Abstract
Context:
Athletes who participate in throwing and racket sports consistently demonstrate adaptive changes in glenohumeral-joint internal and external rotation in the dominant arm. Measurements of these motions have demonstrated excellent intrarater and poor interrater reliability.
Objective:
To determine intrarater reliability, interrater reliability, and standard error of measurement for shoulder internal rotation, external rotation, and total arc of motion using an inclinometer in 3 testing procedures in National Collegiate Athletic Association Division I baseball and softball athletes.
Design:
Cross-sectional study.
Setting:
Athletic department.
Patients or Other Participants
Thirty-eight players participated in the study. Shoulder internal rotation, external rotation, and total arc of motion were measured by 2 investigators in 3 test positions. The standard supine position was compared with a side-lying test position, as well as a supine test position without examiner overpressure.
Results:
Excellent intrarater reliability was noted for all 3 test positions and ranges of motion, with intraclass correlation coefficient values ranging from 0.93 to 0.99. Results for interrater reliability were less favorable. Reliability for internal rotation was highest in the side-lying position (0.68) and reliability for external rotation and total arc was highest in the supine-without-overpressure position (0.774 and 0.713, respectively). The supine-with-overpressure position yielded the lowest interrater reliability results in all positions. The side-lying position had the most consistent results, with very little variation among intraclass correlation coefficient values for the various test positions.
Conclusions:
The results of our study clearly indicate that the side-lying test procedure is of equal or greater value than the traditional supine-with-overpressure method.
Key Words: shoulder, glenohumeral internal-rotation deficit, inclinometer, baseball, softball, range of motion
Key Points
Overhead athletes have been shown to demonstrate adaptive changes in glenohumeral internal and external rotation in the dominant arm.
To make decisions about appropriate interventions, clinicians must be able to accurately assess glenohumeral rotation.
For all 3 test positions, the side-lying test procedure demonstrated excellent reliability and, thus, is of equal or greater value than the traditional supine-with-overpressure method.
Athletes who participate in throwing and racket sports consistently demonstrate adaptive changes in glenohumeral-joint (GHJ) internal rotation (IR) and external rotation (ER) in the dominant arm.1 Numerous studies of throwing athletes substantiate that these athletes demonstrate a loss of IR and a gain in ER in the throwing arm.2–5 In a sample of 372 professional baseball players, Wilk et al5 noted that IR was an average of 7° less and ER was an average of 7° greater in the dominant arm than in the nondominant arm. Female softball players also display a similar pattern of IR loss and ER gain in the throwing shoulder.6
A loss of GHJ IR as compared with the contralateral side is termed glenohumeral IR deficit (GIRD). Glenohumeral IR deficit has received much attention, as it has been clinically and empirically linked to several musculoskeletal injuries, including superior labral anterior-posterior (SLAP) lesions,7 internal impingement,8 ulnar collateral ligament injury,9 and subacromial impingement.10,11 Injured throwers typically demonstrate a greater IR deficit than their uninjured counterparts.8,12 Based on the available literature,3,4,8,13 the average GIRD in throwers without a history of injury ranges from 10° to 15°. In a retrospective study, Dines et al9 found that throwers with ulnar collateral ligament insufficiency had an average GIRD of 28.5° compared with demographically matched asymptomatic throwers. In a retrospective study, Myers et al8 demonstrated 19.7° of GIRD in 11 throwers with pathologic internal impingement compared with matched asymptomatic throwers. Based on clinical observations, Burkhart et al7 retrospectively demonstrated that throwers with type II SLAP lesions and internal impingement had an average GIRD of 25°.
Pitchers with GIRD of 20° or more were nearly twice as likely to be injured as those with values less than 20°.12 Furthermore, those with a deficit of greater than 5° in total rotational range of motion (ROM), defined as the value of ER plus IR ROM at 90° of abduction, were 2.5 times more likely to sustain a shoulder injury.12
The cause of altered GHJ rotation in throwers is multifactorial and includes adaptive changes in the capsular, musculotendinous, and osseous structures. Differing opinions exist as to the relative contributions of the aforementioned factors. Regardless of the exact cause of GIRD, its presence is problematic and places throwers at risk for injury. Therefore, clinicians who work with this population must have reliable and valid methods of assessing rotational GHJ ROM to determine the necessity and effect of interventions designed to decrease GIRD. Despite the widespread interest in evaluating and treating GIRD, a universally accepted and reliable method of assessing IR has not been established. Numerous measurement techniques have been described in the literature, with little consistency in performance, position, or clinometric properties. Subtle differences in patient positioning, examiner stabilization, and instrumentation make comparisons and generalization of the data difficult.
