Abstract
Macular oedema (ME) occurs in a wide variety of pathological conditions and accounts for different degrees of vision loss. Early detection of ME is therefore critical for diagnosis and therapeutic management. Optical coherence tomography (OCT) is a non-contact, diagnostic method that uses infrared light, which allows the analysis of the retinal structure by means of high-resolution tomographic cross sections. The identification, localisation, quantification and long-term follow-up of fluid collections are the most important capabilities of OCT. Since the introduction of OCT in clinical practice, it has become an invaluable diagnostic tool and different patterns of ME have been reported. The purpose of this manuscript is to review OCT profiles of ME according to the aetiology and describe what has been reported regarding intraretinal features in vivo.
Keywords: Macula, Imaging, Retina, Vitreous
Introduction
Traditional methods of accessing macular oedema (ME) include contact and non-contact slit lamp biomicroscopy, indirect ophthalmoscopy, fluorescein angiography and fundus stereo photography. However, since the introduction of optical coherence tomography (OCT) in 1991, it has become an invaluable tool in the diagnosis and management of different retinal disorders including ME.1 OCT is a non-contact, micron-level, high-resolution diagnostic method that uses infrared light in the 800–840 nm wavelength range to provide real-time non-invasive imaging of the retina. OCT is based on the principal of Michelson interferometry. An interference pattern is produced by splitting a beam of light into two paths, bouncing the beams back (one from the targeted tissue, the other from a reference mirror) and recombining them by using semitransparent mirrors.2 OCT measurements are similar to those of ultrasound B-mode examinations, but have much higher resolution since light is used instead of sound waves. Ultrasound B-mode examinations have a resolution of 150 μ, while current OCT scanners have less than 5 μ resolution. Spectral or Fourier domain OCT technology has replaced the older, and slower, time domain OCT. Initial SD OCT could acquire images at higher rates up to 20 000 axial scans per second with almost 5 µm resolution. Today, state-of-the-art SD-OCT can acquire between 40 and 70 000A-scans per second. In the future, swept source and longer bandwidth light sources will improve even those numbers.
The normal retinal tissue has different reflectivity patterns on OCT. The nerve fibres and the retinal pigment epithelium display high reflectivity. The plexiform and the nuclear layers display medium reflectivity. The photoreceptors display low reflectivity. There are several scan protocols that are currently used in clinical practice, and the most common are the line and cube or volume scans. The OCT software measures retinal thickness automatically while it is evaluating variations and deviations from the normal values. The distance between the vitreoretinal interface and the anterior surface of the retinal pigment epithelium is generally 200–275 μ. The foveal depression ranges from 170 to 190 μ. The mean thickness measured by OCT in the peripheral retina is generally 220–280 μ. Using several mathematic algorithms, cube scans also allow measurement of the volume of the macula.
OCT has been routinely used in measuring retinal thickness for the evaluation of ME caused by diseases such as age-related macular degeneration, diabetic retinopathy, hereditary retinal degenerations, retinal vein occlusion, after cataract surgery, epiretinal membrane (ERM) and uveitis.3–10 Given its excellent reproducibility, OCT can be used to quantitatively and qualitatively follow retinal thickness over time. Images acquired with OCT today have been found to correlate well with retinal histology as demonstrated with light microscopy.11 Furthermore, topographical studies have shown that subclinical ME caused by different diseases may only be detected by OCT. The advantages of OCT over other imaging modalities available include its non-invasive approach, quick imaging acquisition and safety profile. This review highlights the use of OCT in the diagnosis of ME in patients with different diseases and the different patterns that have been reported.
