Abstract
Context:
A cornerstone of the recent consensus statements on concussion is a multifaceted concussion-assessment program at baseline and postinjury and when tracking recovery. Earlier studies of athletic trainers' (ATs') practice patterns found limited use of multifaceted protocols; however, these authors typically grouped diverse athletic training settings together.
Objective:
To (1) describe the concussion-management practice patterns of National Collegiate Athletic Association (NCAA) Division I ATs, (2) compare these practice patterns to earlier studies, and (3) objectively characterize the clinical examination.
Design:
Cross-sectional study.
Setting:
Online survey.
Patients or Other Participants:
A total of 610 ATs from NCAA Division I institutions, for a response rate of 34.4%.
Main Outcome Measure(s):
The survey had 3 subsections: demographic questions related to the participant's experiences, concussion-assessment practice patterns, and concussion-recovery and return-to-participation practice patterns. Specific practice-pattern questions addressed balance, cognitive and mental status, neuropsychological testing, and self-reported symptoms. Finally, specific components of the clinical examination were examined.
Results:
We identified high rates of multifaceted assessments (ie, assessments using at least 3 techniques) during testing at baseline (71.2%), acute concussion assessment (79.2%), and return to participation (66.9%). The specific techniques used are provided along with their adherence with evidence-based practice findings. Respondents endorsed a diverse array of clinical examination techniques that often overlapped objective concussion-assessment protocols or were likely used to rule out associated potential conditions. Respondents were cognizant of the Third International Consensus Statement, the National Athletic Trainers' Association position statement, and the revised NCAA Sports Medicine Handbook recommendations.
Conclusions:
Athletic trainers in NCAA Division I demonstrated widespread use of multifaceted concussion-assessment techniques and appeared compliant with recent consensus statements and the NCAA Sports Medicine Handbook.
Key Words: baseline testing, head injuries, return to participation
Key Points
Certified athletic trainers were using a multifaceted concussion-assessment protocol for baseline, acute injury assessment, and return-to-participation testing.
The use of standardized concussion-assessment techniques has increased considerably in the last decade.
Certified athletic trainers are largely compliant with National Collegiate Athletic Association concussion-management protocols and recent position statements.
Recent years have seen the topic of sport-related concussions move beyond the traditional sports medicine community of peer-reviewed research and conference presentations to permeate the popular press with newspaper and magazine stories, television specials, and Internet Web site and social-media features. As of April 2013, this increased media attention culminated in 47 states, the District of Columbia, and the city of Chicago having passed legislation regulating sport-related concussion management.1 This media attention has likely arisen in response to the recent findings suggesting possible connections between concussions and both acute (eg, second-impact syndrome) and later-life conditions (eg, chronic traumatic encephalopathy).2,3 Indeed, several high-profile suicides of former professional football players and the resulting Congressional hearings have heightened the awareness and concerns associated with sport-related concussions.4,5 In April 2010, the National Collegiate Athletic Association (NCAA) revised its Sports Medicine Handbook with both new requirements and recommended best practices in concussion management.6 These recommendations are largely derived from the Third International Consensus Statement on Concussion in Sports (Third CIS)7 and the National Athletic Trainers' Association (NATA) position statement on concussions.8
The cornerstone of the consensus statements and the revised NCAA policy is the need for a multifaceted baseline and postinjury protocol including measures of an individual's (1) balance, (2) cognitive and mental status, and (3) neuropsychological performance, as well as the individual's (4) self-reported symptoms.7,8 Although a multifaceted approach has sensitivity rates approaching 96% for the acute recognition of a concussion, the sensitivity of any 1 domain has failed to exceed 70%.9,10 Thus, the lack of a multifaceted assessment, either during acute recognition or when tracking recovery, may result in inappropriate concussion management, including (1) the failure to identify the presence of a concussion; (2) premature postconcussion return to participation, potentially exposing the individual to a substantially elevated risk of repeat concussion, which is likely to be more severe and have prolonged symptoms; and (3) the potential for the rare, but often fatal, second-impact syndrome.11,12 The earliest study13 on athletic trainers' (ATs') concussion-management practice patterns, from 1999 (published in 2001), indicated limited use of objective techniques. By 2004, the use of objective techniques had increased, but only 3% of respondents performed 3 components of the multifaceted concussion-assessment protocol.14 Finally, the most recent studies15,16 showed a continued increase in objective assessment techniques; however, awareness of the international consensus statement was limited. Furthermore, the most commonly used tool in evaluating a concussion and determining recovery has consistently been the clinical examination, yet the specifics of this assessment technique have not been established.13–16
The releases of the Third CIS and the updated NCAA concussion-specific guidelines in the Sports Medicine Handbook have provided a framework for appropriate concussion management for sports medicine clinicians in NCAA settings. Over the last decade, ATs have gradually increased their use of a multifaceted concussion-management approach; however, these studies were conducted across diverse employment settings; generally did not differentiate among baseline, acute evaluation, and recovery for testing protocols; and occurred before the Third CIS and new NCAA guidelines. Therefore, the purpose of our study was threefold: (1) to identify the current concussion-management practice patterns among a relatively homogeneous population of ATs—those employed at NCAA Division I institutions, (2) to compare the current practice patterns with previous investigations over the last decade to identify changes, and (3) to objectively describe the clinical examination used by ATs. We selected National Collegiate Athletic Association Division I ATs because of the public availability of their contact information and their perceived access to appropriate resources for concussion management. We hypothesized that use of a multifaceted approach to concussion management by NCAA Division I ATs would be widespread and that use of this approach would have increased since previous practice-pattern studies were conducted.
