Abstract
Optical coherence tomography (OCT) has become pivotal in the practice of ophthalmology. Similar to other ophthalmic subspecialties, ophthalmic oncology has also incorporated OCT into practice. Anterior segment OCT (AS-OCT), ultra-high resolution OCT (UHR-OCT), spectral domain OCT (SD-OCT) and enhanced depth imaging OCT (EDI-OCT), have all been described to be helpful in the diagnosis, treatment planning and monitoring response of ocular and periocular tumours. Herein we discuss the role of OCT including the advantages and limitations of its use in the setting of common intraocular and adnexal tumours.
Keywords: Imaging, Neoplasia, Pathology
Introduction
Optical coherence tomography (OCT) has become pivotal in the practice of ophthalmology.1 Similar to other ophthalmic subspecialties, ophthalmic oncology has also incorporated OCT into practice. Spectral domain OCT quickly replaced conventional time domain OCT because of its superior speed, sensitivity and resolution (3–7 µm).2 Anterior segment OCT (AS-OCT), ultra-high resolution OCT (UHR-OCT), spectral domain OCT (SD-OCT) and enhanced depth imaging OCT (EDI-OCT), have all been described to be helpful in the diagnosis, treatment planning and monitoring response of ocular and periocular tumours. As OCT technology quickly evolves to more portable units with higher resolution and the capacity to image more peripheral lesions, there is no question it will become increasingly important in clinical practice. Herein we discuss the role of OCT in the management of ocular tumours as well as the advantages and limitations of its use in the setting of common intraocular and adnexal tumours.
Eyelid and adnexa
Basal cell carcinoma (BCC) represents 80–90% of non-melanoma skin cancers of the eyelid.3 Adequately assessing the extent of the tumour is essential in achieving complete surgical excision without risking the integrity of the eye or cosmetic result. This is particularly true in the periocular skin where redundant skin is scarce.
Although diagnostic biopsy represents the gold standard for diagnosis, several groups have explored OCT as a diagnostic tool in dermatology.4–6 In the setting of BCC, OCT is capable of visualising the altered skin architecture with good histopathologic correlation. In a preliminary study, OCT matched histologic features of superficial, nodular, micronodular and infiltrative BCC.
In the context of Mohs micrographic surgery (MMS), lesion margin mapping with OCT was also used to determine if further resection is needed. In a study of 52 patients, OCT was used to identify the transition point between the lesion and benign tissue. With OCT guidance, the authors were able to predict prior to MMS, the cases in which the lesion extended past the clinically apparent margins.7
Pelosini and colleagues studied 15 patients with biopsy-proven periocular BCC, and observed a strong positive correlation between the margins obtained with in vivo OCT and histology. Only a weak correlation for depth of invasion was observed, as the maximum imaging depth with current technology is limited to 1.5–2.0 mm.6 Dense architecture, light-scattering properties and the small size of anatomic components continue to present challenges to imaging human skin.7
Cornea and conjunctiva
Similar to eyelid skin lesions, differentiation of ocular surface lesions is mostly based on clinical examination. Non-invasive imaging techniques, such as OCT and confocal microscopy, can aid in the diagnosis of ocular surface lesions.8 With in vivo confocal microscopy, cellular characteristics suggestive of malignancy, such as enlarged nuclei with high nuclear to cytoplasmic ratio can be observed although clinical interpretation is often challenging. Several authors have assessed the role of AS-OCT in the diagnosis and management of ocular surface lesions.9–12 These studies have shown excellent correlations with histopathology. Furthermore, the introduction of UHR-OCT with a resolution of 3 microns has overcome some of the initial challenges of low-resolution images obtained with time-domain OCT.
