Abstract
Context:
Competitive sports are recognized as having unique health benefits and risks, and the effect of sports on life-span health among elite athletes has received increasing attention. However, supporting scientific data are sparse and do not represent modern athletes.
Objective:
To assess holistic life-span health and health-related quality-of-life (HRQL) among current and former National Collegiate Athletic Association student–athletes (SAs).
Design:
Cross-sectional study.
Setting:
A large Division I university.
Patients or Other Participants:
Population-based sample of 496 university students and alumni (age 17–84 years), including SAs and an age-matched and sex-matched nonathlete (NA) control group.
Main Outcome Measure(s):
Participants completed anonymous, self-report questionnaires. We measured the Short-Form 12 (SF-12) physical and mental component HRQL scores and cumulative lifetime experience and relative risk of treatment for joint, cardiopulmonary, and psychosocial health concerns.
Results:
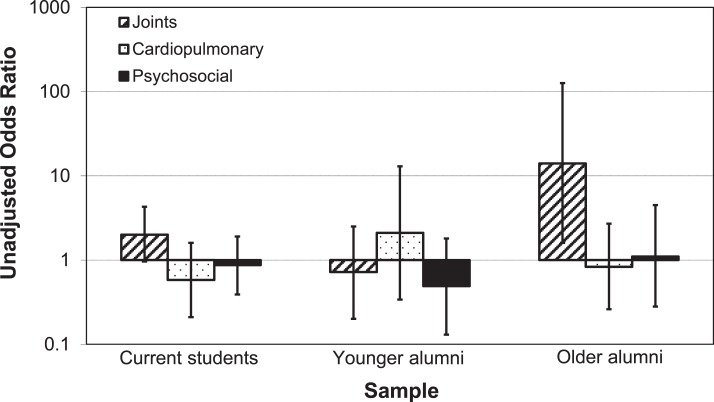
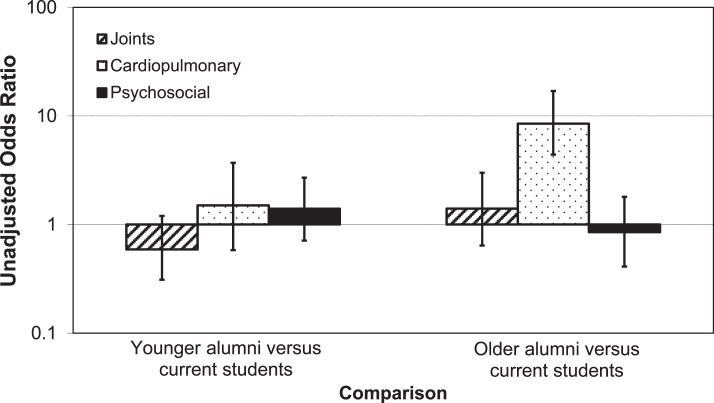
Older alumni (age 43+ years) SAs reported greater joint health concerns than NAs (larger joint summary scores; P = .04; Cohen d = 0.69; probability of clinically important difference [pCID] = 77%; treatment odds ratio [OR] = 14.0, 95% confidence interval [CI] = 1.6, 126). Joint health for current and younger alumni SAs was similar to that for NAs. Older alumni reported greater cardiopulmonary health concerns than younger alumni (summary score P < .001; d = 1.05; pCID = 85%; OR = 5.8, 95% CI = 2.0, 16) and current students (P < .001; d = 2.25; pCID >99.5%; OR = 7.1, 95% CI = 3.3, 15), but the risk was similar for SAs and NAs. Current SAs demonstrated evidence of better psychosocial health (summary score P = .006; d = −0.52; pCID = 40%) and mental component HRQL (P = .008; d = 0.50; pCID = 48%) versus NAs but similar psychosocial treatment odds (OR = 0.87, 95% CI = 0.39, 1.9). Psychosocial health and mental component HRQL were similar between alumni SAs and NAs. No differences were observed between SAs and NAs in physical component HRQL.
Conclusions:
The SAs demonstrated significant, clinically meaningful evidence of greater joint health concerns later in life, comparable cardiopulmonary health, and differences in life-span psychosocial health and HRQL profiles compared with NAs. These data provide timely evidence regarding a compelling public issue and highlight the need for further study of life-span health among modern athletes.
Key Words: athletes, quality of life, questionnaires, National Collegiate Athletic Association
Key Points
Compared with their nonathlete peers, former National Collegiate Athletic Association intercollegiate student–athletes demonstrated a greater risk for joint health concerns later in life, similar life-span cardiopulmonary health, and different age-related profiles of psychosocial health and health-related quality of life.
These findings highlight the need for additional research studies and proactive, evidence-based intervention programs addressing holistic, life-span health, and wellness outcomes among modern competitive athletes.
The life-span health of elite competitive athletes presents one of the more compelling challenges in sports medicine today. Sports stars are viewed as icons of health, are renowned for their physical prowess, and are known to possess superior cardiorespiratory fitness, strength, and power—physiologic characteristics that are positively associated with health.1,2 Conversely, competitive sports are recognized for their unique health risks. Public scrutiny of these risks, in particular orthopaedic injury,3 cardiovascular disease,4 head injury,5 and related psychosocial concerns,6 has driven a prominent public discourse. Related inquiry from the US Congress,7,8 legal action,9 and important changes to health policy10 have subsequently emerged. As a result, institutions (eg, colleges and universities) and organizations (eg, the National Collegiate Athletic Association [NCAA] and professional sports leagues) are compelled to better understand and promote athletes' health. Similarly, health professionals are increasingly challenged to provide effective, evidence-based treatment and guidance to this unique population.
Despite this attention, there are few conclusive answers. Health science and evidence-based medicine have evolved from a principal focus on diagnosis and physiologic explanation of dysfunction to a holistic paradigm embracing the shared importance of physical, mental, social, and psychological health. Yet formal scientific inquiry to date has focused largely on specific diseases and conditions in certain populations and on acute outcome measures—for instance, lower extremity osteoarthritis in soccer,11 track and field,12 and football13 athletes; cardiovascular disease in football players14–16; concussion diagnosis, mechanisms, and management17; breast cancer18; and injury surveillance.19 To date, a comprehensive, descriptive understanding of competitive sports' overall influence on athletes' lifetime health and well-being is lacking.
Data on holistic health outcomes across the life span, including mental and emotional health and health-related quality-of-life (HRQL), are sparse. The most comprehensive source is the Finnish former athlete cohort, a group of internationally competitive male athletes who represented Finland between 1920 and 1965. Using a combination of questionnaires and public medical records, authors20–26 of longitudinal studies have evaluated a diverse range of life-span health-related outcomes in this population. More recently, the National Football League (NFL) conducted a retrospective study among retired players, comparing outcomes with age-matched and race-matched normative public health data.27 An important concern about the results of these studies is their limited generalizability to diverse, modern populations of competitive athletes. The advent of highly structured, specialized, and intensive sports training over the past 50 years draws a sharp contrast between these athletes and those of the Finnish cohort.25 Although NFL players certainly provide a more contemporary sample, they do not reflect the diversity of modern athletes, most particularly the participation of women.