METHODS
Participants
To identify all NCAA Division I ATs, we viewed the intercollegiate athletics Web site of each of the 335 institutions classified as Division I in the 2010–2011 academic year.17 There were 120 institutions classified as Division I–Football Bowl Subdivision and 118 institutions classified as Division I–Football Championship Subdivision; the remaining 97 institutions were classified as Division I–do not sponsor football.17 The inclusion criteria were being classified as a full-time certified or licensed AT who provided athletic training services to the institution's intercollegiate athletics program and had a publicly available e-mail address. Potential participants were excluded if they were classified as part time, interns, or graduate assistant ATs; if the individual was not certified or licensed as an AT; or if the individual was not employed by the host institution. Every effort was made to specifically identify only clinically practicing ATs and to exclude academic or research faculty members unless the intercollegiate athletics Web site indicated they also provided clinical athletic training services (eg, they were listed as being responsible for athletic training services for a specific team). From these criteria, we identified 1890 e-mail addresses. The study was approved by the institutional review board of the host institution and participants provided implied consent by actively selecting the link within the e-mail to begin the questionnaire.
Procedures
We e-mailed the 1890 potential participants in January 2011 with an invitation to participate in the study, with follow-up reminder e-mails sent 7 and 14 days after the initial e-mail. However, 116 e-mails were returned as undeliverable or invalid. The e-mail included an overview of the study, appropriate informed consent documentation, and a hyperlink to the questionnaire, which the individual could select if opting to participate in the study. If the individual agreed to participate, he or she was taken to a Web site (http://www.SurveyMonkey.com; Survey Monkey, Palo Alto, CA) to complete the questionnaire. Participants were not required to answer all questions and could exit the questionnaire at any time, but they were not provided the option of returning to an earlier page and changing an answer.
The 65-item questionnaire was developed by the lead author (K.C.K.). It was based on the previous investigations of ATs' concussion-management practice patterns and expanded those questionnaires to include detailed follow-up questions.13–16 Face and content validity were established by ATs and a neuropsychologist, who were concussion experts. Furthermore, the questionnaire was initially administered to 10 ATs to identify question and content clarity as well as ease of administration.
The questionnaire consisted of 3 sections: (1) a demographic section, excluding personal or institutional identifying information, which consisted of 13 questions related to the individual's demographics, professional experience, number of concussions assessed, and awareness of concussion consensus statements; (2) a concussion-assessment section that consisted of 31 questions on the acute evaluation of a suspected concussion; and (3) a concussion-management section that consisted of 21 questions specific to recovery and return-to-participation procedures after a concussion. Sections 2 and 3 began with questions regarding the use of general testing techniques (eg, balance testing), and the sections clearly delineated between acute assessment and recovery. Follow-up questions were then designed to ascertain the specific practice patterns of the respondent who indicated using a particular test (eg, which test was used, when the test was conducted, how often was it performed, and in what environment the test took place). These questions used the logic feature of the questionnaire; thus, not all respondents were presented with all questions in section 2 or 3 (eg, if a respondent indicated not using neuropsychological testing, he or she was not provided the follow-up questions on that specific practice pattern but was asked different, mutually exclusive follow-up questions on why he or she did not use neuropsychological testing). Many of the follow-up questions allowed the respondent to check all that apply, as more than 1 option might have been reasonable; therefore, responses may exceed 100%. Finally, respondents were permitted to skip questions, resulting in different response numbers for each question. For the questions on the clinical examination, the participant was asked to select from 22 potential evaluative procedures, derived from the literature and from responses ascertained during pilot testing, and was allowed to write in any additional responses.
Data Analysis
The responses were downloaded into a Microsoft Excel (2010 version; Microsoft Corporation, Redmond, WA) spreadsheet for analysis. We report demographic data and questionnaire responses with frequencies as well as means and standard deviations. To assess the concept of a multifaceted concussion assessment, balance, cognitive or mental status, neuropsychological testing, and symptom reporting were evaluated at each of the 3 time points of interest: baseline, acute postinjury, and return to participation. Pearson correlations were performed to identify the relationship among multifaceted assessments at each of the 3 time points. We used a linear regression to identify which independent variables (years of experience as an AT, NCAA Division I subclassification, awareness of the Third CIS, awareness of the NCAA guidelines, undergraduate athletic training program type, and number of concussions evaluated in a typical year) predicted the use of a multifaceted approach at any of the 3 time points. The clinical examination was presented as a frequency distribution of the 22 items in the questionnaire. We classified evaluation procedures, which were written in by respondents, and, if appropriate, added them to the selected options, grouped with similar write-in options, or reported independently.
