Abstract
Studies on the biologic and molecular genetic underpinnings of multiple myeloma (MM) have identified the pleiotropic, pro-inflammatory cytokine, interleukin-6 (IL-6), as a factor crucial to the growth, proliferation and survival of myeloma cells. IL-6 is also a potent stimulator of osteoclastogenesis and a sculptor of the tumor microenvironment in the bone marrow of patients with myeloma. This knowledge has engendered considerable interest in targeting IL-6 for therapeutic purposes, using a variety of antibody- and small-molecule-based therapies. However, despite the early recognition of the importance of IL-6 for myeloma and the steady progress in our knowledge of IL-6 in normal and malignant development of plasma cells, additional efforts will be required to translate the promise of IL-6 as a target for new myeloma therapies into significant clinical benefits for patients with myeloma. This review summarizes published research on the role of IL-6 in myeloma development and describes ongoing efforts by the University of Iowa Myeloma Multidisciplinary Oncology Group to develop new approaches to the design and testing of IL-6-targeted therapies and preventions of MM.
Keywords: IL-6 signaling in neoplastic plasma cells, Myeloma stem cells and minimal residual disease, Small-drug- and monoclonal antibody-based inhibitors, Genetically engineered mouse models of human myeloma
Interleukin-6 (IL-6) plays a prominent role in multiple myeloma (MM)
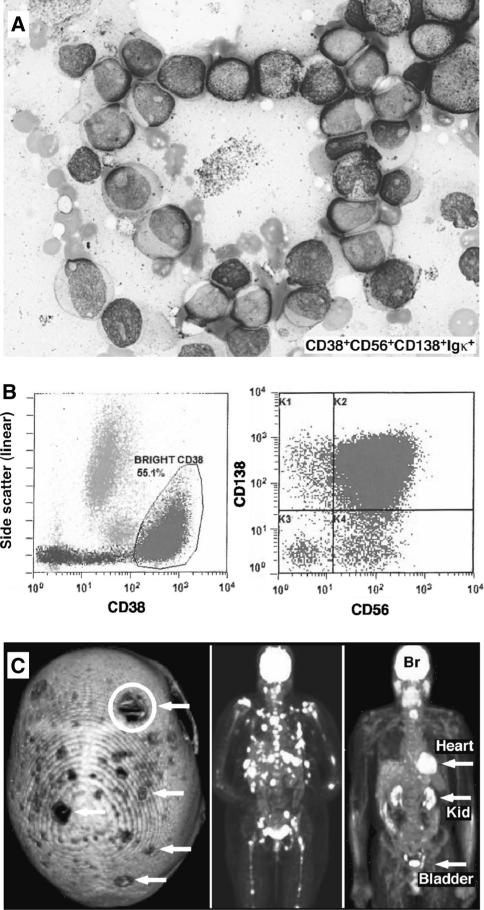
Interleukin-6 is a pleiotropic cytokine that not only orchestrates a plethora of vital physiological functions, but also impacts many types of solid and liquid cancers [1]. Prominent among the latter are B-cell lineage neoplasms, such as Hodgkin [2] and nonHodgkin lymphoma [3], plasmacytoma and Castleman disease [4] and multiple myeloma (MM) [5]. IL-6 is important for the growth and survival of myeloma cells [6] and stimulates osteoclasto-genesis [7]. The importance of IL-6 for myeloma [8–10] and its involvement in normal and malignant development of plasma cells [5, 11, 12] have been recognized a long time ago, yet the translation of this insight into effective IL-6-targeted therapies for MM patients has remained elusive. MM is the second most common blood cancer in developed countries. It arises in the hematopoietic bone marrow as a neoplasm of terminally differentiated immunoglobulin-producing B-lymphocytes called plasma cells. The diagnosis of MM relies on clinical symptoms, histopathologic findings (Fig. 1a) and laboratory investigations such as flow cytometry (Fig. 1b). MM is a “bone-eating” tumor that causes characteristic osteolytic lesions throughout the blood cell-producing skeleton (Fig. 1c, left). The resulting bone pain is often excruciating if not outright debilitating. A good diagnostic imaging method for myeloma is [18] F-fluorodeoxyglucose positron emission tomography (FDG-PET), which readily detects tumor nodules due to increased metabolic activity (glucose uptake) of myeloma cells (Fig. 1c, center and right). In the USA, more than 20,000 patients are diagnosed with MM annually. The plasma cell tumor accounts for ~1 % of all cancer diagnoses but ~2 % of all cancer deaths. Newly developed and FDA-approved myeloma drugs (e.g., bortezomib, lenalidomide, carfilzomib, pomalidomide and pegylated liposomal doxorubicin) have significantly improved myeloma treatment in the past decade. Nonetheless, the overall 5-year survival rate of patients receiving therapies that do not involve transplantation of autologous hematopoietic stem cells (ASCT) does not exceed ~40 %. Treatment protocols including ASCT afford better outcomes, but eligibility for the procedure depends on patient age, co-morbidities and a host of other considerations—the discussion of which goes beyond the scope of this article. The bottom line is that, with or without ASCT, MM remains incurable in the great majority of cases and thus defines an unmet medical need. The University of Iowa (UI) Myeloma Multidisciplinary Oncology Group (MOG) is eager to address this need, and is doing so, in part, by investigating IL-6, a promising but evasive therapeutic target in myeloma.
Fig. 1.
Diagnostic features of MM. a Cytological features of myeloma, using a recent case of refractory myeloma post-multiple therapies as example. BM touch preparation containing large, atypical plasma cells with high nuclear to cytoplasmic ratio, fine chromatin, eccentric nuclei and prominent nucleoli. b Flow cytometric detection of myeloma cells. In this patient, CD38bright myeloma cells comprised 55 % of all BM cells (left panel, circled). The tumor cells contained monotypic cytoplasmic Igj (not shown) and exhibited immunoreactivity for CD56 and CD138 (right panel) but not for CD27, CD28, CD45 and CD54 (not shown). c Radiological features of myeloma bone disease. The left panel shows a computed tomography (CT) image of the cranium. Osteolytic lesions appear as “punched out” holes (indicated by white arrows and a white circle). The middle panel demonstrates widespread tumor dissemination in the central skeleton, using FDG-PET ([18] F-fluorodeoxyglucose positron emission tomography) as imaging tool. Myeloma lesions appear as white spots in ribs, spine, pelvis, shoulder regions and upper legs. The right panel presents a control image from an individual without myeloma, showing that high signal strength in brain (Br), heart, kidneys (Kid) and urinary bladder (all labeled) is normal
Complexity of IL-6 signaling in myeloma cells
Interleukin-6 signals via a heterodimeric IL-6R/gp130 receptor, whose engagement triggers tyrosine phosphorylation of constitutively associated Janus family kinases (JAK). This is followed by activation of downstream effectors, such as signal transducer and activator of transcription (STAT), rat sarcoma virus oncogene homolog (RAS)-mitogen-activated protein kinase (MAPK) and phospatidylinositol 3-kinase (PI3 K)-v-akt murine thymomaviral oncogene homolog (AKT) [11, 13–16]; (Fig. 2a). Stimulation of these effector pathways facilitates myeloma-cell proliferation and survival and limits apoptosis when cells are treated with myeloma drugs such as dexamethasone [17–19]. To fully appreciate the complexity of IL-6 signaling in myeloma cells, it is important to remember that there are two possibilities for assembling a functional IL-6 receptor on the myeloma-cell surface: One leads to so-called classic IL-6 signaling (Fig. 2b) and the other to what has been dubbed IL-6 trans-signaling (Fig. 2c). Like normal T- and B-lymphocytes and normal plasma cells, most myeloma cells are able to undergo classic IL-6 signaling, in which IL-6 binds to its membrane-bound cognate receptor, IL-6R (gp80), which subsequently couples to membrane-bound gp130 to form a functional signaling complex. Additionally, myeloma cells can undergo IL-6 trans-signaling, in which IL-6 in the circulation (blood stream) or the interstitium (extracellular space in tissues) binds to soluble IL-6R (gp55), which is either shed from the surface of IL-6R-expressing cells or produced by alternative splicing of the IL-6R mRNA. Importantly, IL-6 trans-signaling has the capacity to confer IL-6 responsiveness to myeloma cells that may have lost expression of gp80 either during the course of tumor progression or as a consequence of myeloma-cell adaptation to growth in permanent cell culture. Evidence indicates that although IL-6 may be dispensable for some (but not all) human myeloma-cell lines (HMCLs), it is of crucial importance for incipient myeloma cells during tumor development.
Fig. 2.
