Abstract
Objective
Our goal was to perform a comparative effectiveness study of intravenous (IV)-only versus IV + enteral contrast in computed tomographic (CT) scans performed for patients undergoing appendectomy across a diverse group of hospitals.
Background
Small randomized trials from tertiary centers suggest that enteral contrast does not improve diagnostic performance of CT for suspected appendicitis, but generalizability has not been demonstrated. Eliminating enteral contrast may improve efficiency, patient comfort, and safety.
Methods
We analyzed data for adult patients who underwent nonelective appendectomy at 56 hospitals over a 2-year period. Data were obtained directly from patient charts by trained abstractors. Multivariate logistic regression was utilized to adjust for potential confounding. The main outcome measure was concordance between final radiology interpretation and final pathology report.
Results
A total of 9047 adults underwent appendectomy and 8089 (89.4%) underwent CT, 54.1% of these with IV contrast only and 28.5% with IV + enteral contrast. Pathology findings correlated with radiographic findings in 90.0% of patients who received IV + enteral contrast and 90.4% of patients scanned with IV contrast alone. Hospitals were categorized as rural or urban and by their teaching status. Regardless of hospital type, there was no difference in concordance between IV-only and IV + enteral contrast. After adjusting for age, sex, comorbid conditions, weight, hospital type, and perforation, odds ratio of concordance for IV + enteral contrast versus IV contrast alone was 0.95 (95% CI: 0.72–1.25).
Conclusions
Enteral contrast does not improve CT evaluation of appendicitis in patients undergoing appendectomy. These broadly generalizable results from a diverse group of hospitals suggest that enteral contrast can be eliminated in CT scans for suspected appendicitis.
Keywords: appendicitis, comparative effectiveness, Computed tomography, diagnosis, enteral contrast, oral contrast
Acute appendicitis is the most common indication for urgent intra-abdominal surgery.1 Lifetime risk of appendicitis has been estimated at 8.6% for males and 6.7% for females.2 Given its frequency, the ability to conduct an accurate and evidence-based assessment of suspected appendicitis is crucial. The clinical imperative has been to maintain a high sensitivity so that cases of appendicitis are not missed. Historically, this was achieved by accepting a high number of false-positive diagnoses, recognized only after patients were taken to the operating room for “negative appendectomies” (NA). The underlying strategy was to prevent delays in diagnosis that could result in perforation.3 However, over the past 25 years, numerous studies have demonstrated that including imaging, especially computed tomography (CT) and ultrasound (US), into the assessment pathway for appendicitis reduces NA without increasing the frequency of perforation.4–12 CT has become commonplace in the evaluation of suspected appendicitis, and most centers report excellent results.
Technology has not remained static since the early days of CT imaging for appendicitis. Single detector scanners have given way to multidetector helical scanners, and interpretation has improved with higher-quality images produced by such advances as thin isotropic multiplanar reconstruction.13 Given these advances, investigators have begun to question whether aspects of CT scanning used in the past (eg, the use of rectal and/or oral contrast) are still necessary to achieve acceptable diagnostic accuracy.14,15 Forgoing enteral contrast may decrease time spent in the emergency department (ED), costs, and patient discomfort. To our knowledge, there are 3 small, randomized studies performed in tertiary centers that have demonstrated comparable accuracy between CT scans using only IV contrast and those performed with both IV and oral contrast.15–17 Some have expressed concern, however, that results achieved within study protocols carried out in high-volume academic centers are not applicable to other settings. Therefore, with efficacy of IV-only CT scans established, the objective of the current study was to investigate the clinical effectiveness of CT scans performed without oral contrast in a variety of settings, including academic, nonacademic, rural, suburban, and urban hospitals. Even though the risks may be minimal, when an intervention (ie, administering oral contrast) cannot be shown to provide a benefit, its use should be discontinued so that patients are not unnecessarily exposed to such harms as aspiration, allergy, or inadvertent administration of the wrong agent.