Macular OCT findings
Patterns of ME
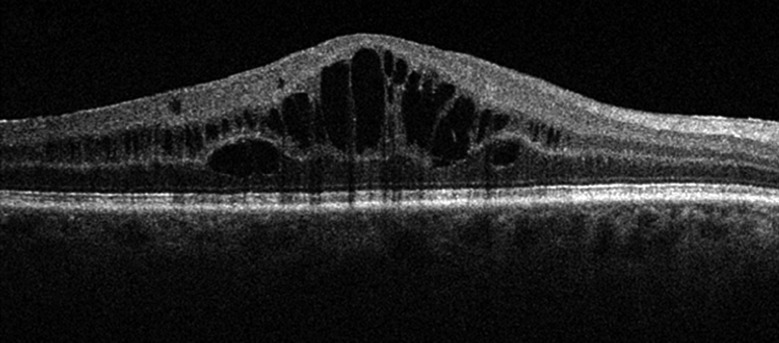
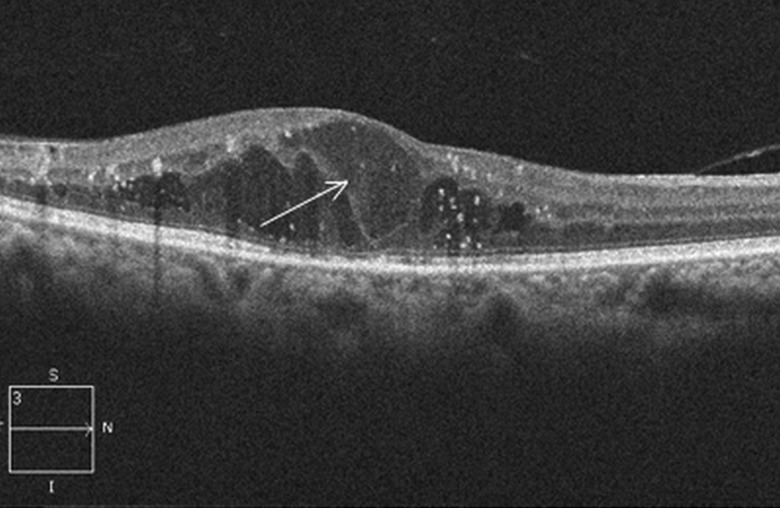
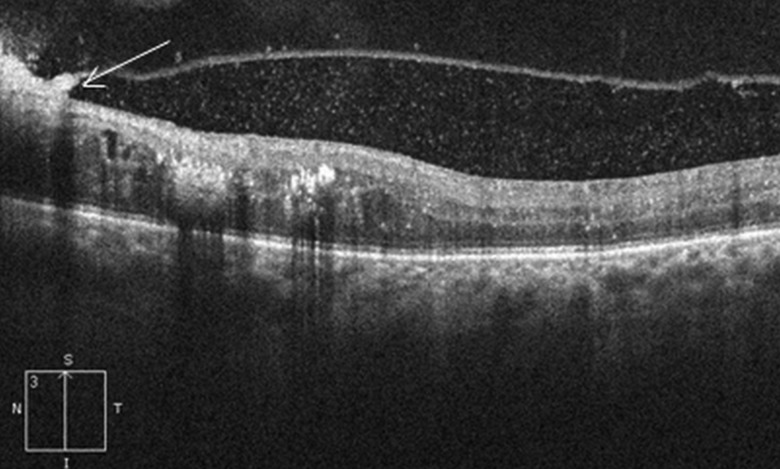
OCT has provided new insights into the morphological changes that occur in patients with ME. There are many causes of ME (table 1). Studies using OCT in diabetic patients have reported different patterns of fluid accumulation in diabetic macular oedema (DME). Otani described three patterns of structural changes in DME: diffuse retinal thickening (DRT), cystoid macular oedema (CME) and serous retinal detachment (SRD).12 Focal or diffuse oedema first appears as a reduction in the reflectivity of the tissue and as increased retinal thickness. Later the retina appears ‘spongy’. CME includes the accumulation of intraretinal fluid in well-defined spaces (figures 1 and 2). Cystoid spaces are formed in the vicinity of the outer plexiform layer, and the rosette appearance seen in late views on fluorescein angiography is caused by the anatomical structure of the plexiform layer. The arrangement of the cystoid cavities is determined by the Müller fibres, which are vertical. The anatomy is clearly delineated on OCT and also becomes very clear in late fluorescein angiography where one sees the typical petalloid leakage. Serous detachment of the retina is usually due to chronic oedema (figure 3). In these patients, the sensory retina is elevated and the cystic cavities often merge.
Table 1.
Causes of macular oedema45
| Frequent causes | Less frequent causes |
|---|---|
| Diabetic retinopathy | Macular telangiectasis |
| Age-related macular degeneration | Coats’ disease |
| Venous occlusion | Leber's disease |
| Hypertensive retinopathy | Retinal arterial macroaneurysm |
| Central serous chorioretinopathy | Retinal capillary angioma |
| Irvine–Gass syndrome | Choroidal cavernous haemangioma |
| Pars planitis | Choroidal melanoma |
| Uveitis and iridocyclitis | Metastatic tumour |
| Choroiditis | Radiation retinopathy |
| Birdshot retinopathy | Retinal surgery |
| Retinitis pigmentosa | Local epinephrine toxicity, prostaglandin analogues |
Figure 1.
Optical coherence tomography appearance of cystoid macular oedema (CME).
Figure 2.
