Abstract
Background and Objectives:
This study describes perioperative patient safety outcomes comparing laparoscopic appendectomy with open appendectomy in the elderly population (defined as age ≥65 years) during the diffusion of laparoscopic appendectomy into widespread clinical practice.
Methods:
We performed a cross-sectional analysis of patients undergoing open or laparoscopic appendectomy in the US Nationwide Inpatient Sample, a 20% sample of inpatient discharges from 1056 hospitals, from 1998 to 2009, and used weighted sampling to estimate national trends. Multivariate logistic regression modeling was used to examine the association of laparoscopy with perioperative outcomes.
Results:
Patients who met the inclusion criteria totaled 257 484. Of these, 87 209 (34%) underwent laparoscopic appendectomy. These patients were younger (P < .001); had lower Charlson comorbidity scores (P < .001); were more likely to be white (P < .001), to be privately insured (P = .005), and to undergo surgery in urban hospitals (P < .001); and were less likely to have appendiceal rupture (P < .001). Laparoscopic appendectomy was associated with a decreased length of stay (4.44 days vs 7.86 days, P < .001), fewer total patient safety indicator events (1.8% vs 3.5%, P < .001), and a decreased mortality rate (0.9% vs 2.8%, P < .001). On multivariate analyses, we observed a 32% (odds ratio, 0.68) decreased probability of patient safety events occurring in laparoscopic appendectomy cases versus open appendectomy cases as measured by patient safety indicators.
Conclusion:
The data suggest that laparoscopic appendectomy is associated with improved clinical outcomes in the elderly and that diffusion of laparoscopic appendectomy is not associated with adverse patient safety events in this population.
Keywords: Appendectomy, Patient safety indicator, Surgery in elderly
INTRODUCTION
Laparoscopic appendectomy (LA) is an established treatment method for uncomplicated acute appendicitis.1 It has the advantage of using small incisions to obtain good-quality visualization and access to the abdominal cavity.2 Compared with open appendectomy (OA), LA is associated with a decreased likelihood of superficial wound infection, decreased need for postoperative analgesics, quicker return to preoperative functional status, and improved cosmetic results.3–10 Although these outcomes are appropriate measures for younger patients, their relevance as measures of quality of care and patient safety in the elderly remains undefined.
Numerous factors, including the US baby boom, better health coverage, and longer life expectancy, have led to an increase in the elderly population. About 1 in 8 Americans were elderly in 1994 (defined as age ≥65 years), but about 1 in 5 will be elderly by the year 2030.11 The lifetime risk of appendectomy is 12.0% in males and 23.1% in females. On the basis of these trends—an aging population and a relatively high lifetime prevalence of appendectomy—the prevalence of appendectomies in the elderly is increasing.12 Elderly surgery patients tend to have increased comorbidities, less physiologic reserve, and an altered nutritional status and show increased postoperative morbidity and mortality rates compared with younger adults.13,14 Reported complication rates after OA in the elderly range from 12% to 74%; the mortality rate is as high as 14%.15–18
In the groundbreaking report To Err Is Human: Building a Safer Health System, the Institute of Medicine observed that medical errors occurring in contemporary health care systems result primarily from problems inherent within organizations and processes rather than individuals.19 Patient safety indicators (PSIs), designed as robust and accessible standardized process measures of patient safety events, are useful metrics of preventable medical errors that have been broadly applied and validated.20–22
Although prior studies have suggested that LA is associated with improved outcomes in elderly patients compared with OA,14,23–25 comprehensive patient safety analyses, using validated, process-driven measures, have yet to be performed. Safety analyses incorporating validated patient safety outcomes would potentially inform the selection of operative approaches for appendectomy in the elderly. Therefore we compared the prevalence of adverse patient safety events occurring in LA cases and OA cases in a national database over a 12-year period.
