Abstract
Unexpected medical care spending imposes considerable financial risk on developing country households. Based on managed care models of health insurance in wealthy countries, Colombia’s Régimen Subsidiado is a publicly financed insurance program targeted to the poor, aiming both to provide risk protection and to promote allocative efficiency in the use of medical care. Using a “fuzzy” regression discontinuity design, we find that the program has shielded the poor from some financial risk while increasing the use of traditionally under-utilized preventive services – with measurable health gains.
In developing countries, the inability to smooth consumption directly reduces welfare and leads to informal risk management strategies that stifle productive activity (Paxson 1993, Townsend 1994, Morduch 1995). Because unexpected illness is a leading source of economic risk, the expansion of health insurance is therefore a public policy priority in many parts of the developing world (Gertler and Gruber 2002, GTZ, WHO, and ILO 2005, WHO 2010, Mohanan 2012).1 Such initiatives are often large, centrally-planned programs operated exclusively through the public sector – and they focus primarily on reducing the out-of-pocket price of medical care.2
An early exception is Colombia’s Régimen Subsidiado (or “Subsidized Regime,” henceforth “SR”). Introduced in 1993, the SR is a pluralistic, publicly-financed health insurance program targeted to the poor.3 Colombians meeting a proxy means-test (determined by the Sistema de Identificación de Beneficiarios, or SISBEN) are fully-subsidized to purchase insurance from private, government-approved insurers. In contrast to the classical ‘managed competition’ model of insurance (Enthoven 1978a and 1978b), participating insurers must offer standardized benefits packages and accept standardized premiums. Insurers can, however, form restrictive medical care networks, deny reimbursement for services deemed ‘unnecessary,’ and pay health care providers in ways that encourage higher quality and lower cost medical care (through capitated payment contracts, for example – fixed payments per enrollee per month). Overall, Colombia’s SR shares features of managed care models of health insurance that emphasize cost-containment and allocative efficiency traditionally found only in wealthy countries. It therefore represents important early experience in a markedly different institutional environment.
This paper studies the impact of the SR on financial risk protection, service use, and health outcomes among Colombia’s poor. Program eligibility is supposed to be determined according to a discrete threshold in the continuous SISBEN index, so in principle we could use a regression discontinuity design to do so. Because SISBEN scores are manipulated in practice (BDO and CCRP 2000, DNP 2001, DNP 2003a, and 2003b, Fresneda 2003, Camacho and Conover 2011), we instead use underlying index components collected through independent household surveys to generate our own (un-manipulated) SISBEN score calculations. We then instrument for SR enrollment with our re-constructed eligibility measure (Hahn, Todd, and Van der Klaauw 2001). In general, our estimates are robust across a variety of parametric and non-parametric specifications.
Despite our strategy for addressing manipulation of eligibility, our approach has limitations. First, because we use household surveys to implement a “fuzzy” regression discontinuity design, our samples are relatively small. Second, we measure SISBEN index components after official SISBEN classification occurred, presumably resulting in a degree of measurement error. Third, due to financial shortfalls, many of Colombia’s municipios (hereafter, “counties”) used eligibility thresholds that fell short of the official one. Following Chay, McEwan, and Urquiola (2005), we therefore estimate and use county-specific thresholds. These limitations introduce noise into the regression discontinuity design and generally bias us against finding behavioral responses to the SR.
We first find evidence that by the mid-2000s, the SR succeeded in protecting poor Colombians from financial risk associated with the medical costs of unexpected illness. In particular, SR enrollment appears to have reduced the variability of out-of-pocket spending for inpatient care. Despite this reduction in risk, however, we observe little evidence of meaningful portfolio choice effects (changes in the composition of household assets, human capital investments, or household consumption), perhaps because the SR falls short of providing full insurance.
Our results also suggest that SR enrollment is associated with large increases in the use of traditionally under-utilized preventive services – some of which nearly doubled. Moreover, we find evidence of health improvement under the SR as well – specifically, gains along margins sensitive to the increases in preventive care that we observe. There is more mixed evidence of changes in the use of curative services (although theoretical predictions about the use of curative care are ambiguous).
We conclude by discussing the underlying behavioral mechanisms that may explain our results. Because the SR is complex and multi-faceted, it is important to note that we cannot draw firm inferences about them; we emphasize this as an important direction for future research. Overall, we highlight two mechanisms that we suspect are important: high-powered supply-side incentives and the possibility that enrollees receive care from higher-quality private sector facilities.
I. Background and Policy Context
A. Public Sector Health Insurance for Colombia’s Poor Prior to the Reform
Prior to the introduction of the SR in 1993, roughly 25% of Colombians (a subset of those with formal sector jobs) had any form of explicit health insurance (Pinto 2008). However, Colombians lacking formal insurance also had a degree of implicit insurance provided through the public sector. Specifically, they could receive medical care from public sector hospitals and clinics for a fraction of the full cost of their services; out-of-pocket payments were generally progressive and loosely based on socio-economic status. Public sector facilities, in turn, covered their losses with direct transfers from national and local governments, and health care professionals were typically paid fixed salaries that did not reward productivity. Thus, poor Colombians effectively had a degree of implicit health insurance coupled with inefficient provider incentives – and the reform that we study aimed to expand coverage while improving efficiency.
B. Overview of Colombia’s Subsidized Health Insurance Regime for the Poor
Under Law 100 in 1993, Colombia introduced the SR, a novel form of publicly-financed health insurance for the poor (Gwatkin, Wagstaff and Yazbeck 2005, Escobar 2005). Primarily through SR expansion, formal health insurance coverage in Colombia grew from about 25% of the population in 1993 to 80% in 2007 (CENDEX 2008). The SR is organized as a variant of the classical ‘managed competition’ model (Enthoven 1978a and 1978b). Beneficiaries are fully subsidized to purchase health insurance from competing health plans. During our study period (the mid-2000s), subsidies were financed by a combination of public resources including payroll taxes and national and local general revenue. These resources are transferred to county governments, which in turn are responsible for eligibility determination, enrollment, and contracting with health plans. This role of local government has important implications for our empirical analysis.
Health plans charge county health authorities a government-regulated premium per enrollee and offer a standardized package of benefits (see Appendix A for the details of these benefits).4 Participating health plans then act as group purchasers of health services for their enrollees by contracting with a network of health facilities and clinicians. Because premiums and benefit packages are standardized by law (unlike the classical ‘managed competition’ model), health plans compete for enrollees on the basis of provider networks and service quality. In practice, however, very few cities had more than one insurer during the years that we study.
Insurers’ ability to contract with health care providers (hospitals and medical groups) for more efficient service provision is a central innovation of the SR. Insurers receive premiums (fixed payments per enrollee per unit time) for all covered services, giving them strong incentives to constrain total spending. Insurers then (partially) transmit these incentives to provider organizations through capitated payment contracts, and they have the authority to deny reimbursement for services deemed inefficient.5
In the next section we describe the major demand- and supply-side incentive changes under the SR, and Section II then provides predictions based on them for health service use, out-of-pocket spending on medical care, and health outcomes.
C. Changes in Demand- and Supply-Side Incentives under the SR
There were important changes in both demand- and supply-side incentives with the introduction of the SR. On the demand-side, out-of-pocket prices for covered curative services are 10% of the full price (as opposed to 30% for poor uninsured Colombians).6 Moreover, total out-of-pocket spending per episode of illness each year is capped at half of the monthly minimum wage for SR beneficiaries – while the same cap is six times as large for uninsured patients (Decreto 2357 and Acuerdo 260 of the Consejo Nacional de Seguridad Social en Salud). Notably, preventive services are essentially free regardless of insurance status.
On the supply-side, changes in provider payment contracts created substantially different incentives for the provision of health services. Specifically, there are two types of contracts between insurers and provider organizations under the SR: capitated primary care contracts and fee-for-service specialty care contracts. For primary care, insurers pay providers fixed amounts per month for all services used by enrollees (“capitation”). These contracts create strong incentives for providers to constrain total spending on primary care and have important implications for both preventive and curative health care (as discussed in the next section). Importantly, promotion of preventive care can be a central means of reducing total expenditures.7
For specialty care, insurers generally pay providers a pre-determined fee for each covered service that they supply (i.e., on a “fee-for-service” basis). These contracts encourage the provision of all reimbursable services (both efficient and inefficient). However, SR insurers also have the authority to deny reimbursement on a case-by-case basis for inefficient specialty care (termed “utilization review”), allowing them to limit wasteful service use.8
D. Eligibility for the SR
Eligibility for the SR is determined using a poverty-targeting index called SISBEN (or Sistema de Identificación de Beneficiarios). The original SISBEN index consisted of fourteen components measuring different aspects of household well-being (such as housing material, access to public utilities, ownership of durable assets, demographic composition, educational attainment, and labor force participation – for a complete description, see Appendix B).9 On each dimension, households are classified according to mutually exclusive, collectively exhaustive categories with varying weights assigned to each category; these weights vary between urban and rural areas. A household’s SISBEN score is then calculated by summing points across components. Possible scores range from 0 to 100 (with 0 being the most impoverished) and are divided into six strata. Households scoring in SISBEN strata 1 and 2 (the lowest strata) are eligible for the SR (below 48 in urban areas, below 31 in rural areas).10
E. Eligibility and Enrollment in Practice
Although eligibility for the SR increases the likelihood of enrollment, neither one necessarily implies the other for at least three reasons: misclassification or manipulation of SISBEN scores, shortfalls in local government revenue, and enrollment that preceded SISBEN enumeration.11
First, both local governments and households have incentives to manipulate SISBEN scores. Local governments receive fixed transfers from the national government for each resident they enroll, creating incentives to maximize enrollment. The selective enrollment of key constituents can also provide political benefits (Camacho and Conover 2011). Households prefer enrollment over “uninsurance” as well because co-payments are lower for SR beneficiaries than for those lacking formal insurance. Consistent with both types of incentives, there is evidence of considerable SISBEN score manipulation between 1997 and 2003 (Camacho and Conover 2011).12
Second, most local governments lack sufficient revenue to finance the enrollment of all eligible residents. According to law, those with lower SISBEN scores and those belonging to specific targeted groups (such as children under five and pregnant women) are therefore prioritized for enrollment.13 This means that many counties use de facto eligibility thresholds that fall below the uniform national threshold.
Third, some counties began enrolling residents in the SR before all of their residents had been classified using SISBEN. These counties instead used other means-test criteria such as residents’ estrato, a neighbourhood-level measure of socio-economic status used to establish electricity prices paid by local households.
In general, these realities of the program’s implementation have two broad implications for our empirical analyses (which we discuss in greater detail in Section IIIB). One is the necessity of an empirical strategy that addresses manipulation of SISBEN scores. The other is that de facto county threshold must be estimated (because they are not officially reported).
F. Previous Studies
Several previous empirical papers have studied Colombia’s SR as well (see Giedion and Uribe (2009) for a comprehensive review). Trujillo, Portillo, and Vernon (2005) use propensity score matching to compare SR enrollees to observationally similar uninsured Colombians, finding that the SR is associated with greater medical care use. Giedion et al. (2009) also use propensity score matching and find that SR enrollment is associated with more visits to health care providers, higher vaccination coverage rates, and fewer reports of not seeking medical care for financial reasons. Gaviria, Medina, and Mejía (2007) instrument for SR enrollment using length of time a household head lived in his/her current place of residence and report that SR enrollment is associated with better self-reported health, more preventive and curative outpatient care, and fewer hospitalizations. Finally, matching official SISBEN score data with birth records, Camacho and Conover (2008) use a regression discontinuity design in two samples: a county lacking clear evidence of manipulation and selected counties observed shortly after SR implementation. They find that SR enrollment is associated with increased birth weight and better APGAR scores but not antenatal care use, medical supervision of deliveries, or probability of hospital delivery. Relative to previous studies of the SR, our paper employs a different strategy for addressing manipulation of program eligibility, uses an approach that disentangles the role of the SR from other public programs using SISBEN, and studies a broader range of behavioral responses to health insurance.14
II. Empirical Predictions on the Interaction of Supply- and Demand-Side Incentives
Although we emphasize the centrality of changes in supply-side incentives under the SR, out-of-pocket prices for covered services also fell. This section therefore considers the joint effect of supply- and demand-side changes in formulating predictions about changes in risk protection, the use of preventive and curative services, and health outcomes. Section IV then provides empirical evidence on each.
Risk Protection and Out-of-Pocket Medical Spending
Protecting households against medical care costs associated with unexpected illness is a central objective of health insurance. As Appendix A shows, the SR covers many of the most expensive services including trauma care, dialysis, and major joint replacement (hips and knees, for example). It also caps total out-of-pocket spending per episode of illness each year at half of the monthly minimum wage. The SR should therefore reduce the variability of out-of-pocket medical spending. Assuming that the price elasticity of demand for medical care is less than one, the SR should also reduce total out-of-pocket spending for medical care.
