Abstract
Background and Objectives:
The single-incision approach in laparoscopic surgery is a relatively new concept. This systematic review of the literature was performed to appraise the existing clinical evidence concerning the use of the single-incision technique for spleen resection.
Methods:
We performed a systematic search of the PubMed and Scopus databases, and the studies retrieved were included in our review. The references of the included studies were also hand searched.
Results:
Thirty-one relevant studies were found in the field including 81 patients with an age range from 0.6 to 90 years and a body mass index range from 18 to 36.7 kg/m2. Splenomegaly (44.6%), idiopathic thrombocytopenic purpura (31%), and immune thrombocytopenic purpura (6.8%) were the most common indications for the procedure. Concerning the applied port system, multiple single ports (5 to 12 mm) were used in 54.4% of patients, the SILS port (Covidien, Mansfield, Massachusetts) was used in 26.6%, the TriPort (Advanced Surgical Concepts, Wicklow, Ireland) was used in 7.6%, glove ports were used in 6.3%, and the GelPort (Applied Medical, Rancho Santa Margarita, California) was used in 5.1%. The median operative time was 125 minutes (range, 45–420 minutes), and the median quantity of blood loss was 50 mL (range, 10–450 mL). No conversion to open surgery and no transfusion were needed. The length of hospital stay was between 1 and 9 days. Low rates of complications and no patient deaths were found. The existing evidence on cosmesis is limited.
Conclusion:
Single-site/single-port laparoscopic surgery is a minimally invasive procedure that seems to be a challenging alternative in the management of spleen resection.
Keywords: Single incision, Splenectomy, Laparoendoscopic single site
INTRODUCTION
Current advances in surgical minimally invasive techniques have trended mainly toward two directions: natural orifice transluminal endoscopic surgery and laparoendoscopic single-site surgery. Both can be accomplished with the use of ordinary laparoscopic instruments without a significant increase in surgical costs, and they are also evolving to include a more acceptable scarless surgical technique.1 Since the era of Georg Kelling's first laparoscopic operation in dogs in 1902 and of Hans Christian Jacobaeus' first laparoscopic operation in humans in 1910, laparoscopic procedures have been developed to become a safe surgical approach in common use.2 In 1991 laparoscopic splenectomy was performed for the first time at Royal Brisbane Hospital.3 Nowadays, laparoscopic splenectomy is a conventional procedure in everyday surgical practice in the hands of well-trained surgeons. Technical improvements in the field of single-incision laparoscopic surgery have permitted the realization of single-incision laparoscopic splenectomy (SILS), further pushing the limits of minimally invasive surgery.
The objective of this review is to present the clinical data presently available regarding the application of SILS in cases of clinical syndromes in which splenectomy is judged an essential method of treatment.
METHODS
Data Sources
We performed a systematic search of PubMed (June 6, 2013) and Scopus (June 6, 2013). The applied search strategy, in both the PubMed and Scopus databases, included the combination of the following key words: single incision AND (laparoscopic OR laparoendoscopic OR robotic) AND splenectomy. The references of the included articles were also hand searched.
Study Selection Criteria
Studies reporting data on SILS were included in this review. Conference papers, abstracts, letters to the editor, and animal studies were excluded. Studies published in the English, German, Greek, French, Italian, or Spanish language were included in this review.
Definitions
Studies with ≤9 patients were considered case reports to include greater numbers of patients.
RESULTS
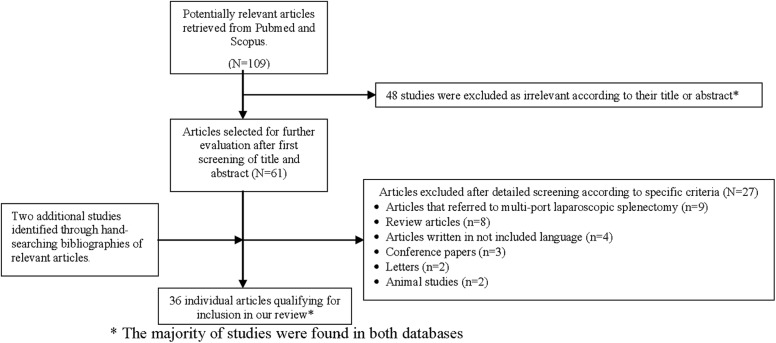
Our search of PubMed and Scopus retrieved 47 studies and 62 studies, respectively, among which 34 studies (29 case reports and 5 case series) met the inclusion criteria of our systematic review.1–34 Two additional studies were included through hand searching of references.35,36 The adopted search strategy is schematically presented in Figure 1.
Figure 1.
Flow diagram of selection process for articles included in review.
