Abstract
Context:
Hip-joint laxity may be a relevant anterior cruciate ligament injury risk factor. With no devices currently available to measure hip laxity, it is important to determine if clinical measurements sufficiently capture passive displacement of the hip.
Objective:
To examine agreement between hip internal-external–rotation range of motion measured clinically (HIERROM) versus internal-external–rotation laxity measured at a fixed load (HIERLAX) and to determine their relationships with knee laxity (anterior-posterior [KAPLAX], varus-valgus [KVVLAX], and internal-external rotation [KIERLAX]) and general joint laxity (GJL).
Design
Cross-sectional study.
Setting:
Controlled research laboratory.
Patients or Other Participants:
Thirty-two healthy adults (16 women, 16 men; age = 25.56 ± 4.08 years, height = 170.94 ± 10.62 cm, weight = 68.86 ± 14.89 kg).
Main Outcome Measure(s):
Participants were measured for HIERROM, HIERLAX at 0° and 30° hip flexion (−10 Nm, 7 Nm), KAPLAX (−90 N to 133 N), KVVLAX (±10 Nm), KIERLAX (±5 Nm), and GJL. We calculated Pearson correlations and 95% limits of agreement between HIERROM and HIERLAX_0° and HIERLAX_30°. Correlation analyses examined the strength of associations between hip laxity, knee laxity, and GJL.
Results:
The HIERROM and HIERLAX had similar measurement precision and were strongly correlated (r > 0.78). However, HIERROM was systematically smaller in magnitude than HIERLAX at 0° (95% limits of agreement = 29.0° ± 22.3°) and 30° (21.4° ± 19.3°). The HIERROM (r = 0.51–0.66), HIERLAX_0° (r = 0.52–0.69) and HIERLAX_30° (r = 0.53–0.76) were similarly correlated with knee laxity measures and GJL. The combinations of KVVLAX and either HIERROM, HIERLAX_0°, or HIERLAX_30° (R2 range, 0.42–0.44) were the strongest predictors of GJL.
Conclusions:
Although HIERROM and HIERLAX differed in magnitude, they were measured with similar consistency and precision and were similarly correlated with knee laxity and GJL measures. Individuals with greater GJL also had greater hip laxity. These findings are relevant to clinicians and investigators conducting prospective risk factor studies, given the need for accessible, efficient, and low-cost alternatives for characterizing an individual's laxity profile.
Key Words: anterior cruciate ligament injuries, risk factors, lower extremity
Key Points
Differences between measures of hip internal-external–rotation range of motion and laxity were large and systematic, even though the measures demonstrated comparable precision and were strongly correlated in relative magnitude.
Measures of hip internal-external–rotation range of motion and laxity were strongly correlated with measures of knee laxity and general joint laxity.
Clinical measurement of hip internal-external–rotation range of motion may be a reliable, efficient, and low-cost measure of passive hip-joint displacement.
Anterior cruciate ligament (ACL)–injured patients tend to have greater general joint laxity (GJL) than uninjured controls.1–3 For example, in a prospective study by Uhorchak et al,2 individuals who scored 5 or greater on the Beighton and Horan Joint Mobility Index4 were 2.8 times more likely to tear their ACLs. However, the nature of this association is not entirely clear, as GJL has been reported at times to be poorly correlated with sagittal-plane knee laxity5,6 and has been associated with alterations in knee-joint biomechanics that are distinct from those of sagittal-plane knee laxity.5 Because GJL represents a general condition of joint hypermobility across multiple joints,7–10 GJL may reflect associated laxities in other lower extremity joints that also contribute to injury risk (eg, hip). For instance, hip-joint conditions in children that are characterized by a more internally rotated hip are thought to develop secondarily to hip instability (hip acetabular dysplasia, congenital hip dislocation), which has been associated with greater GJL.9,11 Further, in a recent study,12 hip acetabular dysplasia was more prevalent in ACL-injured females than uninjured controls, and this condition was also associated with greater magnitudes of anterior knee laxity and GJL. Collectively, these findings suggest that GJL (and knee laxity) may be capturing some aspect of hip-joint laxity, which may play an important role in ACL injury risk.
In vivo joint-laxity testing assesses the combined passive resistance of the ligaments, muscles, and capsule to a displacing load. Although knee laxity and GJL have been commonly studied as ACL injury risk factors, hip-joint laxity has received little attention to date, despite the perceived importance of the proximal hip in controlling motion at the knee.13–16 This is likely due in large part to the lack of instrumented devices to measure laxity at the hip. However, limited research using a clinical measure of passive hip range of motion (hip internal-external–rotation range of motion [HIERROM] = range through which the joint can freely and painlessly move, based on the subjective judgment of passive resistance by the investigator)9,16–18 has identified associations between high-risk biomechanics16,19 and ACL injury risk,20 suggesting this is a worthy area of study.
Biomechanical studies have revealed higher-risk landing biomechanics in those with less relative hip external-rotation motion (demonstrating greater frontal-plane knee excursion)16 and those with greater relative hip internal-rotation motion (demonstrating greater relative hip adduction and knee valgus and external rotation).19 Conversely, in a case-control study of male soccer players with ACL injuries from noncontact mechanisms,20 the ACL-injured cohort had, on average, 14° less total HIERROM (primarily driven by decreased hip internal-rotation motion) than the control group. Although these findings suggest that the magnitude of passive hip-joint motion may be associated with higher-risk hip and knee biomechanics and ACL injury potential, the directions of these associations are inconsistent. One reason for inconsistent findings could be the subjective nature of the measure, as the displacement is not performed at a standardized load. Authors16 of only 1 of the aforementioned studies reported reliability estimates for the measure, and although they noted strong reliability within a person, measurement precision was not quantified. Given the inherent large intersubject variability in passive hip motion (values ranging from 20°–60° and 13°–54° for internal and external range of motion, respectively16) and the fact that intraclass correlation coefficients can be inflated with large distributions in scores, quantifying measurement precision may be equally important. To date, we are not aware of any researchers who have compared the precision of this more clinical measure of HIERROM with an instrumented measure of hip-joint laxity where joint displacement is measured at a fixed load limit (HIERLAX). Such findings may inform future researchers who seek to examine the role of hip-joint laxity in functional lower extremity biomechanics and ACL injury risk and, subsequently, to identify appropriate clinical screening measures to assess injury risk potential.
