Abstract
Background and Objectives:
The goal of this study is to obtain updated surveillance statistics for hysterectomy procedures in the United States and identify factors associated with undergoing a minimally invasive approach to hysterectomy.
Methods:
A cross-sectional analysis of the 2009 United States Nationwide Inpatient Sample was performed. Subjects included all women aged 18 years or older who underwent hysterectomy of any type. Logistic regression and multivariate analyses were performed to assess the proportion of hysterectomies performed by various routes, as well as factors associated with undergoing minimally invasive surgery (laparoscopic, vaginal, or robotic).
Results:
A total of 479 814 hysterectomies were performed in the United States in 2009, 86.6% of which were performed for benign indications. Among the hysterectomies performed for benign indications, 56% were completed abdominally, 20.4% were performed laparoscopically, 18.8% were performed vaginally, and 4.5% were performed with robotic assistance. Factors associated with decreased odds of a minimally invasive hysterectomy included the following: minority race (P < .0001), fibroids (P < .0001), concomitant adnexal surgery (P < .0001), self-pay (P = .01) or Medicaid as insurer (P < .0001), and increased severity of illness (P < .0001). Factors associated with increased odds of a minimally invasive hysterectomy included the following: age >50 years (P < .0001), prolapse or menstrual disorder (P < .0001), median household income of $48 000–$62 999 (P = .007) or ≥$63 000 (P = .009), and location in the West (P = .02). A length of stay >1 day was most common in abdominal hysterectomy cases (96.1%), although total mean charges were highest for robotic cases ($38 161).
Conclusion:
The US hysterectomy incidence in 2009 decreased from prior years' reports, with an increasing frequency of laparoscopic and robotic approaches. Racial and socioeconomic factors influenced hysterectomy mode.
Keywords: Hysterectomy, Surveillance, Socioeconomic
INTRODUCTION
Hysterectomy is the most common nonobstetric surgical procedure among women. As such, it is imperative to continue evaluating trends in the performance of this procedure, including factors associated with undergoing different modes of hysterectomy. Many guidelines have been published regarding the optimal manner in which to perform hysterectomy, with both the American Congress of Obstetricians and Gynecologists and the American Association of Gynecologic Laparoscopists endorsing a minimally invasive approach whenever feasible.1,2 Although the benefits of minimally invasive hysterectomy are well documented,3 the available literature shows that the vast majority of hysterectomies in the United States are not performed in this manner.4,5 Using the 2005 Nationwide Inpatient Sample (NIS), Jacoby et al4 reported that 518 828 hysterectomies were performed for benign indications that year, 64% abdominally, 14% laparoscopically, and 22% vaginally. Prior work with the 2003 NIS also showed that most hysterectomies were performed abdominally; during that year, 538 722 hysterectomies were undertaken for benign disease, 66.1% abdominally, 11.8% laparoscopically, and 21.8% vaginally.5
Following the introduction of the robotic surgical platform for gynecologic procedures in 2005, the impact of robotic-assisted surgery has also been examined regarding its effect on the mode of access for hysterectomy. Wright et al6 queried the Perspective database (an all-payer, fee-supported database that represents approximately 15% of all the hospital discharges in the United States) to identify >200 000 benign hysterectomy cases between the years 2007 and 2010; during this time frame, the proportion of hysterectomies performed with robotic assistance increased from 0.5% to 9.5%. In this cohort the breakdown by mode of access for hysterectomy in 2010 was as follows: 40.1% abdominal, 30.5% laparoscopic, 9.5% robotic assisted, and 19.9% vaginal.
Given the evolving trends in technology and training, it is critical to maintain an understanding of factors affecting the mode of hysterectomy. The aim of this study is to use a national database to obtain updated surveillance statistics for hysterectomy procedures as of 2009 in the United States. Specific outcomes to be investigated include the proportion of hysterectomies being performed by each route (abdominal, vaginal, laparoscopic, robot assisted), as well as clinical and demographic characteristics associated with undergoing minimally invasive hysterectomy on the national level.
MATERIALS AND METHODS
The 2009 NIS was used to perform a cross-sectional analysis of all hysterectomies performed in the United States during that year.7 Managed by the Agency for Healthcare Research and Quality, the NIS is a 20% stratified random sample of discharges from all nonfederal, short-term hospitals in the United States. As such, it represents 90% of all hospitals and is the largest national all-payer database of hospital discharges. The database includes medical and demographic variables, as well as information about hospital characteristics and total charges. The 2009 dataset contains data on 7 810 762 discharges from 1050 hospitals in 44 states. This study was deemed exempt by the local institutional review board.
Patients who underwent a hysterectomy procedure of any type during their hospitalization were identified by procedure coding corresponding to International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes between 68.3 and 68.99. The hysterectomy ICD-9-CM codes were grouped as abdominal (68.39, 68.49, and 68.69), laparoscopic (68.31, 68.41, 68.51, 68.61, and 68.71), vaginal (68.59 and 68.79), or other (68.8 and 68.9). Although robotically assisted hysterectomy cases do not possess an individual procedure code, these cases were identified using ICD-9-CM codes for robotic assistance during a surgical procedure (codes 17.41–17.44 and 17.49). Of note, the vast majority of these cases (88%) were colabeled as laparoscopic hysterectomies; however, 9% of the robotic-assisted cases were also coded as abdominal procedures, with the remainder coded as vaginal or other. Although it was unclear whether the cases coded as both robotic and abdominal/vaginal procedures represented conversions or were misclassified, we chose to treat all cases coded with modifiers for robotic assistance as a separate category of hysterectomy. Key variables that were abstracted from the dataset included the following: concomitant adnexal or tubal surgery (ICD-9-CM codes 65.3, 65.31, 65.39, 65.4, 65.41, 65.49, 65.51–65.54, and 65.61–65.64); indication for surgery (fibroids [ICD-9-CM codes 218.0–218.2 and 218.9], endometriosis [Clinical Classification Software (CCS) code 169], prolapse [CCS code 170], cancer [CCS codes 25–28], or menstrual disorders [CCS code 171]); age; race; payer; median household income; region of country; urban-rural location; hospital teaching status; hospital bed size; percent of all hospital operations performed on an outpatient basis; severity of illness; comorbidity measure for obesity; length of hospital stay; and total hospital charges. Female patients were excluded if they were aged <18 years or had undergone a cesarean hysterectomy. Regions of the country were defined using US census designations as coded by the NIS.
The NIS sampling design consists of a stratified, single-stage cluster sample. Details on the sampling scheme can be found elsewhere.7 In brief, a stratified random sample of hospitals (clusters) was drawn, and all discharges were included from each selected hospital. There are 60 strata defined by region (North, South, East, West); location (urban, rural); teaching status; bed size category (small, medium, large); and ownership (public, private nonprofit, private for profit). The sample weights are provided in the NIS dataset and are calculated within each stratum as the ratio of total discharges that were eligible for sampling to discharges in the sample. Because of the sampling design, weighted analyses were carried out using the survey analysis procedures in the SAS program, version 9.2 (SAS Institute, Cary, North Carolina).
