Abstract
Background Radiocarpal fracture-dislocations are challenging injuries that are often associated with postoperative pain, stiffness, instability, or early arthrosis.
Case Description We report a 1-year follow-up of a ligamentous radiocarpal dislocation (Dumontier group I) treated with a dorsal wrist-spanning plate and volar capsular repair with good results.
Literature Review Historically, Dumontier group I injuries treated with a variety of techniques (closed reduction and casting, percutaneous pinning, and open fixation) have been associated with stiffness and loss of reduction.
Clinical Relevance Distraction plating is a safe and effective technique for treating select distal radius fractures, and we suggest it has the potential to produce good outcomes when used to treat radiocarpal fracture-dislocations.
Keywords: radiocarpal dislocation, wrist dislocation, distraction plating, internal fixation, surgical technique
Radiocarpal fracture-dislocations are uncommon injuries characterized by dorsal or volar dislocation of the carpus with or without associated fracture of the distal radius. These injuries are frequently open and can be complicated by neurologic deficits, vascular compromise, or intercarpal ligamentous disruption. Dumontier et al classified radiocarpal fracture-dislocations into two groups. Group 1 included purely ligamentous injuries or those associated with a small radial styloid avulsion; group 2 injuries included a radial styloid fracture involving at least one-third of the scaphoid fossa. Group 1 injuries are particularly challenging to treat because the global ligamentous injury increases the risk of persistent radiocarpal instability, with generally poor outcomes reported if they present with ulnocarpal translocation.1
A variety of treatment techniques have been described, but current treatment recommendations involve surgical management. Goals of surgery include a concentric reduction of the radiocarpal joint, decompression of neurovascular structures, treatment of associated intercarpal injuries, and soft tissue repair.2 Unfortunately, even with successful open treatment, patient outcomes can be compromised by a 30–40% decrease in wrist motion and by persistent radiocarpal instability,1 2 3 4 suggesting improved surgical techniques are still required.
We report on a group I radiocarpal fracture-dislocation treated with a dorsal wrist-spanning plate and open repair of the volar capsule, and we compare our results to those reported historically.
Case Report
A 32-year-old man was transferred to our emergency department as a trauma activation following a high-speed motor vehicle collision. Examination of the left wrist showed obvious deformity consistent with dorsal translation of the carpus. The skin was intact. The patient had palpable radial and ulnar pulses and reported intact sensation in the left hand. He was able to flex and extend his fingers, but a more detailed motor exam was limited by patient discomfort. Radiographs of the left wrist demonstrated a dorsal radiocarpal dislocation with a small avulsion fracture of the radial styloid (Dumontier group 1; Fig. 1a). Additional injuries included a closed ipsilateral femur fracture and bilateral pulmonary contusions.
Fig. 1.

(a) Posteroanterior (PA) and lateral radiographs of the left wrist at the time of injury show dorsal dislocation of the carpus with associated radial styloid avulsion fracture. (b) Postreduction PA and lateral radiographs of the left wrist show a concentric reduction of the radiocarpal joint without any obvious associated intercarpal ligamentous injury, but there was ulnar translocation of the carpus.
Initial management of the left wrist involved closed reduction and application of a sugar-tong splint. Postreduction radiographs showed a concentric alignment of the radiocarpal joint without evidence of intercarpal injury, but there was ulnar translocation of the carpus (Fig. 1b). Radiographs of the hand, forearm, and elbow showed no additional fractures. The patient was stabilized overnight in the intermediate care unit and taken to the operating theater the following day for intramedullary nailing of his left femur and operative treatment of his left wrist.
Surgery was performed under general anesthesia, with a brachial tourniquet used for intraoperative hemostasis. Anatomic reduction of the radiocarpal joint was confirmed with fluoroscopy. The reduction was maintained by placing a dorsal wrist-spanning plate (DePuy Synthes, West Chester, PA) using a previously described dorsal three-incision technique.5 The plate was fixed distally to the long finger metacarpal and proximally to the radial diaphysis using locking screws at both ends. The volar radiocarpal ligaments were then exposed through a trans–flexor carpi radialis sheath approach, and the radioscaphocapitate and long radiolunate ligaments were found to be avulsed from the distal radius (Fig. 2a). These ligaments were repaired back to their origins on the distal radius using Mitek GII suture anchors (DePuy, Warsaw, IN). The distal radioulnar joint was evaluated under dynamic fluoroscopy and was felt to be stable.