RESULTS
Participant Characteristics
A total of 610 ATs responded to the 1774 valid e-mailed invitations (34.4% response rate; Table 1). The respondents had a mean of 11.7 ± 8.7 years of experience as an AT; the vast majority (92.2%; 558 of 605) had earned at least a master's degree; all 10 NATA districts were represented; the respondents reported earning a mean of 3.0 ± 3.3 continuing education units specifically related to concussion over the past 3 years; and they reported assessing a mean of 5.3 ± 3.7 concussions per year. Finally, the overwhelming majority of respondents reported being aware of the NATA position statement (453 of 478 [94.8%]), the NCAA updated concussion-management policy recommendations and requirements (430 of 457 [94.1%]), and the Third CIS (493 of 583 [84.6%]).
Table 1.
Respondent Characteristics
| Characteristic |
No./Total (%) |
| Sex | |
| Men | 335/605 (55.4) |
| Women | 270/605 (44.6) |
| Certification route | |
| CAATE/CAAHEP program | 350/595 (58.8) |
| Internship program | 151/595 (25.4) |
| Pre-CAATE/CAAHEP curriculum program | 94/595 (15.6) |
| National Collegiate Athletic Association subdivision classification | |
| Division I-A/FBS | 300/587 (51.1) |
| Division I-AA/FCS | 180/587 (30.7) |
| Division I-AAA/nonfootball | 107/587 (18.2) |
| Job titlea | |
| Assistant athletic trainer | 352/588 (59.9) |
| Head athletic trainer | 91/588 (15.5) |
| Director of sports medicine | 49/588 (8.3) |
| Associate athletic trainer | 48/588 (8.2) |
| Staff athletic trainer | 32/588 (5.4) |
| Athletic training sport responsibilitiesa,b | |
| Basketball | 195/588 (33.2) |
| Football | 179/588 (30.4) |
| Soccer | 132/588 (22.4) |
| Tennis | 91/588 (15.5) |
| Track and field | 79/588 (13.4) |
| Volleyball | 78/588 (13.3) |
| Golf | 74/588 (12.6) |
| Cross-country | 66/588 (11.2) |
| Baseball | 65/588 (11.1) |
| Softball | 62/588 (10.5) |
| Lacrosse | 44/588 (7.5) |
| Swimming/diving | 37/588 (6.3) |
| Cheerleading | 30/588 (5.1) |
| Ice hockey | 29/588 (4.9) |
| Field hockey | 23/588 (3.9) |
| Rowing | 23/588 (3.9) |
| Wrestling | 16/588 (2.70) |
| Gymnastics | 14/588 (2.4) |
| Water polo | 9/588 (1.5) |
| Fencing | 8/588 (1.4) |
Abbreviations: CAAHEP, Commission on Accreditation of Allied Health Education Programs; CAATE, Commission on Accreditation of Athletic Training Education; FBS, Football Bowl Subdivision; FCS, Football Championship Subdivision.
These questions were classified as choose all that apply and therefore the total may exceed 100%.
Respondents were asked to choose all sports they directly provided athletic training services to, but they were not asked to include sports in which they supervised graduate assistants, interns, or other staff members.
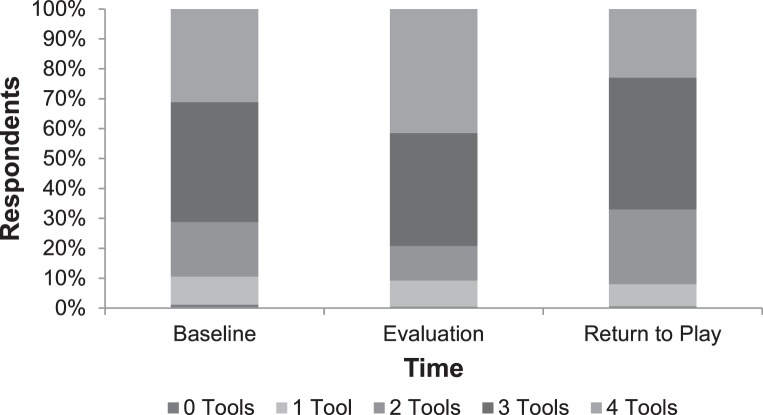
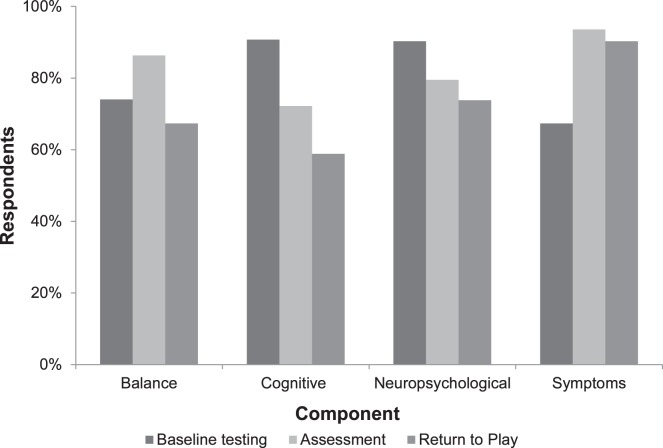
Most respondents reported using multifaceted objective assessment techniques, defined herein as at least 3 techniques, during baseline testing (71.2%), during acute concussion evaluation (79.2%), and in making return-to-participation decisions (66.9%; Figures 1 and 2). Significant positive correlations were demonstrated for the number of objective assessment techniques used between baseline and acute evaluation (r = 0.851, P < .01), baseline and return to play (r = 0.468, P < .01), and acute evaluation and return to play (r = 0.460, P < .01). We found no significant relationships between number of assessment techniques used at baseline, acute evaluation, or recovery and (1) years of experience as an AT (P = .54 for baseline, .45 for evaluation, and .07 for recovery), (2) NCAA Division I subclassification (P = .68, .33, and .36, respectively), (3) awareness of the Third CIS (P = .76, .49, and .46, respectively), (4) awareness of the NCAA guidelines (P = .65, .13, and .73, respectively), (5) undergraduate athletic training program type (P = .43, .37, and .66, respectively), and (6) number of concussions evaluated per year (P = .53, .74, and .50, respectively).