Among women who had hysterectomies for benign indications, odds ratios and 95% confidence intervals were calculated using logistic regression analyses to estimate the associations between patient and hospital characteristics and risk of minimally invasive surgery (defined as either laparoscopic, vaginal, or robotic) compared with abdominal hysterectomy. One multivariate model was run with all predictors included. Although most variables had no or only small amounts of missing data (0.3%–2% for median household income, urban-rural location, primary payer, percent of all operations performed on an outpatient basis, hospital teaching status, and bed size), the race classification was missing for 14% of the sample. To prevent variables with missing values from being dropped from analyses, we assigned missing indicators and included these indicators in the regression models. Only the odds ratio (95% confidence interval) for the race missing indicator is shown in the results.
RESULTS
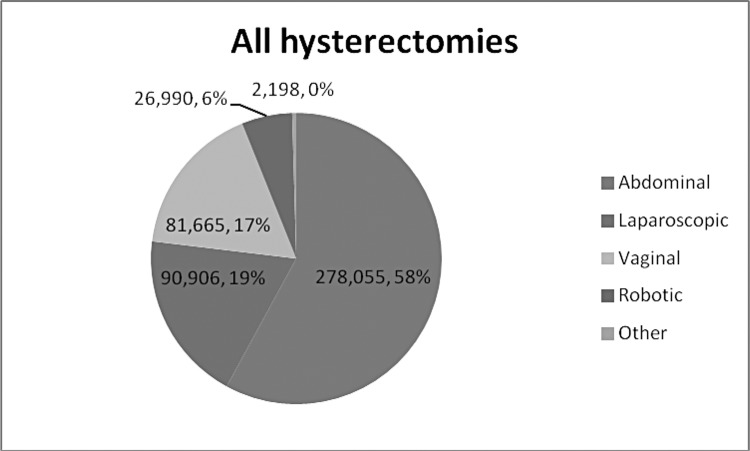
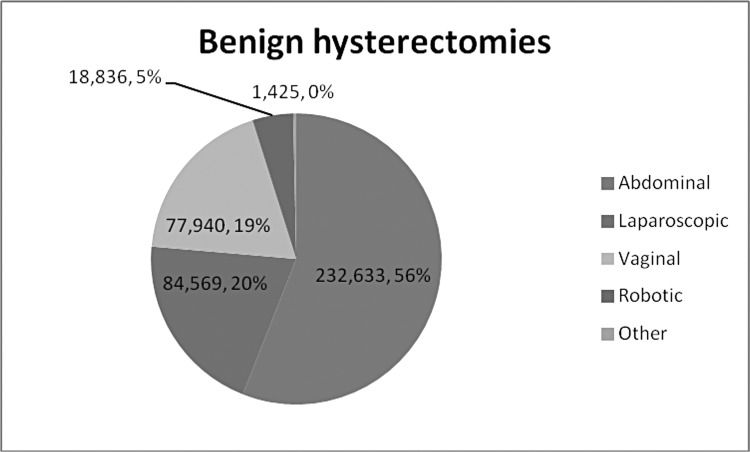
Based on analysis of the analysis of the 2009 NIS, 479 814 hysterectomies were performed in the United States that year, 415 404 (86.6%) of which were performed for benign indications. Table 1 shows the frequency of each procedure type among all hysterectomies and stratified by those performed for benign and malignant conditions. Among the benign cases, 53 430 (12.9%) were subtotal procedures in which the cervix was not removed. The relative proportions of the main modes of hysterectomy are shown for all cases and for benign cases in Figures 1 and 2. Regarding hysterectomies for benign indications, 56% were completed abdominally whereas 20.4% were performed laparoscopically, 18.8% vaginally, and 4.5% with robotic assistance. As described earlier, cases coded as including robotic assistance were considered a separate category of hysterectomy that was mutually exclusive from any other procedure type. Among all hysterectomies in 2009, 26 992 were performed with robot assistance, representing 5.6% of all hysterectomy cases.
Table 1.
Summary of All Hysterectomies in 2009
| All Hysterectomies |
Benign Hysterectomies |
Malignant Hysterectomies |
||||
|---|---|---|---|---|---|---|
| n | (%) | n | (%) | n | (%) | |
| Abdominal | ||||||
| Total abdominal hysterectomy | 240 488 | (50.1) | 201 152 | (48.4) | 39 336 | (61.1) |
| Other subtotal abdominal hysterectomy, NOSa | 32 278 | (6.7) | 30 692 | (7.4) | 1586 | (2.5) |
| Radical abdominal hysterectomy NECa/NOS | 5290 | (1.1) | 790 | (0.2) | 4500 | (7.0) |
| Vaginal | ||||||
| Other vaginal hysterectomy | 81 143 | (16.9) | 77 610 | (18.7) | 3532 | (5.5) |
| Radical vaginal hysterectomy NEC/NOS | 522 | (0.1) | 330 | (0.1) | 192 | (0.3) |
| Laparoscopic | ||||||
| Laparoscopic supracervical hysterectomy | 20 365 | (4.2) | 20 217 | (4.9) | 148 | (0.2) |
| Laparoscopic total abdominal hysterectomy | 15 414 | (3.2) | 13 226 | (3.2) | 2189 | (3.4) |
| Laparoscopic-assisted vaginal hysterectomy | 53 747 | (11.2) | 50 226 | (12.1) | 3520 | (5.5) |
| Laparoscopic radical abdominal hysterectomy | 1143 | (0.2) | 794 | (0.2) | 349 | (0.5) |
| Laparoscopic radical vaginal hysterectomy | 237 | (0.03) | 106 | (0.03) | 131 | (0.2) |
| Other | ||||||
| Other unspecified hysterectomy | 586 | (0.1) | 445 | (0.1) | 141 | (0.2) |
| Pelvic evisceration | 1612 | (0.3) | 980 | (0.2) | 632 | (1.0) |
| Roboticb | ||||||
| Total abdominal hysterectomy | 1976 | (0.4) | 1123 | (0.3) | 853 | (1.3) |
| Other subtotal abdominal hysterectomy, NOS | 273 | (0.06) | 267 | (0.1) | <10 | (0.008) |
| Radical abdominal hysterectomy NEC/NOS | 142 | (0.03) | 10 | (0.002) | 132 | (0.2) |
| Other vaginal hysterectomy | 588 | (0.01) | 429 | (0.1) | 159 | (0.2) |
| Radical vaginal hysterectomy NEC/NOS | 19 | (0.004) | <10 | (0.001) | 14 | (0.02) |
| Laparoscopic supracervical hysterectomy | 2291 | (0.5) | 2254 | (0.5) | 37 | (0.1) |
| Laparoscopic total abdominal hysterectomy | 11 767 | (2.5) | 8057 | (1.9) | 3710 | (5.8) |
| Laparoscopic-assisted vaginal hysterectomy | 7332 | (1.5) | 5602 | (1.3) | 1730 | (2.7) |
| Laparoscopic radical abdominal hysterectomy | 2048 | (0.4) | 881 | (0.2) | 1166 | (1.8) |
| Laparoscopic radical vaginal hysterectomy | 348 | (0.07) | 41 | (0.01) | 307 | (0.5) |
| Other unspecified hysterectomy | 124 | (0.03) | 89 | (0.02) | 36 | (0.1) |
| Pelvic evisceration | 84 | (0.02) | 79 | (0.02) | <10 | (0.008) |
| Total No. of hysterectomies | 479 814 | 415 404 | 64 410 | |||
NEC = Not Elsewhere Classified; NOS = Not Otherwise Specified.