In one study with 34 eyes of 34 patients with conjunctival lesions suspicious for ocular surface squamous neoplasia (OSSN) and pterygia, UHR-OCT revealed a significant degree of morphologic correlation with histopathologic results. Moreover, differences in the measured maximal epithelial thickness using UHR-OCT between OSSN and pterygia, were statistically significant. Using a cut of value of 142 um, the sensitivity and specificity of UHR-OCT for differentiating between OSSN and pterygia was 94% and 100%, respectively.11
In a second study, eyes that had been treated with interferon alfa-2b or 5-fluorouracil for conjunctival and corneal intraepithelial neoplasia (CCIN) were compared with patients who had undergone surgical excision of pterygia. Ultra-high-resolution OCT images were useful in guiding medical treatment, and could prevent premature termination of chemotherapy in the presence of subclinical disease. Images of patients with surgically excised pterygia demonstrated similar findings to resolved CCIN cases.12 The same group assessed 54 eyes of 53 patients with a variety of biopsy-proven ocular-surface lesions, including primary acquired melanosis, amelanotic melanoma, naevi, OSSN, histiocytosis, conjunctival lymphoma, conjunctival amyloidosis and pterygia. The authors reported UHR-OCT to be helpful in providing a non-invasive means of guiding diagnosis and management (figure 1).8
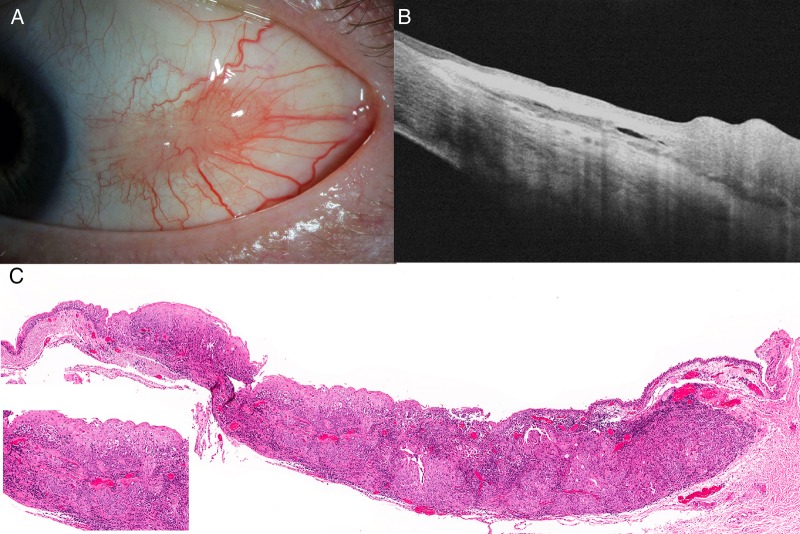
Figure 1.
Left eye conjunctival lesion noticed 4 months prior to referral to the oncology clinic after treatment with topical steroids failed. Slit lamp photographs reveal a vascularised cream-coloured lesion (A). Nasally, the lesion appeared to arise from the epithelium with two small pearl lesions consistent with leukoplakia while the temporal aspect was mainly subconjunctival. Optical coherence tomography revealed thickened epithelium with invasion into the subconjunctival space (B). Photomicrgraph of H&E-stained slide of conjunctival invasive squamous cell carcinoma. The neoplastic epithelium is much thicker than the peripheral non-neoplastic epithelium, and exhibits disordered maturation toward the surface (C). At the right, the carcinoma is seen undermining the non-neoplastic conjunctival epithelium (original magnification ×31). The inset depicts a higher-power photomicrograph, wherein the atypical cytologic and architectural features as well as the irregular, invasive stromal interface characteristic of squamous cell carcinoma, are more easily observed (original magnification ×180)
Shields et al used AS-OCT to evaluate 22 eyes of 21 patients with conjuntival naevi. The anterior, posterior and lateral margins were visualised in 100, 82 and 86% of cases, respectively. By comparison with histopathology, AS-OCT detected intrinsic cysts with a sensitivity of 80% and specificity of 100%. The major drawback was optical shadowing of deeper structures from the pigment within the naevi.
Iris and ciliary body
Ultrasound biomicrosopy (UBM) is the main imaging modality for assessing iris and ciliary body tumours.13 The main limitation of UBM is that it is cumbersome and time consuming, requiring an experienced technician and direct contact with the eye. Anterior segment OCT has only recently been used to image iris tumours.14 Although AS-OCT allows for a less complicated clinical examination without contact with the patient and minimal technical skill, it does suffer from limited penetration. This is particularly true when trying to image through pigmented tissue such as the posterior pigmented layer of the iris (figure 2). The usefulness of OCT in the setting of anterior segment tumours is therefore limited to the iris tumours, hypopigmented tumours and those with limited thickness.
