Abstract
Laparoscopic hernia repair is more difficult than open hernia repair. The totally extraperitoneal procedure with 3 trocars on the midline is more comfortable for the surgeon. We studied the impact of the length between the umbilicus and the pubis on the totally extraperitoneal procedure (95 hernias operated on in 70 patients). This length did not influence the totally extraperitoneal procedure in this study.
Background:
The laparoscopic repair of hernias is considered to be difficult especially for the totally extra-peritoneal technique (TEP) due to a limited working space and different appreciation of the usual anatomical landmarks seen through an anterior approach. The aim of our study has been to answer a question: does the umbilical-pubic distance, which influences the size of the mesh, affect the TEP technique used in the treatment of inguinal hernias?
Methods:
From January 2001 to May 2011, the umbilical-pubic (UP) distance was measured with a sterile ruler graduated in centimeters in all patients who underwent a symptomatic inguinal hernia by the TEP technique in two hernia surgery centers. The sex, age, BMI, hernia type, UP distance, operation time, hospital stay and complications were prospectively examined based on the medical records.
Results:
Seventy patients underwent 95 inguinal hernia repairs by the TEP technique. The umbilical-pubic distance average was 14 cm (10 to 22) and a 25 kg/m2 (16–30) average concerning the body mass index (BMI). Seventy percent of patients were treated on an outpatient basis. The postoperative course was very simple. There was no recurrence of hernia within this early postoperative period.
Conclusion:
The umbilical-pubic distance had no influence on the production of TEP with 3 trocars on the midline in this study.
Keywords: Inguinal hernia, Laparoscopy, Herniorrhaphy
INTRODUCTION
After appendectomy and right before cholecystectomy, surgical repair of hernias is the second most common surgical procedure in France and Brazil. Laparoscopy is applied for this indication in 30% of cases.1,2 It is generally believed that the learning curve for performing endoscopic inguinal hernia repair is longer than that for open repair. Laparoscopic repair of hernias is considered difficult especially with the totally extraperitoneal (TEP) technique because of a limited working space and different appreciation of the usual anatomic landmarks seen through an anterior approach.3 The risk of serious complications may be higher during the learning-curve period, and adequate patient selection and training might minimize the risks for rare but serious complications.
The aim of our study was to answer the following question: Does the umbilical-pubic (UP) distance, which influences the size of the mesh, affect the TEP technique used in the treatment of inguinal hernias?
METHODS
From January to May 2011, the UP distance was measured with a sterile ruler graduated in centimeters in all patients who underwent symptomatic inguinal hernia repair by means of the TEP technique4 in 2 hernia surgery centers (Clinique Chirurgicale Mutualiste de Saint Etienne, Saint Etienne, France, and Professor Edmundo Vasconcelos Hospital, São Paulo, Brazil).
An infraumbilical transverse incision was made to obtain extraperitoneal access. A 10-mm trocar was inserted in the subcutaneous plane in a horizontal direction and then slowly lifted up and introduced at an angle of 60° toward the sacrum. The laparoscope was introduced through the infraumbilical port for the preperitoneal dissection.
The gender, age, body mass index (BMI), hernia type, UP distance (Figure 1), operative time, length of hospital stay, and complications were prospectively examined based on the medical records. The study was conducted by senior expert surgeons using the TEP technique.5,6 The contraindications for the TEP technique in this study were as follows: the choice of the patient, patients aged <18 years, pregnant women, high–surgical risk patients (American Society of Anesthesiologists status 3 or 4), obesity (BMI >35 kg/m2), strangulated hernias, patients receiving anticoagulant treatment, large inguinal-scrotal hernias, and previous surgery in the preperitoneal space (radical prostatectomy, relapse after laparoscopic hernia repair).
Figure 1.
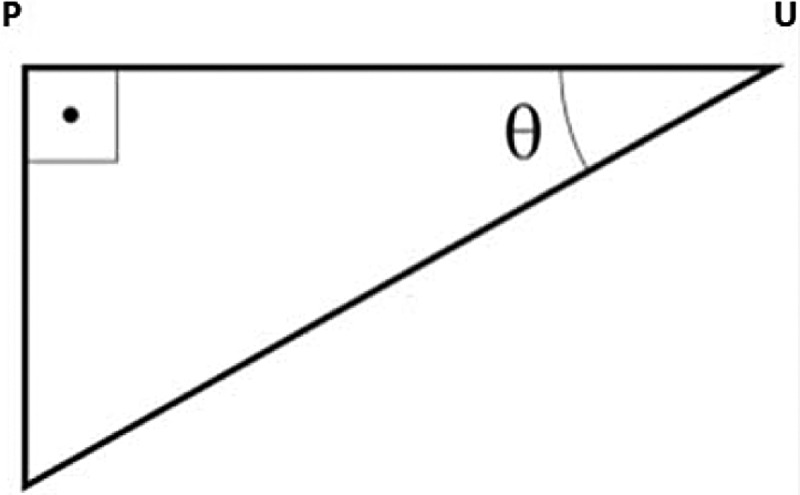
The smaller the umbilical-pubic (UP) distance, the greater the angulation during surgery.