It is generally accepted that scapular stabilization is required to allow for isolated GHJ motion. Investigators have found that IR measures are significantly lower with manual scapular stabilization when compared with no stabilization.14 Measurement of GHJ IR and ER in the supine position with the shoulder abducted to 90° and the scapula manually stabilized has been described by various authors12,15,16 and is commonly used in clinical practice. Scapular motion is manually restricted by applying a posterior force to the coracoid process and clavicle. Reliability statistics for this measurement have varied. Wilk et al12 analyzed the intrarater reliability of this measure and found an intraclass correlation coefficient (ICC) of 0.81 for IR and 0.87 for ER. Laudner et al17 obtained ICC values of 0.95 and 0.98 for intrarater reliability of ER and IR, respectively.
The sleeper stretch is a common exercise given to overhead athletes to increase the extensibility of the posterior soft tissue structures of the shoulder. The person lies on the side to be stretched, elevates the humerus to 90° on the support surface, and then passively internally rotates the shoulder with the opposite arm.18 One of the benefits of the stretch is that the scapula is stabilized by the supporting surface, theoretically allowing for isolated glenohumeral motion.
A few researchers have looked at the effectiveness of the sleeper stretch in increasing GHJ IR and noted mixed results. Laudner et al19 examined the acute effects of a manual application of the sleeper stretch on IR and ER in 33 National Collegiate Athletic Association Division I baseball players. Range-of-motion measurements were taken before and after completion of 3 sets of 30-second passive sleeper stretches. The data showed small but statistically significant increases in IR measures after the stretches. McClure et al18 compared changes in IR ROM after a 4-week stretching program in 2 groups, 1 that performed the sleeper stretch and 1 that performed the cross-body adduction stretch. Contrary to the authors' hypothesis, gains in the sleeper-stretch group were not significant compared with those of the control group or those of the cross-body stretch group. This result may, however, have been due to a small sample size that precluded the detection of statistical differences among groups.
The purpose of our study was to determine the intrarater reliability, interrater reliability, and standard error of measurement (SEM) for measurements of GHJ IR, ER, and total-arc ROM using an inclinometer under 3 testing procedures (supine with overpressure, supine without overpressure, and side lying) in Division I baseball and softball athletes. We also sought to determine whether ROM values differed between raters, among testing positions, or both.
METHODS
Participants
Participants in the study were National Collegiate Athletic Association Division I baseball and softball players. We chose a sample of convenience and enrolled 30 baseball and 8 softball players in the study. Participants were excluded if they had undergone shoulder surgery in the dominant arm, had concurrent adhesive capsulitis or concurrent cervical radiculopathy, or were less than 18 years of age. A signed informed consent was obtained for each participant, and institutional review board approval was obtained from the Mary Black Health System.
Procedures
Data collection took place on a single day during the teams' preseason physicals. Two licensed physical therapists performed all testing procedures. Before testing, the examiners attended two 1-hour training sessions to assure consistency in measurement techniques. An MIE bubble inclinometer (Patterson Medical Holdings, Inc/Sammons Preston, Warrenville, IL) was used to perform all measures. Glenohumeral-joint IR and ER were measured in 3 test positions by the 2 examiners. Test position and examiner order were randomized using the Microsoft Office Excel (Microsoft Corporation, Redmond, WA) random-number generation function. Measurements were taken on the dominant arm only.
Inclinometers were zeroed out on a vertical surface between participants. For all test positions, the inclinometer was positioned just proximal to the styloid process of the ulna on the dorsal surface of the forearm. Measurements were read aloud to assistants who recorded the measurements. Three trials were recorded for both GHJ IR and ER in each of the 3 test positions.
Supine-With-Overpressure Position
This test position is similar to the position typically described in the orthopaedic literature for the measurement of GHJ IR and ER with 90° of abduction.12,14,20 However, to save time and minimize potential error between examiners, we did not place a folded towel under the arm being measured. The athlete was asked to lie supine on the plinth. The examiner positioned the shoulder into 90° of abduction and 90° of elbow flexion with the arm in neutral rotation. Palpation of the coracoid process was used to judge scapular movement. The examiner moved the arm into IR until a capsular end feel was achieved, scapular movement occurred, or the participant complained of pain. Once the measurement was recorded, the arm was returned to neutral rotation before the next measurement trial took place. For ER, the examiner reset the arm into the starting position of 90° of abduction and 90° of elbow flexion with neutral rotation. The arm was moved into maximal ER with the plinth providing scapular stabilization until the examiner obtained a capsular end feel or the participant complained of pain. Three trials were performed and the arm was returned to neutral rotation between trials.
Supine-Without-Overpressure Position
This test position closely resembled the first test position. The key difference was that the examiner did not judge end ROM or provide scapular stabilization. Instead, the athlete allowed gravity to assist the extremity to end ROM independently without interference from the table or examiner. The athlete was positioned supine on the plinth with the arm positioned to 90° of abduction and 90° of elbow flexion with neutral GHJ rotation. The athlete was given oral instructions to “relax the arm forward.” As the gravity-assisted motion stopped, the inclinometer was placed in the same location as described above, and the measurement was recorded. If the athlete appeared to actively assist the arm to increase ROM, the trial was stopped, the instructions were reviewed, and a trial with tactile cues was used as needed. External rotation was measured in the same fashion. The athlete was again given oral instruction to “relax the arm backwards” into ER. Three trials were performed, with the examiner assisting the arm back to neutral rotation between trials.