Case Reports of SILS
The most important characteristics of the studies included in this review (demographic data, medical history, clinical features of SILS performed, operative parameters, outcomes) are shown in Table 1. A total of 81 patients were included in our study. The patients' ages ranged from 0.6 to 73 years. Most of the patients were female (46 of 81, 56.8%). Most of the patients had comorbidities (57 of 81, 70.4%), such as thrombocytopenia, sickle cell anemia, β-thalassemia intermedia, and hepatitis B. The median body mass index (BMI) of the included patients was 23 kg/m2 (range, 18–35.7 kg/m2). Splenomegaly (33 of 74, 44.6%), idiopathic thrombocytopenic purpura (23 of 74, 31%), immune thrombocytopenic purpura (5 of 74, 6.8%), lymphomas (5 of 74, 6.8%), splenic cysts (4 of 74, 5.4%), traumatic rupture (2 of 74, 2.8%), hydatid cyst (1 of 74, 1.3%), and multiple splenic abscesses (1 of 74, 1.3%) were the most common indications for SILS. Partial splenectomy was performed in only 2 cases (2.5%). After our literature search, no restrictions apart from the high BMI were found regarding the patients approached by the SILS technique. The patients were positioned in either the semilateral (49 of 79, 62%) or lateral (30 of 79, 38%) position. The most frequent surgical approach was umbilical (57 of 81, 70.4%), whereas periumbilical (17 of 81, 21%), supraumbilical (5 of 81, 6.1%), and left upper quadrant (2 of 81, 2.5%) approaches were also common. The median weight of the resected spleen was 446 g (range, 125–590 g). Regarding the port system used, 2 or 3 single ports (5- to 12-mm trocars) were applied in 43 of 79 patients (54.4%), the SILS port (Covidien, Mansfield, Massachusetts) was used in 21 (26.6%), the TriPort (Advanced Surgical Concepts, Wicklow, Ireland) was used in 6 (7.6%), glove ports were used in 5 (6.3%), and the GelPort (Applied Medical, Rancho Santa Margarita, California) was used in 4 (5.1%). The size of the incision varied from 10 to 35 mm.
Table 1.
Characteristics and Outcomes of Patients After SILS
| Data | |
|---|---|
| Demographic data | |
| Age [median (range)] (y) | 23 (0.6–73) |
| Male sex | 35 of 81 (43.2) |
| Medical history | |
| Presence of comorbidities | 57 of 81 (70.4) |
| BMI [median (range)] (kg/m2) | 23 (18–35.7) |
| Clinical features of SILH performed | |
| Diagnosis | |
| Splenomegaly | 33 of 74 (44.6) |
| Idiopathic thrombocytopenic purpura | 23 of 74 (31) |
| Immune thrombocytopenic purpura | 5 of 74 (6.8) |
| Lymphomas | 5 of 74 (6.8) |
| Splenic cysts | 4 of 74 (5.4) |
| Traumatic rupture | 2 of 74 (2.8) |
| Hydatid cyst | 1 of 74 (1.3) |
| Multiple splenic abscesses | 1 of 74 (1.3) |
| Type of splenectomy | |
| Partial splenectomy | 2 of 81 (2.5) |
| Patient position | |
| Semilateral | 49 of 79 (62) |
| Lateral | 30 of 79 (38) |
| Surgical approach | |
| Umbilical | 57 of 81 (70.4) |
| Periumbilical | 17 of 81 (21) |
| Supraumbilical | 5 of 81 (6.1) |
| Left upper quadrant | 2 of 81 (2.5) |
| Weight of spleen [median (range)] (g) | 446 (125–590) |
| Operative parameters | |
| Port system applied | |
| 2 or 3 single ports (5- to 12-mm trocars) | 43 of 79 (54.4) |
| SILS port | 21 of 79 (26.6) |
| TriPort | 6 of 79 (7.6) |
| Glove port | 5 of 79 (6.3) |
| GelPort | 4 of 79 (5.1) |
| Size of incision [median (range)] (mm) | 22 (10–35) |
| Outcomes | |
| Operative time [median (range)] (min) | 125 (45–420) |
| Blood loss [median (range)] (mL) | 50 (10–450) |
| Conversions | 4 of 81 (4.9) |
| Transfusion needed | 11 of 81 (13.6) |
| Hospital stay [median (range)] (d) | 3 (1–9) |
| Complications | 6 of 81 (7.4) |
| Death | 0 of 81 |
| Positive cosmesis | 42 of 81 (51.8) |
Data are presented as number (percent) unless otherwise indicated.
The median operative time was 125 minutes (range, 45–420 minutes), and the median quantity of blood loss was 50 mL (range, 10–450 mL). In 4 of 81 cases (4.9%), conversion to either open or multi-port laparoscopic surgery was necessary, and transfusions were needed in 11 cases (13.6%). The duration of hospital stay was between 1 and 9 days. Complications related to splenectomy (eg, bleeding) were present in 6 of 81 patients (7.4%). The complications retrieved from the included case reports comprised 3 cases of bleeding (3 of 81, 3.7%), 1 case of intra-abdominal hematoma (1 of 81, 1.2%), 1 case of wound infection (1 of 81, 1.2%), and 1 case of incidental gastric wall injury (1 of 81, 1.2%). No patient deaths were reported. Of 81 patients, 42 (51.8%) had a positive opinion regarding cosmesis after the application of the single-incision laparoscopic technique for splenectomy.
