Abstract
Objective
To evaluate the performance of China’s infectious disease automated alert and response system in the detection of outbreaks of hand, foot and mouth (HFM) disease.
Methods
We estimated size, duration and delay in reporting HFM disease outbreaks from cases notified between 1 May 2008 and 30 April 2010 and between 1 May 2010 and 30 April 2012, before and after automatic alert and response included HFM disease. Sensitivity, specificity and timeliness of detection of aberrations in the incidence of HFM disease outbreaks were estimated by comparing automated detections to observations of public health staff.
Findings
The alert and response system recorded 106 005 aberrations in the incidence of HFM disease between 1 May 2010 and 30 April 2012 – a mean of 5.6 aberrations per 100 days in each county that reported HFM disease. The response system had a sensitivity of 92.7% and a specificity of 95.0%. The mean delay between the reporting of the first case of an outbreak and detection of that outbreak by the response system was 2.1 days. Between the first and second study periods, the mean size of an HFM disease outbreak decreased from 19.4 to 15.8 cases and the mean interval between the onset and initial reporting of such an outbreak to the public health emergency reporting system decreased from 10.0 to 9.1 days.
Conclusion
The automated alert and response system shows good sensitivity in the detection of HFM disease outbreaks and appears to be relatively rapid. Continued use of this system should allow more effective prevention and limitation of such outbreaks in China.
Résumé
Objectif
Évaluer les résultats du système automatisé d'alerte et d'action pour les maladies infectieuses de la Chine en matière de détection des épidémies de maladie des mains, pieds et bouche (MMPB).
Méthodes
Nous avons estimé la taille, la durée et le retard du signalement des épidémies de MMPB à partir des cas notifiés entre le 1er mai 2008 et le 30 avril 2010 et entre le 1er mai 2010 et le 30 avril 2012, c'est-à-dire avant et après l'intégration de la MMPB dans le système automatisé d'alerte et d'action. La sensibilité, la spécificité et la rapidité de la détection des aberrations dans l'incidence des épidémies de MMPB ont été estimées en comparant les détections automatisées aux observations du personnel des services de santé publique.
Résultats
Le système d'alerte et d'action a enregistré 106 005 aberrations dans l'incidence de la MMPB entre le 1er mai 2010 et le 30 avril 2012 – une moyenne de 5,6 erreurs pour 100 jours dans chaque comté qui avait signalé la MMPB. Le système d'action avait une sensibilité de 92,7% et une spécificité de 95,0%. Le retard moyen entre le signalement du premier cas d'une épidémie et la détection de cette épidémie par le système d'action était de 2,1 jours. Entre les périodes de la première et de la seconde étude, la taille moyenne d'une épidémie de MMPB a diminué de 19,4 à 15,8 cas, et l'intervalle moyen entre le début et le signalement initial d'une telle épidémie au système de notification d'urgence des services de santé publique a diminué, passant de 10,0 à 9,1 jours.
Conclusion
Le système automatisé d'alerte et d'action présente une bonne sensibilité en matière de détection des épidémies de MMPB et semble être relativement rapide. L'utilisation continue de ce système devrait permettre de prévenir et de limiter plus efficacement ces épidémies en Chine.
Resumen
Objetivo
Evaluar el rendimiento del sistema de alerta y respuesta automática a enfermedades infecciosas de China en la detección de brotes de la enfermedad boca-mano-pie (EBMP).
Métodos
Calculamos la magnitud, la duración y la demora en la notificación de brotes de la enfermedad BMP a partir de casos notificados entre el 1 de mayo de 2008 y el 30 de abril de 2010, y entre el 1 de mayo de 2010 y el 30 de abril 2012, antes y después de que el sistema de alerta y respuesta automáticas incluyera la enfermedad BMP. Se estimó la sensibilidad, especificidad y oportunidad de la detección de aberraciones en la incidencia de los brotes de enfermedad BMP mediante la comparación de las detecciones automáticas con las observaciones del personal de salud pública.
Resultados
El sistema de alerta y respuesta registró 106 005 aberraciones en la incidencia de la EBMP entre el 1 de mayo de 2010 y el 30 de abril de 2012 - una media de 5,6 aberraciones por cada 100 días en cada condado que notificó dicha enfermedad. El sistema de respuesta tuvo una sensibilidad del 92,7 % y una especificidad del 95,0 %. La demora media entre la notificación del primer caso de un brote y la detección de ese brote por el sistema de respuesta fue de 2,1 días. Entre el primer y el segundo período de estudio, las dimensiones medias de un brote de EBMP disminuyeron de 19,4 a 15,8 casos, y el intervalo medio entre el comienzo de un brote y el primer informe en el sistema de notificación de emergencia de salud pública se redujo de 10,0 a 9,1 días.
Conclusión
El sistema de alerta y respuesta automática muestra una buena sensibilidad en la detección de los brotes de EBMP y parece ser relativamente rápido. El uso continuado de este sistema debería permitir una prevención y limitación más eficaces de dichos brotes en China.