Cases colabeled as robotic and another mode were treated as robotic for the purposes of analysis.
Figure 1.
Relative mode of all hysterectomies in 2009.
Figure 2.
Relative mode of benign hysterectomies in 2009.
Table 2 shows patient and hospital characteristics by mode of hysterectomy for all hysterectomies, as well as the benign-only subgroup. Concomitant adnexal surgery was performed in 52.9% of all benign hysterectomies and 57.2% of all hysterectomies, although within the vaginal hysterectomy groups, only 23% of cases were associated with adnexal procedures. Overall, fibroids and menstrual disorders were the most frequent indications for hysterectomy. Women who underwent vaginal hysterectomy were older and more likely to have a surgical indication of prolapse compared with those who underwent an alternate mode of hysterectomy. Black women and women in the lowest median income category more frequently underwent abdominal hysterectomies. Higher comorbidity and obesity classifications were seen in the women who underwent abdominal hysterectomy.
Table 2.
Patient and Hospital Characteristics by Mode of Hysterectomy
| All Hysterectomies |
Benign Hysterectomies |
|||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| All (n = 479 814) | Abdominal (n = 278 055) | Laparoscopic (n = 90 906) | Vaginal (n = 81 665) | Robotic (n = 26 990) | All (n = 415 404) | Abdominal (n = 232 633) | Laparoscopic (n = 84 569) | Vaginal (n = 77 940) | Robotic (n = 18 836) | |||||||||||
| Age [mean (SE)] (y) | 48.0 | (0.2) | 47.8 | (0.2) | 45.4 | (0.2) | 50.6 | (0.3) | 50.7 | (0.6) | 46.5 | (0.1) | 45.7 | (0.1) | 44.6 | (0.2) | 50.8 | (0.3) | 47.1 | (0.4) |
| Race/ethnicity [n (%)] | ||||||||||||||||||||
| White | 277 315 | (57.8) | 148 855 | (53.5) | 58 535 | (64.4) | 52 098 | (63.8) | 16 429 | (60.9) | 237 870 | (57.3) | 121 790 | (52.4) | 53 892 | (63.7) | 49 741 | (63.8) | 11 630 | (61.7) |
| Black | 62 657 | (13.1) | 47 791 | (17.2) | 7731 | (8.5) | 4828 | (5.9) | 2088 | (7.7) | 57 810 | (13.9) | 43 829 | (18.8) | 7460 | (8.8) | 4658 | (6.0) | 1705 | (9.1) |
| Hispanic | 44 801 | (9.3) | 27 248 | (9.8) | 7223 | (7.9) | 8277 | (10.1) | 1948 | (7.2) | 39 501 | (9.5) | 23 478 | (10.1) | 6717 | (7.9) | 7747 | (9.9) | 1474 | (7.8) |
| Asian/Pacific Islander | 10 638 | (2.2) | 7053 | (2.5) | 1580 | (1.7) | 1348 | (1.7) | 611 | (2.3) | 8802 | (2.1) | 5649 | (2.4) | 1402 | (1.7) | 1305 | (1.7) | 410 | (2.2) |
| Native American | 3744 | (0.8) | 1647 | (0.6) | 750 | (0.8) | 948 | (1.2) | 394 | (1.5) | 3132 | (0.8) | 1320 | (0.6) | 718 | (0.8) | 920 | (1.2) | 169 | (0.9) |
| Other | 12 798 | (2.7) | 8199 | (2.9) | 1760 | (1.9) | 2099 | (2.6) | 666 | (2.5) | 10 883 | (2.6) | 6779 | (2.9) | 1591 | (1.9) | 2003 | (2.6) | 466 | (2.5) |
| Missing | 67 860 | (14.1) | 37 262 | (13.4) | 13 327 | (14.7) | 12 067 | (14.8) | 4854 | (18.0) | 57 405 | (13.8) | 29 788 | (12.8) | 12 791 | (15.1) | 11 567 | (14.8) | 2982 | (15.8) |
| Indicationa [n (%)] | ||||||||||||||||||||
| Fibroids | 223 492 | (46.6) | 148 811 | (53.5) | 41 469 | (45.6) | 22 626 | (27.7) | 10 338 | (38.3) | 214 689 | (51.7) | 142 501 | (61.3) | 40 518 | (47.9) | 22 133 | (28.4) | 9325 | (49.5) |
| Endometriosis | 100 831 | (21.0) | 61 981 | (22.3) | 24 024 | (26.4) | 10 339 | (12.7) | 4385 | (16.2) | 97 044 | (23.4) | 59 311 | (25.5) | 23 579 | (27.9) | 10 038 | (12.9) | 4033 | (21.4) |
| Prolapse | 79 464 | (16.6) | 13 449 | (4.8) | 14 332 | (15.8) | 49 263 | (60.3) | 2383 | (8.8) | 77 535 | (18.7) | 12 812 | (5.5) | 13 930 | (16.5) | 48 492 | (62.2) | 2264 | (12.0) |
| Gynecologic cancer | 64 410 | (13.4) | 45 422 | (16.3) | 6337 | (7.0) | 3724 | (4.6) | 8154 | (30.2) | ||||||||||
| Menstrual disorder | 216 080 | (45.0) | 122 936 | (44.2) | 51 203 | (56.3) | 32 228 | (39.5) | 9537 | (35.3) | 212 615 | (51.2) | 120 861 | (52.0) | 50 583 | (59.8) | 31 686 | (40.7) | 9310 | (49.4) |
| Other | 42 514 | (8.9) | 29 101 | (10.5) | 6812 | (7.5) | 2434 | (3.0) | 3107 | (11.5) | 42 514 | (10.2) | 29 101 | (12.5) | 6812 | (8.1) | 2434 | (3.1) | 3107 | (16.5) |
| Adnexal surgery [n (%)] | 274 639 | (57.2) | 188 609 | (67.8) | 48 605 | (53.5) | 19 010 | (23.3) | 17 926 | (66.4) | 219 608 | (52.9) | 147 086 | (63.2) | 43 554 | (51.5) | 18 033 | (23.1) | 10 614 | (56.3) |
| Urban–rural location [n (%)] | ||||||||||||||||||||
| “Central” ≥1 million | 125 683 | (26.5) | 75 365 | (27.4) | 21 753 | (24.3) | 18 520 | (23.0) | 9343 | (34.7) | 106 815 | (26.0) | 62 194 | (27.0) | 20 135 | (24.2) | 17 576 | (22.9) | 6405 | (34.2) |
| “Fringe” ≥1 million | 121 907 | (25.7) | 71 752 | (26.1) | 23 897 | (26.7) | 18 732 | (23.3) | 6993 | (26.0) | 104 660 | (25.5) | 59 549 | (25.9) | 21 962 | (26.4) | 17 871 | (23.3) | 4932 | (26.3) |