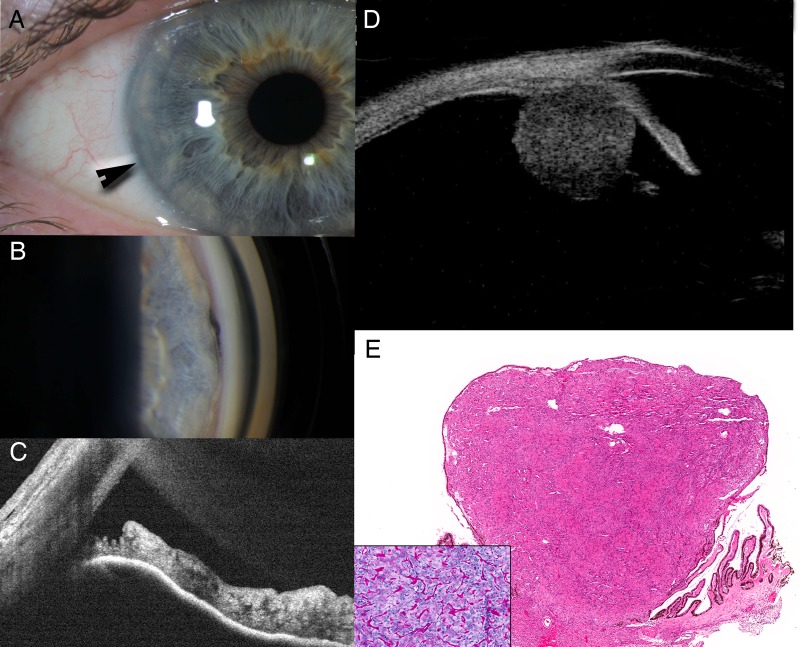
Figure 2.
Iris elevation noted after cataract surgery. Slit lamp photographs reveal anteriorly displaced iris from 8 to 9 o'clock (A). Gonioscopy revealed an open angle with pigmentation at the iris root that does not cross schwabes line (B). Anterior segment-OCT (AS-OCT) was consistent with an open angle and a concave iris with no view past the iris-pigmented epithelium (C). Ultrasonography revealed a 3.7 mm round tumour arising from the pars plicata consistent with a Fuch's adenoma (D). H&E-stained section of a ciliary body lesion, demonstrating a moderately cellular epithelioid neoplasm emanating from the ciliary body (E, original magnification ×34). Inset depicts PAS-stained section that highlights the cords and nests of uniform epithelioid cells, and the PAS-positive basement membrane-like material characteristic of non-pigmented ciliary epithelial adenoma (original magnification ×200).
Bianciotto et al9 studied 200 eyes with anterior segment tumours imaged with AS-OCT and UBM. Overall, UBM provided superior tumour visualisation (69% vs 31%) and better resolution of the posterior margin (74% vs 27%) compared to AS-OCT. Better resolution of the anterior margin (20% vs 80%) and anterior segment anatomy (21% vs 80%) was observed with AS-OCT. This and other studies conclude that UBM continues to be the best method for imaging and following tumours of the iris and ciliary body.14
Choroid and retina
Naevus and melanoma
With reported prevalence rates from 0.2% to 30% in the white population, clinicians regularly face the challenge of differentiating common choroidal naevus from the much less common but potentially fatal melanoma. Although the latter usually presents as an elevated choroidal mass with associated orange pigment and subretinal fluid, approximately 30% are small and difficult to differentiate from naevi on clinical examination.15 In the setting of a suspicious naevus, small choroidal melanoma or intermediate melanocytic lesions, OCT has been a helpful tool in identifying potentially important signs. Subretinal fluid (91% vs 14%), retinal oedema (61% vs 14%) and subretinal deposits (61% vs 11%) all have a significantly higher prevalence in melanoma compared to naevus.16
Although OCT features of choroidal naevus have been extensively documented, the limited visualisation of the deeper layers of the choroid and sclera secondary to light scattering from the retinal pigment epithelium (RPE) and choroid have limited these descriptions to the retina and anterior choroid. To overcome this, EDI-OCT has been used to visualise the choroidal anatomy.2 In this method, the OCT objective lens is pushed closer to the eye yielding an inverted image with improved resolution of the deeper layers of the choroid and sclera.