METHODS
Study Population and Setting
Consecutive adult patients were included in this prospective cohort if they underwent CT scan before nonelective appendectomy at 56 hospitals in Washington State between January 1, 2010, and December 31, 2011. The Surgical Care Outcomes and Assessment Program (SCOAP) is a physician-led quality surveillance program initiated in 2006. Recent estimates derived from the state’s abstract reporting system suggest that greater than 85% of nonelective appendectomies performed in Washington are captured by SCOAP. Participating hospitals submit data for all nonelective appendectomies. Data are collected prospectively by trained abstractors. Unlike administrative data sets in which billing codes are used to obtain information about diagnosis and treatment, SCOAP relies on direct review of clinical records. Although data are collected primarily for quality improvement, it is also a source of data for research. In 2010, the Agency for Healthcare Research and Quality funded the creation of a comparative effectiveness research platform using SCOAP data. That network—the Comparative Effectiveness Research Translation Network (CERTAIN)—developed this research study, and data collection on contrast type was added to the chart review protocol in 2010. The Washington Department of Health institutional review board approved this project. The STROBE Statement Checklist was utilized in planning and reporting this research.18
Descriptive Variables
Demographic information, clinical characteristics, radiology interpretations, operative findings, and pathology results were abstracted from each patient’s clinical record using standardized definitions. Abstracted data are audited for quality control and to verify that charts are being evaluated in a similar way across sites. A comorbidity score was calculated on the basis of documentation of the following comorbid conditions: coronary artery disease, asthma, diabetes, HIV/AIDS, diabetes, and/or elevated serum creatinine. White blood cell (WBC) count was based on the result obtained most proximal to surgery. Body mass index (BMI) was calculated from recorded height and weight at the time of the procedure. Because height is frequently not measured, body weight was used instead of BMI in the multivariate analysis.
Outcome Variables
The outcome of interest was concordance between each patient’s final radiology interpretation and the final pathology report. Positive pathology results included documented appendicitis or an appendiceal mass. Imaging results were based on the final radiologist interpretation and were reported as positive for appendicitis, negative for appendicitis, or indeterminate (definitions are given later). Imaging and pathology reports were considered concordant if imaging results were consistent with appendicitis and the pathology report was positive for disease or if imaging results were not consistent with appendicitis and pathology showed no evidence of disease. Indeterminate radiographic findings were considered discordant regardless of pathologic findings.
Because there is no standardized reporting for appendicitis on CT, abstractors use specific guidelines in evaluating whether reports should be considered positive, negative, or indeterminate. As a general rule, when faced with inconclusive language in a radiology report, abstractors are instructed to categorize as positive any report that conveys suspicion of a positive diagnosis (examples provided in the abstractor dictionary include “highly suspicious for appendicitis,” “probable appendicitis,” and “mild appendicitis”). However, when the radiology report is more circumspect, abstractors are instructed to categorize the results as “indeterminate” (examples provided include “cannot exclude appendicitis” or “possible appendicitis”). Influence of these definitions on our results was tested in a sensitivity analysis.
Statistical Analysis
Contrast regimens were categorized as [1] no contrast, [2] IV-only, [3] IV + enteral contrast (this includes IV + oral, IV + rectal, and IV + oral + rectal), and [4] enteral-only (oral, rectal, or oral + rectal). The primary comparison of interest was between IV-only and IV + enteral contrast (the decision was made to include all oral and rectal contrast into one “enteral” category because these contrast modalities work in the same way: opacification of the cecum and/or the appendix). Descriptive analysis was performed comparing clinical and demographic characteristics of those patients who received IV-only contrast to those who received IV + enteral contrast. Differences in categorical variables were evaluated for significance using the Pearson χ2 test. Student’s t test was used to compare continuous variables. Significance was set at α = 0.05.
The Washington State Department of Health classifies hospitals as “Rural” or “Urban,” and these designations were assigned to each hospital in SCOAP. Information on the presence of surgery residency programs or any residency programs was obtained from the Web site of the Accreditation Council for Graduate Medical Education (accessed July 10, 2012). Using these designations, hospital types were compared in terms of procedural volume, CT scan use, and concordance.
An unadjusted analysis was completed to compare crude odds of concordance for all contrast regimens with IV-only as the referent. Univariate logistic regression was also undertaken for clinical, demographic, and institutional characteristics; quantitative variables were included in continuous format. To adjust for potential confounding, we developed a multivariate logistic regression model. Covariates were initially considered for inclusion in this explanatory regression model if they were known from the surgical literature or from clinical experience to be associated with accuracy in diagnosing appendicitis. Only variables with significant associations in univariate analysis were included in the parsimonious final regression model. Using these a priori criteria, comorbidity score, sex, age, weight, perforation, and institution type were included as covariates. Institution type (urban academic, urban nonacademic, and rural) was initially selected as a covariate because previous studies have demonstrated that CT accuracy is lower outside of rigorously protocoled clinical trials.19–21 Patient weight was initially included because some have suggested that thin patients, with less intra-abdominal fat, may benefit from enteral contrast.14 Using a generalized estimating equation, the model was adjusted for clustering of patients by institution (ie, violations of independence). Observations with missing data were excluded from multivariate analysis. For contrast type, odds ratios (ORs) were generated with IV-only as the referent. STATA versions 10 and 12 were used for analyses (StataCorp LP, College Station, TX).