ملخص
الغرض
تقييم أداء نظام الإنذار والاستجابة الآلي للأمراض المعدية في اكتشاف فاشيات مرض اليد والقدم والفم في الصين.
الطريقة
قمنا بتقدير الحجم والمدة والتأخير في الإبلاغ عن فاشيات مرض اليد والقدم والفم من الحالات التي تم الإخطار بها بين 1 أيار/مايو 2008 و30 نيسان/أبريل 2010 وبين 1 أيار/مايو 2010 و30 نيسان/أبريل 2012، قبل إدراج داء اليد والقدم والفم في الإنذار والاستجابة الآلية وبعده. وتم تقدير حساسية اكتشاف الانحرافات ونوعيتها وتوقيتها في معدل الإصابة بفاشيات مرض اليد والقدم والفم عن طريق مقارنة الاكتشافات والملاحظات الآلية من قبل موظفي الصحة العمومية.
النتائج
سجل نظام الإنذار والاستجابة 106005 انحرافاً في معدل الإصابة بمرض اليد والقدم والفم بين 1 أيار/مايو 2010 و30 نيسان/أبريل2012 - المتوسط 5.6 انحرافاً لكل 100 يوم في كل مقاطعة أبلغت عن مرض اليد والقدم والفم. وكانت حساسية نظام الاستجابة 92.7 % ونوعيته 95.0 %. وكان متوسط التأخير بين الإبلاغ عن الحالة الأولى لإحدى الفاشيات واكتشاف تلك الفاشية عن طريق نظام الاستجابة 2.1 يوم. وانخفض متوسط حجم فاشية مرض اليد والقدم والفم بين الفترتين الدراسيتين الأولى والثانية من 19.4 حالة إلى 15.8 حالة وانخفض متوسط الفاصل بين بداية هذه الفاشية والإبلاغ الأولي عنها إلى نظام الإبلاغ عن حالات الطوارئ في الصحة العمومية من 10.0 إلى 9.1 يوماً.
الاستنتاج
يشير نظام الإنذار والاستجابة الآلي إلى حساسية جيدة في اكتشاف فاشيات مرض اليد والقدم والفم ويبدو أنه سريع نسبياً. وينبغي أن يسمح الاستخدام المتواصل لهذا النظام بزيادة فعالية الوقاية وتقييد هذه الفاشيات في الصين.
摘要
目的
评价中国传染病自动预警与响应系统在探测手足口疾病(HFM)爆发方面的表现。
方法
我们利用2008年5月1日和2010年4月30日之间以及2010年5月1日和2012年4月30日之间(即自动预警与响应系统将手足口病纳入之前和之后)报告的病例估算了手足口病病爆发的规模、持续时间和报告延迟时间。将预警与响应系统自动探测的结果与公共卫生工作人员的观察结果进行比较,评估该系统用于探测手口足病爆发的灵敏度、特异度和及时性。
结果
在2010年5月1日至2012年4月30日期间,预警和响应系统发出了106005条预警信号,——在每个有手足口病病例报告的县,平均每100天产生5.6条手足口病预警信号。响应系统敏感度为92.7%,特异度为95.0%。从爆发的第一例病例报告至自动预警与响应系统探测到爆发之间的平均时间间隔是2.1天。在自动预警与响应系统将手足口病纳入之前和之后,手足口病爆发的平均规模从19.4例下降到15.8例,从爆发首例病例发病至向突发公共卫生事件报告系统进行报告之间的平均时间间隔从10.0天下降到9.1天。
结论
自动预警与响应系统在探测手足口病爆发方面具有良好的灵敏度和及时性。持续使用该系统应该能够更有效地预防和控制中国手足口病的爆发。
Резюме
Цель
Оценить эффективность автоматизированной системы оповещения и реагирования в Китае, используемой для обнаружения вспышек вирусной пузырчатки полости рта и конечностей (HFM — от англ. hand, foot and mouth disease).
Методы
Размер, продолжительность вспышек и задержка сообщений о вспышках HFM оценивались на основе случаев, зарегистрированных в период с 1 мая 2008 года по 30 апреля 2010 года и в период с 1 мая 2010 года по 30 апреля 2012 года, как до, так и после начала использования системы автоматического оповещения и реагирования о данном заболевании. Чувствительность, специфичность и своевременность обнаружения отклонений в уровне заболеваемости HFM оценивались путем сравнения данных автоматизированной системы обнаружения с наблюдения специалистов общественного здравоохранения.
Результаты
Системой оповещения и реагирования было зарегистрировано 106 005 отклонений в уровне заболеваемости HFM в период с 1 мая 2010 года по 30 апреля 2012 года, что составило в среднем 5,6 отклонений на 100 дней в каждом округе, сообщившем о случаях заболевания HFM. Чувствительность и специфичность системы реагирования составляли 92,7% и 95,0% соответственно. Средняя задержка между сообщением о первом случае вспышки заболевания и выявлением данной вспышки системой реагирования составила 2,1 дня. Между первым и вторым периодами исследования средний размер вспышки HFM уменьшился с 19,4 до 15,8 случаев, а средний интервал между началом вспышки и первоначальным сообщением о данной вспышке в систему аварийной отчетности здравоохранения уменьшился с 10,0 до 9,1 дней.