Case Series of SILS
We identified 5 case series that included 58 patients who underwent resection of the spleen by the single-incision laparoscopic method (Table 2).7,9,22,23,26 Most of the case series referred to an adult population (4 of 5) with patients aged between 24 and 73 years. Only 1 study was performed in children (median age, 7 years; age range, 1–15 years). Of the 5 studies, 3 mentioned the BMI of the patients, which varied between 18.9 and 35.1 kg/m2. Immune thrombocytopenic purpura, spherocytosis, and malignancy were the most common diagnoses. Five different types of port systems were applied in the 5 different studies included (GelPOINT (Applied Medical, Rancho Santa Margarita, CA, USA), OCTO port (Dalim Corporation, Seoul, South Korea)/glove port QuadPort (Advanced Surgical Concepts, Bray, Ireland), SILS port (Covidien, Norwalk, CT, USA) and 3 ports/multi-access single port). The weight of the resected spleen varied between 20.7 and 866.5 g. The size of the incision in the SILS procedures ranged from 15 to 40 mm. The duration of the procedure was between 40 and 378 minutes, and the overall amount of blood loss was between 0 and 378 mL. Conversion to an open procedure because of bleeding occurred in only 2 cases. In 4 of 58 patients (6.9%) the transfusion of blood or blood derivatives was necessary. The length of hospital stay was between 1 and 9 days. Complications related to SILS were reported in 6 of 58 patients (10.3%), comprising bleeding (3 of 58, 5.2%), pneumonia (1 of 58, 1.7%), deep vein thrombosis (1 of 58, 1.7%), and severe epistaxis (1 of 58, 1.7%). The final cosmesis of the surgical wounds was evaluated in only 1 study; the difference between the single-incision group and the classical laparoscopic group was statistically significant.
Table 2.
Main Characteristics and Outcomes of Patients After SILS in Published Case Series
| Author, Year, Country | Publication Type | No. of Patients | Age of Patients (y) | BMI (kg/m2) | Diagnosis | Port System Applied in SILSa | Weight of Spleen (g) | Size of Incision in SILS (mm) | Duration of Procedure (min) | Blood Loss (mL) | Conversions (%) | Transfusion Needed | Hospital Stay (d) | Complications | Cosmesis |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Boone et al,7 2013, USA | Retrospective, comparative study | LSa: 18 of 26 (69.2%), SILS: 8 of 26 (30.7%) | LS: 49.3 ± 16.6 (mean ± SD), SILS: 51.4 ± 21.6 (mean ± SD), P = .81 | LS: 26.9 ± 5.5 (mean ± SD), SILS: 27 ± 8.1 (mean ± SD), P = .98 | LS: myeloproliferative disorder in 8 of 26 (30.7%), ITPa in 6 of 26 (23%), hemolytic anemia in 2 of 26 (7.7%), splenic cyst in 1 of 26 (3.8%), splenic infarction in 1 of 26 (3.8%); SILS: myeloproliferative disorder in 3 of 26 (11.5%), ITP in 2 of 26 (7.7%), hemolytic anemia in 2 of 26 (7.7%), splenic cyst in 1 of 26 (3.8%) | GelPOINT | LS: 473.8 ± 331.8 (mean ± SD), SILS: 422.9 ± 443.6 (mean ± SD), P = .77 | 40 | LS: 185.9 ± 76.6 (mean ± SD), SILS: 101.6 ± 31.2 (mean ± SD), P = .003 | LS: 398.1 ± 494.3 (mean ± SD), SILS: 78.9 ± 68.2 (mean ± SD), P = .25 | LS: 5 of 26 (19.2%), SILS: 0 of 26 | LS: 6 of 26 (23%), SILS: 2 of 26 (7.7%) | LS: 5.1 ± 2.5 (mean ± SD), SILS: 4.4 ± 2.8 (mean ± SD), P = .51 | LS: 5 of 26 (19.2%), SILS: 2 of 26 (7.7%) | NRa |
