Abstract
Context
Chondroitin sulfate proteoglycans (CSPGs), a main component of the brain extracellular matrix, regulate developmental and adult neural functions that are highly relevant to the pathogenesis of schizophrenia. Such functions, together with marked expression of CSPGs in astrocytes within the normal human amygdala and evidence of a disruption of astrocytic functions in this disease, point to involvement of CSPG-glial interactions in schizophrenia.
Hypothesis
Chondroitin sulfate proteoglycan–related abnormalities involve glial cells and extracellular matrix pericellular aggregates (perineuronal nets) in the amygdala and entorhinal cortex of subjects with schizophrenia.
Design
Postmortem case-control study.
Setting
The Translational Neuroscience Laboratory at McLean Hospital, Harvard Medical School. Specimens were obtained from the Harvard Brain Tissue Resource Center at McLean Hospital.
Participants
Two separate cohorts of healthy control (n = 15; n = 10) and schizophrenic (n = 11; n = 10) subjects and a cohort of subjects with bipolar disorder (n=11).
Interventions
Quantitative, immunocytological, and histological postmortem investigations.
Main Outcome Measures
Numerical densities of CSPG-positive glial cells and perineuronal nets, glial fibrillary acidic protein-positive astrocytes, and total numbers of parvalbumin-positive neurons in the deep amygdala nuclei and entorhinal cortex.
Results
In schizophrenia, massive increases in CSPG-positive glial cells were detected in the deep amygdala nuclei (419%–1162%) and entorhinal cortex (layer II; 480%–1560%). Perineuronal nets were reduced in the lateral nucleus of the amygdala and lateral entorhinal cortex (layer II). Numerical densities of glial fibrillary acidic protein-positive glial cells and total numbers of parval-bumin-positive neurons were unaltered. Changes in CSPG-positive elements were negligible in subjects with bipolar disorder.
Conclusions
Marked changes in functionally relevant molecules in schizophrenia point to a pivotal role for extracellular matrix–glial interactions in the pathogenesis of this disease. Disruption of these interactions, unsuspected thus far, may represent a unifying factor contributing to disturbances of neuronal migration, synaptic connectivity, and GABAergic, glutamatergic, and dopaminergic neurotransmission in schizophrenia. The lack of CSPG abnormalities in bipolar disorder points to a distinctive aspect of the pathophysiology of schizophrenia in key medial temporal lobe regions.
The involvement in schizophrenia of specific neurotransmitter/neuronalsystems such as the glutamatergic, GABA (γ-aminobutyric acid)–ergic, and dopaminergic systems is well established.1–3 Emerging evidence also points to abnormalities affecting glial cells, particularly oligodendrocytes and astrocytes.4,5 Decreased expression of the extracellular matrix (ECM) glycoprotein reelin and abnormalities in a number of ECM-related molecules have also been described in schizophrenia, raising the possibility that interactions between cellular and ECM abnormalities may play a role in the pathogenesis of this disease.6–8
The neural ECM has a unique molecular composition, with a hyaluronic acid scaffold associated with glycoproteins and proteoglycans that regulate its molecular properties. Chondroitin sulfate proteoglycans (CSPGs), one of the main components of the brain ECM, are thought to function as organizers of the neural ECM9 and constitute one of the main components of perineuronal nets (PNNs), ECM aggregates enveloping neuronal soma and dendrites and known to play a crucial role in the regulation of neuronal functions in adults.9,10 The CSPGs are synthesized by several neuronal and glial cell populations and subsequently secreted into the ECM. We have shown that a subpopulation of astrocytes in the human amygdala expresses CSPGs.11
Several key CSPG functions bear direct relevance to the pathophysiology of schizophrenia. Neuronal migration, one of the main known CSPG functions during development, is thought to be affected in this disease.12 Regulatory CSPG functions over synaptic maturation and stabilization, neural circuit formation, and structural plasticity10 resonate with hypotheses postulating a disruption of connectivity and synaptic functions in schizophrenia. The PNNs predominantly surround neurons that express parvalbumin (PVB), which are affected in schizophrenia.13 Finally, interactions between CSPGs and the glutamatergic, GABAergic, and dopaminergic systems include CSPG guidance of dopaminergic axons, PNN regulation of the physiological properties of PVB-positive neurons as well as glutamatergic and GABAergic modulation of CSPG expression and PNN formation.14,15
The involvement of CSPGs in the pathogenesis of schizophrenia has not been investigated thus far. In this postmortem study, we tested the hypothesis that schizophrenia may be associated with CSPG abnormalities in the amygdala and entorhinal cortex (ECx), 2 regions known to be affected in this disorder16–19 and in which the relationships between PVB-positive neurons, PNNs, CSPG-positive glial cells, and astrocytes have been extensively investigated in humans.11,17,20–23 To assess the involvement of glial cells in CSPG abnormalities, we measured numerical densities of CSPG-positive glial cells. Because in the normal amygdala virtually all CSPG-positive cells also expressed glial fibrillary acidic protein (GFAP),11 numerical densities of GFAP-positive astrocytes were quantified to confirm that increased numerical densities of CSPG-positive glial cells do not reflect astrocytosis. To test whether increases in CSPG-positive glial cells are associated with CSPG changes within the ECM, we measured numerical densities of PNNs. Total numbers of PVB-positive neurons were measured in the deep amygdala nuclei21 to determine whether PNN changes reflect ECM abnormalities or loss of PNN-associated neurons. A group of subjects with bipolar disorder was included to test whether CSPG abnormalities are specific to schizophrenia or represent a feature shared among major psychoses. Expression of versican, aggrecan, brevican, neurocan, and phosphacan messenger RNA (mRNA), encoding for 5 of the CSPGs most commonly expressed in the neural ECM, was measured in the basal nucleus of the amygdala (BN) in a separate cohort of control and schizophrenic subjects.
METHODS
HUMAN SUBJECTS
Tissue blocks containing the whole amygdala and ECx from 11 donors with schizophrenia, 11 with bipolar disorder, and 15 control donors were used for histochemical and immunocytochemical investigations. Additional tissue blocks from 10 healthy control and 10 schizophrenic subjects were used for quantitative real-time polymerase chain reaction (qRT-PCR). All tissue blocks were obtained from the Harvard Brain Tissue Resource Center, McLean Hospital, Belmont, Massachusetts (Table 1 and Table 2; eTable 1 and eTable 2; http://www.archgenpsychiatry.com). Diagnoses were made by retrospective review of medical records and an extensive questionnaire about social and medical history provided by family members of the donor. Two psychiatrists reviewed all records and applied the criteria of Feighner et al25 for the diagnosis of schizophrenia and DSM-III-R for the diagnosis of bipolar disorder. Several regions from each brain were examined by a neuropathologist. The cohort used for this study did not include subjects with neuropathological or clinical evidence of gross and/or macroscopic brain changes consistent with Alzheimer disease, cerebrovascular accident, or lacking sufficient medical records. A modified Bielchowsky stain was used to test for Alzheimer disease. Subjects with Braak stages III or higher were not included in our cohort.
Table 1.
Sample Demographic and Descriptive Characteristics of the Cohort Used for Histochemical and Immunocytochemical Studies
| Subject Code/Sex/Age, y | PMI, h | Cause of Death | Hemisphere | Brain Weight, g | Storage time, mo |
|---|---|---|---|---|---|
| Schizophrenia | |||||
| Subject | |||||
| 20/M/49 | 19.1 | Suicide, hanging | Left | 1440 | 55 |
| 1/M/62 | 25.3 | Sepsis | Left | 1340 | 15 |
| 32/M/32 | 7.8 | Cardiac arrest | Right | 1400 | 56 |
| 38/M/55 | 21.4 | Cardiac arrest | Right | 1380 | 61 |
| 4/F/60 | 19.6 | Cancer | Right | 1220 | 61 |
| 42/F/92 | 17.8 | Cardiac arrest | Left | 1120 | 53 |
| 15/F/73 | 24.0 | Cancer | Right | 1170 | 52 |
| 18/F/48 | 33.8 | Cardiac arrest | Left | 1330 | 71 |
| 7/F/82 | 23.9 | Cancer | Left | 1110 | 68 |
| 22/F/72 | 21.8 | Cancer | Right | 1065 | 46 |
| 13/F/61 | 14.1 | Pneumonia | Right | 1200 | 50 |
| Total (mean [SD]) | |||||
| 4 M, 7 F (62.3 [16.8]) | (20.7 [6.6]) | 5 Left, 6 Right | (1252.2 [130.5]) | (53.45 [14.8]) | |
|
| |||||
| Bipolar Disorder | |||||
| Subject | |||||
| 12/M/42 | 23.2 | Cardiac arrest | Right | 1360 | 38 |
| 17/F/76 | 22.8 | Cardiac arrest | Left | 1170 | 70 |
| 3/M/74 | 24.8 | Pneumonia | Left | 1270 | 68 |
| 6/F/73 | 17.0 | Cancer | Right | 1020 | 47 |
| 9/M/83 | 17.5 | Sepsis | Right | 860 | 37 |
| 37/M/73 | 7.2 | Pneumonia | Left | 1190 | 66 |
| 34/M/25 | 12.6 | Pulmonary failure | Left | 1480 | 61 |
| 30/M/66 | 17.4 | Pneumonia | Left | 1480 | 61 |
| 26/F/73 | 20.8 | Kidney failure | Right | 1060 | 52 |
| 46/F/75 | 36.0 | Cardiac arrest | Right | 1310 | 51 |
| 29/M/74 | 14.2 | Pneumonia | Right | 1340 | 50 |
| Total (mean [SD]) | |||||
| 7 M, 4 F (66.7 [17.3]) | (19.4 [7.5]) | 5 Left, 6 Right | (1230.9 [194.1]) | (54.63 [11.5]) | |
|
| |||||
| Controls | |||||
| Subject | |||||
| 5/F/68 | 14.8 | Cardiac arrest | Left | 1330 | 71 |
| 2/M/70 | 23.2 | Cardiac arrest | Left | 1360 | 71 |
| 19/M/52 | 32.1 | Cardiac arrest | Left | … | 66 |
| 25/M/71 | 24.0 | Cardiac arrest | Left | 1580 | 65 |
| 11/M/37 | 18.8 | Electrocution | Right | 1460 | 64 |
| 31/M/65 | 17.3 | Cardiac arrest | Left | 1240 | 64 |
| 21/F/53 | 24.0 | Melanoma | Right | 1330 | 62 |
| 23/M/62 | 29.2 | Cardiac arrest | Left | 1300 | 62 |
| 36/M/70 | 17.3 | Aortic aneurism | Left | 1400 | 62 |
| 14/F/58 | 17.8 | Cancer | Right | 1345 | 58 |
| 16/M/72 | 28.2 | Cardiac arrest | Right | 1560 | 52 |
| 35/F/74 | 12.1 | Cancer | Right | 1145 | 45 |
| 28/M/74 | 15.8 | Cardiac arrest | Left | 1490 | 38 |
| 43/M/85 | 20.3 | Cancer | Left | 1225 | 46 |
| 8/F/78 | 23.9 | Cancer | Right | 1100 | 46 |
| Total | |||||
| 10 M, 5 F (65.9 [12.0]) | (21.2 [5.7]) | 9 Left, 6 Right | (1347.5 [143.2]) | (58.13 [10.2]) | |
Abbreviation: PMI, postmortem interval.