Вывод
Автоматизированная система оповещения и реагирования продемонстрировала хорошую чувствительность при обнаружении вспышек вирусной пузырчатки полости рта и конечностей и относительно высокую скорость реагирования. Дальнейшее использование этой системы должно обеспечить более эффективное предотвращение и ограничение вспышек данного заболевания в Китае.
Introduction
To improve control of infectious disease outbreaks, it is critical to establish early detection and warning systems. In recent decades, technological advances in computing and communication and mathematical aberrancy-detection algorithms have been applied to high-volume data sets, to generate alerts and draw the attention of epidemiologists to statistical anomalies that may indicate a localized outbreak or the elevated risk of such an outbreak.1–3 Several national public health agencies have successfully developed and operated automated early warning systems for the prompt detection of disease outbreaks.4–8 Some epidemiologists have simulated outbreaks to evaluate the performance of such systems and the associated outbreak-detection algorithms.9,10 However, there have been few prospective evaluations of the performance of early warning systems in operational settings.11,12
In April 2008, a web-based automated system for the early detection of – and rapid response to – outbreaks of infectious disease was implemented across China.13 This system – the China infectious disease automated alert and response system (hereafter referred to as the response system) – was developed by the Chinese Centre for Disease Control and Prevention, with the support of the Chinese Ministry of Health and the World Health Organization. The response system was based on surveillance data on dozens of notifiable diseases and on several statistical algorithms for the automated and routine detection of aberrations in such data, at county level, that might indicate the early stages of potential outbreaks.
Although hand, foot and mouth (HFM) disease can be caused by serotypes of several enteroviruses, it is most frequently caused by coxsackie virus A16 and human enterovirus 71. Most affected people develop only mild symptoms but some cases may result in serious and even fatal complications.14–16 In China, HFM disease is frequently detected in children aged less than five years17 and there have been over a million cases of the disease, including hundreds of fatal cases, reported annually over recent years.18,19
In this study, we aimed to evaluate the performance of the response system by analysing the sensitivity, specificity and timeliness in the detection of HFM disease outbreaks. We also wished to evaluate the response system’s effectiveness by comparing the size and duration of HFM disease outbreaks – and the post-onset delay in reporting such outbreaks – before and after HFM disease was included in the response system.
Methods
Case reporting system
All HFM disease cases that occurred in China after May 2008 – when HFM disease became a notifiable disease in China20 – should have been reported, by attending clinicians, via the nationwide notifiable infectious diseases reporting information system (hereafter referred to as the case reporting system). This system enables health-care institutes across China to report information on each case of a notifiable infectious disease rapidly, via the Internet, to the Chinese Centre for Disease Control and Prevention. For our study, we used the information on each laboratory-confirmed or clinically diagnosed case of HFM disease that was reported to the case reporting system between 1 May 2008 and 30 April 2012.
Automated detection of outbreaks
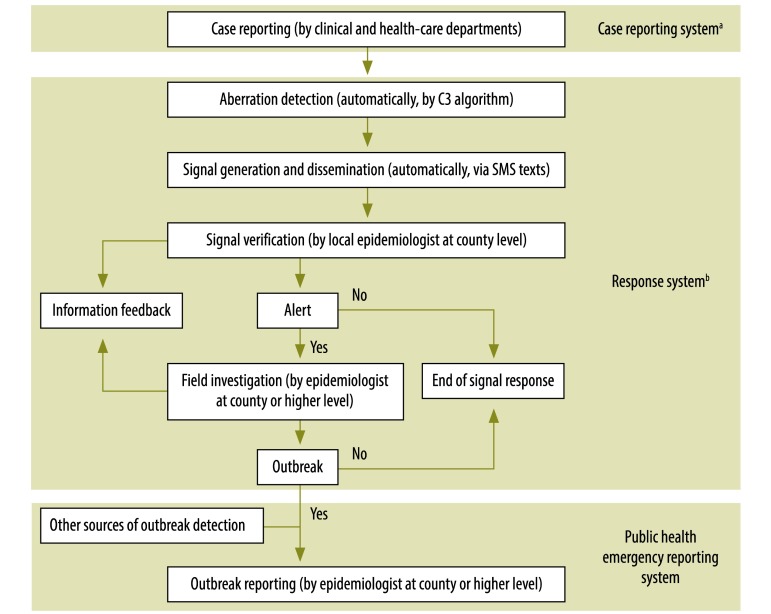
Currently, the automated alert and response system searches the data collected in the case reporting system for aberrations in the incidence of HFM disease and another 29 notifiable infectious diseases.13 HFM disease has only been included in the response system since 1 May 2010. In the response system, an aberration in incidence at county level leads to the automated generation of a warning signal and that signal’s dissemination to the relevant county-level Centre for Disease Control and Prevention. Each signal is then investigated further by epidemiologists in the specific county (Fig. 1).
Fig. 1.