| Choi et al,9 2013, South Korea | Retrospective, comparative study | LS: 18 of 34 (53%), SILS: 16 of 34 (47%) | LS: 45.8 ± 20.2 (mean ± SD), SILS: 51.7 ± 12.7 (mean ± SD), P > .99 | LS: 22.93 ± 2.59 (mean ± SD), SILS: 25.02 ± 4.17 (mean ± SD), P = .422 | LS: ITP in 11 of 34 (32.3%)b; SILS: ITP in 9 of 34 (26.5%)b | OCTO port/glove port | LS: 132.29 ± 72.84 (mean ± SD), SILS: 80.27 ± 38.49 (mean ± SD), P = .109 | 30 | LS: 88.94 ± 21.68 (mean ± SD), SILS: 95.06 ± 32.35 (mean ± SD), P = .603 | LS: 206.25 ± 142.45 (mean ± SD), SILS: 111.11 ± 99.58 (mean ± SD), P = .047 | LS: 0 of 34, SILS: 0 of 34 | LS: 1 of 34 (3%), SILS: 1 of 34 (3%) | LS: 4.67 ± 2.72 (mean ± SD), SILS: 5.13 ± 1.67 (mean ± SD), P = .564 | LS: 2 of 34 (5.9%), SILS: 1 of 34 (3%) | NR |
| Perger et al,26 2013, USA | Prospective, comparative study | LS: 14 of 30 (47%), SILS: 16 of 30 (53%) | LS: 7 (2–17) [median (range)], SILS: 7 (1–15) [median (range)], P = .44 | NR | LS: spherocytosis in 6 of 30 (20%), sickle cell disease in 5 of 30 (17%), ITP in 3 of 30 (10%); SILS: spherocytosis in 8 of 30 (27%), sickle cell disease in 4 of 30 (13%), ITP in 3 of 30 (10%), autoimmune hemolytic anemia in 1 of 30 (3%) | QuadPort | LS: 229 (62–1145) [median (range)], SILS: 169 (49–536) [median (range)], P = .86 | 15 | LS: 99 (51–154) [median (range)], SILS: 84 (40–190) [median (range)], P = .89 | LS: 10 (5–60) [median (range)], SILS: 10 (5–600) [median (range)], P = .61 | LS: 1 of 30 (3%), SILS: 2 of 30 (6%) | NR | LS: 2 (1–5) [median (range)], SILS: 2 (1–8) [median (range)], P = .2 | LS: 2 of 30 (6%), SILS: 3 of 30 (7%) | NR |
| Monclova et al,23 2013, Spain | Prospective, comparative study | LS: 14 of 32 (43.8%), SILS: 8 of 32 (25%), RPASa: 10 of 32 (31.2%) | LS: 55 ± 18 (mean ± SD), SILS: 50 ± 19 (mean ± SD), RPAS: 41 ± 13 (mean ± SD), P = NSa | LS: 28 ± 5 (mean ± SD), SILS: 25 ± 4 (mean ± SD), RPAS: 24 ± 4.5 (mean ± SD), P = NS | LS: ITP in 13 of 14 (93%), autoimmune hemolytic anemia in 1 of 14 (7%); SILS: ITP in 3 of 8 (37.5%), spherocytosis in 2 of 8 (25%), malignancy in 3 of 8 (37.5%); RPAS: ITP in 8 of 10 (80%), autoimmune hemolytic anemia in 1 of 10 (10%), malignancy in 1 of 10 (10%) | 3 ports/multi-access single port | LS: 212 ± 127 (mean ± SD), SILS: 394 ± 153 (mean ± SD), RPAS: 230 ± 87 (mean ± SD), P = .02 | NR | LS: 83 ± 19 (mean ± SD), SILS: 131 ± 43 (mean ± SD), RPAS: 81 ± 22 (mean ± SD), P = .01 | NR | LS: 0 of 14, SILS: 0 of 8, RPAS: 0 of 10 | LS: 1 of 14 (7%), SILS: 1 of 8 (12.5%), RPAS: 0 of 10, P = NS | LS: 5 ± 3 (mean ± SD), SILS: 4 ± 2 (mean ± SD), RPAS: 3 ± 2 (mean ± SD), P = NS | NR | Body Image Indexc—LS: 7.3 ± 2.8, SILS: 5.8 ± 1.3, RPAS: 5.1 ± 0.4, P < .02 |
| Misawa et al,22 2011, Japan | Prospective study | 10 | 53 (24–66) [median (range)] | NR | ITP in 3 of 10 (30%), liver cirrhosis in 2 of 10 (20%), splenic aneurysm in 2 of 10 (20%), splenic simple cyst in 1 of 10 (10%), epithelial cyst in 1 of 10 (10%), splenic tumor in 1 of 10 (10%) | SILS port | 260 (100–580) [median (range)] | 20 | 230 (150–378) [median (range)] | 15 (0–100) [median (range)] | 1 of 10 (10%) | NR | 6.8 ± 2.3 (mean ± SD) | 0 of 10 | NR |
ITP = immune thrombocytopenic purpura; LS = laparoscopic splenectomy; NR = not referred; NS = not statistically significant; RPAS = reduced–port access splenectomy; SILS = single–port access splenectomy.