Table 2.
Disease-Related Descriptive Characteristics of the Cohort Used for Histochemical and Immunocytochemical Studiesa
| Subject Code | Age at Onset, y | Duration of Illness, y | LT CPZ, g | 6-mo CPZg | LT LI, g | 6-mo LI, g | SSRIs | VPA, g | ECTb | Nicotineb | Ethanolb | Drugs of Abuse |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Schizophrenia | ||||||||||||
| 20 | 19 | 30 | 801.5 | 36.0 | 0 | 0 | No | 913.1 | 2 | 1 | 3 | LSD, amphetamines |
| 1 | 31 | 31 | 1169.0 | 162.0 | 0 | 0 | Yes | 1370 | 0 | 0 | 3 | None |
| 32 | 16 | 16 | 671.2 | 30.38 | 0 | 0 | No | 0 | 0 | 3 | 2 | Cocaine, marijuana |
| 38 | 35 | 20 | 792.6 | 27.0 | 0 | 0 | No | 0 | 0 | 1 | 0 | None |
| 4 | 38 | 22 | 365.2 | 23.55 | 0 | 0 | Yes | 0 | 0 | 1 | 0 | None |
| 42 | 24 | 68 | 0 | 0 | 0 | 0 | No | 0 | 0 | 0 | 0 | None |
| 15 | 22 | 51 | 497.7 | 23.55 | 0 | 0 | Yes | 0 | 4 | 3 | 0 | None |
| 18 | 17 | 31 | 771.6 | 0 | 3287 | 0 | No | 0 | 0 | 1 | 0 | None |
| 7 | NK | NK | 0 | 0 | 0 | 0 | No | 0 | 0 | 0 | 0 | None |
| 22 | 24 | 48 | 420.0 | 31.5 | 0 | 0 | Yes | 0 | 0 | 1 | 1 | None |
| 13 | 20 | 41 | 3550.0 | 36.18 | 0 | 0 | Yes | 0 | 3 | 2 | 1 | Amphetamines |
| Mean (SD) | 24.6 (7.6) | (32.5 (18.7) | 821.0 (970.3) | 33.6 (44.8) | ||||||||
|
| ||||||||||||
| Bipolar Disorder | ||||||||||||
| 12 | 32 | 10 | 0 | 0 | 0 | 0 | No | 0 | 0 | 1 | 0 | None |
| 17 | 67 | 9 | 77.9 | 2.7 | 1321.0 | 27 | No | 0 | 0 | 4 | 4 | None |
| 3 | 52 | 22 | 102.5 | 29.25 | 3945.0 | 0 | No | 547.9 | 0 | 1 | 0 | None |
| 6 | 35 | 38 | 82.2 | 20.25 | 2191.5 | 0 | No | 182.6 | 0 | 0 | 0 | None |
| 9 | 43 | 40 | 0 | 0 | 2191.5 | 0 | Yes | 803.6 | 0 | 0 | 0 | None |
| 37 | 30 | 43 | 10.8 | 3.6 | 0 | 0 | No | 0 | 0 | 1 | 0 | None |
| 34 | 15 | 10 | 328.7 | 90 | 3945.0 | 216 | Yes | 0 | 0 | 3 | 4 | Heroin, marijuana |
| 30 | 35 | 31 | 731.3 | 1.0 | 1096.0 | 54 | No | 0 | 0 | 4 | 0 | None |
| 26 | 20 | 53 | 202.7 | 13.95 | 4273.0 | 0 | No | 0 | 0 | 1 | 0 | None |
| 46 | 27 | 48 | 0 | 0 | 0 | 0 | No | 0 | 0 | 1 | 0 | None |
| 29 | 18 | 56 | 2842.0 | 20.0 | 2192.0 | 54 | No | 2739.0 | 2 | 4 | 0 | None |
| Mean (SD) | 34.0 (15.4) | 32.7 (17.5) | 398.0 (839.3) | 16.4 (26.4) | 1923.1 (1614.1) | 31.9 (64.8) | ||||||
Abbreviations: 6-mo CPZ, chlorpromazine-equivalent dose of antipsychotics during last 6 months of life; ECT, electroconvulsive therapy; 6-mo LI, total grams of lithium during the last 6 months of life; LSD, lysergic acid diethylamide; LT CPZ, CPZ-equivalent dose of antipsychotics during the subject’s lifetime; LT LI, total grams of LI during subject’s lifetime; NK, not known; SSRI, selective serotonin-reuptake inhibitor; VPA, valproic acid use over the subject’s lifetime.
We analyzed medical records for exposure to various classes of psychotropic and neurotropic drugs. Estimated daily milligram doses of antipsychotic drugs were converted to the approximate equivalent of chlorpromazine as a standard comparator24 and corrected on the basis of a qualitative assessment of treatment adherence based on taking prescribed psychotropic medicines more or less than approximately half of the time, as indicated by the extensive antemortem clinical records. Exposure to lithium salt was estimated in the same manner.
Data on nicotine and alcohol exposure were only available for subjects with schizophrenia or bipolar disorder; on the basis of the subjects’ records, exposure was considered absent, low, moderate, or high (rated on a scale of 1–4) as well as present or absent during the last 10 years of life.
TISSUE PROCESSING AND HISTOCHEMICAL/IMMUNOCYTOCHEMICAL PROCEDURES
Tissue blocks for histochemistry/immunocytochemistry were processed as previously described.21,26 All sections (40 μm) within a compartment per subject were selected for each marker (ie, PVB, GFAP, CSPG), thus respecting the equal opportunity rule.27,28 Histochemical labeling for CSPGs was obtained using biotinylated Wisteria floribunda agglutinin (WFA) as described previously.11 Wisteria floribunda agglutinin selectively binds to N-acetyl-galactosamine,29–32 a molecule specifically represented in the glycosaminoglycan chains characteristic of CSPGs.33 Immunocytochemical detection of GFAP and PVB was performed as previously described 11,21 using a monoclonal primary antisera raised in mouse against GFAP (1:8000 μL, G 3893; Sigma-Aldrich, St Louis, Missouri) and a monoclonal anti-PVB antibody (48 hours at 4°C, 1:10 000, P3088; Sigma-Aldrich), respectively. All sections were coverslipped and coded for quantitative analysis blinded to diagnosis. Sections from all brains included in the study were processed simultaneously to avoid procedural differences. Omission of streptavidin or bio-tinylated WFA, or replacement of biotinylated WFA with an unconjugated form (Vector Laboratories, Burlingame, California), or omission of the primary (GFAP or PVB) or secondary antibodies did not result in detectable signal.
CHONDROITINASE ABC DIGESTION
Following antigen unmasking with citric acid buffer, as above, sections were incubated overnight at 37°C in chondroitinase buffer (1:8 chondroitinase ABC, 10 mU/μL, C-2905 [Sigma-Aldrich] in 50mM Tris, pH 8.0, 60mM sodium acetate, 0.02% bovine albumin serum). Sections were then rinsed in phosphate buffer and processed for WFA histochemistry.
QUALITATIVE REAL-TIME POLYMERASE CHAIN REACTION
Levels of mRNA coding for the CSPGs versican, brevican, neurocan, aggrecan, and phosphacan were measured in tissue samples of the BN using standard qRT-PCR assay (supplementary Methods are available at http://www.archgenpsychiatry.com).
DATA COLLECTION
Numerical densities of WFA-positive glial cells and PNNs were assessed in the lateral (LN), BN, accessory basal (AB), and cortical (CO) nuclei of the amygdala and the lateral (ECx-L), rostral (ECx-R), intermediate (ECx-I), and caudal (ECx-C) subregions of the ECx (subdivided into 6 cortical layers) and identified on the basis of morphological criteria (eFigure 1, B and C; http://www.archgenpsychiatry.com). Astrocytes expressing GFAP (eFigure 1D) were counted in the LN, BN, ABN, and CO and layer II of all ECx subdivisions. The other ECx layers were not considered for GFAP counts because changes in CSPG-positive glial cells were only detected in layer II. Total numbers and numerical densities of PVB-positive neurons were assessed in all amygdalar subdivisions. A Zeiss Axioskop 2 Plus (Carl Zeiss MicroImaging Inc, Thornwood, New York) interfaced with StereoInvestigator 6.0 (Microbrightfield Inc, Williston, Vermont) was used for analysis. Intrarater reliability of at least 95% was established before the actual quantification process was begun and assessed on a regular basis throughout the quantification process (H.P.). Each traced region was systematically scanned through the full x-, y-, and zaxes to count each PVB-, WFA-, and GFAP-labeled element within the traced borders of each amygdala nucleus and ECx subdivision/layer.
