Abstract
Context:
Cooling the body before exercise (precooling) has been studied as an ergogenic aid for many thermal conditions; however, airflow accompanying exercise is seldom reported.
Objective:
To determine whether the physiologic and ergogenic benefits of precooling before endurance exercise may be negated with semirealistic airflow in hot conditions.
Design:
Crossover study.
Setting:
Climate-controlled chamber in a research laboratory.
Patients or Other Participants:
Ten fit, healthy cyclists.
Intervention(s):
After a familiarization trial, participants completed 4 randomized, counterbalanced sessions consisting of no precooling versus precooling and no fan airflow versus airflow (~4.8 m/s) during exercise. Precooling was via chest-deep immersion (~24°C) for 1 hour or until core temperature dropped 0.5°C. Participants then cycled at 95% ventilatory threshold in a hot environment (temperature = 30°C, relative humidity = 50%) until volitional exhaustion, core temperature reached >39.5°C, or heart rate reached >95% of maximum.
Main Outcome Measure(s):
Thermal strain was assessed via core temperature (esophageal and rectal thermistors) and mean skin temperature (thermistors at 10 sites) and cardiovascular strain via heart rate and ratings of perceived exertion.
Results:
Endurance time (28 ± 12 minutes without precooling or airflow) increased by 30 ± 23 minutes with airflow (~109%; 95% confidence interval = 12, 45 minutes; P < .001) and by 16 ± 15 minutes with precooling (~61%; 95% confidence interval = 4, 25 minutes; P = .013), but it was not further extended when the strategies were combined (29 ± 21 minutes longer than control). During cycling without precooling or airflow, mean core and skin temperatures were higher than in all other trials. Precooling reduced heart rate by 7–11 beats/min during the first 5 minutes of exercise, but this attenuation ended by 15 minutes.
Conclusions:
Most laboratory-based precooling studies have (inadvertently) overestimated the extent of the physiologic and ergogenic benefits for typical athlete-endurance situations. Precooling increases work capacity effectively when airflow is restricted but may have little or no benefit when airflow is present.
Key Words: exercise, thermoregulation, endurance, cardiovascular strain, convection, cooling
Key Points
To attain realistic physiologic- and performance-specific results when testing athletes in a laboratory environment, airflow must be provided, at least for athletes who compete in sports in which there is natural airflow during competition (eg, running, cycling, and rowing).
Precooling is especially effective in reducing the initial cardiovascular and thermal strain of exercise exertion for activities lasting <15 minutes.
Combining precooling and airflow did not enhance performance results and did not decrease the thermal or cardiovascular strain of exercise any more than providing airflow alone in laboratory situations. Therefore, in sports that do not require protective gear, the benefits of precooling may be overestimated in the current literature.
Heat production during exercise causes body temperature to rise, challenging thermoregulatory homeostasis. High rates of body heat storage are associated with reduced exercise capacity in humans1–3 and other animals.4 Moderate heat strain combined with exercise has been shown to lower cardiac output, stroke volume, and central blood volume and to compromise cutaneous and even muscle perfusion.5 Although it has been shown that exercise in the heat can be limited by a critically high internal core temperature (TC),1,4 others have found that central fatigue occurs gradually as TC increases,6 potentially altering exercise pacing.7 Thus, the roles of high TC and cardiovascular strain as limiting factors in heat tolerance are not disputed, and interventions that delay or lessen the total volume of thermal strain experienced may improve work capacity.
Cooling the body before exercise (precooling) has been studied as an ergogenic aid for a range of exercise and environmental circumstances. Precooling is considered to benefit performance by widening the available margin for heat storage,3 thus allowing more work to be completed before the individual's core body temperature reaches the point at which impairments may arise. For example, fluid balance and cardiovascular strain may theoretically benefit from precooling via delayed or reduced requirements for sweating, cutaneous vasodilation, and redirected blood flow.1,8 Precooling can elicit varying physiologic and psychophysical effects. Some have reported that marked decreases in core and skin temperature at the onset of exercise as well as decreases in heart rate (HR) and cutaneous blood flow increase the volume of work completed,3,8 whereas others have shown less effective performance benefits9 or even adverse effects,10 although the disparities in the literature among various precooling, exercise, and thermometry protocols are substantial.11–13
A notable limitation within the precooling literature and, therefore, its interpretation, is that the natural airflow accompanying laboratory-based exercise is either seldom reported or is artificially low. Restricting airflow in warm environments reduces convective and evaporative heat loss,14 increases cardiovascular drift,15 and impairs exercise tolerance.16,17 This has been demonstrated when comparing stationary cycling in a laboratory with minimal airflow versus the same exercise with simulated outdoor wind and solar radiant heat load or with actual outdoor cycling.18 Namely, sweating rates were higher without fans compared with fanned or outdoor cycling (although the increase in rectal temperature was attenuated only in outdoor cycling in that study, unlike in other studies).14,17 Overall, the potential for an artificially low heat transfer exists within much of the precooling literature, which may lead to an overestimation of its physiologic and performance effects. Analogous to this potential overestimation, Saunders et al17 proposed that adequate laboratory airflow could negate any beneficial physiologic or performance effects from rehydration during cycling in the heat.