Key aspects of IL-6 signaling in multiple myeloma. a Interleukin 6 (formerly known as b2-interferon; indicated by black rectangle) is a pro-inflammatory cytokine that stimulates the humoral immune response. IL-6 signals through a cell-surface type I cytokine receptor complex that consists of the ligand-binding IL-6R chain (CD126, gp80; depicted in gray) and the signal-transducing component, gp130 (CD130, black). gp130 is the common signal transducer for several cytokines, including leukemia inhibitory factor (LIF), oncostatin M, IL-11, IL-27 and Kaposi's sarcoma-associated herpes virus interleukin 6-like protein (KSHV-IL6) [111]. Unlike gp80, gp130 is ubiquitously expressed in most tissues. In myeloma cells, IL-6 initiates three different signal transduction cascades—the JAKSTAT, RAS-MAPK and PI3 K-AKT pathways. b In classic IL-6 signaling, IL-6 binds to membrane-bound gp80, which triggers the association of gp80 with gp130 (indicated by horizontal arrows below the middle panel, which denote the lateral movement of gp130 in the cell membrane). This results in receptor activation, JAK phosphor-ylation and downstream signaling. c In IL-6 trans-signaling, IL-6 binds to soluble IL-6R (sIL-6R), which is shorter (gp55) than the membrane-bound receptor (gp80). The IL-6/IL-6R complex then associates with membrane-bound gp130, after which the downstream signaling events depicted in panel A are initiated. IL-6/gp55 can also bind to soluble gp130, and also to a naturally occurring, truncated form of gp130 called gp130-RAPS. The latter is unable to trigger downstream signaling and, therefore, acts as an inhibitor of IL-6 signaling by virtue of removing “active” IL-6 from the circulation. Under normal conditions, the molar ratio of sgp130- and gp130-RAPS-containing complexes is approximately 1:70. The ratio in myeloma patients has not yet been determined. The significance of IL-6 trans-signaling for myeloma cells, particularly at the later stages of tumor progression when gp80 may get lost, is not known. As in classic IL-6 signaling, IL-6 trans-signaling can be maintained by IL-6 from either an autocrine or paracrine source. d Myeloma cells may be supported by two sources of IL-6 in the TME: BMSC-derived “paracrine” IL-6, which is believed to be the main source of the cytokine, and tumor cell-derived “autocrine” IL-6. BMSCs able to release IL-6 into the extracellular space include tumor-associated macrophages (TAM), mast cells (MC), dendritic cells (DC), CD4+ or CD8+ T cells, osteoclasts (OC), osteoblasts and other cell types. An important source of IL-6 is TAMs, which are of prognostic importance in MM [112]. TAMs support myeloma cells [113] by releasing VEGF [114], a potent stimulator of angiogenesis in myeloma [115]. TAMs also protect myeloma cells from drug-induced apoptosis by virtue of adhesion-mediated survival pathways that depend on selectins, such as ICAM-1 and CD18 [116]. MM, just like most types of cancer [117], contain an abundance of Treg cells [118, 119], the function of which is to decrease the immune response. The frequency of Treg cells in the BM is inversely correlated with survival of patients with myeloma; i.e., having fewer Treg cells is a positive prognostic indicator [120, 121]. After ASCT, the frequency of Treg cells rises dramatically [122], suggesting that this subset of T-lymphocytes protects residual post-transplantation myeloma cells from immune-based deletion. Consistent with that hypothesis, Treg cells obtained from MM patients suppress T-cell proliferation in vitro [121]. The role of Th17 cells, a highly inflammatory subset of CD4 T cells, is less clear in myeloma [123]. On the one hand, an increase in Th17 cells is welcomed if one considers that it is usually accompanied by a decrease in Treg cells [123]. On the other hand, Th17 cells have been implicated in promoting MM cell proliferation and perpetuating myeloma bone disease [124, 125]—obviously, an unwelcome feature of inducible Th17 responses in myeloma. The role of CD8 T cells in myeloma is also unclear. On the plus side, the presence of these cells in the TME has been associated with good prognosis of myeloma patients. In keeping with that, clonotypic myeloma-reactive CD8 T cell clones induce apoptosis in myeloma cells in vitro [126]. There is also circumstantial evidence suggesting that CD8 T cells may be able to block the MGUS-to-MM progression during tumor development as long as the incipient myeloma cells maintain sufficient antigen-presentation capability to cytotoxic CD8 T cells [127]. On the minus side, a report on a significant increase in the number of suppressive CD8 T cells in MM suggests that these cells may in fact contribute to both the local immune suppression in the TME and the systemic immune deficiency commonly seen in patients with myeloma [128]
Two principal sources of IL-6 in myeloma
Myeloma progenitors and frank myeloma cells in the bone marrow (BM) microenvironment may take advantage of two different sources of IL-6 to promote tumor development and tumor maintenance in vivo: myeloma-cell-derived, autocrine IL-6 and tumor microenvironment (TME)-derived, paracrine IL-6 released by nonmalignant bystander cells in the myeloma stroma (Fig. 3a). Many studies support a role of autocrine IL-6 in MM. Patient-derived myeloma cells producing IL-6 were found to be resistant to spontaneous and dexamethasone-induced apoptosis, whereas non-IL-6-secreting myeloma cells were sensitive to it [20]. Inhibition of IL-6 signaling in myeloma-cell lines in an in vitro cell culture model of extra-cellular matrix-dependent drug resistance increased their sensitivity to bortezomib [21]. IL-6 conferred protection from FAS-induced apoptosis by virtue of IL-6/JAK/ STAT3-induced up-regulation of the anti-apoptotic protein, Bcl-XL, in myeloma cells [22, 23]. Consistent with this, we have shown that enforced expression of Bcl-XL in plasma cells promotes myeloma-like plasma-cell tumors in transgenic mice [24]. These findings lend credence to the notion that autocrine IL-6 is important for myeloma. Other lines of investigation stress the role of paracrine IL-6 in myeloma. Bone marrow stroma cells (BMSCs) produce high levels of IL-6 [25], which enhances the interaction with and supports the survival of myeloma cells by increasing secretion of growth factors by both cell types. For example, myeloma cells produce vascular endothelial growth factor (VEGF) and fibroblast growth factor (FGF), which, in turn, stimulate IL-6 production by the BMSCs. Elevated IL-6 production by BMSCs then stimulates myeloma cells to secrete additional VEGF and FGF, thus creating a cytokine/growth factor amplification loop in situ [26, 27]. BMSCs harvested from newly diagnosed, untreated MM patients express IL-6 at much higher levels than BMSCs from healthy donors [28]. Moreover, the level of IL-6 production in BM specimens from myeloma patients correlates with clinical disease stage [20]. Altogether, these findings indicate that IL-6, derived from either a malignant plasma cell or the stroma, fosters myeloma development and promotes drug resistance in patients with myeloma.
Fig. 3.
Targeting MRD/MMSC with small-drug inhibitors, immune-based interventions and IL-6-targeted therapies may result in a cure for patients with myeloma. a Curative blueprint for myeloma. The currently available myeloma therapies are highly efficient in killing the great majority of myeloma cells (excentric nucleus, rich cytoplasm, paranuclear Golgi zone) but are unable to eradicate a tiny subpopulation of cells that exhibit stem cell-like features and are called MMSCs. These cells underlie MRD and often acquire drug resistance in the course of myeloma treatment, leading to relapse of a therapy-resistant tumor. Treatments that target MMSC/MRD efficiently may result in a cure for myeloma. Owing to the genetic complexity of myeloma and its perpetual clonal diversification [129– 133], targeted eradication of MRD cells may be best accomplished in an adjuvant setting at a relatively early stage of myeloma treatment. b Two principal forms of MRD/MMSC-targeted therapies: small-drug inhibitors and immunological approaches. Inhibitors target stemness genes, such as MYC (JQ1); stemness pathways, such as Wnt (celecoxib), Notch (BMS-906024) and Hedgehog (itraconazole, cyclopamine); drug resistance pathway, such as multidrug resistance (sildenafil); and, last but not least, individual candidate MMSC genes, such as RARA2 (ATRA), NEK2 (CCT250863) and BTK (ibrutinib). Immune-based therapies for targeting MRD include CAR-T cells and dendritic cell vaccines (see main text for details). Also included is a growing panel of therapeutic monoclonal antibodies exhibiting reactivity to CS1 (elotuzumab), CD38 (daratumumab), CD56 (lorvotuzumab), VEGF (bevacizumab), EGR (cetuximab), KIR (IPH2101), FGFR3 (MFGR1877S), BAFF (LY2127399) and other myeloma targets. To be fully effective, immunotherapy must probably be combined with small-drug inhibitors and IL-6-targeted drugs shown in panel C. c Approaches to inhibit IL-6 signaling in myeloma including cancer stem cell-like cells (bottom) and bone marrow stroma cells (top) [70]. Labeled circles indicate active research areas, which can be categorized as follows: a Tocilizumab is a humanized antibody to IL-6R, which competitively inhibits IL-6 signaling by virtue of binding to the receptor's ligand-binding site [134]. The antibody inhibits both canonical/classical IL-6 signaling and IL-6 trans-signaling because it binds to both cell membrane-bound IL-6R and soluble IL-6R [135]. Tocilizumab has been approved for the treatment of arthritis and is currently undergoing clinical testing for other disease. However, there are no clinical trials of myeloma at this juncture. b Antibodies neutralizing IL-6 include mouse BE-8 (elsilimomab) and siltuximab (CNTO 328, Centocor). Siltuximab is a chimeric human-mouse antibody and thus less immunogenic than BE-8. Siltuximab shows promising activity in MM, even under conditions of dexamethasone-refractory disease [136]. Siltuximab is now in clinical trial for patients with high-risk smoldering myeloma (NCT01484275). A fully humanized, high-affinity derivative of B-E8, designated mAb 1339, has been developed recently. It showed promising preclinical activity in studies using mice and the IL-6-dependent HMCL, INA-6 [137], but has not yet been advanced to clinical testing. A different approach for targeting the IL-6R, which relies on a recombinant protein instead of a monoclonal antibody, is afforded by Sant7. “Sant” stands for super antagonist; i.e., a genetically engineered human IL-6 that binds to gp80 with higher affinity than normal IL-6 does. However, because Sant7 does not recruit gp130 to the IL-6R, it blocks IL-6 signaling. Although Sant7 was highly effective in preclinical model systems of myeloma [138–140], it has not been further developed for clinical applications [70]. c An interesting development is a fusion protein that consists of soluble gp130 (sgp130) linked to the Fc-region of human IgG. The recombinant protein, dubbed FE999301, is jointly being developed for clinical use by CONARIS Research Institute (Kiel, Germany) and Ferring Pharmaceuticals (Saint-Prex, Switzerland) [70]. FE999301 builds on knowledge that sgp130 is a natural inhibitor of IL-6/sIL-6R [141]. FE999301 blocks primarily IL-6 trans-signaling, the main driver of IL-6's inflammatory functions. FE999301 was shown to be effective in a mouse model of inflammation-induced cancer [142]. d Inhibitors of gp130, such as gp130-targeting peptides [143]. e Small-molecule inhibitors that may block IL-6 production in BMSCs. One example is a recently developed indolinone inhibitor that abrogates the kinase activity of FGF and VEGF receptor tyrosine kinases, resulting in disruption of the IL-6/VEGF/FGF amplification loop described in the main text. This, in turn, led to enhanced spontaneous and dexamethasone-induced apoptosis of HMCLs and patient myeloma cells without inducing death in normal cells, such as B-lymphocytes [144]. Similarly, a newly developed histone deacetylase inhibitor dramatically reduces IL-6 production in BMSCs (by 80–95 %), and the subsequent induction of apoptosis in HMCLs and freshly isolated myeloma cells [145]
IL-6 released by BMSCs may contribute to the immunosuppressive milieu in the TME of MM
IL-6 may shape, in part, the complex and poorly understood bidirectional interaction of myeloma cells with the surrounding stroma, which transforms the BM microenvironment into a tumor-promoting, bone-resorbing and immunosuppressive milieu (Fig. 2d). Immunosuppression in the TME of MM may be of great importance for the design and testing of novel myeloma therapies, because it suggests that drug-based approaches for killing myeloma cells should be combined with immune-based interventions to reverse the local immune suppression and unleash an effective anti-myeloma immune response. Besides IL-6-reactive suppressor T cells, such as CD4+ regulatory T (Treg) cells, distinct populations of myeloid cells, designated myeloid-derived suppressor cells, may block anti-myeloma immune responses [29]. Myeloid lineage cells, such as macrophages, mast cells, dendritic cells and eosinophils, have long been recognized as significant sources of IL-6 in the BM microenvironment, and the myeloma-promoting role of eosinophils has been demonstrated recently [30]. Eosinophils were also shown to be critical for maintaining survival niches of normal long-lived plasma cells in the BM [31], by virtue of secreting IL-6, IL-4, APRIL and other cytokines [31]. IL-6 plays an important role in T-cell differentiation and activation; e.g., it functions as a major regulator of the balance between Treg cells and pro-inflammatory, IL-17-producing CD4+ T cells called Th17 cells. In conjunction with transforming growth factor-β, IL-6 stimulates the generation of Th17 cells but inhibits the induction of Treg cells. This results in an IL-6-dependent, pro-inflammatory environment, in which tumor-suppressive Treg responses are down regulated and may facilitate malignant growth, as Th17 cells have been shown to promote colon cancer in humans [32] and mice [33]. On the other hand, Th17 cells have also been implicated as regulators of immune surveillance [34], suggesting that this subset of helper T cells may also have tumor-suppressive functions. What role Th17 cells play in myelomagenesis is not known. The role of CD8 T cells is in myeloma is similarly unclear, with some evidence pointing to tumor inhibition (cytotoxicity to myeloma cells) and other findings pointing to tumor promotion (see legend to Fig. 2d for details). Additional research on the inner mechanics of the immune system in myeloma is certainly warranted. These results and other findings not discussed have generated a great deal of interest in blocking IL-6 production specifically in BMSCs as a means to overcome the immune-suppressive microenvironment in MM.