Also unknown is the extent to which measures of HIERROM or HIERLAX would provide unique information about an individual's laxity profile (and thus injury risk potential) that is not already captured through current clinical (eg, GJL) and instrumented (knee anterior-posterior, varus-valgus, and internal-external–rotation) laxity measurements. Because of these unknowns, our purpose was 2-fold. First, we examined the reliability, precision, and level of agreement between a clinical measurement of HIERROM and an instrumented measure of HIERLAX at a fixed load. We hypothesized that agreement between HIERLAX and HIERROM would be good to moderate but greater precision of measurement would be afforded by HIERLAX, based on a more objective determination of end range of motion. Our secondary purpose was to examine relationships between HIERLAX and HIERROM with existing measures of GJL and knee laxity (anterior-posterior [KAPLAX], varus-valgus [KVVLAX]), and internal-external rotation [KIERLAX]). We hypothesized that HIERLAX/HIERROM would be moderately correlated with both GJL and knee-laxity measures but that HIERLAX/HIERROM would explain additional variance in GJL not accounted for by knee laxity.
METHODS
A total of 32 healthy participants (16 women, 16 men, age = 25.56 ± 4.08 years [range, 19–35 years], height = 170.94 ± 10.62 cm, weight = 68.86 ± 14.89 kg) were measured for HIERROM, HIERLAX, measures of knee laxity (anterior knee laxity, KVVLAX, and KIERLAX), and GJL in a single session. Participants were recruited from the university and surrounding community, and healthy was operationally defined as no history of left hip or knee ligament injury or surgery and no medical conditions affecting the connective tissue (eg, muscle, ligament). Before enrolling, participants signed an informed consent form approved by the university institutional review board, which also approved the study. The order of testing for all participants was KVVLAX, KIERLAX, KAPLAX, HIERROM, GJL, HIERLAX_0°, and HIERLAX_30°. This order allowed us to change the setup of the Vermont Knee Laxity Device (University of Vermont, Burlington, VT) from knee- to hip-laxity testing while obtaining the clinical laxity measurements. The specific procedures for each measurement follow.
Clinical Measurement Procedures
The HIERROM was measured with the participant lying prone, knee flexed to 90°, and hip in 0° of hip abduction-adduction.17,21 The pelvis was stabilized against the table to ensure that motion was limited to the hip joint. With an inclinometer (Universal Inclinometer; Performance Attainment Associates, Saint Paul, MN) attached along the long axis of the tibia, the tibia was positioned perpendicularly to the table to establish an initial zero position, as confirmed by the inclinometer's vertical zero reference position. The hip was then rotated internally and externally until firm tissue resistance was felt, and the range of motion (degrees) in each direction was measured. Three measurements of internal-rotation and external-rotation range of motion were summed and then averaged, and the total internal-external–rotation motion was used for analysis. For the purposes of this study, we compared total motion with all subsequent laxity measures because prior work22 has shown these measures to be more reliable (owing to difficulty in identifying a true zero reference point with knee-laxity measures), and our goal was to simply determine the extent to which the magnitude of passive motion at one joint was related to the magnitude of passive motion at another joint.
The GJL was assessed with the Beighton and Horan Joint Mobility Index4 and was scored from 0 to 9, with 1 point for each of the following criteria: fifth finger extension > 90°, elbow hyperextension > 10°, thumb opposition to the forearm, knee hyperextension > 10° (all measured bilaterally), and placing the palms flat on the floor with the knees fully extended.
Instrumented Knee- and Hip-Laxity Measures
Anterior-posterior knee laxity (KAPLAX) was assessed with a knee arthrometer (model KT-2000; Medmetric Corporation, San Diego, CA) from a posterior-directed force of 90 N to an anterior-directed force of 133 N with the participant lying supine with the knee flexed to 25° ± 5°, using methods previously described.23,24 Three consecutive measurements were averaged for analysis.
The HIERLAX, KVVLAX, and KIERLAX were measured with the Vermont Knee Laxity Device. To measure force and displacement data, we applied clusters of 4 optical LED markers (IMPULSE Motion Capture System; PhaseSpace Inc, San Leandro, CA) to the pelvis, left thigh, and left shank and digitized joint centers by using centroid (knee and ankle)25 methods and those of Leardini et al.26 Kinematic (240 Hz) and kinetic (500 Hz) data were simultaneously captured during each laxity measurement by using an 8-camera optical system (IMPULSE) and MotionMonitor acquisition software (version 8.62; Innovative Sports Training Inc, Chicago, IL).
The KVVLAX and KIERLAX were measured by using procedures previously reported, with the participant lying supine, the knee flexed to 20° (confirmed by goniometry), and gravitational loads eliminated.22 The KVVLAX was measured as the total varus-valgus displacement while ±10 Nm of valgus and varus torque was applied, whereas the KIERLAX was measured as the total internal-external displacement while ±5-Nm internal-external–rotation torque was applied. For each measure, a conditioning trial was followed by 2 test trials of 3 consecutive cycles. The last 2 cycles of the 2 test trials were averaged for analysis.
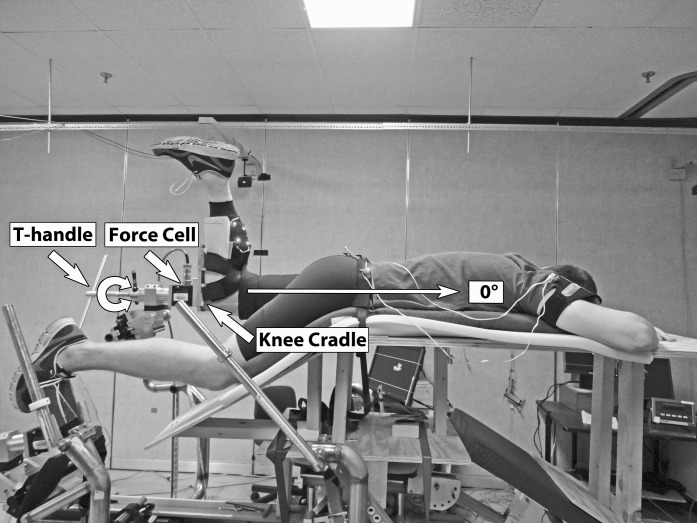
The HIERLAX was measured by attaching a wooden platform to the Vermont Knee Laxity Device to allow positioning of the pelvis and thigh for testing in neutral (Figure 1) and in 30° of hip flexion (Figure 2). We chose these test positions to account for the varying contributions of the hip capsular ligaments (ie, ischiofemoral ligament controlling internal rotation in flexion and extension, lateral iliofemoral ligament controlling internal and external rotation in flexion, and pubofemoral ligament with contributions from the medial and lateral iliofemoral ligaments controlling external rotation in extension).27 With the participant lying prone, the pelvis restrained to keep the torso parallel to the floor, and the left knee flexed to 90° and secured in the knee cradle, we positioned the hip in 0° of flexion, rotation, and abduction-adduction, consistent with HIERROM positioning. The nontest leg rested comfortably on a support. The participant was instructed to relax while internal-external–rotation torques of 10 Nm and 7 Nm, respectively, were applied to the hip joint. During pilot testing, these torques were determined to be the maximum participants could comfortably tolerate without muscle guarding or pain or elevating the pelvis. A conditioning trial was followed by 2 test trials of 3 consecutive internal-external–rotation cycles. Hip laxity was first measured in neutral (HIERLAX_0°) and then in 30° of hip flexion, as confirmed by goniometry (HIERLAX_30°; Figure 2). For each measure, the total internal-external–rotation displacements of the last 2 cycles of the test trials were averaged for analysis. Internal- and external-rotation values were recorded for descriptive purposes.