Sensitivity Analysis
As a sensitivity analysis, we recategorized all “indeterminate” CT scans as “positive” and repeated the original analyses. Because suspicion was high enough for all patients in this cohort to undergo appendectomy, many of the CT scans categorized as “indeterminate” by SCOAP may not have been viewed as such by surgeons making clinical decisions. To ensure that our findings were not sensitive to our own definitions of indeterminate and concordance, we then recalculated concordance with the recoded CT scans. This strategy has been adopted in previous studies as a primary categorization15 and as part of a sensitivity analysis.5 Finally, in an effort to assess whether selection bias influenced our findings, we generated a propensity-matched cohort based on nearly all of the clinical and demographic variables collected by SCOAP (many more than were used in the multivariate regression model) and repeated our analyses using this matched cohort.
RESULTS
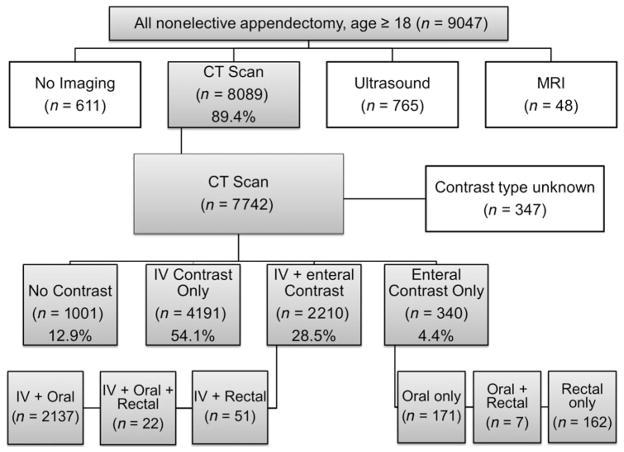
A total of 9047 adult patients underwent a nonelective appendectomy in SCOAP hospitals from January 2010 to December 2011. Most patients (89.4%) were evaluated by CT scan. The Figure illustrates how patients were allocated to various imaging modalities. Of those who underwent CT, the 2 largest groups were those who had IV contrast only (54.1%) and those who had IV + enteral contrast (28.5%). By far, the most common IV + enteral regimen included oral contrast.
FIGURE.
Imaging Modality and Contrast Choice in SCOAP. The Figure details how patients were distributed among the various available imaging modalities. The gray boxes track those patients considered in this study. Percentages in the fourth band indicate the percentage of overall CT scans performed with each contrast regimen. These are also the categories utilized in univariate and multivariate logistic regression analysis.
Patients in the IV-only group and IV + enteral group were similar (Table 1). The IV + enteral group were, on average, 1 year older (P = 0.01). Mean WBC count, serum creatinine, BMI, and weight were similar between groups as was the proportion of patients with 1 or more comorbid conditions. Among patients with enteral contrast, perforation was slightly more frequent (14.7% vs 17.4%, P = 0.005). Mean duration from ED admission to OR start time was increased by 48 minutes for those who had enteral contrast (P < 0.01).
TABLE 1.
Clinical and Demographic Characteristics of the CT Cohort
| Patient Characteristics | IV Contrast Only | IV + Enteral Contrast (Oral, Rectal, or Both) | P |
|---|---|---|---|
| N | 4191 | 2210 | |
| Male, % | 52.9% [2214/4189] | 50.7% [1121/2210] | NS (0.105) |
| Mean age (SD) | 39.4 (16.1) | 40.5 (17.0) | 0.011 |
| Mean WBC count (SD) | 13.4 (4.4) | 13.2 (4.6) | NS (0.110) |
| Mean serum creatinine (SD) | 0.9 (0.6) | 0.9 (0.6) | NS (0.598) |
| Mean BMI (SD) | 29.2 (0.9) | 29.0 (0.9) | NS (0.904) |
| Mean weight (SD) | 82.3 (21.5) | 81.6 (22.2) | NS (0.216) |
| Comorbidity index, % | |||
| 0 | 86.7% [3635/4191] | 87.6% [1935/2210] | NS (0.352) |
| 1 | 11.3% [474/4191] | 11.0% [242/2210] | NS (0.664) |
| 2 | 1.4% [58/4191] | 1.1% [25/2210] | NS (0.396) |
| 3+ | 0.6% [24/4191] | 0.4% [8/2210] | NS (0.256) |
| Perforation, % (NA excluded) | 14.7% [598/4066] | 17.4% [370/2124] | 0.005 |
| Negative appendectomy, % | 2.7% [111/4184] | 3.5% [78/2202] | 0.046 |
| Mean hours from ER admit to OR start | 8.3 h | 9.1 h | <0.001 |
| Concordance, % | 90.4% [3077/4177] | 90.0% [1981/2201] | NS (0.591) |
Patients who received the contrast regimens of primary interest are compared in Table 1. For continuous variables, standard deviations (SD) are presented in parentheses. Independent Student’s t test was used to test differences between continuous variables presented as means, and the Pearson χ2 test was used in comparisons of categorical variables. Where percentages are shown, exact numbers are denoted in brackets.