Side-Lying Position
This test position was similar to the sleeper stretch, with very specific body positioning designed to limit torso rotation and maintain proper scapular position and stabilization. The participant lay on the dominant side with the arm at 90° of forward GHJ flexion and 90° of elbow flexion. The nondominant leg was positioned to 90° of hip flexion and placed on the plinth in front of the participant. The examiner manually positioned the scapula into maximal adduction and retraction by reaching around the participant and pulling the lateral scapular border toward the spine. The participant's nondominant hand was placed palm down in front of his or her stomach. The participant received oral instructions to maintain this position throughout testing. The examiner rotated the arm until a capsular end feel was obtained or the participant reported pain. Three trials were performed for each direction.
Data Analysis
We entered data into a Microsoft Office Excel spreadsheet and SPSS (version 21; SPSS Inc, Chicago, IL) for analysis. Intrarater and interrater reliability were assessed for IR, ER, and total-arc ROM in all 3 test positions using the ICC (model [2,k]) and associated 95% confidence interval as previously described.21 Additionally, from the obtained ICC and SD values, we determined precision of the measurement by calculating the SEM for all measurement conditions. Intraclass correlation coefficient values were interpreted as follows: values <0.40 indicated poor reproducibility, values in the range 0.40 to 0.75 indicated fair to good reproducibility, and values >0.75 indicated excellent reproducibility.22
A 2-way, mixed-model analysis of variance was used to determine the effect of test position and rater on measurements of IR, ER, and total arc of motion. An α level of .05 was set a priori. First, interaction effects (test position × rater) were assessed. If a significant interaction was present, we examined simple effects (effect of rater at each test position). Bonferroni adjusted P values were used to adjust for multiple pairwise comparisons.
RESULTS
Intrarater and interrater reliability results appear in Figures 1 and 2, respectively. Excellent intrarater reliability was noted for all 3 test positions and ROMs, with ICC values ranging from 0.93 to 0.99. Results for interrater reliability were less favorable. Reliability of IR was highest in the side-lying position (0.68), and reliability of ER and total-arc ROM was highest in the supine-without-overpressure position (0.774 and 0.713, respectively). The supine-with-overpressure position yielded the lowest interrater reliability results for all 3 measures. The side-lying position had the most consistent results, with very little variation among ICC values for the various test positions.
Figure 1.
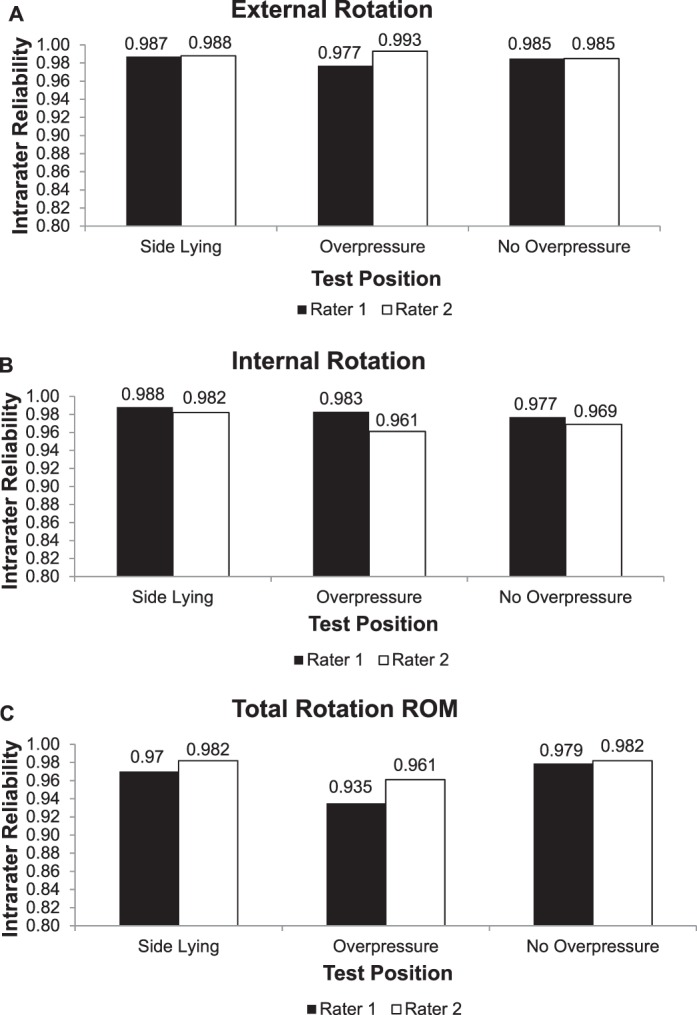
Intrarater reliability summarized in terms of intraclass correlation coefficients (model [2,k]). Abbreviation: ROM, range of motion.
Figure 2.