Preventive Health Services
Most preventive services in Colombia are free regardless of insurance status (i.e., free both for SR enrollees and the uninsured), so the main difference in incentives for preventive care originate on the supply-side. Primary care providers are paid on a capitated basis, so they have strong incentives to limit total primary care spending. Increasing preventive service use can reduce the need for more costly curative care – and can therefore be cost-saving – so capitated primary care incentives are likely to increase preventive care use.15
An opposing force at work is ex ante moral hazard: SR enrollees may have weaker incentives to use preventive services because they pay less for curative care (Nordquist and Wu 1976, Phelps 1978). Although we fail to find evidence of ex ante moral hazard (as shown in Section IVE) and there is little evidence of it in other studies (Kenkel 2000), our preventive care estimates reflect the net effect of these forces.16 Because preventive services generate important positive externalities (both pecuniary and infectious disease-related), increases in their use presumably improve welfare.17
Curative Medical Care
Three changes under the SR are likely to influence the use of curative medical care: reductions in out-of-pocket prices, increases in the use of preventive services, and supply-side incentives for limiting total medical spending. First, for negative price elasticities of demand, reductions in out-of-pocket prices will increase the use of curative care. This increase is inefficient under standard assumptions (ex post moral hazard); however, curative care in developing countries may produce positive externalities, and there may also be important credit constraints. Second, any increases in preventive service use may reduce the use of curative care (an efficient result). Third, both capitation and utilization review produce incentives for providers to limit the use of curative medical care. Some reductions may be efficient (counterbalancing demand-side incentives leading to ex post moral hazard) while others may be inefficient (leading to “stinting” – see for example Ellis and McGuire (1990), Holmstrom and Milgrom (1991), Ma and McGuire (1997), and McGuire (2000)). Predictions about changes in curative care under the SR as well as their welfare implications are therefore ambiguous.
Health Outcomes
Both preventive and curative services are inputs into health production. If at least one of these two types of care increases and neither of them decreases, health should presumably improve to some degree. Alternatively, the prediction is ambiguous if one type increases and the other decreases. In our empirical analyses, we are able to examine the prevalence of infectious diseases common among children (diarrhea, cough and fever) as well as the number of days lost to illness.
III. Data and Empirical Strategy
A. Data
Our empirical approach requires household survey data containing three types of information: (1) enrollment in the SR, (2) components of the SISBEN index (enabling us to simulate SR eligibility), and (3) potential behavioral responses and outcomes of interest (both welfare-improving and distortionary). There are two candidate Colombian household surveys that meet these criteria: the Encuestas de Calidad de Vida (ECV) and the Demographic and Health Surveys (DHS). The ECVs are nationally-representative household surveys designed to measure socioeconomic well-being and “quality of life,” broadly defined. The DHS data reports detailed fertility, health, and socio-economic information for nationally-representative samples of fertile age women (defined as ages 15–49) and their households. Because the de facto implementation of the SR occurred in 1996/1997, we use the 2003 ECV and the 2005 DHS for our analyses.18 Table 1 shows descriptive statistics by type of behavior/outcome for the full samples as well as those with and without SR coverage.
Table 1.
Descriptive Statistics
| Variable | Total
|
Data Source | Not Enrolled in the Subsidized Regime
|
Enrolled in the Subsidized Regime
|
Data Source | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | N | Mean | SD | N | Mean | SD | N | |||
| Outcome Variables | |||||||||||
| Risk Protection, Consumption Smoothing, and Portfolio Choice | |||||||||||
| Individual Inpatient Medical Spending | 10,794 | 129,777 | 4219 | ECV | 11,360 | 129,227 | 2252 | 10,145 | 130,435 | 1967 | ECV |
| Individual Outpatient Medical Spending | 2,118 | 22,565 | 4218 | ECV | 2,513 | 20,170 | 2249 | 1,666 | 25,019 | 1969 | ECV |
| Variability of Individual Inpatient Medical Spending | 21,935 | 127,975 | 4219 | ECV | 26,338 | 126,615 | 2252 | 16,894 | 129,363 | 1967 | ECV |
| Variability of Individual Outpatient Medical Spending | 5,477 | 21,993 | 4218 | ECV | 7,343 | 19,017 | 2249 | 3,347 | 24,796 | 1969 | ECV |
| Individual Education Spending | 7,588 | 20,279 | 3567 | ECV | 7,501 | 23,234 | 1874 | 7,684 | 16,407 | 1693 | ECV |
| Household Education Spending | 35,145 | 48,468 | 4222 | ECV | 34,089 | 52,464 | 2253 | 36,352 | 43,428 | 1969 | ECV |
| Total Spending on Food | 274,881 | 217,392 | 4096 | ECV | 279,128 | 201,735 | 2171 | 270,091 | 233,756 | 1925 | ECV |
| Total Monthly Expenditure | 654,552 | 599,861 | 966 | ECV | 688,065 | 716,382 | 479 | 621,590 | 455,559 | 487 | ECV |
| Has Car | 0.03 | 0.16 | 3334 | DHS | 0.03 | 0.18 | 1758 | 0.02 | 0.15 | 1576 | DHS |
| Has Radio | 0.61 | 0.49 | 3334 | DHS | 0.60 | 0.49 | 1758 | 0.62 | 0.49 | 1576 | DHS |
| Medical Care Use | |||||||||||
| Preventive Physician Visit | 0.47 | 0.50 | 4222 | ECV | 0.39 | 0.49 | 2253 | 0.57 | 0.49 | 1969 | ECV |
| Number of Growth Development Checks Last Year | 1.16 | 1.81 | 1167 | DHS | 1.00 | 1.75 | 683 | 1.38 | 1.87 | 484 | DHS |
| Curative Care Use (Not Conditional on Health Status) | 0.06 | 0.24 | 4222 | ECV | 0.06 | 0.23 | 2253 | 0.07 | 0.26 | 1969 | ECV |
| Primary Care | 0.05 | 0.21 | 4222 | ECV | 0.04 | 0.20 | 2253 | 0.06 | 0.23 | 1969 | ECV |
| Medical Visit - Specialist | 0.02 | 0.12 | 4222 | ECV | 0.01 | 0.12 | 2253 | 0.02 | 0.13 | 1969 | ECV |
| Hospital Stay | 0.08 | 0.26 | 4222 | ECV | 0.07 | 0.25 | 2253 | 0.08 | 0.28 | 1969 | ECV |
| Medical Visit for Chronic Disease | 0.58 | 0.49 | 564 | ECV | 0.52 | 0.50 | 262 | 0.64 | 0.48 | 302 | ECV |
| Curative Care Use among Children (Not Conditional on Health Status) | 0.31 | 0.46 | 1161 | DHS | 0.29 | 0.45 | 680 | 0.34 | 0.48 | 481 | DHS |
| Health Status | |||||||||||
| Child Days Lost to Illness | 0.60 | 2.01 | 1161 | DHS | 0.65 | 2.14 | 680 | 0.53 | 1.82 | 481 | DHS |
| Cough, Fever Diarrhea | 0.56 | 0.50 | 1167 | DHS | 0.56 | 0.50 | 682 | 0.56 | 0.50 | 485 | DHS |
| Any Health Problem | 0.65 | 0.48 | 1161 | DHS | 0.64 | 0.48 | 680 | 0.66 | 0.47 | 481 | DHS |
| Birthweight (KG) | 3.26 | 0.57 | 897 | DHS | 3.25 | 0.53 | 534 | 3.27 | 0.63 | 363 | DHS |
| Behavioral Distortions | |||||||||||
| Drank Alcohol during Pregnancy | 0.11 | 0.31 | 998 | DHS | 0.12 | 0.32 | 504 | 0.10 | 0.30 | 494 | DHS |
| Number of Drinks per Week during Pregnancy | 2.75 | 9.76 | 110 | DHS | 3.15 | 10.85 | 60 | 2.28 | 8.36 | 50 | DHS |
| Months Child Breastfed | 12.58 | 10.87 | 946 | DHS | 11.15 | 10.18 | 578 | 14.83 | 11.53 | 368 | DHS |
| Folic Acid During Pregnancy | 0.54 | 0.50 | 988 | DHS | 0.56 | 0.50 | 500 | 0.53 | 0.50 | 488 | DHS |
| Number Months Folic Acid during Pregnancy | 3.96 | 2.42 | 515 | DHS | 4.05 | 2.39 | 266 | 3.86 | 2.45 | 249 | DHS |
| Contributory Regime Enrollment | 0.09 | 0.29 | 4222 | ECV | 0.17 | 0.38 | 2253 | 0.00 | 0.00 | 1969 | ECV |
| Contributory Regime Enrollment | 0.14 | 0.34 | 3334 | DHS | 0.26 | 0.44 | 1758 | 0.00 | 0.00 | 1576 | DHS |
| Other Health Insurance | 0.44 | 0.50 | 4222 | ECV | 0.82 | 0.39 | 2253 | 0.00 | 0.00 | 1969 | ECV |
| Other Health Insurance | 0.01 | 0.09 | 3334 | DHS | 0.01 | 0.12 | 1758 | 0.00 | 0.00 | 1576 | DHS |
| Uninsured | 0.00 | 0.06 | 4222 | ECV | 0.01 | 0.08 | 2253 | 0.00 | 0.00 | 1969 | ECV |
| Uninsured | 0.38 | 0.49 | 3334 | DHS | 0.73 | 0.45 | 1758 | 0.00 | 0.00 | 1576 | DHS |
| Baseline Demographic Variables | |||||||||||
| Balance | |||||||||||
| Household Head Age | 46.81 | 14.81 | 3334 | DHS | 47.36 | 15.37 | 1758 | 46.18 | 14.14 | 1576 | DHS |
| Household Head Age | 46.58 | 14.79 | 4222 | ECV | 45.71 | 15.12 | 2253 | 47.57 | 14.35 | 1969 | ECV |
| Completed Elementary School | 0.18 | 0.39 | 3333 | DHS | 0.18 | 0.38 | 1757 | 0.19 | 0.39 | 1576 | DHS |
| Completed Elementary School | 0.19 | 0.39 | 3764 | ECV | 0.18 | 0.39 | 1985 | 0.19 | 0.39 | 1779 | ECV |
| Completed Secondary School | 0.20 | 0.40 | 3333 | DHS | 0.21 | 0.41 | 1757 | 0.19 | 0.39 | 1576 | DHS |
| Completed Secondary School | 0.07 | 0.26 | 3764 | ECV | 0.08 | 0.27 | 1985 | 0.07 | 0.25 | 1779 | ECV |
| Household Head Completed Elementary School | 0.30 | 0.46 | 3334 | DHS | 0.29 | 0.45 | 1758 | 0.31 | 0.46 | 1576 | DHS |
| Household Head Completed Elementary School | 0.28 | 0.45 | 4222 | ECV | 0.27 | 0.45 | 2253 | 0.28 | 0.45 | 1969 | ECV |
| Household Head Completed Secondary School | 0.02 | 0.15 | 3334 | DHS | 0.02 | 0.13 | 1758 | 0.03 | 0.18 | 1576 | DHS |
| Household Head Completed Secondary School | 0.02 | 0.13 | 4222 | ECV | 0.01 | 0.11 | 2253 | 0.02 | 0.15 | 1969 | ECV |
| Student Received School Grant | 0.08 | 0.26 | 1305 | ECV | 0.05 | 0.22 | 651 | 0.10 | 0.30 | 654 | ECV |
| Benefits to Buy House | 0.01 | 0.08 | 4222 | ECV | 0.00 | 0.06 | 2253 | 0.01 | 0.10 | 1969 | ECV |
| Attended Training | 0.05 | 0.21 | 3010 | ECV | 0.06 | 0.23 | 1593 | 0.04 | 0.19 | 1417 | ECV |
| Household in Hogar Comunitario program | 0.10 | 0.30 | 4222 | ECV | 0.09 | 0.29 | 2253 | 0.11 | 0.31 | 1969 | ECV |
| Services from Bienstar Familiar | 0.18 | 0.38 | 4222 | ECV | 0.16 | 0.37 | 2253 | 0.20 | 0.40 | 1969 | ECV |
Notes: All data summarized is from samples of “urban” individuals within two SISBEN index points of county-specific eligibility thresholds in either the 2003 Encuesta de Calidad de Vida (ECV) or the 2005 Demographic and Health Survey (DHS) (as indicated in the last column). SISBEN index calculations are described in detail in Appendix 2, and estimation of county-specific eligibility thresholds is presented in Section IIIB. The first group of three columns present summary statistics for the entire bandwidth of 2 sample, the second group for those not enrolled in the Subsidized Regime, and the third group for those enrolled in the Subsidized Regime.