Hospitals differed by processes of care and by concordance (Table 2). The vast majority of patients were treated in urban hospitals (91.3%). More than half were treated at hospitals that support some kind of residency program, but only 17% were treated at hospitals with surgical residencies. Urban hospitals and teaching hospitals used CT scan slightly less than rural and nonteaching hospitals. There was also a difference in the use of contrast. Urban hospitals and teaching institutions were substantially more likely to utilize only IV contrast than rural hospitals and those without training programs. Rural hospitals had higher overall concordance than urban hospitals, as did hospitals with surgical residency programs compared with those without. Regardless of hospital type, there was no difference in concordance comparing IV-only to IV + enteral CT scans (Table 3).
TABLE 2.
CT Use, Contrast Regimen, and Concordance by Hospital Type
| Urban | Rural | P | Surgery Residents | No Surgery Residents | P | Any Residency Programs | No Residency Program | P | |
|---|---|---|---|---|---|---|---|---|---|
| Percent of total SCOAP volume | 91.3% [8259/9047] | 8.7% [788/9047] | 16.9% [1526/9047] | 83.1% [7521/9047] | 56.7% [5128/9047] | 43.3% [3919/9047] | |||
| Percent CT scan use | 89.2% [7367/8259] | 91.6%* [722/788] | 0.035 | 87.6% [1337/1436] | 89.8%* [6752/7521] | 0.012 | 88.6% [4541/5128] | 90.5%* [3548/3919] | 0.002 |
| Percent of patients who received IV contrast only | 52.3% [3855/7367] | 46.5%* [336/722] | 0.003 | 62.5% [835/1337] | 49.7%* [3356/6752] | < 0.001 | 54.2% [2461/4541] | 48.8%* [1730/3548] | < 0.001 |
| Overall CT concordance | 89.2% [6573/7367] | 91.8%* [663/722] | 0.03 | 91.7% [1226/1337] | 89.0%* [6010/7521] | 0.004 | 89.7% [4075/4541] | 89.1% [3161/3548] | NS (0.35) |
P < 0.05 in a Pearson χ2 test is indicated by an asterisk (*). Exact numbers are presented with each percentage.
TABLE 3.
Concordance by Hospital Type: IV-Only Versus IV + Enteral Contrast
| Hospital Type | IV Contrast Only (% Concordance) | IV + Enteral Contrast (% Concordance) | P |
|---|---|---|---|
| Urban | 90.2% [3466/3844] | 89.7% [1763/1966] | NS (0.55) |
| Rural | 93.4% [311/333] | 92.8% [218/235] | NS (0.77) |
| Surgery residency program | 92.8% [773/833] | 90.9% [91/320] | NS (0.29) |
| No surgery residency program | 89.8% [3004/3344] | 89.9% [1690/1881] | NS (0.99) |
| Any residency programs | 91.1% [2237/2455] | 90.1% [1096/1217] | NS (0.30) |
| No residency programs | 89.4% [1540/1722] | 89.9% [885/984] | NS (0.68) |
Differences in percent concordance were tested using the Pearson χ2 test. Exact numbers are presented with each percentage in brackets.
For the entire cohort, concordance for IV-only scans was 90.4% and for IV + enteral scans was 90.0%. Completely unenhanced scans were 85.7% concordant, and those with enteral-contrast only were 92.6% concordant. Completely unenhanced CT was the only modality that differed significantly from IV-only CT (unadjusted OR of concordance was 0.63, 95% CI: 0.05–0.79). After adjusting for age, sex, comorbid conditions, weight, hospital type, and perforation, there was no difference in concordance between IV-only contrast and IV + enteral contrast (OR = 0.95, 95% CI: 0.72–1.25). Independent predictors of discordant CT scans were lack of any contrast (IV or enteral) and the presence of 3 or more comorbid conditions (Table 4). Increasing age was associated with concordance, and increasing weight had a small but significant impact on concordance. Presence of a perforated appendix was the strongest predictor of concordance, with adjusted OR of 2.17 (95% CI: 1.65–2.87).