Amygdala
The borders of the LN, BN, AB, and CO nuclei of the amygdala (Figure 1) were identified in sections counterstained with methyl green nuclear stain (WFA labeled sections) and adjacent Nissl-stained sections according to cytoarchitectonic criteria as described by Amaral et al34 and Sims and Williams.35 The nomenclature adopted was that used by Sorvari et al.36 The intercalated cell masses were not included within the borders of these nuclei. The paralaminar nucleus could not be distinguished reliably from the ventral BN and was included within its borders. The central, medial, and anterior nuclei could not be considered in quantitative investigations because their dorsomedial portion was damaged in a number of samples. Glial cells and PNNs labeled with WFA and GFAP-immunoreactive (IR) cells were counted in 4 sections per subject, selected across the rostral to caudal extent of the amygdala. Particular care was taken to match the rostro-caudal level of each section across all subjects according exclusively to well-identifiable morphological and cytoarchitectonic criteria and under conditions strictly blind to diagnosis. Neurons expressing PVB were counted over complete sets of serial sections (6–10 sections) representing the whole extent of the amygdala from each subject (section interval, 1040 μm).
Figure 1.
Marked increase in Wisteria floribunda agglutinin (WFA)–labeled elements in subjects with schizophrenia. Photographic composites show sample coronal sections, labeled histochemically with WFA (black reaction product), containing the amygdala nuclei and entorhinal cortex (ECx) from a healthy control subject (A) and a subject with schizophrenia (B). Note the markedly increased WFA labeling in the subject with schizophrenia. Dashed lines (A) indicate the borders of each region. C, A detailed image of the regions is shown. E and D, Photomicrographs show a portion of the superficial layers of the ECx (segment shown in E corresponds to that marked by arrows in B). F, G, H, and I, Portions of the superficial layers of lateral ECx are shown for matched pairs of healthy controls and subjects with schizophrenia. Note the distribution of perineuronal nets in the control subjects, which is typically more dorsal with respect to WFA-labeled glial cells. AA indicates anterior nucleus of the amygdala; ABN, accessory basal nucleus of the amygdala; BN, basal nucleus of the amygdala; CE, central nucleus of the amygdala; CO, cortical nucleus of the amygdala; HP, hippocampus; LN, lateral nucleus of the amygdala; LV, lateral ventrical; PRCx, perirhinal cortex.
Entorhinal Cortex
Entorhinal cortex subdivisions were identified in 3 sections per subject according to the well-established criteria of Insausti et al21,37 and under conditions strictly blind to diagnosis. Briefly, the most rostral section included the ECx-R and the rostral portion of the ECx-L. The middle section contained the ECx-I and the caudal portion of the ECx-L. The third, most caudal section contained the ECx-C and was located rostrally to the transitional zone that defines the distinct features of the caudal limiting subdivision of the ECx. Within these subdivisions, cortical layers were identified according to the criteria of Insausti et al.37 Particular care was taken to match the rostro-caudal level of each section across all subjects.
NUMERICAL DENSITIES AND TOTAL NUMBER ESTIMATES
Total number (N) of PVB-IR neurons was calculated as N = i × Σn, where Σn is the sum of the cells counted in each subject and i is the section interval (ie, number of serial sections between each section and the next within each compartment, ie 26).26 Numerical densities of PVB were calculated as Nv= ΣN/ΣV, where V is the volume of each amygdala nucleus, calculated as V = z × ssf × Σa, where z is the thickness of the section (40 μm), ssf is the section sampling fraction (1/13; ie, number of serial sections between each section and the following one within a compartment), and a is the area of the region of interest (eg, amygdala nucleus or ECx subdivision or layer).
Numerical densities (Nv) of GFAP-positive cells and WFA-labeled glial cells and PNNs were calculated as Nv=Σn/Vs, where Σn is the sum of the number of neurons counted in a subregion and Vs the fraction of volume of each subregion contained within the each section examined (Vs= z × as, where as is the surface area of the subregion examined within a section).
STATISTICAL ANALYSIS
Differences between groups relative to the main outcome measures in each of the regions examined were assessed for statistical significance using a stepwise linear regression process. A logarithmic transformation was uniformly applied to all original values because the data were not normally distributed. Statistical analyses were performed using JMP v5.0.1a (SAS Institute Inc, Cary, North Carolina). Each marker and region combination was treated as a univariate outcome; thus, our results are to be interpreted separately for each combination. We first fit the most complex linear model with diagnoses and all covariates. These models are analyses of covariance, ie, analyses of variance models for the diagnostic effects that also account simultaneously for the possible effects of the other covariates. We then used model selection criteria based on likelihood ratio tests that compared complex models with simpler models nested within them. Subjects with bipolar disorder and schizophrenia were first compared separately with healthy controls. Subsequently, the 3 groups were considered together to test for differences between diagnostic groups and Bonferroni corrected for multiple comparisons. Age, sex, postmortem time interval, hemisphere, cause of death (acute, eg, myocardial infarction or chronic, eg, cancer), brain weight, exposure to alcohol or nicotine, electroconvulsive therapy, and lifetime and final 6 months’ exposure to antipsychotic drugs and lithium treatment were tested systematically for their effects on the main outcome measures and included in the model if they significantly improved the model goodness-of-fit. Subtypes of schizophrenia (eg, paranoid, catatonic, disorganized) and levels of functioning indexes (ie, capability of living independently, marital and employment status), could be not tested reliably because the number of subjects in each category was too low. However, these variables were taken into account as a possible explanation when apparent clustering of subjects was observed. Sensitivity analysis was performed for all models to identify potential influential observations. This analysis was intended to address potential issues relative to sample size. Each model was refit when each subject was removed and then replaced. Cronbach α was used to measure internal data consistency and reliability (0 indicates completely unreliable; 1,completely reliable), using amygdalar nuclei and ECx subdivisions as repeated measures.
RESULTS
WFA-LABELED GLIAL CELLS
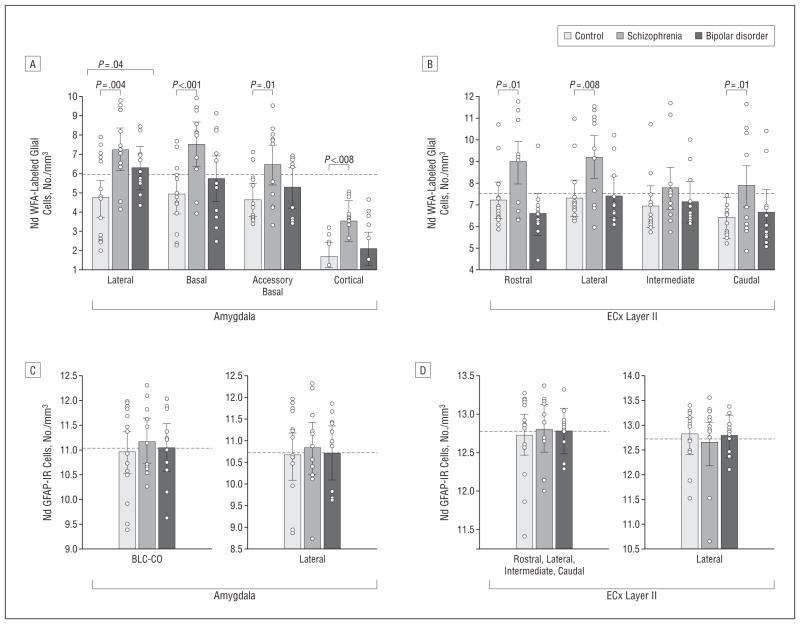
In subjects with schizophrenia, numerical densities of WFA-positive glial cells were significantly increased in the deep amygdala nuclei (LN, P=.004, 794%; BN, P<.001, 1162%; AB, P=.01, 991%; CO, P<.001, 419%) (Figure 2 and Figure 3; Table 3), as well as in layer II of the ECx-L (P=.008, 480%), ECx-R (P=.01, 586%), ECx-C (P=.02, 567%), and layer III of the ECx-L (P = .03, 1560%) (Figures 1, 2, and 3, A and C; Table 3). No changes were detected in other ECx layers. Sensitivity analyses show that the significance of the diagnostic effect for amygdala nuclei varied from .001 to .01 for LN, <.001 to .004 for BN, .002 to .03 for ABN, and <.001 to .002 for CO, all well below .05. Blind subjective observations suggest that numbers of WFA-positive glial cells are also massively increased in the superficial amygdala nuclei, particularly in the anterior, central, and medial nuclei (Figure 1). Quantitative assessments in the superficial nuclei could not be performed reliably because some samples did not include their mediodorsal portion.
Figure 2.
Wisteria floribunda agglutinin (WFA)–labeled glial cells are increased in deep amygdala nuclei and entorhinal cortex (ECx) (layer II) in subjects with schizophrenia. Numerical densities (Nd) (cells/mm3; logarithmic transformation) of WFA-labeled glial cells (A and B) and glial fibrillary acidic protein (GFAP)–positive cells (C and D) in deep amygdala nuclei (A and C) and ECx (layer II; B and D) of control subjects and subjects with schizophrenia and bipolar disorder. Significance values are derived from a stepwise linear regression process. Scatterplots show the mean (bar) and 95% confidence intervals of the mean (error bars); dashed lines represent the total response sample mean. IR indicates immunoreactive.