The purpose of our study, therefore, was to determine the separate and combined effects of precooling and exercise-realistic airflow on thermal, cardiovascular, and exercise tolerance responses during exercise in a warm, laboratory-based environment. We hypothesized that both precooling-only and airflow-only trials would decrease thermal, cardiovascular, and psychophysical strain and increase endurance capacity, whereas these benefits of precooling would be lessened in the presence of airflow.
METHODS
Ten active, healthy men were recruited to participate in this study, which was approved by the university's Human Ethics Committee in accordance with the Declaration of Helsinki. Participants were given a concise explanation of all experimental procedures and potential risks before granting their written, informed consent. Participants were local cyclists, ranging from recreationally active to regional multisport athletes. All were physically active on average 3–5 times per week for ~30–120 minutes per training session (road cycling, mountain biking, running); people who were active <3 times per week were not considered for this study. All participants were nonsmokers, were not taking any medication, and were free of any cardiovascular or respiratory diseases. No participant was acclimatized to the heat, as all testing took place during the Southern Hemisphere fall and winter (average minimum and maximum ambient temperatures from 7°C to 17°C) and all testing sessions with exposure to the heat chamber environment were separated by at least 1 week. We estimated adiposity using the Jackson-Pollock 7-site skinfold protocol.19
Research Design
After preliminary testing and a fully instrumented familiarization trial, each participant completed 4 trials in counterbalanced order after random assignment: (1) no precooling before exercise, no fan airflow during exercise (NP + NF); (2) no precooling, with fan airflow during exercise (NP + F); (3) precooling, no fan airflow (P + NF); (4) both precooling and fan airflow (P + F). Trials were performed at the same time of day within participants and separated by at least 7 days. Participants lay submerged chest deep in a custom-insulated bath for 1 hour before exercise in all trials, in either thermoneutral water (35°C) or cool water (24°C, details follow), before cycling at 95% ventilatory threshold (VT1) in an environment with a temperature of 30°C and relative humidity of 50%. Cycling began with a 2-minute warmup at 70% of the participant's workload, then progressed to 2 minutes at 80% before stepping to 95% VT1 until either volitional exhaustion or the ethically restricted end point of core temperature (>39.5°C) or HR (>95% maximum) was exceeded.
Experimental Measurements
We measured peak oxygen uptake from an incremental cycling test. Participants began cycling at 100 W on an electromagnetically braked cycle ergometer (Velotron v1.5; RaceMate Inc, Seattle, WA), increasing by 50 W every 3 minutes until volitional fatigue. Heart rate was monitored continuously using the R-R interval of consecutive depolarizations (Vantage NV; Polar Electro Inc, Port Washington, NY). Expired air was sampled breath by breath for calculation of ventilation (V̇E) and rates of oxygen uptake and CO2 production (Cortex Biophysik Metalyzer 3B, Leipzig, Germany). Criteria used to determine a valid V̇O2 peak were respiratory exchange ratio >1.15, attainment of age-predicted maximum HR, and volitional fatigue. We determined the first ventilatory threshold (VT1) using the ventilatory equivalent of oxygen method (V̇E/V̇O2), whereby a systematic increase in the V̇E/V̇O2 ratio occurred without a corresponding increase in the ventilatory equivalent of CO2.20
Chest-deep water immersion occurred at 24°C for precooling trials and 35°C for thermoneutral trials, and the water was stirred manually every 5 minutes. The choice of 24°C for precooling, as used previously,21–23 was intended to be practical and sufficiently cold to promote conductive and convective transfer while minimizing cold shock, discomfort, and shivering thermogenesis. Precooling stopped when core temperature decreased by 0.5°C or 1 hour had elapsed. The pre-exercise water immersion took place in the laboratory anteroom directly adjacent to the environmental chamber. Participants began the cycling protocol exactly 10 minutes after exiting the bath; this period was required for drying off, changing attire, and transferring to the environmental chamber. During trials requiring airflow, a large fan (655-mm diameter blade; Imasu IMS International, Tsuen Wan, Hong Kong) was placed 1 m in front of the participant. The fan height was adjusted to include airflow over the head, torso, both arms, and the upper legs, covering as much surface area as possible in the cycle position. The maximum average wind velocity at 1 m was 4.8 m/s. Whereas this air velocity is low for cyclists (and even for some competitive runners), the exponential effect of air velocity in heat transfer means that 4.8 m/s provides nearly all of the cooling effect that is observed in the airflow generated by cycling at competitive velocities.17 Hence, we use the term “semirealistic” airflow in this article. The lower airflow used here would also tend to cause a negative testing bias in our hypothesis, potentially underestimating the effect of airflow.