With more than 450 000 active participants, a figure that has increased greater than 60% over the past 20 years,28 NCAA intercollegiate sports provide one of the most diverse representations of today's elite competitive athletes. To our knowledge, no researchers to date have examined life-span health outcomes among current and former NCAA athletes alongside those of a representative control group.
Therefore, as part of a collaborative research and education program—Trojan Lifetime Champions (TLC)—we assessed holistic life-span health, exercise, and HRQL among current and former university students, including NCAA intercollegiate student–athletes (SAs). In the present study, we examined summary measures of joint, cardiopulmonary, and psychosocial health and HRQL to capture a concise, whole-person health perspective. Our objectives were to better understand the unique influence of elite competitive sports on life-span health and well-being and to provide scientific support for programs and interventions that improve health outcomes and enhance quality of life. The development and formal validation of our measurement instrument29 and exercise outcomes30 are reported separately.
METHODS
Study Design
In this cross-sectional epidemiologic study, we focused on students and alumni of the University of Southern California (USC), a large, NCAA Division I university. Current and former varsity SAs and nonathletes (NAs) completed anonymous questionnaires documenting lifetime physical, mental, and emotional health; HRQL; and exercise behaviors and attitudes. Surveys were collected between September 2008 and November 2011.
Participants
Participants consisted of a convenience sample of 2 groups: SAs and NAs. To be eligible for participation, SAs must have practiced or competed in Division I intercollegiate athletics at USC. The NAs were current and former undergraduate USC students who never practiced or competed in Division I intercollegiate athletics at any university. The NAs were excluded from participation if they indicated any experience in organized club sports during college. Those with high school or university intramural sports experience also participated.
We recruited prospective study participants with the assistance of athletic department and university records, student and alumni organizations, and personal referrals. The study population was selected to provide a representative cross-section of the USC SA source population, along with an age-matched and sex-matched control group. These procedures have been previously described in detail.29 Briefly, demographics (sex, age, and sport) of the SA source population were estimated using media guides for each varsity sport. The SA participants were targeted to proportionally match these demographic characteristics. An NA control group with comparable age and sex demographics was similarly selected. Each participant provided informed consent, and the experimental protocol was approved by the USC Health Sciences Institutional Review Board.
Data Collection
On condition of anonymity, participants completed the TLC Health Survey (TLC Survey). Details of the survey, including formal assessment of its validity and test-retest reliability, have been described previously.29 Briefly, the questionnaire consisted of basic demographic information (age, sex, ethnicity, height, and weight), history of intercollegiate sports participation, a standard HRQL measure (Short-Form 12 [SF-12], Version 2, Health Survey; QualityMetric Inc, Lincoln, RI),31 recent (previous week's) exercise behavior, perceptions of exercise and health, and a health inventory that included 59 items across 6 domains (joints; bone and muscle; cardiopulmonary; neurologic; other clinical; and psychosocial). For each item, respondents described lifetime and recent (in the past 3 years) concerns using a 4-point ordinal scale calibrated to the degree of professional treatment and the age at which they first experienced symptoms. Concerns were defined with respect to a specific body part (eg, knee) or condition (eg, high blood pressure) without discrimination of specific conditions (eg, ligament versus cartilage injury).
This investigation focused on the joint, cardiopulmonary, and psychosocial domains. Items in the joint domain were ankle, knee, hip, lower back, upper back, neck, shoulder, elbow, wrist, fingers and toes, and jaw/TMJ [temperomandibular joint]. Items in the cardiopulmonary domain were heart, cardiovascular disease; lungs, pulmonary disease; circulatory system (eg, varicose veins, blood clots in arms/legs); high blood pressure; high cholesterol and/or triglycerides; overweight, obesity; diabetes (type 1); and diabetes (type 2). Items in the psychosocial domain were relationships (eg, intimate, friendship, or family); body image; eating; binge drinking; substance use (prescription); substance use (recreational); academic and/or professional concerns; problems with concentration; anger management; adjustment (to school, work, new living situation, etc); depression; anxiety; and sports performance concerns.
Each participant completed a paper or Internet-based, electronic version of the survey, either in dedicated team or class meetings (current students) or via postal mailings (alumni). Excellent parallel form reliability (equivalence) between the paper and electronic versions of the survey has been reported.29 We took care to provide identical information to each group, including a DVD video for alumni participants that gave instructions emulating those given to current students during the in-person meetings. The same investigator (S.C.S.) provided all instructions. All current SA surveys were collected during the 2008–2009 academic year. Collection of surveys from alumni and NA current students continued through fall 2011. All participants received a $5 coffee-house gift card incentive (as approved by the Office of Athletic Compliance).
Current SAs represented all 20 varsity sports and approximately 74% (407 of 550) of the SA population. The survey response rate among recruited alumni was 79% (86 of 109), including 76% (44 of 58) of SAs and 82% (42 of 51) of NAs. Alumni responders and nonresponders were similar in age, sex, intercollegiate sports participation, and survey type (ie, paper versus electronic).29 We excluded 34 surveys containing incomplete or illegible data (27 current SAs, 6 current NA students, and 1 NA alumnus). Demographic characteristics, including age, sex, and sport distribution, were evaluated between the SA alumni source and study populations to assess external validity.
Data Analysis
We calculated descriptive statistics (mean ± standard deviation [SD] or number [percentage]) to compare demographic characteristics of SAs versus NAs. Primary independent variables included intercollegiate athletic participation (ie, SA versus NA) and age. Participants were classified into 1 of 3 age groups as follows: current students, younger alumni, or older alumni. Alumni were stratified into younger and older groups based on the median age (43 years) of all alumni participants.
Primary dependent variables were SF-12 physical component score (PCS) and mental component score (MCS) summary HRQL measures and holistic lifetime health, as indicated by TLC Survey lifetime joint, cardiopulmonary, and psychosocial domain summary scores. The SF-12 PCS and MCS scores were computed from a proprietary algorithm for summary physical and mental health.31 A score of 50 reflects the approximate population mean for all US adults; higher scores indicate better health, and lower scores indicate worse health. We calculated lifetime domain summary scores by summing individual lifetime item scores from each domain; thus, the summary scores reflect a study participant's cumulative lifetime experience with health concerns in that domain.29 A domain summary score of 0 indicates “perfect” health, and higher scores indicate greater evidence of concerns. In addition, for each domain, the lifetime prevalence of professional treatment (ie, treatment by a medical professional) for any concern was computed as a dichotomous outcome.
Before statistical analysis, we screened all data for integrity, including identification of spurious and outlier values. Spurious data included miscoded responses (eg, calendar birth year reported under Age or ambiguous descriptive text). A 2-stage outlier-screening process was used for continuous variables, including (1) visual inspection of a scatter plot and (2) assessment of statistical variance versus the group mean. Outliers were defined as data points that demonstrated apparent perturbation from combined group data via visual inspection and that deviated by more than 3 standard deviations from the mean. For categorical and ordinal variables, reported values out of the specified range were considered outliers. All spurious and outlier data were excluded from subsequent analysis.