| Metropolitan areas of 250 000–999 999 population | 84 012 | (17.7) | 46 710 | (17.0) | 15 569 | (17.4) | 15 907 | (19.8) | 5459 | (20.3) | 73 107 | (17.8) | 39 174 | (17.0) | 14 525 | (17.5) | 15 343 | (20.0) | 3840 | (20.5) |
| Metropolitan areas of 50 000–249 999 population | 48 053 | (10.1) | 25 115 | (9.1) | 10 714 | (12.0) | 9769 | (12.2) | 2273 | (8.5) | 43 025 | (10.5) | 21 567 | (9.4) | 10 138 | (12.2) | 9370 | (12.2) | 1850 | (9.9) |
| Micropolitan counties | 59 041 | (12.5) | 34 999 | (12.7) | 11 171 | (12.5) | 10 825 | (13.5) | 1772 | (6.6) | 51 884 | (12.7) | 29 894 | (13.0) | 10 549 | (12.7) | 10 208 | (13.3) | 1080 | (5.8) |
| Not metropolitan or micropolitan counties | 35 137 | (7.4) | 21 056 | (7.7) | 6291 | (7.0) | 6623 | (8.2) | 1059 | (3.9) | 30 572 | (7.5) | 17 655 | (7.7) | 5874 | (7.1) | 6331 | (8.3) | 637 | (3.4) |
| Median household income national quartile for patient ZIP code [n (%)] | ||||||||||||||||||||
| $1–$38 999 | 116 974 | (24.9) | 73 903 | (27.2) | 19 430 | (21.9) | 18 253 | (22.8) | 4895 | (18.4) | 102 320 | (25.2) | 63 225 | (27.8) | 18 146 | (21.9) | 17 218 | (22.6) | 3385 | (18.3) |
| $39 000–$47 999 | 122 021 | (26.0) | 71 462 | (26.3) | 21 838 | (24.6) | 22 140 | (27.7) | 6018 | (22.6) | 106 474 | (26.2) | 60 414 | (26.6) | 20 493 | (24.8) | 21 136 | (27.7) | 4090 | (22.1) |
| $48 000–$62 999 | 116 437 | (24.8) | 63 775 | (23.5) | 23 572 | (26.5) | 21 274 | (26.6) | 7282 | (27.4) | 101 425 | (25.0) | 53 317 | (23.5) | 22 085 | (26.7) | 20 410 | (26.8) | 5237 | (28.3) |
| ≥$63 000 | 113 704 | (24.2) | 62 404 | (23.0) | 24 043 | (27.1) | 18 291 | (22.9) | 8379 | (31.5) | 95 975 | (23.6) | 50 313 | (22.1) | 21 983 | (26.6) | 17 530 | (23.0) | 5797 | (31.3) |
| Primary payer [n (%)] | ||||||||||||||||||||
| Medicare | 61 863 | (12.9) | 33 610 | (12.1) | 7270 | (8.0) | 15 596 | (19.1) | 4618 | (17.1) | 41 303 | (10.0) | 18 386 | (7.9) | 5452 | (6.5) | 15 022 | (19.3) | 1899 | (10.1) |
| Medicaid | 50 774 | (10.6) | 32 299 | (11.6) | 8337 | (9.2) | 8119 | (10.0) | 1753 | (6.5) | 44 590 | (10.8) | 28 066 | (12.1) | 7749 | (9.2) | 7346 | (9.4) | 1273 | (6.8) |
| Private including HMOc | 329 717 | (68.9) | 187 855 | (67.7) | 69 043 | (76.2) | 52 422 | (64.3) | 19 388 | (71.9) | 296 699 | (71.6) | 165 233 | (71.2) | 65 566 | (77.8) | 50 469 | (64.9) | 14 782 | (78.5) |
| Self-pay | 16 743 | (3.5) | 11 916 | (4.3) | 2347 | (2.6) | 2032 | (2.5) | 393 | (1.5) | 14 339 | (3.5) | 10 127 | (4.4) | 2115 | (2.5) | 1826 | (2.3) | 240 | (1.3) |
| No charge | 1891 | (0.4) | 1200 | (0.4) | 388 | (0.4) | 252 | (0.3) | 46 | (0.2) | 1 642 | (0.4) | 1020 | (0.4) | 358 | (0.4) | 228 | (0.3) | 30 | (0.2) |
| Other | 17 662 | (3.7) | 10 474 | (3.8) | 3265 | (3.6) | 3063 | (3.8) | 773 | (2.9) | 15 793 | (3.8) | 9203 | (4.0) | 3082 | (3.7) | 2873 | (3.7) | 602 | (3.2) |
| Region of hospital [n (%)] | ||||||||||||||||||||
| Northeast | 74 787 | (15.6) | 42 755 | (15.4) | 15 497 | (17.0) | 11 552 | (14.1) | 4499 | (16.7) | 63 471 | (15.3) | 35 217 | (15.1) | 13 814 | (16.3) | 11 042 | (14.2) | 3079 | (16.3) |
| Midwest | 112 415 | (23.4) | 63 719 | (22.9) | 18 559 | (20.4) | 21 997 | (26.9) | 7476 | (27.7) | 95 012 | (22.9) | 50 965 | (21.9) | 17 438 | (20.6) | 21 104 | (27.1) | 5045 | (26.8) |
| South | 193 769 | (40.4) | 122 029 | (43.9) | 34 951 | (38.4) | 27 740 | (34.0) | 8461 | (31.3) | 172 334 | (41.5) | 106 308 | (45.7) | 32 972 | (39.0) | 26 365 | (33.8) | 6309 | (33.5) |
| West | 98 843 | (20.6) | 49 552 | (17.8) | 21 899 | (24.1) | 20 376 | (25.0) | 6554 | (24.3) | 84 586 | (20.4) | 40 144 | (17.3) | 20 344 | (24.1) | 19 430 | (24.9) | 4403 | (23.4) |
| % of all operations performed on outpatient basis [mean (SE)] | 59.4 | (0.7) | 59.5 | (0.7) | 60.1 | (0.9) | 59.8 | (0.9) | 54.4 | (1.4) | 59.8 | (0.7) | 60.0 | (0.7) | 60.4 | (0.9) | 59.9 | (0.9) | 54.5 | (1.6) |
| Location and teaching status [n (%)] | ||||||||||||||||||||
| Rural | 56 926 | (12.1) | 33 169 | (12.2) | 11 189 | (12.5) | 11 994 | (15.0) | 487 | (1.9) | 53 371 | (13.1) | 30 754 | (13.5) | 10 829 | (13.0) | 11 349 | (14.9) | 357 | (2.0) |
| Urban non-teaching | 202 908 | (43.2) | 115 964 | (42.6) | 39 815 | (44.6) | 36 963 | (46.2) | 9642 | (36.8) | 184 822 | (45.5) | 103 389 | (45.5) | 38 018 | (45.7) | 35 600 | (46.6) | 7441 | (40.7) |
| Urban teaching | 209 812 | (44.7) | 122 771 | (45.2) | 38 338 | (42.9) | 31 044 | (38.8) | 16 103 | (61.4) | 168 344 | (41.4) | 93 221 | (41.0) | 34 263 | (41.2) | 29 411 | (38.5) | 10 492 | (57.4) |
| Hospital bed size [n (%)] | ||||||||||||||||||||