Shah and associates evaluated 104 eyes with choroidal naevus EDI-OCT found that only 51 (49%) displayed image detail suitable for study. The most common EDI-OCT imaging features in included choroidal shadowing deep to the naevus (partial 59%, complete 35%), choriocapillaris thinning overlying the naevus (94%), RPE atrophy (43%), RPE loss (14%), RPE nodularity (8%), photoreceptor loss (43%), inner segment outer segment (IS-OS) junction irregularity (37%), IS-OS loss, (6%), external limiting membrane irregularity (18%), outer nuclear and outer plexiform layer irregularity (8%), inner nuclear layer irregularity (6%) and subretinal fluid (16%). The authors also observed that EDI-OCT could allow for more precise measurements of naevus thickness and judgment of related effects on the surrounding structures (figure 3).17
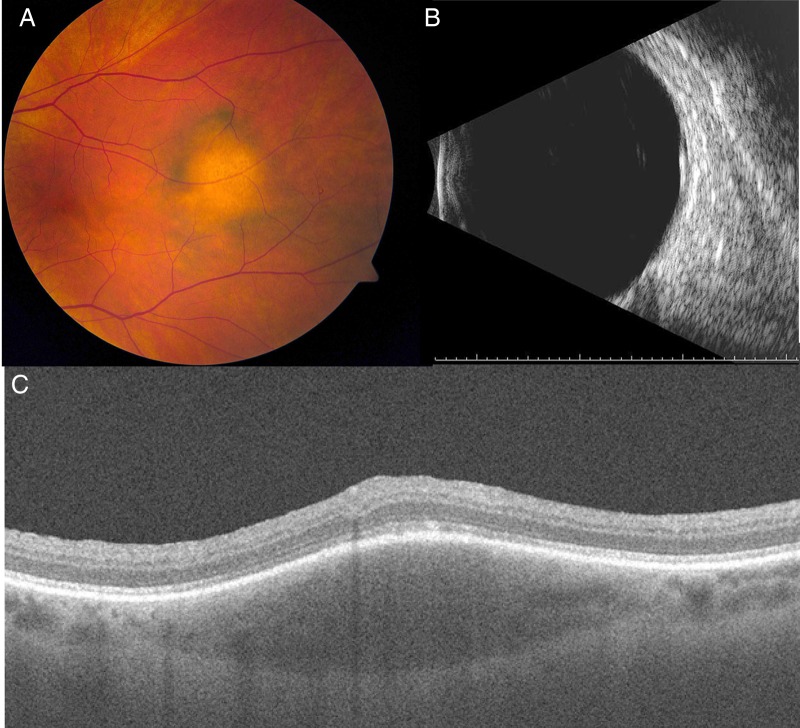
Figure 3.
Patient to the oncology clinic for evaluation of a 6×5×1.5 mm choroidal lesion was found on routine eye examination. Fundus photographs of an amelanotic choroidal naevus temporal to the fovea with overlying retinal pigment epithelium changes and drusen (A). No intrinsic vasculature, orange pigment or subretinal fluid is appreciated. Ultrasonography of the lesion was difficult and the lesion is barely appreciable with high reflectivity (B). Optical coherence tomography was, however, useful in delineating the margins (C). The lesion has low reflectivity and little to no shadowing.
In another study, 37 eyes with small choroidal melanoma were imaged using EDI-OCT. Choroidal shadowing and choriocapillaris thinning was found in 100% of the eyes. Compared with similar sized choroidal naevus, statistically significant EDI-OCT features included intraretinal oedema, loss of photoreceptors, loss of external limiting membrane, loss of IS-OS junction, irregularity of inner plexiform layer and irregularity of ganglion cell layer. Elongated photoreceptors were observed overlying small choroidal melanoma in 49% of cases, but were not observed overlying choroidal naevus.18
Our group reported on 23 eyes with amelanotic choroidal naevus, melanotic choroidal naevus, choroidal melanoma, circumscribed choroidal haemangioma (CCH) and choroidal metastasis.2 Using EDI-OCT, the authors were able to identify the tumour distinctly from the surrounding normal choroid. Maximum tumour diameter and thickness could be measured only by EDI-OCT in 10 cases, all of which were <9.0 mm in diameter and <1 mm in thickness (undetectable by ultrasonography). Consequently, we suggest that EDI-OCT may be used as a complementary technique to ultrasonography for measuring tumours less than 1 mm in height. Qualitative analysis revealed variable reflectivity and vasculature depending on the type of lesion imaged (table 1). A particular advantage of the OCT is the ability to simultaneously display the choroidal tumour and associated retina changes.
Table 1.
Enhanced depth-imaging OCT features of choroial tumours
| Clinical diagnosis | Choroidal reflectivity | Choroidal shadowing | Choriocapillaris visibility | Large vessel visibility | Inner sclera |
|---|---|---|---|---|---|
| Amelanotic naevus | Medium | − | + | + | + |
| Melanotic naevus | High | +/− | +/− | +/− | − |
| Melanoma | High | + | − | − | − |
| Haemangioma | Low to medium | + | +/− | − | − |
| Metastasis | Low | − | + | + | + |
+, detectable; −, non-detectable; +/−, variably detectable.