As our empirical strategy requires, we calculate household-level SISBEN scores to simulate SR eligibility because simulated eligibility should not reflect manipulation of SISBEN scores (Camacho and Conover 2011).19 However, not all household surveys contain all necessary components of the SISBEN index. Appendix B provides a complete description of the SISBEN components present in each survey.20 We impute values using ordered probit models for the few variables that are missing (firm size and per-capita income in the DHS and primary roof material in both surveys). Estrato is also missing for some households and we impute them on the basis of the most common in the household’s neighborhood.
B. Empirical Strategy
Instrumenting for Enrollment with Simulated Eligibility
In principle, the SISBEN index’s SR eligibility threshold can be used to study behavioral responses associated with SR enrollment. This discontinuity induces an abrupt shift in eligibility (and enrollment) along otherwise smooth distributions of household characteristics; coincident shifts in behaviors and outcomes can reasonably be linked to the program. However, adverse or propitious selection into eligibility – or manipulation according to unobserved household characteristics, as discussed in Section IE – is likely to bias the estimates of interest (McCrary 2008).
To circumvent this difficulty, we employ an instrumental variables strategy closely resembling one proposed by Hahn, Todd, and Van der Klaauw (2001). Conceptually, we seek to reconstruct ‘true’ SISBEN scores when both official SISBEN scores and observed SR enrollment reflect manipulation. To do so, we calculate SISBEN scores for each household in the ECV and DHS data and then use calculated scores to instrument for SR enrollment (for prominent examples of simulated instruments, see Currie and Gruber (1996a and 1996b), and Cutler and Gruber (1996), and Hoxby (2001)).21
Using urban households with simulated SISBEN scores near the urban eligibility threshold (we do not use rural households because of sufficiently inconsistent application of the rural scale)22, we could in principle begin by estimating the following first-stage equation for individuals i in household h:
| (1) |
where enroll is an indicator for whether or not individual i is enrolled in the SR, below is an indicator for simulated SISBEN score lying below the eligibility threshold, SISBEN is simulated SISBEN score, and estrato is a dummy variable for an estrato category (a neighborhood-level measure of socio-economic status used to establish electricity prices paid by local households). Using Two-Stage Least Squares (2SLS), we could then estimate the following second-stage equation:
| (2) |
instrumeting for enroll with below. The relationship between behavioral outcomes of interest (outcome) and SR enrollment would then be captured by estimates of the parameter λ.
Estimating County-Specific Eligibility Thresholds
As described in Section IE, financial shortfalls led many Colombian counties to use SR eligibility thresholds at SISBEN scores below the official national threshold. We therefore use county-specific eligibility thresholds. In addition to improving the strength of our first stage, this approach offers another key benefit: because some local governments use the official national threshold for other public benefits, changes in outcomes observed at county-specific SR thresholds will not reflect behavioral responses to other public programs. (Section IVA shows that participation in other public programs is not discontinuous at county-specific thresholds.)
Exact county-specific eligibility thresholds are unknown, so we estimate them following Chay, McEwan, and Urquiola (2005). Specifically, using our full samples, we establish county-specific breaks in SR eligibility at the SISBEN score that maximize the goodness-of-fit of a model of SR enrollment as a function of a dichotomous indicator for whether or not a household’s score falls below the threshold.23 This approach establishes thresholds that maximize the percentage of individuals correctly classified as eligible in each county. Threshold means in the ECV and DHS are 45.03 and 45.83, respectively, and their interquantile ranges are 4.96 and 3.89. Intuitively, estimated thresholds are positively correlated with current county income (the sum of taxes, transfers from the state, and non-tax income) and negatively correlated with the share of households having unmet basic needs.24
We then use county-specific thresholds to re-code the variable below for each individual i in households h and Colombian counties c and estimate the following first stage equation:
| (3) |
where below is now an indicator for whether or not individual i’s simulated SISBEN score falls below the eligibility threshold in the individual’s county c, SISBEN_diff is the difference between an individual’s simulated SISBEN score and the estimated eligibility threshold in the individual’s county (i.e., relative SISBEN score), μc represents county fixed effects (allowing us to focus on within-county variation in simulated eligibility across county-specific thresholds), and all other variables are defined as in equation (1). To adhere transparently to the identifying assumption that individuals with simulated SISBEN scores very near the threshold are comparable with the exception of their eligibility, we conservatively focus on individuals whose calculated scores lie within two index points of the county-specific cutoff (our main estimates persist across various bandwidths, as shown in Section IVF).25
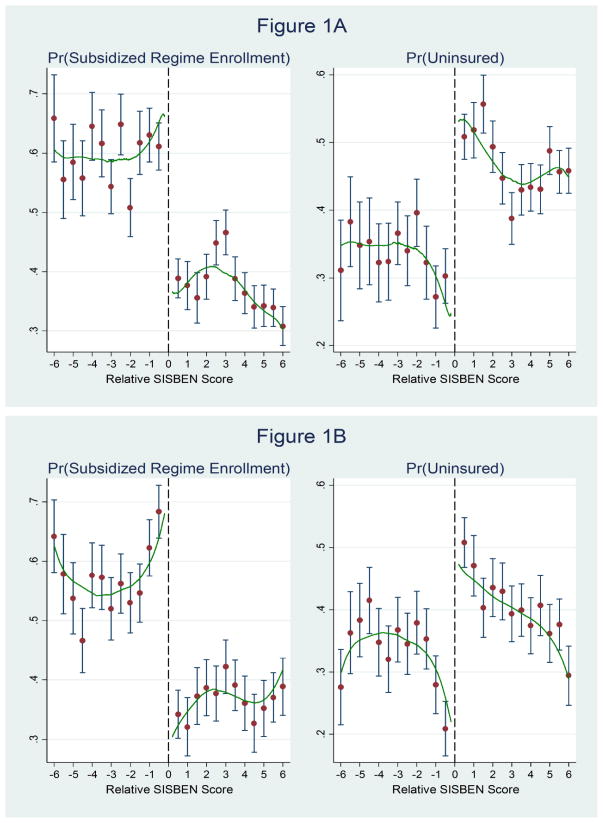
Figures 1A and 1B use ECV and DHS data to show SR enrollment and “uninsurance” by simulated SISBEN score relative to county-specific eligibility thresholds. Each county’s threshold is normalized to zero, and the figure then shows means and 95% confidence intervals for each SISBEN index integer relative to the threshold as well as non-parametric kernel density plots on either side. The figure illustrates large discrete increases in the probability of enrollment and concomitant decreases in the probability of uninsurance at the threshold ranging between 25 to 30 percentage points. Figures 2A and 2B show the enrollment and “uninsurance” separately by regions of Colombia as well. It is worth noting than SR enrollment falls short of 100% at low (calculated) SISBEN scores. This may not only be due to mistargeting, but also to our use of household survey data (rather than official data) to construct SISBEN scores
Figure 1. Subsidized Regime Enrollment and ‘Uninsurance’ across SISBEN Eligibility Thresholds.
Notes: Source of Figure A is ECV 2003 and of Figure B is DHS 2005
Figure 2.
Subsidized Regime Enrollment and ‘Uninsurance’ across SISBEN Eligibility Thresholds by Region
Using our re-coded variable below to instrument for enroll, we then estimate the following equation by 2SLS:
| (4) |
where the estimate of interest is the estimate of λ.26 Section IVF shows that our results are robust across bandwidths to including higher-order relative SISBEN score polynomials, using interactions between relative SISBEN scores and simulated eligibility, and excluding county fixed effects. We also estimate λ using local linear regression without any covariates other than relative SISBEN score.27
Limitations of the Empirical Strategy
Although our approach addresses key irregularities in SR implementation, it also has shortcomings. First, because the ECV and DHS household survey data that we use to calculate SISBEN scores was collected after official SISBEN classification, our calculations presumably include measurement error (even absent manipulation of official SISBEN status). Second, our estimates of county-specific eligibility thresholds presumably do not match those used in practice exactly, introducing additional noise into the relationship between our measure of simulated eligibility and actual enrollment. Third, manipulation of official SISBEN scores further weakens the strength of the first stage relationship. Fourth, our sample sizes are relatively small in the neighborhood of the eligibility thresholds. Overall, these limitations clearly compromise the power of our estimates (few are significant at significance thresholds below α=0.10) and suggest that our results should also be interpreted as lower bounds.
IV. Results
This section presents empirical evidence on a variety of important behavioral responses to the SR. We begin by demonstrating that both background characteristics not influenced by the program and participation in other social programs using SISBEN are balanced across estimated SR eligibility thresholds. We then investigate the effectiveness of health insurance in protecting households against financial risk (and possibly changing the optimal composition of household spending and assets). Next, we study changes in the use of traditionally under-utilized preventive services in light of the SR’s emphasis on allocative efficiency. In doing so, we also examine changes in health outcomes that are sensitive to the use of important preventive services. We then analyze how SR enrollment is related to changes in the use of curative medicine. To investigate possible behavioral distortions, we also test for reductions in private health investments (ex ante moral hazard) and insurance ‘crowd-out’ associated with SR enrollment. Finally, we assess the robustness of our estimates through a variety of additional parametric and non-parametric specifications.28
A. Balance across Discontinuous Eligibility Thresholds
Our empirical approach assumes that no individual or household characteristics – other than SR enrollment – that could influence the outcomes of interest vary discontinuously across our estimated eligibility thresholds. To test this assumption, Table 2 shows results obtained by estimating equations (3) and (4) for individual attributes that could not reasonably change in response to SR enrollment (such as age or educational attainment among adults). Consistent with our assumption, the estimates are not generally distinguishable from zero. (Examining the distribution of simulated SISBEN scores across eligibility discontinuities, Appendix C shows evidence in support of this assumption as well.)
Table 2.
Balance Across Eligibility Thresholds
| Panel A
| ||||||||
|---|---|---|---|---|---|---|---|---|
| Outcome | Household Head Age | Household Head Age | Completed Elementary School | Completed Elementary School | Completed Secondary School | Completed Secondary School | Household Head Completed Elementary School | Household Head Completed Elementary School |
| 2SLS Estimate, Subsidized Regime Enrollment | 4.38 [3.05] | 3.05 [7.68] | 0.01 [0.08] | −0.15 [0.10] | 0.03 [0.07] | 0.05 [0.05] | −0.09 [0.12] | −0.37 [0.24] |
| Intent to Treat Estimate | 1.77 [1.22] | 0.79 [1.84] | 0.01 [0.03] | −0.04** [0.02] | 0.01 [0.03] | 0.01 [0.01] | −0.04 [0.05] | −0.10** [0.05] |
| First Stage Estimate, Below Eligibility Threshold | 0.40*** [0.04] | 0.26*** [0.07] | 0.40*** [0.04] | 0.25*** [0.06] | 0.40*** [0.04] | 0.25*** [0.06] | 0.40*** [0.04] | 0.26*** [0.07] |
| First Stage F-Statistic | 125.75 | 14.08 | 125.91 | 17.02 | 125.91 | 17.02 | 125.75 | 14.08 |
|
| ||||||||
| OLS Estimate | −0.04 [0.66] | 1.62*** [0.55] | 0.00 [0.01] | 0.00 [0.01] | −0.01 [0.02] | −0.01 [0.01] | 0.02 [0.02] | −0.01 [0.02] |
| Mean for those Not Enrolled in the Subsidized Regime | 47.36 | 45.71 | 0.18 | 0.18 | 0.21 | 0.08 | 0.29 | 0.27 |
| Observations | 3,334 | 4,222 | 3,333 | 3,764 | 3,333 | 3,764 | 3,334 | 4,222 |
| Data Source | DHS | ECV | DHS | ECV | DHS | ECV | DHS | ECV |
| Panel B
| |||||||
|---|---|---|---|---|---|---|---|
| Outcome | Household Head Completed Secondary School | Household Head Completed Secondary School | Student Received School Grant | Benefits to Buy House | Attended Training | Household in Hogar Comunitario Program | Services from Bienestar Familiar |
| 2SLS Estimate, Subsidized Regime Enrollment | −0.02 [0.03] | −0.04 [0.07] | −0.06 [0.11] | 0.02 [0.01] | 0.01 [0.04] | 0.03 [0.08] | −0.04 [0.13] |
| Intent to Treat Estimate | −0.01 [0.01] | −0.01 [0.02] | −0.01 [0.02] | 0.00** [0.00] | 0.00 [0.01] | 0.01 [0.02] | −0.01 [0.03] |
| First Stage Estimate, Below Eligibility Threshold | 0.40*** [0.04] | 0.26*** [0.07] | 0.21*** [0.09] | 0.26*** [0.07] | 0.27*** [0.06] | 0.26*** [0.07] | 0.26*** [0.07] |
| First Stage F-Statistic | 125.75 | 14.08 | 5.17 | 14.08 | 23.45 | 14.08 | 14.08 |
|
| |||||||
| OLS Estimate | 0.01* [0.01] | 0.01 [0.01] | 0.03 [0.02] | 0.00** [0.00] | −0.02*** [0.00] | 0.01 [0.01] | 0.02 [0.02] |
| Mean for those Not Enrolled in the Subsidized Regime | 0.02 | 0.01 | 0.05 | 0.00 | 0.06 | 0.09 | 0.16 |
| Observations | 3,334 | 4,222 | 1,305 | 4,222 | 3,010 | 4,222 | 4,222 |
| Data Source | DHS | ECV | ECV | ECV | ECV | ECV | ECV |
Notes: Individual-level “urban” data for those within two SISBEN index points of county-specific eligibility thresholds from the 2003 ECV and 2005 DHS. Dependent variables are shown at the top of each column. The first row shows 2SLS estimates for enrollment in the Subsidized Regime (SR), instrumenting for SR enrollment using simulated eligibility. The second row shows reduced-form intent-to-treat estimates for simulated SISBEN score falling below the county-specific eligibility threshold. The third row shows first stage estimates from OLS regressions of Subsidized Regime enrollment on an indicator for falling below the county-specific eligibility threshold. All specifications
Significant at the 1 percent level.