Figure 1.
Multifaceted concussion-assessment protocols. Three or more objective assessment tools were used by 71.2% of respondents at baseline, by 79.2% during the acute concussion assessment, and by 66.9% for the return-to-participation evaluation.
Figure 2.
Respondents' use of each component of the multifaceted concussion-assessment protocol at baseline, after injury, and in making return-to-participation decisions.
Baseline Testing and Assessment
The use of baseline testing for balance (74.0%), cognitive or mental status (90.7%), neuropsychological performance (90.3%), and self-reported symptoms (67.3%) was widespread among respondents (Figure 2). Most commonly, baseline testing was performed on 1 occasion, when the student–athlete entered the institution by the team's specific AT, and the results were stored in the student–athlete's medical file (Table 2).
Table 2.
Concussion-Assessment Practice Patterns, % (No./Total)a
| Assessment |
||||
| Balance |
Cognitive or Mental Status |
Neuropsychological |
Symptoms |
|
| Overall use | 74.0 (370/500) | 90.7 (496/547) | 90.0 (371/412) | 67.3 (323/480) |
| Most common baseline test | BESS, 73.9 (331/448) | SAC, 72.2 (285/395) | ImPACT, 88.8 (333/375) | N/A |
| Romberg test, 22.5 (101/448) | ||||
| When is baseline test performed? | 1× Only; S-A enters program, 71.3 (239/335) | 1× Only; S-A enters program, 71.8 (196/273) | 1× Only; S-A enters program, 80.7 (241/316) | 1× Only; S-A enters program, 76.3 (241/316) |
| Annually, 24.8 (83/335) | Annually, 20.9 (58/273) | Biennially, 10.2 (32/316) | Annually, 14.6 (46/316) | |
| Who performs baseline test? | Team-specific AT, 44.2 (146/330) | Team-specific AT, 45.7 (122/267) | N/A | N/A |
| Any available AT, 31.8 (105/330) | Any available AT, 33.3 (89/267) | |||
| Where are test results stored? | Student file, 74.9 (254/339) | Student file, 74.6 (203/272) | N/A | Student file, 60.5 (178/294) |
| Where is test performed postinjury? | Athletic training room, 58.1 (170/291) | Sidelines, 58.6 (215/367) | N/A | N/A |
| Sidelines, 44.1 (129/291) | Athletic training room, 53.7 (197/367) | |||
| When is test first performed postinjury? | Once symptom free, 60.1 (196/326) | Day 1 postinjury, 58.1 (155/267) | Once symptom free, 52.9 (182/344) | Day 1 postinjury, 94.0 (377/401) |
| Day 1 postinjury, 35.0 (114/326) | Once symptom free, 38.2 (102/267) | Day 1 postinjury, 36.3 (125/344) | Day 2 postinjury, 5.0 (20/401) | |
| How often is test performed during recovery? | Daily, 69.4 (197/284) | Daily, 72.3 (170/235) | Daily, 33.6 (86/256) | Daily, 86.7 (360/415) |
| Every other d, 16.2 (46/284) | Every other d, 16.2 (38/235) | Every other d, 30.1 (77/256) | Every other d, 6.3 (26/415) | |
Abbreviations: AT, athletic trainer; BESS, Balance Error Scoring System; ImPACT, Immediate Post-Concussion Assessment and Cognitive Testing; N/A, not applicable; S-A, student-athlete; SAC, Standardized Assessment of Concussion.
Some questions allowed respondents to select multiple responses and therefore some responses may exceed 100%.
After a suspected concussion, most respondents endorsed a multifaceted approach (Figures 1 and 2). The most commonly used balance test was the Balance Error Scoring System (BESS; 331 of 448 [73.9%]); the Sensory Organization Test (1 of 448 [0.2%]) and other computerized force-plate tests (6 of 448 [1.3%]) were rarely used. The BESS was typically performed using the original (3 stances on 2 surfaces) protocol (184 of 253 [72.7%]), was most commonly performed between 5 and 15 minutes postinjury (100 of 274 [36.5%]), and was conducted with the athlete either wearing socks (115 of 292 [39.4%]) or barefoot (104 of 292 [35.6%]). Scoring of the BESS was split between the revised version, with multiple simultaneous errors being counted as 1 error (156 of 295 [52.9%]), and the original version, with each error being counted independently (134 of 295 [45.4%]).