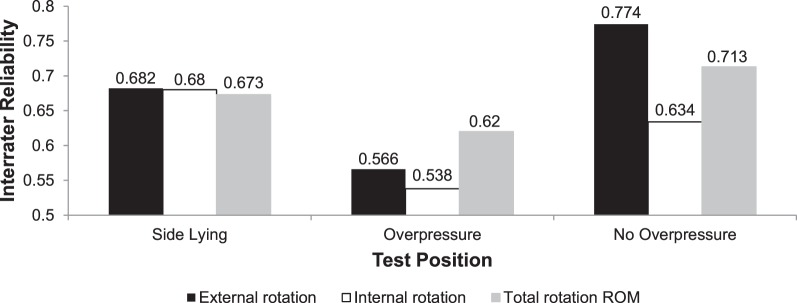
Interrater reliability summarized in terms of intraclass correlation coefficients (model [2,k]). Abbreviation: ROM, range of motion.
Next, we performed a 2-way analysis of variance to assess the effect of test position and rater on IR, ER, and total-arc ROM. A significant rater × test position interaction effect was noted for IR (P < .01). Subsequently, significant simple effects (the effect of position for each rater) were demonstrated (P < .01). Post hoc testing revealed differences among the side-lying, supine-with-overpressure, and supine-without-overpressure conditions for each rater (Table 1).
Table 1.
Internal Rotation Measured by 2 Raters in 3 Test Positions, ° (Mean, SD, and Standard Error of Measurement)
| Position, Rater |
Mean ± SD |
Standard Error of Measurement |
|
| Side lying, rater 1 | 54.5 ± 16.7a | 2.7 | |
| Side lying, rater 2 | 45.7 ± 12.0a | 1.9 | |
| Supine with overpressure, rater 1 | 42.1 ± 13.3b | 2.2 | |
| Supine with overpressure, rater 2 | 57.7 ± 9.9b | 1.6 | |
| Supine without overpressure, rater 1 | 65.6 ± 16.5c | 2.7 | |
| Supine without overpressure, rater 2 | 78.3 ± 15.1c | 2.5 |
Indicates difference between side-lying and supine-with-overpressure positions, based on Bonferroni adjusted P values.
Indicates difference between supine-with-overpressure and supine-without-overpressure positions, based on Bonferroni adjusted P values.
Indicates difference between side-lying and supine-without- overpressure positions, based on Bonferroni adjusted P values.
Similarly, a significant rater × test position interaction effect was noted for ER (P < .01). Subsequently, significant simple effects (the effect of position for each rater) were observed (P < .01). Post hoc testing revealed differences among the side-lying, supine-with-overpressure, and supine-without-overpressure conditions for each rater (Table 2).
Table 2.
External Rotation Measured by 2 Raters in 3 Test Positions, ° (Mean, SD, and Standard Error of Measurement)
| Position, Rater |
Mean ± SD |
Standard Error of Measurement |
| Side lying, rater 1 | 105.9 ± 11.8a | 1.9 |
| Side lying, rater 2 | 100.8 ± 14.2a | 2.3 |
| Supine with overpressure, rater 1 | 110.8 ± 11.6b | 1.9 |
| Supine with overpressure, rater 2 | 114.3 ± 18.5b | 3.0 |
| Supine without overpressure, rater 1 | 90.3 ± 15.5c | 2.5 |
| Supine without overpressure, rater 2 | 88.3 ± 16.4c | 2.7 |
Indicates difference between side-lying and supine-with-overpressure positions, based on Bonferroni adjusted P values.
Indicates difference between supine-with-overpressure and supine-without-overpressure positions, based on Bonferroni adjusted P values.
Indicates difference between side-lying and supine-without-overpressure positions, based on Bonferroni adjusted P values.
Lastly, a significant rater × test position interaction effect was also noted for total-arc ROM (P = .03). Subsequently, significant simple effects (the effect of position for each rater) were noted (P < .01). Post hoc testing revealed differences among the side lying and 2 supine conditions for rater 2 but not rater 1 (Table 3).
Table 3.
Total Arc of Motion Measured by 2 Raters in 3 Test Positions, ° (Mean, SD, and Standard Error of Measurement)
| Position, Rater |
Mean ± SD |
Standard Error of Measurement |
| Side lying, rater 1 | 160.1 ± 15.9 | 2.6 |
| Side lying, rater 2 | 147.1 ± 18.3a | 3.0 |
| Supine with overpressure, rater 1 | 154.3 ± 18.7 | 3.0 |
| Supine with overpressure, rater 2 | 170.8 ± 20.4 | 3.3 |
| Supine without overpressure, rater 1 | 155.6 ± 24.2 | 3.9 |
| Supine without overpressure, rater 2 | 166.4 ± 25.6b | 4.1 |
Indicates difference between side-lying and supine-with-overpressure positions, based on Bonferroni adjusted P values.
Indicates difference between side-lying and supine-without-overpressure positions, based on Bonferroni adjusted P values.