Fig. 2.
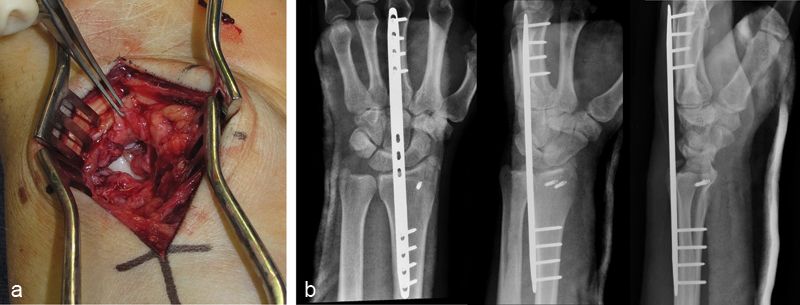
(a) Clinical photograph of the volar wrist showing avulsion of the radial origin of the radiocarpal ligaments (held in forceps). (b) Postoperative PA, oblique, and lateral radiographs of the left wrist show maintained reduction of the radiocarpal joint after placement of a dorsal wrist-spanning plate and repair of the volar radiocarpal ligaments using suture anchors.
Postoperatively, the patient was placed in a volar splint with the elbow and metacarpophalangeal (MP) joints free, and he was started immediately on supination and pronation exercises. Weight bearing through the left elbow was permitted to facilitate use of a platform walker after fixation of his ipsilateral femur fracture. Immediate postoperative radiographs confirmed a concentric reduction and stable fixation of the radiocarpal joint (Fig. 2b).
Four months after the initial surgery, the patient was returned to the operating theater and the dorsal plate was removed through the prior incisions without complication. The patient was referred to hand therapy and began wrist flexion and extension exercises three times weekly under the supervision of a therapist, with home exercises performed several times daily between visits. Six months after the initial injury and two months after the second surgery, the patient reported occasional mild wrist pain relieved with ibuprofen. Wrist flexion measured 55° and wrist extension measured 65° in the injured wrist, compared with wrist flexion of 75° and wrist extension of 80° in the uninjured wrist. Pronation and supination were symmetric with the contralateral side. At 1 year from initial injury, flexion measured 65° (87% of uninjured wrist) and extension 70° (83% of uninjured wrist; Fig. 3a); radiographs showed a healed radial styloid fracture and maintained alignment of the radiocarpal joint without significant dorsal or ulnar translation (Fig. 3b). The patient reported minimal wrist pain and had returned to full work duties without restrictions.
Fig. 3.
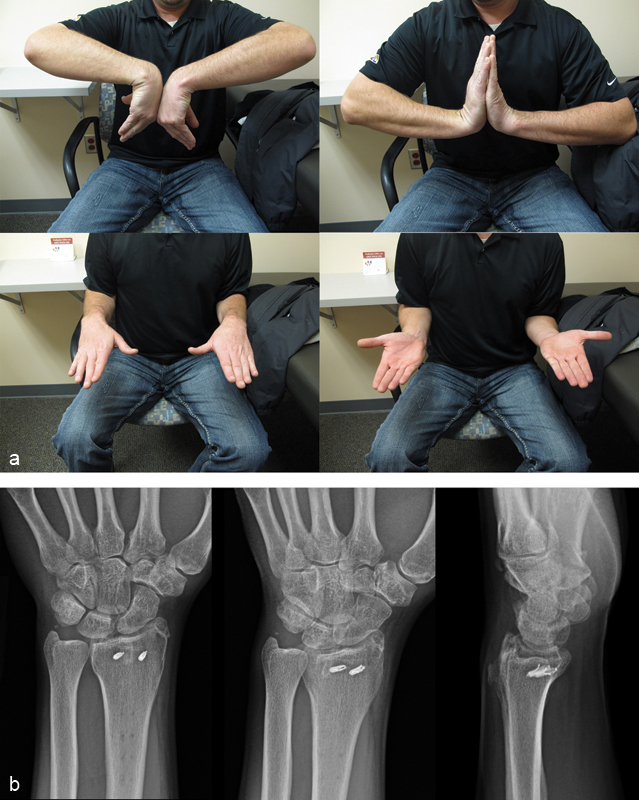
(a) Clinical photographs show flexion, extension, pronation, and supination of the injured wrist (left) compared with the contralateral uninjured wrist (right) at 1 year postinjury. (b) PA, oblique, and lateral radiographs of the left wrist at 1 year postinjury show a healed radial styloid fracture and maintained reduction of the radiocarpal joint without dorsal or ulnar translation of the carpus.