Role of IL-6 in myeloma stemness, minimal residual disease (MRD) and targeted therapies
A large body of clinical evidence indicates that a small but therapy-resistant subpopulation of myeloma cells comprises the principal roadblock to curing myeloma [35]. Depending on the investigator team, these cells are variably referred to as myeloma-initiating, myeloma-propagating, transit-amplifying, dormant or drug-resistant myeloma cells or, a term the UI Myeloma MOG prefers, multiple myeloma stem cells (MMSCs) [36–40]. The tight association of these cells with minimal residual disease (MRD) [41], acquired drug resistance and relapsed myeloma underscores the urgency to develop new therapies for targeting the MMSC [42] in order to achieve the long-term goal of finding a cure for myeloma (Fig. 3a); [43]. We acknowledge that the MMSC model has not been fully embraced by the myeloma community, owing in part to a lack of a coherent set of criteria for defining these cells unambiguously [44–48]. Nonetheless, the model has catalyzed myeloma research, enhanced our appreciation of the complexity of myeloma biology and promoted the development of small-drug inhibitors and immunotherapies in myeloma (Fig. 3b). The latter include monoclonal antibodies, chimeric antigen receptor (CAR)-T cells and dendritic cell (DC) vaccines. CAR-T cells harbor an engineered T-cell receptor that consists of three parts: the antibody portion, which denotes specificity; a suicide signal for programed cell death; and a co-stimulatory region that contains both CD28, a potent proliferation signal, and 41BB, a critical survival signal [49]. CAR-T cells reactive to CD19 have been successfully used for treatment of B-cell lymphoma [50]. Potential targets for CAR-T cells in myeloma include an isoform of CD44, CD44v6 [51], B-cell maturation antigen (BCMA) [52] and syndecan-1 (CD138) [53]. DC vaccination strategies rely on professional antigen-presenting cells [54] that are generally suppressive in cancer [55] yet critical in the development of functional anti-tumor immune responses [56]. Two methods have been explored to devise DC-based myeloma vaccines. The first involves stimulating DCs ex vivo with tumor cell lysates, which allows the DCs to cross-present the tumor antigens to CD8+ T cells. A phase 2 study using DCs that had been loaded with Id (immunoglobulin idiotype peptides) revealed the vaccine to be safe, albeit not particularly effective [57]. Another study that employed DCs loaded with RNA that encodes certain myeloma antigens (MAGE3, survivin, BCMA) induced the intended immune response in myeloma patients, with 3 of 12 patients experiencing a complete remission and the majority of the remaining patients demonstrating a partial response [58]. The second method relies on the fusion of DCs with myeloma cells, followed by the adoptive transfer of the DC/MM hybrids to patients. This approach has also shown promise in clinical trials, which demonstrated both stabilization of disease due to expansion of activated CD4+ T cells and CTLs in vivo [59] and compatibility with ASCT-based frontline therapies of myeloma [60]. It is possible that the therapeutic approaches depicted in Fig. 3b will synergize with emerging IL-6/JAK/STAT3-targeted drugs to kill MMSCs in BM survival niches. However, more needs to be learned about the specific role of IL-6 in MMSCs before combination therapies of this sort can be seriously considered. The importance of IL-6 for breast cancer stem cells [61, 62], including mammosphere-based in vitro models of breast cancer stemness [63], is firmly established. IL-6/JAK/STAT3 signaling also plays an important role in cancer stem cell-like cells in lung cancer [64], colon cancer [65, 66], glioblastoma [67] and liver cancer [68]. These studies provide a blueprint for future work aimed at elucidating the role of IL-6 in MMSCs.
Emerging IL-6 inhibitory strategies to treat and prevent myeloma
The considerations presented above suggest that targeting IL-6 production in the TME affords a viable strategy for the treatment and prevention of MM. Indeed, the lingering pessimism that followed the disappointing results of early clinical trials using an IL-6-targeted monoclonal antibody in myeloma patients [69] has recently been lifted as a consequence of exciting new results with agents that either nonspecifically inhibit IL-6 as part of their highly pleio-tropic action (e.g., lenalidomide and related immunomodulatory drugs) or specifically target IL-6 in both myeloma and BMSCs [70]. Specific inhibition of IL-6 can be achieved with monoclonal antibodies (mAbs) to IL-6 (siltuximab) or the IL-6R (tocilizumab), with recombinant proteins that function as IL-6R antagonists, or with small molecules that inhibit the cellular IL-6 signal transduction pathway or the cross talk of that pathway with other signaling networks in myeloma (Fig. 3c). Among the recombinant proteins mentioned above is Sant-7, FE999301, and a newly designed immunotoxin, designated IL6(T23)-PE38KDEL, that consists of IL-6 and Pseudo-monas exotoxin and exhibits efficacy in a mouse models of MM [71]. Small-molecule inhibitors of IL-6 signaling include drugs that target JAK tyrosine kinases, which are now in clinical trial for lymphoma [72], but also show promise for myeloma as evidenced by down-regulation of survival and angiogenesis pathways in myeloma [73–75]. Additional therapeutic opportunities (not included in Fig. 3c) are provided by compounds that either inhibit biochemical pathways that can activate IL-6 signaling indirectly (e.g., NFjB inhibitors [76], such as 6-amino-4- quinazoline [77]; Hsp90 inhibitors, such as SNX-2112 [78]; PI3 K/mTor inhibitors, such as NVP-BEZ235 [79]) or activate biochemical pathways that can inhibit IL-6 signaling indirectly (e.g., PPARc inhibitors [80]). The most effective use of new IL-6-targeted therapies will depend in large measure on enhanced understanding of the biological role of IL-6 in myeloma, and on identifying the patients that may benefit the most. We believe the mouse models described in the following will make a nice contribution to the preclinical validation of IL-6-targeted therapies for myeloma.
IL-6-dependent plasma-cell tumors (PCTs) in laboratory mice
Building on the classic mouse model of inflammation-induced peritoneal plasmacytoma in BALB/c (C) mice developed by Dr. Michael Potter at the US National Cancer Institute [81], we have recently generated a number of IL-6 dependent genetically engineered mouse models of human myeloma, which lend themselves to addressing knowledge gaps on the role of IL-6 in myeloma development and therapy. Evidence for the pathogenetic significance of IL-6 in both the widely known “Potter tumors” and the newly generated transgenic tumors ranges from studies in normal C mice (carried out in the 1980s) showing that the growth of plasmacytoma in vivo is enhanced by exogenous IL-6 but inhibited by antibodies to either IL-6 or the IL-6 receptor [82]; across studies in IL-6 deficient C mice (1990s) demonstrating that mice homozygous for a null allele of Il6 are resistant to both inflammation-induced plasmacytoma [83] and Myc/Raf retrovirus-induced plasmacytoma [84]; to studies in IL-6 transgenic mice (2000s) indicating that C mice carrying a widely expressed human IL-6 transgene designated H2-Ld-IL6 develop plasmacytoma spontaneously [85]. We reported some time ago that iMycEμ-induced peritoneal plasmacytoma is greatly accelerated by chronic granulomatous inflammation [86], a process that is known to produce copious amounts of IL-6 at the site of tumor development [87, 88]. Our most recent, unpublished findings indicate that two closely related mouse strains, iMycΔEμ and iMycCα [89], are as hyper-susceptible to plasmacytoma as iMycEμ mice are (Fig. 4). In agreement with that, all three iMyc alleles collaborate effectively with enforced IL-6 expression (H2-Ld-IL6 transgene) in malignant plasma-cell transformation [90, 91]. Indeed, the double-transgenic iMycIL-6 strains of mice provide a robust experimental model system characterized by short time to tumor onset and complete penetrance of the malignant phenotype (100 % tumor incidence) that is now available for preclinical studies on IL-6-targeted therapies in myeloma. The utility of this model system will be illustrated below, following a brief description of Potter's classic mouse models of MM.
Fig. 4.
Peritoneal plasmacytoma in pristane-treated C.iMycΔEμ mice. Low-power microscopy (a) shows that inflammatory granulomas in the peritoneal cavity are densely infiltrated with neoplastic plasma cells. Higher magnification (b) demonstrates an area in a granuloma in which relatively normal looking plasma cells (concentrated in the center) border on sheets of aberrant blast-like plasma cells (bottom). The cytological features of the latter include eccentric nuclei containing prominent nucleoli (c)
Peritoneal plasmacytoma in inbred BALB/c mice
The classic model system of neoplastic plasma-cell development in laboratory mice is peritoneal plasmacytomagenesis in strain C (Fig. 5); [92]. Unlike most common inbred mice, the C strain is highly susceptible to peritoneal plasmacytoma [93]. The underlying genetic trait is complex and includes hypomorphic (weak-efficiency) alleles of genes that encode the cell-cycle inhibitor p16INK4a [94] and the FKBP12 rapamycin-associated protein Frap [95]. Virtually all peritoneal plasmacytomas harbor a Myc-activating chromosomal translocation [96], which takes the form of a T(12;15)(Igh-Myc) in the majority (~85 %) of cases. The development of plasma-cytoma requires maintenance of the mice in a “dirty” non-SPF (specific pathogen-free) colony, i.e., one that is rich in gut flora; this environment is thought to promote tumori-genesis by exposing the mice to environmental stimuli including gut flora-derived antigen [97]. Consistent with this notion, C mice raised in “gut flora-poor” conditions (either SPF or germ-free) either exhibit a dramatically reduced plasmacytoma incidence [98] or are completely free of tumors [99]. Peritoneal plasmacytomas do not develop spontaneously but can be readily induced by intraperitoneal (i.p.) administration of pro-inflammatory agents such as pristane [100]. Pristane acts by provoking the formation of a chronic granulomatous tissue, which serves as a microenvironment conducive to plasmacytoma development [101]. The administration of steroidal anti-inflammatory drugs, such as cortisol, to pristane-treated mice abrogates plasmacytoma by preventing the development of granulomas [102], and dietary depletion of the micronutrient selenium in mice has similar effects [103]. Treatment of pristane-primed mice with nonsteroidal anti-inflammatory drugs, such as the cyclooxygenase-2 inhibitors indomethacin and sulindac, also abrogates plasmacytoma, but in this case without preventing granuloma formation [104]. The fact that key properties of plasma-cytoma point to IL-6 as a critical regulator of tumorigenesis indicates that this model is valuable for studies on IL-6-based approaches to myeloma prevention. However, this model of plasma-cell neoplasia also has practical limitations that seriously compromise its utility in the laboratory. These include incomplete penetrance (tumor incidence ≤60 %), long tumor latency (220 days on average) and, sometimes, poor reproducibility between experiments.
Fig. 5.
Histogenesis and diagnosis of peritoneal plasmacytoma in inbred BALB/c (C) mice. a Histological section of inflammatory granuloma on day 20 post-tumor induction using pristane (H&E, 20×). A large pristane vacuole (labeled) is walled off by stroma. Plasma cells are not present at this stage of tumor development. b Small focus of immunostained, j light chain-producing, premalignant plasma cells (surrounded by thick black oval) on day 85 post-tumor induction (40×). c Histological section of a primary plasmacytoma that developed in the inflammatory pristane oil granuloma by day 220 post-tumor induction (H&E, 40×). e Plasmacytoma cells with typical paranuclear halo (arrow), among macrophages and small lymphocytes in a Giemsa-stained cytofuge specimen of peritoneal exudate cells (80×)
Accelerated transgenic mouse models of IL-6-driven PCT
Following up on reports that IL-6 promotes IgA+ plasma-cell production in the gut-associated lymphatic tissue (GALT) [105], we turned our attention to mice that carry a widely expressed human IL-6 transgene [106, 107]. We found that the IL-6 transgenic C mice develop plasmacytoma spontaneously [85], with most [85] but not all [108] tumors carrying a Myc-activating T(12;15) translocation. The tumors developed predominantly in the GALT, followed by systemic dissemination of malignant plasma cells in bone marrow and other tissue sites. Although these results further validated IL-6 as a key driver of plasma-cell neoplasia, this model exhibited the same practical limitations in terms of tumor incidence and long latency mentioned above. In a parallel line of investigation, we used gene targeting in mice to recapitulate the fine structure of the T(12;15) translocation found in classic and IL6-transgenic plasmacytoma: the head-to-head juxtaposition of Myc and the immunoglobulin heavy-chain locus, Igh. The gene-targeted mice, designated iMyc, contain a His6-tagged mouse Myc cDNA, MycHis, inserted head-to-head in Igh [24, 109, 110]. Three different iMyc alleles were produced: iMycEμ, iMycΔEμ and iMycCα [89]. Transfer of the iMyc transgenes from the original, mixed genetic background of segregating C57BL/6 × 129/SvJ alleles to the C background resulted in hypersusceptibility to inflammation-induced PCT. One of the newly developed, double-transgenic strains of iMycIL-6 mice, which was investigated in greater depth, is prone to myeloma bone disease [91], a shortcoming of many previously developed GEMMs of human myeloma. We are currently employing this strain to continue with the IL-6 theme, which includes a study on the biological significance of autocrine versus paracrine sources of IL-6 in tumor development (Fig. 6).