| Small | 51 419 | (10.9) | 27 913 | (10.3) | 13 042 | (14.6) | 8315 | (10.4) | 1880 | (7.2) | 45 048 | (11.1) | 23 607 | (10.4) | 12 356 | (14.9) | 8011 | (10.5) | 878 | (4.8) |
| Medium | 119 172 | (25.4) | 69 976 | (25.7) | 23 488 | (26.3) | 20 327 | (25.4) | 5072 | (19.3) | 106 582 | (26.2) | 60 556 | (26.6) | 22 482 | (27.1) | 19 524 | (25.6) | 3812 | (20.8) |
| Large | 299 055 | (63.7) | 174 015 | (64.0) | 52 813 | (59.1) | 51 359 | (64.2) | 19 280 | (73.5) | 254 907 | (62.7) | 143 202 | (63.0) | 48 272 | (58.1) | 48 825 | (63.9) | 13 601 | (74.4) |
| Severity of illness subclass [n (%)] | ||||||||||||||||||||
| Minor loss of function | 323 017 | (67.3) | 174 860 | (62.9) | 69 196 | (76.1) | 60 535 | (74.1) | 18 088 | (67.0) | 296 068 | (71.3) | 159 007 | (68.4) | 65 312 | (77.2) | 57 911 | (74.3) | 13 572 | (72.1) |
| Moderate loss of function | 131 882 | (27.5) | 83 828 | (30.1) | 20 089 | (22.1) | 19 803 | (24.2) | 7875 | (29.2) | 105 354 | (25.4) | 63 633 | (27.4) | 17 981 | (21.3) | 18 833 | (24.2) | 4726 | (25.1) |
| Major loss of function | 20 565 | (4.3) | 15 968 | (5.7) | 1423 | (1.6) | 1185 | (1.5) | 914 | (3.4) | 11 727 | (2.8) | 8253 | (3.5) | 1128 | (1.3) | 1069 | (1.4) | 479 | (2.5) |
| Extreme loss of function | 4351 | (0.9) | 3400 | (1.2) | 198 | (0.2) | 141 | (0.2) | 114 | (0.4) | 2255 | (0.5) | 1741 | (0.7) | 148 | (0.2) | 127 | (0.2) | 59 | (0.3) |
| AHRQc comorbidity measure for obesity [n (%)] | 55 739 | (11.6) | 37 633 | (13.5) | 8134 | (8.9) | 5813 | (7.1) | 3981 | (14.7) | 43 074 | (10.4) | 28 179 | (12.1) | 7158 | (8.5) | 5414 | (6.9) | 2214 | (11.8) |
categories not mutually exclusive
AHRQ = Agency for Healthcare Research and Quality; HMO = Health Maintenance Organization.
Regional variations in the incidence and mode of access for hysterectomy are highlighted in Table 3. Forty percent of all US hysterectomies were performed in the South, which also had the highest incidence of abdominal hysterectomy (63.0% of all cases). Abdominal hysterectomy was performed least often in the West (50.1% of all cases). The Northeast and West had the highest incidences of the laparoscopic approach (20.7% and 22.2%, respectively), whereas the vaginal approach was most common in the Midwest (19.6%) and West (20.6%). The frequency of robotic operations was lowest in the South but was similar across other regions.
Table 3.
Rate and Mode of Hysterectomy by Region: All Indications
| North | Midwest | South | West | |
|---|---|---|---|---|
| Abdominal [n (%)] | 42 755 (57.2) | 63 719 (56.7) | 122 029 (63.0) | 49 550 (50.1) |
| Laparoscopic [n (%)] | 15 497 (20.7) | 18 559 (16.5) | 34 951 (18.0) | 21 899 (22.2) |
| Vaginal [n (%)] | 11 552 (15.4) | 21 997 (19.6) | 27 740 (14.3) | 20 376 (20.6) |
| Robotic [n (%)] | 4499 (6.0) | 7476 (6.7) | 8461 (4.4) | 6554 (6.6) |
| Other [n (%)] | 484 (0.6) | 664 (0.6) | 588 (0.3) | 463 (0.5) |
| Total No. of hysterectomies | 74 787 | 112 415 | 193 769 | 98 843 |
| % of national hysterectomies | 15.6 | 23.4 | 40.4 | 20.6 |
A logistic regression analysis was performed to assess factors associated with undergoing minimally invasive hysterectomy (laparoscopic, vaginal, or robotic) versus abdominal hysterectomy for benign indications (Table 4). Women aged >50 years had higher odds of undergoing minimally invasive surgery (P < .0001), as did women in ZIP codes with higher median household incomes (P = .007 and P = .009 for median income of $48 000–$62 999 and ≥$63 000, respectively). Compared with white women, all races except Native Americans were less likely to undergo a minimally invasive hysterectomy; black, Hispanic, and Asian women had 30% to 50% lower odds of undergoing minimally invasive hysterectomies (P < .0001). Women with prolapse or menstrual disorder were more likely to undergo minimally invasive operations, whereas the indication of fibroids was associated with a higher odds of abdominal surgery (P < .0001). Concomitant adnexal surgery was associated with a 60% decreased odds of undergoing minimally invasive surgery (P < .0001). Compared to women with private insurance, women who were covered by Medicaid and who were covered by Medicaid or who were self-pay had 22% and 31% decreased odds of undergoing minimally invasive surgery, respectively (P < .0001 and P = .01, respectively). In addition, compared with women in the Northeast, women in the West had 50% greater odds of undergoing minimally invasive surgery (P = .02). No difference was seen regarding urban–rural location or teaching status of the hospital. Increasing severity of illness was associated with decreased odds of undergoing minimally invasive hysterectomy (P < .0001), although no effect was seen regarding obesity.
Table 4.