RESULTS
Seventy patients underwent 95 inguinal hernia repairs by means of the TEP technique. There were 82 primary hernias, 13 recurrent hernias, 60 external oblique hernias, 43 direct hernias, 1 crural hernia, 16 mixed hernias, and 25 bilateral hernias. There were 67 men and 3 women. The mean age of the patients was 54 years (range, 18–79 years); the mean operative time was 44 minutes (range, 15–130 minutes), with an average time of 38 minutes per hernia.
The mean UP distance was 14 cm (range, 10 to 22 cm), and the mean BMI was 25 kg/m2 (range, 16–30 kg/m2) (Table 1).
Table 1.
Estimates of Coefficient of Linear Correlation Between BMI (Kilograms per Square Meter), UP Distance (Centimeters), and Direct and Indirect Hernia With Respect to Operating Time (Minutes)
| Bilateral |
Unilateral |
|||
|---|---|---|---|---|
| With Previous Surgery | Without Previous Surgery | With Previous Surgery | Without Previous Surgery | |
| BMIa | ||||
| rb | 0.477 | 0.398 | –0.047 | 0.236 |
| Pc | .099 | .027 | .819 | .092 |
| nd | 13 | 31 | 26 | 52 |
| UPa distance | ||||
| rb | –0.217 | 0.077 | 0.241 | 0.198 |
| Pc | .477 | .681 | .235 | .160 |
| nd | 13 | 31 | 26 | 52 |
| Direct hernia | ||||
| rb | 0.002 | –0.178 | –0.326 | –0.338 |
| Pc | .993 | .272 | .064 | .005 |
| nd | 22 | 40 | 33 | 66 |
| Indirect hernia | ||||
| rb | 0.105 | 0.225 | 0.325 | 0.215 |
| Pc | .641 | .162 | .065 | .082 |
| nd | 22 | 40 | 33 | 66 |
BMI = body mass index; UP = umbilical-pubic.
Estimate of linear correlation coefficient of Pearson.
Descriptive level.
Pairs of subjects used in estimation of linear correlation coefficient of Pearson.
There were 3 openings in the peritoneum; they were closed with an Endoloop (Ethicon, Somerville, New Jersey). There were no perioperative complications. The mean length of stay was 1 day (range, 0–3 days). Seventy percent of patients were treated on an outpatient basis. The postoperative course was very simple. The series was stopped at 70 patients because the UP distance never influenced the course of the TEP procedure. There was no recurrence of hernia within the early postoperative period.
DISCUSSION
Hernioplasty is the standard treatment for adults.1 Laparoscopy allows a physiological and anatomic treatment reinforcing the myopectineal orifice (described by Fruchaud7) by a mesh placed behind the pectineal muscle orifice in the cleavable retrofascial preperitoneal and prevesical layer described by Stoppa and colleagues.8 The TEP technique and transabdominal preperitoneal approach are effective and incorporate the principles described by Stoppa and colleagues: “the forces that were at the origin of the hernia are used to repair the hernia.” The surgeon chooses the technique with which he or she feels most at ease.3
Our standard technique is the TEP technique because we are loyal to Stoppa and colleagues8 within the classic surgical procedure. The benefits of laparoscopy compared with the inguinal approach are numerous: Laparoscopy is the only technique that can repair the wall without damaging it, which is the purpose of treatment; mesh covers all areas of weakness in the inguinal region; and the risk of postoperative chronic pain is less significant because the dissection by laparoscopy is in a plane that is different from the nerves' anatomic plane.3 Laparoscopy is used in about 30% of hernias operated on in France. It is recommended for the treatment of bilateral inguinal hernias or recurrent hernias by the French Society of Digestive Surgery.1,9 It is recommended for unilateral inguinal hernias by 2 other societies: French Society of Endoscopic Surgery and European Hernia Society.10
Laparoscopy is considered difficult and not reproducible, and this is applicable especially for the TEP technique because the workspace is more limited and the anatomy is less familiar to the surgeon.4 Our surgical technique is standardized in 4 steps: dissection in the midline, lateral dissection, hernia reduction by parietalization of the spermatic cord elements, and placement of prosthetic reinforcement.
The position of the 3 trocars on the midline improves the comfort of the surgeon while avoiding pain in the shoulder and decreasing the triangulation of instruments. In theory, this triangulation is reduced when the UP distance is smaller; therefore we studied the impact of the UP distance at each stage of TEP progress for the treatment of inguinal hernias. To our knowledge, such a study has never been previously published.