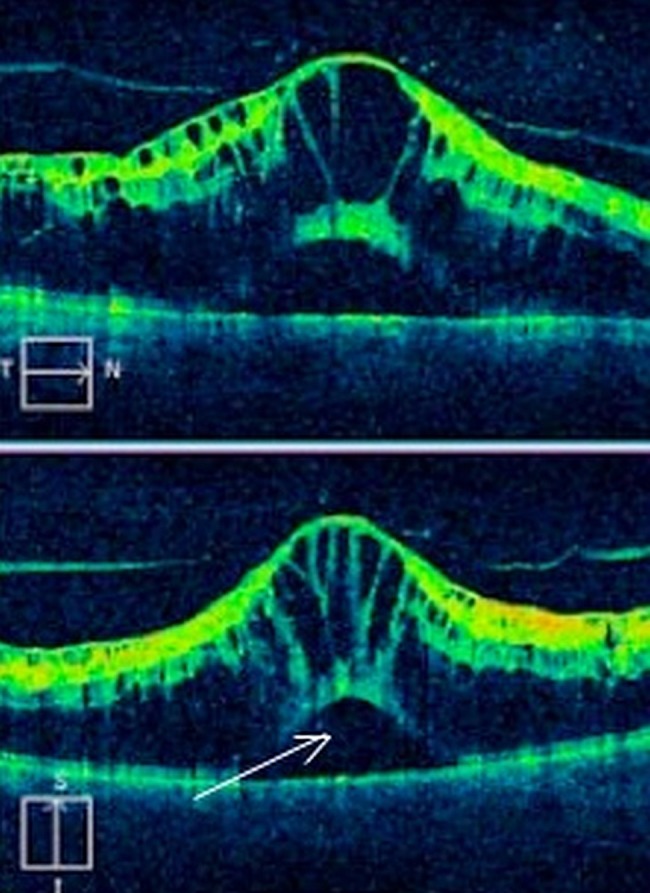
Optical coherence tomography appearance of cystoid macular oedema (CME) with associated subretinal fluid.
Figure 3.
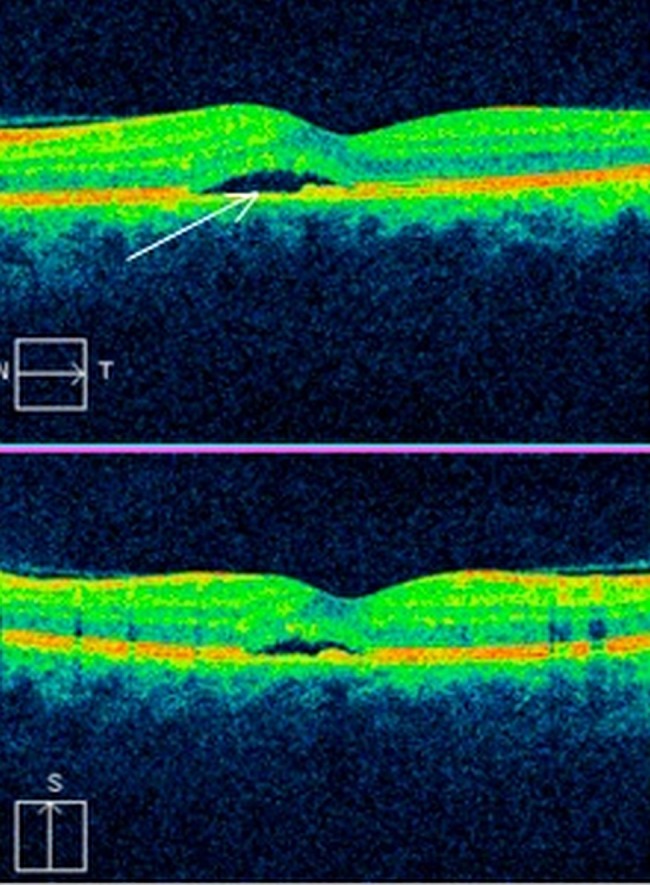
Optical coherence tomography appearance of subretinal fluid under the fovea.
We first reported on OCT findings in a subset of diabetic patients with macular oedema (DME) from posterior hyaloidal traction (PHT).13 The patients all had a subclinical tractional retinal detachment (TRD) that was only visible on OCT. These patients are better treated with surgery instead of medical therapy. We later reported five OCT patterns of DME—the fifth pattern was PHT without TRD. In retrospective, observational, case series 276 scans of 164 patients were analysed and the prevalence of these five OCT patterns were 97% for DRT, 55% for CME, 7% for SRD, 12.7% for PHT without TRD and 2.9% for PHT with TRD14 (figures 4 and 5). The actual OCT image of patients with DRT shows increased retinal thickness with areas of reduced intraretinal reflectivity. CME demonstrates large ovoid areas of low reflectivity, separated by highly reflective septae that represent intraretinal cystoid-like cavities. PHT appears as a highly reflective band over the retinal surface. SRD appears as a dark accumulation of subretinal fluid beneath the high reflective and dome-like elevation of detached retina. The highly reflective band, which represents the outer surface of the detached retina, helps differentiate SRF from intraretinal fluid. TRD is identified as the area of low signal underlying the highly reflective border of detached retina. TRD often take a peaked-shaped configuration. These results were similar to reports by Otani and Yamamoto, who showed that the most common OCT finding in DME was DRT with prevalence of 88% and 60%, respectively. CME was similar with 47% prevalence by Otani and 40% by Yamamoto.15 All these studies also agree that there is a correlation between retinal thickness and visual acuity in patients with DME. Kim et al reported that a 100 µm increase in retinal thickening corresponds to worsening of visual acuity by 0.16 logMAR units. The OCT pattern that was found to be associated with worse visual acuity was CME. The mere presence of CME corresponded to a mean reduction in logMAR acuity of 0.40 compared with 0.16 for other patients.