Figure 1.
Participant placement in the Vermont Knee Laxity Device (University of Vermont, Burlington, VT) for measuring hip internal-external–rotation laxity in neutral position.
Figure 2.
Participant placement in the Vermont Knee Laxity Device (University of Vermont, Burlington, VT) for measuring hip internal-external–rotation laxity in 30° of hip flexion.
Because this was the first study in which we obtained HIERLAX measures, we asked the first 10 participants to return for a second session (24 to 48 hours later) to determine day-to-day HIERLAX measurement consistency and precision at 0° and 30° of hip flexion. For all other laxity measures, testers had previously established their measurement reliability and precision as part of their initial laboratory training. All reliability estimates are based on 10 healthy participants measured on 2 days spaced 24 to 48 hours apart (intraclass correlation coefficient [ICC 2,3] [standard error of the mean] for HIERROM = 0.97 [1.5°], for HIRROM = 0.97 [1.1°], for HERROM = 0.98 [1.4°], for GJL = 0.99 [0.2 points], for KAPLAX = 0.98 [0.3 mm], for KVVLAX22 = 0.91 [0.87°], and for KIERLAX22 = 0.75 [2.67°]). A single investigator (L.F.) with 5 years of clinical training and research experience obtained all clinical measures (HIERROM, GJL, KAPLAX), whereas a team of 2 investigators (due to instrumentation demands) obtained HIERLAX (L.F., T.J.C.) and KVVLAX/KIERLAX (T.J.C., A.J.T.) measures. For the latter 2 measures, the individual providing the force application (L.F. or A.J.T.) was consistent across all participants, and each examiner had at least 5 years of clinical training and research experience.
Statistical Analysis
To address the first hypothesis, we computed the ICC [2,k] and standard error of the measurement (SEM)28 by using the SPSS Statistics Package (version 18; IBM Corporation, Armonk, NY), and 68% and 95% limits of agreement by using Bland-Altman plots29 (version 12.2.1.0; MedCalc Statistical Software, Ostend, Belgium) to assess the day-to-day measurement consistency of HIERLAX_0° and HIERLAX_30° for the first 10 participants. (For comparative purposes, we included the 68% and 95% limits of agreement obtained for HIERROM on 10 participants during the investigators' prior training). The SEM provides a unit of measurement precision that is based on the distribution in scores.30 Because our small sample of healthy individuals may not adequately reflect the distribution in scores of a larger population (or of other populations such as athletes), we also calculated the 95% limits of agreement, which do not depend on sample characteristics.29 As such, the 95% limits of agreement provide an unbiased estimate of the absolute error that may be expected and may further assist clinicians in determining if the magnitude of error is acceptable.
We then used Pearson correlation coefficients and 95% limits of agreement to determine the level of association and agreement, respectively, between HIERROM, HIERLAX_0°, and HIERLAX_30° in the entire sample. For the 95% limits of agreement, we examined the raw data as opposed to a logarithmic transformation of the data. Although the logarithmic transformation is recommended to control for increasing differences between scores as the magnitude of the measure increases, results using the raw values are more clinically interpretable.29 Moreover, we believed it was important to identify these measurement concerns if present.
To answer the second hypothesis, we calculated Pearson correlations to examine relationships between measures of hip laxity (HIERLAX_0°, HIERLAX_30°, and HIERROM), measures of knee laxity (KAPLAX, KVVLAX, and KIERLAX), and GJL. Correlations were interpreted as weak (r < 0.25), fair (r = 0.26–0.50), moderate (r = 0.51–0.75), or strong (r > 0.76).30 Using this convention, we had 90% power to detect a moderate correlation with 32 participants.30 We then conducted backward stepwise linear regression analyses to determine the extent to which HIERLAX predicted GJL when knee-laxity variables were also accounted for (tolerance for removal from the model = P < .20).31 With a sample size of 32 participants, we had 60% to 85% power to detect an R2 value of 0.25 (considered a large effect),31 depending on the number of variables that remained in the model (from 4 to 1, respectively).30 Because GJL,2,24 HIERROM,17,21 and measures of knee laxity2,24 differ by sex, we also examined these associations within each sex. Significance was determined at P ≤ .05 by using a 1-tailed test (assuming associations would be positive in nature).
RESULTS
Descriptive data for all measured variables are provided in Table 1. Women had greater total laxity than men for all variables except KAPLAX (P = .09). However, greater values of total HIERROM, HIERLAX_0°, and HIERLAX_30° in women versus men were primarily due to women having greater magnitudes of hip internal rotation (P < .01) but not hip external rotation (P > .278).
Table 1.
Laxity Variables for the Total Sample and Stratified by Sex, Mean ± SD
| Laxity Variable |
Total Sample (N = 32) |
Women (n = 16) |
Men (n = 16) |
| Hip internal-external–rotation range of motion measured clinically, ° | |||
| Internal rotation | 38.9 ± 8.7 | 42.7 ± 10.3a | 35.1 ± 4.7 |
| External rotation | 41.5 ± 6.4 | 41.1 ± 6.4 | 41.9 ± 6.6 |
| Total | 80.4 ± 9.7 | 83.8 ± 11.0a | 77.0 ± 6.9 |
| Hip internal-external–rotation laxity measured at 0°, ° | |||
| Internal rotation | 54.9 ± 11.3 | 60.9 ± 11.7a | 48.8 ± 6.8 |
| External rotation | 54.1 ± 12.8 | 55.7 ± 13.0 | 52.4 ± 12.9 |
| Total | 109.4 ± 17.2 | 117.1 ± 15.5a | 101.1 ± 15.6 |
| Hip internal-external–rotation laxity measured at 30°, ° | |||
| Internal rotation | 54.0 ± 11.2 | 60.9 ± 10.4a | 47.0 ± 7.0 |
| External rotation | 47.5 ± 10.9 | 49.6 ± 10.0 | 45.3 ± 11.7 |
| Total | 101.8 ± 15.6 | 110.9 ± 12.7a | 92.8 ± 12.9 |
| General joint laxity, score (range, 0–9) | 2.0 ± 2.0 | 2.8 ± 1.7a | 1.3 ± 2.1 |
| Knee internal-external–rotation laxity, ° | 26.4 ± 7.8 | 31.4 ± 7.4a | 21.3 ± 4.3 |
| Knee varus-valgus laxity, ° | 8.8 ± 3.6 | 11.1 ± 3.5a | 6.5 ± 1.8 |
| Knee anterior-posterior laxity, mm | 10.2 ± 2.2 | 10.9 ± 2.5b | 9.6 ± 1.7 |
P < .05.