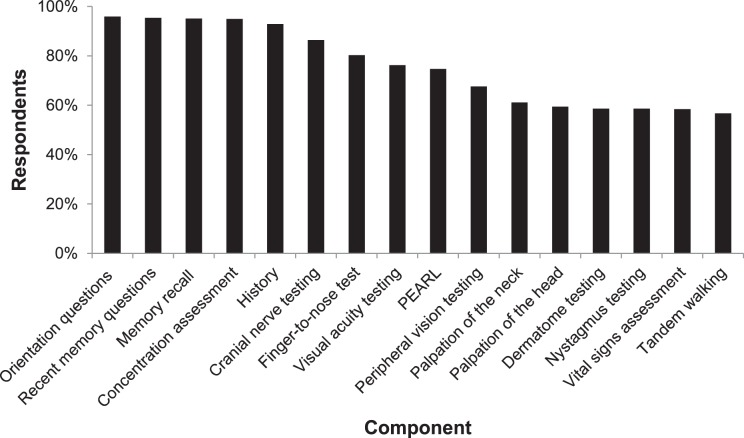
Both cognitive and mental status (496 of 547 [90.7%]) and neuropsychological (371 of 412 [90.0%]) testing was extensively endorsed by the respondents. Neuropsychological test results were most often evaluated by the team physician (244 of 383 [63.7%]) and rarely by a neuropsychologist (37 of 383 [9.7%]). Of those who did not use neuropsychological testing, the most frequently endorsed reason was insufficient funding to obtain testing materials (37 of 98 [37.8%]). The majority of respondents reported using a symptom checklist in the acute assessment of a concussion (483 of 516 [93.6%]). A minority of respondents used a concussion grading scale during an acute assessment (187 of 520 [36.0%]). Furthermore, most respondents also reported using a clinical examination as a component of acute concussion assessment (421 of 436 [96.6%]). The most commonly used components of a clinical examination were cognitive screening questions, which frequently overlapped with the Standardized Assessment of Concussion (SAC; Figure 3). The least common components of a clinical examination were reflex testing (192 of 411 [46.7%]), the serial 7 test (163 of 411 [39.7%]), brachial plexus palpation (92 of 411 [22.4%]), and the past-pointing test (43 of 411 [10.5%]).
Figure 3.
Components of the clinical examination that exceeded 50% of respondents' endorsement. Abbreviation: PEARL, pupils equal and reactive to light.
Concussion Return-to-Participation Assessment
Consistent with both baseline and acute assessment, a multifaceted concussion-assessment protocol was used to identify recovery from a concussion (Figures 1 and 2). The majority of respondents began cognitive or mental status testing, using the SAC, and symptom checklists on the first day postinjury. Conversely, both balance and neuropsychological testing began once the athlete reported being symptom free. Once initiated, most respondents indicated that each test was performed daily until the athlete achieved baseline values for the specific test (Table 2).
DISCUSSION
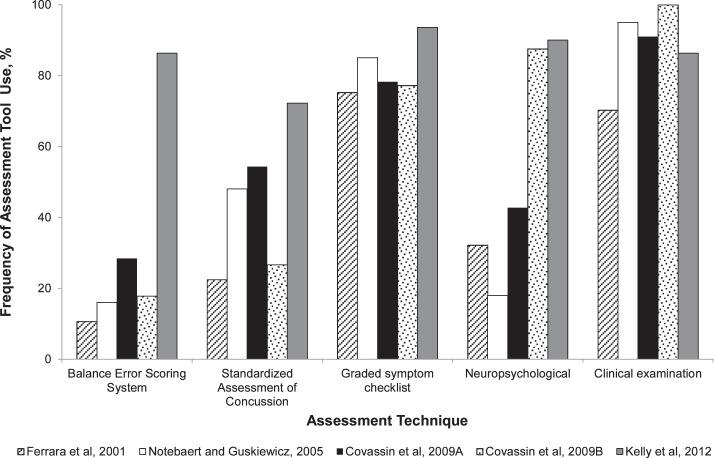
A core principle of contemporary concussion management is the use of a multifaceted approach: each component resolves independently and overreliance on any individual assessment tool may inappropriately either fail to identify the presence of a concussion or allow premature return to participation.9,10,18 Our main finding was, among NCAA Division I ATs, a substantial increase in the use of these multifaceted concussion-assessment techniques for baseline testing, as well as both acute injury identification and monitoring recovery. Indeed these respondents overwhelmingly used a multifaceted approach, with approximately 90% using at least 2 and about 70% using 3 assessment techniques. This result represents a substantial increase over the past decade in both the use of individual assessment tools and a multifaceted approach (Figure 4). Indeed, only 3% of ATs indicated using 3 objective techniques in 2004.14 Finally, we noted that fewer than 10% of respondents used only 1 assessment tool, with self-reported symptoms being the most common indicator.
Figure 4.
Historical trends of concussion-assessment techniques. Citations: Ferrara et al,13 2001; Notebaert and Guskiewicz,14 2005; Covassin et al,15 2009a; Covassin et al,16 2009b.