DISCUSSION
Several authors3,4,23 have documented increased humeral retroversion in the dominant arm of throwers, and they attribute the loss of GHJ IR and gain in ER ROM to this bony adaptation. A larger angle of retroversion would allow greater ER before the anterior capsule and glenohumeral ligaments limit further movement. Conversely, a larger angle of retroversion would result in less IR, as the humeral head would more quickly be limited by the posterior capsule.15 These authors found that although the arc of shoulder ROM shifts toward greater ER and IR, the total-arc ROM should remain the same as the contralateral limb. In other words, if the loss of IR equals the gain of ER, this can be attributed to osseous changes and should be considered physiologic. However, if the loss of IR exceeds the gain in ER, this is attributed to soft tissue changes and is considered pathologic.20
Glenohumeral-joint IR reaches peak angular velocities of nearly 7000°/s,24,25 and deceleration during the follow-through phase of pitching occurs at a velocity of 500 000°/s,26 creating a large force for the posterior shoulder to counteract. Over time, this repetitive stress is thought to result in microtrauma to the posterior capsule, leading to thickening and adaptive shortening. Several researchers7,27,28 reported similar results based on surgical observations that throwers who displayed GIRD had a contracted and thickened posterior-inferior recess of the posterior band of the inferior glenohumeral ligament complex.
Contrary to these reports, other investigators1 have found no side-to-side differences in anterior or posterior GHJ translation in professional pitchers, calling into question the theory of posterior capsular tightness. Another group29 found that maximal IR values displayed by pitchers are not a fixed value and that decreased passive IR can be seen up to 24 hours after a throwing session. The deceleration phase of throwing creates large compressive forces at the shoulder and requires the posterior rotator cuff musculature to contract eccentrically. The cumulative effect of eccentric muscle trauma may contribute to the pathologic loss of GHJ IR. Furthermore, in a recent report30 on Division I baseball players, an intrasession improvement in GHJ horizontal adduction and IR was noted after the application of a muscle-energy technique designed to lengthen the musculotendinous units of the posterior shoulder. Collectively, these findings highlight the contribution of musculotendinous structures, such as the posterior deltoid and posterior rotator cuff, in the development of GIRD in overhead athletes. Taken as a whole, this large body of research establishes a great need for reliable measures of GHJ IR ROM in this population.
The SEM for all 3 test positions is relatively low, ranging from 2.6° to 4.0°, with the side-lying position yielding the lowest SEM. Using a testing technique with low SEM is vitally important, as a recent study12 demonstrated that athletes with a total-arc ROM difference of as little as 5° were at 2.5 times greater risk for injury. Our measurement techniques must be accurate enough to detect this small amount of motion beyond measurement error for us to recommend appropriate interventions.
Our study differs from many previous studies in that a single examiner using an inclinometer performed all measurements, whereas previous researchers used a 2-examiner measurement system. Single-examiner testing may be less time consuming and allows greater autonomy on the part of the examiner. Inclinometer measurements may also be more time efficient and associated with less error than goniometry.
Supine ROM measurements in our study were taken in the coronal plane without a towel placed under the humerus, in contrast to many previous groups who used a towel to avoid horizontal abduction. We selected this position because it more closely resembles the shoulder position required during throwing, specifically in the late cocking and acceleration phases. In addition, previous authors12,31,32 have used this test position with good to excellent reliability statistics. However, the lack of towel placement under the humerus likely placed the arm in slight horizontal abduction. This position may have placed tension on the anterior band of the inferior glenohumeral ligament complex and resulted in lower ER values.
We measured total-arc ROM because this measure would be least affected by the arm's starting position. The mean total-arc ROM in our study ranged from 154° to 162°. These values are substantially lower than those reported in many other studies.* The smallest total-arc ROM previously reported was 159.3°,4 and the largest was 203.4°,33 with most measurements ranging from 170° to 200°. One possible explanation for our small ROM results is that the examiners were overly tentative in their measurements and did not provide adequate pressure to fully achieve end ROM. Secondly, the single-examiner testing technique could have impaired force generation and end-range determination. Alternatively, the smaller ROM could indicate greater scapular stabilization, as this was a high priority during examiner training sessions. Several groups have documented that manual scapular stabilization decreases GHJ IR.14,16,31 Boon and Smith14 also noted improved intrarater and interrater reliability for IR when the scapula was stabilized.
Results for intrarater reliability for IR and ER were extremely high in all 3 test positions. These results are consistent with findings from previous authors12,15,17,27,29,35,36 who investigated the supine-with-overpressure technique. However, the interrater reliability results were quite different. Although interrater reliability values varied with the test position, all 3 test positions yielded values in the same fair to good reproducibility category.22 Interestingly, the only measure with excellent interrater reliability was ER in the supine-without-overpressure position. The greater reliability may be due to improved scapular stabilization provided by the table and overpressure provided by gravity, thus eliminating examiner influence. The modest ICC values obtained for interrater reliability must be interpreted in light of the small SEM we noted. Although we tested 38 participants, our sample was fairly homogeneous, resulting in a relatively small between-subjects variance, especially compared with the between-raters variance. This may have contributed to low interrater reliability ICC values in the presence of the small SEM noted in our results.22 This study was performed with Division I athletes who participate in throwing sports because of their particular susceptibility to GIRD-related loss of function. However, future studies may be needed to assess reliability in samples with a wider variance of shoulder-rotation ROM.