Significant at the 5 percent level.
Significant at the 10 percent level.
We then consider whether or not our estimates from equation (4) could be attributed to participation in other public programs that also use the SISBEN index. Before investigating this possibility directly, we first note that it is unlikely because these programs use the uniform national eligibility threshold, while we estimate and utilize de facto county-specific thresholds for the SR – many of which fall below the uniform national threshold. To confirm this, we re-estimate equations (3) and (4) using a dichotomous indicator for participation in these other programs – including job training, home mortgage subsidies, education vouchers, Hogares Comunitarios (a large child care program), and services provided by the Instituto Colombiano de Bienestar Familiar (the largest social welfare agency in Colombia) – as the dependent variable in equation (4).29 Table 2 presents these results, suggesting that participation in other programs is also balanced across county-specific SR eligibility thresholds.
B. Financial Risk Protection and Portfolio Choice
Although a key innovation of the SR is its emphasis on allocative efficiency, a central objective of any health insurance program is to provide protection against financial risk. We therefore begin by examining the relationship between SR enrollment and both level and variability of out-of-pocket medical spending. To construct our variability measure, we first calculate mean individual spending separately among those enrolled and those not enrolled in the SR. For each individual, we then measure the difference between each individual’s spending and the mean among those with the same enrollment status, constructing our variability measure as the absolute value of this difference. We analyze outpatient and inpatient out-of-pocket spending (within the past twelve months) separately and emphasize the latter because of idiosyncrasies in how outpatient spending is reported.30
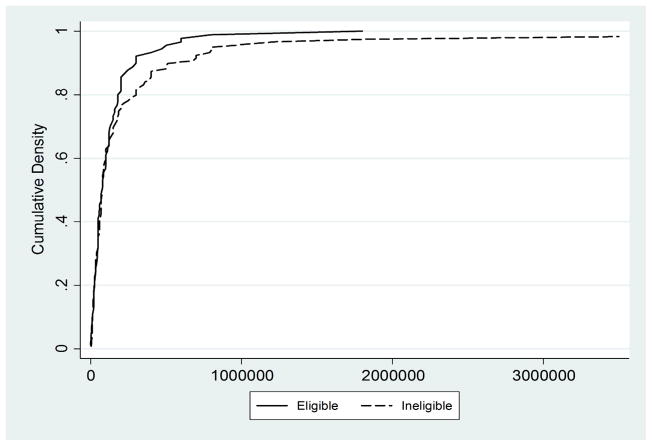
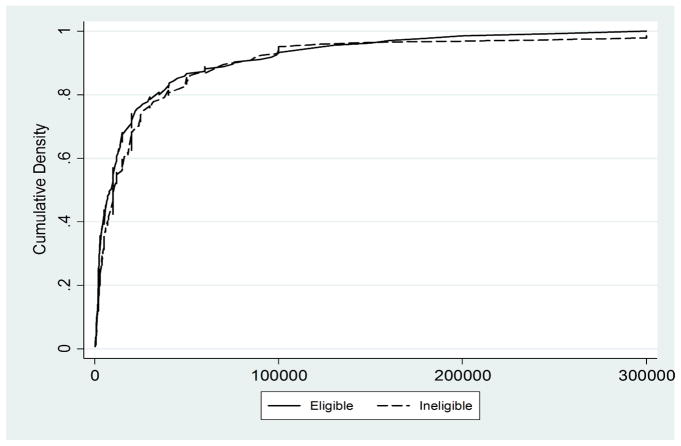
We first graphically examine shifts in the distribution of medical spending associated with simulated eligibility for the SR. Figure 3 shows cumulative density functions for inpatient medical spending in the preceding year separately for those falling above and below county-specific thresholds (using our sample of those within two index points of the cutoff).31 Both distributions are heavily right-skewed, but mass in the distribution for those who are eligible (those below the threshold) falls to the left of the distribution for those who are ineligible. No clearly comparable pattern is present for outpatient medical spending (Figure 4). Overall, these figures suggest that SR eligibility is associated with reductions in right-tail inpatient medical spending – a pattern consistent with risk protection.32
Figure 3. Individual Inpatient Medical Spending (Among those within Two Points of County-Specific Eligibility Thresholds).
Notes: Source ECV 2003
Figure 4. Individual Outpatient Medical Spending (Among those within Two Points of County-Specific Eligibility Thresholds).
Notes: Source ECV 2003
The first four columns of Panel A in Table 3 then present econometric results obtained by estimating equations (3) and (4) for medical spending by type. The first row presents IV estimates for SR enrollment, and the second row reports intent-to-treat (ITT) estimates for simulated SR eligibility (estimates for a dummy variable coding whether or not an individual falls below the eligibility threshold obtained by OLS regressions of outcomes on this dummy and the other covariates in equation 4). The first column suggests that SR enrollment lowers mean inpatient spending by about 60,000 pesos (α=0.10), around a 30% reduction among those using any inpatient services. Perhaps more importantly for assessing protection against financial risk, the third column shows that SR enrollment is associated with reductions in the variability of inpatient medical spending (α=0.05).33 There is no statistically significant association for outpatient care. Appendix D Figure 1 graphically shows all outcomes examined in Panel A across county-specific eligibility thresholds (essentially, graphical versions of our intent-to-treat analyses).
Table 3.
Risk Protection and Portfolio Choice
| Panel A: Risk Protection
| ||||
|---|---|---|---|---|
| Outcome | Individual Inpatient Medical Spending | Individual Outpatient Medical Spending | Variability of Individual Inpatient Medical Spending | Variability of Individual Outpatient Medical Spending |
| 2SLS Estimate, Subsidized Regime Enrollment | −58,870* [33,263] | 3,562 [2,702] | −67,499.38** [32,906] | 167.57 [2,417] |
| Intent to Treat Estimate | −15,108* [8,888] | 918.23 [821] | −17322.90* [9,120] | 43.20 [626] |
|
| ||||
| First Stage Estimate, Below Eligibility Threshold | 0.26*** [0.07] | 0.26*** [0.07] | 0.26*** [0.07] | 0.26*** [0.07] |
| First Stage F-Statistic | 13.91 | 14.01 | 13.91 | 14.01 |
| OLS Estimate | −5,655 [3,898] | −1,204*** [342] | −13,888*** [3,893] | −4,387*** [357] |
|
| ||||
| Mean for those Not Enrolled in the Subsidized Regime | 11,359.86 | 2,512.98 | 26338.40 | 7342.59 |
| Observations | 4,219 | 4,218 | 4,219 | 4,218 |
| Data Source | ECV | ECV | ECV | ECV |
| Panel B: Portfolio Choice
| ||||||
|---|---|---|---|---|---|---|
| Outcome | Individual Education Spending | Household Education Spending | Total Spending on Food | Total Monthly Expenditure | Has Car | Has Radio |
| 2SLS Estimate, Subsidized Regime Enrollment | −341.68 [3,781] | 30,366 [25,055] | 32,136 [103,540] | −33,826 [278,060] | 0.01 [0.04] | 0.17 [0.11] |
| Intent to Treat Estimate | −84.72 [945] | 7,815 [4,880] | 8,709 [28,491] | −14,036 [115,736] | 0.01 [0.01] | 0.07 [0.05] |
| First Stage Estimate, Below Eligibility Threshold | 0.25*** [0.06] | 0.26*** [0.07] | 0.27*** [0.06] | 0.41*** [0.12] | 0.40*** [0.04] | 0.40*** [0.04] |
| First Stage F-Statistic | 19.28 | 14.08 | 18.80 | 12.18 | 125.75 | 125.75 |
|
| ||||||
| OLS Estimate | 122.82 [231] | 2,952.32*** [902] | −12,036 [10,330] | −39,273 [58,730] | −0.01 [0.01] | 0.03 [0.02] |
| Mean for those Not Enrolled in the Subsidized Regime | 7,501 | 34,089 | 279,128 | 688,065 | 0.03 | 0.60 |
| Observations | 3,567 | 4,222 | 4,096 | 966 | 3,334 | 3,334 |
| Data Source | ECV | ECV | ECV | ECV | DHS | DHS |
Notes: Individual-level “urban” data for those within two SISBEN index points of county-specific eligibility thresholds from the 2003 ECV and 2005 DHS. Dependent variables are shown at the top of each column. The first row shows 2SLSestimates for enrollment in the Subsidized Regime (SR), instrumenting for SR enrollment using simulated eligibility. The second row shows reduced-form intent-to-treat estimates for simulated SISBEN score falling below the county-specific eligibility threshold. The third row shows first stage estimates from OLS regressions of Subsidized Regime enrollment on an indicator for falling below the county-specific eligibility threshold. All specifications also include SISBEN score, distance from the county-specific threshold, estrato dummy variables, and county fixed effects. Standard errors (clustered by county) are shown in brackets below each estimate.
Significant at the 1 percent level.
Significant at the 5 percent level.
Significant at the 10 percent level.
Overall, the results shown in Table 3 Panel A suggest that SR enrollment is associated with meaningful risk protection benefits. By reducing household exposure to financial risk, SR enrollment could also produce meaningful changes in the composition of household assets, human capital investments, and household consumption (i.e., portfolio choice effects). Specifically, it may increase investments not previously undertaken because of costly informal risk-management activities (such as precautionary saving). Panel B of Table 3 presents estimates for durable goods not used to construct the SISBEN index (car and radio ownership) as well as household education and consumption expenditures. In general, it implies that SR enrollment is not associated with discernible portfolio choice effects (perhaps because the SR falls short of providing full insurance).
C. Preventive Service Use and Health Status
As described earlier, a key innovation of the SR is its focus on improving allocative efficiency in medical care. In particular, increasing the use of highly beneficial preventive services – many of which produce large positive externalities – is likely to improve welfare. These externalities are due both to reduced rates of infectious disease transmission and to reduced curative care costs borne by others through risk pools.
The first two columns of Table 4 report estimates for different types of preventive care use obtained from equations (3) and (4) (Appendix D Figure 2 shows graphical versions of the intent-to-treat analyses). In general, they suggest substantial increases in the use of preventive health care services.34 Specifically, SR enrollment is associated with a 29 percentage point increase in the probability of a preventive physician visit in the past year (a 75% increase; α=0.01). Importantly, the SR is also associated with 1.50 more growth-monitoring and well-care visits in the past year, a 50% increase relative to uninsured children (α=0.05). These well-care visits are a principal way of addressing important childhood health problems (parents receive nutritional advice, iron supplements, and de-worming medications, for example – which are important for strengthening children’s immune systems and making them less susceptible to major childhood illnesses such as severe diarrhea and acute respiratory infections/pneumonia).35
Table 4.