Discussion
To our knowledge, treatment of a Dumontier I radiocarpal fracture-dislocation with a wrist-spanning plate has not been reported in the literature. Historically, some of the major challenges in treating ligamentous radiocarpal dislocations have included restoring adequate stability to the radiocarpal articulation, avoiding late ulnar translation of the carpus, and minimizing stiffness with wrist flexion and extension.
In the largest published series to date, Dumontier et al reported the functional and radiographic outcomes of twenty-seven radiocarpal fracture-dislocations treated with a variety of techniques.1 Seven of their 27 patients had purely ligamentous dislocations, or dislocations associated with an avulsion fracture of the radial styloid (group 1), while 20 had associated radial styloid fractures involving more than one-third of the scaphoid fossa (group 2).
Of the seven group 1 patients, two were treated with closed reduction and long-arm cast immobilization, three were treated with percutaneous pinning of the radial styloid fragment and long-arm cast immobilization (one patient also had radioscaphoid and radiolunate pinning), and two were treated with open fixation of the radial styloid and suture repair of the volar ligaments through a single approach. Two patients were lost to follow-up, leaving five patients with clinical and radiographic follow-up of at least 1 year. Four patients reported mild pain, and one reported moderate pain. Pronation averaged 76°, supination 66°, wrist flexion 54°, and wrist extension 54°.1 Mudgal et al reported similar limitation of postoperative wrist motion in their series of 12 patients, with flexion averaging 59° and extension 53°.3
In Dumontier's series, four of five group 1 patients developed immediate or late ulnar translation of the carpus. Only the patient who had supplementary radioscaphoid and radiolunate pinning maintained a concentric radiocarpal reduction. The patient reported mild pain, but he was troubled by postoperative stiffness, with wrist flexion of 50° and wrist extension of 40° at 16 months postinjury.1
Dumontier's article highlights the difficulty of effectively treating these injuries and the particular challenge with group 1 patients of maintaining a concentric radiocarpal joint without provoking excessive postoperative stiffness. In considering treatment options for the patient presented here, we were influenced by the favorable results reported by Ruch, Hanel, and others after distraction plating of comminuted distal radius fractures.6 7 8 In the published reports, the indication for selecting plating over traditional internal fixation is the presence of articular or metaphyseal comminution, which makes anatomic fixation of these small osseous fragments difficult or impossible. The technique is also used in polytraumatized patients, where the injured upper limb is required to assist with protected lower-extremity weight bearing.6 We hypothesized that group 1 radiocarpal dislocations may represent a relatively analogous patient population where no significant bony repair is possible. Instead, a successful result might be had by using a wrist-spanning plate to maintain the proper relationship between the carpus and the radius until soft tissue healing takes place, with the added benefits of being placed extraarticularly (versus Kirschner wires [K-wires] passed through the articular surface of the radioscaphoid and radiolunate joints) and permitting the injured extremity to assist with postoperative weight bearing.