We used a combination of traditional statistical tests and magnitude-based inferences32 to analyze the study data. For the primary analysis, stratified assessment of age and athletic participation effects on continuous dependent variables (including PCS, MCS, and TLC domain summary scores) was conducted using independent-samples t tests, and magnitude-based methods that included probabilistic interpretation of effects relative to a priori threshold values of substantial clinical meaning.32,33 Threshold values were as follows: TLC domain scores, 2 units, corresponding to a single health concern in that domain requiring medical treatment or 2 subclinical concerns; SF-12 HRQL summary scores, 5 units, corresponding to a minimal clinically important difference suggested by the previous literature, using a standardized effect-size benchmark of 0.50.34 The TLC Survey has demonstrated adequate precision to detect effects of this magnitude.29 A significance level of α = .05 was used for the traditional statistical tests. Probabilistic interpretation of magnitude-based tests used the following scale, based on the guidelines of Hopkins et al32: <0.5%, most unlikely; 0.5%–5%, very unlikely; 5%–25%, unlikely; 25%–75%, possibly; 75%–95%, likely; 95%–99.5%, very likely; and >99.5%, most likely.
In the secondary analysis, we evaluated estimates of relative risk for professional treatment of joint, cardiopulmonary, and psychosocial health concerns using unconditional logistic regression (odds ratios with 95% confidence intervals). Again, these assessments were stratified across the primary independent variables. The Tarone test of homogeneity was used to assess the validity of Mantel-Haenszel common odds ratios across strata. Common odds are reported when the Tarone test indicated homogeneity (P > .05), and crude odds are reported when homogeneity was not established.
Potential confounding variables sex, ethnicity, height, body mass, and body mass index (BMI) were evaluated as potential analysis covariates. Sex and ethnicity were excluded due to the small sample sizes (n < 10) in selected combinations of the independent variables. We assessed each potential covariate according to criteria for confounding35 and assumptions of the analysis of covariance (ANCOVA) model (eg, homogeneity of variance and regression). Body mass met confounding criteria for both SF-12 PCS and psychosocial domain summary scores. However, its inclusion in a multivariate ANCOVA model with athletic participation and age resulted in minimal changes in group means relative to the unadjusted model (effect size ∼0.1 [Cohen d]; ∼10% of threshold values of clinical meaning). Similarly, covariate analysis was conducted on the relative treatment risk assessments. We recoded height, body mass, and BMI into tertiles and then assessed their relationships with the dichotomous outcomes. Height met confounding criteria for psychosocial health treatment but again demonstrated a minimum effect (change in odds ratio ∼0.1). Unadjusted values are therefore reported throughout.
Statistical analyses were conducted using SPSS (version 16; SPSS Inc, Chicago, IL), Intercooled STATA (version 10; StataCorp, College Station, TX), and Hopkins's spreadsheet for magnitude-based inferences.33
RESULTS
Age and sex distributions were similar between the SA alumni source and study populations (independent-samples t test and χ2 proportion test P > .05). Sport distribution differed between the source and study populations (χ2 proportion test P < .001). Specifically, the study population overrepresented athletes in women's basketball, rowing, and volleyball and in men's golf, swimming and diving, tennis, and volleyball. It underrepresented athletes in men's basketball, football, and track and field and in women's cross-country, track and field, and water polo (Table 1).
Table 1.
Demographic Characteristics of Alumni Participants in the Trojan Lifetime Champions Study, 2010–2011, Compared With the University of Southern California Varsity Student–Athlete Alumni Source Population
| Variable |
Student–Athlete Source Population |
Study Populationa |
|
| Student–Athletes |
Nonathletes |
||
| Age, y (mean ± SD) | 46.0 | 45.6 ± 16.2 | 46.2 ± 16.7 |
| Men, % | 73 | 73 | 61 |
| Women, % | 27 | 27 | 39 |
| Intercollegiate sports participation, % | |||
| Men's baseball | 8 | 7 | Not applicable |
| Men's basketball | 4 | 2c | |
| Women's basketball | 3 | 7 | |
| Women's cross country | 1 | 0 | |
| Men's football | 24 | 7c | |
| Men's golf | 2 | 7 | |
| Women's golf | 1 | 0d | |
| Women's rowing | 2 | 5 | |
| Women's soccer | 2 | 2 | |
| Men's swimming and diving | 7 | 16 | |
| Women's swimming and diving | 4 | 5 | |
| Men's tennis | 2 | 7 | |
| Women's tennis | 1 | 0d | |
| Men's track and field | 12 | 7 | |
| Women's track and field | 9 | 2 | |
| Men's volleyball | 5 | 9 | |
| Women's volleyball | 3 | 5 | |
| Men's water polo | 9 | 9 | |
| Women's water polo | 2 | 0 | |
| Men's multisport | Not applicablebNot applicableb | 2c | |
| Women's multisport | 2d | ||
Alumni participants only.
Multisport athlete proportions were not estimated in the source population.
The men's multisport athlete reported competing in basketball and football.
The women's multisport athlete reported competing in golf and tennis.
Subsequent to outlier screening, we excluded data for 4 participants from HRQL outcome analysis. Three participants were excluded from the psychosocial health domain variables.
Demographic characteristics of the study population are shown in Table 2. Among both current students and alumni, SAs were similar to NAs in age and sex distribution. The SAs were taller and heavier than the NAs but had similar BMIs. Ethnicity distribution differed between SAs and NAs, primarily because of a lower proportion of Asian and a higher proportion of white participants among the SAs.
Table 2.
Demographic Characteristics for Participants in the Trojan Lifetime Champions Study, 2008–2011a
| Characteristic |
Current Students |
Alumni |
||||
| Student–Athletes (n = 380) |
Nonathletes (n = 31) |
P Valueb |
Student–Athletes (n = 44) |
Nonathletes (n = 41) |
P Valueb |
|
| Demographics, mean ± SD | ||||||
| Age, y | 19.6 ± 1.3 | 19.8 ± 1.3 | .34 | 45.6 ± 16.2 | 46.2 ± 16.7 | .88 |
| Age range, y | 17–23 | 18–22 | 24–77 | 24–84 | ||
| Height, cm | 180.7 ± 11.2 | 169.8 ± 9.2 | <.001 | 180.8 ± 10.0 | 172.2 ± 11.3 | <.001 |
| Mass, kg | 79. ± 18.0 | 66.8 ± 12.0 | <.001 | 86.7 ± 17.1 | 75.3 ± 17.6 | .004 |
| Body mass index (mass [kg]/height [m2]) | 24.1 ± 3.5 | 23.1 ± 3.6 | .12 | 26.3 ± 4.2 | 25.1 ± 3.5 | .18 |
| Intercollegiate athletic experience, y | 1.5 ± 1.3 | Not applicable | Not applicable | 3.0 ± 1.3 | Not applicable | Not applicable |
| Sex, No. (%) | ||||||
| Men | 208 (55) | 15 (48) | .58 | 32 (73) | 25 (61) | .36 |
| Women | 171 (45) | 16 (52) | 12 (27) | 16 (39) | ||
| Ethnicity, No. (%) | ||||||
| White | 240 (64) | 12 (39) | <.001 | 38 (88) | 28 (68) | .01 |
| Black | 52 (14) | 4 (13) | 3 (7) | 2 (5) | ||
| Hispanic | 21 (6) | 5 (16) | 0 (0) | 0 (0) | ||
| Asian | 22 (6) | 8 (26) | 0 (0) | 9 (22) | ||
| Other | 42 (11) | 2 (7) | 2 (5) | 2 (5) | ||
Because of rounding, percentages may not total 100. Four student–athletes responded “prefer not to answer” to the question about ethnicity. One student–athlete did not provide sex data.