OCT, optical coherence tomography.
Lymphoma
Intraocular lymphoid tumours can be grouped into primary intraocular lymphoma, a variant of primary central nervous system lymphoma (PCNSL-O) with predominantly ophthalmic involvement and uveal lymphoma. PCNSL-O can masquerade as uveitis, and differential diagnosis should include all causes of chronic posterior uveitis, such as syphilis, sarcoidosis and tuberculosis. Diagnosis may be challenging and is, therefore, usually delayed, sometimes even for years, after initial presentation. The gold standard for diagnosis of lymphoma involves biopsy of the involved tissue. Ancillary testing, such as OCT, has been shown to be helpful in the diagnosis. Fardeau et al19 examined 61 eyes with biopsy-proven vitreoretinal lymphoma where OCT images showed nodular hyper-reflective lesions at the level of the RPE (figure 4). Others have shown the presence of hyper-reflective bands or nodules distributed across the retinal layers.
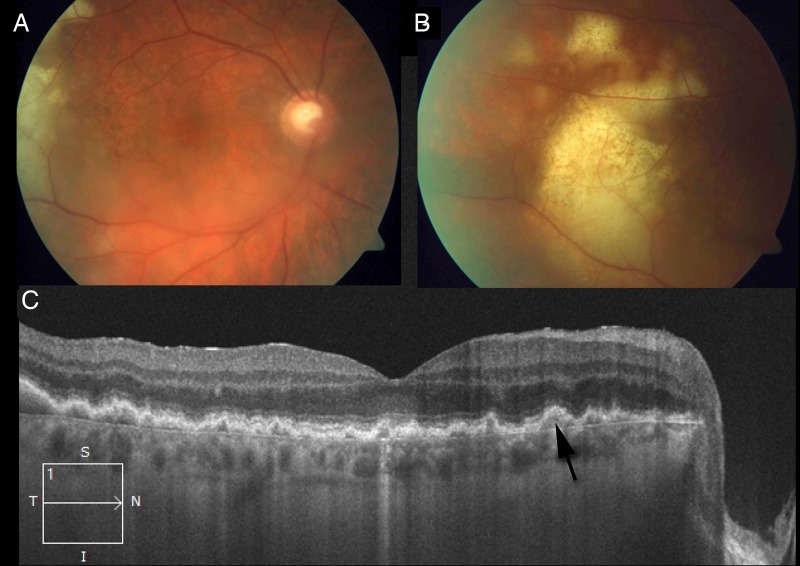
Figure 4.
Patient with a 6-month history of vitritis that was initially treated as a posterior uveitis but subsequently noted to rebound and develop subretinal lesions. Fundus photographs show mild vitritis and a 7×6 mm infiltrative subretinal patch (A and B). On optical coherence tomography nodular hyper-reflective lesions in the retinal pigment epithelium are observed (C).
Uveal lymphoma may involve any portion of the uvea and are sometimes accompanied by conjunctival or obital tumour. For lymphoma involving the choroid, OCT shows regular intermittent placoid choroidal thickening and loss of choriocapillaris with an unaffected RPE and retina. Ultrasonography is still recommended on these patients as, unlike OCT, ultrasonography can detect extrascleral extension.
Haemangioma
Choroidal haemangiomas represent benign hamartomatous vascular tumours that may be confined to the globe or be a manifestation of a widespread hemangiomatous disorder. Although the iris and ciliary body may be involved, these tumours most frequently affect the choroid where they can be classified as circumscribed or diffuse depending on the extent of choroidal involvement. The diagnosis of CCH can be challenging. The funduscopic appearance may be similar to that of other amelanotic choroidal lesions, such as an amelanotic choroidal melanoma, choroidal metastasis, posterior scleritis, choroidal granuloma, choroidal osteoma, varix of vortex vein ampulla, lymphoma or atypical central serous retinopathy. Although ultrasonographic findings and indocyanine green (ICG) are typically most helpful in diagnosis, OCT can also be used to evaluate secondary retinal morphologic changes, such as shallow subretinal fluid or cystoid macular oedema.