Figure 3.
Enzymatic treatment with chondroitinase ABC eliminates Wisteria floribunda agglutinin (WFA) labeling in perineuronal nets (PNNs) and glial cells. Photomicrographs show neuronal clusters in layer II of the entorhinal cortex in sections processed for WFA (black reaction product) and counterstained in a control subject (A and B) and a subject with schizophrenia (C and D). B and D, Sections were treated with chondroitinase ABC prior to WFA histochemistry. This treatment ablated WFA labeling of PNNs and glial cells. Note that in the untreated control (A), WFA mainly labeled PNNs (arrow) while WFA-positive glial cells are less frequent. In the untreated sections from a subject with schizophrenia (C), PNNs are reduced, while WFA-labeled glial cells (arrow) are increased.
Table 3.
Numerical Densities of WFA-Labeled Glial Cells in Deep Amygdala Nuclei and ECxa
| Brain Region | Controls
|
Schizophrenia
|
Bipolar Disorder
|
||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean (SD) Nv, Cells/mm3 | Mean (SD) Nv, Cells/mm3 | Difference, % | F Ratio | P Value | Mean (SD) Nv, Cells/mm3 | Difference, % | F Ratio | P Value | |
| Amygdala nucleus | |||||||||
| Lateral | 13.22 (19.90) | 118.28 (159.89) | 794.4 | 9.81 | .004 | 28.07 (37.52) | 112.2 | 3.59 | .04 |
| Basal | 9.91 (15.22) | 124.88 (148.21) | 1162.0 | 31.31 | 3.001b | 43.37 (69.91) | 337.5 | 1.61 | .28 |
| Accessory basal | 5.11 (7.08) | 55.84 (86.12) | 990.9 | 8.19 | .01 | 10.43 (9.58) | 103.8 | 1.67 | .26 |
| Cortical | 11.39 (11.74) | 59.08 (45.33) | 418.9 | 15.58 | 3.001 | 20.26 (29.72) | 77.9 | 0.73 | .46 |
| ECx subdivisions | |||||||||
| ECx-L II | 137.49 (346.55) | 798.21 (864.23) | 480.3 | 8.29 | .008 | 111.07 (196.81) | −19.2 | 0.02 | .89 |
| ECx-L III | 5.86 (1.81) | 80.68 (231.37) | 1559.7 | 5.43 | .03c | 6.50 (5.99) | −50.6 | 5.73 | .02c |
| ECx-L IV/V | 45.49 (27.07) | 56.53 (55.22) | 24.2 | 0.46 | .71 | 31.49 (18.14) | −30.7 | 2.45 | .13 |
| ECx-L VI | 7.30 (2.43) | 7.68 (2.54) | 5.1 | 1.50 | .74 | 5.85 (1.69) | −19.9 | 2.84 | .11 |
| ECx-R II | 114.59 (272.18) | 786.45 (1043.34) | 586.3 | 7.13 | .01 | 50.92 (115.90) | −55.5 | 1.29 | .25 |
| ECx-R III | 16.16 (37.72) | 91.44 (240.27) | 465.8 | 0.61 | .63 | 10.08 (11.59) | −37.5 | 1.09 | .34 |
| ECx-R IV/V | 37.71 (24.22) | 31.85 (12.48) | −15.5 | 0.04 | .85 | 39.12 (44.99) | 3.7 | 0.11 | .74 |
| ECx-R VI | 7.68 (3.98) | 8.02 (2.23) | 4.4 | 0.46 | .48 | 6.33 (2.49) | −17.6 | 0.99 | .33 |
| ECx-I II | 98.89 (266.73) | 453.76 (929.38) | 338.6 | 1.70 | .20 | 86.49 (155.01) | −12.5 | 0.19 | .66 |
| ECx-I III | 25.99 (68.54) | 96.77 (199.69) | 272.1 | 0.97 | .48 | 24.45 (38.44) | −5.9 | 0.22 | .94 |
| ECx-I IV/V | 36.68 (19.94) | 33.69 (20.53) | −8.16 | 0.09 | .77 | 33.92 (16.83) | −7.5 | 0.04 | .86 |
| ECx-I VI | 9.71 (5.62) | 8.61 (2.67) | −11.27 | 0.07 | .81 | 9.15 (7.94) | −5.7 | 0.29 | .58 |
| ECx-C II | 67.82 (209.96) | 452.54 (826.89) | 567.2 | 6.63 | .02c | 107.25 (237.28) | 58.1 | 0.18 | .70 |
| ECx-C III | 7.69 (17.96) | 85.34 (257.14) | 1009.9 | 1.22 | .28 | 4.92 (5.59) | −35.9 | 0.05 | .77 |
| ECx-C IV/V | 21.69 (15.36) | 40.49 (65.07) | 86.6 | 0.88 | .36 | 25.32 (19.32) | 16.7 | 0.19 | .68 |
| ECx-C VI | 5.79 (4.53) | 32.94 (62.77) | 468.2 | 2.42 | .13 | 8.11 (10.47) | 39.9 | 0.25 | .65 |
Abbreviations: ECx-C, caudal entorhinal cortex (roman numerals correspond to the layer); ECx-I, intermediate ECx; ECX-L, lateral ECx; ECx-R, rostral ECx; Nv, numerical density; WFA, Wisteria floribunda agglutinin.
Significance values were derived from stepwise regression models. Significance values and percentage of difference refer to comparisons with the control group. Degrees of freedom are 1, 25, except where modified for significant covariate effects.
Significance values for the basal nucleus were adjusted for the effects of lifetime exposure to antipsychotics (chlorpromazine equivalent; F = 9.12; P = .006) and postmortem time interval (F = 8.82; P = .007); for ECx-L layer III, effects of age (F = 4.88; P = .04) and age × diagnosis (F = 4.93; P = .04); and for layer II ECx-C, effect of age (F = 5.66; P = .03). No covariates were found to have significant effects and to improve the goodness of fit of the model.
Adjusted for effect of lifetime exposure to lithium (F = 6.71; P = .02).
In subjects with bipolar disorder, a more modest increase of WFA-positive glial cells was detected only in the LN (P = .04, 112%). In the ECx, WFA-positive glial cells were decreased in layer III of the ECx-L (P = .02, −51%) (Figure 2; Table 3).
GFAP-POSITIVE GLIAL CELLS
No significant changes were detected in the schizophrenia and bipolar disorder groups compared with controls in any of the subdivisions and layers examined (Figure 3; eTable 3).
PERINEURONAL NETS
In subjects with schizophrenia, numerical densities of PNNs were markedly decreased in the LN (62%; P=.01) and layer II of ECx-L (P=.004; 65%) (Figure 4; Table 4). In subjects with bipolar disorder, the numerical density of PNNs was decreased only in layer II of ECx-C (P=.04; 54%) (Figure 4; Table 4). Notably, in healthy human subjects, LN and ECx superficial layers contain by far the highest densities of PNNs.20,22 Thus, lack of PNN changes in amygdalar and ECx subdivisions other than the LN and ECx superficial layers is to be expected, even in the presence of more encompassing CSPG-positive glial abnormalities.
Figure 4.
Wisteria floribunda agglutinin (WFA)–labeled perineuronal nets (PNNs) are decreased in the lateral nucleus and layer II of the lateral entorhinal cortex (ECx-L) in subjects with schizophrenia. Numerical densities (Nd) (cells/mm3) of WFA-labeled PNNs (A and B) and numerical densities and total numbers of parvalbumin-positive neurons in the amygdala (C and D). Logarithmic transformation was applied to all values. Significance values are derived using stepwise linear regression process. Scatter plots show the mean (bar) and 95% confidence intervals of the mean (error bars); dashed lines represent the total response sample mean. IR indicates immunoreactive.
Table 4.
