Abstract
Background and Objectives:
Meckel diverticulum can present with a variety of complications but is often found incidentally during other surgical procedures. The role of laparoscopy in the management of Meckel diverticulum is established. We reviewed our experience with complicated cases of Meckel diverticulum in children managed with laparoscopy.
Methods:
A 15-year retrospective chart review revealed 14 cases of complicated Meckel diverticulum managed with laparoscopy. Incidentally found Meckel diverticulum and cases done by laparotomy were excluded. Ages varied from 2 years to 16 years old. There were 10 males and four females. Eight cases had small bowel obstruction; of those, three had extensive intestinal gangrene. Four cases had significant rectal bleeding, three had acute diverticulitis, and two had intussusception caused by the diverticulum.
Results:
Eleven cases were treated with laparoscopic Meckel diverticulectomy and three with laparoscopic-assisted bowel resection because of extensive gangrene of the intestine. Two of the three cases with significant intestinal gangrene returned several weeks later with small bowel obstruction secondary to adhesions. They were successfully managed with laparoscopic lysis of adhesions. There were no other complications.
Conclusions:
Laparoscopy is safe and effective in the management of complicated Meckel diverticulum in children. Most cases can be managed with simple diverticulectomy. Laparoscopy is useful when the diagnosis is uncertain. When extensive gangrene is present, laparoscopy can help to mobilize the intestine and evaluate the degree of damage, irrigate and cleanse the peritoneal cavity, and minimize the incision necessary to accomplish the bowel resection.
Keywords: Meckel's diverticulum, Bowel obstruction, Bowel resection, Laparoscopy
INTRODUCTION
Meckel diverticulum is caused by an incomplete obliteration of the vitelline duct early in embryonic life, usually at around seven weeks of gestation. It is a blind-ending true diverticulum occurring in 2% to 4% of the population, making it the most common congenital malformation of the gastrointestinal tract.1 It is often discovered incidentally during surgery for other clinical disease, and it has a lifetime clinical complication rate of 4%.2 Clinical complications of Meckel diverticulum in decreasing order of likelihood include intestinal obstruction, gastrointestinal bleeding, acute intraabdominal inflammation, and umbilical anomalies.3
Given the low mortality, lifetime complication rate, and the not-so-insignificant operative morbidity associated with Meckel diverticulum, there is controversy regarding surgical resection of incidentally found Meckel diverticulum.2,4–6 However, it is widely accepted that in symptomatic cases, resection should be undertaken. Unfortunately, despite a large amount of literature on the topic, surgical treatment recommendations come mostly from single-institution case series. A recent study of national trends in the field shows that laparoscopy, though safe and feasible,7,8 is currently used much less frequently than the traditional open approach.9
The purpose of this study was to review our center's experience with laparoscopy and to reiterate that laparoscopy is a viable option, even for pediatric patients with complicated Meckel diverticulum. Laparoscopy has been shown to be equivalent to the open approach in terms of safety, and appears to decrease length of stay and cost.9 As more centers adopt the laparoscopic approach, data will be generated and can be examined to compare the laparoscopic with the open approach to determine superiority.
MATERIALS AND METHODS
The study was reviewed and approved by the New York Medical College's institutional review board. Patient consent was waived because there was minimal risk to patients and no identifying information was collected. A 15-year retrospective chart review revealed 14 cases of complicated Meckel diverticulum managed with laparoscopy of a total 36 cases of Meckel diverticulum that underwent surgical resection. Incidentally-found Meckel diverticulum and cases done by laparotomy were excluded.
There were 10 males and 4 females, with a mean age of 7 years of age ranging from 2 to 16 years old. Table 1 summarizes the patient characteristics. Preoperative diagnoses included small bowel obstruction, acute appendicitis with small bowel obstruction, bleeding Meckel diverticulum, and intussusception. Postoperative diagnoses included small bowel obstruction secondary to Meckel diverticulitis, small bowel obstruction secondary to Meckel band (Figure 1), small bowel obstruction secondary to perforated Meckel diverticulum (Figure 2), bleeding Meckel diverticulum, and intussusception with Meckel diverticulum acting as a lead point in two cases (Figure 3).
Table 1.