P values are from independent-samples t tests for age, height, mass, and body mass index and χ2 proportion tests for sex and ethnicity.
Outcome measures and stratified assessment of age and athletic participation effects for the dependent variables are summarized in Tables 3 through 5 and Figures 1 and 2. In general, the SF-12 PCS was similar between SAs and NAs and across the 3 age groups. Effect sizes were small, and there was little evidence of clinically relevant differences. One exception was that older alumni SAs had significantly worse SF-12 PCS scores than younger alumni SAs, and this difference was possibly (38%) clinically relevant with a moderate (−0.78) effect size. Current SAs reported better SF-12 MCS scores compared with NAs. The difference was statistically significant with a small effect size (0.50) and possible (48%) clinical relevance. Collapsed across intercollegiate athletic participation groups, older alumni reported better MCS scores than younger alumni and current students. Differences were statistically significant with small to moderate effect sizes (0.56–0.60) and possible (42%–71%) clinical relevance. Age differences were substantially stronger for NAs (moderate to large effect sizes; 84%–99% probability of clinical relevance), thereby offsetting the differences observed between current SAs and NAs.
Table 3.
Summary Outcome Statistics for Participants in the Trojan Lifetime Champions Study, 2008–2011 Extended on Next Page
| Measure |
Age Group |
||
| Current Students | |||
| Student–Athletes |
Nonathletes |
Collapsed |
|
| n | 380 | 31 | 411 |
| Men | 208 | 15 | 223 |
| Women | 171 | 16 | 187 |
| Age, y, (mean ± SD) | 19.6 ± 1.3 | 19.8 ± 1.3 | 19.6 ± 1.3 |
| Health-related quality of life: Short Form-12 outcomes, mean ± SD | |||
| Physical component score | 53.2 ± 6.9 | 55.3 ± 6.1 | 53.4 ± 6.9 |
| Mental component score | 46.7 ± 9.9 | 41.8 ± 10.5 | 46.3 ± 10.0 |
| Lifetime health outcomes, mean ± SD | |||
| Joint summary score | 4.95 ± 3.54 | 4.45 ± 3.29 | 4.91 ± 3.51 |
| Treatment prevalence | 74% | 58% | 73% |
| Cardiopulmonary summary score | 0.35 ± 0.81 | 0.84 ± 1.24 | 0.39 ± 0.86 |
| Treatment prevalence | 10% | 16% | 11% |
| Psychosocial summary score | 3.68 ± 3.55 | 5.52 ± 3.21 | 3.83 ± 3.56 |
| Treatment prevalence | 29% | 32% | 29% |
Table 5.
Summary Results for Participants in the Trojan Lifetime Champions Study, 2008–2011: Pairwise Comparison of Age Effects by Intercollegiate Athletic Participation Group Extended on Next Page
| Measure |
Student–Athletes |
||
| YA Versus CS |
OA Versus YA |
OA Versus CS |
|
| Health-related quality of life: Short Form-12 | |||
| Physical component score | |||
| Difference in means | 3.68 | –4.44 | –0.76 |
| P valuea | .02 | .02 | .61 |
| Effect sizeb | 0.54 | –0.78 | –0.11 |
| Probability of CIDc | 21% | 38% | <0.5% |
| Mental component score | |||
| Difference in means | 2.92 | 1.88 | 4.80 |
| P valuea | .21 | .51 | .03 |
| Effect sizeb | 0.30 | 0.21 | 0.49 |
| Probability of CIDc | 18% | 13% | 46% |
| Lifetime health outcomes | |||
| Joints | |||
| Difference in mean summary score | 0.40 | 2.92 | 3.32 |
| P valuea | .63 | .02 | <.001 |
| Effect sizeb | 0.11 | 0.76 | 0.93 |
| Probability of CIDc | 3% | 78% | 95% |
| Relative risk for treatment (95% CI)d | 0.48 (0.19–1.2) | 15.8 (1.8–140) | 7.5 (0.99–56) |
| Cardiopulmonary | |||
| Difference in mean summary score | 0.65 | 2.43 | 3.08 |
| P valuea | .06e | .003e | <.001e |
| Effect sizeb | 0.76 | 0.98 | 2.81 |
| Probability of CIDc | <0.5% | 72% | >99.5% |
| Relative risk for treatment (95% CI)d | 2.1 (0.68–6.6) | 3.9 (1.0–15) | 8.3 (3.4–20) |
| Psychosocial | |||
| Difference in mean summary score | –0.06 | 0.43 | 0.37 |
| P valuea | .94 | .71 | .65 |
| Effect sizeb | –0.02 | 0.12 | 0.10 |
| Probability of CIDc | 1% | 9% | 2% |
| Relative risk for treatment (95% CI)d | 0.97 (0.37–2.6) | 0.94 (0.25–3.6) | 0.91 (0.35–2.4) |
Abbreviations: CI, confidence interval; CID, clinically important difference; CS, current students; OA, older alumni; YA, younger alumni.
P values are for 2-sided, independent-samples t tests.
Effect sizes are reported as the Cohen d.
Clinically important differences: health-related quality of life, 5 units; lifetime health outcomes, 2 units.
Unadjusted odds ratios.
Levene test for equality of variances, P < .05; t test for unequal variances is reported.
Tarone test of homogeneity, P > .05. Mantel-Haenszel common odds ratio is reported.
Tarone test of homogeneity, P < .05. Crude odds ratio is reported.
Figure 1.
Age-stratified relative risk of treatment for student–athletes versus nonathletes. Trojan Lifetime Champions study (2008–2011): Intercollegiate athletic participation effect, odds ratios. Error bars indicate 95% confidence intervals.
Figure 2.
Age-related relative risk of treatment for all participants combined. Trojan Lifetime Champions study (2008–2011): Age effect, odds ratios. Error bars indicate 95% confidence intervals.
Table 3.