Numerical Densities of PNNs in Deep Amygdala Nuclei and ECxa
| Brain Region | Control
|
Schizophrenia
|
Bipolar Disorder
|
||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean (SD) Nv, Cells/mm3 | Mean (SD) Nv, Cells/mm3 | Difference, % | F Ratio | P Value | Mean (SD) Nv, Cells/mm3 | Difference, % | F Ratio | P Value | |
| Amygdala nucleus | |||||||||
| Lateral | 50.15 (32.74) | 19.15 (14.80) | −61.8 | 6.90 | .02 | 30.48 (27.36) | −39.2 | 1.61 | .22 |
| Basal | 11.23 (8.73) | 6.99 (19.27) | −37.7 | 2.84 | .15 | 9.13 (17.21) | −18.7 | 1.18 | .29 |
| Accessory basal | 8.79 (12.20) | 11.99 (20.87) | 36.4 | 0.01 | .94 | 6.69 (10.56) | −23.8 | 0.77 | .31 |
| Cortical | 11.34 (5.41) | 15.66 (16.10) | 38.0 | 2.18 | .15 | 12.91 (17.67) | 13.8 | 1.46 | .11 |
| ECx subdivisions | |||||||||
| ECx-L II | 209.16 (157.93) | 72.99 (89.36 | −65.1 | 9.69 | .004 | 139.45 (147.64) | −33.3 | 0.98 | .36 |
| ECx-L III | 279.48 (154.85) | 218.25 (240.55) | −21.9 | 0.92 | .34 | 242.11 (157.06) | −13.3 | 0.27 | .60 |
| ECx-L IV/V | 87.40 (53.09) | 107.90 (73.44) | 23.4 | 0.20 | .66 | 84.73 (99.31) | −3.0 | 0.91 | .34 |
| ECx-L VI | 104.49 (94.41) | 91.89 (127.34) | −12.0 | 0.31 | .56 | 121.36 (127.09) | 16.1 | 0.01 | .93 |
| ECx-R II | 381.10 (408.65) | 123.07 (120.43) | −67.7 | 3.17 | .09 | 118.81 (114.17) | −68.8 | 2.66 | .12 |
| ECx-R III | 347.24 (305.36) | 124.41 (181.23) | −64.1 | 2.78 | .11 | 333.31 (622.48) | −4.0 | 1.09 | .31 |
| ECx-R IV/V | 114.92 (99.23) | 52.53 (61.99) | −54.2 | 0.09 | .77 | 59.59 (53.59) | −48.1 | 2.18 | .15 |
| ECx-R VI | 85.94 (111.58) | 102.73 (154.04) | 19.5 | 0.06 | .8 | 138.01 (240.78) | 60.5 | 3.65 | .07 |
| ECx-I II | 291.13 (331.02) | 156.37 (216.28) | −46.2 | 2.02 | .17 | 192.65 (155.53) | −33.8 | 0.38 | .54 |
| ECx-I III | 250.19 (195.15) | 170.46 (188.58) | −31.8 | 1.76 | .20 | 273.75 (253.84) | 9.4 | 0.05 | .83 |
| ECx-I IV/V | 55.38 (48.01) | 85.61 (104.76) | 54.5 | 0.37 | .55 | 112.59 (174.28) | 103.3 | 1.30 | .27 |
| ECx-I VI | 89.27 (83.10) | 73.29 (70.14) | −17.9 | 0.27 | .6 | 285.35 (419.51) | 219.6 | 1.62 | .22 |
| ECx-C II | 428.87 (395.51) | 201.99 (189.11) | −52.9 | 0.75 | .4 | 197.60 (239.90) | −53.9 | 4.46 | .04 |
| ECx-C sIII | 334.32 (217.75) | 334.08 (284.85) | −0.07 | 0.83 | .37 | 358.81 (296.79) | 7.3 | 1.30 | .27 |
| ECx-C IV/V | 73.34 (67.55) | 104.00 (158.04) | 41.8 | 0.02 | .75 | 87.51 (83.24) | 19.3 | 0.01 | .95 |
| ECx-C VI | 103.12 (70.43) | 97.58 (106.84) | −5.3 | 0.72 | .41 | 262.10 (336.01) | 154.1 | 0.33 | .61 |
Abbreviations: ECx-C, caudal entorhinal cortex (roman numerals correspond to the layer); ECx-I, intermediate ECx; ECX-L, lateral ECx; ECx-R, rostral ECx; Nv, numerical density; PNNs, perineuronal nets.
Significance values were derived from stepwise regression models and refer to comparisons with the control group. No other covariates tested were found to have significant effects and to improve the goodness of fit of the relative models.
PVB-POSITIVE NEURONS
Numerical densities (cells/mm3) and total numbers of PVB-positive neurons were not significantly altered in the amygdalas of subjects with schizophrenia or bipolar disorder (Figure 4 and eTable 4).
EFFECTS OF CONFOUNDING VARIABLES
Schizophrenia
In the BN, significance values for CSPG-positive glial cells were adjusted for lifetime exposure to antipsychotics (P=.006; t=−3.02) and postmortem time interval (P=.007; t=−2.97) (Table 3). The negative effects of these covariates, confirmed by negative correlations with the main outcome measure, indicate that antipsychotic exposure and postmortem time interval tend to decrease CSPG-positive glial cells in BN and are, therefore, unlikely to be responsible for the observed increase. Significance values for ECx-L layer III were adjusted for the effects of age (t=2.21; P=.04) and age × diagnosis (t=2.22; P=.04), and values for layer II ECx-C were adjusted for the effect of age (t=2.38; P=.03). No covariates showed significant effects on CSPG-positive glial cells in any other amygdala and ECx subregions. None of the covariates tested showed significant effects on PNNs or PVB-IR neurons in any of the amygdala and ECx subdivisions examined (Tables 4; eTable 4). Notably, exposure to antipsychotic drugs (lifetime or last 6 months of life), electroconvulsive therapy, duration of illness, and age at illness onset did not significantly correlate with numerical densities of CSPG-positive glial cells and PNNs in subjects with schizophrenia and did not significantly affect differences between groups in stepwise linear regression models. Cause of death had a significant effect on numerical densities of GFAP-IR cells but did not affect comparisons between diagnosis groups.
Bipolar Disorder
None of the covariates considered had statistically significant effects on numerical densities of CSPG-positive glial cells in the LN. Statistical significance values for CSPG-positive cells in layer III of ECx-L were adjusted for effect of lifetime exposure to lithium (t = 2.59; P = .02). Correlations between these parameters were positive, but did not reach statistical significance, suggesting perhaps a mild corrective effect of lithium treatment. Brain weight and postmortem time interval were included as covariates in linear regression models testing the effect of diagnosis on volume of amygdala nuclei (eTable 4). No other covariates showed significant effects.
Schizophrenia and Bipolar Disorder
Values for CSPG-positive glial cells and PNNs in the schizophrenia and bipolar disorder groups (Figure 2 and Figure 4) show possibly bimodal distributions, suggesting the presence of distinct subgroups of subjects with schizophrenia and/or bipolar disorder. However, sensitivity analyses, together with a review of the medical records including exposure to antipsychotics and other psychotropic drugs, lithium salts, anticholinergic drugs, electroconvulsive therapy, response to treatment, age at onset, duration of the illness, prevalence of negative or positive symptoms, subtypes of schizophrenia, levels of functioning, exposure to alcohol, nicotine, or other drugs of abuse, and history of birth complications did not provide distinguishing features that may characterize distinct subpopulations.
DATA RELIABILITY ANALYSIS
In the amygdala, Cronbach α values were as follows: for healthy control subjects, .613; schizophrenic subjects, .842; subjects with bipolar disorder, .745; and all 3 groups combined, .864. In the ECx, Cronbach α values were .924 for healthy control subjects; .776 for schizophrenic subjects; .829 for subjects with bipolar disorder; and .860 for all 3 groups combined.
EFFECTS OF CHONDROITINASE ABC TREATMENT
Pretreatment with chondroitinase ABC, an enzyme known to degrade chondroitin sulfate glycosaminoglycan chains, ie, the binding site of WFA, abolished WFA labeling of glial cells and PNNs in the amygdala and ECx (Figure 3). Labeling with WFA of bordering epithelium and/or blood vessels, detected in a small number of subjects in each group (Figure 1), was not affected by treatment with chondroitinase ABC.
CSPG mRNA EXPRESSION IN THE BN
In the BN, the expression of mRNA coding for 5 distinct CSPGs was increased in subjects with schizophrenia compared with healthy control subjects. In particular, we detected a 2.03-fold increase in versican mRNA (P=.05); 1.52-fold, neurocan mRNA; 1.43-fold, brevican mRNA; 1.31-fold, aggrecan mRNA; and 1.55-fold, phosphacan (PTPRZ1) mRNA (eTable 5).
COMMENTS
Glial cells expressing CSPGs were massively increased in the deep nuclei of the amygdala and in ECx layer II of subjects with schizophrenia. These changes were not accompanied by increases in GFAP-positive astrocytes. Reductions of PNNs were instead detected in the LN and layer II of the ECx-L in the absence of altered PVB-positive neuron numbers, a finding consistent with CSPG anomalies within the ECM, rather than loss of PNN-associated neurons. These results point to substantial, specific anomalies affecting CSPG expression in glial cells and ECM perineuronal aggregates in schizophrenia but not bipolar disorder. The functional relevance to schizophrenia of molecules and cell populations found to be affected, combined with effect sizes unusually large for this disease (CSPG-positive glial cell increases, 419%–1560%), suggest that a glial/ECM disruption may play a fundamental role in the pathophysiology of schizophrenia.
TECHNICAL CONSIDERATIONS
In previous studies, the total number of Nissl-stained neurons and volume of the LN, BN, ABN, and CO and the volume of the ECx were not found to be altered in a largely overlapping cohort of subjects with schizophrenia.21,26 In the present study, changes in numerical densities of labeled elements, or lack thereof, in these subjects are thus not likely to be due to volumetric abnormalities. This interpretation is supported by the fact that increases, decreases, and no changes were found in the same regions of subjects with schizophrenia and that both total numbers and numerical densities of PVB-positive neurons were unaltered. In contrast to the massive increases in WFA-labeled glial cells detected in schizophrenia, subjects with bipolar disorder presented modest increases in these cells only in the LN (Table 3). The volume of this nucleus was found to be reduced in the same cohort of subjects with bipolar disorder26 (eTable 4), raising the possibility that increased numerical density of WFA-labeled glial cells in the LN of subjects with bipolar disorder may be, at least in part, an effect of volumetric reduction rather than increased numbers of CSPG-positive cells.
The lectin WFA, isolated from the seeds of Wisteria floribunda, was used to detect CSPGs. The specificity of WFA as a marker for these macromolecules is supported by extensive literature as well as the present findings.14,38–41 In this study, a subsample of sections was treated with chondroitinase ABC. This enzyme degrades the binding site of WFA and is routinely used to investigate the effects of CSPG elimination.14,42–45 Virtually complete abolition of WFA labeling following preincubation with chondroitinase ABC confirms the specificity of WFA for CSPGs and supports the claim that, in our study, WFA-positive cells correspond to cells expressing CSPGs. Further support comes from qRT-PCR results in the BN that showed increased mRNA levels for 5 of the major CSPGs expressed in the neural ECM.
We have recently shown that, in the normal human amygdala, virtually all cells with intracellular CSPG labeling also express GFAP and thus correspond to astrocytes.11 In the present study, blind subjective observations suggest that the morphological characteristics of WFA-labeled cells were homogeneous within each subject and indistinguishable between groups. While these findings suggests that astrocytes may be the main glial population affected by CSPG changes in schizophrenia, it is possible that other macroglial cell types with morphological characteristics similar to those typical of astrocytes, eg, NG2-glia,46 may also be involved. This possibility is currently being investigated.