We measured core temperature at 2 locations using flexible thermistors (Mon-a-therm 400; Mallinckrodt Medical Inc, St Louis, MO). Esophageal thermistors were inserted to a depth estimated as adjacent to the right atrium.24 Rectal thermistors were inserted ~10 cm past the anus. Rectal temperatures were not recorded in the bath because water could penetrate the connection leads, potentially causing an offset in the recorded data. Skin temperature was measured at 10 right-side sites using insulated skin thermistors affixed to the skin surface with adhesive tape (Type EU; Grant Instruments, Cambridge, UK). We calculated mean skin temperature (T̄ SK) using standard area-based weightings25: T̄ SK = (0.07·forehead) + (0.175·scapula) + (0.0875·chest) + (0.0875·abdominal) + (0.07·bicep) + (0.07·forearm) + (0.05·finger) + (0.19·thigh) + (0.15·calf) + (0.05·foot). Temperatures were logged at 1-minute intervals (Grant 1200 series Squirrel data logger; Grant Instruments).
We obtained blood samples from finger pricks at rest and exhaustion to determine blood lactate concentrations in duplicate (1500 Sport YSI lactate analyzer; YSI Life Sciences, Yellow Springs, OH). Urine specific gravity was measured using a handheld refractometer (Atago, Tokyo, Japan). Sweat onset time was measured using 284-mm2 capsules glued to the upper-left chest (Collodion Flexible BP; PSM Healthcare, Auckland, New Zealand). The capsule was ventilated with dry air at a flow rate of 0.5–0.6 L/min (airflow model AWM5101; Honeywell, Freeport, IL). Changes in airflow and effluent humidity were relayed to a data-acquisition system for calculation of sweat onset (Chart Software v. 4.2.3; ADInstruments, Bella Vista, Australia). Body mass was measured before and after exercise. Participants were allowed to drink water ad libitum, and we added the amount of ingested water to their net mass loss when estimating sweat loss. Psychophysical measures were obtained at 15-minute intervals throughout the testing protocol and consisted of ratings of perceived thermal comfort or discomfort, thermal sensation,26 and ratings of perceived exertion.27
Data Analysis
We based our sample size on the majority of the precooling literature, in which significant results were noted when testing populations of 7 to 13 participants. Esophageal temperatures were graphed for each trial to remove artifacts (eg, due to water ingestion or aberrant swallowing) before conducting statistical analyses or averaging across participants. For all data, we calculated a 3-way repeated-measures analysis of variance (initial status [precooling or thermoneutral], airflow [airflow or no airflow], and time [baseline, end bath, 5 minutes of exercise, 15 minutes of exercise, end of exercise]). Analyses were limited to reduce the likelihood of type I error, and family-wise significance was set at an alpha level of .05. Five and 15 minutes were chosen as analysis points because they represented an early exercise point and the last point common to all participants in all trials, respectively. When 3-way interactions were not evident, 2-way analysis of variance was performed to test the interactive or (if absent) main effects of initial status and airflow while also checking for equal variance. We used the Sidak multiple-comparisons test post hoc. Data were analyzed using SPSS (version 17.0; SPSS Inc, Surrey, UK) and are expressed as means ± SDs, with 95% confidence intervals (CIs) for effects of interest.
RESULTS
Without precooling or fan airflow (NP + NF), participants cycled 28 ± 12 minutes, which was less than in any other experimental condition (P < .001). Precooling (P + NF) extended cycle time by 61% (43 ± 21 minutes; 95% CI = 4, 25 minutes; P = .013), and airflow (NP + F) increased cycle time by 109% (57 ± 31 minutes; 95% CI = 12, 45 minutes; P = .025) compared with the NP + NF trial. Performance time with precooling (before exercise) and airflow (during exercise) (P + F) was not further increased compared with airflow only (56 ± 29 minutes; 95% CI = −8, 7 minutes).