P < .10.
The reliability coefficients for HIERLAX_0°, HIERLAX_30°, and HIERROM are shown in Table 2, and the Bland-Altman plots for the test-retest measurement consistency appear in Figure 3. The ICC values were excellent for all 3 measures. The SEM and 68% and 95% limits of agreement indicated little systematic bias in measures across days and smaller SEMs and absolute errors (ie, better measurement precision) for HIERROM than for either HIERLAX_0° or HIERLAX_30°. However, this smaller absolute error appears to be largely a function of the smaller values and smaller dispersion among values when measuring HIERROM versus HIERLAX (Table 1). That is, when we compared the magnitude of the measurement error with the magnitude of the measure, the measurement error was relatively proportional to the respective average range of motion for each measure (eg, the 95% limits of agreement were 7.3%, 8.4%, and 8.0% of the mean values for HIERROM, HIERLAX_0°, and HIERLAX_30°, respectively).
Table 2.
Day-to-Day Repeated Measurements of Hip Range of Motion and Laxity
| Hip Variable |
Day, Mean ± SD |
Intraclass Correlation Coefficient (Standard Error of Measurement), ° |
Limits of Agreement |
||
| 1 |
2 |
68% |
95% |
||
| Internal-external–rotation range of motion measured clinically, ° | 77.9 ± 9.7 | 77.7 ± 7.8 | 0.97 (1.5) | –1.1° ± 2.9° | –1.1° ± 5.7° |
| Internal-external–rotation laxity measured at 0, ° | 111.6 ± 13.6 | 112.3 ± 14.4 | 0.95 (3.1) | –0.6° ± 4.7° | –0.6° ± 9.2° |
| Internal-external–rotation laxity measured at 30, ° | 103.0 ± 11.2 | 102.5 ± 13.5 | 0.96 (2.5) | –1.3° ± 4.2° | –1.3° ± 8.2° |
Figure 3.
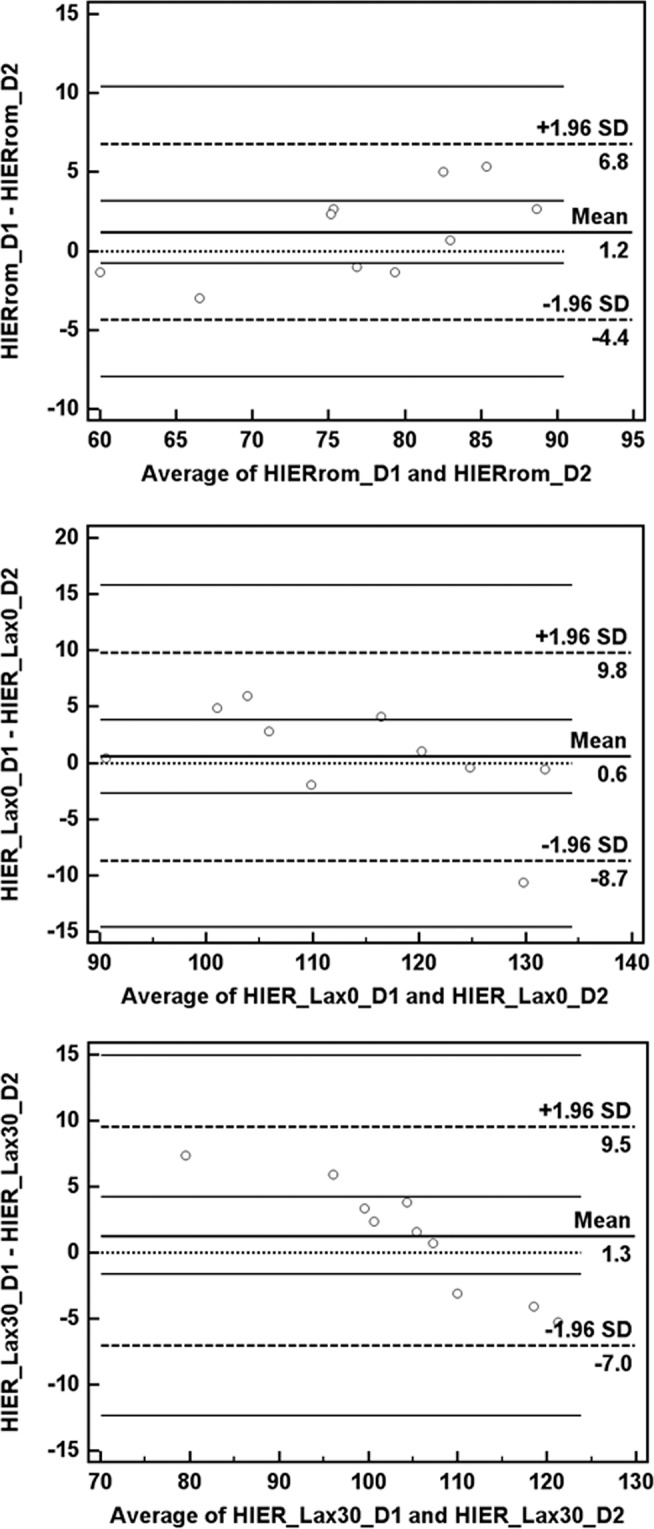
The 95% limits-of-agreement Bland-Altman plots for the test-retest measurement consistency for hip internal-external–rotation range of motion (HIERrom) and internal-external–rotation laxity in 0° and 30° of hip flexion (HIER_Lax0 and HIER_Lax30, respectively).
Pearson correlation coefficients are provided in Table 3. Graphic depictions of the 95% limits-of-agreement Bland-Altman plots examining the level of agreement between the clinically derived HIERROM and the 2 instrumented hip-laxity measures are available in Figure 4. The HIERLAX_0° (r = 0.78) and HIERLAX_30° (r = 0.79) were both strongly correlated with HIERROM, and these relationships held for both sexes (Table 4). However, Pearson correlations can be inflated with large distributions in participants' scores and are not sensitive to systematic differences between measurement methods. In this regard, the 95% limits of agreement (Figure 4) between HIERROM and HIERLAX_0° and between HIERROM and HIERLAX_30° clearly indicate that HIERROM was systematically smaller in magnitude than HIERLAX_0° (−29.0°) and HIERLAX_30° (−21.4°), with the actual mean differences falling between −6.7 and −51.2 and −2.1 and −40.8, respectively, in 95% of the cases. Further, the difference between measures tended to increase as the values became larger. When we compared HIERLAX_0° and HIERLAX_30° (Pearson r = 0.96), the 95% limits of agreement indicated that HIERLAX_0° was systematically greater in magnitude than HIERLAX_30° (7.6°, 95% confidence interval = −1.9°, 17.0°), with the difference between measures increasing with higher magnitudes of laxity.