Ramasubramanian and colleagues described OCT findings in choroidal haemangiomas. For CCH, subretinal fluid, retinal oedema, retinal schisis, macular oedema and localised photoreceptor loss were observed in 19, 42, 12, 24 and 35% of the cases, respectively. For diffuse choroidal haemangioma, subretinal fluid, retinal oedema and phoroteceptor loss were observed 28, 14 and 43% of the time, respectively.20 To determine the chronicity of the serous retinal detachment and, therefore, potential for visual function, OCT has been used to assess photoreceptor atrophy. On EDI-OCT, CCH appears as a low to medium reflective band with homogenous signal and intrinsic spaces.2
Although traditionally fluorescein angiography and ICG have been used to monitor treatment results, currently, OCT is the primary imaging modality used to detect and quantify associated retinal changes, such as retinoschisis, photoreceptor loss, or atrophy and subretinal or intraretinal fluid.21
Metastasis
Meteastasis to the uvea is by far the most common intraocular malignancy, and the vast majority develop in the choroid. Breast cancer accounts for more than half of all patients with uveal metastases, followed by lung cancer, which accounts for another quarter of all patients. Uveal metastases are usually diagnosed in the setting of a known primary tumour making diagnosis straightforward, but they may, however, also arise as the initial manifestation of an unknown primary. In these cases, differential diagnosis includes all other intraocular tumours, in particular, amelanotic choroidal melanoma. Although OCT has been used to aid in the diagnosis of uveal metasasis, it has, perhaps, been more valuable in monitoring resolution of subretinal fluid and, hence, treatment response. Choroidal metastases usually appear as a hyporeflective band in the deeper choroid causing enlargement of the suprachoroidal space (figure 5). Overlying retinal changes on OCT are non-specific and include a dome-shaped elevation with overlying retinal atrophy, intraretinal oedema and subretinal fluid.2
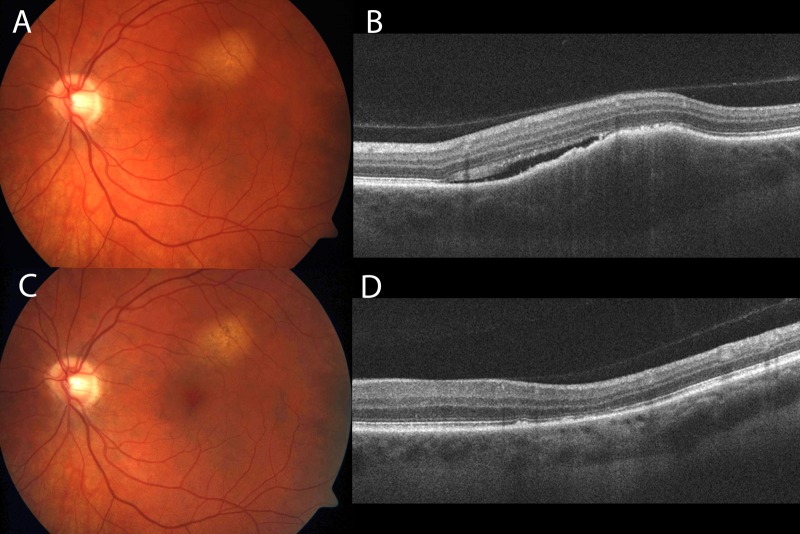
Figure 5.
Patient with a history of stage IV adenocarcinoma of the right lung who presented to the clinic with decreased vision in the left eye. On fundus photography, an amelanotic choroidal lesion approximately 3.5×2.5×1.3 mm in size is observed superior to the fovea with subretinal fluid and no orange pigmentation (A). Enhanced depth imaging optical coherence tomography (OCT) reveals a hyporeflective band in the deeper choroid causing enlargement of the suprachoroidal space (B). Subretinal fluid and some retinal pigment epithelium (RPE) changes are observed. Fundus photograph 2 months after chemotherapy (C). Note a decrease in tumour size, resolution of subretinal fluid and increase in RPE mottling is observed. Enhanced depth imaging OCT (EDI-OCT) confirms these changes (D).
Retinoblastoma
Retinoblastoma is the most common primary intraocular tumour in children. It appears as a yellow-white retinal mass that may exhibit an endophytic or exophytic growth pattern. A rare diffuse pattern of growth characterised by horizontal growth can masquerade as uveitis. Individual tumours appear as thickening and disorganisation of the outer retinal layers with posterior shadowing. On OCT, calcification is sometimes observed. Unlike retinal astrocytic harmartoma which mainly involve thickening of the inner retinal layers, retinal thickening in retinoblastoma involves the outer retinal layers. Because OCT requires certain patient compliance seldom found in the young age group, reports on OCT of retinoblastoma were scarce in the past.