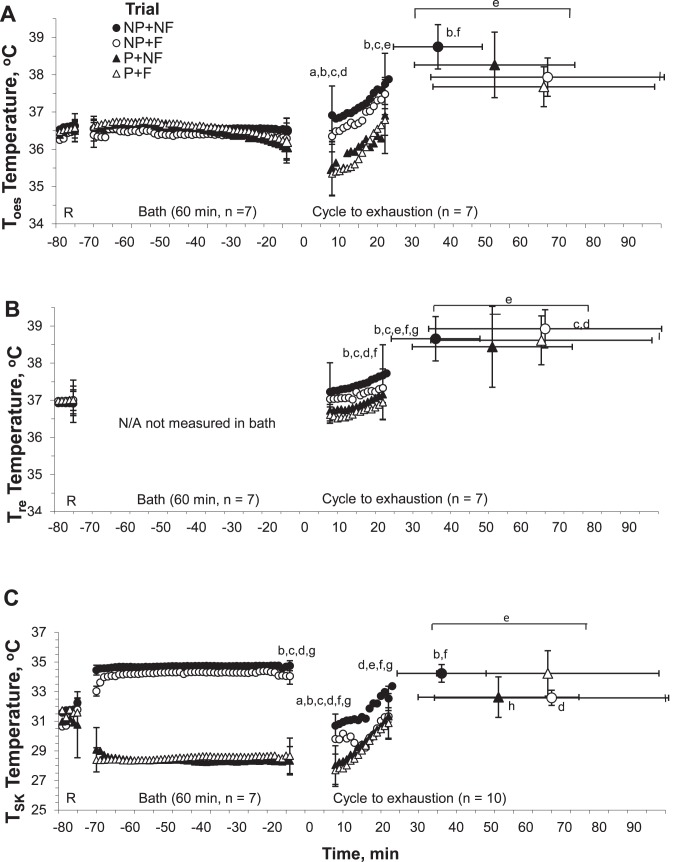
Two participants terminated the 60-minute precooling bath early (both within the last 5 minutes) after attaining the −0.5°C limit. There was no decrease in esophageal temperature immediately on completion of whole-body precooling; however, it showed a prominent after-drop of a full degree (−1.1 ± 0.7°C) when transitioning from the bath to cycle (Figure 1; P < .001). Esophageal temperature increased after 15 minutes of cycling (37.5 ± 0.8°C) and at exhaustion (38.2 ± 0.7°C) compared with baseline (36.5 ± 0.3°C) when collapsed across experimental trials (P < .001). Esophageal temperature at exhaustion was 0.9°C higher with no cooling (NP + NF; 95% CI = 0.3°C, 1.4°C) than with airflow (NP + F, P = .007) and 1.1°C higher than with both precooling and airflow (P + F; 95% CI = 0.5°C, 1.6°C; P = .003), but it was not different from precooling alone (NF + P; 95% CI = −0.5°C, 1.6°C; P = .160). The differences in rectal temperature (Tre) between trials were evident from the first 5 minutes of cycling, being higher in the control (NP + NF) and airflow (NP + F) trials than in both precooling trials (P < .001). The effect of precooling on Tre was maintained 15 minutes into cycling, whereas airflow alone had not yet attenuated Tre at this time. Rectal temperature was marginally higher at exhaustion in the NP + F trial compared with precooling alone (P + NF; 95% CI = 0.01°C, 0.6°C; P = .046) and precooling with the fan (P + F; 95% CI = 0.1°C, 0.5°C; P = .013). Precooling decreased T̄ SK by 3°C (95% CI = −4.3°C, −1.9°C, P = .026; Figure 1C). However, the lower T̄ SK attributed to precooling was not evident or distinguishable from the fan effect after 15 minutes of cycling; that is, there were no significant 2-way interaction effects (P = .964).
Figure 1.
A, Esophageal, B, rectal, and C, skin temperatures during the immersion and subsequent exercise protocol for each of the 4 trials: NP + NF, no precooling, no fan airflow during exercise (• closed circles); NP + F, no precooling, with fan airflow during exercise (○ open circles); P + NF, precooling, no fan airflow (▴ closed triangles); and P + F, both precooling and fan airflow (▵ open triangles). Data are means ± SD. a Indicates significant interaction between variables; b NP + NF different from P + F; c NP + F different from P + F; d NP + F different from P + NF; e A significant increase from baseline across all trials; f NP + NF different from NP+F; g NP + NF different from P+NF; h P + NF different from P + F (P < .05).
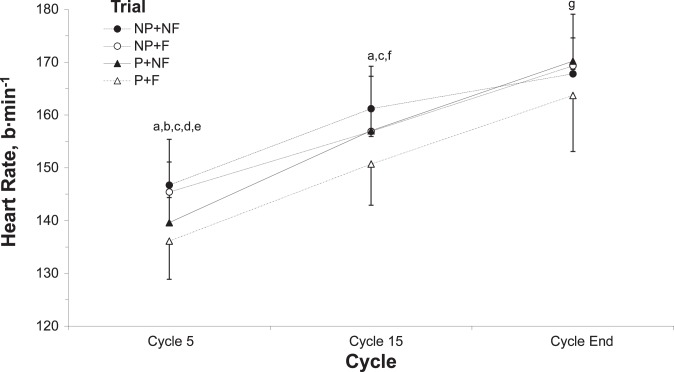
Heart rate increased from 62 to 142 beats/min after 5 minutes of cycling across all trials before drifting to 168 beats/min at exhaustion (88 ± 6% of HR range, P = .006; Figure 2). Bath temperature did not alter HR when participants were immersed, but precooling attenuated the rise in HR during the first 5 minutes of exercise by 7 and 11 beats/min, respectively (with and without airflow, P = .009 and P = .002, respectively). This effect disappeared at 15 minutes of cycling (P = .055). Fan airflow alone did not attenuate HR significantly at 5 or 15 minutes or exhaustion, yet the time of exhaustion occurred later with airflow (Figure 2).
Figure 2.
Heart rate in response to the immersion and subsequent exercise protocol for each of the 4 trials: NP + NF, no precooling, no fan airflow during exercise (• closed circles); NP + F, no precooling, with fan airflow during exercise (○ open circles); P + NF, precooling, no fan airflow (▴ closed triangles); P + F, both precooling and fan airflow (▵ open triangles). Data are means ± SD. a Indicates NP + NF different from P + F; b NP + NF different from P + NF; c NP + F different from P + F; d NP + F different from P + NF; e Significant interaction between trials; f P + NF different from P + F; g P + F different from all other trials (P < .05).