Patient Characteristics
| Characteristics | |
|---|---|
| Age, y | |
| Range | 2–16 |
| Sex, n | |
| Male | 10 |
| Female | 4 |
| Clinical presentation | |
| Abdominal pain | 12 |
| Abdominal distention | 10 |
| Nausea and/or vomiting | 8 |
| Lower gastrointestinal bleeding | 4 |
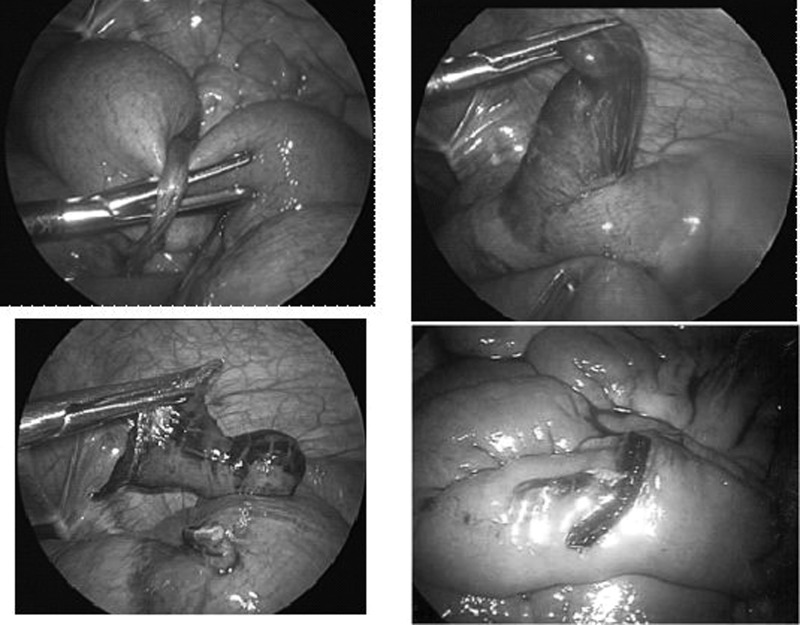
Figure 1.
Laparoscopic resection of Meckel band and diverticulum causing small bowel obstruction.
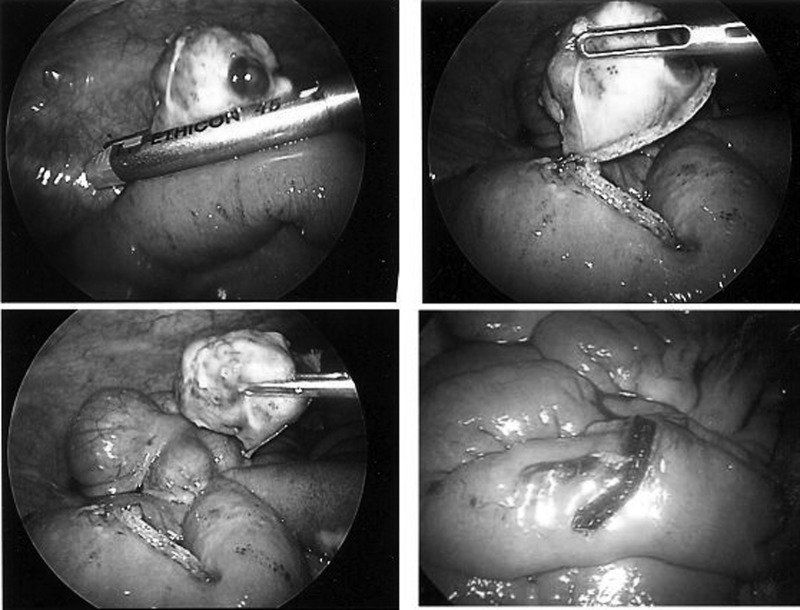
Figure 2.
Laparoscopic diverticulectomy for perforated Meckel diverticulum.