The influence of the UP distance has been studied by Stoppa and colleagues8,11 to calculate the correct size of prosthetic reinforcement. Tall patients tend to have a greater UP distance and require a larger mesh. On the basis of anatomic studies, a mesh measuring 10 × 15 cm would be sufficient for all individuals. This should be wide enough to fully cover all areas of weakness of the inguinal region and anticipate the tissue's retraction around the reinforcement, which can be up to 30% (shrinkage).12 At the same time, individuals with a shorter UP distance have less space in which to operate and accommodate smaller mesh; this may lead to difficulty in surgery. The UP distance was similar in the 2 countries in which the study was conducted (France and Brazil) and did not influence the positioning of the mesh, the size used, or the operative time. We had the impression that the shortest UP distance would entail technical difficulty, but this was not found.
Moreover, we noted that the operative time was correlated with BMI increasingly in the group of patients with bilateral surgery and no history of surgery (P = .027) and decreasingly with direct hernia in the group of patients with unilateral surgery and without previous surgery (P = .005). However, no relation to the UP distance was found.
We must take into account the skill and experience of the surgeons involved, which can minimize the results. If we had collected data from surgeons with little experience, the results may have been different.
CONCLUSION
The UP distance had no influence on the production of the TEP procedure with 3 trocars on the midline in this study.
Contributor Information
Alberto Meyer, Department of Surgery, Professor Edmundo Vasconcelos Hospital, São Paulo, Brazil..
Pierre Blanc, Clinique Chirurgicale Mutualiste de Saint Etienne, Saint Etienne, France..
Radwan Kassir, Department of Digestive Surgery, CHU Hospital, Jean Monnet University, Saint Etienne, France..
Jérôme Atger, Service de Chirurgie Générale & Digestive, CHICAS, Gap, France..
References:
- 1. Slim K. Gap between evidence-based guidelines and the daily surgical practices. World J Surg. 2010;34(7):1716–1717 [DOI] [PubMed] [Google Scholar]
- 2. Meyer AL, Berger E, Monteiro O, Jr, Alonso PA, Stavale JN, Gonçalves MP. Quantitative and qualitative analysis of collagen types in the fascia transversalis of inguinal hernia patients. Arq Gastroenterol. 2007;44(3):230–234 [DOI] [PubMed] [Google Scholar]
- 3. Kukleta JF. TAPP, the logic of hernia repair. Le Jour de Coelio-chir. 2010;76:14–20 [Google Scholar]
- 4. Meyer A, Dulucq JL, Mahajna A. Laparoscopic totally extraperitoneal hernioplasty with nonfixation of three-dimensional mesh: Dulucq's technique. Arq Bras Cir Dig. 2013;26(1):59–61 [DOI] [PubMed] [Google Scholar]
- 5. Meyer A, Dulucq JL, Mahajna A. Laparoscopic hernia repair: nonfixation mesh is feasibly? Arq Bras Cir Dig. 2013;26(1):27–30 [DOI] [PubMed] [Google Scholar]
- 6. Meyer A, Blanc P, Balique JG, et al. Laparoscopic totally extraperitoneal inguinal hernia repair: twenty-seven serious complications after 4565 consecutive operations. Rev Col Bras Cir. 2013;40(1):32–36 [DOI] [PubMed] [Google Scholar]
- 7. Read RC. Inguinofemoral herniation: evolution of repair through the anterior approach to the groin. In: Zuidema GD, ed. Surgery of the alimentary tract. 4th ed. Philadelphia: W.B. Saunders Company, 1996:108–128 [Google Scholar]
- 8. Odimba BF, Stoppa R, Laude M, Henry X, Verhaeghe P. Subparietal cleavable spaces in the abdomen [in French]. J Chir (Paris). 1980;117(11):621–627 [PubMed] [Google Scholar]
- 9. Peschaud F, Alves A, Berdah S, et al. Indications for laparoscopy in general and gastrointestinal surgery. Evidence-based recommendations of the French Society of Digestive Surgery [in French]. J Chir (Paris). 2006;143(1):15–36 [DOI] [PubMed] [Google Scholar]
- 10. Simons MP, Aufenacker T, Bay-Nielsen M, et al. European Hernia Society guidelines on the treatment of inguinal hernia in adult patients. Hernia. 2009;13(4):343–403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Stoppa R. Hernia if the abdominal wall. In: Chevrel JP, ed. Hernias and surgery of the abdominal wall. 2nd ed. Berlin, Heildelberg, New York, Tokio: Springer-Verlag; 1998:171–277 [Google Scholar]
- 12. Scheidbach H, Tamme C, Tannapfel A, Lippert H, Köckerling F. In vivo studies comparing the biocompatibility of various polypropylene meshes and their handling properties during endoscopic total extraperitoneal (TEP) patchplasty: an experimental study in pigs. Surg Endosc. 2004;18(2):211–220 [DOI] [PubMed] [Google Scholar]