Our early results with this technique are encouraging. Dorsal plating for distal radius fractures is associated with a low rate of complications, and it might be expected to be similarly safe for this indication.6 Our patient maintained a concentric radiocarpal reduction at 1 year after injury with a 135° arc of wrist flexion and extension, minimal pain, and a return to full employment. This compares favorably to historical reports, where concentric reductions were infrequently maintained1 and postoperative stiffness was common, with wrist arc of motion reported to range from 90–110° with other treatment methods.1 3
This report is limited by the fact that it considers a single patient at 1-year follow-up, and direct comparison to other patients treated with alternative methods is not possible. Others have reported good outcomes with volar ligamentous repair alone9 or ligamentous repair plus dorsal lip plate fixation.10 The main utility of the spanning plate is that it can stay in longer than K-wires, allowing more time for ligamentous healing to take place. In polytraumatized patients, it also permits the injured upper extremity to assist with weight bearing to facilitate early mobilization for pulmonary care.
In the patient reported here, the lunate and scaphoid remain radiographically well-aligned at 1 year, but there is concern the patient may be developing early arthrosis of the wrist, which might lead to worsening clinical results at later time points (Fig. 3b). However, given the infrequency of group 1 radiocarpal dislocations reported in the literature, we submit that the promising results in this case make wrist-spanning plating for this indication a technique worthy of further investigation.
Footnotes
Conflict of Interest None
References
- 1.Dumontier C, Meyer zu Reckendorf G, Sautet A, Lenoble E, Saffar P, Allieu Y. Radiocarpal dislocations: classification and proposal for treatment. A review of twenty-seven cases. J Bone Joint Surg Am. 2001;83-A(2):212–218. doi: 10.2106/00004623-200102000-00008. [DOI] [PubMed] [Google Scholar]
- 2.Ilyas A M, Mudgal C S. Radiocarpal fracture-dislocations. J Am Acad Orthop Surg. 2008;16(11):647–655. doi: 10.5435/00124635-200811000-00005. [DOI] [PubMed] [Google Scholar]
- 3.Mudgal C S, Psenica J, Jupiter J B. Radiocarpal fracture-dislocation. J Hand Surg [Br] 1999;24(1):92–98. doi: 10.1016/s0266-7681(99)90047-5. [DOI] [PubMed] [Google Scholar]
- 4.Nyquist S R, Stern P J. Open radiocarpal fracture-dislocations. J Hand Surg Am. 1984;9(5):707–710. doi: 10.1016/s0363-5023(84)80018-0. [DOI] [PubMed] [Google Scholar]
- 5.Ginn T A Ruch D S Yang C C Hanel D P Use of a distraction plate for distal radial fractures with metaphyseal and diaphyseal comminution. Surgical technique J Bone Joint Surg Am 200688 Pt 1 29–36. [DOI] [PubMed] [Google Scholar]
- 6.Hanel D P, Ruhlman S D, Katolik L I, Allan C H. Complications associated with distraction plate fixation of wrist fractures. Hand Clin. 2010;26(2):237–243. doi: 10.1016/j.hcl.2010.01.001. [DOI] [PubMed] [Google Scholar]
- 7.Richard M J, Katolik L I, Hanel D P, Wartinbee D A, Ruch D S. Distraction plating for the treatment of highly comminuted distal radius fractures in elderly patients. J Hand Surg Am. 2012;37(5):948–956. doi: 10.1016/j.jhsa.2012.02.034. [DOI] [PubMed] [Google Scholar]
- 8.Ruch D S, Ginn T A, Yang C C, Smith B P, Rushing J, Hanel D P. Use of a distraction plate for distal radial fractures with metaphyseal and diaphyseal comminution. J Bone Joint Surg Am. 2005;87(5):945–954. doi: 10.2106/JBJS.D.02164. [DOI] [PubMed] [Google Scholar]
- 9.Brown D, Mulligan M T, Uhl R L. Volar ligament repair for radiocarpal fracture-dislocation. Orthopedics. 2013;36(6):463–468. doi: 10.3928/01477447-20130523-07. [DOI] [PubMed] [Google Scholar]
- 10.Oberladstätter J, Arora R, Dallapozza C, Smekal V, Kammerlander C, Lutz M. Radiological radio-carpal and mid-carpal motion after operative treatment of dorsal radio-carpal fracture dislocations. Arch Orthop Trauma Surg. 2010;130(1):77–81. doi: 10.1007/s00402-009-0902-0. [DOI] [PubMed] [Google Scholar]