Fig. 6.
Evaluating the role of B-cell-derived “autocrine” IL-6 and TME-derived “paracrine” IL-6 in PCT development in mice. a Rationale for, and overview of, experimental model. Motivated by the increasing push in the cancer genetics community to supplement the widely used but time-consuming “conventional” or “germline” transgenic mouse models of human cancer with more flexible and less expensive “nongermline” models [146], we developed such a model for the in vivo validation of myeloma genes, such as IL-6. The cornerstone of the new method is adoptive B-cell transfer. Mature, iMyc-transgenic CD45.2+ B-lymphocytes genetically “hard wired” to undergo malignant cell transformation are transferred to CD45.1+ hosts, in which the cells complete neoplastic transformation. The donor B cell can be genetically modified in vitro by virtue of retro- or lentiviral gene transduction (not shown). The new method affords several advantages, including a the use of B cells and hosts genetically deficient in key factors of the myeloma development (IL-6 deficiency in this case) and b the generation of “waves” of genetically tagged PCTs in a predictable, timely, economic fashion. The allotypic difference of CD45.1 (host) and CD45.2 (donor B cell) is used as marker in this case. Note that one donor mouse suffices to reconstitute up to 20 hosts. B cells are isolated using MACSÒ magnetic bead columns and transferred to sub-lethally irradiated (4.5 Gy) C.CD45.1+ congenic mice (kind gift of Dr. Lyse Norian, UI) treated one week later with 0.2 ml pristane ip. b Flow cytometry contour plots 138 days post-B-cell transfer, indicating the presence of a CD45.2+CD138+ PCT in a CD45.1+ C mouse. Approximately 80 % of CD45.2-gated cells expressed high levels of the PC marker syndecan-1 (CD138). c Shown to the left is a tissue section of a representative CD45.2+ tumor (from a peripheral lymph node in this case) from a CD45.1+ C mouse (H&E; 63×). Shown to the right is a serum electropherogram indicating transplantability of PCT. The electropherogram contains at the bottom the M-spike (boxed) of a mouse that harbored a primary (G0) CD45.2+ tumor (lane 2) as well as the same M-spike from a C mouse 5 weeks after transfer of one million tumor cells harboring the transplanted (G1) tumor (lane 3). A serum sample from a normal C mice was included as control (lane 1). d Ongoing study of TRR's thesis project on the specific roles of autocrine and paracrine IL-6 in tumor development. Myc-transgenic B220+ splenocytes proficient for IL-6 (IL-6+) or deficient for IL-6 (IL-6−) were transferred to sublethally irradiated and pristane-primed hosts that were either able to produce IL-6 (IL-6+) or unable to produce it (IL-6−). The endpoints of the study include tumor incidence, tumor onset and tumor pattern. Transfer of IL-6+ B cells to IL-6− hosts results in a situation in which incipient PCT cells must rely on autocrine IL-6 for tumor development. Conversely, transfer of IL-6− B cells to IL-6+ hosts generates a system in which oncogenesis depends on paracrine supply of IL-6. Preliminary results indicate that paracrine IL-6 is more important for tumor development than B-cell-derived IL-6. This result, which is currently prepared for publication in an original research article, has interesting implications for IL-6-targeted therapies in human myeloma
Conclusion
Interleukin-6-dependent mouse models of human myeloma may further our understanding of the role of IL-6 in the natural history of myeloma and permit us to test emerging IL-6/JAK/STAT3-targeted therapies in the genetically and environmentally controlled setting of a preclinical mouse study. Immune-competent mouse models of myeloma, such as iMycIL6, may also provide a good opportunity to elucidate the mechanism by which the pro-inflammatory, immune-suppressive bone marrow microenvironment promotes myeloma development and acquisition of drug resistance in myeloma. In keeping with the spirit of the recently proposed blueprint for a cure of myeloma [43], IL-6-targeted therapies may afford further improvements for patients with MM. A potentially promising approach is therapies that combine the targeting of IL-6 in the myeloma microenvironment with immune-based strategies for eradicating MM stem cells and minimal residual disease. However, despite enormous progress in cancer immuno-therapy in the past few years, additional research is warranted to translate this promise to myeloma. Outstanding problems include the optimization of DC vaccination methods (e.g., development of more effective delivery vehicles) and the incorporation of CAR-T cells in therapeutic regimens that mainly rely at this juncture on monoclonal antibodies. The success and failure of the much heralded new era of individualized myeloma therapy will depend, in part, on the effective collaboration of basic, translational and clinical scientists in innovative frameworks such as the UI Myeloma MOG.
Acknowledgments
This research was performed by TRR in partial fulfillment of the requirements for the degree Doctor of Philosophy in the Graduate Immunology Program of the University of Iowa. He wishes to thank Dr. Kristin Ness for expert technical assistance and mouse husbandry. This work was supported in part by NIH Predoctoral Training Grant 5T32 AI007485 (to TRR), by R01CA152105 from the NCI (to FZ); by a Translational Research Program award from the Leukemia and Lymphoma Society (to FZ); by institutional start-up funds from the Department of Internal Medicine, Carver School of Medicine, University of Iowa (to FZ and GT); by P30CA086862 from the NCI; by a Senior Research Award from the Multiple Myeloma Research Foundation (to SJ); by a career development award from NCI P50CA097274 (to SJ); and by R01CA151354 from the NCI (to SJ).
Biography
Timothy R. Rosean Siegfried Janz

Footnotes
Conflict of interest The authors declare no competing financial interest.
Contributor Information
Timothy R. Rosean, Interdisciplinary Graduate Program in Immunology, Carver College of Medicine, University of Iowa, Iowa City, IA, USA
Van S. Tompkins, Department of Pathology, Carver College of Medicine, University of Iowa, Iowa City, IA, USA
Guido Tricot, Department of Internal Medicine, Carver College of Medicine, University of Iowa, Iowa City, IA, USA; Myeloma Multidisciplinary Oncology Group, Holden Comprehensive Cancer Center, University of Iowa, 500 Newton Road, 1030 Medical Laboratories, Iowa City, IA 52242, USA.
Carol J. Holman, Department of Pathology, Carver College of Medicine, University of Iowa, Iowa City, IA, USA Myeloma Multidisciplinary Oncology Group, Holden Comprehensive Cancer Center, University of Iowa, 500 Newton Road, 1030 Medical Laboratories, Iowa City, IA 52242, USA.
Alicia K. Olivier, Department of Pathology, Carver College of Medicine, University of Iowa, Iowa City, IA, USA
Fenghuang Zhan, Department of Internal Medicine, Carver College of Medicine, University of Iowa, Iowa City, IA, USA; Myeloma Multidisciplinary Oncology Group, Holden Comprehensive Cancer Center, University of Iowa, 500 Newton Road, 1030 Medical Laboratories, Iowa City, IA 52242, USA.
Siegfried Janz, Interdisciplinary Graduate Program in Immunology, Carver College of Medicine, University of Iowa, Iowa City, IA, USA; Department of Pathology, Carver College of Medicine, University of Iowa, Iowa City, IA, USA; Myeloma Multidisciplinary Oncology Group, Holden Comprehensive Cancer Center, University of Iowa, 500 Newton Road, 1030 Medical Laboratories, Iowa City, IA 52242, USA.
References
- 1.Hong DS, Angelo LS, Kurzrock R. Interleukin-6 and its receptor in cancer: implications for translational therapeutics. Cancer. 2007;110:1911–28. doi: 10.1002/cncr.22999. [DOI] [PubMed] [Google Scholar]
- 2.Kurzrock R, Redman J, Cabanillas F, Jones D, Rothberg J, Talpaz M. Serum interleukin 6 levels are elevated in lymphoma patients and correlate with survival in advanced Hodgkin's disease and with B symptoms. Cancer Res. 1993;53:2118–22. [PubMed] [Google Scholar]
- 3.Lam LT, Wright G, Davis RE, Lenz G, Farinha P, Dang L, Chan JW, Rosenwald A, Gascoyne RD, Staudt LM. Cooperative signaling through the signal transducer and activator of transcription 3 and nuclear factor-{kappa}B pathways in subtypes of diffuse large B-cell lymphoma. Blood. 2008;111:3701–13. doi: 10.1182/blood-2007-09-111948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nishimoto N, Kanakura Y, Aozasa K, Johkoh T, Nakamura M, Nakano S, Nakano N, Ikeda Y, Sasaki T, Nishioka K, Hara M, Taguchi H, Kimura Y, Kato Y, Asaoku H, Kumagai S, Kodama F, Nakahara H, Hagihara K, Yoshizaki K, Kishimoto T. Humanized anti-interleukin-6 receptor antibody treatment of multicentric Castleman disease. Blood. 2005;106:2627–32. doi: 10.1182/blood-2004-12-4602. [DOI] [PubMed] [Google Scholar]
- 5.Klein B, Tarte K, Jourdan M, Mathouk K, Moreaux J, Jourdan E, Legouffe E, De Vos J, Rossi JF. Survival and proliferation factors of normal and malignant plasma cells. Int J Hematol. 2003;78:106–13. doi: 10.1007/BF02983377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chen-Kiang S. Plasma cells and multiple myeloma. Immunol Rev. 2003;194:5–7. doi: 10.1034/j.1600-065x.2003.00065.x. [DOI] [PubMed] [Google Scholar]
- 7.Lowik CW, van der Pluijm G, Bloys H, Hoekman K, Bijvoet OL, Aarden LA, Papapoulos SE. Parathyroid hormone (PTH) and PTH-like protein (PLP) stimulate interleukin-6 production by osteogenic cells: a possible role of interleukin-6 in osteoclastogenesis. Biochem Biophys Res Commun. 1989;162:1546–52. doi: 10.1016/0006-291x(89)90851-6. [DOI] [PubMed] [Google Scholar]
- 8.Hardin J, MacLeod S, Grigorieva I, Chang R, Barlogie B, Xiao H, Epstein J. Interleukin-6 prevents dexamethasone-induced myeloma cell death. Blood. 1994;84:3063–70. [PubMed] [Google Scholar]
- 9.Klein B, Zhang XG, Lu ZY, Bataille R. Interleukin-6 in human multiple myeloma. Blood. 1995;85:863–72. [PubMed] [Google Scholar]