MATERIALS AND METHODS
Patient Cohort
We analyzed the association of perioperative adverse patient safety events occurring in LA cases and OA cases in the elderly. Data on inpatient procedures and adverse events were obtained from the Healthcare Cost and Utilization Project Nationwide Inpatient Sample (NIS) produced by the US Agency for Healthcare Research and Quality (AHRQ). The NIS represents the largest hospital inpatient dataset in the United States and consists of a 20% sample of inpatient discharges from 40 states and 1044 hospitals. It contains deidentified patient, physician, and hospital clinical data with safeguards to protect privacy and is compiled from 7 to 12 million hospital stays each year. Weighted sampling provides estimates for national trends. The NIS is a unique database that provides information on a variety of patient groups, regardless of payer, including persons covered by Medicare, Medicaid, and private insurance, as well as uninsured persons. All discharges with a principal diagnosis of acute appendicitis identified through International Classification of Diseases, Ninth Revision, Clinical Modification codes were evaluated. All identified patients from 1998 to 2009 were included in the analysis and divided into “laparoscopy” and “open” based on document procedure codes. Complicated appendicitis was defined as perforated or abscessed.
Patient Safety Indicators
Developed by the AHRQ, PSIs are metrics of adverse outcomes26–28 (Table 1) that provide hospital- and national-level safety performance measures with greater specificity than other methods while avoiding the problems of reporting bias.29 PSIs include the following: development of anesthetic complications, pneumothorax, hemorrhage/hematoma, decubitus ulcer, venous thrombosis/pulmonary embolism, hip fracture, postoperative physiologic and metabolic derangements, postoperative respiratory failure, sepsis, and accidental puncture or laceration during a procedure. Accidental punctures or lacerations include injuries to the surrounding organs including the bowel or other solid organ injuries and represent a wide spectrum of injury from minor to severe.
Table 1.
US Agency for Healthcare Research and Quality PSIs
| Complications of anesthesia (No. 1) |
| Death in low-mortality diagnosis-related groups (No. 2) |
| Decubitus ulcer (No. 3) |
| Failure to rescue (No. 4) |
| Iatrogenic pneumothorax (No. 6) |
| Selected infections due to medical care (No. 7) |
| Postoperative hip fracture (No. 8) |
| Postoperative hemorrhage or hematoma (No. 9) |
| Postoperative physiologic and metabolic derangements (No. 10) |
| Postoperative respiratory failure (No. 11) |
| Postoperative PEa/DVTa (No. 12) |
| Postoperative sepsis (No. 13) |
| Postoperative wound dehiscence (No. 14) |
| Accidental puncture or laceration (No. 15) |
| Transfusion reaction (No. 16) |
DVT = deep venous thrombosis; PE = pulmonary embolism.
Outcome Measures
The primary outcome variable was the occurrence of any PSI, a robust screening measure for identifying general systems problems that merit further examination.21 Secondary outcome measures included total mortality rate and length of stay (LOS). A subset analysis of the total number of PSI events was also conducted.
The primary outcome variable was operation type (LA vs OA), with adjustment for known covariates. Covariates included in the analysis were age, sex, race (white, African American, or other), ruptured appendix/abscess of appendix, income (<$45 000 or ≥$45 000), insurance (private, Medicare, Medicaid, or other), hospital type (teaching or nonteaching), and hospital location (rural or urban); in addition, we included year (1998–2009) as a covariate to address evolving indications for, and collective expertise with, LA. Associated comorbidities were controlled for by use of the Charlson index (0–2 or ≥3).30,31 Complication and mortality rates were evaluated as categorical variables. Independent univariate analyses were performed assessing secondary outcomes defined as individual AHRQ PSI events (Table 1), including deaths in low-mortality diagnosis-related groups—an indicator for identifying in-hospital deaths occurring in patients unlikely to die during hospitalization. A cost analysis of the median and quartile range of total hospital charges adjusted for inflation was investigated as a secondary outcome measure.
Statistical Analysis
Statistical analysis was performed with STATA software, version 11.2 SE (STATA Corp LP, College Station, Texas). Univariate independent t tests were used for comparisons of quantitative variables; Fisher exact and χ2 tests were used to assess differences in the categorical variables. Adjusted odds ratios for multiple logistic regression models were obtained to evaluate risk-adjusted endpoints.
