross-Section Surveys: Fixed or Random Effects? Sociological Methods and Research. 2008;36:297–326. [Google Scholar]
- Yang Yang, Lee Linda C. Sex and Race Disparities in Health: Cohort Variation in Life Course Patterns. Social Forces. 2009;87:2093–2124. [Google Scholar]
- Zajacova Anna, Hummer Robert A. Gender Differences in Education Effects on All-Cause Mortality for White and Black Adults in the United States. Social Science and Medicine. 2009;69:529–37. doi: 10.1016/j.socscimed.2009.06.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.