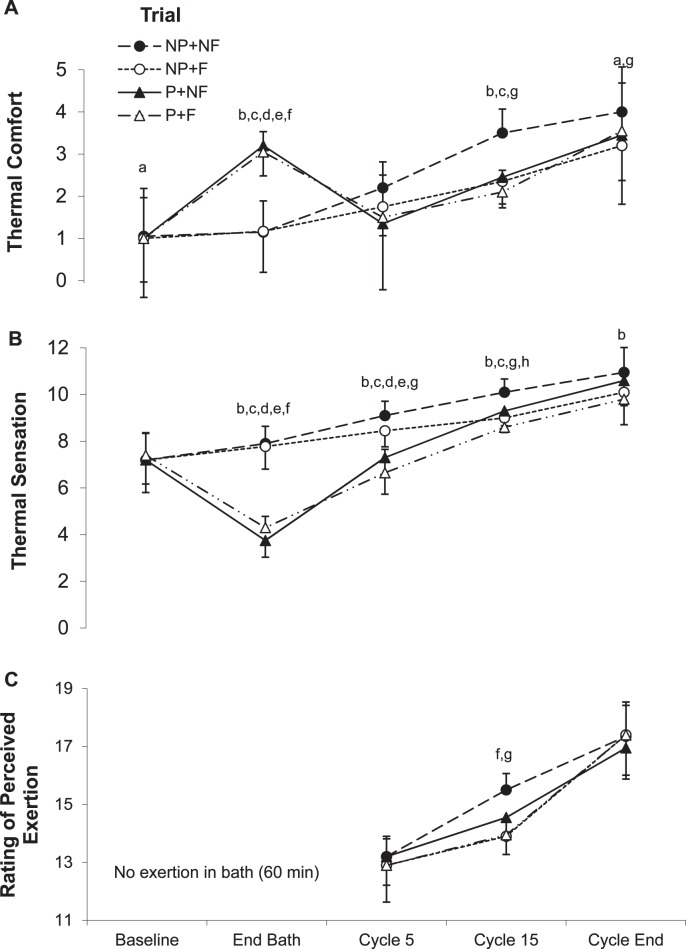
On average, participants gave mean ratings of 4 (cool) and 3 (uncomfortable) after precooling compared with mean ratings of 8 (warm) and 1 (comfortable) after the control bath for the thermal sensation and comfort scales, respectively (Figure 3). After 5 minutes of cycling, participants gave mean ratings of 7 (neutral) yet concurrently ranked their thermal comfort as 2 (slightly uncomfortable) in precooling trials. By 15 minutes, participants felt hotter, more uncomfortable, and as if they were at higher exertion rates in the NP + NF trial than with precooling, airflow, or combined, but the ratings were equivalent among the 3 intervention trials. At exhaustion, participants gave mean ratings of 10 (very hot) for thermal sensation and 4 (very uncomfortable) for comfort, irrespective of trial. The reasons for stopping differed across trials. In the control trial (NP + NF), 6 participants reached volitional tolerance and 4 stopped because of TC >39.5°C. With airflow (NP + F), 7 participants reached volitional tolerance and another showed signs of intolerance (ie, dizziness and nausea), whereas 2 stopped because of TC >39.5°C and 1 stopped because of HR >95% maximum. With precooling, irrespective of airflow (P + NF, P + F), 9 participants cited exhaustion as the reason for stopping, and the remaining participant had TC >39.5°C in P + F and subjective heat intolerance in P + NF.
Figure 3.
Changes in A, thermal comfort, B, thermal sensation, and C, ratings of perceived exertion (RPE) across the pre-bath and cycling protocol for each of the 4 trials: NP + NF, no precooling, no fan airflow during exercise (• closed circles); NP + F, no precooling, with fan airflow during exercise (○ open circles); P + NF, precooling, no fan airflow (▴ closed triangles); P + F, both precooling and fan airflow (▵ open triangles). Data are means ± SD. a Indicates difference among all data points across all trials; b NP + NF different from P + F; c NP + NF different from P + NF; d NP + F different from P + F; e NP + F different from P + NF; f Significant interaction between variables; g NP + NF different from all other trials; h P + NF different from P + F (P < .05).
Participants were euhydrated at baseline (urine specific gravity, 1.013 ± 0.009), equivalent across trials (P = .949). Sweat onset was delayed to 7.3 ± 1.4 minutes and 8.9 ± 1.5 minutes, respectively, for the P + NF and P + F trials, compared with the control trial (3.2 ± 1.0 minutes, P < .001). Relative rates of mass loss per hour were highest in the NP + NF trial (2.3 ± 1.1%·h−1) compared with P + NF (1.5 ± 1.0%·h−1), NP + F (1.6 ± 0.9%·h−1), and P + F (1.6 ± 0.8%·h−1; P = .046). The average amount of water consumed was higher in trials using airflow (NP + F = 818 ± 565 mL, P + F = 599 ± 666 mL versus NP + NF = 530 ± 505 mL, P + NF = 434 ± 352 mL; P = .039). However, when these data were expressed as a relative rate of water consumed (in milliliters) per minute of cycle time, the highest rates of water consumption occurred in trials without precooling: NP + NF = 19 ± 16 mL/min, NP + F = 18 ± 20 mL/min versus P + NF = 12 ± 11 mL/min, P + F = 11 ± 9 mL/min (P = .047). Lactate concentrations at exhaustion were not different among trials (from rest 1.3 ± 0.5 to 4.8 ± 2.0 mmol/L, P = .543).