Figure 4.
Optical coherence tomography appearance of diffuse retinal thickening (DRT) in diabetic patients.
Figure 5.
Macular optical coherence tomography of a diabetic patient with posterior hyaloidal traction (PHT).
Hassenstein et al16 were the first to describe the use of OCT in patients with uveitis and found it to be very useful especially when trying to detect early ME and treatment efficacy, especially in the presence of vitreous cells. Markomichelakis et al defined specific OCT patterns that were identified in uveitic ME. They studied 60 patients with uveitis and uveitic ME and noted three different patterns of fluid accumulation that were similar to the ones reported in diabetic ME by Otani: diffuse macular oedema (DME), CME and SRD.17 Iannetti et al also reported OCT findings in patients with ME from uveitis. Out of 43 eyes that were imaged with OCT, 58% had CME and 42% had DME. SRD was noted in 28% of all cases.18
Spaide et al evaluated the incidence of SRD secondary to branch retinal vein occlusion (BRVO) by OCT. Out of 14 eyes that he evaluated, he found that 10 (71.4%) had SRD involving any portion of the macula. That was an interesting finding given that SRD was rarely discovered on clinical examination in the past. In addition, subretinal haemorrhage can occur in patients with BRVO and the authors propose that blood gravitates through the subretinal fluid to settle behind the retina.19
Catier et al retrospectively reviewed OCT images from patients with different retinal diseases including diabetic retinopathy, central retinal vein occlusion (CRVO), pseudophakia, posterior uveitis and retinitis pigmentosa. They reported that ME was located in the outer retinal layers 92% of all cases. Serous retinal detachment was present in 37% of cases, and it was more frequent in central retina vein occlusion. This detachment did not correlate with poorer visual acuity. Macular thickening only correlated with visual loss in diabetic retinopathy and pseudophakia.20 Also, there is a correlation between angiographic leakage and patterns of ME. Brar et al retrospectively reviewed fluorescein angiography and SD-OCT images of 87 patients with ME due to diabetes, ERM, uveitis, pseudophakia and vein occlusion. They concluded that cystoid leakage on FA is always associated with cystic changes on SD-OCT. Furthermore, diffuse non-cystoid angiographic ME may show microcysts on SD-OCT, but diffuse oedema is more commonly associated with thickening and distortion of the retinal layers without cyst formation.21
Choroidal neovascularisation (CNV) in wet age-related macular degeneration and other causes is associated with intraretinal fluid, subretinal fluid accumulation and pigment epithelial detachments as seen by OCT. Sandhu et al22 analysed 131 eyes of 118 patients and found that OCT with stereo images is 94% sensitive and 89% specific compared with fluorescein angiography in detecting new CNV lesions. Khuraha et al23 had similar results and also demonstrated the superiority of SD-OCT versus TD-OCT.
Drugs like prostaglandin analogues have been reported to induce CME presumably by inducing an inflammatory reaction that causes breakdown of the blood retinal barrier.24 Similar is the effect of epinephrine and epinephrine-like drugs. CME can be seen on OCT without leakage on FA and a well-recognised cause is the use of nicotinic acid to treat hypercholesterolaemia. Other causes are the oncology drugs docetaxel and paclitaxel.25 26 Also, there are some reports that thiazolidinedione agents (pioglitazone and rosiglitazone) can exacerbate ME in 5–15% of patients.27
Intraocular vascular tumours like choroidal hemangiomas, retinal hemangioblastomas, vasoproliferative tumours can cause leakage and cystoid oedema of the retina. Sayanagi et al28 used 3D SD-OCT and analysed 67 eyes with different choroidal tumours and showed that subretinal deposits, subretinal fluid and intraretinal oedema were detected significantly more frequently in the eyes with malignant melanoma compared with choroidal nevus.
Vitreoretinal interface disorders and ME
Epiretinal membrane
ERM is an avascular, fibrocellular membrane on the inner surface of the retina (figure 6). ERM, also known as cellophane retinopathy, results from proliferative changes at the vitreoretinal interface and can be either idiopathic or secondary to other ocular conditions. Secondary causes include retinal tears, retinal vascular diseases (BRVO and CRVO), uveitis, trauma or retinal detachment surgery.29 Idiopathic premacular membranes have a wide range of severity. Tangential traction from ERM may cause macular thickening with or without fluorescein leakage. Also, ERMs can cause significant distortion of the underlying retina and create cystoid spaces.
Figure 6.