- 10.Lichtenstein A, Tu Y, Fady C, Vescio R, Berenson J. Interleukin-6 inhibits apoptosis of malignant plasma cells. Cell Immunol. 1995;162:248–55. doi: 10.1006/cimm.1995.1076. [DOI] [PubMed] [Google Scholar]
- 11.Kishimoto T. Interleukin-6: from basic science to medicine—40 years in immunology. Annu Rev Immunol. 2005;23:1–21. doi: 10.1146/annurev.immunol.23.021704.115806. [DOI] [PubMed] [Google Scholar]
- 12.Ishikawa H, Tsuyama N, Kawano MM. Interleukin-6-induced proliferation of human myeloma cells associated with CD45 molecules. Int J Hematol. 2003;78:95–105. doi: 10.1007/BF02983376. [DOI] [PubMed] [Google Scholar]
- 13.Berger LC, Hawley TS, Lust JA, Goldman SJ, Hawley RG. Tyrosine phosphorylation of JAK-TYK kinases in malignant plasma cell lines growth-stimulated by interleukins 6 and 11. Biochem Biophys Res Commun. 1994;202:596–605. doi: 10.1006/bbrc.1994.1970. [DOI] [PubMed] [Google Scholar]
- 14.Ogata A, Chauhan D, Teoh G, Treon SP, Urashima M, Schlossman RL, Anderson KC. IL-6 triggers cell growth via the Ras-dependent mitogen-activated protein kinase cascade. J Immunol. 1997;159:2212–21. [PubMed] [Google Scholar]
- 15.Chauhan D, Kharbanda S, Ogata A, Urashima M, Teoh G, Robertson M, Kufe DW, Anderson KC. Interleukin-6 inhibits FAS-induced apoptosis and stress-activated protein kinase activation in multiple myeloma cells. Blood. 1997;89:227–34. [PubMed] [Google Scholar]
- 16.Hideshima T, Nakamura N, Chauhan D, Anderson KC. Biologic sequelae of interleukin-6 induced PI3-K/Akt signaling in multiple myeloma. Oncogene. 2001;20:5991–6000. doi: 10.1038/sj.onc.1204833. [DOI] [PubMed] [Google Scholar]
- 17.Juge-Morineau N, Francois S, Puthier D, Godard A, Bataille R, Amiot M. The gp 130 family cytokines IL-6, LIF and OSM but not IL-11 can reverse the anti-proliferative effect of dexamethasone on human myeloma cells. Br J Haematol. 1995;90:707–10. doi: 10.1111/j.1365-2141.1995.tb05605.x. [DOI] [PubMed] [Google Scholar]
- 18.Urashima M, Teoh G, Chauhan D, Hoshi Y, Ogata A, Treon SP, Schlossman RL, Anderson KC. Interleukin-6 overcomes p21WAF1 upregulation and G1 growth arrest induced by dexamethasone and interferon-gamma in multiple myeloma cells. Blood. 1997;90:279–89. [PubMed] [Google Scholar]
- 19.Chauhan D, Pandey P, Hideshima T, Treon S, Raje N, Davies FE, Shima Y, Tai YT, Rosen S, Avraham S, Kharbanda S, Anderson KC. SHP2 mediates the protective effect of interleukin-6 against dexamethasone-induced apoptosis in multiple myeloma cells. J Biol Chem. 2000;275:27845–50. doi: 10.1074/jbc.M003428200. [DOI] [PubMed] [Google Scholar]
- 20.Frassanito MA, Cusmai A, Iodice G, Dammacco F. Autocrine interleukin-6 production and highly malignant multiple myeloma: relation with resistance to drug-induced apoptosis. Blood. 2001;97:483–9. doi: 10.1182/blood.v97.2.483. [DOI] [PubMed] [Google Scholar]
- 21.Voorhees PM, Chen Q, Kuhn DJ, Small GW, Hunsucker SA, Strader JS, Corringham RE, Zaki MH, Nemeth JA, Orlowski RZ. Inhibition of interleukin-6 signaling with CNTO 328 enhances the activity of bortezomib in preclinical models of multiple myeloma. Clin Cancer Res. 2007;13:6469–78. doi: 10.1158/1078-0432.CCR-07-1293. [DOI] [PubMed] [Google Scholar]
- 22.Catlett-Falcone R, Landowski TH, Oshiro MM, Turkson J, Levitzki A, Savino R, Ciliberto G, Moscinski L, Fernandez-Luna JL, Nunez G, Dalton WS, Jove R. Constitutive activation of Stat3 signaling confers resistance to apoptosis in human U266 myeloma cells. Immunity. 1999;10:105–15. doi: 10.1016/s1074-7613(00)80011-4. [DOI] [PubMed] [Google Scholar]
- 23.Cheung WC, Van Ness B. Distinct IL-6 signal transduction leads to growth arrest and death in B cells or growth promotion and cell survival in myeloma cells. Leukemia. 2002;16:1182–8. doi: 10.1038/sj.leu.2402481. [DOI] [PubMed] [Google Scholar]
- 24.Cheung WC, Kim JS, Linden M, Peng L, Van Ness B, Polakiewicz RD, Janz S. Novel targeted deregulation of c-Myc cooperates with Bcl-X(L) to cause plasma cell neoplasms in mice. J Clin Invest. 2004;113:1763–73. doi: 10.1172/JCI20369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lu Y, Zhang J, Dai J, Dehne LA, Mizokami A, Yao Z, Keller ET. Osteoblasts induce prostate cancer proliferation and PSA expression through interleukin-6-mediated activation of the androgen receptor. Clin Exp Metastasis. 2004;21:399–408. doi: 10.1007/s10585-005-0056-6. [DOI] [PubMed] [Google Scholar]
- 26.Bisping G, Leo R, Wenning D, Dankbar B, Padro T, Kropff M, Scheffold C, Kroger M, Mesters RM, Berdel WE, Kienast J. Paracrine interactions of basic fibroblast growth factor and interleukin-6 in multiple myeloma. Blood. 2003;101:2775–83. doi: 10.1182/blood-2002-09-2907. [DOI] [PubMed] [Google Scholar]
- 27.Dankbar B, Padro T, Leo R, Feldmann B, Kropff M, Mesters RM, Serve H, Berdel WE, Kienast J. Vascular endothelial growth factor and interleukin-6 in paracrine tumor-stromal cell interactions in multiple myeloma. Blood. 2001;95:2630–6. [PubMed] [Google Scholar]
- 28.Arnulf B, Lecourt S, Soulier J, Ternaux B, Lacassagne MN, Crinquette A, Dessoly J, Sciaini AK, Benbunan M, Chomienne C, Fermand JP, Marolleau JP, Larghero J. Phenotypic and functional characterization of bone marrow mesenchymal stem cells derived from patients with multiple myeloma. Leukemia. 2007;21:158–63. doi: 10.1038/sj.leu.2404466. [DOI] [PubMed] [Google Scholar]
- 29.Gorgun GT, Whitehill G, Anderson JL, Hideshima T, Maguire C, Laubach J, Raje N, Munshi NC, Richardson PG, Anderson KC. Tumor-promoting immune-suppressive myeloid-derived suppressor cells in the multiple myeloma microenvironment in humans. Blood. 2013;121:2975–87. doi: 10.1182/blood-2012-08-448548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wong TW, Kita H, Hanson CA, Walters DK, Arendt BK, Jelinek DF. Induction of malignant plasma cell proliferation by eosinophils. PLoS ONE. 2013;8:e70554. doi: 10.1371/journal.pone.0070554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chu VT, Frohlich A, Steinhauser G, Scheel T, Roch T, Fillatreau S, Lee JJ, Lohning M, Berek C. Eosinophils are required for the maintenance of plasma cells in the bone marrow. Nat Immunol. 2011;12:151–9. doi: 10.1038/ni.1981. [DOI] [PubMed] [Google Scholar]
- 32.Tosolini M, Kirilovsky A, Mlecnik B, Fredriksen T, Mauger S, Bindea G, Berger A, Bruneval P, Fridman WH, Pages F, Galon J. Clinical impact of different classes of infiltrating T cytotoxic and helper cells (Th1, th2, treg, th17) in patients with colorectal cancer. Cancer Res. 2011;71:1263–71. doi: 10.1158/0008-5472.CAN-10-2907. [DOI] [PubMed] [Google Scholar]
- 33.Grivennikov SI, Wang K, Mucida D, Stewart CA, Schnabl B, Jauch D, Taniguchi K, Yu GY, Osterreicher CH, Hung KE, Datz C, Feng Y, Fearon ER, Oukka M, Tessarollo L, Coppola V, Yarovinsky F, Cheroutre H, Eckmann L, Trinchieri G, Karin M. Adenoma-linked barrier defects and microbial products drive IL-23/IL-17-mediated tumour growth. Nature. 2012;491:254–8. doi: 10.1038/nature11465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Martin-Orozco N, Muranski P, Chung Y, Yang XO, Yamazaki T, Lu S, Hwu P, Restifo NP, Overwijk WW, Dong C. T helper 17 cells promote cytotoxic T cell activation in tumor immunity. Immunity. 2009;31:787–98. doi: 10.1016/j.immuni.2009.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mahindra A, Laubach J, Raje N, Munshi N, Richardson PG, Anderson K. Latest advances and current challenges in the treatment of multiple myeloma. Nat Rev Clin Oncol. 2012;9:135–43. doi: 10.1038/nrclinonc.2012.15. [DOI] [PubMed] [Google Scholar]
- 36.Bergsagel DE, Valeriote FA. Growth characteristics of a mouse plasma cell tumor. Cancer Res. 1968;28:2187–96. [PubMed] [Google Scholar]
- 37.Billadeau D, Ahmann G, Greipp P, Van Ness B. The bone marrow of multiple myeloma patients contains B cell populations at different stages of differentiation that are clonally related to the malignant plasma cell. J Exp Med. 1993;178:1023–31. doi: 10.1084/jem.178.3.1023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Matsui W, Huff CA, Wang Q, Malehorn MT, Barber J, Tanhehco Y, Smith BD, Civin CI, Jones RJ. Characterization of clonogenic multiple myeloma cells. Blood. 2004;103:2332–6. doi: 10.1182/blood-2003-09-3064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Agarwal JR, Matsui W. Multiple myeloma: a paradigm for translation of the cancer stem cell hypothesis. Anticancer Agents Med Chem. 2010;10:116–20. doi: 10.2174/187152010790909344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Boucher K, Parquet N, Widen R, Shain K, Baz R, Alsina M, Koomen J, Anasetti C, Dalton W, Perez LE. Stemness of B-cell progenitors in multiple myeloma bone marrow. Clin Cancer Res. 2012;18:6155–68. doi: 10.1158/1078-0432.CCR-12-0531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Munshi NC, Anderson KC. Minimal residual disease in multiple myeloma. J Clin Oncol. 2013;31:2523–6. doi: 10.1200/JCO.2013.49.2124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cruz RD, Tricot G, Zangari M, Zhan F. Progress in myeloma stem cells. Am J Blood Res. 2011;1:135–45. [PMC free article] [PubMed] [Google Scholar]
- 43.Roschewski M, Korde N, Wu SP, Landgren O. Pursuing the curative blueprint for early myeloma. Blood. 2013;122:486–90. doi: 10.1182/blood-2013-01-481291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Yaccoby S. The phenotypic plasticity of myeloma plasma cells as expressed by dedifferentiation into an immature, resilient, and apoptosis-resistant phenotype. Clin Cancer Res. 2005;11:7599–606. doi: 10.1158/1078-0432.CCR-05-0523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Matsui W, Wang Q, Barber JP, Brennan S, Smith BD, Borrello I, McNiece I, Lin L, Ambinder RF, Peacock C, Watkins DN, Huff CA, Jones RJ. Clonogenic multiple myeloma progenitors, stem cell properties, and drug resistance. Cancer Res. 2008;68:190–7. doi: 10.1158/0008-5472.CAN-07-3096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kim D, Park CY, Medeiros BC, Weissman IL. CD19-CD45 low/− CD38 high/CD138+ plasma cells enrich for human tumorigenic myeloma cells. Leukemia. 2012;26:2530–7. doi: 10.1038/leu.2012.140. [DOI] [PubMed] [Google Scholar]