DISCUSSION
In this study, we investigated the physiologic and performance effects of applying whole-body precooling before exercise in a warm environment and compared these effects with both the separate and combined influences of precooling with airflow. Although precooling increased exercise tolerance at a fixed absolute work rate, it was to a lesser extent than with modest airflow alone. Furthermore, the combination of precooling and airflow did not confer any greater effect than that provided by airflow alone. Overall, the ergogenic effects of precooling before exercise may partially reflect an artifactual lack of airflow in many laboratory-based investigations.
Providing airflow appears to be underrepresented in the experimental precooling literature in spite of evidence that it attenuates thermal and cardiovascular strain during exercising heat stress.18 Indeed, authors of only 1 laboratory-based precooling study appear to have reported realistic airflow in their experimental design, and they found the ergogenic effect for cycling performance to be modest (ie, 3.8% faster preloaded cycling time trial) despite using a substantive precooling intervention of a 30-minute immersion and a 40-minute ice-vest application.23 That study was not designed to investigate the separate and potentially additive effects of both precooling and airflow on performance. Decreases in skin temperature from adequate airflow are associated with reductions in skin blood flow and presumably reductions in cutaneous blood volume. Even at lower velocities of airflow, such as those experienced while running outdoors, the maximum heat-loss potential for evaporation can increase between 26% and 38% compared with typical laboratory testings.28 In this study, airflow reduced T̄ SK by 2°C at the end of exercise, which is comparable with the effects of precooling. More importantly, the beneficial effects of airflow would become more important with increasing exercise duration,15 just when precooling effects become less pronounced as core temperature increases.
Precooling may elicit much of its benefit from attenuating the heavily interdependent rises in cardiovascular, thermal, and psychophysical strain early in exercise. Precooling can enable higher work capacity by attenuating cardiovascular strain, limiting the inevitable elevations in HR1,3 and skin blood flow.8 An elevated HR can contribute to higher perceived exertion at a given exercise duration.27 The measurable cardiovascular29 and thermal effects of precooling appear to last up to 30 minutes into exercise30 but were less evident in the current study despite large magnitudes of cooling compared with other precooling studies.3,8,21 Precooling blunted the rise in HR by ~7 to 11 beats/min at the start of exercise; airflow in combination with precooling was the only trial that maintained this decrease 15 minutes into cycling. The lower HR with precooling and airflow presumably reflects less cutaneous blood flow1,8 and volume arising from cooler skin, irrespective of whether the core is cooler or not.
These results do not mean that conclusions from previous precooling studies are fallacious, only that the convective cooling provided by airflow is at least as effective in aiding exercise capacity and reducing physiologic strain. The extent of performance improvement with airflow is similar to previously reported improvements after precooling: 1% to 17%8,21,31 for exercise work or time trials and 12% to 37% for time-to-exhaustion trials in uncompensable heat.1,3 Note that time-to-exhaustion effects are many times larger than equivalent mean power effects. We had hypothesized that adding airflow to precooling would limit the physiologic and exercise capacity benefits of precooling, which it did. We had still anticipated that precooling and airflow together would produce the greatest exercise capacity and would attenuate measurable indices of cardiovascular and thermal strain compared with trials using only airflow or only precooling. However, performance time was not greater with strategies combined. Core and skin temperatures were also not different among precooling only, airflow only, or with strategies combined from the onset of exercise up to 15 minutes of cycling. Indeed, in every thermal, cardiovascular, and psychophysical variable tested, we found no appreciable differences between using realistic airflow and combining airflow with precooling.
Investigations on heat stress and exercise capacity can be influenced by research constraints, such as exercise type (free versus fixed pacing), and ethical constraints. One goal of our design was to explore whether a critical internal temperature for voluntary exhaustion exists, thus necessitating both a fixed-intensity design and prolonged exercise to elevate core temperature. Within this fixed–work-intensity design, we observed that, rather than terminate the cycling at a consistent core temperature across conditions, participants ended their sessions due to “exhaustion” (including perceptions of peripheral fatigue) across a range of core temperatures (TC from 37.4°C to 39.6°C) in trials using precooling. Although we acknowledge that differences in end-point criteria are not optimal, the fact remains that the participants did not reach a consistent critical internal temperature before ending exercise.
The placebo effects of precooling on performance outcomes can be substantial. Inherent in this study and most thermal physiology studies is the difficulty in blinding participants to the thermal environment or manipulation being used. In view of prevalent commercial and popular articles touting the benefits of precooling, it is challenging to prevent possible placebo effects in precooling studies, and this limitation is only sometimes acknowledged in the literature.12 Skin temperature and its rate of cooling provide powerful thermal inputs for perceptions of thermal status32 affecting thermal comfort, perceived exertion, and performance in the absence of core temperature changes. Given these and other methodologic discrepancies in the literature, the actual physiologic benefit of externally applied precooling as a method of reducing thermal and cardiovascular strain when participants are exposed to airflow indexed to their own power output remains to be proven. Finally, this study is limited to the thermal benefits of precooling before a single and sustained bout of exercise in the heat rather than the use of cooling as a recovery modality between multiple bouts of exercise or from exercise-induced hyperthermia. These latter scenarios present different dominant rationales and priorities for the use of cooling, namely as a muscular and metabolic recovery tool and a clinical priority, respectively.