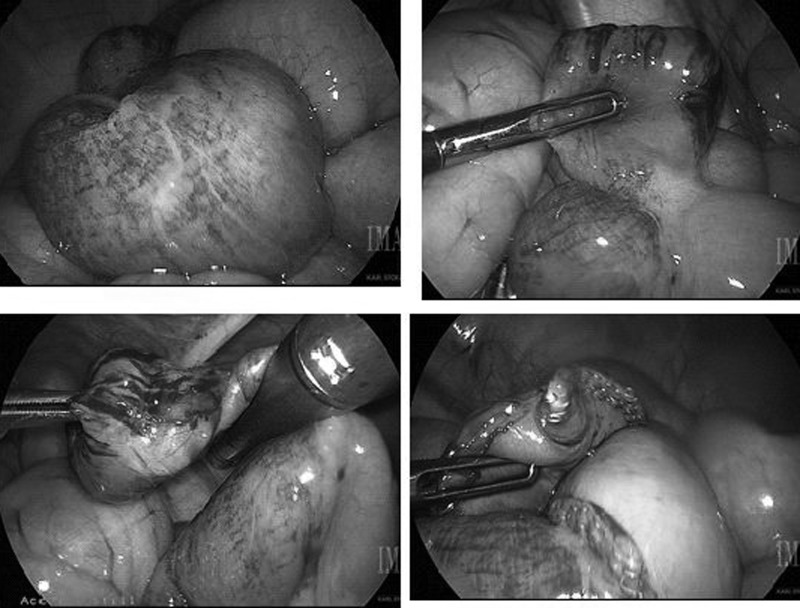
Figure 3.
Laparoscopic reduction of intussusception and resection of Meckel diverticulum.
Three patients underwent laparoscopic Meckel diverticulectomy and laparoscopic-assisted ileal resection with hand-sewn anastomosis (Figure 4).
Figure 4.

Laparoscopic assisted ileal resection with hand-sewn anastomosis.
Eight cases had small bowel obstruction; of those, three had extensive intestinal gangrene. Four cases had significant rectal bleeding, three had acute diverticulitis, and two had intussusception caused by the diverticulum. There was more than one clinical finding in each patient.
Simple laparoscopic diverticulectomy was done in 10 patients under general anesthesia using three laparoscopic ports: a 5-mm port in the umbilicus (later converted to a size 12), a 3- or 5-mm port in the left lower quadrant, and a 3- or 5-mm port in the left suprapubic region; conversion to a size 12-mm port was necessary to introduce the endoscopic stapler. One case was done through a single-incision pediatric endosurgery technique. The small bowel was run and inspected in its entirety to exclude other anomalies. The blood supply of the diverticulum was divided with the Harmonic scalpel (Ethicon, Cincinnati, Ohio) or electrosurgery (Bovie hook; Bovie Medical Corp, Clearwater, Florida). The diverticulum was removed transversely using an endoscopic surgical stapler, ensuring excision of all ectopic mucosa and retaining adequate lumen of the remaining small bowel (Figure 1). All specimens were sent to pathology for examination. For the three patients requiring small bowel resection for frank intestinal necrosis, similar initial port placement was used for lysis of adhesions, mobilization of the bowel, and identification of the Meckel diverticulum. The umbilical incision was then extended or a small right lower quadrant McBurney incision was done to achieve a laparoscopic-assisted bowel resection with hand-sewn primary anastomosis, after which the bowel could be easily and safely reduced into the abdomen, thus minimizing the size of the incision needed).
RESULTS
There were no operative or immediate postoperative complications. Two patients who underwent ileal resection for bowel necrosis presented several weeks later with small bowel obstruction secondary to adhesions, which were successfully managed with laparoscopic lysis of adhesions. Follow-up varied from 6 months to 15 years.
DISCUSSION
This study examines our experience with laparoscopy in complicated Meckel diverticulum in a pediatric population. The data from this retrospective review mimic those found in previous case series regarding the epidemiology, as well as the safety and feasibility, of laparoscopy for complicated cases.7–11 As is the case with this series, most of the published literature make recommendations based on single-institution experiences, and there is a paucity of randomized clinical trials. Our series, however, looks specifically at complicated cases of Meckel diverticulum and shows that even in these clinical presentations, laparoscopy is feasible and safe.
Laparoscopy has been shown to be equivalent to the open approach in terms of safety and appears to decrease length of stay and decrease cost.9 Although national trends have not yet been shown to reflect the safety and feasibility of laparoscopy in a complicated clinical setting,9 studies such as this one may encourage clinicians to adopt laparoscopy more consistently and for a wider selection of patients. At the very least they show the minimum nonsuperiority evidence needed to design and carry out randomized trials comparing laparoscopy with the open approach for complicated Meckel diverticulum. This study also shows that even in the setting of frank bowel necrosis, laparoscopy is a viable option, assisting in mobilization of bowel, abdominal washout, and minimization of incision size. As more centers adopt the laparoscopic approach, data will be generated and can be examined to compare the laparoscopic with the open approach, potentially preparing for a shift in management practices nationally, and improving patient experience.