RESULTS
Prevalence of LA
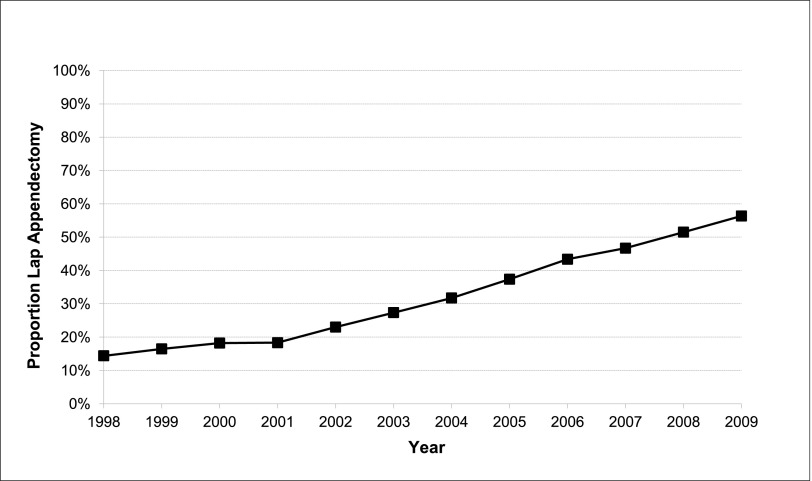
From 1998 to 2009, 257 484 appendectomies were performed for acute appendicitis in adults aged ≥65 years in the NIS. Of those, 170 276 (66%) were OAs and 87 209 (34%) were LAs. The annual prevalence of LA in the elderly increased from 14.4% in 1998 to 56.3% in 2009. In 2008 the number of appendectomies performed laparoscopically exceeded the number performed in an open manner for the first time (Figures 1 and 2).
Figure 1.
Appendectomy by year (NIS, age ≥65 years, 1998–2009).
Figure 2.
Proportion appendectomy performed laparoscopically by year (NIS, age ≥65 years, 1998–2009).
Demographic Data
Elderly patients undergoing LA were significantly younger, were more likely to be white, had lower Charlson comorbidity scores, were more likely to undergo surgery in urban hospitals, and were less likely to have a ruptured appendix; they were also marginally significantly more likely to have private insurance and undergo surgery at nonteaching hospitals (Table 2).
Table 2.
Demographic Data
| Open (n = 170 276) | Laparoscopy (n = 87 209) | P Value | |
|---|---|---|---|
| Agea (mean ± SE) (y) | 74.09 ± 0.04 | 73.16 ± 0.05 | < .001b |
| Sex (male/female)b | 48.3%/51.7% | 48.1%/51.9% | .6604 |
| Racec | < .001d | ||
| White | 105 428.3 (61.9%) | 56 730.3 (65.1%) | |
| African American | 7403.1 (4.3%) | 2662.6 (3.1%) | |
| Other | 57 444.3 (33.7%) | 27 816.4 (31.9%) | |
| Charlson index | < .001d | ||
| 0–2 | 138 916.3 (81.6%) | 78 054.8 (89.5%) | |
| ≥3 | 31 359.4 (18.4%) | 9154.5 (10.5%) | |
| Ruptured appendix/abscess of appendix | 79 574.6 (46.7%) | 33 750.4 (38.7%) | < .001d |
| Income (by ZIP code) | .3729 | ||
| <$45 000 | 118 978.2 (69.9%) | 61 608.7 (70.6%) | |
| ≥$45 000 | 51 297.5 (30.1%) | 25 600.6 (29.4%) | |
| Insurance | .0054d | ||
| Private | 18 640.4 (10.9%) | 10 575.1 (12.1%) | |
| Medicare | 146 593.7 (86.1%) | 74 204.7 (85.1%) | |
| Medicaid | 2090.1 (1.2%) | 902.0 (1.0%) | |
| Other | 2951.6 (1.7%) | 1527.6 (1.8%) | |
| Hospital type | .0890 | ||
| Nonteaching | 104 545.5 (61.5%) | 55 376.5 (63.7%) | |
| Teaching | 65 392.2 (38.5%) | 31 601.4 (36.3%) | |
| Hospital location | < .001d | ||
| Rural | 32 879.3 (19.3%) | 14 029.4 (16.1%) | |
| Urban | 137 058.3 (80.7%) | 72 948.5 (83.9%) |
P value by independent t test.
P value by Fisher exact test.
P value by χ2 test.
Significant by 2-tailed test.
Outcomes
Compared with OA, LA was associated with a decreased LOS; fewer total PSI events; a decreased total mortality rate; and a lower likelihood of failure to rescue, iatrogenic pneumothorax, infections due to medical care, postoperative respiratory failure, and postoperative pulmonary embolism or deep venous thrombosis; as well as fewer accidental punctures or lacerations (Table 3).
Table 3.