Table 3.
Bivariate Pearson Correlations Between Measures of Hip Laxity, Knee Laxity, and General Joint Laxity, All Participants (N = 32)a
| Variable |
HIERROM |
HIERLAX_0° |
HIERLAX_30° |
GJL |
KIERLAX |
KVVLAX |
KAPLAX |
| HIERROM | – | ||||||
| HIERLAX_0° | 0.78 | – | |||||
| HIERLAX_30° | 0.79 | 0.96 | – | ||||
| GJL | 0.57 | 0.58 | 0.64 | – | |||
| KIERLAX | 0.65 | 0.61 | 0.68 | 0.53 | – | ||
| KVVLAX | 0.66 | 0.69 | 0.76 | 0.60 | 0.79 | – | |
| KAPLAX | 0.51 | 0.52 | 0.53 | 0.33 | 0.47 | 0.57 | – |
Abbreviations: GJL, general joint laxity; HIERLAX_0°, hip internal-external–rotation laxity measured at 0°; HIERLAX_30°, hip internal-external–rotation laxity measured at 30°; HIERROM, hip internal-external–rotation range of motion measured clinically; KAPLAX, knee anterior-posterior laxity; KIERLAX, knee internal-external–rotation laxity; KVVLAX, knee varus-valgus laxity.
All values: P < .05.
Figure 4.
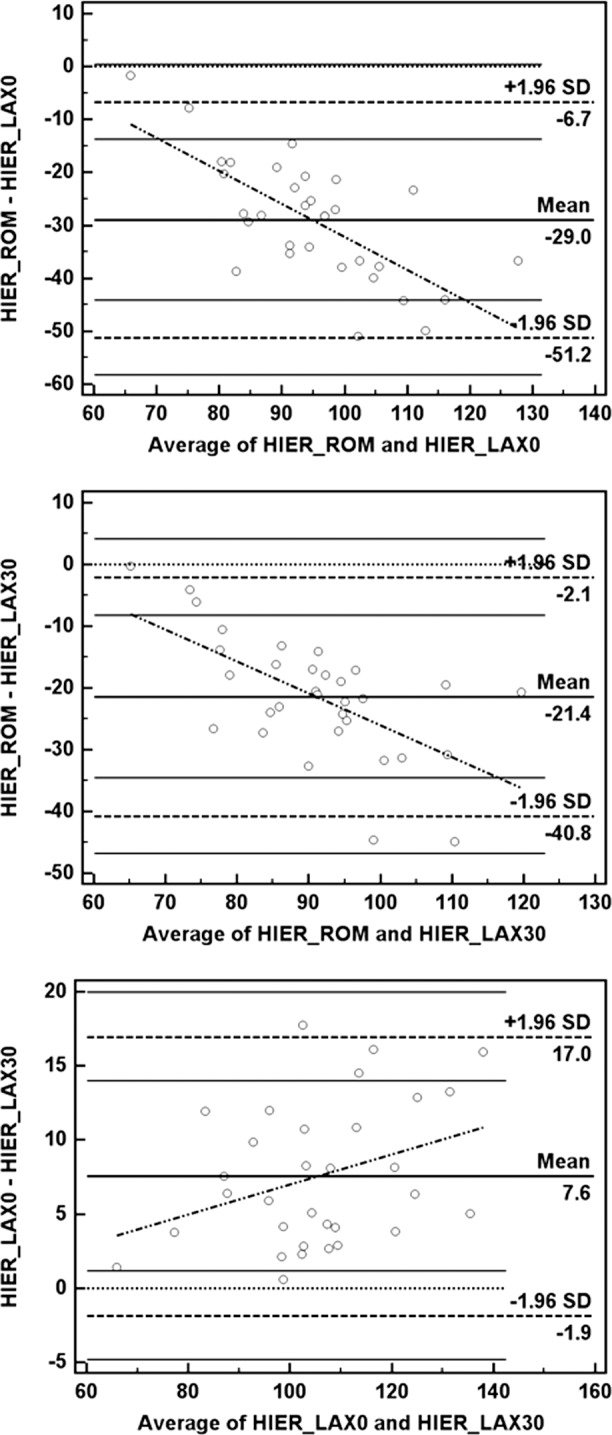
The 95% limits-of-agreement Bland-Altman plots between hip internal-external–rotation range of motion (HIER_rom) and hip internal-external–rotation laxity in 0° and 30° of hip flexion (HIER_Lax0 and HIER_Lax30, respectively).
Table 4.
Bivariate Pearson Correlations Between Measures of Hip Laxity, Knee Laxity, and General Joint Laxity by Sexa,b
| Women |
|||||||
| Men |
HIERROM |
HIERLAX_0° |
HIERLAX_30° |
GJL |
KIERLAX |
KVVLAX |
KAPLAX |
| HIERROM | 0.72 | 0.74a | 0.51a | 0.53a | 0.65a | 0.39 | |
| HIERLAX_0° | 0.84a | 0.96a | 0.59a | 0.41 | 0.71a | 0.39 | |
| HIERLAX_30° | 0.88a | 0.97a | 0.66a | 0.42 | 0.74a | 0.39 | |
| GJL | 0.57a | 0.44a | 0.50a | 0.42 | 0.57a | 0.12 | |
| KIERLAX | 0.75a | 0.62a | 0.62a | 0.50a | 0.66a | 0.23 | |
| KVVLAX | 0.44a | 0.43a | 0.49a | 0.57a | 0.59a | 0.53a | |
| KAPLAX | 0.59a | 0.55a | 0.57a | 0.43a | 0.75a | 0.51a | |
Abbreviations: GJL, general joint laxity; HIERLAX_0°, hip internal-external–rotation laxity measured at 0°; HIERLAX_30°, hip internal-external–rotation laxity measured at 30°; HIERROM, hip internal-external–rotation range of motion measured clinically; KAPLAX, knee anterior-posterior laxity; KIERLAX, knee internal-external–rotation laxity; KVVLAX, knee varus-valgus laxity.
All values: P < .05 (1-tailed test).
Bold values indicate the female correlations.