The remaining 13 patients had the following diagnoses: autoimmune hemolytic anemia, angiosarcoma, simple cyst, pseudocyst, diffuse large B-cell lymphoma, hemangioma, histiocytic sarcoma, inflammatory pseudotumor, metastatic lung adenocarcinoma, metastatic clear-cell ovarian carcinoma, sclerosing angiomatoid nodular transformation, lymphoid follicular hyperplasia associated with systemic lupus erythematosus, and vascular malformation.
The Body Image Index ranges from 4 (lowest) to 20 (highest).
Surgical Technique
In most of the published literature, the surgical technique applied during SILS had several characteristics in common. The surgeon's position is between the patient's open legs, the patient is in the reverse Trendelenburg position, and the monitor is on the patient's left side. An umbilical or periumbilical vertical incision of 12 to 40 mm can be used, and the fascia is exposed while 2 absorbable stay sutures are applied to it. A high-definition camera, 2 assistant ports, and an insufflator cannula through a single-port device can be safely and easily inserted into the abdominal cavity through the incision by use of a Mayo-Guyon clamp. Pneumoperitoneum is induced by carbon dioxide insufflation through the specific single-port cannula, at a constant pressure of < 10 to 12 mm Hg to prevent gas embolism. A high-definition 30° laparoscope with a diameter of 5 to 10 mm can be inserted throughout the single-port device, and the rest of the instruments are introduced under vision. Subsequently, the patient is adjusted into a semilateral or lateral position to expose the spleen. The splenogastric ligaments, as well as the short gastric vessels, can then be opened to render the splenic hilum visible. The splenic artery is clamped and dissected with the use of an endoscopic stapler. Afterward, with the use of an intestinal retractor on the lower pole of the spleen, the splenophrenic, splenorenal, and splenocolic ligaments can be dissected with the use of bipolar forceps and harmonic shears (Ethicon Endo-Surgery, Cincinnati, Ohio). At this moment, the spleen is entirely free of its attachments. The resected specimen is extracted, in a plastic bag, from the abdominal cavity through the umbilical hole after removal of the single-port device. In cases in which the spleen has large dimensions, it can undergo morcellation with Péan forceps. A single drain may be placed at the splenic flexure; it comes out from the abdominal cavity through the umbilical incision. Careful hemostasis is achieved, and both the fascia and skin are closed individually.
DISCUSSION
With the development of minimally invasive techniques surgeons are shifting from performing major invasive techniques for traditional open surgery to “scarless surgery.” In the past 10 years, technical problems, such as the lack of articulating instruments, the absence of specifically designed single-port systems, instrumental crowding and clashing, and decreased visualization, as well as the absence of triangulation between instruments, have restrained the broad use of the single-port surgical technique.
At present, several different types of port systems are available. Generally, either single-channel or multichannel port devices, including the GelPort, the SILS port, the TriPort, and common single surgical ports (5- to 12-mm trocars; Kanger, Tong Lu, China), are used. More specifically, the GelPort system consists of a surgical wound retractor with a plastic inner ring joined to an outer ring with a clear cover that can be used in fascial incisions between 15 and 70 mm. Its principal advantage is that it can be applied in patients with deep abdominal walls (>10 cm).37 The SILS port is a flexible port system that requires an incision of 18 to 30 mm and can be easily placed; in addition, 1 to 3 instruments can be collocated at the same time through a single incision. The TriPort system comprises one 12-mm port and two 5-mm ports and requires fascial incisions from 12 to 25 mm. The TriPort system is another multichannel system that has the capacity to maintain pneumoperitoneum. The wide range of angles at the various ports reduces the crowding of instruments. Nevertheless, the main disadvantage is that this system can be used at a maximum depth of 10 cm. Moreover, the use of single laparoscopic ports with the use of traditional wound retractors has no limitation with regard to the diameter of the applied ports and the dimension of the single incision. The major advantage of this method is that it enables greater manipulation of the instruments because the location of the ports can be variable. However, the removal of resected specimens necessitates a new fascial incision, permitting the loss of pneumoperitoneum. Lastly, the application of surgical gloves as a port in comparison with the single-port technique has an extremely lower cost and can easily be achieved.18 The glove port technique guarantees the surgeon more freedom regarding the mobility of the instruments, even though manipulation of the surgical specimens is more difficult compared with the standard multiport approach.