Use of Preventive Medical Care and Health Status
| Use of Preventive Care | Health Status (Children) | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| Outcome | Preventive Physician Visit | Number of Growth Dev. Checks Last Year | Child Days Lost to Illness | Cough, Fever, Diarrhea | Any Health Problem | Birthweight (KG) |
| 2SLS Estimate, Subsidized Regime Enrollment | 0.29*** [0.11] | 1.50** [0.69] | −1.40** [0.65] | −0.18 [0.17] | −0.06 [0.18] | 0.26 [0.29] |
| Intent to Treat Estimate | 0.08*** [0.03] | 0.55** [0.25] | −0.49** [0.20] | −0.07 [0.06] | −0.02 [0.06] | 0.11 [0.12] |
| First Stage Estimate, Below Eligibility Threshold | 0.26*** [0.07] | 0.36*** [0.07] | 0.35*** [0.07] | 0.37*** [0.07] | 0.35*** [0.07] | 0.41*** [0.09] |
| First Stage F-Statistic | 14.08 | 25.24 | 23.46 | 25.19 | 23.46 | 19.10 |
|
| ||||||
| OLS Estimate | 0.17*** [0.01] | 0.33*** [0.12] | −0.04 [0.17] | 0.01 [0.04] | 0.03 [0.04] | 0.04 [0.05] |
| Mean for those Not Enrolled in the Subsidized Regime | 0.39 | 1.00 | 0.65 | 0.56 | 0.64 | 3.25 |
| Observations | 4,222 | 1,167 | 1,161 | 1,167 | 1,161 | 897 |
| Data Source | ECV | DHS | DHS | DHS | DHS | DHS |
Notes: Individual-level “urban” data for those within two SISBEN index points of county-specific eligibility thresholds from the 2003 ECV and 2005 DHS. Dependent variables are shown at the top of each column. The first row shows 2SLS estimates for enrollment in the Subsidized Regime (SR), instrumenting for SR enrollment using simulated eligibility. The second row shows reduced-form intent-to-treat estimates for simulated SISBEN score falling below the county specific eligibility threshold. The third row shows first stage estimates from OLS regressions of Subsidized Regime enrollment on an indicator for falling below the county-specific eligibility threshold. All specifications also include SISBEN score, distance from the county-specific threshold, estrato dummy variables, and county fixed effects. Standard errors (clustered by county) are shown in brackets below each estimate.
Significant at the 1 percent level.
Significant at the 5 percent level.
Significant at the 10 percent level.
We then investigate whether or not health status has improved under the SR – in particular, dimensions of health that are sensitive to the use of preventive care. Although our preventive physician visit variable is not service-specific, our measure of childhood growth and development checks should correspond directly with infectious disease prevalence. Columns three through six of Table 4 show estimates for child health outcomes linked to preventive care use. SR enrollment is associated with 1.4 fewer child days absent from usual activities due to illness in the past month (α=0.05). Enrollment is also associated with an 18 percentage point reduction in the self-reported incidence of cough, fever, or diarrhea among children in the preceding two weeks (but it is not statistically significant at conventional levels). Appendix D Figure 2 shows graphical versions of the intent-to-treat analyses for these health outcomes as well.36 Because these health gains can be linked to increases in preventive service use, they are also likely to improve welfare.
D. Use of Curative Medical Care
As Section II discusses, there are a variety of competing incentives and other forces influencing curative medical care under the SR. These include reductions in out-of-pocket prices, increases in the use of preventive services, and supply-side incentives for limiting total medical spending. Predictions about changes in curative service use under the SR – and their welfare implications – are therefore ambiguous, but they remain a central interest of policymakers and are important for assessing the costs of Colombia’s innovative health insurance reform.
Table 5 reports estimates for various categories of curative care obtained from equations (3) and (4) (Appendix D Figure 3 shows graphical versions of the intent-to-treat analyses). We find that SR enrollment is associated with a 13 percentage point increase in reported physician visits because of health problems within the past 30 days (α=0.05). There is no change in use of curative care among children, which may be due to improvements in child health associated with SR enrollment (as Table 4 shows). Finally, there is no meaningful relationship at conventional significance levels between participation in the SR and hospitalizations.
Table 5.
Use of Curative Medical Care
| Outcome | Curative Use (Not Conditonal on Health Status) | Curative Use among Children (Not Conditional on Health Status) | Medical Visit for Chronic Disease | Hospital Stay |
|---|---|---|---|---|
| 2SLS Estimate, Subsidized Regime Enrollment | 0.13** [0.05] | −0.00 [0.16] | 0.51* [0.28] | −0.04 [0.11] |
| Intent to Treat Estimate | 0.03* [0.02] | 0.00 [0.06] | 0.18*** [0.06] | −0.01 [0.03] |
| First Stage Estimate, Below Eligibility Threshold | 0.26*** [0.07] | 0.35*** [0.07] | 0.35*** [0.10] | 0.26*** [0.07] |
| First Stage F-Statistic | 14.08 | 23.46 | 13.49 | 14.08 |
|
| ||||
| OLS Estimate | 0.03*** [0.01] | 0.07* [0.04] | 0.13*** [0.03] | 0.02** [0.01] |
| Mean for those Not Enrolled in the Subsidized Regime | 0.06 | 0.29 | 0.52 | 0.07 |
| Observations | 4,222 | 1,161 | 564 | 4,222 |
| Data Source | ECV | DHS | ECV | ECV |
Notes: Individual-level “urban” data for those within two SISBEN index points of county-specific eligibility thresholds from the 2003 ECV and 2005 DHS. Dependent variables are shown at the top of each column. The first row shows 2SLS estimates for enrollment in the Subsidized Regime (SR), instrumenting for SR enrollment using simulated eligibility. The second row shows reduced-form intent-to-treat estimates for simulated SISBEN score falling below the county specific eligibility threshold. The third row shows first stage estimates from OLS regressions of Subsidized Regime enrollment on an indicator for falling below the county-specific eligibility threshold. All specifications also include SISBEN score, distance from the county-specific threshold, estrato dummy variables, and county fixed effects. Standard errors (clustered by county) are shown in brackets below each estimate.
Significant at the 1 percent level.
Significant at the 5 percent level.
Significant at the 10 percent level.
E. Ex Ante Moral Hazard and Insurance Crowd-Out
Protection from financial risk associated with unexpected illness weakens private incentives for costly health protection (ex ante moral hazard) (Pauly 1968). Because we find evidence of greater risk protection, we investigate how protective private health behaviors not directly linked to medical care change with SR enrollment.37 As Table 6 Panel A and Appendix D Figure 4 show, however, we find no meaningful change in breastfeeding or maternal investments in fetal health (alcohol, drug, or tobacco use during pregnancy; or prenatal dietary supplementation with iron, calcium, or folic acid), suggesting little ex ante moral hazard associated with SR enrollment.38
Table 6.
Behavioral Distortion – Ex ante Moral Hazard and Insurance Crowd-out
| Panel A: Ex-Ante Moral Hazard
| |||
|---|---|---|---|
| Outcome | Drank Alcohol during Pregnancy | Months Breastfed as Child | Folic Acid During Pregnancy |
| 2SLS Estimate, Subsidized Regime Enrollment | −0.10 [0.11] | −0.23 [5.36] | 0.10 [0.18] |
| Intent to Treat Estimate | −0.04 [0.04] | −0.07 [1.64] | 0.04 [0.07] |
| First Stage Estimate, Below Eligibility Threshold | 0.40*** [0.07] | 0.31*** [0.07] | 0.41*** [0.07] |
| First Stage F-Statistic | 28.83 | 19.00 | 30.12 |
|
| |||
| OLS Estimate | −0.02 [0.02] | 4.02*** [0.91] | 0.02 [0.03] |
| Mean for those Not Enrolled in the Subsidized Regime | 0.12 | 11.15 | 0.56 |
| Observations | 998 | 946 | 988 |
| Data Source | DHS | DHS | DHS |
| Panel B: Insurance Crowd-Out
| ||||||
|---|---|---|---|---|---|---|
| Outcome | Contributory Regime Enrollment | Uninsured | Other Health Insurance | Contributory Regime Enrollment | Uninsured | Other Health Insurance |
| Intent to Treat Estimate | −0.02 [0.02] | −0.23*** [0.06] | −0.00 [0.00] | −0.05** [0.02] | −0.35*** [0.04] | −0.01* [0.01] |
|
| ||||||
| Mean for those Not Enrolled in the Subsidized Regime | 0.17 | 0.01 | 0.82 | 0.26 | 0.73 | 0.01 |
| Observations | 4,222 | 4,222 | 4,222 | 3,334 | 3,334 | 3,334 |
| Data Source | ECV | ECV | ECV | DHS | DHS | DHS |
Notes: Individual-level “urban” data for those within two SISBEN index points of county-specific eligibility thresholds from the 2003 ECV and 2005 DHS. Dependent variables are shown at the top of each column. The first row shows 2SLS estimates for enrollment in the Subsidized Regime (SR), instrumenting for SR enrollment using simulated eligibility. The second row shows reduced-form intent-to-treat estimates for simulated SISBEN score falling below the county-specific eligibility threshold. Intent-to-treat estimates only are reported for the crowd-out analyses of other insurance types (the last six columns). The third row shows first stage estimates from OLS regressions of Subsidized Regime enrollment on an indicator for falling below the county-specific eligibility threshold. All specifications also include SISBEN score, distance from the county-specific threshold, estrato dummy variables, and county fixed effects. Standard errors (clustered by household) are shown in brackets below each estimate.
Significant at the 1 percent level.
Significant at the 5 percent level.
Significant at the 10 percent level.
Manipulation of official SISBEN scores suggests that Colombians perceive benefits of SR enrollment, so we also investigate the possibility that SR enrollment displaces other forms of explicit health insurance.39 Table 6 Panel B also presents intent-to-treat (ITT) estimates obtained by estimating equation (3) with dichotomous indicators for Regimen Contributivo enrollment, other forms of health insurance (those for the military, police officers, and certain industrial groups like oil industry workers, for example), and “uninsurance” as dependent variables. The Regimen Contributivo estimates are generally small (−0.02 in the ECV and minus;0.05 in the DHS) and the latter is statistically significant (α=0.05), suggesting that some modest crowding-out of formal insurance may have occurred.
F. Robustness
To investigate the robustness of our results, we estimate a variety of alternative parametric and non-parametric specifications based on our main estimating equations. First, we re-estimate equations (3) and (4) using SISBEN score bandwidths ranging between two and four. Second, at each bandwidth we estimate specifications that include higher order polynomials of relative SISBEN scores (including squared, cubic, and fourth power terms) as well as models that include interactions between relative SISBEN scores and simulated eligibility (although allowing SISBEN gradients to vary on either side of the eligibility threshold should matter little given our narrow bandwidth). Third, we re-estimate specifications that do not include county fixed effects (at each bandwidth), allowing us also to make cross-county comparisons among individuals with identical simulated SISBEN scores but that fall on opposite sides of county-specific eligibility thresholds. Finally, we also estimate models using non-parametric local linear regression.40 As Tables 1–4 of Appendix E show that our results are generally robust (with some variation in precision) across these alternative bandwidths and specifications.
G. Heterogeneity and External Validity
While RD estimates can have good internal validity, their external validity is often limited because they typically utilize a sample only in the neighborhood of the discontinuity (Imbens and Lemieux 2008, Lee and Lemieux 2010). However, because SR eligibility thresholds vary by county, our empirical strategy allows us to investigate the external validity of our estimates by extending equation (4) to include interactions between absolute SISBEN score and SR enrollment.41 This allows us to test for heterogeneity by SISBEN score, a summary measure of socio-economic status. As Appendix F Tables 1–4 show, we find little evidence of heterogeneous effects, suggesting that our estimates are not sensitive to local variation in SISBEN scores and may therefore apply to a broader range of the Colombian population.42 We note, however, that the interaction terms’ standard errors are large, so our power to detect heterogeneity is limited.
V. Conclusion
This paper studies the role of Colombia’s Régimen Subsidiado in protecting the poor against financial risk, influencing their use of health services, and ultimately affecting their health status. Unusual among middle- and low-income countries at the time of its introduction, the SR is a publicly-financed health insurance program with features of managed care emphasizing allocative efficiency that are traditionally only found in wealthy countries. We find evidence that the SR provides some protection against financial risk and is associated with greater use of preventive services having positive externalities – as well as with measurable health gains among children.
Pinpointing the mechanisms through which complex insurance programs such as SR work is an important topic of future research. In our case, because preventive services are generally free regardless of insurance status, one plausible interpretation of the increase in prevention that we observe links them to the SR’s high-powered supply-side incentives (if providers with capitated contracts believe that prevention is cost-saving). Another potentially important channel is patient substitution from public to private sector providers contracting with insurance plans under the SR (if private providers were more likely to supply preventive care). Although we suspect that these two mechanisms may be most salient, we cannot rule out others (individual feeling more comfortable going to the doctor when insured, the provision of insurance making the universal entitlement to preventive care more salient, etc.).
We conclude by emphasizing that the welfare-improving potential of SR has yet to be fully realized. For example, a variety of political concessions followed the creation of the SR – including exemptions from the end of government subsidies as well as requirements that insurers contract with public facilities for a minimum share of the services that they finance. These concessions presumably limit the ability of health plans to contract with medical care providers in ways that best encourage higher quality and lower cost services.