Logistic Regression Analysis Comparing Minimally Invasive Hysterectomy (Laparoscopic, Vaginal, or Robotic) With Abdominal Hysterectomy Among Women With Benign Conditions
| Abdominal (n = 232 633) |
Minimally Invasive (n = 181 346) |
Crude ORa (95% CIa) | Adjustedb OR (95% CI) | P Value | |||
|---|---|---|---|---|---|---|---|
| n | (%) | n | (%) | ||||
| Age | |||||||
| 18–34 y | 22 947 | (9.9) | 19 596 | (10.8) | 1.00 (reference) | 1.00 (reference) | |
| 35–39 y | 32 685 | (14.0) | 25 461 | (14.0) | 0.91 (0.85–0.98) | 0.99 (0.92–1.06) | .69 |
| 40–44 y | 55 285 | (23.8) | 36 000 | (19.9) | 0.76 (0.71–0.82) | 0.94 (0.87–1.01) | .09 |
| 45–49 y | 60 805 | (26.1) | 38 314 | (21.1) | 0.74 (0.68–0.80) | 1.03 (0.95–1.11) | .47 |
| 50–54 y | 30 480 | (13.1) | 21 374 | (11.8) | 0.82 (0.75–0.90) | 1.21 (1.10–1.32) | <.0001 |
| ≥55 y | 30 432 | (13.1) | 40 601 | (22.4) | 1.56 (1.40–1.75) | 1.34 (1.21–1.49) | <.0001 |
| Race/ethnicity | |||||||
| White | 121 790 | (52.4) | 115 264 | (63.6) | 1.00 (reference) | 1.00 (reference) | |
| Black | 43 829 | (18.8) | 13 823 | (7.6) | 0.33 (0.30–0.37) | 0.51 (0.45–0.57) | <.0001 |
| Hispanic | 23 478 | (10.1) | 15 937 | (8.8) | 0.72 (0.63–0.81) | 0.67 (0.59–0.78) | <.0001 |
| Asian/Pacific Islander | 5649 | (2.4) | 3117 | (1.7) | 0.58 (0.47–0.72) | 0.58 (0.46–0.74) | <.0001 |
| Native American | 1320 | (0.6) | 1807 | (1.0) | 1.45 (0.91–2.29) | 1.68 (1.04–2.71) | .03 |
| Other | 6779 | (2.9) | 4059 | (2.2) | 0.63 (0.53–0.76) | 0.70 (0.58–0.84) | .0002 |
| Missing | 29 788 | (12.8) | 27 339 | (15.1) | 0.97 (0.79–1.19) | 1.09 (0.89–1.33) | .43 |
| Indicationb | |||||||
| Fibroids | 142 501 | (61.3) | 71 976 | (39.7) | 0.42 (0.39–0.44) | 0.51 (0.48–0.54) | <.0001 |
| Endometriosis | 59 311 | (25.5) | 37 650 | (20.8) | 0.77 (0.71–0.83) | 0.93 (0.86–1.01) | .08 |
| Prolapse | 12 812 | (5.5) | 64 687 | (35.7) | 9.51 (8.18–11.1) | 6.53 (5.60–7.62) | <.0001 |
| Menstrual disorder | 120 861 | (52.0) | 91 579 | (50.5) | 0.94 (0.89–1.01) | 1.33 (1.24–1.43) | <.0001 |
| Other | 29 101 | (12.5) | 12 353 | (6.8) | 0.51 (0.47–0.56) | 0.71 (0.64–0.79) | <.0001 |
| Adnexal surgery | 147 086 | (63.2) | 72 200 | (39.8) | 0.38 (0.36–0.41) | 0.39 (0.36–0.41) | <.0001 |
| Urban–rural location | |||||||
| “Central” ≥1 million | 62 194 | (27.0) | 44 117 | (24.7) | 1.00 (reference) | 1.00 (reference) | |
| “Fringe” ≥1 million | 59 549 | (25.9) | 44 765 | (25.1) | 1.06 (0.91–1.24) | 0.93 (0.78–1.12) | .45 |
| Metropolitan areas of 250 000–999 999 population | 39 174 | (17.0) | 33 708 | (18.9) | 1.21 (0.98–1.50) | 1.03 (0.81–1.32) | .80 |
| Metropolitan areas of 50 000–249 999 population | 21 567 | (9.4) | 21 358 | (12.0) | 1.40 (1.07–1.82) | 1.30 (0.98–1.72) | .07 |
| Micropolitan counties | 29 894 | (13.0) | 21 836 | (12.2) | 1.03 (0.84–1.26) | 0.92 (0.73–1.16) | .50 |
| Not metropolitan or micropolitan counties | 17 655 | (7.7) | 12 842 | (7.2) | 1.03 (0.85–1.24) | 0.93 (0.74–1.15) | .49 |
| Median household income national quartile for patient ZIP code | |||||||
| $1-$38 999 | 63 225 | (27.8) | 38 749 | (21.8) | 1.00 (reference) | 1.00 (reference) | |
| $39 000-$47 999 | 60 414 | (26.6) | 45 718 | (25.8) | 1.23 (1.11–1.37) | 1.02 (0.92–1.13) | .65 |
| $48 000-$62 999 | 53 317 | (23.5) | 47 732 | (26.9) | 1.46 (1.28–1.66) | 1.18 (1.04–1.32) | .007 |
| ≥$63 000 | 50 313 | (22.1) | 45 311 | (25.5) | 1.47 (1.26–1.71) | 1.21 (1.05–1.39) | .009 |
| Primary payer | |||||||
| Medicare | 18 386 | (7.9) | 22 372 | (12.4) | 1.54 (1.41–1.67) | 1.05 (0.96–1.14) | .30 |
| Medicaid | 28 066 | (12.1) | 16 368 | (9.0) | 0.74 (0.67–0.82) | 0.78 (0.71–0.85) | <.0001 |
| Private including HMOa | 165 233 | (71.2) | 130 817 | (72.3) | 1.00 (reference) | 1.00 (reference) | |
| Self-pay | 10 127 | (4.4) | 4181 | (2.3) | 0.52 (0.40–0.69) | 0.69 (0.51–0.93) | .01 |
| No charge | 1020 | (0.4) | 616 | (0.3) | 0.76 (0.54–1.07) | 1.16 (0.73–1.85) | .52 |
| Other | 9203 | (4.0) | 6557 | (3.6) | 0.90 (0.76–1.07) | 0.94 (0.78–1.14) | .53 |
| Region of hospital | |||||||
| Northeast | 35 217 | (15.1) | 27 935 | (15.4) | 1.00 (reference) | 1.00 (reference) | |
| Midwest | 50 965 | (21.9) | 43 587 | (24.0) | 1.08 (0.81–1.43) | 1.06 (0.76–1.48) | .74 |
| South | 106 308 | (45.7) | 65 647 | (36.2) | 0.78 (0.60–1.02) | 0.94 (0.68–1.29) | .70 |
| West | 40 144 | (17.3) | 44 177 | (24.4) | 1.39 (1.04–1.85) | 1.51 (1.08–2.12) | .02 |
| % of all operations performed on outpatient basis | |||||||
| <55 | 71 724 | (31.7) | 59 987 | (34.5) | 1.00 (reference) | 1.00 (reference) | |
| 55–65.9 | 74 897 | (33.1) | 51 603 | (29.7) | 0.82 (0.67–1.02) | 0.79 (0.63–0.98) | .04 |
| ≥66 | 79 887 | (35.3) | 62 125 | (35.8) | 0.93 (0.77–1.12) | 0.85 (0.68–1.06) | .15 |
| Location and teaching status | |||||||
| Rural | 30 754 | (13.5) | 22 535 | (12.7) | 1.00 (reference) | 1.00 (reference) | |
| Urban non-teaching | 103 389 | (45.5) | 81 059 | (45.6) | 1.07 (0.85–1.35) | 0.97 (0.73–1.29) | .82 |
| Urban teaching | 93 221 | (41.0) | 74 167 | (41.7) | 1.09 (0.86–1.37) | 1.13 (0.84–1.53) | .42 |
| Hospital bed size | |||||||
| Small | 23 607 | (10.4) | 21 246 | (12.0) | 1.00 (reference) | 1.00 (reference) | |
| Medium | 60 556 | (26.6) | 45 818 | (25.8) | 0.84 (0.66–1.08) | 0.77 (0.59–1.00) | .05 |
| Large | 143 202 | (63.0) | 110 698 | (62.3) | 0.86 (0.70–1.05) | 0.82 (0.64–1.06) | .13 |
| Severity of illness subclass | |||||||
| Minor loss of function | 159 007 | (68.4) | 136 795 | (75.4) | 1.00 (reference) | 1.00 (reference) | |
| Moderate loss of function | 63 633 | (27.4) | 41 540 | (22.9) | 0.76 (0.72–0.80) | 0.73 (0.69–0.77) | <.0001 |
| Major loss of function | 8253 | (3.5) | 2677 | (1.5) | 0.38 (0.33–0.43) | 0.43 (0.37–0.49) | <.0001 |
| Extreme loss of function | 1741 | (0.7) | 334 | (0.2) | 0.22 (0.17–0.30) | 0.26 (0.19–0.35) | <.0001 |
| AHRQa comorbidity measure for obesity | 28 179 | (12.1) | 14 787 | (8.2) | 0.64 (0.59–0.70) | 0.93 (0.85–1.01) | .10 |
AHRQ = Agency for Healthcare Research and Quality; CI, confidence interval; HMO = Health Maintenance Organization; OR, odds ratio.