The potential benefits of single-port surgery include a shorter hospital stay, decreased morbidity, less postoperative pain, and cosmetic advantages. The patient's body type can affect the choice of the single-port system used, as well as the selection of the single-port incision area. One of the most common motives for conversion to open laparotomy is bleeding that cannot be controlled otherwise. The rate of conversion in the studies included in this review was relatively low, most likely because of the limited number of included patients and possibly because of the innovation of the technique; that is, the surgeons were more conservative regarding the management of complications. Alternatively, the published rates of conversion for various laparoscopic operations are considered relatively low.38 The findings related to the single-port technique are comparable with the quite low incidences of complications and deaths after traditional laparoscopy.39
Although the continuous technical development is unique in the field of both port systems and laparoscopic instruments, there are some technical issues during single-port operations that should be taken into consideration. The effects of instrument crowding, as well as the absence of triangulation, are among the most common technical issues.11,27 Consequently, the variety of movements is limited because of the proximity of the instruments. This issue can be resolved by various means. Initially, the surgeon can just cross the instruments. However, this can cause counterintuitive movements as the surgeon manipulates the instruments on the reverse side of the surgical field. According to the literature search, the use of surgical ports with a large outer cap (Alexis® wand protector/retractor, at GelPOINT platform, Applied Medical Rancho Santa Margarita, CA, USA) can increase the instrument distance. Finally, in conventional laparoscopy, the effect of triangulation limits significantly the movements of the instruments, while the rigid structure and respective ports can offer only a minimal flexibility. Alternatively, the presence of a single port for both the camera and the laparoscopic instruments reduces the effect of triangulation. Nevertheless, the presence of proximally curved coaxial instruments with double bending (S-Portal curved instruments; Karl Storz, Tuttlingen, Germany) permits the crossing over of instruments and allows their apposite triangulation.
In two of the included studies, SILS was also applied in the treatment of splenic trauma.35,36 In patients with blunt trauma of the spleen, there are many risk factors that make splenectomy obligatory (Injury Severity Score [≥20], high grade of splenic injury [grade III or more], presence of hemoperitoneum in ≥2 recesses, low Glasgow Coma Scale score). Often, an open surgical procedure or at least a traditional multiport laparoscopic approach is selected so as to have a better overall view of the abdominal cavity. The use of a single-port technique in the management of splenic trauma may be so valuable that permits to the surgeon to perform the most beneficial for the patient treatment (Splenectomy) with the least possible surgical trauma (Minimally Invasive Technique).40
Among the included studies in this review, there is no evidence regarding the learning curve for the single-port procedure. Although the data on the surgeons' training or experience are not sufficient, all of them should have had training and experience in advanced multiport laparoscopy to be able to complete such a technically demanding operation. For this reason, it is necessary to develop training programs that unite the application of simulators with animal or cadaveric models so as to familiarize particularly the trainees with SILS. Furthermore, it is recommended that before a surgeon gains sufficient experience in performing SILS, he or she should avoid performing either partial spleen resection or splenectomy as a result of blunt trauma to the spleen, at least in the beginning.
The use of the single-port technique also has some patient-related limitations. The use of the umbilicus as the entry point for the single port restricts the number of patients who can be deemed appropriate candidates for SILS because of the patients' BMI. According to the literature search, this restriction can be bypassed with the use of 8-mm ports in place of 5-mm ports as well as a camera at 30° up or down with the intention to avoid instrument crowding. In addition, the use of flexible endoscopes may increase the intra-abdominal visualization of the surgical field.41 An additional weakness of the technique is the fact that manipulation of the laparoscopic instruments can possibly create gas leakage from the entry point of the port system, decreasing the least required pneumoperitoneum necessary in order to carry out the entire operation.
Some limitations should be taken into consideration when analyzing the results of this study. A review of SILS with a limited number of cases is difficult to present in concise form; however, we have combined the most important elements of this technique, which are also presented in Table 2. The small sample of included patients and the small number of included studies are indications of the fact that the use of a single-incision laparoscopic technique for spleen resection is an innovation that is on the path of continuous evolution. The possible indications and contraindications of SILS should also be clarified. In addition, one could raise the idea that splenectomy is a procedure less needed in surgical practice nowadays; however, it is still used especially in patients with splenic ruptures caused by trauma, patients with hematologic disorders, or patients undergoing debulking procedures for cancer. For this reason, SILS is suggested as an alternative to the traditional methods. Regarding the cost analysis for this technique, there are not enough data to perform such an analysis. We did not perform a cost comparison among the various ports that are commercially available because there are differences in either the current price or value added tax in the various countries, which makes such a comparison difficult. In addition, randomized controlled trials with better methodologic quality are essential not only to standardize the SILS procedure but also to compare the complication rates between the multi-port and open surgical methods. Finally, with regard to our search strategy, although it had a broad range, it may be considered restricted because of the exclusion of letters, conference papers, abstracts, animal studies, and editorials.
CONCLUSION
Single-site/single-port laparoscopic surgery is gaining popularity. The development of the existing port technology may be able to present SILS as a common practice procedure in the near future. The low morbidity rate, reduced length of hospitalization, and good cosmetic outcome are some of the clear benefits of such a minimal access technique. An additional decrease in the operating time is expected as surgeons gain more experience and confidence, and new and more delicate instruments may overcome ergonomic difficulties. The standard way of reporting on laparoscopic complications is lacking; before firm conclusions can be drawn regarding the advantages of single-incision splenectomy over laparoscopic splenectomy, a well-balanced prospective cohort study with long-term follow-up is required. Moreover, with the intention of better defining the limits of SILS, further studies with a better methodologic setup are required.