Lunden et al37 compared IR in the supine versus side-lying test position and found the former position yielded higher interrater reliability. These authors noted ICC values of 0.81 and 0.88 for the supine and side-lying measurements, respectively. Our results support those of Lunden et al37 in that the side-lying test position had greater interrater reliability; however, the ICC values were substantially lower (0.54 and 0.68, respectively). Lunden et al37 did not measure ER, so we cannot compare the total-arc ROM measurements.
The side-lying test position had the most consistent levels of interrater reliability for IR, ER, and total-arc ROM. This may indicate that better scapular stabilization was achieved in this position. Scapular stabilization is accomplished by having the participant's body weight fix the scapula against the plinth and is independent from examiner influence. This eliminates 1 source of error between examiners and allows greater focus on end-range determination and ROM measurement. Also, the side-lying test position places more isolated strain on the posterior shoulder musculature because the arm is positioned in 90° of horizontal adduction. The horizontal adduction or Tyler test for posterior shoulder tightness is positively correlated with GIRD.10,17,27,38 Using muscle-energy techniques to stretch the shoulder horizontal abductors improves ROM of IR and horizontal adduction more effectively than using muscle-energy techniques to stretch the shoulder external rotators.30 For this reason, the side-lying position may more accurately target the tissues responsible for GIRD.
The analysis of variance assessed whether ROM differed between testing positions and between examiners. For ER, there was a significant effect of position, indicating that ER values differed based on the position in which they were measured. Furthermore, the interaction was significant, demonstrating that the effect of the testing position was not the same for both examiners. These same interactions were also present for total-arc ROM. Analysis of IR revealed significant effects of both position and rater, reflecting that ROM differed significantly between testing positions and between examiners. Collectively, the results of the analysis of variance help to explain potential sources of error and indicate that the observed differences in the ROM values for each test position were greater than would be expected by chance alone.
Our study had several limitations. First, the sample size was relatively small and included both baseball and softball athletes at all positions. Additionally, the number of measurement trials per athlete might have been excessive. Testing all 3 positions in each direction for 3 trials for both examiners resulted in 18 measurement trials per athlete. Excessive shoulder manipulation might have altered the pliability of tissues during testing. Examiner and test order were randomized in an attempt to mitigate the effect of repeated measures; however, in future studies, researchers may consider performing fewer measurement trials per athlete. Furthermore, we did not use a towel underneath the humerus to limit horizontal abduction, and this may have led to smaller values for ER and total arc than in previous investigations. Lastly, the poor results for the supine-with-overpressure test position could be accounted for by lack of appropriate training. Training time for this test position was less because it is so common to clinical practice, and this may have resulted in less consistency between examiners.
CONCLUSIONS
The results of our study clearly indicate that the side-lying test procedure is of equal or greater value than the traditional supine-with-overpressure method for determining intrarater and interrater reliability and standard error of measurement for shoulder IR, ER, and total-arc ROM. These positive results may be due to the improved scapular stabilization provided by the plinth and decreased examiner error. Additionally, testing without overpressure involves the least examiner influence and may be worthy of further consideration based on the high ER interrater reliability we observed. Adding a consistent force, such as a 3- to 5-pound (1.4–2.3-kg) weight, may improve the consistency of ROM values. We encourage future researchers to focus on test positions feasible for a single examiner, as 2-person procedures pose many barriers to implementation in the clinical setting.
Footnotes
References 1, 3–5, 12, 14, 15, 27, 29, 33, 34.