TABLE 4.
Contrast Type and Concordance: Univariate and Multivariate Analysis
| Variable | Unadjusted
|
Fully Adjusted
|
||
|---|---|---|---|---|
| Odds Ratio | 95% Confidence Interval | Odds Ratio | 95% Confidence Interval | |
| IV contrast only | Ref | Ref | ||
| IV + Enteral contrast | 0.95 | 0.72–1.27 | 0.95 | 0.72–1.25 |
| Enteral contrast only | 1.33 | 0.90–1.96 | 1.46 | 0.92–2.31 |
| No contrast | 0.63 | 0.05–0.79 | 0.62 | 0.49–0.79 |
| Age (centered at 40) | 1.015 | 1.01–1.02 | 1.02 | 1.01–1.02 |
| Female | Ref | Ref | ||
| Male | 1.63 | 1.41–1.88 | 1.59 | 1.37–1.85 |
| Comorbid condition(s) score | ||||
| 0 | Ref | Ref | ||
| 1 | 0.97 | 0.79–1.19 | 0.86 | 0.67–1.10 |
| 2 | 0.76 | 0.44–1.31 | 0.55 | 0.29–1.02 |
| 3+ | 0.54 | 0.30–0.97 | 0.35 | 0.18–0.65 |
| Patient weight | 1.01 | 1.00–1.01 | 1.01 | 1.00–1.01 |
| Urban nontraining hospital | Ref | Ref | ||
| Urban training hospital | 1.43 | 0.998–2.06 | 1.25 | 0.89–1.77 |
| Rural hospital | 1.49 | 1.01–2.20 | 1.52 | 0.94–2.43 |
| Nonperforated appendix | Ref | Ref | ||
| Perforated appendix | 2.17 | 1.71–2.75 | 1.98 | 1.52–2.55 |
The sensitivity analysis based on indeterminate scans recategorized as positive and the propensity-matched analysis both generated nearly identical results as the original analysis: concordance was the same for IV-only and IV + enteral CT scans.
DISCUSSION
In a population of patients undergoing nonelective appendectomy, enteral contrast did not improve accuracy in the diagnosis of appendicitis compared with IV contrast alone. Although this study did not evaluate all patients undergoing CT for suspected appendicitis, several small randomized trials of IV-only versus IV + enteral contrast in patients undergoing evaluation for suspected appendicitis have yielded similar results.15–17 Other, nonrandomized studies of IV-only contrast use in patients with suspected appendicitis also report good performance.7,22,23 Our study provides substantial additional data to these prospective trials by demonstrating broad clinical effectiveness. We conclude that IV contrast alone is sufficient for the diagnosis of appendicitis in a wide variety of hospitals, outside of tertiary centers and strict research protocols.
Although, oral contrast does not reach the cecum in as many as 30% of patients,15,24 several benefits of oral contrast have been suggested. One of the purported benefits of oral contrast is opacification of the appendix, which can assist in its identification and location; a traditional radiographic sign of appendicitis is the non-opacified appendix (suggestive of luminal obstruction). Despite wide use, there are no published data to support the hypothesis that radiopaque oral contrast benefits the detection of acute or chronic abdominal conditions by multidetector CT. Gastric or intestinal distension may assist interpretation, but oral contrast may also generate false positive findings.14,25
Forgoing enteral contrast offers several potential benefits. The first of these is reduced time in the ED. A recent randomized trial found that patients who received oral contrast awaited disposition an average of 90 minutes longer than those who did not.15 In our analysis, patients who received enteral contrast waited an average of 48 minutes longer than those who did not. Another benefit is that patients, who may be nauseated from their gastrointestinal symptoms, are not required to consume a large volume of oral contrast material (in some cases not long before induction of general anesthesia)24 or required to undergo rectal catheterization for administration of rectal contrast. There is a long-standing debate in the literature whether oral contrast is a risk factor before induction of general anesthesia, but there are numerous case reports describing adverse pulmonary events in the setting of aspirated water-soluble and barium-based oral contrast agents, and several authors recommend forgoing contrast when possible before anesthesia.26–28 Finally, there may be a benefit in terms of cost reduction. As enteral contrast is not very expensive (a liter of positive oral contrast costs less than $3.00), savings may be achieved primarily through shortened time in the ED, improving efficient use of scarce emergency medicine resources14 and possibly increasing revenue for hospitals. Clearly, despite these benefits and despite data from previous studies, many patients who undergo CT for suspected appendicitis still receive enteral contrast (for instance, nearly a third of the patients in this cohort). The findings presented here, generated from a diverse group of hospitals, may help to drive practice change toward a more evidence-based workup for suspected appendicitis.