Recently, with the advent of intraoperative OCT, its use has become more popularised. Intraoperative OCT has aided in the diagnosis and management of treatment complications, such as cystoid macular oedema, epiretinal membranes and atrophic retinal holes (figure 6).22 It has also been helpful in visualising subtle retinal findings that are difficult to detect on indirect ophthalmoscopic examination.
Figure 6.
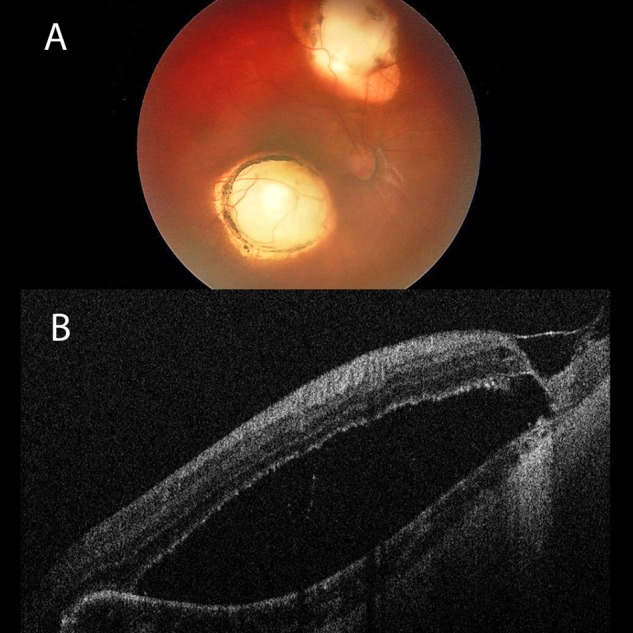
Patient referred for evaluation of a possible retinal detachment. The past medical history is significant for retinoblastoma diagnosed at 2 months of age and treated with multiple cryotherapy and laser trans-pupillary thermotherapy sessions. She had been evaluated by multiple retinal surgeons who debated the presence of schisis and/or full thickness retinal hole. Fundus photograph of the right eye shows two large areas of chorioretinal atrophy due to prior treatment (A). The retina between these two lesions appears to be elevated. Intraoperative optical coherence tomography confirmed the presence of atrophic retinal hole and retinal detachment overlying the area of chorioretial atrophy (B).
Summary
New imaging modalities, such as SD-OCT, ED-OCT, AS-OCT and UHR-OCT offer improvements in diagnosis, treatment planning and monitoring response in patients with ophthalmic tumours. Furthermore, these technologies continue to evolve and become more readily available through ophthalmology practices. It is, however, important to understand the limitations of OCT, mainly its penetration into deep pigmented tissue. Whereas imaging of the cornea and conjunctiva is mainly limited by resolution, imaging of the skin and uvea is limited by penetration. Furthermore, imaging of pigmented and vascularised lesions is also limited. Although, OCT provides valuable information regarding the status of the retina, RPE and inner choroid, ultrasonography including UBM, are still essential in the majority of patients with intraocular tumours.
Footnotes
Contributors: All three authors were involved in design, acquisition of data, analysis/interpretation as well as drafting the article or revising it. Final approval of the submitted version was obtained from all three authors.