We observed moderate correlations between hip laxity and measures of knee laxity and GJL, regardless of whether hip laxity was measured as HIERROM, HIERLAX_0°, or HIERLAX_30° (Table 3). Although these correlations generally held within each sex, relationships with hip laxity tended to be lower in women (fair) than in men (moderate) for KIERLAX and KAPLAX and tended to be lower in men (fair) than in women (moderate) for KVVLAX (Table 4). Results from the backward stepwise linear regression analyses indicate that when measures of knee laxity were accounted for, hip laxity in combination with KVVLAX was the strongest predictor of GJL (Table 5). This finding was consistent whether HIERROM (R2 = 0.42), HIERLAX_0° (R2 = 0.42), or HIERLAX_30° (R2 = 0.44) was entered into the model. However, because measures of HIERROM/HIERLAX were moderately correlated with KVVLAX, this combined model explained only 3% to 12% more variance than hip laxity (R2 range, 32.3% [HIERROM] to 41.0% [HIERLAX_30°]) or KVVLAX (R2 = 36.6%) explained independently. When analyses were stratified by sex (thus, the sample size was smaller and statistical power was lower), typically HIERROM/HIERLAX or KVVLAX (but not both) remained in the model.
Table 5.
Final Regression Summary Statistics When Predicting General Joint Laxity From Hip- and Knee-Laxity Measuresa
| Participants |
Hip Laxity Variable Entered |
R2 Value |
P Value |
Final Regression Equation: General Joint Laxity = |
| All | 0.417 | <.001 | –5.104 + 0.230KVVLAXb + 0.064HIERROMc | |
| HIER_0° | 0.417 | <.001 | –3.982 + 0.219KVVLAXb + 0.037HIERLAX_0°c | |
| HIER_30° | 0.442 | <.001 | –5.067 + 0.157KVVLAXc + 0.056HIERLAX_30°d | |
| Women | 0.324 | .021 | –0.359 + 0.281KVVLAXb | |
| HIER_0° | 0.347 | .016 | –4.980 + 0.066HIERLAX_0°b | |
| HIER_30° | 0.434 | .005 | –7.248 + 0.090HIERLAX_30°b | |
| Men | 0.448 | .021 | –10.902 + 0.463KVVLAXc + .119HIERROMc | |
| HIER_0° | 0.326 | .021 | –3.009 + 0.662KVVLAXb | |
| HIER_30° | 0.326 | .021 | –3.009 + 0.662KVVLAXb |
Abbreviations: HIERLAX_0°, hip internal-external–rotation laxity measured at 0°; HIERLAX_30°, hip internal-external–rotation laxity measured at 30°; HIERROM, hip internal-external–rotation range of motion measured clinically; KVVLAX, knee varus-valgus laxity.
Results reflect the final prediction equation once variables not significantly contributing to the model were removed.
P ≤ .05.
P ≤ .20.
P ≤ .10.
DISCUSSION
Our primary findings were large systematic differences between measures of HIERLAX and HIERROM, despite the fact that both measures were obtained with comparable precision and were strongly correlated in relative magnitude. The magnitude of error appears to be smaller for HIERROM than HIERLAX (based on both SEM and 95% limits-of-agreement calculations), but this largely reflects the smaller deviations in scores and magnitude of values for HIERROM. Consequently, we observed similar strengths of correlations between HIERLAX and HIERROM with measures of knee laxity and GJL. Once knee-laxity variables were also accounted for, the combination of either HIERROM or HIERLAX with KVVLAX was the strongest predictor of GJL, explaining about 40% of the variance. These findings were similar between sexes.
When we compared our clinical HIERROM values with those of previous researchers, the average values we obtained (80.4° ± 9.7°) were quite similar to other reported measures in healthy adults (range, 73.9° ± 11.8° to 82.98° ± 18.22°),17,21,32,33 as was our finding of greater motion in women (driven by greater hip internal rotation).17,21,34 We were unable to locate instrumented hip-laxity measures with which to compare our values. We were somewhat surprised to obtain higher laxity values in 0° than in 30° of hip flexion (due primarily to greater hip external-rotation motion), given prior cadaveric work demonstrating greater hip internal-external–rotation motion and less change in motion with ligament dissection at 30° versus 0°.27 However, direct comparisons between our in vivo values with this study may not be valid, as the authors of the cadaveric study did not report a standardized load limit at which motion was measured for each condition and removed all musculature to isolate the ligamentous support. As previously noted, in vivo laxity testing represents the combined passive resistance of the ligaments, muscles, and capsule to a displacing load. Musculotendinous structures that cross the joint may differentially affect passive resistance to hip displacement when measured at these same joint positions.
When comparing the clinical measurement of HIERROM versus instrumented measurement of HIERLAX, our hypotheses were only partially supported. Specifically, we found comparable levels of measurement precision and stronger associations between HIERLAX and HIERROM than we expected. However, despite these strong correlations, we obtained substantially larger values for HIERLAX than for HIERROM, even though both measurements (HIERLAX_0° and HIERROM) were taken in similar test positions. Although this difference in magnitude may be attributed to a greater load at which end motion was determined for HIERLAX, it is important to note that the magnitude of difference between these measurements became systematically larger as the magnitude of the measure increased (Figure 4). Despite these systematic differences, we observed similar strengths of association between HIERROM with knee-laxity measures and GJL as we did with HIERLAX (Tables 3 and 4). Thus, even though the 2 measures clearly differed in magnitude, our results suggest that comparable consistency and precision can be achieved with either HIERROM or HIERLAX, and they may be equally representative of relative passive hip-joint displacement. Yet our results are limited to a single tester and a single measurement of instrumented hip laxity; further work is needed to establish the extent to which each of these measures represents true capsuloligamentous laxity of the hip or predictive ability in assessing injury risk potential. Continuation of this research may be particularly relevant to those conducting prospective risk factor studies who wish to screen a large group of individuals for passive hip-joint displacement, given the need for more accessible, efficient, and low-cost measurement methods to facilitate this type of research.35 Additionally, given the subjective nature of determining end motion for HIERROM, it will be important to determine if comparable values can be obtained by multiple testers to ensure valid comparisons across studies and collaborating centers.