Acknowledgments
We are grateful to Orazio Attanasio, Jay Bhattacharya, Adriana Camacho, Pedro Carneiro, Ken Chay, Will Dow, Alan Garber, Ursula Giedion, Mike Grossman, Ted Joyce, Robert Kaestner, Carlos Medina, Costas Meghir, Imran Rasul, anonymous referees, and numerous seminar participants for helpful suggestions; to Luis Carlos Ortiz, Renata Pardo, Licerole Ruiz, Sandra Sterling, and Elisa Torrenegra for discussions about the health policy context in Colombia; to the Departamento Nacional de Planeación (DNP), the Departamento Administrativo Nacional de Estadística (DANE), and Profamilia for data and SISBEN index information; to Adriana Ruiz for GIS assistance; and to the Economic and Social Research Council (RES-167-25-0124), Economic and Social Research Council-NCRM (ES/I03685X/1), Advanced ERC Grant (249612) on “Exiting Long Run Poverty: The Determinants of Asset Accumulation in Developing Countries”, the Inter-American Development Bank, the National Institute of Child Health and Human Development (K01 HD053504), and the Stanford Center on the Demography and Economics of Health and Aging for financial support. Soledad Giardili, Carolina Mejia, Nicole Smith, and Julieta Trias provided excellent research assistance. We alone are responsible for the views in this paper as well as all errors.
Footnotes
For example, one study finds that 5% of Latin American households spend 40% or more of ‘non-subsistence’ income on medical care each year (Xu et al. 2003). As Gertler and Gruber (2002) note, there are two major costs of illness: medical care costs and reduced labor income. Health insurance (our focus) addresses the former, while disability insurance addresses the latter.
See Abel-Smith (1992); Dow et al. (1997); WHO (2000); WHO Commission on Macroeconomics and Health (2001); Gertler and Solon (2002); Dow, Gonzalez, and Rosero-Bixby (2003); Dow and Schmeer (2003); Gakidou et al. (2006); Pauly et al. (2006); Hughes and Leethongdee (2007); Wagstaff (2007); Wagstaff and Yu (2007); O’Donnell et al. (2008); Pauly, Blavin, and Meghan (2008); and Gruber, Hendren, and Townsend (2012).
According to Article 153 of Law 100 (authorizing the creation of the SR), one of the SR’s guiding principles is Proteccion Integral: “The System of Social Security in health will provide health care to the population in: education, information, health promotion and prevention, diagnostic, treatment and rehabilitation in quantity and quality according to the Plan Obligatorio de Salud.”
During our study period, the benefits package of the SR (Plan Obligatorio de Salud Subsidiado) emphasized coverage for primary and basic outpatient services, drugs, and some catastrophic care. There was limited coverage for specialist services, and there were substantial gaps in coverage for hospital care.
Provider organizations, in turn, must transmit the incentives they face to individual clinicians whom they employ. Our interviews with stakeholders in the Colombian health care system suggest that organizations solve this agency problem through non-financial rather than payment-based incentives (systematic data on organizational incentives and clinician contracts is unfortunately unavailable).
The Colombian Ministry of Social Protection maintains a fee schedule (SOAT) regulating out-of-pocket prices. For example, the full price for a physician consultation was 17,300 pesos in 2007 and 18,460 pesos in 2008 (approximately US $10). Medical facility social workers assess uninsured patients’ “ability to pay” and may charge them sliding scale out-of-pocket fees (greater than 10% of the full price) on a case-by-case basis.
Many medical professionals believe that increasing prevention reduces overall medical spending – whether or not this is true depends on prices, the health production function, and competing risks. Cohen, Neumann and Weinstein (2008) find that 20% of preventive measure in the US are cost saving.
Utilization review does little to promote services traditionally used sub-optimally.
Eligibility also varies within households because certain demographic groups (including pregnant women and young children) are prioritized for enrollment.
SISBEN eligibility shifts abruptly at each county’s cabecera boundary, an administrative demarcation formally distinguishing urban and rural parts of each county and loosely corresponding to the fringe of public utility infrastructure. Distinct urban and rural SISBEN scales are applied to households on corresponding sides of the boundary, differing both in component parts and in the weighting of response categories for each component. We implemented a research design exploiting these urban/rural index differences, but inconsistent application of the rural index and data limitations prevent us from drawing meaningful conclusions from it. In this paper we therefore focus on urban eligibility.
Administrative mistakes in the enrollment process are also important.
Using results from the 2005 population census, the Colombian newspaper El Tiempo reports that there are more SR enrollees than residents in some counties (El Tiempo, October 26, 2006). Camacho and Conover (2011) show that the distribution of official SISBEN scores exhibits both large leftward shifts in density over time and the formation of a mass point just to the left of the national eligibility threshold in urban areas. Neither are present in Colombian household surveys. The former suggests misrepresentation by households, while the latter suggests misrepresentation by enumerators or officials.
The laws formalizing this prioritization are Acuerdos 244 and 253 of the Consejo Nacional de Seguridad Social en Salud. This prioritization also means that although SISBEN scores are calculated at the level of family “nucleus,” individuals within families can vary in enrollment status; we observe this in our household survey data.
See Card, Dobkin, and Maestas (2008), Card, Dobkin, and Maestas (2009), Chandra, Gruber, and McKnight (2010a), and Anderson, Dobkin, and Gross (2012) for recent regression discontinuity studies of health insurance in the United States. For recent work on the United States using other methodologies, see Doyle (2005), Dafny and Gruber (2005), Finkelstein (2007), Finkelstein and McKnight (2008), Kolstad and Kowalski (2010), Chandra, Gruber, and McKnight (2010b), and Kowalski (2011).
One randomized controlled trial in the US and another in the UK show that capitation increases preventive service use (Manning et al. 1984, Lennon et al. 1990). This finding is also consistent with the evidence from observational studies summarized by Miller and Luft (1994) and more recent research by Keenan et al. (2009).
The RAND Health Insurance Experiment reports no sizeable or significant effect of insurance coverage on health behaviors (smoking, drinking, and exercise) (Newhouse and the Insurance Experiment Group 1993). Medicare coverage has also been reported not to increase unhealthy behaviors (Dave and Kaestner 2006).
Popular conditional cash transfer programs – including the Familias en Acción program in Colombia – aim to increase the use of preventive services even though they are otherwise available for free. At least eleven developing countries have introduced such conditional cash transfer programs (Fiszbein and Schady 2009).
There was also a Colombian DHS survey conducted in 2000, but it is much smaller and contains few outcome variables of interest. We do not use the 1997 wave of the ECV because SR enrollment was still very low in that year.
Reliable official SISBEN scores are also not available in the datasets that we use.
In theory, SISBEN scores should be calculated at the family (or “nucleus”) level. However, we treat entire households as families given reports that SISBEN enumerators adopted this definition in practice due to difficulties in conforming to the technical definition.
We emphasize “old” SISBEN scores – those calculated using the official scale in effect between the beginning of the SR and 2003. Enrollees eligible only under the old scale were not disenrolled with the introduction of the “new scale,” and the old (but not the new) eligibility discontinuity is evident in the 2005 DHS.
The combination of smaller sample size and inconsistent application of the scale in rural areas means that our first-stage relationships are considerably weaker than in urban areas. In the DHS, the first-stage F-statistics are about 9 for the sample of children (N=574) and about 3 for the sample of mothers (N=302). In the ECV, the first-stage F-statistics are about 18, but the size of the rural sample is roughly one quarter of the urban one (1318 vs. 4129).
There are 84 counties in the ECV and 220 counties in the DHS. We exclude individuals from a few counties using two criteria related to having very few observations in some counties. One is having the first percentile in the SISBEN score distribution lie above the national threshold or the 99th percentile score lie below the national threshold. The other is having an estimated threshold with those below it having relatively lower SR enrollment rates than those above it. The total number of observations excluded for these reasons is minor (3.8% of the sample in the ECV data and 5.2% of the sample in the DHS data). Estimated thresholds are constrained to be lower than 49 to allow for measurement error.
To assess this, we ran an OLS regression of county-specific eligibility thresholds on current county income and the share of households in the county having unmet basic needs (a composite indicator that collapses across household population density, water source, toilet availability at home, education of household head, ratio of employed household members to all household members, and children’s school attendance rate). Using the ECV sample, the estimate for current county income is 0.0091 with a standard error of 0.004; in the DHS, the estimate is 0.0043 with a standard error of 0.002. For the share of households with unmet basic needs, the estimates are −0.0456 and −0.0444 with standard errors of 0.024 and 0.015, respectively.
Because eligibility thresholds vary by county, our approach essentially averages across sample respondents with different absolute SISBEN scores. To investigate how our estimates vary with absolute SISBEN score, we also estimate variants of equation (4) below with interactions between SR enrollment and absolute SISBEN score (instrumenting for this term with interactions between an indicator for falling below county-specific thresholds and absolute SISBEN score) and find insignificant estimates for this interaction term (see Section IVG).
We estimate equations (3) and (4) using linear models; marginal probabilities computed using bivariate probit models yield similar results to the 2SLS estimates for dichotomous outcomes examined throughout the paper. We calculate our standard errors clustered by county.
For comparison, we also estimate equation (4) by OLS and show the results at the bottom of our tables.
As expected, power is lower in all analyses if we use the uniform national threshold rather than estimated county-specific ones. In contrast to the F statistics shown in our main tables, using the uniform national threshold yields first stage F statics of 4.7 in the ECV and 18 in the DHS. Even so, many of our key results on health care use and health outcomes are nonetheless present when we use the uniform national threshold.
The program Empleo en Acción (a workfare program active in 2003 but abolished in 2004) is the only public program of which we are aware that used the uniform national SISBEN eligibility threshold for which the 2003 ECV does not contain data. Participation in the program was low (only 7.4% of those in SISBEN strata 1 or 2) and provided no benefits directly related to health (it paid 60% of the minimum wage to individuals who worked on official program projects an average of at least 30 hours per week for 2.4 months) (IFS-SEI-Econometria 2005). We do not have information about participation in Familias en Acción, a Colombian conditional cash transfer program, but the eligibility threshold for this program (36) is considerably lower, falling more than two standard deviations below the mean of our estimated SR thresholds.
The ECV 2003 question about outpatient spending in the preceding 30 days excludes outpatient costs associated with illness ultimately leading to hospitalization; the inpatient expenditure question asks about all inpatient spending in the past 12 months.
These graphs do not correspond exactly to our formal RD estimates for several reasons. One is that they only include observations with positive expenditures and hence do not capture differential selection into any spending between those above vs. below the eligibility threshold. Another is that using our bandwidth of two sample, they depict mean differences between those above vs. below the eligibility threshold (rather than differences between the two groups as one converges to the threshold from above vs. below). Conducting a Kolmogorov-Smirnov test for equality of distributions, we are unable to reject the null hypothesis of equality, presumably because of these limitations and small sample sizes when conditioning on any spending. They are nonetheless suggestive.
These figures may understate the magnitude of risk protection under the SR for two reasons: (1) some people may not receive medical care at all, but nonetheless incur non-medical financial expenses due to poor health, and (2) the figures show densities by eligibility rather than enrollment status (because enrollment is endogenous).
Although this result is unsurprising given that Colombia’s reform caps the amount that SR enrolees are required to pay out-of-pocket, it cannot be taken for granted in a developing country context. For example, Wagstaff and Lindelow (2008) find that health insurance in China increases financial risk due to a combination of poor regulation and asymmetric information.
This increase in preventive care use dominates any ex ante moral hazard (which would reduce prevention – although Section IVE suggests no evidence of ex ante moral hazard).
See Fogel (1994), Santos et al. (2001), Alderman (2007), Currie, Decker, and Lin (2008), Galasso and Umapathi (2009), and Linnemayr and Alderman (2011) on the relationship between preventive care and child health.
Interestingly, for some of the more statistically pronounced results (such as physician visits for preventive care and children’s healthy days lost due to illness), the graphical pattern of results shown in Figure 2 Appendix D closely resemble the graphical pattern enrollment in the SR shown in Figure 1: a more or less flat relationship to the left of the threshold, and a monotonic relationship to the right of the threshold. Although suggestive, these shape similarities must still be interpreted cautiously.
More generally, private health behaviors and public health services could theoretically be either complements or substitutes for publicly provided health services. While reductions in the price of medical care may raise the return to private health investments given competing risks, cheaper health services could also instead ‘crowd-out’ costly private health behaviors (Dow, Holmes, Philipson, and Sala-i-Martin 1999, Murphy and Topel 2003).
We cannot rule-out the possibility that social desirability bias in reporting might attenuate a true effect.