- 47.Van Valckenborgh E, Matsui W, Agarwal P, Lub S, Dehui X, De Bruyne E, Menu E, Empsen C, van Grunsven L, Agarwal J, Wang Q, Jernberg-Wiklund H, Vanderkerken K. Tumor-initiating capacity of CD138- and CD138+ tumor cells in the 5T33 multiple myeloma model. Leukemia. 2012;26:1436–9. doi: 10.1038/leu.2011.373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Tanno T, Lim Y, Wang Q, Chesi M, Bergsagel PL, Matthews G, Johnstone RW, Ghosh N, Borrello I, Huff CA, Matsui W. Growth Differentiating Factor 15 enhances the tumor initiating and self-renewal potential of multiple myeloma cells. Blood. 2013;123:725–33. doi: 10.1182/blood-2013-08-524025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Budde LE, Berger C, Lin Y, Wang J, Lin X, Frayo SE, Brouns SA, Spencer DM, Till BG, Jensen MC, Riddell SR, Press OW. Combining a CD20 chimeric antigen receptor and an inducible caspase 9 suicide switch to improve the efficacy and safety of T cell adoptive immunotherapy for lymphoma. PLoS ONE. 2013;8:e82742. doi: 10.1371/journal.pone.0082742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kochenderfer JN, Wilson WH, Janik JE, Dudley ME, Stetler-Stevenson M, Feldman SA, Maric I, Raffeld M, Nathan DA, Lanier BJ, Morgan RA, Rosenberg SA. Eradication of B-lineage cells and regression of lymphoma in a patient treated with autologous T cells genetically engineered to recognize CD19. Blood. 2010;116:4099–102. doi: 10.1182/blood-2010-04-281931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Casucci M, Nicolis di Robilant B, Falcone L, Camisa B, Norelli M, Genovese P, Gentner B, Gullotta F, Ponzoni M, Bernardi M, Marcatti M, Saudemont A, Bordignon C, Savoldo B, Ciceri F, Naldini L, Dotti G, Bonini C, Bondanza A. CD44v6-targeted T cells mediate potent antitumor effects against acute myeloid leukemia and multiple myeloma. Blood. 2013;122:3461–72. doi: 10.1182/blood-2013-04-493361. [DOI] [PubMed] [Google Scholar]
- 52.Carpenter RO, Evbuomwan MO, Pittaluga S, Rose JJ, Raffeld M, Yang S, Gress RE, Hakim FT, Kochenderfer JN. B-cell maturation antigen is a promising target for adoptive T-cell therapy of multiple myeloma. Clin Cancer Res. 2013;19:2048–60. doi: 10.1158/1078-0432.CCR-12-2422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Davila ML, Bouhassira DC, Park JH, Curran KJ, Smith EL, Pegram HJ, Brentjens R. Chimeric antigen receptors for the adoptive T cell therapy of hematologic malignancies. Int J Hematol. 2013;99:361–71. doi: 10.1007/s12185-013-1479-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Steinman RM, Cohn ZA. Identification of a novel cell type in peripheral lymphoid organs of mice. I. Morphology, quantitation, tissue distribution. J Exp Med. 1973;137:1142–62. doi: 10.1084/jem.137.5.1142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ostrand-Rosenberg S, Sinha P, Beury DW, Clements VK. Cross-talk between myeloid-derived suppressor cells (MDSC), macrophages, and dendritic cells enhances tumor-induced immune suppression. Semin Cancer Biol. 2012;22:275–81. doi: 10.1016/j.semcancer.2012.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Spel L, Boelens JJ, Nierkens S, Boes M. Antitumor immune responses mediated by dendritic cells: how signals derived from dying cancer cells drive antigen cross-presentation. Oncoimmunology. 2013;2:e26403. doi: 10.4161/onci.26403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Zahradova L, Mollova K, Ocadlikova D, Kovarova L, Adam Z, Krejci M, Pour L, Krivanova A, Sandecka V, Hajek R. Efficacy and safety of Id-protein-loaded dendritic cell vaccine in patients with multiple myeloma—phase IIstudy results. Neoplasma. 2012;59:440–9. doi: 10.4149/neo_2012_057. [DOI] [PubMed] [Google Scholar]
- 58.Hobo W, Strobbe L, Maas F, Fredrix H, Greupink-Draaisma A, Esendam B, de Witte T, Preijers F, Levenga H, van Rees B, Raymakers R, Schaap N, Dolstra H. Immunogenicity of dendritic cells pulsed with MAGE3, survivin and B-cell maturation antigen mRNA for vaccination of multiple myeloma patients. Cancer Immunol Immunother. 2013;62:1381–92. doi: 10.1007/s00262-013-1438-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Rosenblatt J, Vasir B, Uhl L, Blotta S, Macnamara C, Somaiya P, Wu Z, Joyce R, Levine JD, Dombagoda D, Yuan YE, Francoeur K, Fitzgerald D, Richardson P, Weller E, Anderson K, Kufe D, Munshi N, Avigan D. Vaccination with dendritic cell/tumor fusion cells results in cellular and humoral antitumor immune responses in patients with multiple myeloma. Blood. 2011;117:393–402. doi: 10.1182/blood-2010-04-277137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Rosenblatt J, Avivi I, Vasir B, Uhl L, Munshi NC, Katz T, Dey BR, Somaiya P, Mills H, Campigotto F, Weller E, Joyce R, Levine JD, Tzachanis D, Richardson P, Laubach J, Raje N, Boussiotis V, Yuan YE, Bisharat L, Held V, Rowe J, Anderson K, Kufe D, Avigan D. Vaccination with dendritic cell/tumor fusions following autologous stem cell transplant induces immunologic and clinical responses in multiple myeloma patients. Clin Cancer Res. 2013;19:3640–8. doi: 10.1158/1078-0432.CCR-13-0282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Chang Q, Bournazou E, Sansone P, Berishaj M, Gao SP, Daly L, Wels J, Theilen T, Granitto S, Zhang X, Cotari J, Alpaugh ML, de Stanchina E, Manova K, Li M, Bonafe M, Ceccarelli C, Taffurelli M, Santini D, Altan-Bonnet G, Kaplan R, Norton L, Nishimoto N, Huszar D, Lyden D, Bromberg J. The IL-6/JAK/Stat3 feed-forward loop drives tumorigenesis and metastasis. Neoplasia. 2013;15:848–62. doi: 10.1593/neo.13706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Chin AR, Wang SE. Cytokines driving breast cancer stemness. Mol Cell Endocrinol. 2014;382:598–602. doi: 10.1016/j.mce.2013.03.024. [DOI] [PubMed] [Google Scholar]
- 63.Sansone P, Storci G, Tavolari S, Guarnieri T, Giovannini C, Taffurelli M, Ceccarelli C, Santini D, Paterini P, Marcu KB, Chieco P, Bonafe M. IL-6 triggers malignant features in mammospheres from human ductal breast carcinoma and normal mammary gland. J Clin Invest. 2007;117:3988–4002. doi: 10.1172/JCI32533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Yi H, Cho HJ, Cho SM, Jo K, Park JA, Kim NH, Amidon GL, Kim JS, Shin HC. Blockade of interleukin-6 receptor suppresses the proliferation of H460 lung cancer stem cells. Int J Oncol. 2012;41:310–6. doi: 10.3892/ijo.2012.1447. [DOI] [PubMed] [Google Scholar]
- 65.Lin L, Fuchs J, Li C, Olson V, Bekaii-Saab T, Lin J. STAT3 signaling pathway is necessary for cell survival and tumorsphere forming capacity in ALDH(+)/CD133(+) stem cell-like human colon cancer cells. Biochem Biophys Res Commun. 2011;416:246–51. doi: 10.1016/j.bbrc.2011.10.112. [DOI] [PubMed] [Google Scholar]
- 66.Lin L, Liu A, Peng Z, Lin HJ, Li PK, Li C, Lin J. STAT3 is necessary for proliferation and survival in colon cancer-initiating cells. Cancer Res. 2011;71:7226–37. doi: 10.1158/0008-5472.CAN-10-4660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Garner JM, Fan M, Yang CH, Du Z, Sims M, Davidoff AM, Pfeffer LM. Constitutive activation of signal transducer and activator of transcription 3 (STAT3) and nuclear factor kappaB signaling in glioblastoma cancer stem cells regulates the Notch pathway. J Biol Chem. 2013;288:26167–76. doi: 10.1074/jbc.M113.477950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Myung SJ, Yoon JH, Yu SJ. STAT3 & cytochrome P450 2C9: a novel signaling pathway in liver cancer stem cells. Biomed Pharmacother. 2012;66:612–6. doi: 10.1016/j.biopha.2012.08.011. [DOI] [PubMed] [Google Scholar]
- 69.Trikha M, Corringham R, Klein B, Rossi JF. Targeted anti-interleukin-6 monoclonal antibody therapy for cancer: a review of the rationale and clinical evidence. Clin Cancer Res. 2003;9:4653–65. [PMC free article] [PubMed] [Google Scholar]
- 70.Burger R. Impact of interleukin-6 in hematological malignancies. Transfus Med Hemother. 2013;40:336–43. doi: 10.1159/000354194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Guo DJ, Han JS, Li YS, Liu ZS, Lu SY, Ren HL. In vitro and in vivo antitumor effects of the recombinant immunotoxin IL6(T23)-PE38KDEL in multiple myeloma. Oncol Lett. 2012;4:311–8. doi: 10.3892/ol.2012.733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Younes A, Romaguera J, Fanale M, McLaughlin P, Hagemeister F, Copeland A, Neelapu S, Kwak L, Shah J, de Castro Faria S, Hart S, Wood J, Jayaraman R, Ethirajulu K, Zhu J. Phase I study of a novel oral Janus kinase 2 inhibitor, SB1518, in patients with relapsed lymphoma: evidence of clinical and biologic activity in multiple lymphoma subtypes. J Clin Oncol. 2012;30:4161–7. doi: 10.1200/JCO.2012.42.5223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Burger R, Le Gouill S, Tai YT, Shringarpure R, Tassone P, Neri P, Podar K, Catley L, Hideshima T, Chauhan D, Caulder E, Neilan CL, Vaddi K, Li J, Gramatzki M, Fridman JS, Anderson KC. Janus kinase inhibitor INCB20 has antiproliferative and apoptotic effects on human myeloma cells in vitro and in vivo. Mol Cancer Ther. 2009;8:26–35. doi: 10.1158/1535-7163.MCT-08-0149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Monaghan KA, Khong T, Burns CJ, Spencer A. The novel JAK inhibitor CYT387 suppresses multiple signalling pathways, prevents proliferation and induces apoptosis in phenotypically diverse myeloma cells. Leukemia. 2011;25:1891–9. doi: 10.1038/leu.2011.175. [DOI] [PubMed] [Google Scholar]
- 75.Scuto A, Krejci P, Popplewell L, Wu J, Wang Y, Kujawski M, Kowolik C, Xin H, Chen L, Kretzner L, Yu H, Wilcox WR, Yen Y, Forman S, Jove R. The novel JAK inhibitor AZD1480 blocks STAT3 and FGFR3 signaling, resulting in suppression of human myeloma cell growth and survival. Leukemia. 2011;25:538–50. doi: 10.1038/leu.2010.289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Malara N, Foca D, Casadonte F, Sesto MF, Macrina L, Santoro L, Scaramuzzino M, Terracciano R, Savino R. Simultaneous inhibition of the constitutively activated nuclear factor kappaB and of the interleukin-6 pathways is necessary and sufficient to completely overcome apoptosis resistance of human U266 myeloma cells. Cell Cycle. 2008;7:3235–45. doi: 10.4161/cc.7.20.6832. [DOI] [PubMed] [Google Scholar]