Our secondary purpose was to examine relationships between HIERLAX and HIERROM with measures of knee laxity and GJL. Our expectation that hip laxity would be a significant predictor of GJL was in large part supported. Associations between GJL and HIERROM, HIERLAX_0°, or HIERLAX_30° were consistently positive and moderate in strength (r = 0.44–0.66), and greater hip laxity (whether measured as HIERROM, HIERLAX_0°, or HIERLAX_30°) combined with greater frontal-plane knee laxity (KVVLAX) predicted the greatest variance in GJL (42%–44%). Collectively, these findings indicate that greater GJL, based on sagittal-plane thumb, wrist, elbow, and knee hyperextension and lumbar flexion mobility,4 also indicates greater transverse- and frontal-plane hip and knee laxity. Hence, individuals with greater GJL may have more challenges in stabilizing the hip and knee during sport activity, potentially explaining prior associations observed between GJL and ACL injury risk.1–3,12
Similarly, the moderate to strong correlations between hip and knee laxity may clarify why females with greater magnitudes of transverse- and frontal-plane knee laxity had greater relative inward collapse at the hip and knee during landing36 and why individuals with greater hip internal rotation landed in greater relative knee valgus and external rotation.19 This suggestion is biomechanically plausible, as a greater magnitude of hip laxity in females is largely driven by a greater magnitude of passive hip internal rotation, which may lead to a more internally rotated hip position upon landing. The relative balance of internal versus external hip rotation and laxity may also be important, based on observations of greater frontal-plane knee excursion in those with less relative hip external-rotation motion.16 More work is needed to determine the extent to which hip-laxity characteristics influence lower extremity neuromechanics during tasks that mimic the mechanical demands commonly associated with ACL injury mechanisms.35
Despite these associations, it is not yet clear whether the assessment of hip laxity would further discriminate injury potential beyond the laxity variables previously examined. To date, associations between joint laxity and ACL injury risk are largely based on sagittal-plane joint laxity (GJL, anterior knee laxity, genu recurvatum),1–3,37–41 with 1 study accounting for transverse-plane knee laxity42 and none accounting for rotational hip laxity. Given the growing interest in the role of hip mobility and stability as a potential ACL injury risk factor12,16,19,20 and the associations we observed in this study, further research is warranted to determine if the assessment of hip-joint laxity would (1) increase the sensitivity of GJL in predicting injury risk potential, (2) be a stronger discriminator of injury risk potential (either alone or in combination with discrete knee-laxity measures), or (3) simply provide information redundant to that already provided by GJL and other laxity variables. To facilitate this work, clinically accessible and cost-effective screening measures are needed. From this perspective, our findings suggest that the clinical measure of HIERROM can be used as a reliable, efficient, and low-cost measure of passive hip-joint displacement. Further, the moderate to strong correlations we observed between HIERROM and KVVLAX suggest that adding HIERROM to a generalized hypermobility assessment (if warranted) may capture additional aspects of transverse- and frontal-plane laxity while still maintaining the clinical utility of the examination. However, the current results are based on healthy individuals, and it will be important to examine these associations in athletic populations at risk for ACL and other lower extremity musculoskeletal injuries. Continuing efforts to identify the clinical assessments that best characterize an athlete's laxity profile and discriminate the injury risk potential are critical if we are to develop the most accurate clinical screening tools.
REFERENCES
- 1.Ramesh R, Von Arx O, Azzopardi T, Schranz PJ. The risk of anterior cruciate ligament rupture with generalised joint laxity. J Bone Joint Surg Br. 2005;87(6):800–803. doi: 10.1302/0301-620X.87B6.15833. [DOI] [PubMed] [Google Scholar]
- 2.Uhorchak JM, Scoville CR, Williams GN, Arciero RA, St Pierre P, Taylor DC. Risk factors associated with noncontact injury of the anterior cruciate ligament: a prospective four-year evaluation of 859 West Point cadets. Am J Sports Med. 2003;31(6):831–842. doi: 10.1177/03635465030310061801. [DOI] [PubMed] [Google Scholar]
- 3.Kramer LC, Denegar CR, Buckley WE, Hertel J. Factors associated with anterior cruciate ligament injury: history in female athletes. J Sports Med Phys Fitness. 2007;47(4):446–454. [PubMed] [Google Scholar]
- 4.Beighton P, Solomon L, Soskolne CL. Articular mobility in an African population. Ann Rheum Dis. 1973;32(5):413–418. doi: 10.1136/ard.32.5.413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shultz SJ, Schmitz RJ, Nguyen AD, Levine BJ. Joint laxity is related to lower extremity energetics during a drop jump landing. Med Sci Sports Exerc. 2010;42(4):771–780. doi: 10.1249/MSS.0b013e3181bbeaa6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Trimble MH, Bishop MD, Buckley BD, Fields LC, Rozea GD. The relationship between clinical measurements of lower extremity posture and tibial translation. Clin Biomech (Bristol Avon) 2002;17(4):286–290. doi: 10.1016/s0268-0033(02)00010-4. [DOI] [PubMed] [Google Scholar]
- 7.Bayer JL, Sekiya JK. Hip instability and capsular laxity. Oper Tech Orthop. 2010;20(4):237–241. [Google Scholar]
- 8.Philippon MJ, Schenker ML. Athletic hip injuries and capsular laxity. Oper Tech Orthop. 2005;15(3):261–266. [Google Scholar]
- 9.Carr AJ, Jefferson RJ, Benson MK. Joint laxity and hip rotation in normal children and in those with congenital dislocation of the hip. J Bone Joint Surg Br. 1993;75(1):76–78. doi: 10.1302/0301-620X.75B1.8421041. [DOI] [PubMed] [Google Scholar]
- 10.Sullivan D, Warren RF, Pavlov H, Kelman G. Stress fractures in 51 runners. Clin Orthop Relat Res. 1984;(187):188–192. [PubMed] [Google Scholar]
- 11.Wynne-Davies R. Acetabular dysplasia and familial joint laxity: two etiological factors in congenital dislocation of the hip: a review of 589 patients and their families. J Bone Joint Surg Br. 1970;52(4):704–716. [PubMed] [Google Scholar]
- 12.Yamazaki J, Muneta T, Ju YJ, Morito T, Okuwaki T, Sekiya I. Hip acetabular dysplasia and joint laxity of female anterior cruciate ligament-injured patients. Am J Sports Med. 2011;39(2):410–414. doi: 10.1177/0363546510381588. [DOI] [PubMed] [Google Scholar]
- 13.Chaudhari AM, Andriacchi TP. The mechanical consequences of dynamic frontal plane limb alignment for non-contact ACL injury. J Biomech. 2006;39(2):330–338. doi: 10.1016/j.jbiomech.2004.11.013. [DOI] [PubMed] [Google Scholar]