Formal sector employees are mandated to enroll in an employment-based health insurance system called Regimen Contributivo. This mandate holds even for individuals with SISBEN scores falling below the SISBEN eligibility threshold for the SR.
Specifically, we use local linear regression functions with triangle kernels to estimate conditional means of outcome variables (conditioning on SISBEN_diff) on either side of the eligibility threshold, and we repeat this estimation process for enrollment in the SR. We then construct Wald statistics using differences in the estimated conditional means of the outcome variable on either side of the threshold as numerators and the difference in the conditional mean of SR enrollment on either side of the threshold as the denominator. We estimate our standard errors using 250 bootstrap replications. Details of the implementation can be found in Nichols (2007).
Specifically, we estimate: outcomeihc = φ + λenrollihc + θSISBENh + δ(enrollihc×SISBENh) + ψSISBEN_diffhc + Σkπkestratohk + μc + ξihc, using belowhc and (belowhc×SISBENh) as instruments. All variables are defined as in equations (3) and (4).
Contributor Information
Grant Miller, Email: ngmiller@stanford.edu, Center for Health Policy/Center for Primary Care and Outcomes Research, Stanford University, 117 Encina Commons, Stanford, CA 94305-6019, USA, and National Bureau of Economic Research.
Diana Pinto, Email: dpinto@iadb.org, Inter-American Development Bank, 1300 New York Avenue, N.W., Washington, DC 20577, USA.
Marcos Vera-Hernández, Email: m.vera@ucl.ac.uk, Department of Economics, University College London, Gordon street, London, WC1E 6BT, UK, and Institute for Fiscal Studies (IFS).
References
- Abel-Smith Brian. Health Insurance in Developing Counties: Lessons from Experience. Health Policy and Planning. 1992;7(3):215–226. doi: 10.1093/heapol/7.3.215. [DOI] [PubMed] [Google Scholar]
- Alderman Harold. Improving Nutrition Through Community Growth Promotion: Longitudinal Study of the Nutrition and Early Child Development Program in Uganda. World Development. 2007 Aug;35(8):1376–1389. [Google Scholar]
- Anderson Michael, Dobkin Carlos, Gross Tal. The Effect of Health Insurance Coverage on the Use of Medical Services. American Economic Journal: Economic Policy. 2012;4(1):1–27. [Google Scholar]
- Arrow Kenneth. Uncertainty and the Welfare Economics of Medical Care. The American Economic Review. 1963;53:941–973. [Google Scholar]
- BDO International and Corporación Centro Regional de Población (CCRP) Evaluation of SISBEN: Efficiency, Institutional Efficacy of the Identification, Classification and Beneficiary Selection Processes. Bogotá: Ministry of Health; 2000. [Google Scholar]
- Bhushan I, Bloom E, Clingingsmith D, Hong R, King E, Kremer M, Loevinsohn B, Schwartz B. Contracting for Health: Evidence from Cambodia. Harvard University; 2006. Unpublished Manuscript. [Google Scholar]
- Black Robert E, Morris Saul S, Bryce Jennifer. Where and Why are 10 Million Children Dying Every Year? The Lancet. 2003;361:2226–2234. doi: 10.1016/S0140-6736(03)13779-8. [DOI] [PubMed] [Google Scholar]
- Camacho Adriana, Conover Emily. Centro de Estudios sobre Desarrollo Económico (CEDE) Working Paper 14. Universidad de Los Andes; 2008. Effects of Subsidized Health Insurance on Newborn Health in a Developing Country. [Google Scholar]
- Camacho Adriana, Conover Emily. Manipulation of Social Program Eligibility. American Economic Journal: Economic Policy. 2011;3(2):41–65. [Google Scholar]
- Card David, Dobkin Carlos, Maestas Nicole. The Impact of Nearly Universal Coverage on Health Care: Evidence from Medicare. American Economic Review. 2008;98(5):2242–2258. doi: 10.1257/aer.98.5.2242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Card David, Dobkin Carlos, Maestas Nicole. Does Medicare Save Lives? Quarterly Journal of Economics. 2009;124(2):597–636. doi: 10.1162/qjec.2009.124.2.597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CENDEX. Resultados de la Encuesta Nacional de Salud 2007. 2008 Power point presentation available online at: http://www.cendex.org.co.
- Chandra Amitabh, Gruber Jonathan, McKnight Robin. Patient Cost-Sharing in Low Income Populations. American Economic Review Papers and Proceedings. 2010a;100(2):303–308. doi: 10.1257/aer.100.2.303. [DOI] [PubMed] [Google Scholar]
- Chandra Amitabh, Gruber Jonathan, McKnight Robin. Patient Cost-Sharing and Hospitalization Offsets in the Elderly. American Economic Review. 2010b;100(1):193–213. doi: 10.1257/aer.100.1.193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaudhury Nazmul, Hammer Jeffrey. Ghost Doctors: Absenteeism in Rural Bangladeshi Health Facilities. World Bank Economic Review. 2004;18(3):423–441. [Google Scholar]
- Chay Kenneth Y, McEwan Patrick J, Urquiola Miguel. The Central Role of Noise in Evaluating Interventions that Use Test Scores to Rank Schools. American Economic Review. 2005;95(4):1237–1258. [Google Scholar]
- Cohen Joshua T, Neumann Peter J, Weinstein Milton C. Does Preventive Care Save Money? Health Economics and the Presidential Candidates. New England Journal of Medicine. 2008;358(7):661–663. doi: 10.1056/NEJMp0708558. [DOI] [PubMed] [Google Scholar]
- Currie Janet, Gruber Jonathan. Health Insurance Eligibility, Utilization of Medical Care, and Child Health. Quarterly Journal of Economics. 1996a;111(2):431–466. [Google Scholar]
- Currie Janet, Gruber Jonathan. Saving Babies: The Efficacy and Cost of Recent Changes in the Medicaid Eligibility of Pregnant Women. Journal of Political Economy. 1996b;104(6):1263–96. [Google Scholar]
- Currie Janet, Decker Sandra, Lin Wanchuan. Has Public Health Insurance for Older Children Reduced Disparities in Access to Care and Health Outcomes? Journal of Health Economics. 2008;27(6):1407–1652. doi: 10.1016/j.jhealeco.2008.07.002. [DOI] [PubMed] [Google Scholar]
- Cutler David M. Health Care and the Public Sector. In: Auerbach A, Feldstein M, editors. Handbook of Public Economics. 4. Amsterdam: Elsevier; 2002. [Google Scholar]
- Cutler David, Gruber Jonathan. Does Public Insurance Crowd Out Private Insurance? Quarterly Journal of Economics. 1996;111(2):391–430. [Google Scholar]
- Cutler David, Zeckhauser Richard. The Anatomy of Health Insurance. In: Culyer AJ, Newhouse JP, editors. Handbook of Health Economics. 1. Vol. 11. Amsterdam: Elsevier; 2000. [Google Scholar]
- Dafny Leemore, Gruber Jonathan. Public Insurance and Child Hospitalizations: Access and Efficiency Effects. Journal of Public Economics. 2005;89(1):109–129. [Google Scholar]
- Das Jishnu, Hammer Jeffrey. Money for Nothing: The Dire Straits of Medical Practice in Delhi, India. Journal of Development Economics. 2007;83(1):1–36. [Google Scholar]
- Dave Dhaval, Kaestner Robert. NBER Working Paper 12764. Cambridge, MA: 2006. Health Insurance and Ex-ante Moral Hazard: Evidence from Medicare. [DOI] [PubMed] [Google Scholar]
- Department of National Planning (DNP) Programa Familias en Acción –Condiciones Iniciales de los Beneficiarios e Impactos Preliminares. Bogotá: Department of National Planning; 2004. [Google Scholar]
- Department of National Planning (DNP) and Ministry of Social Protection. Proceedings of the National Conference on SISBEN: Integral Evaluation. Bogotá: Department of National Planning; 2001. [Google Scholar]
- Department of National Planning (DNP) and Ministry of Social Protection. Who Benefits from SISBEN? Integral Evaluation. Bogotá: Department of National Planning; 2003a. [Google Scholar]
- Department of National Planning (DNP) and Ministry of Social Protection. Results of the Evaluation Survey of SISBEN at the Municipal Level. Bogotá: Department of National Planning; 2003b. [Google Scholar]
- Dow William, Gertler Paul, Schoeni Robert, Strauss John, Thomas Duncan. Labor and Population Working Paper 97-01. RAND; 1997. Health Care Prices, Health, and Labor Outcomes: Experimental Evidence. [Google Scholar]
- Dow William, Philipson Tomas, Sala-i-Martin Xavier. Longevity Complementarities under Competing Risks. American Economic Review. 1999;89(5):1358–1371. [Google Scholar]
- Dow William, Gonzalez Kristine, Rosero-Bixby Luis. NBER Working Paper 9827. Cambridge, MA: 2003. Aggregation and Insurance-Mortality Estimation. [Google Scholar]
- Dow William, Schmeer Kammi K. Health Insurance and Child Mortality in Costa Rica. Social Science and Medicine. 2003;57(6):975–986. doi: 10.1016/s0277-9536(02)00464-1. [DOI] [PubMed] [Google Scholar]
- Doyle Joseph. Health Insurance, Treatment and Outcomes: Using Auto Accidents as Health Shocks. Review of Economics and Statistics. 2005;87(2):256–270. [Google Scholar]
- Duflo Esther, Banerjee Abhijit, Deaton Angus. Wealth, Health, and Health Services in Rural Rajasthan. American Economic Review Papers and Proceedings. 2004;94(2):326–330. doi: 10.1257/0002828041301902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellis Randall, McGuire Thomas. Optimal Payment Systems for Health Services. Journal of Health Economics. 1990;9:375–396. doi: 10.1016/0167-6296(90)90001-j. [DOI] [PubMed] [Google Scholar]
- Ellis Randall, McGuire Thomas. Supply-Side and Demand-Side Cost Sharing In Health Care. Journal of Economic Perspectives. 1993;7(4):135–151. doi: 10.1257/jep.7.4.135. [DOI] [PubMed] [Google Scholar]
- Enthoven Alain. Consumer Choice Health Plan (first of two parts). Inflation and Inequity in Health Care Today: Alternatives for Cost Control and an Analysis of Proposals for National Health Insurance. New England Journal of Medicine. 1978;298:650–658. doi: 10.1056/NEJM197803232981204. [DOI] [PubMed] [Google Scholar]
- Enthoven Alain. Consumer Choice Health Plan (second of two parts). A National Health Insurance Proposal Based on Regulated Competition in the Private Sector. New England Journal of Medicine. 1978;298:709–720. doi: 10.1056/NEJM197803302981304. [DOI] [PubMed] [Google Scholar]
- Escobar Maria Luisa. Development Outreach Magazine. World Bank Institute; Washington, D.C: 2005. Health sector reform in Colombia. [Google Scholar]
- Filmer Deon, Hammer Jeffrey, Pritchett Lant H. Weak Links in the Chain: A Diagnosis of Health Policy in Poor Countries. World Bank Research Observer. 2000;15(2):199–224. [Google Scholar]
- Finkelstein Amy. The Aggregate Effects of Health Insurance: Evidence from the Introduction of Medicare. Quarterly Journal of Economics. 2007;122(3):1–37. [Google Scholar]
- Finkelstein Amy, McKnight Robin. What Did Medicare Do? The Initial Impact of Medicare on Mortality and Out of Pocket Medical Spending. Journal of Public Economics. 2008;92(7):1644–1669. [Google Scholar]
- Fiszbein Ariel, Schady Norbert. Conditional Cash Transfers –Reducing Present and Future Poverty. The World Bank; Washington D.C: 2009. [Google Scholar]
- Fogel Robert. Economic Growth, Population Theory, and Physiology: The Bearing of Long-term Processes on the Making of Economic Policy. American Economic Review. 1994;84(3):369–395. [Google Scholar]
- Fresneda Bautista. Focusing on the subsidized health regime in Colombia. Revista Salud Pública. 2003;5(3):209–245. [PubMed] [Google Scholar]
- Fuchs Victor. Who Shall Live? Health, Economics, and Social Choice. Singapore: World Scientific Publishing Company; 1974. [Google Scholar]
- Gakidou E, Lozano R, Gonzalez-Pier E, Abbott-Klafter J, Barofsky J. Assessing the Effect of the 2001–2006 Mexican Health Reform: An Interim Report Card. The Lancet. 2006;368:1920–1935. doi: 10.1016/S0140-6736(06)69568-8. [DOI] [PubMed] [Google Scholar]