Several studies have observed reduced specificity and positive predictive value in scans performed with oral contrast, including 1 large systematic review29 and 1 randomized trial.15 Calculations of specificity and positive predictive value are heavily dependent on the frequency of false-positives, which would most frequently manifest clinically as NA. Our study found a slight increase in NA among patients who received enteral contrast (3.5% vs 2.7% in IV-only scans, P = 0.046). Why this is a consistent finding among several studies is not clear, but it may relate to the fact that a nonopacified appendix has traditionally been considered a sign of appendicitis, and “over-calls” of appendicitis may result from scans in which the appendix did not fill with contrast for reasons other than appendicitis.
Previous investigators have studied the accuracy of completely unenhanced CT scans, achieving results equivalent to other contrast regimens.30–32 In our study, 1001 patients underwent completely un-enhanced CT, and concordance was only 85.7%. There are disadvantages to IV contrast, including the risk of renal insult and the risk of iodinated contrast allergy; however, complete lack of enhancement may reduce the ability of CT scan to make alternative diagnoses, which has been one of the arguments for routine use of CT scans in the evaluation of adults with suspected appendicitis.
This study does have limitations. As with any observational study, there may be unrecognized sources of confounding. In particular, we do not know why patients received the contrast regimens they did, which may have led to selection bias. Selection bias would be limited by the use of imaging protocols at participating hospitals, but it is unclear how many patients were imaged according to protocols and how many had contrast regimens selected based on clinical factors. The major discernible difference between the 2 groups was a slight increase in perforation among patients who received enteral contrast. We tested this association in a separate multivariate logistic regression and found that adjusting for age, sex, weight, comorbid conditions, and hospital type eliminated the difference in perforation between patients with IV-only scans and those with IV + enteral contrast (OR = 1.1, 95% CI: 0.90–1.33). Using most of the clinical and demographic variables collected by SCOAP, we also performed a propensity-matched analysis to evaluate for evidence of selection bias. Our findings were unchanged, although 1 limitation of this technique is that it cannot overcome the effects of unmeasured covariates.33 SCOAP data are based on final radiology reports, which are not always available to clinicians making real-time diagnostic decisions. “Wet reads” by ED physicians or consulting surgeons may be different than official radiologist interpretations, which could mean that these findings vary to some extent from how these scans were used in actual clinical practice. Finally, as noted earlier, this is a cohort of patients who underwent appendectomy, not patients with suspected appendicitis. In our view, this limitation is mitigated when the results of the current study are considered in tandem with evidence from randomized trials.
CONCLUSIONS
Data from SCOAP-CERTAIN suggest that enteral contrast does not offer diagnostic benefit for patients who undergo appendectomy. Furthermore, within each category of hospital type, CT scans enhanced only with IV contrast performed as well as CT scans in which enteral contrast was also used, suggesting that these findings are broadly generalizable. Increased ED efficiency, patient comfort, and safety may be improved without compromising diagnostic effectiveness. Enteral contrast should be eliminated in IV-enhanced CT scans performed for suspected appendicitis.
Footnotes
Disclosure: SCOAP-CERTAIN research projects are supported by the Life Discovery Fund of Washington State and the Agency for Healthcare Research and Quality. The administrative home for SCOAP is the Foundation for Healthcare Quality. Dr Drake was supported by the National Institutes of Health in the form of a T32 training fellowship grant from the National Institute of Diabetes & Digestive & Kidney Diseases (grant 5T32DK070555-03). All authors report no potential conflicts of interest.