Competing interests: None.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Huang D, Swanson EA, Lin CP, et al. Optical coherence tomography. Science 1991;254:1178–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Torres VL, Brugnoni N, Kaiser PK, et al. Optical coherence tomography enhanced depth imaging of choroidal tumors. Am J Ophthalmol 2011;151:586–93 e2. [DOI] [PubMed] [Google Scholar]
- 3.Bath-Hextall F, Leonardi-Bee J, Smith C, et al. Trends in incidence of skin basal cell carcinoma. Additional evidence from a UK primary care database study. Int J Cancer 2007;121:2105–8. [DOI] [PubMed] [Google Scholar]
- 4.Welzel J. Optical coherence tomography in dermatology: a review. Skin Res Technol 2001;7:1–9. [DOI] [PubMed] [Google Scholar]
- 5.Pan Y, Farkas DL. Noninvasive imaging of living human skin with dual-wavelength optical coherence tomography in two and three dimensions. J Biomed Opt 1998;3:446–55. [DOI] [PubMed] [Google Scholar]
- 6.Pelosini L, Smith HB, Schofield JB, et al. In vivo optical coherence tomography (OCT) in periocular basal cell carcinoma: correlations between in vivo OCT images and postoperative histology. Br J Ophthalmol 2013;97:890–4. [DOI] [PubMed] [Google Scholar]
- 7.Wang KX, Meekings A, Fluhr JW, et al. Optical coherence tomography-based optimization of mohs micrographic surgery of Basal cell carcinoma: a pilot study. Dermatol Surg 2013;39:627–33. [DOI] [PubMed] [Google Scholar]
- 8.Shousha MA, Karp CL, Canto AP, et al. Diagnosis of ocular surface lesions using ultra-high-resolution optical coherence tomography. Ophthalmology 2013;120:883–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bianciotto C, Shields CL, Guzman JM, et al. Assessment of anterior segment tumors with ultrasound biomicroscopy versus anterior segment optical coherence tomography in 200 cases. Ophthalmology 2011;118:1297–302. [DOI] [PubMed] [Google Scholar]
- 10.Shields CL, Belinsky I, Romanelli-Gobbi M, et al. Anterior segment optical coherence tomography of conjunctival nevus. Ophthalmology 2011;118:915–19. [DOI] [PubMed] [Google Scholar]
- 11.Kieval JZ, Karp CL, Abou Shousha M, et al. Ultra-high resolution optical coherence tomography for differentiation of ocular surface squamous neoplasia and pterygia. Ophthalmology 2012;119:481–6. [DOI] [PubMed] [Google Scholar]
- 12.Shousha MA, Karp CL, Perez VL, et al. Diagnosis and management of conjunctival and corneal intraepithelial neoplasia using ultra high-resolution optical coherence tomography. Ophthalmology 2011;118:1531–7. [DOI] [PubMed] [Google Scholar]
- 13.Pavlin CJ, Sherar MD, Foster FS. Subsurface ultrasound microscopic imaging of the intact eye. Ophthalmology 1990;97:244–50. [DOI] [PubMed] [Google Scholar]
- 14.Bakri SJ, Singh AD, Lowder CY, et al. Imaging of iris lesions with high-speed optical coherence tomography. Ophthalmic Surg Lasers Imaging 2007;38:27–34. [DOI] [PubMed] [Google Scholar]
- 15.Shields CL, Furuta M, Thangappan A, et al. Metastasis of uveal melanoma millimeter-by-millimeter in 8033 consecutive eyes. Arch Ophthalmol 2009;127:989–98. [DOI] [PubMed] [Google Scholar]
- 16.Sayanagi K, Pelayes DE, Kaiser PK, et al. 3D Spectral domain optical coherence tomography findings in choroidal tumors. Eur J Ophthalmol 2011;21: 271–5. [DOI] [PubMed] [Google Scholar]
- 17.Shah SU, Kaliki S, Shields CL, et al. Enhanced depth imaging optical coherence tomography of choroidal nevus in 104 cases. Ophthalmology 2012;119: 1066–72. [DOI] [PubMed] [Google Scholar]
- 18.Shields CL, Kaliki S, Rojanaporn D, et al. Enhanced depth imaging optical coherence tomography of small choroidal melanoma: comparison with choroidal nevus. Arch Ophthalmol 2012;130:850–6. [DOI] [PubMed] [Google Scholar]
- 19.Fardeau C, Lee CP, Merle-Beral H, et al. Retinal fluorescein, indocyanine green angiography, and optic coherence tomography in non-Hodgkin primary intraocular lymphoma. Am J Ophthalmol 2009;147:886–94 e1. [DOI] [PubMed] [Google Scholar]
- 20.Ramasubramanian A, Shields CL, Harmon SA, et al. Autofluorescence of choroidal hemangioma in 34 consecutive eyes. Retina 2010;30:16–22. [DOI] [PubMed] [Google Scholar]
- 21.Liu W, Zhang Y, Xu G, et al. Optical coherence tomography for evaluation of photodynamic therapy in symptomatic circumscribed choroidal hemangioma. Retina 2011;31:336–43. [DOI] [PubMed] [Google Scholar]
- 22.Rootman DB, Gonzalez E, Mallipatna A, et al. Hand-held high-resolution spectral domain optical coherence tomography in retinoblastoma: clinical and morphologic considerations. Br J Ophthalmol 2013;97:59–65. [DOI] [PubMed] [Google Scholar]