- 14.McLean SG, Huang X, Van den Bogert AJ. Association between lower extremity posture at contact and peak knee valgus moment during sidestepping: implications for ACL injury. Clin Biomech (Bristol, Avon) 2005;20(8):863–870. doi: 10.1016/j.clinbiomech.2005.05.007. [DOI] [PubMed] [Google Scholar]
- 15.Pollard CD, Sigward SM, Ota S, Langford K, Powers CM. The influence of in-season injury prevention training on lower-extremity kinematics during landing in female soccer players. Clin J Sport Med. 2006;16(3):223–227. doi: 10.1097/00042752-200605000-00006. [DOI] [PubMed] [Google Scholar]
- 16.Sigward SM, Ota S, Powers CM. Predictors of frontal plane knee excursion during a drop land in young female soccer players. J Orthop Sports Phys Ther. 2008;38(11):661–667. doi: 10.2519/jospt.2008.2695. [DOI] [PubMed] [Google Scholar]
- 17.Staheli LT, Corbett M, Wyss C, King H. Lower-extremity rotational problems in children. Normal values to guide management. J Bone Joint Surg Am. 1985;67(1):39–47. [PubMed] [Google Scholar]
- 18.Van Dillen LR, Bloom NJ, Gombatto SP, Susco TM. Hip rotation range of motion in people with and without low back pain who participate in rotation-related sports. Phys Ther Sport. 2008;9(2):72–81. doi: 10.1016/j.ptsp.2008.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nguyen A, Cone JR, Stevens LM. Influence of hip internal rotation range of motion on hip and knee motions during landing [abstract] J Athl Train. 2009;44((suppl)):S68. [Google Scholar]
- 20.Gomes JL, deCastro JV, Becker R. Decreased hip range of motion and noncontact injuries of the anterior cruciate ligament. Arthroscopy. 2008;24(9):1034–1037. doi: 10.1016/j.arthro.2008.05.012. [DOI] [PubMed] [Google Scholar]
- 21.Svenningsen S, Terjesen T, Auflem M, Berg V. Hip motion related to sex and age. Acta Orthop Scand. 1989;60(1):97–100. doi: 10.3109/17453678909150103. [DOI] [PubMed] [Google Scholar]
- 22.Shultz SJ, Shimokochi Y, Nguyen AD, Schmitz RJ, Beynnon BD, Perrin DH. Measurement of varus-valgus and internal-external rotational knee laxities in vivo, part I: assessment of measurement reliability and bilateral asymmetry. J Orthop Res. 2007;25(8):981–988. doi: 10.1002/jor.20397. [DOI] [PubMed] [Google Scholar]
- 23.Shultz SJ, Levine BJ, Nguyen AD, Kim HS, Montgomery MM, Perrin DH. A comparison of cyclic variations in anterior knee laxity, genu recurvatum and general joint laxity across the menstrual cycle. J Orthop Res. 2010;28(11):1411–1417. doi: 10.1002/jor.21145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shultz SJ, Schmitz RJ, Beynnon BD. Variations in varus/valgus and internal/external rotational knee laxity and stiffness across the menstrual cycle. J Orthop Res. 2011;29(3):318–325. doi: 10.1002/jor.21243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Madigan ML, Pidcoe PE. Changes in landing biomechanics during a fatiguing landing activity. J Electromyogr Kinesiol. 2003;13(5):491–498. doi: 10.1016/s1050-6411(03)00037-3. [DOI] [PubMed] [Google Scholar]
- 26.Leardini A, Cappozzo A, Cantani F, et al. Validation of a functional method for the extimation of hip joint centre location. J Biomech. 1999;32(1):33–103. doi: 10.1016/s0021-9290(98)00148-1. [DOI] [PubMed] [Google Scholar]
- 27.Martin HD, Savage A, Braly BA, Palmer IJ, Beall DP, Kelly B. The function of the hip capsular ligaments: a quantitative report. Arthroscopy. 2008;24(2):188–195. doi: 10.1016/j.arthro.2007.08.024. [DOI] [PubMed] [Google Scholar]
- 28.Denegar CR, Ball DW. Assessing reliability and precision of measurement: an introduction to intraclass correlation and standard error of measurement. J Sport Rehabil. 1993;2(1):35–42. [Google Scholar]
- 29.Bland M. An Introduction to Medical Statistics. 2nd ed. New York, NY: Oxford University Press;; 1995. [Google Scholar]
- 30.Portney LG, Watkins MP. Foundations of Clinical Research: Applications to Practice. 2nd ed. Upper Saddle River, NJ: Prentice Hall;; 2000. [Google Scholar]
- 31.Cohen J. Statistical Power Analysis for Behavioral Sciences. 2nd ed. Hillsdale, NJ: Laurence Erlbaum Associates;; 1988. [Google Scholar]
- 32.Kumar S, Sharma R, Gulati D, Dhammi IK, Aggarwal AN. Normal range of motion of hip and ankle in Indian population. Acta Orthop Traumatol Turc. 2011;45(6):421–424. doi: 10.3944/AOTT.2011.2612. [DOI] [PubMed] [Google Scholar]
- 33.Ellison JB, Rose SJ, Sharman SA. Patterns of hip rotation range of motion: a comparison between healthy subjects and patients with low back pain. Phys Ther. 1990;70(9):537–541. doi: 10.1093/ptj/70.9.537. [DOI] [PubMed] [Google Scholar]
- 34.Brophy RH, Chiaia TA, Maschi R, et al. The core and hip in soccer athletes compared by gender. Int J Sports Med. 2009;30(9):663–667. doi: 10.1055/s-0029-1225328. [DOI] [PubMed] [Google Scholar]
- 35.Shultz SJ, Schmitz RJ, Nguyen A, et al. ACL Research Retreat V: an update on ACL injury risk and prevention, March 25–27, 2010, Greensboro, NC. J Athl Train. 2010;45(5):499–508. doi: 10.4085/1062-6050-45.5.499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Shultz SJ, Schmitz RJ. Effects of transverse and frontal plane knee laxity on hip and knee neuromechanics during drop landings. Am J Sports Med. 2009;37(9):1821–1830. doi: 10.1177/0363546509334225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hewett TE, Lynch TR, Myer GD, Ford KR, Gwin RC, Heidt RS., Jr Multiple risk factors related to familial predisposition to anterior cruciate ligament injury: fraternal twin sisters with anterior cruciate ligament ruptures. Br J Sports Med. 2010;44(12):848–855. doi: 10.1136/bjsm.2008.055798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Loudon JK, Jenkins W, Loudon KL. The relationship between static posture and ACL injury in female athletes. J Orthop Sports Phys Ther. 1996;24(2):91–97. doi: 10.2519/jospt.1996.24.2.91. [DOI] [PubMed] [Google Scholar]
- 39.Myer GD, Ford KR, Paterno MV, Nick TG, Hewett TE. The effects of generalized joint laxity on risk of anterior cruciate ligament injury in young female athletes. Am J Sports Med. 2008;36(6):1073–1080. doi: 10.1177/0363546507313572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Scerpella TA, Stayer TJ, Makhuli BZ. Ligamentous laxity and non-contact anterior cruciate ligament tears: a gender based comparison. Orthopaedics. 2005;28(7):656–660. doi: 10.3928/0147-7447-20050701-12. [DOI] [PubMed] [Google Scholar]
- 41.Woodford-Rogers B, Cyphert L, Denegar CR. Risk factors for anterior cruciate ligament injury in high school and college athletes. J Athl Train. 1994;29(4):343–346. [PMC free article] [PubMed] [Google Scholar]
- 42.Branch TP, Browne JE, Campbell JD, et al. Rotational laxity greater in patients with contralateral anterior cruciate ligament injury than healthy volunteers. Knee Surg Sports Traumatol Arthrosc. 2010;18(10):1379–1384. doi: 10.1007/s00167-009-1010-y. [DOI] [PubMed] [Google Scholar]