In many cases, as illustrated by our data set, patients present with nonspecific preoperative diagnoses such as bowel obstruction of unknown etiology or even intussusception without a definitive diagnosis of Meckel diverticulum. In these cases, laparoscopy is especially useful because it functions as both a diagnostic and a therapeutic tool for the patient, avoiding unnecessary exploratory laparotomy.
The major limitation of our study is that it is a retrospective chart review and therefore not as robust as a prospective study would be. In addition, we did not include patients who initially started as laparoscopic cases and were converted to laparotomies in our data analysis. A comparison of these two groups may have shown factors predictive of failure of laparoscopy in complicated Meckel diverticulum.
CONCLUSION
Laparoscopy is safe and effective in the management of complicated Meckel diverticulum in children. It is useful as both a diagnostic and therapeutic modality. Most cases can be managed with simple diverticulectomy. When extensive gangrene is present, laparoscopy can help to mobilize the intestine, evaluate the degree of damage, irrigate and cleanse the peritoneal cavity, and minimize the incision necessary to accomplish the bowel resection. Further randomized clinical trials are needed to compare the laparoscopic with the open approach.
Contributor Information
Hanna Alemayehu, Department of Surgery, Westchester Medical Center, Valhalla, NY..
Gustavo Stringel, Maria Fareri Children's Hospital, Westchester Medical Center, Valhalla, NY..
Irene J. Lo, Department of Surgery, Westchester Medical Center, Valhalla, NY..
Jamie Golden, Department of Pediatric Surgery, New York Medical College, Valhalla, NY..
Samir Pandya, Department of Pediatric Surgery, New York Medical College, Valhalla, NY..
Whitney McBride, Department of Pediatric Surgery, New York Medical College, Valhalla, NY..
Oliver Muensterer, Department of Pediatric Surgery, New York Medical College, Valhalla, NY..
References:
- 1. Sagar J, Kumar V, Shah DK. Meckel's diverticulum: a systematic review. J R Soc Med. 2006;99:501–505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Zani A, Eaton S, Rees CM, Pierro A. Incidentally detected Meckel diverticulum–to resect or not to resect? Ann Surg. 2008;247:276–281 [DOI] [PubMed] [Google Scholar]
- 3. St-Vil D, Brandt ML, Panic S, et al. Meckel's diverticulum in children: a 20 year review. J Pediatr Surg. 1991;26:1289–1292 [DOI] [PubMed] [Google Scholar]
- 4. Arnold JF, Pellicane JV. Meckel's diverticulum: a ten-year experience. Am Surg. 1997;63:354–355 [PubMed] [Google Scholar]
- 5. Bani-Hani KE, Shatnawi NJ. Meckel's diverticulum: comparison of incidental and symptomatic cases. World J Surg. 2004;28:917–920 [DOI] [PubMed] [Google Scholar]
- 6. Ueberrueck T, Meyer L, Koch A, et al. The significance of Meckel's diverticulum in appendicitis–a retrospective analysis of 233 cases. World J Surg. 2005;29:455–458 [DOI] [PubMed] [Google Scholar]
- 7. Shalaby RY, Soliman SM, Fawy M, Smaha A. Laparopscopic management of Meckel's diverticulum in children. J Pediatr Surg. 2005;40:562–567 [DOI] [PubMed] [Google Scholar]
- 8. Chan KW, Lee KH, Mou JWC, et al. Laparoscopic management of complicated Meckel's diverticulum in children: a 10-year review. Surg Endosc. 2008;1509:1509–1512 [DOI] [PubMed] [Google Scholar]
- 9. Ruscher KA, Fisher JN, Hughes CD, et al. National trends in the surgical management of Meckel's diverticulum. J Pediatr Surg. 2011;46:893–896 [DOI] [PubMed] [Google Scholar]
- 10. Craigie RJ, Forrest N, Nanthakumaran S, Mahomed AA. Laparoscopy in diagnosis and management of Meckel's diverticulum. J Laparoendosc Adv Surg Tech A. 2006;16:70–73 [DOI] [PubMed] [Google Scholar]
- 11. Pepper VK, Stanfill AB, Pearl RH. Diagnosis and management of pediatric appendicitis, intussusception, and Meckel diverticulum. Surg Clin North Am. 2012;92:505–526 [DOI] [PubMed] [Google Scholar]