CONCLUSIONS
Using semirealistic airflow is essential to accurately represent the true thermal environment observed in many sporting situations and for evaluating the physiologic, performance, or psychophysical benefits of ergogenic strategies aimed at reducing strain. As such, in many existing laboratory studies, externally applied precooling may have resulted in overestimation of the physiologic and ergogenic worth for outdoor sports.
Acknowledgments
ACKNOWLEDGMENTS
We thank the participants for their time and efforts, and we thank Mr Dene Irvine and Ms Robyn Bell for invaluable technical support.
FINANCIAL DISCLOSURES
Dr Cheung was supported by a Natural Sciences and Engineering Research Council of Canada Discovery grant (St Catharines, Ontario, Canada). Dr Morrison was supported by an Otago University Prestigious PhD Scholarship, and preparation of this manuscript was supported by an Otago University Postgraduate Publishing Bursary (Dr Morrison; Dunedin, Otago, New Zealand). The authors do not have any competing interests or financial interests regarding this research.
REFERENCES
- 1.González-Alonso J, Teller C, Andersen S, Jensen F, Hyldig T, Nielsen B. Influence of body temperature on the development of fatigue during prolonged exercise in the heat. J Appl Physiol. 1999;86(3):1032–1039. doi: 10.1152/jappl.1999.86.3.1032. [DOI] [PubMed] [Google Scholar]
- 2.Nybo L, Nielsen B. Hyperthermia and central fatigue during prolonged exercise in humans. J Appl Physiol (1985) 2001;91(3):1055–1060. doi: 10.1152/jappl.2001.91.3.1055. [DOI] [PubMed] [Google Scholar]
- 3.Olschewski H, Brück K. Thermoregulatory, cardiovascular, and muscular factors related to exercise after precooling. J Appl Physiol (1985) 1988;64(2):803–811. doi: 10.1152/jappl.1988.64.2.803. [DOI] [PubMed] [Google Scholar]
- 4.Fuller A, Carter RN, Brain Mitchell D. and abdominal temperatures at fatigue in rats exercising in the heat. J Appl Physiol (1985) 1998;84(3):877–883. doi: 10.1152/jappl.1998.84.3.877. [DOI] [PubMed] [Google Scholar]
- 5.González-Alonso J, Calbet JA, Nielsen B. Muscle blood flow is reduced with dehydration during prolonged exercise in humans. J Physiol. 1998;513(3):895–905. doi: 10.1111/j.1469-7793.1998.895ba.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Morrison S, Sleivert GG, Cheung SS. Passive hyperthermia reduces voluntary activation and isometric force production. Eur J Appl Physiol. 2004;91((5–6)):729–736. doi: 10.1007/s00421-004-1063-z. [DOI] [PubMed] [Google Scholar]
- 7.Kay D, Marino FE, Cannon J. Evidence of neuromuscular fatigue during high-intensity cycling in warm, humid conditions. Eur J Appl Physiol. 2001;84((1–2)):115–121. doi: 10.1007/s004210000340. St Clair Gibson A, Lambert MI, Noakes TD. [DOI] [PubMed] [Google Scholar]
- 8.Cotter JD, Sleivert GG, Roberts WS, Febbraio MA. Effect of pre-cooling, with and without thigh cooling, on strain and endurance exercise performance in the heat. Comp Biochem Physiol A Mol Integr Physiol. 2001;128(4):667–677. doi: 10.1016/s1095-6433(01)00273-2. [DOI] [PubMed] [Google Scholar]
- 9.Nielsen B, Strange S, Christensen NJ, Warberg J, Saltin B. Acute and adaptive responses in humans to exercise in a warm, humid environment. Pflugers Arch. 1997;434(1):49–56. doi: 10.1007/s004240050361. [DOI] [PubMed] [Google Scholar]
- 10.Bergh U, Ekblom B. Physical performance and peak aerobic power at different body temperatures. J Appl Physiol Respir Environ Exerc Physiol. 1979;46(5):885–889. doi: 10.1152/jappl.1979.46.5.885. [DOI] [PubMed] [Google Scholar]
- 11.Wegmann M, Faude O, Poppendieck W, Hecksteden A, Fröhlich M, Pre-cooling Meyer T. and sports performance: a meta-analytical review. Sports Med. 2012;42(7):545–564. doi: 10.2165/11630550-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 12.Marino FE. Methods, advantages, and limitations of body cooling for exercise performance. Br J Sports Med. 2002;36(2):89–94. doi: 10.1136/bjsm.36.2.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Quod MJ, Martin DT, Laursen PB. Cooling athletes before competition. Sports Med. 2006;36(8):671–682. doi: 10.2165/00007256-200636080-00004. [DOI] [PubMed] [Google Scholar]
- 14.Adams WC, Mack GW, Langhans GW, Nadel ER. Effects of varied air velocity on sweating and evaporative rates during exercise. J Appl Physiol (1985) 1992;73(6):2668–2674. doi: 10.1152/jappl.1992.73.6.2668. [DOI] [PubMed] [Google Scholar]