Extended From Previous Page
| Age Group | |||||
| Younger Alumni |
Older Alumni |
||||
| Student–Athletes |
Nonathletes |
Collapsed |
Student–Athletes |
Nonathletes |
Collapsed |
| 21 | 20 | 41 | 23 | 21 | 44 |
| 14 | 11 | 25 | 18 | 14 | 32 |
| 7 | 9 | 16 | 5 | 7 | 12 |
| 32.8 ± 6.4 | 32.7 ± 6.9 | 32.7 ± 6.6 | 59.1 ± 12.4 | 57.4 ± 13.1 | 58.2 ± 12.6 |
| 56.9 ± 4.8 | 56.2 ± 4.6 | 56.5 ± 4.7 | 52.5 ± 6.6 | 53.3 ± 7.7 | 52.8 ± 7.1 |
| 49.6 ± 8.4 | 45.6 ± 8.3 | 47.6 ± 8.5 | 51.5 ± 9.6 | 52.9 ± 6.5 | 52.2 ± 8.2 |
| 5.35 ± 3.69 | 5.80 ± 4.32 | 5.58 ± 3.97 | 8.27 ± 4.15 | 5.25 ± 4.88 | 6.83 ± 4.71 |
| 57% | 65% | 61% | 96% | 60% | 79% |
| 1.00 ± 1.52 | 0.50 ± 0.76 | 0.76 ± 1.22 | 3.43 ± 3.19 | 3.19 ± 3.34 | 3.32 ± 3.23 |
| 19% | 10% | 15% | 48% | 52% | 50% |
| 3.62 ± 2.99 | 4.45 ± 3.65 | 4.02 ± 3.31 | 4.05 ± 4.38 | 2.65 ± 2.35 | 3.38 ± 3.59 |
| 29% | 45% | 37% | 27% | 25% | 26% |
Among current students and younger alumni, SAs and NAs reported similar joint domain summary scores and treatment prevalence for joint concerns. Older alumni SAs, however, had significantly worse scores than NAs, with a moderate effect size (0.69), likely (77%) clinical relevance, and 14 times the relative risk of professional treatment (Figure 1). Although treatment prevalence was consistent (58%–65%) across age groups of NAs, older alumni SAs reported a substantially higher rate (96%) than younger alumni SAs (57%) and current SAs (74%).
Cardiopulmonary domain scores and treatment prevalence were similar between SAs and NAs across all age strata. Although a statistically significant difference with a small effect size (−0.58) was observed among current students, this difference was most unlikely (<0.5%) to be clinically relevant. Collapsed across intercollegiate athletic participation groups, older alumni reported worse cardiopulmonary domain scores and higher treatment prevalence compared with younger alumni and current students. Effect sizes were moderate to very large (1.05 and 2.25, respectively), and likely to very likely (85% and >99.5%, respectively) to be clinically relevant. Overall, older alumni were 5.8 times as likely as younger alumni and 7.1 times as likely as current students to report professional treatment for cardiopulmonary health concerns (Figure 2).
Current SAs reported better psychosocial domain summary scores compared with NAs. The difference was statistically significant with a small effect size (−0.52) and possible (40%) clinical relevance. Older alumni SAs demonstrated evidence of worse scores versus NAs but this difference was not statistically significant (effect size, 0.40; probability of clinical relevance, 29%). Similar to findings for SF-12 MCS scores, NAs demonstrated stronger differences across the 3 age groups compared with SAs (Table 5), which offset differences between current SAs and NAs. Treatment prevalence and relative risk measures for the psychosocial domain were similar between SAs and NAs and across the 3 age groups.
Table 4.
Summary Results for Participants in the Trojan Lifetime Champions Study, 2008–2011: Age-Stratified Comparison of Intercollegiate Athletic Participation Effects
| Measure |
Intercollegiate Athletic Participation Effect, Age Stratified |
All Participants |
||
| Current Students |
Younger Alumni |
Older Alumni |
||
| Health-related quality of life: Short-Form 12 | ||||
| Physical component score | ||||
| Difference in means | –2.04 | 0.70 | –0.82 | –1.61 |
| P valuea | .12 | .65 | .71 | .07 |
| Effect sizeb | –0.30 | 0.15 | –0.12 | –0.24 |
| Probability of CIDc | 1% | <0.5% | 3% | <0.5% |
| Mental component score | ||||
| Difference in means | 4.92 | 4.00 | –1.45 | 1.09 |
| P valuea | .008 | .14 | .57 | .39 |
| Effect sizeb | 0.50 | 0.49 | –0.18 | 0.11 |
| Probability of CIDc | 48% | 35% | 8% | <0.5% |
| Lifetime health outcomes | ||||
| Joints | ||||
| Difference in mean summary score | 0.50 | –0.45 | 3.02 | 0.10 |
| P valuea | .45 | .73 | .04 | .83 |
| Effect sizeb | 0.14 | –0.11 | 0.69 | 0.03 |
| Probability of CIDc | 1% | 11% | 77% | <0.5% |
| Relative risk for treatment (95% CI)d | 2.0 (0.96–4.3) | 0.72 (0.20–2.5) | 14.0 (1.6–126) | 1.9f (1.1–3.1) |
| Cardiopulmonary | ||||
| Difference in mean summary score | –0.49 | 0.50 | 0.24 | –0.87 |
| P valuea | .04 | .19 | .81 | .002 |
| Effect sizeb | –0.58 | 0.42 | 0.08 | –0.58 |
| Probability of CIDc | <0.5% | <0.5% | 4% | <0.5% |
| Relative risk for treatment (95% CI)d | 0.58 (0.21–1.6) | 2.1 (0.34–13) | 0.83 (0.26–2.7) | 0.83e (0.41–1.7) |
| Psychosocial | ||||
| Difference in mean summary score | –1.84 | –0.83 | 1.40 | –0.71 |
| P valuea | .006 | .43 | .20 | .12 |
| Effect sizeb | –0.52 | –0.26 | 0.40 | –0.20 |
| Probability of CIDc | 40% | 13% | 29% | <0.5% |
| Relative risk for treatment (95% CI)d | 0.87 (0.39–1.9) | 0.49 (0.13–1.8) | 1.1 (0.28–4.5) | 0.80e (0.4–1.5) |
Abbreviations: CI, confidence interval; CID, clinically important difference.
P values are for 2-sided, independent-samples t tests.
Effect sizes are reported as the Cohen d.
Clinically important differences: health-related quality of life, 5 units; lifetime health outcomes, 2 units.
Unadjusted odds ratios, except where indicated.
Tarone test of homogeneity P > .05. Mantel-Haenszel common odds ratio is reported.
Tarone test of homogeneity P < .05. Crude odds ratio is reported.
Table 5.
Extended From Previous Page
| Nonathletes |
All Participants |
||||
| YA Versus CS |
OA Versus YA |
OA Versus CS |
YA Versus CS |
OA Versus YA |
OA Versus CS |
| 0.94 | –2.92 | –1.98 | 3.15 | –3.69 | –0.54 |
| .56 | .16 | .32 | .23 | .20 | .34 |
| 0.17 | –0.47 | –0.30 | 0.47 | –0.62 | –0.08 |
| 1% | 15% | 6% | 5% | 16% | <0.5% |
| 3.84 | 7.33 | 11.2 | 1.26 | 4.62 | 5.88 |
| .18 | .003e | <.001e | .45 | .02 | <.001e |
| 0.40 | 1.01 | 1.24 | 0.13 | 0.56 | 0.60 |
| 34% | 84% | 99% | 1% | 42% | 71% |
| 1.35 | –0.55 | 0.80 | 0.67 | 1.25 | 1.92 |
| .21 | .71e | .49 | .26 | .20 | .01e |
| 0.37 | –0.12 | 0.20 | 0.19 | 0.29 | 0.53 |
| 27% | 16% | 14% | 1% | 22% | 45% |
| 1.3 (0.42–4.3) | 0.81 (0.22–2.9) | 1.1 (0.35–3.4) | 0.72f (0.35–1.5) | 2.3g (0.89–6.2) | 2.3f (0.94–5.8) |
| –0.34 | 2.69 | 2.35 | 0.37 | 2.56 | 2.93 |
| .28 | .002e | .005e | .07e | <.001e | <.001e |
| –0.32 | 1.13 | 1.03 | 0.41 | 1.05 | 2.25 |
| <0.5% | 82% | 71% | <0.5% | 85% | >99.5% |
| 0.58 (0.10–3.3) | 9.9 (1.8–54) | 5.7 (1.6–21) | 1.3f (0.50–3.5) | 5.8f (2.0–16) | 7.1f (3.3–15) |
| –1.07 | –1.80 | –2.87 | 0.19 | –0.64 | –0.45 |
| .28 | .07e | .001 | .74 | .40 | .44 |
| –0.32 | –0.60 | –1.01 | 0.05 | –0.19 | –0.13 |
| 17% | 42% | 85% | <0.5% | 4% | <0.5% |
| 1.7 (0.54–5.5) | 0.41 (0.11–1.6) | 0.70 (0.20–2.5) | 1.2f (0.59–2.6) | 0.62f (0.24–1.6) | 0.83f (0.38–1.8) |
DISCUSSION
Our primary findings were that former NCAA Division I intercollegiate SAs demonstrated a substantially higher risk of joint health concerns later in life and no significant modification of age-related increases in cardiopulmonary health concerns, compared with an age-matched and sex-matched control group of university alumni. These findings are likely to be of clinical relevance. There was some evidence of better psychosocial health among current SAs compared with NAs and differential, age-related profiles of psychosocial health and HRQL.