REFERENCES
- 1.Borsa PA, Wilk KE, Jacobson JA, et al. Correlation of range of motion and glenohumeral translation in professional baseball pitchers. Am J Sports Med. 2005;33(9):1392–1399. doi: 10.1177/0363546504273490. [DOI] [PubMed] [Google Scholar]
- 2.Bigliani LU, Codd TP, Connor PM, Levine WN, Littlefield MA, Hershon SJ. Shoulder motion and laxity in the professional baseball player. Am J Sports Med. 1997;25(5):609–613. doi: 10.1177/036354659702500504. [DOI] [PubMed] [Google Scholar]
- 3.Crockett HC, Gross LB, Wilk KE, et al. Osseous adaptation and range of motion at the glenohumeral joint in professional baseball pitchers. Am J Sports Med. 2002;30(1):20–26. doi: 10.1177/03635465020300011701. [DOI] [PubMed] [Google Scholar]
- 4.Reagan KM, Meister K, Horodyski MB, Werner DW, Carruthers C, Wilk K. Humeral retroversion and its relationship to glenohumeral rotation in the shoulder of college baseball players. Am J Sports Med. 2002;30(3):354–360. doi: 10.1177/03635465020300030901. [DOI] [PubMed] [Google Scholar]
- 5.Wilk KE, Meister K, Andrews JR. Current concepts in the rehabilitation of the overhead throwing athlete. Am J Sports Med. 2002;30(1):136–151. doi: 10.1177/03635465020300011201. [DOI] [PubMed] [Google Scholar]
- 6.Dover GC, Kaminski TW, Meister K, Powers ME, Horodyski M. Assessment of shoulder proprioception in the female softball athlete. Am J Sports Med. 2003;31(3):431–437. doi: 10.1177/03635465030310031801. [DOI] [PubMed] [Google Scholar]
- 7.Burkhart SS, Morgan CD, Kibler WB. The disabled throwing shoulder: spectrum of pathology, part I: pathoanatomy and biomechanics. Arthroscopy. 2003;19(4):404–420. doi: 10.1053/jars.2003.50128. [DOI] [PubMed] [Google Scholar]
- 8.Myers JB, Laudner KG, Pasquale MR, Bradley JP, Lephart SM. Glenohumeral range of motion deficits and posterior shoulder tightness in throwers with pathologic internal impingement. Am J Sports Med. 2006;34(3):385–391. doi: 10.1177/0363546505281804. [DOI] [PubMed] [Google Scholar]
- 9.Dines JS, Frank JB, Akerman M, Yocum LA. Glenohumeral internal rotation deficits in baseball players with ulnar collateral ligament insufficiency. Am J Sports Med. 2009;37(3):566–570. doi: 10.1177/0363546508326712. [DOI] [PubMed] [Google Scholar]
- 10.Tyler TF, Nicholas SJ, Roy T, Gleim GW. Quantification of posterior capsule tightness and motion loss in patients with shoulder impingement. Am J Sports Med. 2000;28(5):668–673. doi: 10.1177/03635465000280050801. [DOI] [PubMed] [Google Scholar]
- 11.Harryman DT, Sidles JA, Clark JM, McQuade KJ, Gibb TD, Matsen FA. Translation of the humeral head on the glenoid with passive glenohumeral motion. J Bone Joint Surg Am. 1990;72(9):1334–1343. [PubMed] [Google Scholar]
- 12.Wilk KE, Macrina LC, Fleisig GS, et al. Correlation of glenohumeral internal rotation deficit and total rotational motion to shoulder injuries in professional baseball pitchers. Am J Sports Med. 2011;39(2):329–335. doi: 10.1177/0363546510384223. [DOI] [PubMed] [Google Scholar]
- 13.Brown LP, Niehues SL, Harrah A, Yavorsky P, Hirshman HP. Upper extremity range of motion and isokinetic strength of the internal and external shoulder rotators in major league baseball players. Am J Sports Med. 1988;16(6):577–585. doi: 10.1177/036354658801600604. [DOI] [PubMed] [Google Scholar]
- 14.Boon AJ, Smith J. Manual scapular stabilization: its effect on shoulder rotational range of motion. Arch Phys Med Rehabil. 2000;81(7):978–983. doi: 10.1053/apmr.2000.5617. [DOI] [PubMed] [Google Scholar]
- 15.Chant CB, Litchfield R, Griffin S, Thain LM. Humeral head retroversion in competitive baseball players and its relationship to glenohumeral rotation range of motion. J Orthop Sports Phys Ther. 2007;37(9):514–520. doi: 10.2519/jospt.2007.2449. [DOI] [PubMed] [Google Scholar]
- 16.Ellenbecker TS, Roetert EP, Bailie DS, Davies GJ, Brown SW. Glenohumeral joint total rotation range of motion in elite tennis players and baseball pitchers. Med Sci Sports Exerc. 2002;34(12):2052–2056. doi: 10.1097/00005768-200212000-00028. [DOI] [PubMed] [Google Scholar]
- 17.Laudner KG, Stanek JM, Meister K. Assessing posterior shoulder contracture: the reliability and validity of measuring glenohumeral joint horizontal adduction. J Athl Train. 2006;41(4):375–380. [PMC free article] [PubMed] [Google Scholar]
- 18.McClure P, Balaicuis J, Heiland D, Broersma ME, Thorndike CK, Wood A. A randomized controlled comparison of stretching procedures for posterior shoulder tightness. J Orthop Sports Phys Ther. 2007;37(3):108–114. doi: 10.2519/jospt.2007.2337. [DOI] [PubMed] [Google Scholar]