Contributor Information
Ioannis D. Gkegkes, First Department of Surgery, General Hospital of Attica “KAT,” Athens, Greece..
Sarantis Mourtarakos, Department of Surgery, Korinthos General Hospital, Corinth, Greece..
Christos Iavazzo, Gynaecological Oncology Department, Royal Surrey County Hospital, Guildford, England..
References:
- 1. Fan Y, Wu SD, Siwo EA. Emergency transumbilical single-incision laparoscopic splenectomy for the treatment of traumatic rupture of the spleen: report of the first case and literature review. Surg Innov. 2011;18:185–188 [DOI] [PubMed] [Google Scholar]
- 2. Rottman SJ, Podolsky ER, Kim E, et al. Single port access (SPA) splenectomy. JSLS. 2010;14:48–52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Rhodes M, Rudd M, O'Rourke N, et al. Laparoscopic splenectomy and lymph node biopsy for hematologic disorders. Ann Surg. 1995;222:43–46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Barbaros U, Dinccag A. Single incision laparoscopic splenectomy: the first two cases. J Gastrointest Surg. 2009;13:1520–1523 [DOI] [PubMed] [Google Scholar]
- 5. Barbaros U, Sumer A, Tunca F, et al. Our early experiences with single-incision laparoscopic surgery: the first 32 patients. Surg Laparosc Endosc Percutan Tech. 2010;20:306–311 [DOI] [PubMed] [Google Scholar]
- 6. Bell R, Boswell T, Hui T, et al. Single-incision laparoscopic splenectomy in children. J Pediatr Surg. 2012;47:898–903 [DOI] [PubMed] [Google Scholar]
- 7. Boone BA, Wagner P, Ganchuk E, et al. Single-incision laparoscopic splenectomy: preliminary experience in consecutive patients and comparison to standard laparoscopic splenectomy. Surg Endosc. 2013;27:587–592 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Chinnusamy P, Ahluwalia JS, Palanisamy S, et al. Single incision multi-trocar hepatic cyst excision with partial splenectomy. J Minim Access Surg. 2013;9:91–94 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Choi KK, Kim MJ, Park H, et al. Single-incision laparoscopic splenectomy versus conventional multiport laparoscopic splenectomy: a retrospective comparison of outcomes. Surg Innov. 2013;20:40–45 [DOI] [PubMed] [Google Scholar]
- 10. Colon MJ, Telem D, Chan E, et al. Laparoendoscopic single site (LESS) splenectomy with a conventional laparoscope and instruments. JSLS. 2011;15:384–386 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Dapri G, Bron D, Himpens J, et al. Single-access transumbilical laparoscopic splenectomy using curved reusable instruments. Surg Endosc. 2011;25:3419–3422 [DOI] [PubMed] [Google Scholar]
- 12. Dapri G, Casali L, Bruyns J, et al. Single-access laparoscopic surgery using new curved reusable instruments: initial hundred patients. Surg Technol Int. 2010;20:21–35 [PubMed] [Google Scholar]
- 13. Dutta S. Early experience with single incision laparoscopic surgery: eliminating the scar from abdominal operations. J Pediatr Surg. 2009;44:1741–1745 [DOI] [PubMed] [Google Scholar]
- 14. Ergun O, Tiryaki S, Celik A. Single center experience in single-incision laparoscopic surgery in children in Turkey. J Pediatr Surg. 2011;46:704–707 [DOI] [PubMed] [Google Scholar]
- 15. Garey CL, Laituri CA, Ostlie DJ, et al. Single-incision laparoscopic surgery in children: initial single-center experience. J Pediatr Surg. 2011;46:904–907 [DOI] [PubMed] [Google Scholar]
- 16. Garrett D, Emami C, Anselmo DM, et al. Single-incision laparoscopic approach to management of splenic pathology in children: an early experience. J Laparoendosc Adv Surg Tech A. 2011;21:965–967 [DOI] [PubMed] [Google Scholar]
- 17. Hansen EN, Muensterer OJ. Single incision laparoscopic splenectomy in a 5-year-old with hereditary spherocytosis. JSLS. 2010;14:286–288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Ismail E, Akyol C, Basceken SI, et al. Glove port single-incision laparoscopic splenectomy and the treatment of its complications. Clinics (Sao Paulo). 2012;67:1519–1521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Jing K, Shuo-Dong W, Ying F. Transumbilical single-incision laparoscopy surgery splenectomy plus pericaudial devascularization in one case with portal hypertension: the first report. Surg Innov. In press 2013. December;20(6):NP21–4 [DOI] [PubMed] [Google Scholar]