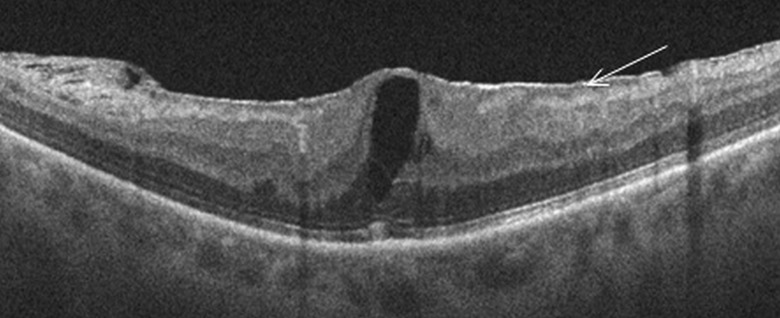
Optical coherence tomography appearance of epiretinal membrane associated with macular oedema.
In clinical practice, SD-OCT has proven useful in the evaluation and treatment of ERMs. Using SD-OCT, one can almost always differentiate the posterior hyaloid, a minimally reflective signal, from an ERM, which is highly reflective.30 Wilkins et al described two patterns of ERM adherence. In his study of 174 eyes, focal attachment was seen in 26% of eyes and 67% eyes had a globally attached ERM. Membrane thickness could be measured in 91% of eyes and was divided into thin (40–60 µm), intermediate (70–100 µm) and thick (120–260 µm).10 OCT has also been helpful in confirming the relationship between PVD and ERM and is valuable for following the natural history of ERMs. Partial or complete PVD has been found in 80–95% of eyes with idiopathic ERM.31 Johnson, in a retrospective observational case series of 43 eyes of 40 patients with idiopathic ERM and no biomicroscopic evidence for complete PVD, reported that all eyes were found by OCT to have partial (87% of eyes) or complete (13% of eyes) PVD.32 It is likely that idiopathic ERM is always associated with PVD and that eyes previously reported as not having PVD have indeed subtle vitreous separation in the macular area that could not be discerned clinically.
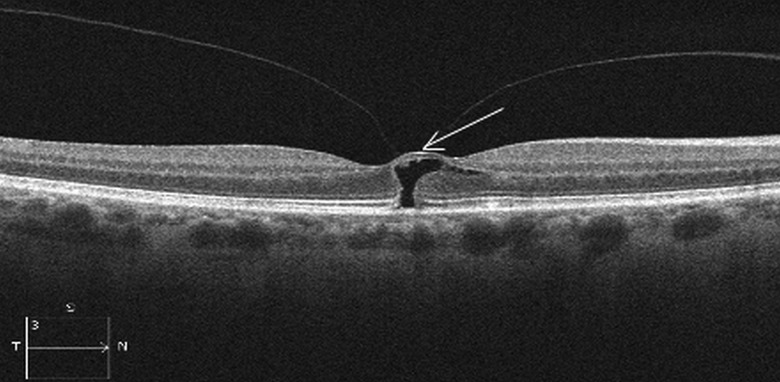
Vitreomacular traction
Vitreomacular traction (VMT) is characterised by partial, anomalous, posterior vitreous detachment that causes anteroposterior traction on the macula in areas of residual vitreous adhesion (figure 7). The adherent vitreous cortex results in a broad, often dumbbell-shaped region encompassing the macular area and optic nerve.33 34 This in turn causes cystoid thickening of the macula. During the Phase III MIVI-TRUST trials of enzymatic vitreolysis with ocriplasmin, assessment of retinal morphology with OCT was performed and confirmed the superiority of OCT to clinical examination. Specifically eyes from the MIVI-TRUST programme with concurrent SD-OCT and TD-OCT at baseline and day 28 were included, and the study concluded that SD-OCT may be superior for formal clinical trial grading due to greater inter-reader reproducibility.35 Based on SD-OCT data, it appears that there are two subclasses of VMT: focal (≤1500 μ) and broad (>1500 μ) adhesion.36 37
Figure 7.
Optical coherence tomography appearance of vitreomacular traction with impending macular hole and cyst formation.
Koizumi et al showed that eyes with focal VMT showed a foveal cavitation, whereas eyes with broad VMT had more widespread CME. In VMT, the posterior hyaloid usually appears hyper-reflective and thickened on OCT. Yamada and Kishi38 suggested that the specific preoperative OCT pattern of VMT may be useful in predicting the postoperative outcome. They described two types of partial PVD patterns. The first type had incomplete vitreous detachment nasally and temporally causing a V-shaped pattern with attachment only at the fovea. The second type had persistent nasal attachment with detachment temporal to the fovea. In their study, the first type of PVD had postoperatively better visual outcomes compared with the second type.