- 77.Park J, Ahn KS, Bae EK, Kim BS, Kim BK, Lee YY, Yoon SS. Blockage of interleukin-6 signaling with 6-amino-4-quinazoline synergistically induces the inhibitory effect of bortezomib in human U266 cells. Anticancer Drugs. 2008;19:777–82. doi: 10.1097/CAD.0b013e32830c236a. [DOI] [PubMed] [Google Scholar]
- 78.Okawa Y, Hideshima T, Steed P, Vallet S, Hall S, Huang K, Rice J, Barabasz A, Foley B, Ikeda H, Raje N, Kiziltepe T, Yasui H, Enatsu S, Anderson KC. SNX-2112, a selective Hsp90 inhibitor, potently inhibits tumor cell growth, angiogenesis, and osteoclastogenesis in multiple myeloma and other hematologic tumors by abrogating signaling via Akt and ERK. Blood. 2009;113:846–55. doi: 10.1182/blood-2008-04-151928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Baumann P, Mandl-Weber S, Oduncu F, Schmidmaier R. The novel orally bioavailable inhibitor of phosphoinositol-3-kinase and mammalian target of rapamycin, NVP-BEZ235, inhibits growth and proliferation in multiple myeloma. Exp Cell Res. 2009;315:485–97. doi: 10.1016/j.yexcr.2008.11.007. [DOI] [PubMed] [Google Scholar]
- 80.Garcia-Bates TM, Bernstein SH, Phipps RP. Peroxisome proliferator-activated receptor gamma overexpression suppresses growth and induces apoptosis in human multiple myeloma cells. Clin Cancer Res. 2008;14:6414–25. doi: 10.1158/1078-0432.CCR-08-0457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Potter M, Robertson CL. Development of plasma-cell neoplasms in BALB/c mice after intraperitoneal injection of paraffin-oil adjuvant, heat-killed staphylococcus mixtures. J Natl Cancer Inst. 1960;25:847–61. doi: 10.1093/jnci/25.4.847. [DOI] [PubMed] [Google Scholar]
- 82.Vink A, Coulie P, Warnier G, Renauld JC, Stevens M, Donckers D, Van Snick J. Mouse plasmacytoma growth in vivo: enhancement by interleukin 6 (IL-6) and inhibition by antibodies directed against IL-6 or its receptor. J Exp Med. 1990;172:997–1000. doi: 10.1084/jem.172.3.997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Lattanzio G, Libert C, Aquilina M, Cappelletti M, Ciliberto G, Musiani P, Poli V. Defective development of pristane-oil-induced plasmacytomas in interleukin-6-deficient BALB/c mice. Am J Pathol. 1997;151:689–96. [PMC free article] [PubMed] [Google Scholar]
- 84.Hilbert DM, Kopf M, Mock BA, Kohler G, Rudikoff S. Inter-leukin 6 is essential for in vivo development of B lineage neoplasms. J Exp Med. 1995;182:243–8. doi: 10.1084/jem.182.1.243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Kovalchuk AL, Kim JS, Park SS, Coleman AE, Ward JM, Morse HC, 3rd, Kishimoto T, Potter M, Janz S. IL-6 transgenic mouse model for extraosseous plasmacytoma. Proc Natl Acad Sci USA. 2002;99:1509–14. doi: 10.1073/pnas.022643999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Park SS, Shaffer AL, Kim JS, du Bois W, Potter M, Staudt LM, Janz S. Insertion of Myc into Igh accelerates peritoneal plasmacytomas in mice. Cancer Res. 2005;65:7644–52. doi: 10.1158/0008-5472.CAN-05-1222. [DOI] [PubMed] [Google Scholar]
- 87.Shacter E, Arzadon GK, Williams J. Elevation of interleukin-6 in response to a chronic inflammatory stimulus in mice: inhibition by indomethacin. Blood. 1992;80:194–202. [PubMed] [Google Scholar]
- 88.Hinson RM, Williams JA, Shacter E. Elevated interleukin 6 is induced by prostaglandin E2 in a murine model of inflammation: possible role of cyclooxygenase-2. Proc Natl Acad Sci USA. 1996;93:4885–90. doi: 10.1073/pnas.93.10.4885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Janz S. Myc translocations in B cell and plasma cell neoplasms. DNA Repair (Amst) 2006;5:1213–24. doi: 10.1016/j.dnarep.2006.05.017. [DOI] [PubMed] [Google Scholar]
- 90.Rutsch S, Neppalli VT, Shin DM, DuBois W, Morse HC, 3rd, Goldschmidt H, Janz S. IL-6 and MYC collaborate in plasma cell tumor formation in mice. Blood. 2010;115:1746–54. doi: 10.1182/blood-2009-08-237941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Duncan K, Rosean TR, Tompkins VS, Olivier A, Sompallae R, Zhan F, Tricot G, Acevedo MR, Ponto LL, Walsh SA, Tygrett LT, Berger AJ, Waldschmidt T, Morse HC, 3rd, Sunderland JJ, Janz S. (18)F-FDG-PET/CT imaging in an IL-6- and MYC-driven mouse model of human multiple myeloma affords objective evaluation of plasma cell tumor progression and therapeutic response to the proteasome inhibitor ixazomib. Blood Cancer J. 2013;3:e165. doi: 10.1038/bcj.2013.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Potter M. Neoplastic development in plasma cells. Immunol Rev. 2003;194:177–95. doi: 10.1034/j.1600-065x.2003.00061.x. [DOI] [PubMed] [Google Scholar]
- 93.Potter M, Pumphrey JG, Bailey DW. Genetics of susceptibility to plasmacytoma induction. I. BALB/cAnN (C), C57BL/6 N (B6), C57BL/Ka (BK), (C times B6)F1, (C times BK)F1, and C times B recombinant-inbred strains. J Natl Cancer Inst. 1975;54:1413–7. doi: 10.1093/jnci/54.6.1413. [DOI] [PubMed] [Google Scholar]
- 94.Zhang SL, DuBois W, Ramsay ES, Bliskovski V, Morse HC, Taddesse-Heath L, Vass WC, DePinho RA, Mock BA. Efficiency alleles of the pctr1 modifier locus for plasmacytoma susceptibility. Mol Cell Biol. 2001;21:310–8. doi: 10.1128/MCB.21.1.310-318.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Bliskovsky V, Ramsay ES, Scott J, DuBois W, Shi W, Zhang S, Qian X, Lowy DR, Mock BA. Frap, FKBP12 rapamycin-associated protein, is a candidate gene for the plasmacytoma resistance locus Pctr2 and can act as a tumor suppressor gene. Proc Natl Acad Sci U S A. 2003;100:14982–7. doi: 10.1073/pnas.2431627100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Shen-Ong GL, Keath EJ, Piccoli SP, Cole MD. Novel myc oncogene RNA from abortive immunoglobulin-gene recombination in mouse plasmacytomas. Cell. 1982;31:443–52. doi: 10.1016/0092-8674(82)90137-4. [DOI] [PubMed] [Google Scholar]
- 97.Niiro H, Clark EA. Regulation of B-cell fate by antigen-receptor signals. Nat Rev Immunol. 2002;2:945–56. doi: 10.1038/nri955. [DOI] [PubMed] [Google Scholar]
- 98.Byrd LG, McDonald AH, Gold LG, Potter M. Specific pathogen-free BALB/cAn mice are refractory to plasmacytoma induction by pristane. J Immunol. 1991;147:3632–7. [PubMed] [Google Scholar]
- 99.McIntire KR, Princler GL. Prolonged adjuvant stimulation in germ-free BALB-c mice: development of plasma cell neoplasia. Immunology. 1969;17:481–7. [PMC free article] [PubMed] [Google Scholar]
- 100.Anderson PN, Potter M. Induction of plasma cell tumours in BALB-c mice with 2,6,10,14-tetramethylpentadecane (pristane). Nature. 1969;222:994–5. doi: 10.1038/222994a0. [DOI] [PubMed] [Google Scholar]
- 101.Potter M, MacCardle RC. Histology of developing plasma cell neoplasia induced by mineral oil in BALB/c mice. J Natl Cancer Inst. 1964;33:497. [PubMed] [Google Scholar]
- 102.Takakura K, Mason WB, Hollander VP. Studies on the pathogenesis of plasma cell tumors. I. Effect of cortisol on development of plasma cell tumors. Cancer Res. 1966;26:596–9. [PubMed] [Google Scholar]
- 103.Felix K, Gerstmeier S, Kyriakopoulos A, Howard OM, Dong HF, Eckhaus M, Behne D, Bornkamm GW, Janz S. Selenium deficiency abrogates inflammation-dependent plasma cell tumors in mice. Cancer Res. 2004;64:2910–7. doi: 10.1158/0008-5472.can-03-2672. [DOI] [PubMed] [Google Scholar]
- 104.Potter M, Wax JS, Anderson AO, Nordan RP. Inhibition of plasmacytoma development in BALB/c mice by indomethacin. J Exp Med. 1985;161:996–1012. doi: 10.1084/jem.161.5.996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Vinderola G, Matar C, Perdigon G. Role of intestinal epithelial cells in immune effects mediated by gram-positive probiotic bacteria: involvement of toll-like receptors. Clin Diagn Lab Immunol. 2005;12:1075–84. doi: 10.1128/CDLI.12.9.1075-1084.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Kovalchuk AL, Kishimoto T, Janz S. Lymph nodes and Peyer’s patches of IL-6 transgenic BALB/c mice harbor T(12;15) translocated plasma cells that contain illegitimate exchanges between the immunoglobulin heavy-chain mu locus and c-myc. Leukemia. 2000;14:1127–35. doi: 10.1038/sj.leu.2401767. [DOI] [PubMed] [Google Scholar]
- 107.Kovalchuk AL, Janz S. Isotype switch-mediated CH deletions are a recurrent feature of Myc/CH translocations in peritoneal plasmacytomas in mice. Int J Cancer. 2002;101:423–6. doi: 10.1002/ijc.10638. [DOI] [PubMed] [Google Scholar]
- 108.McNeil N, Kim JS, Ried T, Janz S. Extraosseous IL-6 transgenic mouse plasmacytoma sometimes lacks Myc-activating chromosomal translocation. Genes Chromosomes Cancer. 2005;43:137–46. doi: 10.1002/gcc.20172. [DOI] [PubMed] [Google Scholar]
- 109.Park SS, Kim JS, Tessarollo L, Owens JD, Peng L, Han SS, Tae Chung S, Torrey TA, Cheung WC, Polakiewicz RD, McNeil N, Ried T, Mushinski JF, Morse HC, 3rd, Janz S. Insertion of c-Myc into Igh induces B-cell and plasma-cell neoplasms in mice. Cancer Res. 2005;65:1306–15. doi: 10.1158/0008-5472.CAN-04-0268. [DOI] [PubMed] [Google Scholar]
- 110.Kim J, Han S, Park S, McNeil N, Janz S. Plasma cell tumour progression in iMyc(Emicro) gene-insertion mice. J Pathol. 2006;209:44–55. doi: 10.1002/path.1940. [DOI] [PubMed] [Google Scholar]
- 111.Suthaus J, Stuhlmann-Laeisz C, Tompkins VS, Rosean TR, Klapper W, Tosato G, Janz S, Scheller J, Rose-John S. HHV-8-encoded viral IL-6 collaborates with mouse IL-6 in the development of multicentric castleman disease in mice. Blood. 2012;119:5173–81. doi: 10.1182/blood-2011-09-377705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Suyani E, Sucak GT, Akyurek N, Sahin S, Baysal NA, Yagci M, Haznedar R. Tumor-associated macrophages as a prognostic parameter in multiple myeloma. Ann Hematol. 2013;92:669–77. doi: 10.1007/s00277-012-1652-6. [DOI] [PubMed] [Google Scholar]