CSPG ABNORMALITIES IN SUBJECTS WITH SCHIZOPHRENIA
In subjects with schizophrenia, increased numbers of CSPG-positive glial cells in the absence of astrocytosis may reflect induction of CSPG expression in cells that do not express these molecules constitutively or overexpression in cells normally expressing them at low levels, perhaps caused by impaired secretion, increased internalization, and/or overproduction; the latter is consistent with increased RNA expression detected in the BN. Interestingly, at least 2 growth factors found to be involved in schizophrenia, ie, epidermal growth factor and transforming growth factor–β1, have been shown to affect astrocytic CSPG expression,47–53 and the gene encoding for the CSPG phosphacan (PTPRZ1) has been recently identified as a potential schizophrenia susceptibility gene.8 Together, these findings point to dysregulation of CSPG expression in astrocytes of subjects with schizophrenia.
Such dysregulation was postulated in this study to affect the availability of CSPGs in the ECM. Decreases in PNNs, the ECM form most extensively studied in adults, support this hypothesis and suggest reduced CSPG levels in the ECM of subjects with schizophrenia. Abnormalities relative to CSPG-positive glial cells and PNNs did not vary with duration of illness or age at onset of illness, indicating that they do not result from nonspecific effects of chronic illness but may instead be inherent to the disease. If these abnormalities were present during development, altered CSPG availability may interfere with neuronal migration, axon outgrowth, synaptic maturation, and the formation of PNNs. Consistent with a developmental abnormality is the slow turnover and stability of mature PNNs,10 which may not be substantially affected by subsequent changes in CSPG levels. Interestingly, the organization of CSPGs into PNNs was shown to control the closure of critical periods, determining the stabilization of successful neural circuits and limiting further plasticity.45 A disruption of CSPG expression and PNN formation in schizophrenia may thus contribute to miswiring and, speculatively, to unstable, unregulated synaptic formation, undermining information processing. Impaired PNN functions in adulthood, such as modulation of neuronal excitability and gap junction transmission,14,54 may further compromise neural functions. In the adult ECM, CSPG abnormalities are also likely to alter volume transmission properties, thus affecting a range of physical and chemical signals, a notable example being dopamine.55 The pathophysiology of schizophrenia may thus result from complex interactions between neuronal, glial, and ECM components.
The expression of CSPGs is dynamically regulated by a number of physiological stimuli including neuronal activity.9,10,47,56,57 Their broad range of functions and responsivity to physiological stimuli may account for the high degree of variability in our study. Specific CSPGs also play an important role in the response to specific types of brain injuries.33,57–60 It is thus important to consider whether, in our samples, increases in CSPG-positive glial cells may be attributable to a schizophrenia-specific anomalous regulation of CSPG expression or reflect, instead, a less specific pathological state. Several considerations support the specificity of these findings. First, the control, schizophrenia, and bipolar disorder groups in this study were well matched for age (Table 1), and duration of the illness was similar for the latter 2 groups (Table 2). Second, no evidence of reactive astrocytosis was detected in this study. This result is consistent with the broadly agreed-on view that astrocytosis is not an intrinsic feature of the pathogenesis of schizophrenia.19,61–64 In particular, the occurrence of astrocytosis has been ruled out in the ECx and amygdala of subjects with this disorder.62,65,66 Third, the cohort used for our studies does not include subjects with evidence of gross and/or macroscopic brain changes and/or clinical history consistent with Alzheimer disease or cerebrovascular accidents. Lack of correlation between increases in WFA-labeled cells in schizophrenia and electroshock treatment and negative history of epilepsy in the schizophrenia group also contributed to rule out non–disease-specific factors. Fourth, the spatial distribution of WFA-labeled glial cells in schizophrenia, widespread to several regions and yet segregated within identifiable subregions in all subjects, eg, ECx layer II cell clusters (Figure 1 and Figure 3, A and C), is not consistent with the random effects of concurrent brain injuries. These considerations support the hypothesis that increases in glial cells that express CSPGs and decreases in PNNs may represent an intrinsic pathological feature of schizophrenia.
Our results provide further evidence of the involvement of the amygdala and ECx in schizophrenia. Presence of CSPG abnormalities in other medial temporal regions is consistent with the widespread distribution of the observed changes in this study (Figure 1) and is currently being investigated. As an example of the relevance the present findings may have to the pathophysiology of schizophrenia, we note that CSPG abnormalities in ECx were selective for layer II cell clusters (Figure 1 and Figure 3, A and C), matching several reports of abnormal cytoarchitecture and position of these cell clusters in schizophrenia67 that are thought to arise from migrational disturbances.68 We postulate that CSPG abnormalities may contribute to disruption of ECx and amygdalar functions, resulting in cognitive impairment, reduction of emotional expression and perception, and increased emotional reactivity, anxiety, and arousal in subjects with schizophrenia.17,69–71
In conclusion, we report massive CSPG abnormalities in glial cells and ECM in deep amygdalar nuclei and ECx layer II cell clusters. Compelling evidence of key CSPG functions during development and adulthood suggests that these abnormalities may contribute to interdependent neuronal, glial, and ECM changes in schizophrenia as well as to pathophysiological differences between this disease and bipolar disorder.
Supplementary Material
Acknowledgments
Funding/Support: This work was funded by the National Institutes of Health grants MH066280, MH066955, and MH083222.
Footnotes
Financial Disclosure: None reported.
Author Contributions: Dr Berretta had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Previous Presentations: These results were presented in part at the Society for Neuroscience Annual Meeting; October 14-18, 2006; Atlanta, Georgia; and the 1st Schizophrenia International Research Society Conference; June 21-25, 2008; Venice, Italy.
Online-Only Material: A detailed description of Methods, the eFigure, and eTables are available at http://www.archgenpsychiatry.com.
References
- 1.Coyle JT. The glutamatergic dysfunction hypothesis for schizophrenia. Harv Rev Psychiatry. 1996;3(5):241–253. doi: 10.3109/10673229609017192. [DOI] [PubMed] [Google Scholar]
- 2.Benes FM, Berretta S. GABAergic interneurons: implications for understanding schizophrenia and bipolar disorder. Neuropsychopharmacology. 2001;25(1):1–27. doi: 10.1016/S0893-133X(01)00225-1. [DOI] [PubMed] [Google Scholar]
- 3.Carlsson A, Carlsson ML. A dopaminergic deficit hypothesis of schizophrenia: the path to discovery. Dialogues Clin Neurosci. 2006;8(1):137–142. doi: 10.31887/DCNS.2006.8.1/acarlsson. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kondziella D, Brenner E, Eyjolfsson EM, Sonnewald U. How do glial-neuronal interactions fit into current neurotransmitter hypotheses of schizophrenia? Neurochem Int. 2007;50(2):291–301. doi: 10.1016/j.neuint.2006.09.006. [DOI] [PubMed] [Google Scholar]
- 5.Halassa MM, Fellin T, Haydon PG. The tripartite synapse: roles for gliotransmission in health and disease. Trends Mol Med. 2007;13(2):54–63. doi: 10.1016/j.molmed.2006.12.005. [DOI] [PubMed] [Google Scholar]
- 6.Guidotti A, Auta J, Davis JM, Di-Giorgi-Gerevini V, Dwivedi Y, Grayson DR, Impagnatiello F, Pandey G, Pesold C, Sharma R, Uzunov D, Costa E, DiGiorgi Gerevini V. Decrease in reelin and glutamic acid decarboxylase67 (GAD67) expression in schizophrenia and bipolar disorder: a postmortem brain study [correction appears in Arch Gen Psychiatry. 2002;59(1):12] Arch Gen Psychiatry. 2000;57(11):1061–1069. doi: 10.1001/archpsyc.57.11.1061. [DOI] [PubMed] [Google Scholar]