Myopic macular schisis
Retinal schisis or splitting is a phenomenon that is commonly seen in patients with high myopia and posterior staphylomas (figure 8). Biomicroscopically it can be challenging to diagnose, and OCT can be very helpful in these cases. Gaucher et al studied 29 high myopic eyes with OCT scans and revealed that the foveoschisis was associated with macular anomalies: a premacular structure was present in 13 (44.8%) of 29 eyes, a foveal detachment in 10 (34.5%) of 29 eyes and a lamellar macular hole in 6 (20.7%) of 29 eyes. Isolated foveoschisis was found in four eyes (13.8%).39 Shimada et al also used OCT and published the natural course of macular retinoschisis in highly myopic eyes without macular hole or retinal detachment. In the study, eight eyes were followed with OCT for 2 years. During follow-up, two eyes that had vitreoretinal adhesions developed a macular hole, one with and one without retinal detachment (RD), and two eyes without detectable vitreoretinal adhesion developed RD without a macular hole. The remaining four eyes did not develop complications, although the thickness of the macula increased significantly.40 In addition, Robichaud et al41 published two cases where subtle macular thickening was found on biomicroscopy and OCT confirmed the presence of macular schisis associated with VMT.
Figure 8.
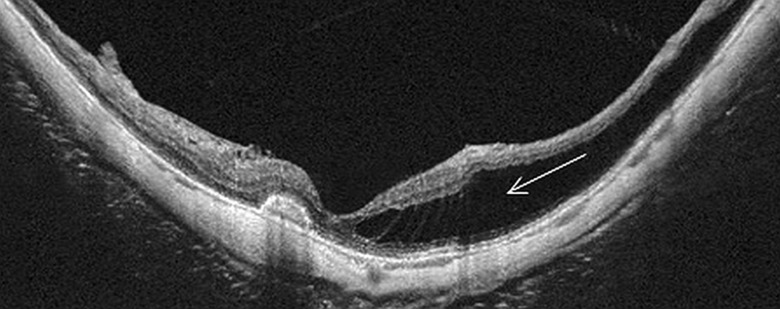
Optical coherence tomography appearance of myopic macular schisis.
Macular schisis associated with optic nerve pits and colobomas
OCT is also helpful in characterising ME or schisis due to optic nerve pits or colobomas (figure 9). In these cases, there is intaretinal fluid accumulation and schisis-like cavity formation within the retina. Karacorlu et al studied 12 eyes with optic nerve pit-associated maculopathy. OCT showed that 10 (83.3%) patients had both retinoschisis and serous macular detachment, one (8.3%) patient had only retinoschisis and one (8.3%) patient had only serous macular detachment. None of the patients had macular hole or vitreoretinal traction.42 Rutledge et al also reported four eyes with optic nerve pit-associated maculopathy. They found retinal oedema and cystic degeneration in all eyes. The oedema was more prominent in the outer plexiform layer.43 Recently, Ohno-Matsui et al used swept-source OCT to evaluation of congenital optic disc pits and optic disc colobomas. Sixteen eyes with congenital optic disc pits and seven eyes with optic disc colobomas were studied. In all of the eyes with optic disc pits, the lamina cribrosa was torn off of the peripapillary sclera at the site of the pits as seen by OCT. In three of seven eyes with disc coloboma, the entire area of the optic disc was observed by OCT.44
Figure 9.

Optical coherence tomography appearance of optic nerve pit associated with intraretinal fluid and macular schisis.
Conclusions
OCT has broadened our basic understanding and interpretation of ME and vitreoretinal interface disorders. It allows early, accurate diagnosis and better follow-up. OCT is now being used routinely in common diseases like diabetic retinopathy and age-related macular degeneration. Diabetes demonstrates the greatest variety of OCT patterns. In our retrospective, observational, case series, the five OCT patterns in diabetes were DRT, CME, SRD, PHT without TRD and PHT with TRD. DRT was the most common OCT finding with 95% prevalence.14 In our daily practice, OCT has become today an invaluable tool in assessing the response to treatment and for the first time we have qualitative and quantitative data of the retinal thickness that we can correlate with visual acuity. In summary, this new non-invasive imaging method is essential in accurately evaluating ME and guide treatment.
Footnotes
Contributors: Both authors contributed in writing and editing this manuscript.
Funding: Research to Prevent Blindness (PKK).
Competing interests: None.
Provenance and peer review: Commissioned; externally peer reviewed.