The operational flow of information on hand, foot and mouth disease to and from the response systema
a China Infectious Disease Automated Alert and Response System.
b Notifiable Infectious Diseases Reporting Information System.
Aberration detection
Aberration detection of HFM disease outbreak in the response system is based on the C3 algorithm of the early aberration reporting system developed by the United States Centers for Disease Control and Prevention.2,9,21–24 C3 compares the count of cases in the current day – day 0 – with the corresponding mean count and standard deviation for seven earlier days – days −9 to −3. If the calculated value of C3 surpasses a preset threshold, a warning signal is generated. Following the advice of senior epidemiologists and statisticians in the response system’s research group, the preset threshold was given a value of 1.3 for HFM disease in May 2010. This value took estimates of the response system’s general sensitivity, timeliness, specificity and positive predictive value in outbreak detection into account.
Signal generation and dissemination
Once a day, the response system searches for aberrations in the county-level incidence of HFM disease. Any warning signals generated are then automatically disseminated via short message service texts sent to the mobile phones of designated staff in the Centres for Disease Control and Prevention in the relevant counties.13,25
Investigation and feedback
A health-care professional who receives a warning signal as a text message is expected to review the HFM disease cases that triggered the signal, further assess the possibility of an outbreak – by integrating information from other sources, such as information collected by direct contact with the reporting clinical and health-care agencies and – if there then seems to be a real threat of an outbreak (which meant that the warning signal became an alert signal) – conduct a field investigation.13,25 If an HFM disease outbreak is confirmed after field investigation, it should be reported to the public health emergency reporting system.
The health-care professionals who receive warning signals are expected to complete two simple, web-based forms, as soon as possible, so that details of how the professionals proceeded with signal verification and – if appropriate – field investigation can be viewed promptly by epidemiologists at higher levels.13 In this way, high-level epidemiologists can carefully monitor and assess the risk of outbreak spread.
Reporting confirmed outbreaks
The Chinese public health emergency reporting system was initiated in 2004, to record outbreaks of infectious diseases identified by local epidemiologists. Aside from the procedures that form part of the response system, staff from local health departments are instructed to conduct a field investigation if, within 1 week, at least five HFM disease cases occur in the same setting – e.g. kindergarten or school – or at least three cases of the disease occur in the same village or community. Any outbreak confirmed by a field investigation should be reported to the public health emergency reporting system.20,26
Evaluating the response system’s effectiveness
The main objectives of our study were to evaluate the response system’s capacity for identifying HFM disease outbreaks and the response system’s impacts on the mean size and duration of an HFM disease outbreak and on the mean delays in the recording of an HFM disease outbreak to the public health emergency reporting system. The HFM disease outbreaks recorded in the public health emergency reporting system were used as the gold standard in our estimations of the response system’s sensitivity, specificity and timeliness. The number of cases detected was used as the measure of the size of an outbreak. The number of days between the onset of symptoms in the first and last known cases that were related to the outbreak was used as the estimate of outbreak duration. Sensitivity was estimated by dividing the number of HFM disease outbreaks detected by the response system, by the corresponding number of such outbreaks recorded in the public health emergency reporting system.9,27 Specificity was estimated by dividing the number of non-outbreak days on which no warning signal was generated for HFM disease – by the response system – by the total number of non-outbreak days. Time to detection was defined as the interval between the first case related to the outbreak being reported to the reporting system and the generation of the first warning signal about the outbreak by the response system.27 Time from detection to report was defined as the interval between the generation of the first warning signal about the outbreak by the response system and the report of the outbreak to the public health emergency reporting system. Time to report – which was investigated both before and after the response system was implemented – was defined as the interval between symptom onset in the first case related to the outbreak and the report of the outbreak to the public health emergency reporting system.
The mean size, duration and time to report of an HFM disease outbreak were estimated for the period 1 May 2008–30 April 2010 – i.e. before HFM disease was covered by the response system – and for the period 1 May 2010–30 April 2012 – i.e. after HFM disease was included in the response system’s remit.
Statistical analyses
We used Pearson’s χ2 test to evaluate the significance of the response system’s sensitivity in the detection of HFM disease outbreaks in three size categories: 3–10, 11–20 and more than 20 cases. Time to detection was investigated by one-way analysis of variance. Student’s t-test was used to examine whether the mean size, duration and time to report of outbreaks were significantly different before and after HFM disease was included in the response system. All analyses were implemented in version 2.14.1 of the R statistical software package (R Foundation for Statistical Computing, Vienna, Austria).
Results
Between 1 May 2008 and 30 April 2012, 5 471 108 cases and 1209 outbreaks of HFM disease were reported in China (Table 1). The number of HFM disease cases per month ranged from 7512 cases in January 2009 to 353 104 cases in May 2010, with a mean value of 113 981 (95% confidence interval, CI: 87 444–140 186). Over this period, HFM disease incidence showed marked seasonality, with a major peak – comprising almost half of all cases –in April–June and a smaller secondary peak – comprising 18.0% of cases – in September–November. Reported outbreaks, warning signals and alerts showed a similar seasonal pattern.