Elevated prevalence of joint and musculoskeletal health disorders compared with reference populations has also been reported in previous studies of elite competitive athletes, including the male Finnish former elite athlete cohort,20,24,25 retired soccer11 and track and field12 athletes, and NFL players.13,27 In our sample, we observed this effect only among older (age >43 years) alumni SAs, and the treatment risk ratio (14.0, 95% confidence interval = 1.6, 126) was larger than that in earlier investigations. We also found no significant age-related differences in joint health in the control group. Our methodologic approach, which collectively assesses all causes of joint morbidity as opposed to a specific condition (eg, arthritis, ligament injury), likely results in higher overall prevalence and may in part explain these differences.
Previous authors have reported equivocal results with regard to cardiopulmonary health in former elite athletes. In general, the Finnish cohort demonstrated a lower prevalence of cardiovascular (CV) disease.25 Similarly, Lynch et al14 found lower CV risk factors, Tucker et al16 reported less fasting glucose impairment, and Weir et al27 demonstrated lower prevalences of heart attack, stroke, and diabetes in former NFL players. Metabolic syndrome,15 hypertension,16 and nonspecific heart disease,27 however, have been reported in higher relative prevalence among the same retired NFL population. We found a substantial age-related increase in cardiopulmonary health concerns that was independent of intercollegiate athletic participation. Thus, being an NCAA athlete as a young adult in itself appears to confer neither protective nor deleterious effects on life-span cardiopulmonary health. We have separately reported that alumni SAs in our sample had similar exercise behavior across the life span compared with NA controls and that higher levels of exercise significantly moderated cardiopulmonary health outcomes.30 In a compilation of earlier study data, Faulkner et al2 showed that aerobic capacity (V̇o2max) in trained distance runners remained elevated versus that of sedentary controls across the life span as long as high-intensity training was maintained. However, the V̇o2max values of elite runners regressed to sedentary levels with detraining. It therefore appears that lifestyle and exercise behaviors after retirement from competitive sport are key determinants of long-term cardiopulmonary health.
Although SAs in our sample reported similar psychosocial summary scores across all age strata, NA alumni had better scores with increasing age. This effectively offset the worse scores observed among current NA students relative to current SAs. Lower lifetime prevalence of psychosocial concerns with increasing age in a cross-sectional study suggests the possibility of a cohort effect. Lacking evidence of a differential bias between SAs and NAs, however, it is reasonable to speculate that the differences in age-related profiles observed between SAs and NAs are valid. Similarly, though differential reporting bias is a plausible explanation for better scores among current SAs (due for example to cultural stigmas promoting mental toughness or minimization of perceived psychological weakness), this would not explain a differential age-related response between the groups. Previous results are equivocal; some authors report less depression22 and better mental health36,37 for competitive athletes versus reference populations and others27,38 report the reverse. Sports psychology and educational development studies suggest that NCAA SAs are a distinct subpopulation facing unique psychosocial challenges compared with their peers, including academic–athletic balance, social isolation, performance expectations, and termination of their athletic careers.39–42 Therefore, SAs might develop effective psychological coping strategies in advance of their peers. Alternatively, the public attention and success enjoyed by SAs during their glory years may lead to self-criticism later in life that compromises psychosocial health. Importantly, although age-related differences among NAs demonstrated evidence of clinical relevance, the clinical relevance of differences between SAs and NAs was unclear, and we noted no differences in the prevalence of psychosocial health treatment. Additional research in this area appears warranted.
Similarly, although both SAs and NAs had better SF-12 MCS scores with increasing age, the effect was stronger for NAs. This offset better scores reported by current SAs compared with NAs. The MCS scores had a significant, moderate, negative correlation (Pearson r = −0.44) with the psychosocial summary score (data not shown). Consistency of results between the measures provides evidence of construct validity and improves confidence in these findings.
As indicated by the SF-12 PCS, physical HRQL across the life span did not differ between SAs and NAs. This finding is somewhat surprising considering the comparatively high rate of joint health concerns among older alumni SAs in our sample. Older alumni SAs had worse PCS scores and worse joint domain scores compared with younger alumni SAs. When collapsed across all groups, we observed a statistically significant association between the variables, but the correlation coefficient (Pearson r = −0.23) was small (data not shown). Despite higher rates of musculoskeletal disorders, older athletes in the Finnish cohort25 had better self-reported general health than referents. Similarly, although hip arthrosis was common in former elite javelin throwers and high jumpers,12 they reported minimal reduction in self-reported functional activities of daily living. Retired professional football players27 had lower self-rated health and reported physical injury as an important factor in retirement. Nonetheless, they still viewed their overall experience in sport favorably. It has been suggested that physical and psychological health benefits afforded by sport may mitigate the potentially deleterious effects of injury and aging.2,24 Unfortunately, associations between specific health outcomes and global measures of HRQL remain uncertain.
It is important to recognize that treatment of health concerns is not necessarily a detrimental outcome. Participants in our study rated their access to quality health care as good to great, and there were no significant differences according to age or athletic participation. Thus, although our findings suggest, for example, that older alumni SAs may require additional resources to address joint health, adequate provision of these resources could mitigate potentially deleterious effects on function and quality of life.
This study has several important limitations. Our sample was small compared with source populations of interest. The survey response rate (79%) was high,29 but we did not have adequate sample size to evaluate sex or ethnicity effects. The USC SAs are not necessarily representative of all NCAA SAs or of elite competitive athletes (eg, Olympic and professional athletes) in general. Our study sample of current SAs had a sex distribution similar to that of other NCAA Division I institutions.28 In regard to ethnicity, a somewhat greater proportion of current SAs in our sample identified themselves as Asian (6% versus 2%), Hispanic (6% versus 4%), or other (11% versus 5%), and a somewhat lower proportion identified themselves as black (14% versus 21%) compared with NCAA Division I averages.43 We are unaware of available normative demographic data for NCAA Division I SA alumni. Sport distribution differed between the source and study populations, and it is possible that sport-specific effects are present that could not be characterized by our limited sample. In this exploratory study, we performed numerous pairwise statistical tests, and some results may have occurred by chance. Although these factors limit generalizability, they support the need for follow-up studies among larger and more diverse populations.