- 15.Shaffrath JD, Adams WC. Effects of airflow and work load on cardiovascular drift and skin blood flow. J Appl Physiol Respir Environ Exerc Physiol. 1984;56(5):1411–1417. doi: 10.1152/jappl.1984.56.5.1411. [DOI] [PubMed] [Google Scholar]
- 16.Nishi Y, Gagge AP. Direct evaluation of convective heat transfer coefficient by naphthalene sublimation. J Appl Physiol. 1970;29(6):830–838. doi: 10.1152/jappl.1970.29.6.830. [DOI] [PubMed] [Google Scholar]
- 17.Saunders AG, Dugas JP, Tucker R, Lambert MI, Noakes TD. The effects of different air velocities on heat storage and body temperature in humans cycling in a hot, humid environment. Acta Physiol Scand. 2005;183(3):241–255. doi: 10.1111/j.1365-201X.2004.01400.x. [DOI] [PubMed] [Google Scholar]
- 18.Brown SL, Banister EW. Thermoregulation during prolonged actual and laboratory-simulated bicycling. Eur J Appl Physiol Occup Physiol. 1985;54(1):125–130. doi: 10.1007/BF00426312. [DOI] [PubMed] [Google Scholar]
- 19.Jackson AS, Pollack ML. Generalized equations for predicting body density of men. Br J Nutr. 1978;40(3):497–504. doi: 10.1079/bjn19780152. [DOI] [PubMed] [Google Scholar]
- 20.Davis JA, Whipp BJ, Wasserman K. The relation of ventilation to metabolic rate during moderate exercise in man. Eur J Appl Physiol Occup Physiol. 1980;44(2):97–108. doi: 10.1007/BF00421087. [DOI] [PubMed] [Google Scholar]
- 21.Booth J, Marino F, Ward JJ. Improved running performance in hot humid conditions following whole body precooling. Med Sci Sports Exer. 1997;29(7):943–949. doi: 10.1097/00005768-199707000-00014. [DOI] [PubMed] [Google Scholar]
- 22.Drust B, Cable NT, Reilly T. Investigation of the effects of the pre-cooling on the physiological responses to soccer specific intermittent exercise. Eur J Appl Physiol. 2000;81((1–2)):11–17. doi: 10.1007/PL00013782. [DOI] [PubMed] [Google Scholar]
- 23.Quod MJ, Martin DT, Laursen PB, et al. Practical precooling: effect on cycling time trial performance in warm conditions. J Sport Sci. 2008;26(14):1477–1487. doi: 10.1080/02640410802298268. [DOI] [PubMed] [Google Scholar]
- 24.Mekjavic IB, Rempel ME. Determination of esophageal probe insertion length based on standing and sitting height. J Appl Physiol. 1990;69(1):376–379. doi: 10.1152/jappl.1990.69.1.376. [DOI] [PubMed] [Google Scholar]
- 25.International Organization for Standardization. Geneva, Switzerland: International Organization for Standardization; 2004. Evaluation of Thermal Strain by Physiological Measurements. Report No.: ISO 9886: 2004(E) [Google Scholar]
- 26.Gagge AP, Stolwijk JA, Hardy JD. Comfort and thermal sensations and associated physiological responses at various ambient temperatures. Environ Res. 1967;1(1):1–20. doi: 10.1016/0013-9351(67)90002-3. [DOI] [PubMed] [Google Scholar]
- 27.Borg GAV. Perceived exertion in relation to physical work load and pulse rate. Kunglia Fysioga Sallsk Lund Forth. 1962;31:105–115. [Google Scholar]
- 28.Cheuvront SN, Carter R, III, Montain SJ, Stephenson LA, Sawka MN. Influence of hydration and airflow on thermoregulatory control in the heat. J Therm Biol. 2004;29((7–8)):471–477. [Google Scholar]
- 29.Brück K, Olschewski H. Body temperature related factors diminishing the drive to exercise. Can J Physiol Pharmacol. 1986;65(6):1274–1280. doi: 10.1139/y87-203. [DOI] [PubMed] [Google Scholar]
- 30.Hessemer V, Langusch D, Brück LK, Bodeker RH, Breidenbach T. Effect of slightly lowered body temperatures on endurance performance in humans. J Appl Physiol Respir Environ Exerc Physiol. 1984;57(6):1731–1737. doi: 10.1152/jappl.1984.57.6.1731. [DOI] [PubMed] [Google Scholar]
- 31.Arngrimsson SA, Petitt DS, Stueck MG, Jorgensen DK, Cureton KJ. Cooling vest worn during active warm-up improves 5-km run performance in the heat. J Appl Physiol (1985) 2004;96(5):1867–1874. doi: 10.1152/japplphysiol.00979.2003. [DOI] [PubMed] [Google Scholar]
- 32.Cotter JD, Zeyl A, Keizer E, Taylor NAS. The role of local skin temperature in determining the perception of local and whole-body thermal state. In: Shapiro Y, Moran DS, Epstein Y, editors. Environmental Ergonomics: Recent Progress and New Frontiers. London, UK: Freund Publishing House, Ltd;; 1996. pp. 85–88. In. eds. [Google Scholar]