- 7.Corfas G, Roy K, Buxbaum JD. Neuregulin 1-erbB signaling and the molecular/cellular basis of schizophrenia. Nat Neurosci. 2004;7(6):575–580. doi: 10.1038/nn1258. [DOI] [PubMed] [Google Scholar]
- 8.Buxbaum JD, Georgieva L, Young JJ, Plescia C, Kajiwara Y, Jiang Y, Moskvina V, Norton N, Peirce T, Williams H, Craddock NJ, Carroll L, Corfas G, Davis KL, Owen MJ, Harroch S, Sakurai T, O’Donovan MC. Molecular dissection of NRG1-ERBB4 signaling implicates PTPRZ1 as a potential schizophrenia susceptibility gene. Mol Psychiatry. 2008;13(2):162–172. doi: 10.1038/sj.mp.4001991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yamaguchi Y. Lecticans: organizers of the brain extracellular matrix. Cell Mol Life Sci. 2000;57(2):276–289. doi: 10.1007/PL00000690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Galtrey CM, Fawcett JW. The role of chondroitin sulfate proteoglycans in regeneration and plasticity in the central nervous system [published online ahead of print January 11, 2007] Brain Res Rev. 2007;54(1):1–18. doi: 10.1016/j.brainresrev.2006.09.006. [DOI] [PubMed] [Google Scholar]
- 11.Pantazopoulos H, Murray EA, Berretta S. Total number, distribution, and phenotype of cells expressing chondroitin sulfate proteoglycans in the normal human amygdala. Brain Res. 2008;1207:84–95. doi: 10.1016/j.brainres.2008.02.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Akbarian S, Kim JJ, Potkin SG, Hetrick WP, Bunney WE, Jr, Jones EG. Maldistribution of interstitial neurons in prefrontal white matter of the brains of schizophrenic patients. Arch Gen Psychiatry. 1996;53(5):425–436. doi: 10.1001/archpsyc.1996.01830050061010. [DOI] [PubMed] [Google Scholar]
- 13.Eyles DW, McGrath JJ, Reynolds GP. Neuronal calcium-binding proteins and schizophrenia. Schizophr Res. 2002;57(1):27–34. doi: 10.1016/s0920-9964(01)00299-7. [DOI] [PubMed] [Google Scholar]
- 14.Dityatev A, Bruckner G, Dityateva G, Grosche J, Kleene R, Schachner M. Activity-dependent formation and functions of chondroitin sulfate-rich extracellular matrix of perineuronal nets. Dev Neurobiol. 2007;67(5):570–588. doi: 10.1002/dneu.20361. [DOI] [PubMed] [Google Scholar]
- 15.Charvet I, Hemming FJ, Feuerstein C, Saxod R. Mosaic distribution of chondroitin and kera-tan sulphate in the developing rat striatum: possible involvement of proteoglycans in the organization of the nigrostriatal system. Brain Res Dev Brain Res. 1998;109(2):229–244. doi: 10.1016/s0165-3806(98)00088-1. [DOI] [PubMed] [Google Scholar]
- 16.Reynolds GP. The amygdala and the neurochemistry of schizophrenia. In: Aggleton JP, editor. The Amygdala. New York, NY: Wiley-Liss; 1992. [Google Scholar]
- 17.Aleman A, Kahn RS. Strange feelings: do amygdala abnormalities dysregulate the emotional brain in schizophrenia? Prog Neurobiol. 2005;77(5):283–298. doi: 10.1016/j.pneurobio.2005.11.005. [DOI] [PubMed] [Google Scholar]
- 18.Longson D, Deakin JF, Benes FM. Increased density of entorhinal glutamate-immunoreactive vertical fibers in schizophrenia. J Neural Transm. 1996;103(4):503–507. doi: 10.1007/BF01276423. [DOI] [PubMed] [Google Scholar]
- 19.Harrison PJ. The neuropathology of schizophrenia: a critical review of the data and their interpretation. Brain. 1999;122(pt 4):593–624. doi: 10.1093/brain/122.4.593. [DOI] [PubMed] [Google Scholar]
- 20.Pantazopoulos H, Lange N, Hassinger L, Berretta S. Subpopulations of neurons expressing parvalbumin in the human amygdala. J Comp Neurol. 2006;496(5):706–722. doi: 10.1002/cne.20961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pantazopoulos H, Lange N, Baldessarini RJ, Berretta S. Parvalbumin neurons in the entorhinal cortex of subjects diagnosed with bipolar disorder or schizophrenia. Biol Psychiatry. 2007;61(5):640–652. doi: 10.1016/j.biopsych.2006.04.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Brückner G, Hausen D, Härtig W, Drlicek M, Arendt T, Brauer K. Cortical areas abundant in extracellular matrix chondroitin sulphate proteoglycans are less affected by cytoskeletal changes in Alzheimer’s disease. Neuroscience. 1999;92(3):791–805. doi: 10.1016/s0306-4522(99)00071-8. [DOI] [PubMed] [Google Scholar]
- 23.Arnold SE. The medial temporal lobe in schizophrenia. J Neuropsychiatry Clin Neurosci. 1997;9(3):460–470. doi: 10.1176/jnp.9.3.460. [DOI] [PubMed] [Google Scholar]
- 24.Baldessarini RJ, Tarazi FI. Pharmacotherapy of psychosis and mania. In: Brunton LL, Lazo JS, Parker KL, editors. Goodman and Gilman’s the Pharmacological Basis of Therapeutics. 11. New York, NY: McGraw-Hill Press; 1995. pp. 461–500. [Google Scholar]
- 25.Feighner JP, Robins E, Guze SB, Woodruff RA, Jr, Winokur G, Munoz R. Diagnostic criteria for use in psychiatric research. Arch Gen Psychiatry. 1972;26(1):57–63. doi: 10.1001/archpsyc.1972.01750190059011. [DOI] [PubMed] [Google Scholar]
- 26.Berretta S, Pantazopoulos H, Lange N. Neuron numbers and volume of the amygdala in subjects diagnosed with bipolar disorder or schizophrenia. Biol Psychiatry. 2007;62(8):884–893. doi: 10.1016/j.biopsych.2007.04.023. [DOI] [PubMed] [Google Scholar]
- 27.Coggeshall RE, Lekan HA. Methods for determining number of cells and synapses: a case for more uniform standard of review. J Comp Neurol. 1996;364(1):6–15. doi: 10.1002/(SICI)1096-9861(19960101)364:1<6::AID-CNE2>3.0.CO;2-9. [DOI] [PubMed] [Google Scholar]
- 28.Gundersen HJ, Jensen EB, Kiêu K, Nielsen J. The efficiency of systematic sampling in stereology: reconsidered. J Microsc. 1999;193(pt 3):199–211. doi: 10.1046/j.1365-2818.1999.00457.x. [DOI] [PubMed] [Google Scholar]
- 29.Nakagawa F, Schulte BA, Spicer SS. Selective cytochemical demonstration of glycoconjugate-containing terminal N-acetylgalactosamine on some brain neurons. J Comp Neurol. 1986;243(2):280–290. doi: 10.1002/cne.902430210. [DOI] [PubMed] [Google Scholar]
- 30.Brückner G, Brauer K, Härtig W, Wolff JR, Rickmann MJ, Derouiche A, Delpech B, Girard N, Oertel WH, Reichenbach A. Perineuronal nets provide a polyanionic, glia-associated form of microenvironment around certain neurons in many parts of the rat brain. Glia. 1993;8(3):183–200. doi: 10.1002/glia.440080306. [DOI] [PubMed] [Google Scholar]
- 31.Härtig W, Brauer K, Brückner G. Wisteria floribunda agglutinin-labelled nets surround parvalbumin-containing neurons. Neuroreport. 1992;3(10):869–872. doi: 10.1097/00001756-199210000-00012. [DOI] [PubMed] [Google Scholar]
- 32.Celio MR, Spreafico R, De Biasi S, Vitellaro-Zuccarello L. Perineuronal nets: past and present. Trends Neurosci. 1998;21(12):510–515. doi: 10.1016/s0166-2236(98)01298-3. [DOI] [PubMed] [Google Scholar]
- 33.Viapiano MS, Matthews RT. From barriers to bridges: chondroitin sulfate proteoglycans in neuropathology. Trends Mol Med. 2006;12(10):488–496. doi: 10.1016/j.molmed.2006.08.007. [DOI] [PubMed] [Google Scholar]
- 34.Amaral DG, Price JL, Pitkanen A, Carmichael ST. Anatomical organization of the primate amygdaloid complex. In: Aggleton JP, editor. The Amygdala: Neurobiological Aspects of Emotion, Memory, and Mental Dysfunction. New York, NY: Wiley-Liss; 1992. [Google Scholar]
- 35.Sims KS, Williams RS. The human amygdaloid complex: a cytologic and histochemical atlas using Nissl, myelin, acetylcholinesterase and nicotinamide adenine dinucleotide phosphate di-aphorase staining. Neuroscience. 1990;36(2):449–472. doi: 10.1016/0306-4522(90)90440-f. [DOI] [PubMed] [Google Scholar]
- 36.Sorvari H, Soininen H, Paljarvi L, Karkola K, Pitkanen A. Distribution of parvalbumin-immunoreactive cells and fibers in the human amygdaloid complex. J Comp Neurol. 1995;360(2):185–212. doi: 10.1002/cne.903600202. [DOI] [PubMed] [Google Scholar]
- 37.Insausti R, Tunon T, Sobreviela T, Insausti AM, Gonzalo LM. The human entorhinal cortex: a cytoarchitectonic analysis. J Comp Neurol. 1995;355(2):171–198. doi: 10.1002/cne.903550203. [DOI] [PubMed] [Google Scholar]
- 38.Galtrey CM, Kwok JC, Carulli D, Rhodes KE, Fawcett JW. Distribution and synthesis of extracellular matrix proteoglycans, hyaluronan, link proteins and tenascin-R in the rat spinal cord. Eur J Neurosci. 2008;27(6):1373–1390. doi: 10.1111/j.1460-9568.2008.06108.x. [DOI] [PubMed] [Google Scholar]
- 39.Corvetti L, Rossi F. Degradation of chondroitin sulfate proteoglycans induces sprouting of intact Purkinje axons in the cerebellum of the adult rat. J Neurosci. 2005;25(31):7150–7158. doi: 10.1523/JNEUROSCI.0683-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Carulli D, Rhodes KE, Fawcett JW. Upregulation of aggrecan, link protein 1, and hyaluronan synthases during formation of perineuronal nets in the rat cerebellum. J Comp Neurol. 2007;501(1):83–94. doi: 10.1002/cne.21231. [DOI] [PubMed] [Google Scholar]