The TLC Survey does not assess smoking or alcohol consumption, in part because of concerns about validity and compliance in administering the questionnaire to underage students. These are important potential confounders to be considered in future studies. Confounding from genetic and sociocultural selection effects, though extremely difficult to control, should also be considered.25,26 Selection bias of NAs who are more interested in health and exercise than the general population is a possibility, though this effect would likely bias results toward the null. Similarly, all self-report instruments are subject to response misclassification (eg, overreporting or underreporting), but without evidence of differential misclassification across groups, this is likely to increase overall variance and, again, bias results toward the null. Finally, our cross-sectional design provides less causative evidence than a longitudinal study; however, it allowed us to collect data in a timely and cost-efficient manner while providing valuable evidence (eg, methods, outcomes, and hypothesis generation) to support long-term studies.
Our study also had important strengths. This is the first known investigation to date of life-span health outcomes among NCAA SAs. As such, it is also the first to reflect the diversity of modern competitive athletes, including substantial representation by women. Outcomes for this population were compared against data from an age-matched and sex-matched control group of students and alumni from the same university, as opposed to normative population-based data. This design helps to isolate the influence of sports participation from potential confounding factors, including education, geography, and social or cultural values. Distinct from comparable studies to date, we used a survey instrument that has undergone formal and robust validation of its psychometric properties,29 including evaluation of error magnitude in relation to thresholds of substantial clinical meaning. Accordingly, our statistical approach included traditional methods, as well as probabilistic interpretations of clinical effect, which have been advocated as a preferred alternative to traditional hypothesis testing versus the null value.32 Finally, we simultaneously evaluated a comprehensive range of holistic health measures. This reflects a modern interpretation of health science and evidence-based medicine, embracing the shared importance of physical, mental, social, and psychological health.44 The comparable magnitude of summary scores observed across joint, cardiopulmonary, and psychosocial health domains accentuates this principle.
Given an understanding of the lifetime health benefits and challenges modern athletes are likely to face, proactive, evidence-based interventions to improve outcomes are possible. With support from athletic institutions and organizations, sports medicine professionals can design and implement wellness programs that optimize the holistic well-being of competitive athletes. The increased risk for joint health concerns, for example, suggests a need for preventive screening and treatment to reduce the effects and progression of these conditions. Similarly, it is imperative for athletes to appreciate that youthful athleticism in itself is unlikely to impart lifetime cardiopulmonary health benefits. Instead, healthy lifestyle and exercise behaviors after retirement from sport must be emphasized. The critical role of psychosocial health, HRQL, and their interdependence with physical health—particularly during an athlete's end-of-career transition—merit increased attention from sports medicine researchers and practitioners alike. Historically prevalent stigmas minimizing the recognition and treatment of psychological health must continue to be challenged. Finally, proactive efforts to improve long-term health also have the potential to improve near-term performance, for example, through prevention of injury, overtraining, or psychological burnout and via individualized strength and conditioning programs. Athletes, coaches, and sports medicine professionals should therefore question the commonly accepted notion of performance and health as fundamentally competing demands.
In conclusion, current and former NCAA Division I SAs in our study demonstrated significant, clinically meaningful evidence of greater joint health concerns, comparable cardiopulmonary health, and differences in life-span psychosocial health profiles compared with NAs and alumni. These data provide timely scientific evidence regarding a compelling public concern, offer support for related health programs and interventions, and highlight the need for additional investigation of holistic life-span health outcomes in modern competitive athletes. Larger-scale studies in diverse populations are necessary to enhance generalizability and inform subsequent, targeted mechanistic research.
ACKNOWLEDGMENTS
We thank Doyle Lee, DPT, for substantial contributions to data processing and Won (Danny) Lee, PhD, for statistical guidance.
REFERENCES
- 1.Haskell WL, Lee IM, Pate RR, et al. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Med Sci Sports Exerc. 2007;39(8):1423–1434. doi: 10.1249/mss.0b013e3180616b27. [DOI] [PubMed] [Google Scholar]
- 2.Faulkner JA, Davis CS, Mendias CL, Brooks SV. The aging of elite male athletes: age-related changes in performance and skeletal muscle structure and function. Clin J Sport Med. 2008;18(6):501–507. doi: 10.1097/JSM.0b013e3181845f1c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vecsey G. Accepting the costs of a life in football. New York Times. 2008 May 12; [Google Scholar]
- 4.Brown C. Former players dealing with lingering health issues. The New York Times. 2007 Feb 1; [Google Scholar]
- 5.Schwarz A. Dark days follow hard-hitting career in N.F.L. The New York Times. 2007 Feb 2; [Google Scholar]
- 6.Agostino J. Once an athletic star, now an unheavenly body. The New York Times. 2006 Jul 6; [Google Scholar]
- 7.Jensen M. Congressional panel hears testimony on concussions. The Philadelphia Inquirer. 2010 Sep 24; [Google Scholar]
- 8.Johnson G. NFL is focus of Senate hearing. Los Angeles Times. 2007 Sep 18; [Google Scholar]
- 9.Fendrich H. NFL Concussion saga moves to new phase: litigation. Associated Press. 2011 Oct 20; [Google Scholar]
- 10.Zarda B. Lawsuit prompts NCAA to screen athletes for sickle cell. USA Today. 2010 Jul 2; [Google Scholar]
- 11.Turner AP, Barlow JH, Heathcote-Elliott C. Long term health impact of playing professional football in the United Kingdom. Br J Sports Med. 2000;34(5):332–336. doi: 10.1136/bjsm.34.5.332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schmitt H, Brocai DR, Lukoschek M. High prevalence of hip arthrosis in former elite javelin throwers and high jumpers: 41 athletes examined more than 10 years after retirement from competitive sports. Acta Orthop Scand. 2004;75(1):34–39. doi: 10.1080/00016470410001708060. [DOI] [PubMed] [Google Scholar]