- 20. Joshi M, Kurhade S, Peethambaram MS, et al. Single-incision laparoscopic splenectomy. J Minim Access Surg. 2011;7:65–67 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Malladi P, Hungness E, Nagle A. Single access laparoscopic splenectomy. JSLS. 2009;13:601–604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Misawa T, Sakamoto T, Ito R, et al. Single-incision laparoscopic splenectomy using the “tug-exposure technique” in adults: results of ten initial cases. Surg Endosc. 2011;25:3222–3227 [DOI] [PubMed] [Google Scholar]
- 23. Monclova JL, Targarona EM, Vidal P, et al. Single incision versus reduced port splenectomy—searching for the best alternative to conventional laparoscopic splenectomy. Surg Endosc. 2013;27:895–902 [DOI] [PubMed] [Google Scholar]
- 24. Oyama K, Sasaki A, Chiba T, et al. Single-incision laparoscopic splenectomy for idiopathic thrombocytopenic purpura: report of a case. Surg Today. 2011;41:1091–1094 [DOI] [PubMed] [Google Scholar]
- 25. Pedziwiatr M, Matlok M, Major P, et al. Laparoscopic surgery of the spleen through single umbilical incision. Wideochir Inne Tech Malo Inwazyjne. 2013;8:8–12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Perger L, Aprahamian CJ, Muensterer OJ, et al. Single-incision pediatric endosurgery (SIPES) splenectomy: a case-control series. J Laparoendosc Adv Surg Tech A. 2013;23:162–165 [DOI] [PubMed] [Google Scholar]
- 27. Podolsky ER, Curcillo PG, II. Single port access (SPA) surgery—a 24-month experience. J Gastrointest Surg. 2010;14:759–767 [DOI] [PubMed] [Google Scholar]
- 28. Taher R, Tawfeeq M. Single-port laparoscopic splenectomy for idiopathic thrombocytopenic purpura. Ann Saudi Med. 2011;31:655–656 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Tam YH, Lee KH, Chan KW, et al. Technical report on the initial cases of single-incision laparoscopic combined cholecystectomy and splenectomy in children, using conventional instruments. Surg Innov. 2010;17:264–268 [DOI] [PubMed] [Google Scholar]
- 30. Tam YH, Lee KH, Sihoe JD, et al. Initial experience in children using conventional laparoscopic instruments in single-incision laparoscopic surgery. J Pediatr Surg. 2010;45:2381–2385 [DOI] [PubMed] [Google Scholar]
- 31. Targarona EM, Balague C, Martinez C, et al. Single-port access: a feasible alternative to conventional laparoscopic splenectomy. Surg Innov. 2009;16:348–352 [DOI] [PubMed] [Google Scholar]
- 32. Targarona EM, Pallares JL, Balague C, et al. Single incision approach for splenic diseases: a preliminary report on a series of 8 cases. Surg Endosc. 2010;24:2236–2240 [DOI] [PubMed] [Google Scholar]
- 33. Vatansev C, Ece I, Jr. Single incision laparoscopic splenectomy with double port. Surg Laparosc Endosc Percutan Tech. 2009;19:e225–e227 [DOI] [PubMed] [Google Scholar]
- 34. Wu SD, Fan Y, Kong J, et al. Transumbilical single-incision laparoscopic splenectomy plus pericardial devascularization using conventional instruments: initial experience of 5 cases. J Laparoendosc Adv Surg Tech A. 2013;23:150–153 [DOI] [PubMed] [Google Scholar]
- 35. Hong TH, Lee SK, You YK, et al. Single-port laparoscopic partial splenectomy: a case report. Surg Laparosc Endosc Percutan Tech. 2010;20:e164–e166 [DOI] [PubMed] [Google Scholar]
- 36. You YK, Lee SK, Hong TH, et al. Single-port laparoscopic splenectomy: the first three cases. Asian J Endosc Surg. 2010;3:33–35 [Google Scholar]
- 37. Sharma A, Dahiya P, Khullar R, et al. Single-incision laparoscopic surgery (SILS) in biliary and pancreatic diseases. Indian J Surg. 2012;74:13–21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Habermalz B, Sauerland S, Decker G, et al. Laparoscopic splenectomy: the clinical practice guidelines of the European Association for Endoscopic Surgery (EAES). Surg Endosc. 2008;22:821–848 [DOI] [PubMed] [Google Scholar]
- 39. Telem D, Chin EH, Colon M, et al. Minimally invasive surgery for splenic malignancies. Minerva Chir. 2008;63:529–540 [PubMed] [Google Scholar]
- 40. Carobbi A, Romagnani F, Antonelli G, et al. Laparoscopic splenectomy for severe blunt trauma: initial experience of ten consecutive cases with a fast hemostatic technique. Surg Endosc. 2010;24:1325–1330 [DOI] [PubMed] [Google Scholar]
- 41. Jung YW, Kim SW, Kim YT. Recent advances of robotic surgery and single port laparoscopy in gynecologic oncology. J Gynecol Oncol. 2009;20:137–144 [DOI] [PMC free article] [PubMed] [Google Scholar]