References
- 1.Korner H, Sondenaa K, Soreide JA, et al. Incidence of acute nonperforated and perforated appendicitis: age-specific and sex-specific analysis. World J Surg. 1997;21:313–317. doi: 10.1007/s002689900235. [DOI] [PubMed] [Google Scholar]
- 2.Addiss DG, Shaffer N, Fowler BS, et al. The epidemiology of appendicitis and appendectomy in the United States. Am J Epidemiol. 1990;132:910–925. doi: 10.1093/oxfordjournals.aje.a115734. [DOI] [PubMed] [Google Scholar]
- 3.Cantrell JR, Stafford ES. The diminishing mortality from appendicitis. Ann Surg. 1955;141:749–758. doi: 10.1097/00000658-195506000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Walker S, Haun W, Clark J, et al. The value of limited computed tomography with rectal contrast in the diagnosis of acute appendicitis. Am J Surg. 2000;180:450–454. doi: 10.1016/s0002-9610(00)00540-7. discussion 454–455. [DOI] [PubMed] [Google Scholar]
- 5.Weyant MJ, Eachempati SR, Maluccio MA, et al. Interpretation of computed tomography does not correlate with laboratory or pathologic findings in surgically confirmed acute appendicitis. Surgery. 2000;128:145–152. doi: 10.1067/msy.2000.107422. [DOI] [PubMed] [Google Scholar]
- 6.Lee CC, Golub R, Singer AJ, et al. Routine versus selective abdominal computed tomography scan in the evaluation of right lower quadrant pain: a randomized controlled trial. Acad Emerg Med. 2007;14:117–122. doi: 10.1197/j.aem.2006.08.007. [DOI] [PubMed] [Google Scholar]
- 7.Kim K, Rhee JE, Lee CC, et al. Impact of helical computed tomography in clinically evident appendicitis. Emerg Med J. 2008;25:477–481. doi: 10.1136/emj.2006.044552. [DOI] [PubMed] [Google Scholar]
- 8.Piper HG, Rusnak C, Orrom W, et al. Current management of appendicitis at a community center–how can we improve? Am J Surg. 2008;195:585–588. doi: 10.1016/j.amjsurg.2007.12.033. discussion 588–589. [DOI] [PubMed] [Google Scholar]
- 9.Wagner PL, Eachempati SR, Soe K, et al. Defining the current negative appendectomy rate: for whom is preoperative computed tomography making an impact? Surgery. 2008;144:276–282. doi: 10.1016/j.surg.2008.03.040. [DOI] [PubMed] [Google Scholar]
- 10.Raja AS, Wright C, Sodickson AD, et al. Negative appendectomy rate in the era of CT: an 18-year perspective. Radiology. 2010;256:460–465. doi: 10.1148/radiol.10091570. [DOI] [PubMed] [Google Scholar]
- 11.Webb EM, Nguyen A, Wang ZJ, et al. The negative appendectomy rate: who benefits from preoperative CT? AJR Am J Roentgenol. 2011;197:861–866. doi: 10.2214/AJR.10.5369. [DOI] [PubMed] [Google Scholar]
- 12.Drake FT, Florence MG, Johnson MG, et al. Progress in the diagnosis of appendicitis: a report from Washington State’s Surgical Care and Outcomes Assessment Program. Ann Surg. 2012;256:586–594. doi: 10.1097/SLA.0b013e31826a9602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dalrymple NC, Prasad SR, El-Merhi FM, et al. Price of isotropy in multidetector CT. Radiographics. 2007;27:49–62. doi: 10.1148/rg.271065037. [DOI] [PubMed] [Google Scholar]
- 14.Lee SY, Coughlin B, Wolfe JM, et al. Prospective comparison of helical CT of the abdomen and pelvis without and with oral contrast in assessing acute abdominal pain in adult emergency department patients. Emerg Radiol. 2006;12:150–157. doi: 10.1007/s10140-006-0474-z. [DOI] [PubMed] [Google Scholar]
- 15.Kepner AM, Bacasnot JV, Stahlman BA. Intravenous contrast alone vs intravenous and oral contrast computed tomography for the diagnosis of appendicitis in adult ED patients. Am J Emerg Med. 2012;30:1765–1773. doi: 10.1016/j.ajem.2012.02.011. [DOI] [PubMed] [Google Scholar]
- 16.Anderson SW, Soto JA, Lucey BC, et al. Abdominal 64-MDCT for suspected appendicitis: the use of oral and IV contrast material versus IV contrast material only. AJR Am J Roentgenol. 2009;193:1282–1288. doi: 10.2214/AJR.09.2336. [DOI] [PubMed] [Google Scholar]