Table 1. Outbreaks of hand, foot and mouth disease in China, 2008–2012.
| Indicator | Period |
||||
|---|---|---|---|---|---|
| 1 May 2008–30 April 2009 | 1 May 2009–30 April 2010 | 1 May 2010–30 April 2011 | 1 May 2011–30 April 2012 | Overall | |
| Cases | |||||
| Cases reported in the case reporting systema | 757 141 | 1 256 320 | 1 576 918 | 1 880 729 | 5 471 108 |
| Outbreaks recorded by the public health emergency reporting system | 211 | 380 | 298 | 320 | 1 209 |
| Ratio of all reported casesb to those recorded in the public health emergency reporting system | 3 588:1 | 3 306:1 | 5 292:1 | 5 877:1 | 4 525:1 |
| No. of cases related to outbreaks | 4 077 | 7 376 | 4 795 | 4 956 | 21 204 |
| Ratio of all reported casesb to cases related to outbreaks | 1:186 | 1:170 | 1:329 | 1:379 | 1:258 |
| Signals | |||||
| Warning signals generated by the response systemc | – | – | 48 916 | 57 089 | 106 005 |
| Ratio of all cases to warning signalb | – | – | 32:1 | 33:1 | 33:1 |
| Alerts recorded in response systemc | – | – | 1 117 | 1 244 | 2 361 |
| Ratio of warning signals to alertsb | – | – | 44:1 | 46:1 | 45:1 |
| Detected outbreaks | – | – | 278 | 295 | 573 |
| Ratio of alerts to detected outbreaksb | – | – | 4:1 | 4:1 | 4:1 |
a Notifiable Infectious Diseases Reporting Information System.
b Rounded to an integer.
c China Infectious Disease Automated Alert and Response System.
The number of outbreaks reported per year ranged from 211 for the period 1 May 2008–30 April 2009 to 380 for the period 1 May 2009–30 April 2010. Between 1 May 2010 and 30 April 2012, 106 005 warning signals in a total of 2608 counties were generated by the response system for HFM disease (Table 1). This represents a mean of 5.6 such signals every 100 days in each of the counties that had at least one signal. Initial verification indicated that 2361 (2.2%) of the signals merited being raised to alert status and field investigation. Field investigation of the response system’s signals led to 573 HFM disease outbreaks being confirmed. The response system received the initial verification results for 94 920 (89.5%) of the signals within 24 h.
As 618 HFM disease outbreaks were recorded in the public health emergency reporting system in the period when 573 such outbreaks were identified in the response system, the overall sensitivity of the response system in the detection of HFM disease outbreaks was 92.7% (Table 2). The response system’s sensitivity was significantly higher for large outbreaks involving more than 20 cases than for small outbreaks that involved no more than 10 cases (99.3% versus 84.6%; P < 0.001). In the detection of HFM disease outbreaks, the overall specificity of the response system was 95.0% (19 74 324/2 078 361) and the overall mean time to detection was 2.1 days (95% CI: 1.8–2.3). The mean time to detection was 1.7 days for outbreaks that involved no more than 10 cases but 2.7 days for outbreaks that involved more than 20 cases. The mean time from detection to report in the public health emergency reporting system was 4.5 days (95% CI: 4.1–5.0).
Table 2. Detection of outbreaks of hand, foot and mouth disease in China, 1 May 2010–30 April 2012.
| No. of cases in outbreak | No. of outbreaks |
Performance of response systema |
|||
|---|---|---|---|---|---|
| Reported in public health emergency reporting system | Detected by response systema | Sensitivity, %b | Mean time to outbreak detection, daysc (95% CI) | ||
| 3–10 | 156 | 132 | 84.6 | 1.7 (1.3–2.1) | |
| 11–20 | 326 | 306 | 93.9 | 1.9 (1.7–2.2) | |
| > 20 | 136 | 135 | 99.3 | 2.7 (1.9–3.5) | |
| Overall | 618 | 573 | 92.7 | 2.1 (1.8–2.3) | |
CI: confidence interval.
a China Infectious Disease Automated Alert and Response System.
b Values differ significantly according to size of outbreak (P < 0.001).
c The time between the reporting of the first known case of an outbreak and the response system’s generation of the first warning signal about that outbreak. Values do not differ significantly according to size of outbreak (one-way analysis of variance; P = 0.28).
In our investigation of the data recorded before HFM disease was included in the response system, the mean size (P = 0.982), duration (P = 0.572) and time to report (P = 0.358) of the HFM disease outbreaks detected between 1 May 2008 and 30 April 2009 were similar to those of the outbreaks detected in the following 12 months. Similarly, in our investigation of the data recorded after HFM disease was included in the response system, the mean size (P = 0.443), duration (P = 0.370) and time to report (P = 0.840) of the HFM disease outbreaks detected between 1 May 2010 and 30 April 2011 were similar to those of the outbreaks detected in the following 12 months. The outbreaks recorded in the two years immediately after HFM disease was included in the response system were generally smaller than those recorded over the previous two years, with mean sizes of 15.8 and 19.4 cases, respectively (Table 3). The mean size of outbreaks that involved more than 20 cases was significantly less in the two years immediately after HFM disease was included in the response system than the corresponding value for the previous two years (29.2 versus 55 cases; P = 0.015).