- 19.Laudner KG, Sipes RC, Wilson JT. The acute effects of sleeper stretches on shoulder range of motion. J Athl Train. 2008;43(4):359–363. doi: 10.4085/1062-6050-43.4.359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lintner D, Mayol M, Uzodinma O, Jones R, Labossiere D. Glenohumeral internal rotation deficits in professional pitchers enrolled in an internal rotation stretching program. Am J Sports Med. 2007;35(4):617–621. doi: 10.1177/0363546506296736. [DOI] [PubMed] [Google Scholar]
- 21.Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull. 1979;86(2):420–428. doi: 10.1037//0033-2909.86.2.420. [DOI] [PubMed] [Google Scholar]
- 22.Portney LG, Watkins MP. Foundations of Clinical Research: Applications to Practice. 2nd ed. New York, NY: Pearson;; 1999. [Google Scholar]
- 23.Osbahr DC, Cannon DL, Speer KP. Retroversion of the humerus in the throwing shoulder of college baseball pitchers. Am J Sports Med. 2002;30(3):347–353. doi: 10.1177/03635465020300030801. [DOI] [PubMed] [Google Scholar]
- 24.Dillman CJ, Fleisig GS, Andrews JR. Biomechanics of pitching with emphasis upon shoulder kinematics. J Orthop Sports Phys Ther. 1993;18(2):402–408. doi: 10.2519/jospt.1993.18.2.402. [DOI] [PubMed] [Google Scholar]
- 25.Pappas AM, Zawacki RM, Sullivan TJ. Biomechanics of baseball pitching: a preliminary report. Am J Sports Med. 1985;13(4):216–222. doi: 10.1177/036354658501300402. [DOI] [PubMed] [Google Scholar]
- 26.Bandy WD, Irion JM. The effect of time on static stretch on the flexibility of the hamstring muscles. Phys Ther. 1994;74(9):845–852. doi: 10.1093/ptj/74.9.845. [DOI] [PubMed] [Google Scholar]
- 27.Myers JB, Oyama S, Wassinger CA, et al. Reliability, precision, accuracy, and validity of posterior shoulder tightness assessment in overhead athletes. Am J Sports Med. 2007;35(11):1922–1930. doi: 10.1177/0363546507304142. [DOI] [PubMed] [Google Scholar]
- 28.Ticker JB, Beim GM, Warner JJ. Recognition and treatment of refractory posterior capsular contracture of the shoulder. Arthroscopy. 2000;16(1):27–34. doi: 10.1016/s0749-8063(00)90124-5. [DOI] [PubMed] [Google Scholar]
- 29.Reinold MM, Wilk KE, Macrina LC, et al. Changes in shoulder and elbow passive range of motion after pitching in professional baseball players. Am J Sports Med. 2008;36(3):523–527. doi: 10.1177/0363546507308935. [DOI] [PubMed] [Google Scholar]
- 30.Moore SD, Laudner KG, McLoda TA, Shaffer MA. The immediate effects of muscle energy technique on posterior shoulder tightness: a randomized controlled trial. J Orthop Sports Phys Ther. 2011;41(6):400–407. doi: 10.2519/jospt.2011.3292. [DOI] [PubMed] [Google Scholar]
- 31.Awan R, Smith J, Boon AJ. Measuring shoulder internal rotation range of motion: a comparison of 3 techniques. Arch Phys Med Rehabil. 2002;83(9):1229–1234. doi: 10.1053/apmr.2002.34815. [DOI] [PubMed] [Google Scholar]
- 32.Hayes K, Walton JR, Szomor ZR, Murrell GA. Reliability of five methods for assessing shoulder range of motion. Aust J Physiother. 2001;47(4):289–294. doi: 10.1016/s0004-9514(14)60274-9. [DOI] [PubMed] [Google Scholar]
- 33.Borsa PA, Dover GC, Wilk KE, Reinold MM. Glenohumeral range of motion and stiffness in professional baseball pitchers. Med Sci Sports Exerc. 2006;38(1):21–26. doi: 10.1249/01.mss.0000180890.69932.15. [DOI] [PubMed] [Google Scholar]
- 34.Downar JM, Sauers EL. Clinical measures of shoulder mobility in the professional baseball player. J Athl Train. 2005;40(1):23–29. [PMC free article] [PubMed] [Google Scholar]
- 35.Riddle DL, Rothstein JM, Lamb RL. Goniometric reliability in a clinical setting: shoulder measurements. Phys Ther. 1987;67(5):668–673. doi: 10.1093/ptj/67.5.668. [DOI] [PubMed] [Google Scholar]
- 36.Thomas SJ, Swanik KA, Swanik CB, Kelly JD. Internal rotation and scapular position differences: a comparison of collegiate and high school baseball players. J Athl Train. 2010;45(1):44–50. doi: 10.4085/1062-6050-45.1.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lunden JB, Muffenbier M, Giveans MR, Cieminski CJ. Reliability of shoulder internal rotation passive range of motion measurements in the supine versus sidelying position. J Orthop Sports Phys Ther. 2010;40(9):589–594. doi: 10.2519/jospt.2010.3197. [DOI] [PubMed] [Google Scholar]
- 38.Tyler TF, Roy T, Nicholas SJ, Gleim GW. Reliability and validity of a new method of measuring posterior shoulder tightness. J Orthop Sports Phys Ther. 1999;29(5):262–274. doi: 10.2519/jospt.1999.29.5.262. [DOI] [PubMed] [Google Scholar]