All variables in the table were added to one logistic regression model.
Table 5 shows the data regarding cost and length of stay for hysterectomies by varying mode of access. Cost was defined as the total mean charges reported by the hospital; professional fees and noncovered charges are generally not included in this calculation, although slight reporting differences exist on a state-by-state basis.7 Looking at the group of all hysterectomies, we found that vaginal hysterectomy had the lowest mean charge per case ($20 144) whereas robotic hysterectomy had the highest ($38 161); abdominal and laparoscopic hysterectomy costs differed by just under $2500 per case. Similar findings were seen in the benign-only hysterectomy group, although the abdominal and laparoscopic hysterectomy groups had more similar mean charges among this subset. A length of stay >1 day was markedly more common in the abdominal hysterectomy categories, with most laparoscopic or robotic hysterectomy patients being discharged on the first postoperative day.
Table 5.
Total Charges and Length of Stay for All and Benign Hysterectomies by Mode
| All Hysterectomies |
Benign Hysterectomies |
|||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| All (n = 479 814) | Abdominal (n = 278 055) | Laparoscopic (n = 90 906) | Vaginal (n = 81 665) | Robotic (n = 26 990) | All (n = 415 404) | Abdominal (n = 232 633) | Laparoscopic (n = 84 569) | Vaginal (n = 77 940) | Robotic (n = 18 836) | |||||||||||
| Length of stay [n (%)] | ||||||||||||||||||||
| 0 | 1842 | (0.4) | 147 | (0.05) | 1048 | (1.2) | 350 | (0.4) | 297 | (1.1) | 1734 | (0.4) | 142 | (0.06) | 1008 | (1.2) | 341 | (0.4) | 244 | (1.3) |
| 1 | 128 187 | (26.7) | 10 607 | (3.8) | 57 663 | (63.4) | 42 282 | (51.8) | 17 593 | (65.2) | 117 371 | (28.3) | 10 029 | (4.3) | 54 121 | (64.0) | 40 121 | (51.5) | 13 064 | (69.4) |
| 2 | 187 771 | (39.1) | 126 641 | (45.5) | 24 783 | (27.3) | 29 779 | (36.5) | 6364 | (23.6) | 173 796 | (41.8) | 117 822 | (50.6) | 22 999 | (27.2) | 28 738 | (36.9) | 4038 | (21.4) |
| 3 | 94 415 | (19.7) | 81 669 | (29.4) | 4731 | (5.2) | 6501 | (8.0) | 1373 | (5.1) | 80 327 | (19.3) | 68 938 | (29.6) | 4227 | (5.0) | 6257 | (8.0) | 807 | (4.3) |
| ≥4 | 67 600 | (14.1) | 58 991 | (21.2) | 2681 | (2.9) | 2752 | (3.4) | 1363 | (5.1) | 42 176 | (10.2) | 35 703 | (15.3) | 2214 | (2.6) | 2484 | (3.2) | 683 | (3.6) |
| Total charges [mean (SE)] ($) | 27 295 | (844) | 28 173 | (933) | 25 831 | (1046) | 20 144 | (671) | 38 161 | (2358) | 25 000 | (714) | 25 171 | (756) | 25 231 | (954) | 20 112 | (672) | 36 635 | (2649) |
DISCUSSION
Because hysterectomy is one of the most common gynecologic procedures, it is of the utmost importance to investigate trends in national hysterectomy rates. Of the 479 814 hysterectomies performed in 2009 for any indication, 41.8% were completed via minimally invasive mode. In the benign-only subgroup, 44% of the 415 404 hysterectomies were approached in a minimally invasive fashion. Regarding the incidence of robotic assistance, this occurred in 5.6% of all hysterectomies. When considering robotic assistance as a variation on conventional laparoscopy, we found that 16.6% of benign laparoscopic hysterectomy cases and 20.7% of all laparoscopic cases included use of the robot. Logistic regression analysis was performed to control for patient and demographic variables; the results of this analysis show that factors favoring a minimally invasive approach to hysterectomy include patient age >50 years, diagnosis of prolapse or menstrual disorder, higher income, and location in the western United States. Factors associated with the abdominal approach to hysterectomy include minority race, diagnosis of fibroids, concomitant adnexal surgery, self-pay or Medicaid payer, and increasing severity of illness. Although a length of stay >1 day was most common among the abdominal cases, the robotic approach to hysterectomy was associated with a distinctly higher cost than any other mode.
The strengths of this work include the large number of patients and associated characteristics available for analysis. Along with this comes the limitation of inherent misclassification of data in a large cohort, especially when relying on ICD-9-CM codes to determine mode of surgery. This may be a particular issue regarding misidentification or underestimation of robotic-assisted laparoscopic hysterectomy cases because these were only able to be identified by use of modifier codes. Any misclassification due to coding error would presumably have been nondifferential, however. In addition, there were substantial missing data for race in this cohort. Although we used indicators for missing data to ensure that models were run on the entire dataset, we may not have been able to fully adjust for potential confounding by race because of the missing data. Compared with existing literature on the subject, unique aspects of this analysis are the inclusion of oncologic cases and comparison of the abdominal approach with any minimally invasive technique. This may provide more practical information regarding current practices and limitations as gynecologists strive to adhere to published guidelines recommending vaginal or laparoscopic hysterectomy as the primary approach.1,2
Our results represent both a marked decrease from prior years' analyses of annual hysterectomy volume and a notable shift in mode of surgical access. Regarding the decrease in hysterectomy volume, these findings have been echoed in a comparative analysis of US hysterectomy rates between 2008 and 2010.8 Using the NIS, Wright et al8 showed a peak annual hysterectomy incidence of 681 234 in 2002, with a decline to 433 621 cases in 2010. It is not clear whether these findings represent a genuine decline in surgical cases perhaps because of the increasing popularity of medical therapies or non-extirpative procedures. It is also possible that the perceived decrease in volume may reflect the continuing trend toward minimally invasive modes of hysterectomy and the accompanying opportunity for outpatient recovery. Although patients who are discharged home on the day of surgery are accounted for in the NIS, the sample does not include procedures that are performed in ambulatory surgical centers. With the shifts in care toward same-day discharge in appropriate postoperative candidates, it is possible that a larger proportion of laparoscopic or vaginal hysterectomies are being performed in ambulatory centers.9,10 If this is the case, then we may be underestimating not only the national hysterectomy volume but also the relative proportion of cases completed in a minimally invasive fashion.