Table 3. Size, duration and reporting times of hand, foot and mouth (HFM) disease outbreaks before and after response systema application, China, 2008–2012.
| No. of cases before/after inclusion of HFM disease in response systema | Outbreaks of HFM disease reported to public health emergency reporting system |
|||
|---|---|---|---|---|
| No. reported | Mean size, cases (95% CI) | Mean duration, days (95% CI) | Mean time to report, days (95% CI) | |
| Before inclusionb | ||||
| 3–10 | 161 | 6.7 (6.3–7.1) | 9.1 (8.2–10.0) | 8.1 (7.4–8.7) |
| 11–20 | 328 | 14.5 (14.2–14.8) | 14.0 (13.1–14.9) | 10.1 (9.5–10.7) |
| > 20 | 102 | 55.0 (34.3–75.8) | 28.7 (24.4–32.9) | 12.7 (11.1–14.3) |
| Overall | 591 | 19.4 (15.6–23.2) | 15.2 (14.1–16.2) | 10.0 (9.5–10.5) |
| After inclusionc | ||||
| 3–10 | 156 | 6.4 (5.9–6.8) | 8.4 (7.6–9.2) | 7.3 (6.8–7.8) |
| 11–20 | 326 | 14.7 (14.4–15.0) | 14.0 (13.2–14.7) | 9.4 (8.9–9.8) |
| > 20 | 136 | 29.2 (27.2–31.1)d | 26.0 (23.5–28.5) | 10.5 (9.5–11.5)e |
| Overall | 618 | 15.8 (15.0–16.5) | 15.2 (14.4–16.1) | 9.1 (8.7–9.5)f |
CI: confidence interval.
a China Infectious Disease Automated Alert and Response System;
b For the period 1 May 2008–30 April 2010.
c For the period 1 May 2010–30 April 2012.
d Significantly lower than corresponding value for the study period before HFM disease was included in CIDARS (P = 0.015).
e Significantly lower than corresponding value for the study period before HFM disease was included in CIDARS (P = 0.020)
f Significantly lower than corresponding value for the study period before HFMD disease was included in CIDARS (P = 0.004).
The overall mean duration of an HFM disease outbreak was estimated to be 15.2 days for the study periods before and after HFM disease was included in the response system. However, the mean duration of outbreaks that involved more than 20 cases fell from 28.7 days in the two years before HFM disease was included in the response system to 26.0 days in the following two-year period. The corresponding falls in the mean number of days taken to report an HFM disease outbreak of any size – from 10.0 to 9.1 (P = 0.004) – and an HFM disease outbreak that involved more than 20 cases – from 12.7 to 10.5 (P = 0.020) – were significant.
Discussion
Our observations indicate that the response system had good sensitivity and specificity in the detection of HFM disease outbreaks and could lead to a reduction in the eventual size of an outbreak – by shortening the reporting time and so permitting an earlier response.
Our results are consistent with previous research that has found the C3 algorithm to be useful for the detection of aberrancy in the incidence of influenza, bacillary dysentery, HFM disease and other diseases.22,23,27 We found that the response system’s sensitivity in detecting outbreaks of HFM disease that became relatively large – i.e. 99.3% for outbreaks with more than 20 cases – was significantly higher than that for outbreaks that remained small – i.e. 84.6% for outbreaks with no more than 10 cases. Perhaps the outbreaks that grow large expand relatively rapidly and quickly present a large enough deviation from the baseline value for incidence to be easily detected. However, we made no attempt to investigate how responses to the detected outbreaks affected their final size. Overall, 45 HFM disease outbreaks – that were confirmed by health professionals at a time when HFM disease was included in the response system – were not detected by the response system. All 45 remained relatively small and occurred in kindergartens, elementary schools or rural villages. Efforts should be made to increase the sensitivity of the response system – e.g. by using high-resolution spatial detection methods28–30 – to improve the prompt detection of outbreaks while they are small.
Although use of a C3 threshold of 1.3 resulted in good sensitivity, specificity and timeliness in the response system’s detection of HFM disease outbreaks, it also resulted in a low positive predictive value. The health professionals who checked the data decided that only 2.2% of the warning signals that the response system generated for HFM disease merited field investigation. One cause of the low positive predictive value is that almost all of the HFM disease cases seen in China – over 99.6% according to the data that we analysed – are sporadic and never form part of an outbreak. A temporal cluster of sporadic cases may easily trigger a false-positive warning signal in the response system. Such false signals need to be reduced by optimizing the algorithms and thresholds used for outbreak detection – perhaps according to the relevant baseline incidence of HFM disease.31 The procedures for the verification of warning signals at county level also need to be simplified, to reduce the detrimental effects of so many false-positive signals on the morale and workloads of health professionals.