Unadjusted Outcomes
| Open (n = 170 276) | Laparoscopy (n = 87 209) | P Value | |
|---|---|---|---|
| LOS (corrected) (d) | 7.86 ± 0.06 | 4 ± 0.04 | < .001a |
| Total mortality | 4687.3/165 451.6 (2.8%) | 755/86 440 (0.9%) | < .001a |
| Any PSI | 6040.6/170 225.3 (3.5%) | 1576.7/87 118 (1.8%) | < .001a |
| Complications of anesthesia | 113.7/98 090.3 (0.1%) | 96/71 308 (0.1%) | .6264 |
| Death in low-mortality diagnosis-related groups | b | NAc | NA |
| Decubitus ulcer | 490.0/59 087.9 (0.8%) | 136/21 838 (0.2%) | .1727 |
| Failure to rescue | 885.5/5878.4 (15.1%) | 213/2139 (10.0%) | .0066a |
| Iatrogenic pneumothorax | 142.3/94 083.3 (0.2%) | 25/69 974 (0.0%) | .0013a |
| Selected infections due to medical care | 316.5/66 489.7 (0.5%) | 87/46 682 (0.2%) | .0006a |
| Postoperative hip fracture | b | b | .2089 |
| Postoperative hemorrhage or hematoma | 281.7/98 060.1 (0.3%) | 141/71 298 (0.2%) | .1114 |
| Postoperative physiologic and metabolic derangements | 41.6/20 151.7 (0.2%) | 11/8100 (0.1%) | .5547 |
| Postoperative respiratory failure | 731.7/19 957.1 (3.7%) | 103/8050 (1.3%) | < .001a |
| Postoperative PEc/DVTc | 1506.9/97 855.74 (1.5%) | 412/71 263 (0.6%) | < .001a |
| Postoperative sepsis | 132.0/2445.2 (5.4%) | b | .1366 |
| Postoperative wound dehiscence | 485.4/155 023.9 (0.3%) | 14/9774 (0.1%) | .1842 |
| Accidental puncture or laceration | 1651.9/9989.1 (1.7%) | 472/71 274 (0.7%) | < .001a |
| Transfusion reaction | b | NA | NA |
Significant by 2-tailed test.
The number of events was 10 or fewer.
DVT = deep venous thrombosis; NA = not applicable; PE = pulmonary embolism.
On multivariate analysis, LA was associated with a 32% reduction in the probability of any PSI (Table 4). A subgroup analysis holding each independent control fixed was performed as a measure of model sensitivity. LA was associated with a decreased odds ratio for PSI events for each subgroup included in the analysis, except Medicare versus private insurance patients because of unavoidable collinearity when limiting the analysis to age ≥65 years.
Table 4.
Logistic Regression,a Adjusted for Year
| Variable | ORb | 95% CIb |
P Value | |
|---|---|---|---|---|
| Lower | Upper | |||
| Surgery: laparoscopy (reference, open) | 0.677 | 0.588 | 0.781 | < .001 |
| Age, cont | 1.023 | 1.016 | 1.030 | < .001 |
| Sex: female (reference, male) | 0.761 | 0.685 | 0.845 | < .001 |
| Race: other (reference, white) | 0.999 | 0.892 | 1.118 | .980 |
| Charlson index: 3+ (reference, 0–2) | 2.212 | 1.963 | 2.492 | < .001 |
| Ruptured appendix/abscess of appendix | 0.955 | 0.856 | 1.065 | .409 |
| Income: ≥$45 000 (reference, <$45 000) | 1.071 | 0.941 | 1.219 | .300 |
| Insurance (reference, private) | ||||
| Medicare | 1.397 | 1.146 | 1.703 | .001 |
| Medicaid | 1.001 | 0.550 | 1.824 | .996 |
| Other | 1.730 | 1.121 | 2.671 | .013 |
| Teaching | 1.306 | 1.165 | 1.464 | < .001 |
| Location: urban (reference, rural) | 1.191 | 1.024 | 1.385 | .023 |
| Number PSI eligible, cont | 1.629 | 1.563 | 1.697 | < .001 |
The outcome was considered any PSI.
CI = confidence interval; OR = odds ratio.