Review of comparable analyses of the NIS from past years shows a steady increase in use of the laparoscopic approach to surgery; laparoscopic hysterectomy accounted for 12% of benign cases in 2003, 14% of benign cases in 2005, and 20% of benign cases in our work.4,5 Although use of the vaginal approach to hysterectomy has decreased (22% of benign cases in 2003 and 2005 and 18% in 2009), perhaps the most striking change represented in our analysis is the incorporation of robotic-assisted laparoscopy into the available modes of access. Wright et al8 corroborated this finding, reporting that the use of robotic hysterectomy increased from 0.9% in 2008 to 8.2% in 2010. This highlights an important consideration regarding health care cost when one takes into account the increased cost of the robotic approach to hysterectomy. Although this study design is not equipped to provide detailed cost analysis, the reported total mean hospital charges for robotic hysterectomy were 35% to 44% higher than the next most expensive mode of hysterectomy. Previous studies have also shown significantly increased cost associated with robotic hysterectomy.6 It has been suggested that this cost may be partially offset by decreased operative time with increasing surgeon experience, as well as shortened postoperative recovery time with a minimally invasive approach; however, even when one accounts for these elements of the cost equation, robotic hysterectomy remains more expensive than laparoscopic hysterectomy.11,12
The findings of racial disparities in this study are consistent with the existing literature that suggests both a higher rate of hysterectomy among black women and increased odds of an abdominal approach to surgery among minority women.13 In the analysis of the 2005 NIS data by Jacoby et al,4 minority women were found to have 40% to 50% lower odds of undergoing laparoscopic hysterectomy when controlling for other baseline factors and surgical indication. Our findings show that black, Hispanic, and Asian women have a 30% to 50% decreased odds of undergoing minimally invasive hysterectomy (including not only laparoscopic but also vaginal or robotic approaches). Prior work also supports the associations found between income, region, and payer and the mode of hysterectomy.4,14
CONCLUSION
Although our findings show a promising shift toward minimally invasive approaches to hysterectomy (particularly laparoscopic and robotic), important racial, socioeconomic, and regional disparities exist. Increased awareness and training in minimally invasive techniques may help offset some of these barriers to care. As robotic hysterectomy becomes increasingly prevalent, consideration of cost containment will become more important. Future analyses of ambulatory surgical center data may lend additional insight into these and other issues surrounding hysterectomy surveillance.
Acknowledgments
The authors acknowledge the Healthcare Cost and Utilization Project for its work maintaining the NIS.
Contributor Information
Sarah L. Cohen, Division of Minimally Invasive Gynecologic Surgery, Brigham and Women's Hospital, Boston, MA, USA..
Allison F. Vitonis, Department of Obstetrics and Gynecology Epidemiology Center, Brigham and Women's Hospital, Boston, MA, USA..
Jon I. Einarsson, Division of Minimally Invasive Gynecologic Surgery, Brigham and Women's Hospital, Boston, MA, USA..
References:
- 1. ACOG Committee Opinion No. 444: choosing the route of hysterectomy for benign disease. Obstet Gynecol. 2009;114(5):1156–1158 [DOI] [PubMed] [Google Scholar]
- 2. AAGL Advancing Minimally Invasive Gynecology Worldwide. AAGL position statement: route of hysterectomy to treat benign uterine disease. J Minim Invasive Gynecol. 2011;18(1):1–3 [DOI] [PubMed] [Google Scholar]
- 3. Nieboer TE, Johnson N, Lethaby A, et al. Surgical approach to hysterectomy for benign gynaecological disease. Cochrane Database Syst Rev. 2009;(3):CD003677. [DOI] [PubMed] [Google Scholar]
- 4. Jacoby VL, Autry A, Jacobson G, Domush R, Nakagawa S, Jacoby A. Nationwide use of laparoscopic hysterectomy compared with abdominal and vaginal approaches. Obstet Gynecol. 2009;114(5):1041–1048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Wu JM, Wechter ME, Geller EJ, Nguyen TV, Visco AG. Hysterectomy rates in the United States, 2003. Obstet Gynecol. 2007;110(5):1091–1095 [DOI] [PubMed] [Google Scholar]
- 6. Wright JD, Ananth CV, Lewin SN, et al. Robotically assisted vs laparoscopic hysterectomy among women with benign gynecologic disease. JAMA. 2013;309(7):689–698 [DOI] [PubMed] [Google Scholar]
- 7. HCUP Nationwide Inpatient Sample (NIS). Healthcare Cost and Utilization Project (HCUP). Rockville, MD: Agency for Healthcare Research and Quality; 2009. Available at: www.hcup-us.ahrq.gov/nisoverview.jsp [Google Scholar]
- 8. Wright JD, Herzog TJ, Tsui J, et al. Nationwide trends in the performance of inpatient hysterectomy in the United States. Obstet Gynecol. 2013;122(2 Pt 1):233–241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Zakaria MA, Levy BS. Outpatient vaginal hysterectomy: optimizing perioperative management for same-day discharge. Obstet Gynecol. 2012;120(6):1355–1361 [DOI] [PubMed] [Google Scholar]
- 10. Perron-Burdick M, Yamamoto M, Zaritsky E. Same-day discharge after laparoscopic hysterectomy. Obstet Gynecol. 2011;117(5):1136–1141 [DOI] [PubMed] [Google Scholar]
- 11. Shah NT, Wright KN, Jonsdottir GM, Jorgensen S, Einarsson JI, Muto MG. The feasibility of societal cost equivalence between robotic hysterectomy and alternate hysterectomy methods for endometrial cancer. Obstet Gynecol Int. 2011;2011:570464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Barnett JC, Judd JP, Wu JM, Scales CD, Jr, Myers ER, Havrilesky LJ. Cost comparison among robotic, laparoscopic, and open hysterectomy for endometrial cancer. Obstet Gynecol. 2010;116(3):685–693 [DOI] [PubMed] [Google Scholar]
- 13. Jacoby VL, Fujimoto VY, Giudice LC, Kuppermann M, Washington AE. Racial and ethnic disparities in benign gynecologic conditions and associated surgeries. Am J Obstet Gynecol. 2010;202(6):514–521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Abenhaim HA, Azziz R, Hu J, Bartolucci A, Tulandi T. Socioeconomic and racial predictors of undergoing laparoscopic hysterectomy for selected benign diseases: analysis of 341487 hysterectomies. J Minim Invasive Gynecol. 2008;15(1):11–15 [DOI] [PubMed] [Google Scholar]