Previous investigations13–16 of ATs' concussion-management practice patterns focused on which tests were used, with limited attention to the policies and protocols for the testing. In our study of NCAA Division I ATs, the BESS was the most often used balance test, which is not surprising, as it is a quick and cost-effective technique that has been included in position statements despite its many limitations.7,8,19,20 One substantial limitation of the BESS is low interrater reliability (0.57), so it is encouraging that many respondents (44.2%) indicated the team-specific AT performed the baseline test.21 Two limitations of the BESS that were not incorporated include the role of fatigue and a practice effect from repeat administrations.22–24 Fatigue is known to adversely affect BESS performance for up to 20 minutes; however, the most frequent (36.5%) testing window reported herein was 5 to 15 minutes.22,24 Clearly this is a clinically challenging limitation, because waiting at least 20 minutes before performing a concussion assessment may be problematic during competitions and would likely reduce athletes' reporting of potential concussion symptoms. Additionally, repeat administration of BESS is known to improve test performance; however, most respondents (69.4%) performed the BESS test daily once the athlete was symptom free.19 Questions about an absence of improvement during repeated BESS testing and the serial administration of the BESS may deserve consideration by clinicians.19 Interestingly, the most common footwear condition for the BESS was socks (39.4%), which, to our knowledge, has never been recommended as a testing condition and should be grounds for future investigation. Finally, there have been 2 alterations to the BESS since its inception. First, the original scoring method counted each error individually, whereas the revised BESS scoring system counts simultaneous errors as a single error.7,25 The respondents in this study were largely split, with the revised method being used by 52.9%. Second, the Sport Concussion Assessment Tool 2 (SCAT2) also recommends a modified BESS test consisting of firm surfaces only; however, nearly three-fourths of respondents (72.7%) used the original method of 3 stances on 2 surfaces. Interestingly, the Sensory Organization Test, a commonly used research tool to assess postural stability that is occasionally referred to as a gold standard, was used by only 1 respondent, likely because the equipment is cost prohibitive.9,19
The SAC test was created as a brief mental status examination and was designed to be used acutely postconcussion, which differs from more sophisticated neuropsychological tests.8 However, it appears the terms cognitive, neurocognitive, and neuropsychological are used interchangeably in the concussion literature. Multiple respondents in this study referred to the SAC as a neuropsychological test and similarly referred to name-brand computerized neuropsychological tests as cognitive tests. This may be an area for additional clarification during professional presentations and publications on concussion management. The SAC test was the most often used cognitive or mental status test, likely because of its quick, simple, and cost-effective nature. A known practice effect with repeat SAC administrations occurs as early as day 2 postinjury,26 yet the majority of respondents started testing immediately postinjury and tested daily thereafter. The SAC test is most frequently administered on the sidelines, but research on environmental effects and SAC performance is limited.27
The last decade has also seen a substantial increase in the use of neuropsychological testing, from only 15.3% in 2001 to 79.5% among the NCAA Division I ATs in our study. The highest reported rate of neuropsychological testing was 87.5%; however, that study was of registered users of Immediate Post-Concussion Assessment and Cognitive Testing (ImPACT Applications, Inc, Pittsburgh, PA), and thus the rate is not surprising.16 The typical testing pattern endorsed by our respondents was performing neuropsychological testing once the athlete was symptom free (52.9%) and then testing either daily (33.6%) or every other day (30.1%) thereafter. This appears to be a change in practice patterns, as Covassin et al16 reported that neuropsychological testing was typically performed within 1 to 2 days postinjury (53.9%) and then not again until the athlete was symptom free (30.1%) or 3 to 5 days later (28.1%). The most cited reason from our respondents for not performing neuropsychological testing was insufficient funding available to obtain all materials necessary, even though most test programs cost less than $1000 annually and 2010 median revenues of NCAA Division I institutions range from 11 (nonfootball) to 48 (Football Bowl Subdivision) million dollars annually.28
The recent position and consensus statements all endorse a multifaceted approach to concussion management; however, they also agree that an appropriate clinical evaluation should be performed.7,8 Authors13–15 of previous practice-pattern studies have consistently identified clinical evaluation as 1 of the most common assessment techniques. Our findings further the earlier reports by identifying the diagnostic techniques used during a clinical concussion evaluation. As seen in Figure 3, the definition of a clinical examination varies widely, but many of the techniques overlap the objective assessment tools. For example, orientation questions was the most commonly endorsed aspect of a clinical examination and is also the first section of the SAC test, although there is clearly a wide range of potential orientation questions. Furthermore, many of the clinical examination components endorsed appropriately were tests to rule out other related conditions, such as cervical, neurologic, and facial injuries. Finally, the last decade has seen concussion management move away from the grading of concussions to focus more on the individuality of each concussion. Our results suggest the majority (333 of 530 [64.0%]) of NCAA Division I ATs do not grade concussions. In a pair of studies15,16 published in 2009, the use of grading scales by athletic trainers varied widely (22.8%–55.3%). Of the minority of respondents who do grade concussions, there was no consensus in grading scales, with no individual scale receiving more than 20% of responses.