- 41.Härtig W, Brauer K, Bigl V, Brückner G. Chondroitin sulfate proteoglycan-immunoreactivity of lectin-labeled perineuronal nets around parvalbumin-containing neurons. Brain Res. 1994;635(1–2):307–311. doi: 10.1016/0006-8993(94)91452-4. [DOI] [PubMed] [Google Scholar]
- 42.Sugahara K, Shigeno K, Masuda M, Fujii N, Kurosaka A, Takeda K. Structural studies on the chondroitinase ABC-resistant sulfated tetrasaccharides isolated from various chondroitin sulfate isomers. Carbohydr Res. 1994;255:145–163. doi: 10.1016/s0008-6215(00)90976-5. [DOI] [PubMed] [Google Scholar]
- 43.Hamai A, Hashimoto N, Mochizuki H, Kato F, Makiguchi Y, Horie K, Suzuki S. Two distinct chondroitin sulfate ABC lyases: an endoeliminase yielding tetrasaccharides and an exoeliminase preferentially acting on oligosaccharides. J Biol Chem. 1997;272(14):9123–9130. doi: 10.1074/jbc.272.14.9123. [DOI] [PubMed] [Google Scholar]
- 44.Crespo D, Asher RA, Lin R, Rhodes KE, Fawcett JW. How does chondroitinase promote functional recovery in the damaged CNS? Exp Neurol. 2007;206(2):159–171. doi: 10.1016/j.expneurol.2007.05.001. [DOI] [PubMed] [Google Scholar]
- 45.Pizzorusso T, Medini P, Berardi N, Chierzi S, Fawcett JW, Maffei L. Reactivation of ocular dominance plasticity in the adult visual cortex. Science. 2002;298(5596):1248–1251. doi: 10.1126/science.1072699. [DOI] [PubMed] [Google Scholar]
- 46.Butt AM, Kiff J, Hubbard P, Berry M. Synantocytes: new functions for novel NG2 expressing glia. J Neurocytol. 2002;31(6–7):551–565. doi: 10.1023/a:1025751900356. [DOI] [PubMed] [Google Scholar]
- 47.Smith GM, Strunz C. Growth factor and cytokine regulation of chondroitin sulfate proteoglycans by astrocytes. Glia. 2005;52(3):209–218. doi: 10.1002/glia.20236. [DOI] [PubMed] [Google Scholar]
- 48.Gomes FC, de Sousa VO, Romão L. Emerging roles for TGF-beta1 in nervous system development. Int J Dev Neurosci. 2005;23(5):413–424. doi: 10.1016/j.ijdevneu.2005.04.001. [DOI] [PubMed] [Google Scholar]
- 49.Kim YK, Myint AM, Lee BH, Han CS, Lee HJ, Kim DJ, Leonard BE. Th1, Th2 and Th3 cytokine alteration in schizophrenia. Prog Neuropsychopharmacol Biol Psychiatry. 2004;28(7):1129–1134. doi: 10.1016/j.pnpbp.2004.05.047. [DOI] [PubMed] [Google Scholar]
- 50.Benes FM, Lim B, Matzilevich D, Walsh JP, Subburaju S, Minns M. Regulation of the GABA cell phenotype in hippocampus of schizophrenics and bipolars [published online ahead of print June 6, 2007] Proc Natl Acad Sci U S A. 2007;104(24):10164–10169. doi: 10.1073/pnas.0703806104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Zaharieva I, Georgieva L, Nikolov I, Kirov G, Owen MJ, O’Donovan MC, Toncheva D. Association study in the 5q31-32 linkage region for schizophrenia using pooled DNA genotyping. BMC Psychiatry. 2008;8:11. doi: 10.1186/1471-244X-8-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ikeda Y, Yahata N, Ito I, Nagano M, Toyota T, Yoshikawa T, Okubo Y, Suzuki H. Low serum levels of brain-derived neurotrophic factor and epidermal growth factor in patients with chronic schizophrenia. Schizophr Res. 2008;101(1–3):58–66. doi: 10.1016/j.schres.2008.01.017. [DOI] [PubMed] [Google Scholar]
- 53.Futamura T, Toyooka K, Iritani S, Niizato K, Nakamura R, Tsuchiya K, Someya T, Kakita A, Takahashi H, Nawa H. Abnormal expression of epidermal growth factor and its receptor in the forebrain and serum of schizophrenic patients. Mol Psychiatry. 2002;7(7):673–682. doi: 10.1038/sj.mp.4001081. [DOI] [PubMed] [Google Scholar]
- 54.Sheng W, Dong H, Lee DY, Lu WY, Yang BB. Versican modulates gap junction intercellular communication. J Cell Physiol. 2007;211(1):213–219. doi: 10.1002/jcp.20921. [DOI] [PubMed] [Google Scholar]
- 55.Agnati LF, Leo G, Zanardi A, Genedani S, Rivera A, Fuxe K, Guidolin D. Volume transmission and wiring transmission from cellular to molecular networks: history and perspectives. Acta Physiol (Oxf) 2006;187(1–2):329–344. doi: 10.1111/j.1748-1716.2006.01579.x. [DOI] [PubMed] [Google Scholar]
- 56.Schwarzacher SW, Vuksic M, Haas CA, Burbach GJ, Sloviter RS, Deller T. Neuronal hyper-activity induces astrocytic expression of neurocan in the adult rat hippocampus. Glia. 2006;53(7):704–714. doi: 10.1002/glia.20329. [DOI] [PubMed] [Google Scholar]
- 57.Thon N, Haas CA, Rauch U, Merten T, Fässler R, Frotscher M, Deller T. The chondroitin sulphate proteoglycan brevican is upregulated by astrocytes after entorhinal cortex lesions in adult rats. Eur J Neurosci. 2000;12(7):2547–2558. doi: 10.1046/j.1460-9568.2000.00109.x. [DOI] [PubMed] [Google Scholar]
- 58.Naffah-Mazzacoratti MG, Arganaraz GA, Porcionatto MA, Scorza FA, Amado D, Silva R, Bellis-simo MI, Nader HB, Cavalheiro EA. Selective alterations of glycosaminoglycans synthesis and proteoglycan expression in rat cortex and hippocampus in pilocarpine-induced epilepsy. Brain Res Bull. 1999;50(4):229–239. doi: 10.1016/s0361-9230(99)00195-1. [DOI] [PubMed] [Google Scholar]
- 59.McKeon RJ, Jurynec MJ, Buck CR. The chondroitin sulfate proteoglycans neurocan and phosphacan are expressed by reactive astrocytes in the chronic CNS glial scar. J Neurosci. 1999;19(24):10778–10788. doi: 10.1523/JNEUROSCI.19-24-10778.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Beggah AT, Dours-Zimmermann MT, Barras FM, Brosius A, Zimmermann DR, Zurn AD. Lesion-induced differential expression and cell association of neurocan, brevican, versican V1 and V2 in the mouse dorsal root entry zone. Neuroscience. 2005;133(3):749–762. doi: 10.1016/j.neuroscience.2005.03.005. [DOI] [PubMed] [Google Scholar]
- 61.Bogerts B. The neuropathology of schizophrenic diseases: historical aspects and present knowledge. Eur Arch Psychiatry Clin Neurosci. 1999;249(suppl 4):2–13. doi: 10.1007/pl00014181. [DOI] [PubMed] [Google Scholar]
- 62.Falkai P, Honer WG, David S, Bogerts B, Majtenyi C, Bayer TA. No evidence for astrogliosis in brains of schizophrenic patients: a post-mortem study. Neuropathol Appl Neurobiol. 1999;25(1):48–53. doi: 10.1046/j.1365-2990.1999.00162.x. [DOI] [PubMed] [Google Scholar]
- 63.Heckers S. Neuropathology of schizophrenia: cortex, thalamus, basal ganglia, and neurotransmitter-specific projection systems. Schizophr Bull. 1997;23(3):403–421. doi: 10.1093/schbul/23.3.403. [DOI] [PubMed] [Google Scholar]
- 64.Arnold SE. Neurodevelopmental abnormalities in schizophrenia: insights from neuropathology. Dev Psychopathol. 1999;11(3):439–456. doi: 10.1017/s095457949900214x. [DOI] [PubMed] [Google Scholar]
- 65.Damadzic R, Bigelow LB, Krimer LS, Goldenson DA, Saunders RC, Kleinman JE, Herman MM. A quantitative immunohistochemical study of astrocytes in the entorhinal cortex in schizophrenia, bipolar disorder and major depression: absence of significant astrocytosis. Brain Res Bull. 2001;55(5):611–618. doi: 10.1016/s0361-9230(01)00529-9. [DOI] [PubMed] [Google Scholar]
- 66.Pakkenberg B. Pronounced reduction of total neuron number in mediodorsal thalamic nucleus and nucleus accumbens in schizophrenics. Arch Gen Psychiatry. 1990;47(11):1023–1028. doi: 10.1001/archpsyc.1990.01810230039007. [DOI] [PubMed] [Google Scholar]
- 67.Arnold SE, Hyman BT, Van Hoesen GW, Damasio AR. Some cytoarchitectural abnormalities of the entorhinal cortex in schizophrenia. Arch Gen Psychiatry. 1991;48(7):625–632. doi: 10.1001/archpsyc.1991.01810310043008. [DOI] [PubMed] [Google Scholar]
- 68.Kovalenko S, Bergmann A, Schneider-Axmann T, Ovary I, Majtenyi K, Havas L, Honer WG, Bogerts B, Falkai P. Regio entorhinalis in schizophrenia: more evidence for migrational disturbances and suggestions for a new biological hypothesis. Pharmacopsychiatry. 2003;36(suppl 3):S158–S161. doi: 10.1055/s-2003-45124. [DOI] [PubMed] [Google Scholar]
- 69.Lavenex P, Amaral DG. Hippocampal-neocortical interaction: a hierarchy of associativity. Hippocampus. 2000;10(4):420–430. doi: 10.1002/1098-1063(2000)10:4<420::AID-HIPO8>3.0.CO;2-5. [DOI] [PubMed] [Google Scholar]
- 70.de Curtis M, Pare D. The rhinal cortices: a wall of inhibition between the neocortex and the hippocampus. Prog Neurobiol. 2004;74(2):101–110. doi: 10.1016/j.pneurobio.2004.08.005. [DOI] [PubMed] [Google Scholar]
- 71.Prasad KM, Patel AR, Muddasani S, Sweeney J, Keshavan MS. The entorhinal cortex in first-episode psychotic disorders: a structural magnetic resonance imaging study. Am J Psychiatry. 2004;161(9):1612–1619. doi: 10.1176/appi.ajp.161.9.1612. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.