The early detection of potential outbreaks is important in minimizing the impact of HFM disease.19 Inclusion of HFM disease in the national response system cut the time taken to report an outbreak of the disease by almost a day. Since the corresponding warning signals were generated a mean of 4.5 days before the outbreaks were reported, there is clearly scope to further reduce the mean time taken to report a confirmed outbreak. Early detection allows the early implementation of outbreak control measures – such as health surveys for the detection of other cases, case isolation, disinfection of affected settings, health education, promotion of hand hygiene, and closure of affected classes or schools – as well as the early treatment of cases and the prevention of the more severe complications of HFM disease.
One limitation of our study was that, for calculating the sensitivity, specificity and timeliness of the response system, we used the outbreaks reported to the public health emergency reporting system as the gold standard. It seems likely that some outbreaks of HFM disease are either never recorded by the public health emergency reporting system or are reported a long time after they have occurred. These issues need investigation. However, at the time of our study, we believed that the public health emergency reporting system was the best-functioning system for the collection of data on HFM disease outbreaks in China.
Our findings demonstrate that – if well designed and operated – an automated early warning system for outbreaks of infectious disease can help local epidemiologists identify outbreaks rapidly, thereby facilitating the prevention of outbreak spread. The response system’s design framework and methods could provide a useful example for institutes of public health in many countries.
Acknowledgements
We thank the staff members of the World Health Organization’s country office in China and the county-level Centres for Disease Control and Prevention, and the trainers of the International Field Epidemiology Training Programme in the Ministry of Public Health of Thailand. Zhongjie Li and Shengjie Lai contributed equally to this study.
Funding:
This work was supported by grants from the Ministry of Science and Technology of China (2012ZX10004-201), the Ministry of Health of China (201202006), the National Health and Medical Research Council of Australia (1002608), and the China–WHO regular budget cooperation project (WPCHN0801617 and WPCHN1002405).
Competing interests:
None declared.
References
- 1.Buckeridge DL, Okhmatovskaia A, Tu S, O’Connor M, Nyulas C, Musen MA. Understanding detection performance in public health surveillance: modeling aberrancy-detection algorithms. J Am Med Inform Assoc. 2008;15(6):760–9. 10.1197/jamia.M2799 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hutwagner L, Thompson W, Seeman GM, Treadwell T. The bioterrorism preparedness and response Early Aberration Reporting System (EARS). J Urban Health. 2003;80(2) Suppl 1:i89–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Reis BY, Kohane IS, Mandl KD. An epidemiological network model for disease outbreak detection. PLoS Med. 2007;4(6):e210. 10.1371/journal.pmed.0040210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lombardo J, Burkom H, Elbert E, Magruder S, Lewis SH, Loschen W, et al. A systems overview of the Electronic Surveillance System for the Early Notification of Community-Based Epidemics (ESSENCE II). J Urban Health. 2003;80(2) Suppl 1:i32–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Loonsk JW. BioSense–a national initiative for early detection and quantification of public health emergencies. MMWR Morb Mortal Wkly Rep. 2004. ;53Suppl:53–5. [PubMed] [Google Scholar]
- 6.Krause G, Altmann D, Faensen D, Porten K, Benzler J, Pfoch T, et al. SurvNet electronic surveillance system for infectious disease outbreaks, Germany. Emerg Infect Dis. 2007;13(10):1548–55. 10.3201/eid1310.070253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hulth A, Andrews N, Ethelberg S, Dreesman J, Faensen D, van Pelt W, et al. Practical usage of computer-supported outbreak detection in five European countries. Euro Surveill. 2010;15(36):15. [PubMed] [Google Scholar]
- 8.Cakici B, Hebing K, Grünewald M, Saretok P, Hulth A. CASE: a framework for computer supported outbreak detection. BMC Med Inform Decis Mak. 2010;10(1):14. 10.1186/1472-6947-10-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hutwagner L, Browne T, Seeman GM, Fleischauer AT. Comparing aberration detection methods with simulated data. Emerg Infect Dis. 2005;11(2):314–6. 10.3201/eid1102.040587 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kuang J, Yang WZ, Zhou DL, Li ZJ, Lan YJ. Epidemic features affecting the performance of outbreak detection algorithms. BMC Public Health. 2012;12(1):418. 10.1186/1471-2458-12-418 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Morse SS. Public health surveillance and infectious disease detection. Biosecur Bioterror. 2012;10(1):6–16. 10.1089/bsp.2011.0088 [DOI] [PubMed] [Google Scholar]