DISCUSSION
To our knowledge, this is the first study in the United States to investigate perioperative outcomes of LA in the elderly using validated patient safety measures in a national population. With 257 484 patients, it is also—to our knowledge—the largest analytic sample for population-level analyses of appendectomy. We observed a 33% (odds ratio, 0.677) decreased probability of patient safety events occurring in LA cases compared with OA cases as measured by PSIs. Notably, this observation was independent of appendiceal rupture and comorbidity status and occurred during a period of rapid uptake of LA by practicing surgeons. Our results thus suggest that use of LA results in substantially enhanced perioperative patient safety as compared with OA.
This study addresses comparative patient safety analyses in the development of new technology and surgical practices. Although laparoscopic surgery has been shown to offer superior surgical outcomes for most abdominal surgical procedures,32 there is limited evidence on surgical outcomes with regard to patient safety, especially in the elderly population. Existing evidence suggests that LA is as effective as OA with a decreased likelihood of superficial wound infection, a decreased need for postoperative analgesics, and a quicker return to preoperative functional status.3,4 Substantially less research, however, has focused on the elderly population; moreover, although these outcomes may be appropriate measures for younger patients, additional comparative measures are necessary to ensure patient safety in the context of novel surgical techniques and assess quality-improvement efforts.22 Because PSIs measure preventable medical injuries, they are useful metrics for assessing the safety of surgical innovations in populations. It is unclear why OA was associated with an increased risk of preventable medical injuries in elderly patients in the NIS. However, because most of the specific PSIs associated with OA are associated with postoperative morbidity—including iatrogenic pneumothorax, postoperative respiratory failure, and postoperative deep venous thrombosis—it is possible that the longer inpatient convalescence of OA contributed to a greater risk of injury.
Our results are consistent with most prior studies of LA in the elderly, which involved smaller analytic cohorts and focused on patient-driven measures rather than process-driven measures. A review of the National Surgical Quality Improvement Project database showed that OA yielded higher rates of both major and minor postoperative complications than the laparoscopic cases (P < .0001) in the elderly—both overall and before discharge. Multivariate analysis showed no association between operative approach and major complications, as well as a reduced risk of minor complications with laparoscopy and a shorter hospital stay than with OA.23 Another report compared LA and OA in terms of LOS, charges, complications, discharge location, and mortality rate in elderly patients treated for appendicitis in North Carolina over a 6-year period.14 They found that LA was associated with reductions in the mortality rate (0.38% vs 2.08%, P = .007), complication rate (16.3% vs 20.8%, P = .01), and LOS (4.64 days vs 7.29 days, P = .0001) and an increase in the proportion of routine discharges to home (91.4% vs 78.9%, P = .0001) when compared with OA. Similarly, a relatively small case series (N = 150) observed that LA patients had shorter hospital stays (measured in days) and lower rates of postoperative ventilator dependence than OA patients,24 whereas a population-based study in Taiwan concluded that patients aged older than 65 years benefited from LA with respect to LOS.25 In contrast, in a retrospective review of patients who underwent LA comparing those aged ≥60 years with those aged <60 years, complicated appendicitis and conversions were more frequent in the elderly patients, resulting in prolonged operative times and longer hospital stays. Moreover, the overall complication rate was statistically equivalent between the groups, as were the prevalence rates of infectious or surgical-site complications.33
We included only patients aged ≥65 years in this study. It is possible, however, that the mean age of patients undergoing LA increased during the period of study as surgeons became more likely over time to offer LA to older patients. We therefore corrected for evolving indications for LA by including year as a covariate in the regression modeling to reduce potential bias. In addition, the difference in age between the open and laparoscopy groups, though statistically significant, was quite modest: <1 year separated groups, which was likely clinically insignificant (Table 2).
The notable strengths of our study include the large size of the analytic cohort and models that adjusted for comorbidity status, appendiceal rupture, and appendiceal abscess—clinical variables that could potentially bias the selection of surgical techniques for individual patients. The potential limitations also merit discussion. First, intent-to-treat analysis was not possible because data regarding conversion of laparoscopic cases to open cases were not available. Second, patient safety events occurring after hospital discharge could not be measured, nor could the duration of symptoms before hospital admission. Third, despite inclusion of multiple covariates in the regression analyses, the potential existed for residual confounding by complicated appendicitis, which occurred more often among OA patients. Finally, it is important to note that, although PSIs identify potential systems errors, they do not provide detailed root-cause analyses. Root-cause analyses are best performed through in-depth reviews of clinical records.21,34
CONCLUSION
LA is associated with substantially enhanced perioperative patient safety compared with OA in the elderly. The data also suggest that the diffusion of LA into clinical practice is not associated with an increased risk of adverse safety events.