Most NCAA Division I ATs reported high levels of awareness of both the NATA concussion-management position statement and the Third CIS. Specifically, 84.6% of respondents in this study were aware of the Third CIS, which far exceeds the 11% to 15% who were familiar with the Second CIS in a study of both athletic training academics and clinicians.15 However, ATs can become more compliant with current research findings in several areas. Both the BESS and the SAC are designed to be sideline assessment tools; yet most ATs reported storing the results of the baseline test in the athlete's medical file. Although it is not practical to bring every medical file to every event, this may be a good example of the benefit of electronic records in athletic training. In this study, 10% to 20% of respondents, depending on the specific test, indicated they had electronic access to baseline test results. When using neuropsychological testing after a concussion, clinicians must be aware of the licensure acts in their respective states as they pertain to neuropsychological testing; fewer than 10% of respondents indicated that a licensed neuropsychologist evaluated the athlete's test results—a slightly lower rate than in a previous study on neuropsychological testing practices in athletic training.8,16 Furthermore, best practices recommend not performing neuropsychological testing more than twice a week,29 yet almost two-thirds of respondents reported testing either daily or every other day once the athlete was symptom free, which raises concerns about practice or learning effects with repeated administrations. Similarly, clinicians need to be aware of the limitations associated with BESS and SAC administration to ensure appropriate use and interpretation of the tests.27,30
These results represent a focused study of a relatively homogeneous population—full-time NCAA Division I ATs—and their extrapolations to other athletic training populations are limited. Furthermore, we obtained these findings through an anonymous, Internet-based questionnaire, which presents clear limitations. Specifically, a societal response bias may be present such that the respondents gave the more socially acceptable or correct answer, which may not reflect their actual practice patterns (ie, “what I should do” as opposed to “what I actually do”). Furthermore, it was assumed that all respondents clearly understood each question and each potential answer. The questionnaire, as designed, did not differentiate among time points for assessment techniques, and we presumed that the test used as baseline was the same test used postinjury (eg, if ImPACT was reported to be the neuropsychological test used by the AT, it was presumed that ImPACT was used at baseline and acute evaluation and during recovery). Additionally, multiple respondents from the same institution are likely included in the results, which may bias the responses toward institutions with larger athletic training staffs. Furthermore, combining all NCAA Division I institutions into 1 population is a potential limitation, as staffing, resources, and budgets vary by institution. However, despite these differences, this is a more homogeneous population of ATs than studied by previous authors,13,14 who sampled across practice settings (eg, clinics, high schools, colleges, and professionals). Finally, we limited the sample to full-time ATs who provided clinical athletic training services and who had publicly available e-mail addresses, which were collected between 1 and 3 months before the administration of the questionnaire, but it is possible that institutions had not updated their Web sites with new staff or changes in titles or responsibilities. Nonetheless, our respondents totaled 610, for a response rate of 34.4%, which is consistent with the response rates of other computerized concussion-management surveys.14–16
These results suggest that NCAA Division I ATs are contemporary in their concussion-management practices, potentially because of the number of continuing education units related to concussions and their awareness of recent concussion position and consensus statements. Furthermore, the NATA and other sports medicine organizations have featured extensive concussion presentations at state, regional, and national conferences. Most ATs reported performing baseline testing and using a multifaceted approach to concussion assessment and ongoing management. As the scientific understanding of concussions and their potential long-term complications continues to develop, it is imperative that clinicians remain contemporary in their knowledge and practice patterns.
REFERENCES
- 1.Concussion legislation by state. National Football League Web site. 2013 http://www.nflevolution.com/article/Concussion-Legislation-by-State?ref=767. Updated May 2013. Accessed November 13. [Google Scholar]
- 2.Bey T, Ostick B. Second impact syndrome. West J Emerg Med. 2009;10(1):6–10. [PMC free article] [PubMed] [Google Scholar]
- 3.McKee AC, Stern RA, Nowinski CJ, et al. The spectrum of disease in chronic traumatic encephalopathy. Brain. 2013;136((pt 1)):43–64. doi: 10.1093/brain/aws307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schwartz A. Suicide reveals signs of a disease seen in NFL. New York Times. 2010 September 13. A1. [Google Scholar]
- 5.Schwartz A. Penn player's mother to testify about concussions in congressional hearing. New York Times. 2010 September 17. D5. [Google Scholar]
- 6.Klossner D. National Collegiate Athletic Association Sports Medicine Handbook, 2010–2011. Overland Park, KS: National Collegiate Athletic Association;; 2010. ed. [Google Scholar]