References
- 1.Huang D, Swanson EA, Lin CP, et al. Optical coherence tomography. Science 1991;254:1178–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Puliafito CA, Hee MR, Lin CP, et al. Imaging of macular diseases with optical coherence tomography . Ophthalmology 1995;102:217–29. [DOI] [PubMed] [Google Scholar]
- 3.Jaffe GJ, Caprioli J. Optical coherence tomography to detect and manage retinal disease and glaucoma. Am J Ophthalmol 2004;137:156–69. [DOI] [PubMed] [Google Scholar]
- 4.Hirakawa H, Iijima H, Gohdo T, et al. Optical coherence tomography of cystoid macular edema associated with retinitis pigmentosa. Am J Ophthalmol 1999;128:185–91. [DOI] [PubMed] [Google Scholar]
- 5.Forooghian F, Cukras C, Meyerle CB, et al. Evaluation of time domain and spectral domain optical coherence tomography in the measurement of diabetic macular edema. Invest Ophthalmol Vis Sci 2008;49:4290–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Scott IU, VanVeldhuisen PC, Oden NL, et al. Standard Care versus COrticosteroid for REtinal Vein Occlusion Study Investigator Group. Baseline predictors of visual acuity and retinal thickness outcomes in patients with retinal vein occlusion: Standard Care Versus Corticosteroid for retinal Vein Occlusion Study report 10. Ophthalmology 2011;118:345–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hoeh AE, Ruppenstein M, Ach T, et al. OCT patterns of macular edema and response to bevacizumab therapy in retinal vein occlusion. Graefes Arch Clin Exp Ophthalmol 2010;248:1567–72. [DOI] [PubMed] [Google Scholar]
- 8.Vukicevic M, Gin T, Al-Qureshi S. Prevalence of optical coherence tomography diagnosed post-operative cystoid macular oedema in patients following uncomplicated phacoemulsification cataract surgery. Clin Experiment Ophthalmol 2012;40:282–7. [DOI] [PubMed] [Google Scholar]
- 9.Massin P, Allouch C, Haouchine B, et al. Optical coherence tomography of idiopathic macular epiretinal membranes before and after surgery. Am J Ophthalmol 2000;130:732–9. [DOI] [PubMed] [Google Scholar]
- 10.Wilkins JR, Puliafito CA, Hee MR, et al. Characterization of epiretinal membranes using optical coherence tomography. Ophthalmology 1996;103:2142–51. [DOI] [PubMed] [Google Scholar]
- 11.Hee MR, Izatt JA, Swanson EA, et al. Optical coherence tomography of the human retina. Arch Ophthalmol 1995;113:325–32. [DOI] [PubMed] [Google Scholar]
- 12.Otani T, Kishi S, Maruyama Y. Patterns of diabetic macular edema with optical coherence tomography. Am J Ophthalmol 1999;127:688–93. [DOI] [PubMed] [Google Scholar]
- 13.Kaiser PK, Riemann CD, Sears JE, et al. Macular traction detachment and diabetic macular edema associated with posterior hyaloidal traction. Am J Ophthalmol 2001;131:44–9. [DOI] [PubMed] [Google Scholar]
- 14.Kim BY, Smith SD, Kaiser PK. Optical coherence tomographic patterns of diabetic macular edema. Am J Ophthalmol 2006;142:405–12. [DOI] [PubMed] [Google Scholar]
- 15.Yamamoto S, Yamamoto T, Hayashi M. Morphological and functional analyses of diabetic macular edema by optical coherence tomography and multifocal electroretinograms. Graefes Arch Clin Exp Ophthalmol 2001;239:96–101. [DOI] [PubMed] [Google Scholar]
- 16.Hassenstein A, Bialasiewicz AA, Richard G. Optical coherence tomography in uveitis patients. Am J Ophthalmol 2000;130:669–70. [DOI] [PubMed] [Google Scholar]
- 17.Markomichelakis NN, Halkiadakis I, Pantelia E, et al. Patterns of macular edema in patients with uveitis: qualitative and quantitative assessment using optical coherence tomography. Ophthalmology 2004;111:946–53. [DOI] [PubMed] [Google Scholar]
- 18.Iannetti L, Accorinti M, Liverani M, et al. Optical coherence tomography for classification and clinical evaluation of macular edema in patients with uveitis. Ocul Immunol Inflamm 2008;16:155–60. [DOI] [PubMed] [Google Scholar]
- 19.Spaide RF, Lee JK, Klancnik JK, Jr, et al. Optical coherence tomography of branch retinal vein occlusion. Retina 2003;23:343–7. [DOI] [PubMed] [Google Scholar]
- 20.Catier A, Tadayoni R, Paques M, et al. Characterization of macular edema from various etiologies by optical coherence tomography. Am J Ophthalmol 2005;140:200–6. [DOI] [PubMed] [Google Scholar]