- 12.Brownstein JS, Freifeld CC, Madoff LC. Digital disease detection – harnessing the Web for public health surveillance. N Engl J Med. 2009;360(21):2153–5, 2157. 10.1056/NEJMp0900702 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yang WZ, Li ZJ, Lan YJ, Wang JF, Ma JQ, Jin LM, et al. A nationwide web-based automated system for early outbreak detection and rapid response in China. Western Pac Surveill Response J. 2011;2(1):10–5. 10.5365/wpsar.2010.1.1.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chan KP, Goh KT, Chong CY, Teo ES, Lau G, Ling AE. Epidemic hand, foot and mouth disease caused by human enterovirus 71, Singapore. Emerg Infect Dis. 2003;9(1):78–85. 10.3201/eid1301.020112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhang Y, Zhu Z, Yang W, Ren J, Tan X, Wang Y, et al. An emerging recombinant human enterovirus 71 responsible for the 2008 outbreak of hand foot and mouth disease in Fuyang city of China. Virol J. 2010;7(1):94. 10.1186/1743-422X-7-94 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhang Y, Tan XJ, Wang HY, Yan DM, Zhu SL, Wang DY, et al. An outbreak of hand, foot, and mouth disease associated with subgenotype C4 of human enterovirus 71 in Shandong, China. J Clin Virol. 2009;44(4):262–7. 10.1016/j.jcv.2009.02.002 [DOI] [PubMed] [Google Scholar]
- 17.Heymann DL. Control of communicable diseases manual. 19th ed.Washington: American Public Health Association; 2008. pp. 151–4. [Google Scholar]
- 18.Chang ZR, Zhang J, Sun JL, Zhang WD, Wang ZJ. Epidemiological features of hand, foot and mouth disease in China, 2008 - 2009. Zhonghua Liu Xing Bing Xue Za Zhi. 2011;32(7):676–80. Chinese. [PubMed] [Google Scholar]
- 19.A guide to clinical management and public health response for hand, foot and mouth disease [Internet]. Manila: World Health Organization; 2011. Available from: http://www.wpro.who.int/publications/PUB_9789290615255/en/ [cited 2013 Jan 15].
- 20.The declaration of hand, foot and mouth disease as a notifiable disease in China [Internet]. Beijing: Chinese Ministry of Health; 2008. Chinese. Available from: http://www.chinacdc.cn/jkzt/crb/szkb/jszl_2275/200805/t20080506_24699.htm [cited 2013 Feb 1].
- 21.Hutwagner L, Barson JV. Use of the early aberration reporting system (EARS) for detection of bioterrorism agent attacks. Aviat Space Environ Med. 2005;76(10):1001–2. [PubMed] [Google Scholar]
- 22.Yang P, Duan W, Lv M, Shi W, Peng X, Wang X, et al. Review of an influenza surveillance system, Beijing, People’s Republic of China. Emerg Infect Dis. 2009;15(10):1603–8. 10.3201/eid1510.081040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wang X, Zeng D, Seale H, Li S, Cheng H, Luan R, et al. Comparing early outbreak detection algorithms based on their optimized parameter values. J Biomed Inform. 2010;43(1):97–103. 10.1016/j.jbi.2009.08.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fricker RD Jr, Hegler BL, Dunfee DA. Comparing syndromic surveillance detection methods: EARS’ versus a CUSUM-based methodology. Stat Med. 2008;27(17):3407–29. 10.1002/sim.3197 [DOI] [PubMed] [Google Scholar]
- 25.Yang WZ, Lan YJ, Li ZJ, Ma JQ, Jin LM, Sun Q, et al. The application of national outbreak automatic detection and response system, China. Zhonghua Liu Xing Bing Xue Za Zhi. 2010;31(11):1240–4. Chinese. PMID:21176684 [PubMed] [Google Scholar]
- 26.Guideline for hand, foot and mouth disease control and prevention (2009 edition) [Internet]. Beijing: Chinese Ministry of Health; 2009. Chinese. Available from: http://www.chinacdc.cn/jkzt/crb/szkb/jszl_2275/200906/t20090612_24707.htm [cited 2013 Feb 1].
- 27.Li Z, Lai S, Buckeridge DL, Zhang H, Lan Y, Yang W. Adjusting outbreak detection algorithms for surveillance during epidemic and non-epidemic periods. J Am Med Inform Assoc. 2012;19e1:e51–3. 10.1136/amiajnl-2011-000126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Li XZ, Wang JF, Yang WZ, Li ZJ, Lai SJ. A spatial scan statistic for multiple clusters. Math Biosci. 2011;233(2):135–42. 10.1016/j.mbs.2011.07.004 [DOI] [PubMed] [Google Scholar]
- 29.Mammen MP, Pimgate C, Koenraadt CJ, Rothman AL, Aldstadt J, Nisalak A, et al. Spatial and temporal clustering of dengue virus transmission in Thai villages. PLoS Med. 2008;5(11):e205. 10.1371/journal.pmed.0050205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Huang SS, Yokoe DS, Stelling J, Placzek H, Kulldorff M, Kleinman K, et al. Automated detection of infectious disease outbreaks in hospitals: a retrospective cohort study. PLoS Med. 2010;7(2):e1000238. 10.1371/journal.pmed.1000238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zhang H, Lai S, Wang L, Zhao D, Zhou D, Lan Y, et al. Improving the performance of outbreak detection algorithms by classifying the levels of disease incidence. PLoS ONE. 2013;8(8):e71803. 10.1371/journal.pone.0071803 [DOI] [PMC free article] [PubMed] [Google Scholar]