- Galasso Emanuela, Umapathi Nithin. Improving Nutritional Status Through Behavioural Change: Lessons from Madagascar. Journal of Development Effectiveness. 2009;1(1):60–85. [Google Scholar]
- Gaviria Alejandro, Medina Carlos, Mejía Carolina. Assessing Health Reform in Colombia: From Theory to Practice. Economía. 2007;7(1):29–72. [Google Scholar]
- Gertler Paul. Do Conditional Cash Transfers Improve Child Health? Evidence from PROGRESA’s Control Randomized Experiment. American Economic Review Papers and Proceedings. 2004;94(2):336–341. doi: 10.1257/0002828041302109. [DOI] [PubMed] [Google Scholar]
- Gertler Paul, Gruber Jonathan. Insuring Consumption against Illness. American Economic Review. 2002;92(1):51–70. doi: 10.1257/000282802760015603. [DOI] [PubMed] [Google Scholar]
- Gertler Paul, Solon Orville. Who Benefits From Social Health Insurance? Evidence from the Philippines. University of California, Berkeley and the University of the Philippines; 2002. Unpublished Manuscript. [Google Scholar]
- Gruber Jonathan, Hendren Nathaniel, Townsend Robert. NBER Working Paper 17739. Cambridge, MA: 2012. Demand and Reimbursement Effects of Healthcare Reform: Health Care Utilization and Infant Mortality in Thailand. [Google Scholar]
- Giedion Ursula, Uribe Manuela. Colombia’s Universal Health Insurance System. Health Affairs. 2009;28(3):853–863. doi: 10.1377/hlthaff.28.3.853. [DOI] [PubMed] [Google Scholar]
- Giedion Uusula, Díaz Beatrice, Alfonso Educardo, Savedoff William. The Impact of Subsidized Health Insurance on Health Status and on Access to and Use of Health Services. In: Glassman A, Giuffrida A, Escobar M-L, Giedion U, editors. From Few to Many: Ten Years of Health Insurance Expansion in Colombia. Inter-American Development Bank and The Brookings Institution; Washington, D.C: 2009. [Google Scholar]
- GTZ, ILO, and WHO. Recommendations for Action. The International Conference on Social Health Insurance in Developing Countries. Geneva: GTZ, ILO, and WHO; 2005. [Google Scholar]
- Gwatkin Davidson R, Wagstaff Adam, Yazbeck Abdo S. Reaching the Poor with Health, Nutrition and Population Services: What Works, What Doesn’t, and Why. World Bank; Washington, D. C: 2005. [Google Scholar]
- Hahn Jinyong, Todd Petra, Van der Klaauw Wilbert. Identification and Estimation of Treatment Effects with a Regression-Discontinuity Design. Econometrica. 2001;69(1):201–209. [Google Scholar]
- Holmstrom Bengt, Milgrom Paul. Multitask Principal-Agent Analyses: Incentive Contracts, Asset Ownership, and Job Design. Journal of Law, Economics and Organization. 1991;7:24–52. [Google Scholar]
- Hoxby Caroline. All School Finance Equalizations Are Not Created Equal. Quarterly Journal of Economics. 2001;116(4):1189–1231. [Google Scholar]
- Hughes David, Leethongdee Songkramchai. Universal Coverage in the Land of Smiles: Lessons from Thailand’s 30 Baht Health Reforms. Health Affairs. 2007;26(4):999–1008. doi: 10.1377/hlthaff.26.4.999. [DOI] [PubMed] [Google Scholar]
- IFS-SEI-Econometria. Evaluación de Impacto del Programa Empleo en Acción. VI. Bogotá: National Planning Department; 2005. [Google Scholar]
- Imbens Guido, Lemieux Thomas. Regression Discontinuity Designs: A Guide to Practice. Journal of Econometrics. 2008;142(2):615–635. [Google Scholar]
- Keenan P, Elliott M, Cleary P, Zaslavsky A, Landon M. Quality Assessments by Sick and Healthy Beneficiaries in Traditional Medicare and Medicare Managed Care. Medical Care. 2009;47(8):882–888. doi: 10.1097/MLR.0b013e3181a39415. [DOI] [PubMed] [Google Scholar]
- Kenkel Donald. Prevention. In: Culyer AJ, Newhouse JP, editors. Handbook of Health Economics. 1. Vol. 31. Amsterdam: Elsevier; 2000. [Google Scholar]
- Kolstad Jonathan, Kowalski Amanda. NBER Working Paper 16012. Cambridge, MA: 2010. The Impact of Health Care Reform on Hospital and Preventive Care: Evidence from Massachusetts. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kowlaski Amanda. Estimating the Trade-off between Risk Protection and Moral Hazard with a Nonlinear Budget Set Model of Health Insurance. Yale University; 2011. Unpublished Manuscript. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lagarde Mylene, Haines Andy, Palmer Natasha. Conditional Cash Transfers for Improving Uptake of Health Interventions in Low- and Middle-Income Countries: A Systematic Review. Journal of the American Medical Association. 2007;298(16):1900–1910. doi: 10.1001/jama.298.16.1900. [DOI] [PubMed] [Google Scholar]
- Lee David, Lemieux Thomas. Regression Discontinuity Designs in Economics. Journal of Economic Literature. 2010;48:281–355. [Google Scholar]
- Lennon MA, Worthington HV, Coventry P, Mellor AC, Holloway PJ. The Capitation Study. 2. Does Capitation Encourage More Prevention? British Dental Journal. 1990 Mar 10;168(5):213–215. doi: 10.1038/sj.bdj.4807134. [DOI] [PubMed] [Google Scholar]
- Levy Helen, Meltzer David. What Do We Really Know about Whether Health Insurance Affects Health? In: McLaughlin C, editor. Health Policy and the Uninsured: Setting the Agenda. Washington, DC: Urban Institute Press; 2004. [Google Scholar]
- Linnemayr Sebastian, Alderman Harold. Almost Random: Evaluating a Large-scale Randomized Nutrition Program in the Presence of Crossover. Journal of Development Economics. 2011 Sep;96(1):106–114. [Google Scholar]
- Ma Albert C, McGuire Thomas. Optimal Health Insurance and Provider Payment. American Economic Review. 1997;87:685–704. [Google Scholar]
- Manning Willard, Leibowitz Arleen, Goldberg George, Newhouse Joseph, Rogers William. A Controlled Trial of the Effect of a Prepaid Group Practice on Use of Services. New England Journal of Medicine. 1984;310(23):1505–1510. doi: 10.1056/NEJM198406073102305. [DOI] [PubMed] [Google Scholar]
- McGuire Thomas. Physician Agency. In: Culyer AJ, Newhouse JP, editors. Handbook of Health Economics. 1. Vol. 9. Amsterdam: Elsevier; 2000. [Google Scholar]
- Miller Robert H, Luft Harold S. Managed Care Plan Performance Since 1980A Literature Analysis. Journal of the American Medical Association. 1994 May 18;271(19):1512–1519. [PubMed] [Google Scholar]
- Mohanan Manoj. Causal Effects of Health Shocks on Consumption and Debt: Quasi-Experimental Evidence from Bus Accident Injuries. The Review of Economic and Statistics. 2012 doi: 10.1162/REST_a_00262. Forthcoming. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morduch Jonathan. Income Smoothing and Consumption Smoothing. Journal of Economic Perspectives. 1995;9(3):103–114. [Google Scholar]
- Morduch Jonathan. The Microfinance Promise. Journal of Economic Literature. 1999;37(4):1569–1614. [Google Scholar]
- Muralidharan Karthik, Sundararaman Venkatesh. Teacher Performance Pay: Experimental Evidence from India. Journal of Political Economy. 2011;119:39–77. [Google Scholar]
- Murphy Kevin M, Topel Robert H. The Value of Health and Longevity. Journal of Political Economy. 2006;114:871–904. [Google Scholar]
- Newhouse J the Insurance Experiment Group. Free for All? Lessons from the RAND Health Insurance Experiment. Cambridge, MA: Harvard University Press; 1993. [Google Scholar]
- Newhouse Joseph P. Pricing the Priceless – A Health Care Conundrum. Cambridge, MA: MIT Press; 2002. [Google Scholar]
- Nichols Austin. Stata Module for Regression Discontinuity Estimation. 2007 Available online at: http://ideas.repec.org/c/boc/bocode/s456888.html.
- Nordquist Gerald, David Wu S. The Joint Demand for Health Insurance and Preventive Medicine. In: Rosett R, editor. The Role of Health Insurance in the Health Services Sector. New York: National Bureau of Economic Research; 1976. [Google Scholar]
- Odonnell O, et al. Who Pays for Health Care in Asia? Journal of Health Economics. 2008;27:460–475. doi: 10.1016/j.jhealeco.2007.08.005. [DOI] [PubMed] [Google Scholar]
- Panopoulus G, Vélez C. Colombia Poverty Report. Vol. 2. Washington, D.C: The World Bank; 2001. Subsidized Health Insurance, Proxy Means Testing, and the Demand for Health Care among the Poor in Colombia. [Google Scholar]
- Pauly Mark. The Economics of Moral Hazard. American Economic Review. 1968;49:531–537. [Google Scholar]
- Pauly Mark, Blavin Frederic E, Meghan Sudha. NBER Working Paper 14095. Cambridge, MA: 2008. Is There a Market for Voluntary Health Insurance in Developing Countries? [Google Scholar]
- Pauly Mark, Zweifel Peter, Scheffler Richard, Preker Alexander, Bassett Mark. Private Health Insurance in Developing Countries. Health Affairs. 2006;25(2):369–379. doi: 10.1377/hlthaff.25.2.369. [DOI] [PubMed] [Google Scholar]
- Paxson Christina. Consumption and Income Seasonality in Thailand. Journal of Political Economy. 1993;101(1):39–72. [Google Scholar]
- Phelps Charles. Illness Prevention and Medical Insurance. Journal of Human Resources. 1978;13:183–207. [PubMed] [Google Scholar]
- Pinto Diana. Good Practices in Expanding Health Care Coverage. In: Gottret P, Schieber GJ, Waters HR, editors. Good Practices in Health Financing Lessons from Reforms in Low and Middle-Income Countries. The International Bank for Reconstruction and Development/The World Bank; Washington DC: 2008. [Google Scholar]
- Pitt Mark, Khandker Shahidur. The Impact of Group-Based Credit Programs on Poor Households in Bangladesh: Does the Gender of Participants Matter? Journal of Political Economy. 1998;106(5):958–996. [Google Scholar]
- Santos Iná, Victora Cesar, Martines José, Gonçalves Helen, Gigante Denise, Valle Neiva, Pelto Gretel. Nutrition Counseling Increases Weight Gain Among Brazilian Children. The Journal of Nutrition. 2001 Nov;131(11):2866–2873. doi: 10.1093/jn/131.11.2866. [DOI] [PubMed] [Google Scholar]
- Townsend Robert. Risk and Insurance in Village India. Econometrica. 1994;62(3):539–591. [Google Scholar]
- Trujillo Antonio, Portillo Jorge, Vernon John. The Impact of Subsidized Health Insurance for the Poor: Evaluating the Colombian Experience Using Propensity Score Matching. International Journal of Health Care Finance and Economics. 2005;5(3):211–239. doi: 10.1007/s10754-005-1792-5. [DOI] [PubMed] [Google Scholar]
- Wagstaff Adam. Policy Research Paper Series Working Paper 4134. The World Bank; 2007. Health Insurance for the Poor: Initial Impacts of Vietnam’s Health Care Fund for the Poor. [Google Scholar]
- Wagstaff Adam, Yu Shengchao. Do Health Sector Reforms Have Their Intended Impacts? The World Bank’s Health VIII Project in Gansu Province, China. Journal of Health Economics. 2007;26:505–535. doi: 10.1016/j.jhealeco.2006.10.006. [DOI] [PubMed] [Google Scholar]
- WHO Commission on Macroeconomics and Health. Macroeconomics and Health: Investing in Health for Economic Development. Geneva, Switzerland: World Health Organization; 2001. [Google Scholar]
- WHO. The World Health Report: Health Systems Financing: the Path to Universal Coverage. Geneva: World Health Organization; 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu Ke, Evans David, Kawabata Kei, Zeramdini Riadh, Klavus Jan, Murray Christopher. Household Catastrophic Health Expenditure: A Multicountry Analysis. The Lancet. 2003;362(9378):111–117. doi: 10.1016/S0140-6736(03)13861-5. [DOI] [PubMed] [Google Scholar]
- Wagstaff Adam, Lindelow Magnus. Can Insurance Increase Financial Risk? Journal of Health Economics. 2008 Jul;27(4):990–1005. doi: 10.1016/j.jhealeco.2008.02.002. [DOI] [PubMed] [Google Scholar]
- Zeckhauser Richard. Medical Insurance: A Case Study of the Tradeoff between Risk Spreading and Appropriate Incentives. Journal of Economic Theory. 1970;2(1):10–26. [Google Scholar]