- 21.Brar M, Yuson R, Kozak I, et al. Correlation between morphologic features on spectral-domain optical coherence tomography and angiographic leakage patterns in macular edema. Retina 2010;30:383–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sandhu SS, Talks SJ. Correlation of optical coherence tomography, with or without additional colour fundus photography, with stereo fundus fluorescein angiography in diagnosing choroidal neovascular membranes. Br J Ophthalmol 2005;89:967–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Khurana RN, Dupas B, Bressler NM. Agreement of time-domain and spectral- domain optical coherence tomography with fluorescein leakage from choroidal neovascularization. Ophthalmology 2010;117:1376–80. [DOI] [PubMed] [Google Scholar]
- 24.Moroi SE, Gottfredsdottir MS, Schteingart MT, et al. Cystoid macular edema associated with latanoprost therapy in a case series of patients with glaucoma and ocular hypertension. Ophthalmology 1999;106:1024–9. [DOI] [PubMed] [Google Scholar]
- 25.Sarraf D. Sarraf Cystoid macular edema with docetaxel chemotherapy and the fluid retention syndrome. Semin Ophthalmol 2007;22:151–3. [DOI] [PubMed] [Google Scholar]
- 26.Joshi MM, Garretson BR. Paclitaxel maculopathy. Arch Ophthalmol 2007;125:709–10. [DOI] [PubMed] [Google Scholar]
- 27.Ryan EH, Jr, Han DP, Ramsay RC, et al. Diabetic macular edema associated with glitazone use. Retina 2006;26:562–70. [DOI] [PubMed] [Google Scholar]
- 28.Sayanagi K, Pelayes DE, Kaiser PK, et al. 3D Spectral domain optical coherence tomography findings in choroidal tumors. Eur J Ophthalmol 2011;21:271–5. [DOI] [PubMed] [Google Scholar]
- 29.Sebag J. Anatomy and pathology of the vitreo-retinal interface. Eye 1992:6:541–52. [DOI] [PubMed] [Google Scholar]
- 30.Mirza RG, Johnson MW, Jampol LM. Optical coherence tomography use in evaluation of the vitreoretinal interface: a review. Surv Ophthalmol 2007;52:397–421. [DOI] [PubMed] [Google Scholar]
- 31.Kishi S, Shimizu K. Oval defect in detached posterior hyaloid membrane in idiopathic preretinal macular fibrosis. AmJ Ophthalmol, 1994;118:451–6. [DOI] [PubMed] [Google Scholar]
- 32.Johnson MW. Perifoveal vitreous detachment and its macular complications. Trans Am Ophthalmol Soc 2005;103:537–67. [PMC free article] [PubMed] [Google Scholar]
- 33.Jaffe NS. Vitreous traction at the posterior pole of the fundus due to alterations in the vitreous posterior. Trans Am Acad Ophthalmol Otolaryngol 1967;71:642–52. [PubMed] [Google Scholar]
- 34.Smiddy W. Vitreomacular traction syndrome, In: Yanoff N, Duker JS, eds. Ophthalmology. 2nd edn St. Louis: Mosby, 2004:951–5. [Google Scholar]
- 35.Folgar FA, Toth CA, DeCroos FC, et al. Assessment of retinal morphology with spectral and time domain OCT in the phase III trials of enzymatic vitreolysis. Invest Ophthalmol Vis Sci 2012;53:7395–401. [DOI] [PubMed] [Google Scholar]
- 36.Koizumi H, Spaide RF, Fisher YL, et al. Three-dimensional evaluation of vitreomacular traction and epiretinal membrane using spectral-domain optical coherence tomography. Am J Ophthalmol 2008;145:509–e1. [DOI] [PubMed] [Google Scholar]
- 37.Sonmez K, Capone A, Jr, Trese MT, et al. Vitreomacular traction syndrome: impact of anatomical configuration on anatomical and visual outcomes. Retina 2008;28:1207–14. [DOI] [PubMed] [Google Scholar]
- 38.Yamada N, Kishi S. Tomographic features and surgical outcomes of vitreomacular traction syndrome. Am J Ophthalmol 2005;139:112–17. [DOI] [PubMed] [Google Scholar]
- 39.Gaucher D, Haouchine B, Tadayoni R, et al. Long-term follow-up of high myopic foveoschisis: natural course and surgical outcome. Am J Ophthalmol 2007;143:455–62. [DOI] [PubMed] [Google Scholar]
- 40.Shimada N, Ohno-Matsui K, Baba T, et al. Natural course of macular retinoschisis in highly myopic eyes without macular hole or retinal detachment. Am J Ophthalmol 2006;142:497–500. [DOI] [PubMed] [Google Scholar]
- 41.Robichaud JL, Besada E, Basler L, et al. Spectral domain optical coherence tomography of myopic traction maculopathy. Optometry 2011;82:607–13. [DOI] [PubMed] [Google Scholar]
- 42.Karacorlu SA, Karacorlu M, Ozdemir H, et al. Optical coherence tomography in optic pit maculopathy. Int Ophthalmol 2007;27:293–7. [DOI] [PubMed] [Google Scholar]
- 43.Rutledge BK, Puliafito CA, Duker JS, et al. Optical coherence tomography of macular lesions associated with optic nerve head pits. Ophthalmology 1996;103:1047–53. [DOI] [PubMed] [Google Scholar]
- 44.Ohno-Matsui K, Hirakata A, Inoue M, et al. Evaluation of congenital optic disc pits and optic disc colobomas by swept-source optical coherence tomography . Invest Ophthalmol Vis Sci 2013;54:7769–78. [DOI] [PubMed] [Google Scholar]
- 45.Tranos PG, Wickremasinghe SS, Stangos NT, et al. Macular edema. Surv Ophthalmol 2004;49:470–90. [DOI] [PubMed] [Google Scholar]