Contributor Information
Nicholas T. Ward, Department of Surgery, UC San Diego Health System, San Diego, CA, USA..
Sonia L. Ramamoorthy, Department of Surgery, UC San Diego Health System, San Diego, CA, USA..
David C. Chang, Department of Surgery, UC San Diego Health System, San Diego, CA, USA..
J. Kellogg Parsons, Department of Surgery, UC San Diego Health System, San Diego, CA, USA.; Department of Urology, UC San Diego Health System, San Diego, CA, USA. VA San Diego Healthcare System, San Diego, CA, USA.
References:
- 1. Paik PS, Towson JA, Anthone GJ, et al. Intra-abdominal abscesses following laparoscopic and open appendectomies. J Gastrointest Surg. 1997;1:188–192 [DOI] [PubMed] [Google Scholar]
- 2. Garg CP, Vaidya BB, Chengalath MM. Efficacy of laparoscopy in complicated appendicitis. Int J Surg. 2009;7:250–252 [DOI] [PubMed] [Google Scholar]
- 3. Pokala N, Sadhasivam S, Kiran RP, et al. Complicated appendicitis—Is the laparoscopic approach appropriate? A comparative study with the open approach: Outcome in a community hospital setting. Am Surg. 2007;73:737–741 [PubMed] [Google Scholar]
- 4. Long KH, Bannon MP, Zietlow SP. A prospective randomized comparison of laparoscopic appendectomy with open appendectomy: Clinical and economic analyses. Surgery. 2001;129:390–400 [DOI] [PubMed] [Google Scholar]
- 5. Ingraham AM, Cohen ME, Bilimoria KY, Pritts TA, Ko CY, Esposito TJ. Comparison of outcomes after laparoscopic versus open appendectomy for acute appendicitis at 222 ACS NSQIP hospitals. Surgery. 2010;148(4):625–635, discussion 635–637 [DOI] [PubMed] [Google Scholar]
- 6. Tiwari MM, Reynoso JF, Tsang AW, et al. Comparison of outcomes of laparoscopic and open appendectomy in management of uncomplicated and complicated appendicitis. Ann Surg. 2011;254(6):927–932 [DOI] [PubMed] [Google Scholar]
- 7. Guller U, Jain N, Peterson ED, et al. Laparoscopic appendectomy in the elderly. Surgery. 2004;135:479–488 [DOI] [PubMed] [Google Scholar]
- 8. Chung RS, Rowland DY, Li P, Diaz J. A meta-analysis of randomized controlled trials of laparoscopic versus conventional appendectomy. Am J Surg. 1999;177:250–256 [DOI] [PubMed] [Google Scholar]
- 9. McCall JL, Sharples K, Jadallah F. Systematic review of randomized controlled trials comparing laparoscopic with open appendicectomy. Br J Surg. 1997;84:1045–1050 [PubMed] [Google Scholar]
- 10. Pedersen AG, Petersen OB, Wara P, et al. Randomized clinical trial of laparoscopic versus open appendicectomy. Br J Surg. 2001;88:200–205 [DOI] [PubMed] [Google Scholar]
- 11. US Bureau of the Census, Cheeseman Day J. Current Population Reports, P25–1104. Population Projections of the United States, by Age, Sex, Race, and Hispanic Origin: 1993 to 2050. Washington, DC: US Government Printing Office; 1993 [Google Scholar]
- 12. Addiss DG, Shaffer N, Fowler BS, Tauxe RV. The epidemiology of appendicitis and appendectomy in the United States. Am J Epidemiol. 1990;132(5):910–925 [DOI] [PubMed] [Google Scholar]
- 13. Lau WY, Fan ST, Yiu TF, et al. Acute appendicitis in the elderly. Surg Gynecol Obstet. 1985;161:157–160 [PubMed] [Google Scholar]
- 14. Harrell AG, Lincourt AE, Novitsky YW, et al. Advantages of laparoscopic appendectomy in the elderly. Am Surg. 2006;72(6):474–480 [PubMed] [Google Scholar]
- 15. Podnos YD, Jimenez JC, Wilson SE. Intra-abdominal sepsis in elderly persons. Clin Infect Dis. 2002;35:62–68 [DOI] [PubMed] [Google Scholar]
- 16. Kraemer M, Franke C, Ohmann C, Yang Q. Acute appendicitis in late adulthood: incidence, presentation, and outcome. Results of a prospective multicenter acute abdominal pain study and a review of the literature. Langenbecks Arch Surg. 2000;385:470–481 [DOI] [PubMed] [Google Scholar]