- 17.Keyzer C, Cullus P, Tack D, et al. MDCT for suspected acute appendicitis in adults: impact of oral and IV contrast media at standard-dose and simulated low-dose techniques. AJR Am J Roentgenol. 2009;193:1272–1281. doi: 10.2214/AJR.08.1959. [DOI] [PubMed] [Google Scholar]
- 18.von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370:1453–1457. doi: 10.1016/S0140-6736(07)61602-X. [DOI] [PubMed] [Google Scholar]
- 19.Flum DR, McClure TD, Morris A, et al. Misdiagnosis of appendicitis and the use of diagnostic imaging. J Am Coll Surg. 2005;201:933–939. doi: 10.1016/j.jamcollsurg.2005.04.039. [DOI] [PubMed] [Google Scholar]
- 20.Huynh V, Lalezarzadeh F, Lawandy S, et al. Abdominal computed tomography in the evaluation of acute and perforated appendicitis in the community setting. Am Surg. 2007;73:1002–1005. [PubMed] [Google Scholar]
- 21.Frei SP, Bond WF, Bazuro RK, et al. Appendicitis outcomes with increasing computed tomographic scanning. Am J Emerg Med. 2008;26:39–44. doi: 10.1016/j.ajem.2007.06.027. [DOI] [PubMed] [Google Scholar]
- 22.Mun S, Ernst RD, Chen K, et al. Rapid CT diagnosis of acute appendicitis with IV contrast material. Emerg Radiol. 2006;12:99–102. doi: 10.1007/s10140-005-0456-6. [DOI] [PubMed] [Google Scholar]
- 23.Poortman P, Oostvogel HJ, Bosma E, et al. Improving diagnosis of acute appendicitis: results of a diagnostic pathway with standard use of ultrasonography followed by selective use of CT. J Am Coll Surg. 2009;208:434–441. doi: 10.1016/j.jamcollsurg.2008.12.003. [DOI] [PubMed] [Google Scholar]
- 24.Laituri CA, Fraser JD, Aguayo P, et al. The lack of efficacy for oral contrast in the diagnosis of appendicitis by computed tomography. J Surg Res. 2011;170:100–103. doi: 10.1016/j.jss.2011.02.017. [DOI] [PubMed] [Google Scholar]
- 25.Winter T. A plea for oral contrast administration in CT for emergency department patients. AJR Am J Roentgenol. 2010;195:W90. doi: 10.2214/AJR.10.4223. [DOI] [PubMed] [Google Scholar]
- 26.Trulzsch DV, Penmetsa A, Karim A, et al. Gastrografin-induced aspiration pneumonia: a lethal complication of computed tomography. South Med J. 1992;85:1255–1256. doi: 10.1097/00007611-199212000-00025. [DOI] [PubMed] [Google Scholar]
- 27.Morcos SK. Review article: effects of radiographic contrast media on the lung. Br J Radiol. 2003;76:290–295. doi: 10.1259/bjr/54892465. [DOI] [PubMed] [Google Scholar]
- 28.Mahmoud M, McAuliffe J, Kim HY, et al. Oral contrast for abdominal computed tomography in children: the effects on gastric fluid volume. Anesth Analg. 2010;111:1252–1258. doi: 10.1213/ANE.0b013e3181f1bd6f. [DOI] [PubMed] [Google Scholar]
- 29.Anderson BA, Salem L, Flum DR. A systematic review of whether oral contrast is necessary for the computed tomography diagnosis of appendicitis in adults. Am J Surg. 2005;190:474–478. doi: 10.1016/j.amjsurg.2005.03.037. [DOI] [PubMed] [Google Scholar]
- 30.Malone AJ, Jr, Wolf CR, Malmed AS, et al. Diagnosis of acute appendicitis: value of unenhanced CT. AJR Am J Roentgenol. 1993;160:763–766. doi: 10.2214/ajr.160.4.8456661. [DOI] [PubMed] [Google Scholar]
- 31.Lane MJ, Liu DM, Huynh MD, et al. Suspected acute appendicitis: nonenhanced helical CT in 300 consecutive patients. Radiology. 1999;213:341–346. doi: 10.1148/radiology.213.2.r99nv44341. [DOI] [PubMed] [Google Scholar]
- 32.Lowe LH, Penney MW, Stein SM, et al. Unenhanced limited CT of the abdomen in the diagnosis of appendicitis in children: comparison with sonography. AJR Am J Roentgenol. 2001;176:31–35. doi: 10.2214/ajr.176.1.1760031. [DOI] [PubMed] [Google Scholar]
- 33.Hemmila MR, Birkmeyer NJ, Arbabi S, et al. Introduction to propensity scores: a case study on the comparative effectiveness of laparoscopic vs open appendectomy. Arch Surg. 2010;145:939–945. doi: 10.1001/archsurg.2010.193. [DOI] [PubMed] [Google Scholar]