- 13.Golightly YM, Marshall SW, Callahan LF, Guskiewicz K. Early-onset arthritis in retired National Football League players. J Phys Act Health. 2009;6(5):638–643. doi: 10.1123/jpah.6.5.638. [DOI] [PubMed] [Google Scholar]
- 14.Lynch NA, Ryan AS, Evans J, Katzel LI, Goldberg AP. Older elite football players have reduced cardiac and osteoporosis risk factors. Med Sci Sports Exerc. 2007;39(7):1124–1130. doi: 10.1249/01.mss.0b013e3180557466. [DOI] [PubMed] [Google Scholar]
- 15.Miller MA, Croft LB, Belanger AR, et al. Prevalence of metabolic syndrome in retired National Football League players. Am J Cardiol. 2008;101(9):1281–1284. doi: 10.1016/j.amjcard.2007.12.029. [DOI] [PubMed] [Google Scholar]
- 16.Tucker AM, Vogel RA, Lincoln AE, et al. Prevalence of cardiovascular disease risk factors among National Football League players. JAMA. 2009;301(20):2111–2119. doi: 10.1001/jama.2009.716. [DOI] [PubMed] [Google Scholar]
- 17.Meehan WP, III, Micheli LJ. Concussion results in deficits in neurocognitive functioning. Preface. Clin Sports Med. 2011;30(1):xvii–xviii. doi: 10.1016/j.csm.2010.09.008. [DOI] [PubMed] [Google Scholar]
- 18.Wyshak G, Frisch RE. Breast cancer among former college athletes compared to non-athletes: a 15-year follow-up. Br J Cancer. 2000;82(3):726–730. doi: 10.1054/bjoc.1999.0987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hootman JM, Dick R, Agel J. Epidemiology of collegiate injuries for 15 sports: summary and recommendations for injury prevention initiatives. J Athl Train. 2007;42(2):311–319. [PMC free article] [PubMed] [Google Scholar]
- 20.Kettunen JA, Kujala UM, Kaprio J, Koskenvuo M, Sarna S. Lower-limb function among former elite male athletes. Am J Sports Med. 2001;29(1):2–8. doi: 10.1177/03635465010290010801. [DOI] [PubMed] [Google Scholar]
- 21.Backmand H, Kaprio J, Kujala U, Sarna S. Personality and mood of former elite male athletes—a descriptive study. Int J Sports Med. 2001;22(3):215–221. doi: 10.1055/s-2001-16382. [DOI] [PubMed] [Google Scholar]
- 22.Backmand H, Kaprio J, Kujala U, Sarna S. Influence of physical activity on depression and anxiety of former elite athletes. Int J Sports Med. 2003;24(8):609–619. doi: 10.1055/s-2003-43271. [DOI] [PubMed] [Google Scholar]
- 23.Backmand HM, Kaprio J, Kujala UM, Sarna S. Physical activity, mood and the functioning of daily living: a longitudinal study among former elite athletes and referents in middle and old age. Arch Gerontol Geriatr. 2009;48(1):1–9. doi: 10.1016/j.archger.2007.09.002. [DOI] [PubMed] [Google Scholar]
- 24.Kujala U, Orava S, Parkkari J, Kaprio J, Sarna S. Sports career-related musculoskeletal injuries: long-term health effects on former athletes. Sports Med. 2003;33(12):869–875. doi: 10.2165/00007256-200333120-00001. [DOI] [PubMed] [Google Scholar]
- 25.Kujala UM, Marti P, Kaprio J, Hernelahti M, Tikkanen H, Sarna S. Occurrence of chronic disease in former top-level athletes: predominance of benefits, risks or selection effects? Sports Med. 2003;33(8):553–561. doi: 10.2165/00007256-200333080-00001. [DOI] [PubMed] [Google Scholar]
- 26.Kujala UM, Sarna S, Kaprio J, Tikkanen HO, Koskenvuo M. Natural selection to sports, later physical activity habits, and coronary heart disease. Br J Sports Med. 2000;34(6):445–449. doi: 10.1136/bjsm.34.6.445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Weir DR, Jackson JS, Sonnega A. National Football League Player Care Foundation: Study of Retired NFL Players. Ann Arbor: University of Michigan;; 2009. [Google Scholar]
- 28.National Collegiate Athletic Association. 1981–82—2011–12 NCAA Sports Sponsorship and Participation Rates Report. Indianapolis, IN: 2012. [Google Scholar]
- 29.Sorenson SC, Romano R, Scholefield RM, Schroeder ET, Azen SP, Salem GJ. The Trojan Lifetime Champions health survey: development, validity, and reliability. J Athl Train. doi: 10.4085/1062-6050-50.2.10. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sorenson SC, Romano R, Azen SP, Schroeder ET, Salem GJ. Life span exercise among elite intercollegiate student athletes. Sports Health. doi: 10.1177/1941738114534813. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ware JE, Jr, Kosinski M, Turner-Bowker DM, Gandeck B. User's Manual for the SF-12v2 Health Survey With a Supplement Documenting SF-12 Health Survey. Lincoln, RI: Quality Metric Inc;; 2002. [Google Scholar]
- 32.Hopkins WG, Marshall SW, Batterham AM, Hanin J. Progressive statistics for studies in sports medicine and exercise science. Med Sci Sports Exerc. 2009;41(1):3–13. doi: 10.1249/MSS.0b013e31818cb278. [DOI] [PubMed] [Google Scholar]
- 33.Hopkins WG. A spreadsheet for deriving a confidence interval, mechanistic inference and clinical inference from a P value. Sportscience. 2007;11:16–20. [Google Scholar]
- 34.Samsa G, Edelman D, Rothman ML, Williams GR, Lipscomb J, Matchar D. Determining clinically important differences in health status measures: a general approach with illustration to the Health Utilities Index Mark II. Pharmacoeconomics. 1999;15(2):141–155. doi: 10.2165/00019053-199915020-00003. [DOI] [PubMed] [Google Scholar]
- 35.Rothman KJ. Epidemiology: An Introduction. New York, NY: Oxford;; 2002. [Google Scholar]
- 36.McAllister DR, Motamedi AR, Hame SL, Shapiro MS, Dorey FJ. Quality of life assessment in elite collegiate athletes. Am J Sports Med. 2001;29(6):806–810. doi: 10.1177/03635465010290062201. [DOI] [PubMed] [Google Scholar]
- 37.Huffman GR, Park J, Roser-Jones C, Sennett BJ, Yagnik G, Webner D. Normative SF-36 values in competing NCAA intercollegiate athletes differ from values in the general population. J Bone Joint Surg Am. 2008;90(3):471–476. doi: 10.2106/JBJS.G.00325. [DOI] [PubMed] [Google Scholar]
- 38.Watson JC, Kissinger DB. Athletic participation and wellness: implications for counseling college student-athletes. J College Counsel. 2007;10(2):153–162. [Google Scholar]
- 39.Kissinger DB, Miller MT. College Student-Athletes: Challenges, Opportunities, and Policy Implications. Charlotte, NC: Information Age Publishing;; 2009. The contemporary college student athlete as a subpopulation; pp. 1–7. In. eds. [Google Scholar]
- 40.Martin BE. Redefining championship in college sports: enhancing outcomes and increasing student-athlete engagement. In: SR Harper, Quaye SJ., editors. Student Engagement in Higher Education. New York, NY: Routledge;; 2009. pp. 283–293. In. eds. [Google Scholar]
- 41.Parham WD. The intercollegiate athlete: a 1990s profile. Counsel Psychol. 1993;21(3):411–429. [Google Scholar]
- 42.Williams DJ. An Examination of Athletic Identity, Sport Commitment, Time in Sport, Social Support, Life Satisfaction, and Holistic Wellness in College Student-Athletes [dissertation] Greensboro: The University of North Carolina at Greensboro;; 2007. [Google Scholar]
- 43.National Collegiate Athletic Association. NCAA Student-Athlete Ethnicity Report. Indianapolis, IN: 2010. [Google Scholar]
- 44.Denegar CR, Vela LI, Evans TA. Evidence-based sports medicine: outcomes instruments for active populations. Clin Sports Med. 2008;27(3):339–351. doi: 10.1016/j.csm.2008.02.002. vii. [DOI] [PubMed] [Google Scholar]