- 17. Paajanen H, Kettunen J, Kostiainen S. Emergency appendectomies in patients over 80 years. Am Surg. 1994;60:950–953 [PubMed] [Google Scholar]
- 18. Gurleyik G, Gurleyik E. Age-related clinical features in older patients with acute appendicitis. Eur J Emerg Med. 2003;10:200–203 [DOI] [PubMed] [Google Scholar]
- 19. Kohn LT, Corrigan JM, Donaldson M, eds. To Err Is Human: Building a Safer Health System. Washington, DC: Institute of Medicine; 1999 [PubMed] [Google Scholar]
- 20. Zhan C, Miller MR. Excess length of stay, charges, and mortality attributable to medical injuries during hospitalization. JAMA. 2003;290:1868–1874 [DOI] [PubMed] [Google Scholar]
- 21. Chang DC, Handly N, Abdullah F, et al. The occurrence of potential patient safety events among trauma patients: are they random? Ann Surg. 2008;247(2):327–334 [DOI] [PubMed] [Google Scholar]
- 22. Rhee D, Zhang Y, Chang DC, et al. Population-based comparison of open vs laparoscopic esophagogastric fundoplication in children: application of the Agency for Healthcare Research and Quality pediatric quality indicators. J Pediatr Surg. 2011;46(4):648–654 [DOI] [PubMed] [Google Scholar]
- 23. Kim MJ, Fleming FJ, Gunzler DD, et al. Laparoscopic appendectomy is safe and efficacious for the elderly: an analysis using the National Surgical Quality Improvement Project database. Surg Endosc. 2011;25(6):1802–1807 [DOI] [PubMed] [Google Scholar]
- 24. Wu SC, Wang YC, Fu CY, et al. Laparoscopic appendectomy provides better outcomes than open appendectomy in elderly patients. Am Surg. 2011;77(4):466–470 [PubMed] [Google Scholar]
- 25. Yeh CC, Wu SC, Liao CC, Su LT, Hsieh CH, Li TC. Laparoscopic appendectomy for acute appendicitis is more favorable for patients with comorbidities, the elderly, and those with complicated appendicitis: a nationwide population-based study. Surg Endosc. 2011;25(9):2932–2942 [DOI] [PubMed] [Google Scholar]
- 26. Coffey RM, Barrett M, Houchens B, et al. Methods Applying AHRQ Quality Indicators to Healthcare Cost and Utilization Project (HCUP) Data for the Sixth National Healthcare Quality Report. Rockville, MD: Agency for Healthcare Research and Quality; 2008 [Google Scholar]
- 27. Department of Health and Human Services, Agency for Healthcare Research and Quality. AHRQ Quality Indicators: Software Documentation. Version 4.1a for Windows. Rockville, MD: Agency for Healthcare Research and Quality; 2010 [Google Scholar]
- 28. Agency for Healthcare Research and Quality. AHRQ Quality Indicators—Guide to Patient Safety Indicators. Version 3.1. Rockville, MD: Agency for Healthcare Research and Quality; 2007 [Google Scholar]
- 29. Karson AS, Bates DW. Screening for adverse events. J Eval Clin Pract. 1999;5(1):23–32 [DOI] [PubMed] [Google Scholar]
- 30. Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45:613–619 [DOI] [PubMed] [Google Scholar]
- 31. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383 [DOI] [PubMed] [Google Scholar]
- 32. Kirshtein B, Perry ZH, Mizrahi S, et al. Value of laparoscopic appendectomy in the elderly patient. World J Surg. 2009;33(5):918–922 [DOI] [PubMed] [Google Scholar]
- 33. Gruen RL, Jurkovich GJ, McIntyre LK, et al. Patterns of errors contributing to trauma mortality: lessons learned from 2,594 deaths. Ann Surg. 2006;244:371–380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Tiwari MM, Reynoso JF, High R, Tsang AW, Oleynikov D. Safety, efficacy, and cost-effectiveness of common laparoscopic procedures. Surg Endosc. 2011;25(4):1127–1135 [DOI] [PubMed] [Google Scholar]