- 7.McCrory P, Meeuwisse W, Johnston K, et al. Consensus statement on concussion in sport: the 3rd International Conference on Concussion in Sport held in Zurich, November 2008. J Athl Train. 2009;44(4):434–448. doi: 10.4085/1062-6050-44.4.434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Guskiewicz KM, Bruce SL, Cantu RC, et al. National Athletic Trainers' Association position statement: management of sport-related concussion. J Athl Train. 2004;39(3):280–297. [PMC free article] [PubMed] [Google Scholar]
- 9.Broglio SP, Macciocchi SN, Ferrara MS. Sensitivity of the concussion assessment battery. Neurosurgery. 2007;60(6):1050–1057. doi: 10.1227/01.NEU.0000255479.90999.C0. [DOI] [PubMed] [Google Scholar]
- 10.Register-Mihalik JK, Guskiewicz KM, Mihalik JP, Schmidt JD, Kerr ZY, McCrea MA. Reliable change, sensitivity, and specificity of a multidimensional concussion assessment battery: implications for caution in clinical practice. J Head Trauma Rehabil. 2013;28(4):274–283. doi: 10.1097/HTR.0b013e3182585d37. [DOI] [PubMed] [Google Scholar]
- 11.Collins MW, Lovell MR, Iverson GL, Cantu RC, Maroon JC, Field M. Cumulative effects of concussion in high school athletes. Neurosurgery. 2002;51(5):1175–1179. doi: 10.1097/00006123-200211000-00011. [DOI] [PubMed] [Google Scholar]
- 12.Moser RS, Schatz P, Jordan BD. Prolonged effects of concussion in high school athletes. Neurosurgery. 2005;57(2):300–306. doi: 10.1227/01.neu.0000166663.98616.e4. [DOI] [PubMed] [Google Scholar]
- 13.Ferrara MS, McCrea M, Peterson CL, Guskiewicz KM. A survey of practice patterns in concussion assessment and management. J Athl Train. 2001;36(2):145–149. [PMC free article] [PubMed] [Google Scholar]
- 14.Notebaert AJ, Guskiewicz KM. Current trends in athletic training practice for concussion assessment and management. J Athl Train. 2005;40(4):320–325. [PMC free article] [PubMed] [Google Scholar]
- 15.Covassin T, Elbin R, Stiller-Ostrowski JL. Current sport-related concussion teaching and clinical practices of sports medicine professionals. J Athl Train. 2009;44(4):400–404. doi: 10.4085/1062-6050-44.4.400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Covassin T, Elbin RJ, Stiller-Ostrowski JL, Kontos AP. Immediate Post-Concussion Assessment and Cognitive Testing (ImPACT) practices of sports medicine professionals. J Athl Train. 2009;44(6):639–644. doi: 10.4085/1062-6050-44.6.639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.NCAA members by division. National Collegiate Athletic Association Web site. 2013 http://web1.ncaa.org/onlineDir/exec/divisionListing?sortOrder=0&division=1. Accessed November 13. [Google Scholar]
- 18.McCrea M, Guskiewicz KM, Marshall SW, et al. Acute effects and recovery time following concussion in collegiate football players: the NCAA Concussion Study. JAMA. 2003;290(19):2556–2563. doi: 10.1001/jama.290.19.2556. [DOI] [PubMed] [Google Scholar]
- 19.Guskiewicz KM. Balance assessment in the management of sport-related concussion. Clin Sports Med. 2011;30(1):89–102. doi: 10.1016/j.csm.2010.09.004. [DOI] [PubMed] [Google Scholar]
- 20.Burk JM, Munkasy BA, Joyner AB, Buckley TA. Balance error scoring system performance changes after a competitive athletic season. Clin J Sport Med. 2013;23(4):312–317. doi: 10.1097/JSM.0b013e318285633f. [DOI] [PubMed] [Google Scholar]
- 21.Finnoff JT, Peterson VJ, Hollman JH, Intrarater Smith J. and interrater reliability of the Balance Error Scoring System (BESS) PM R. 2009;1(1):50–54. doi: 10.1016/j.pmrj.2008.06.002. [DOI] [PubMed] [Google Scholar]
- 22.Fox ZG, Mihalik JP, Blackburn JT, Battaglini CL, Guskiewicz KM. Return of postural control to baseline after anaerobic and aerobic exercise protocols. J Athl Train. 2008;43(5):456–463. doi: 10.4085/1062-6050-43.5.456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hunt TN, Ferrara MS, Bornstein RA, Baumgartner TA. The reliability of the modified Balance Error Scoring System. Clin J Sport Med. 2009;19(6):471–475. doi: 10.1097/JSM.0b013e3181c12c7b. [DOI] [PubMed] [Google Scholar]
- 24.Wilkins JC. Valovich McLeod TC, Perrin DH, Gansneder BM. Performance on the Balance Error Scoring System decreases after fatigue. J Athl Train. 2004;39(2):156–161. [PMC free article] [PubMed] [Google Scholar]
- 25.Riemann BL, Guskiewicz KM, Shields EW. Relationship between clinical and forceplate measures of postural stability. J Sport Rehabil. 1999;8(2):71–82. [Google Scholar]
- 26.McCrea M, Kelly JP, Randolph C, Cisler R, Berger L. Immediate neurocognitive effects of concussion. Neurosurgery. 2002;50(5):1032–1040. doi: 10.1097/00006123-200205000-00017. [DOI] [PubMed] [Google Scholar]
- 27.Onate JA, Guskiewicz KM, Riemann BL, Prentice WE. A comparison of sideline versus clinical cognitive test performance in collegiate athletes. J Athl Train. 2000;35(2):155–160. [PMC free article] [PubMed] [Google Scholar]
- 28.NCAA Division I intercollegiate athletics programs report: revenues & expenses 2004–2010. National Collegiate Athletic Association Publications Web site. 2012 http://www.ncaapublications.com/p-4237-2004-2010-revenues-and-expenses.aspx. Accessed November 13. [Google Scholar]
- 29.ImPACT test—frequently asked questions. Impact Applications, Inc, Web site. 2013 http://www.impacttest.com/about/?Frequently-Asked-Questions-7. Accessed November 13. [Google Scholar]
- 30.Onate JA, Beck BC, Van Lunen BL. On-field testing environment and balance error scoring system performance during preseason screening of healthy collegiate baseball players. J Athl Train. 2007;42(4):446–451. [PMC free article] [PubMed] [Google Scholar]