- 113.Kim J, Denu RA, Dollar BA, Escalante LE, Kuether JP, Cal-lander NS, Asimakopoulos F, Hematti P. Macrophages and mesenchymal stromal cells support survival and proliferation of multiple myeloma cells. Br J Haematol. 2012;158:336–46. doi: 10.1111/j.1365-2141.2012.09154.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Ribatti D, Moschetta M, Vacca A. Macrophages in multiple myeloma. Immunol Lett. 2013 doi: 10.1016/j.imlet.2013.12.010. doi:10.1016/j.imlet.2013.12.010. [DOI] [PubMed] [Google Scholar]
- 115.Vacca A, Ribatti D. Bone marrow angiogenesis in multiple myeloma. Leukemia. 2006;20:193–9. doi: 10.1038/sj.leu.2404067. [DOI] [PubMed] [Google Scholar]
- 116.Zheng Y, Yang J, Qian J, Qiu P, Hanabuchi S, Lu Y, Wang Z, Liu Z, Li H, He J, Lin P, Weber D, Davis RE, Kwak L, Cai Z, Yi Q. PSGL-1/selectin and ICAM-1/CD18 interactions are involved in macrophage-induced drug resistance in myeloma. Leukemia. 2013;27:702–10. doi: 10.1038/leu.2012.272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Brimnes MK, Vangsted AJ, Knudsen LM, Gimsing P, Gang AO, Johnsen HE, Svane IM. Increased level of both CD4+ FOXP3+ regulatory T cells and CD14+ HLA-DR(−)/low myeloid-derived suppressor cells and decreased level of dendritic cells in patients with multiple myeloma. Scand J Immunol. 2010;72:540–7. doi: 10.1111/j.1365-3083.2010.02463.x. [DOI] [PubMed] [Google Scholar]
- 118.Watanabe MA, Oda JM, Amarante MK, CesarVoltarelli J. Regulatory T cells and breast cancer: implications for immunopathogenesis. Cancer Metastasis Rev. 2010;29:569–79. doi: 10.1007/s10555-010-9247-y. [DOI] [PubMed] [Google Scholar]
- 119.Lindqvist CA, Loskog AS. T regulatory cells in B-cell malignancy—tumour support or kiss of death? Immunology. 2012;135:255–60. doi: 10.1111/j.1365-2567.2011.03539.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Giannopoulos K, Kaminska W, Hus I, Dmoszynska A. The frequency of T regulatory cells modulates the survival of multiple myeloma patients: detailed characterisation of immune status in multiple myeloma. Br J Cancer. 2012;106:546–52. doi: 10.1038/bjc.2011.575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Muthu Raja KR, Rihova L, Zahradova L, Klincova M, Penka M, Hajek R. Increased T regulatory cells are associated with adverse clinical features and predict progression in multiple myeloma. PLoS ONE. 2012;7:e47077. doi: 10.1371/journal.pone.0047077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Atanackovic D, Cao Y, Luetkens T, Panse J, Faltz C, Arfsten J, Bartels K, Wolschke C, Eiermann T, Zander AR, Fehse B, Bokemeyer C, Kroger N. CD4 + CD25 + FOXP3 + T regulatory cells reconstitute and accumulate in the bone marrow of patients with multiple myeloma following allogeneic stem cell transplantation. Haematologica. 2008;93:423–30. doi: 10.3324/haematol.11897. [DOI] [PubMed] [Google Scholar]
- 123.Bryant C, Suen H, Brown R, Yang S, Favaloro J, Aklilu E, Gibson J, Ho PJ, Iland H, Fromm P, Woodland N, Nassif N, Hart D, Joshua DE. Long-term survival in multiple myeloma is associated with a distinct immunological profile, which includes proliferative cytotoxic T-cell clones and a favourable Treg/Th17 balance. Blood Cancer J. 2013;3:e148. doi: 10.1038/bcj.2013.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Dhodapkar KM, Barbuto S, Matthews P, Kukreja A, Mazumder A, Vesole D, Jagannath S, Dhodapkar MV. Dendritic cells mediate the induction of polyfunctional human IL17-producing cells (Th17-1 cells) enriched in the bone marrow of patients with myeloma. Blood. 2008;112:2878–85. doi: 10.1182/blood-2008-03-143222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Prabhala RH, Pelluru D, Fulciniti M, Prabhala HK, Nanjappa P, Song W, Pai C, Amin S, Tai YT, Richardson PG, Ghobrial IM, Treon SP, Daley JF, Anderson KC, Kutok JL, Munshi NC. Elevated IL-17 produced by TH17 cells promotes myeloma cell growth and inhibits immune function in multiple myeloma. Blood. 2010;115:5385–92. doi: 10.1182/blood-2009-10-246660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Michalek J, Ocadlikova D, Matejkova E, Foltankova V, Dudova S, Slaby O, Horvath R, Pour L, Hajek R. Individual myelomaspecific T-cell clones eliminate tumour cells and correlate with clinical outcomes in patients with multiple myeloma. Br J Haematol. 2010;148:859–67. doi: 10.1111/j.1365-2141.2009.08034.x. [DOI] [PubMed] [Google Scholar]
- 127.Racanelli V, Leone P, Frassanito MA, Brunetti C, Perosa F, Ferrone S, Dammacco F. Alterations in the antigen processing-presenting machinery of transformed plasma cells are associated with reduced recognition by CD8 + T cells and characterize the progression of MGUS to multiple myeloma. Blood. 2010;115:1185–93. doi: 10.1182/blood-2009-06-228676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Muthu Raja KR, Kubiczkova L, Rihova L, Piskacek M, Vsianska P, Hezova R, Pour L, Hajek R. Functionally suppressive CD8 T regulatory cells are increased in patients with multiple myeloma: a cause for immune impairment. PLoS ONE. 2012;7:e49446. doi: 10.1371/journal.pone.0049446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Lopez-Corral L, Gutierrez NC, Vidriales MB, Mateos MV, Rasillo A, Garcia-Sanz R, Paiva B, SanMiguel JF. The progression from MGUS to smoldering myeloma and eventually to multiple myeloma involves a clonal expansion of genetically abnormal plasma cells. Clin Cancer Res. 2011;17:1692–700. doi: 10.1158/1078-0432.CCR-10-1066. [DOI] [PubMed] [Google Scholar]
- 130.Egan JB, Shi CX, Tembe W, Christoforides A, Kurdoglu A, Sinari S, Middha S, Asmann Y, Schmidt J, Braggio E, Keats JJ, Fonseca R, Bergsagel PL, Craig DW, Carpten JD, Stewart AK. Whole-genome sequencing of multiple myeloma from diagnosis to plasma cell leukemia reveals genomic initiating events, evolution, and clonal tides. Blood. 2012;120:1060–6. doi: 10.1182/blood-2012-01-405977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Keats JJ, Chesi M, Egan JB, Garbitt VM, Palmer SE, Braggio E, Van Wier S, Blackburn PR, Baker AS, Dispenzieri A, Kumar S, Rajkumar SV, Carpten JD, Barrett M, Fonseca R, Stewart AK, Bergsagel PL. Clonal competition with alternating dominance in multiple myeloma. Blood. 2012;120:1067–76. doi: 10.1182/blood-2012-01-405985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Walker BA, Wardell CP, Melchor L, Hulkki S, Potter NE, Johnson DC, Fenwick K, Kozarewa I, Gonzalez D, Lord CJ, Ashworth A, Davies FE, Morgan GJ. Intraclonal heterogeneity and distinct molecular mechanisms characterize the development of t(4;14) and t(11;14) myeloma. Blood. 2012;120:1077–86. doi: 10.1182/blood-2012-03-412981. [DOI] [PubMed] [Google Scholar]
- 133.Morgan GJ, Walker BA, Davies FE. The genetic architecture of multiple myeloma. Nat Rev Cancer. 2012;12:335–48. doi: 10.1038/nrc3257. [DOI] [PubMed] [Google Scholar]
- 134.Kishimoto T. IL-6: from its discovery to clinical applications. Int Immunol. 2010;22:347–52. doi: 10.1093/intimm/dxq030. [DOI] [PubMed] [Google Scholar]
- 135.Mihara M, Kasutani K, Okazaki M, Nakamura A, Kawai S, Sugimoto M, Matsumoto Y, Ohsugi Y. Tocilizumab inhibits signal transduction mediated by both mIL-6R and sIL-6R, but not by the receptors of other members of IL-6 cytokine family. Int Immunopharmacol. 2005;5:1731–40. doi: 10.1016/j.intimp.2005.05.010. [DOI] [PubMed] [Google Scholar]
- 136.Voorhees PM, Manges RF, Sonneveld P, Jagannath S, Somlo G, Krishnan A, Lentzsch S, Frank RC, Zweegman S, Wijermans PW, Orlowski RZ, Kranenburg B, Hall B, Casneuf T, Qin X, van de Velde H, Xie H, Thomas SK. A phase 2 multicentre study of siltuximab, an anti-interleukin-6 monoclonal antibody, in patients with relapsed or refractory multiple myeloma. Br J Haematol. 2013;161:357–66. doi: 10.1111/bjh.12266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Fulciniti M, Hideshima T, Vermot-Desroches C, Pozzi S, Nanjappa P, Shen Z, Patel N, Smith ES, Wang W, Prabhala R, Tai YT, Tassone P, Anderson KC, Munshi NC. A high-affinity fully human anti-IL-6 mAb, 1339, for the treatment of multiple myeloma. Clin Cancer Res. 2009;15:7144–52. doi: 10.1158/1078-0432.CCR-09-1483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Burger R, Neipel F, Fleckenstein B, Savino R, Ciliberto G, Kalden JR, Gramatzki M. Human herpesvirus type 8 interleukin-6 homologue is functionally active on human myeloma cells. Blood. 1998;91:1858–63. [PubMed] [Google Scholar]
- 139.Honemann D, Chatterjee M, Savino R, Bommert K, Burger R, Gramatzki M, Dorken B, Bargou RC. The IL-6 receptor antagonist SANT-7 overcomes bone marrow stromal cell-mediated drug resistance of multiple myeloma cells. Int J Cancer. 2001;93:674–80. doi: 10.1002/ijc.1388. [DOI] [PubMed] [Google Scholar]
- 140.Tassone P, Neri P, Burger R, Savino R, Shammas M, Catley L, Podar K, Chauhan D, Masciari S, Gozzini A, Tagliaferri P, Venuta S, Munshi NC, Anderson KC. Combination therapy with interleukin-6 receptor superantagonist Sant7 and dexamethasone induces antitumor effects in a novel SCID-hu In vivo model of human multiple myeloma. Clin Cancer Res. 2005;11:4251–8. doi: 10.1158/1078-0432.CCR-04-2611. [DOI] [PubMed] [Google Scholar]
- 141.Jostock T, Mullberg J, Ozbek S, Atreya R, Blinn G, Voltz N, Fischer M, Neurath MF, Rose-John S. Soluble gp130 is the natural inhibitor of soluble interleukin-6 receptor transsignaling responses. Eur J Biochem. 2001;268:160–7. doi: 10.1046/j.1432-1327.2001.01867.x. [DOI] [PubMed] [Google Scholar]
- 142.Rabe B, Chalaris A, May U, Waetzig GH, Seegert D, Williams AS, Jones SA, Rose-John S, Scheller J. Transgenic blockade of interleukin 6 transsignaling abrogates inflammation. Blood. 2008;111:1021–8. doi: 10.1182/blood-2007-07-102137. [DOI] [PubMed] [Google Scholar]
- 143.Hausherr A, Tavares R, Schaffer M, Obermeier A, Miksch C, Mitina O, Ellwart J, Hallek M, Krause G. Inhibition of IL-6-dependent growth of myeloma cells by an acidic peptide repressing the gp130-mediated activation of Src family kinases. Oncogene. 2007;26:4987–98. doi: 10.1038/sj.onc.1210306. [DOI] [PubMed] [Google Scholar]
- 144.Bisping G, Kropff M, Wenning D, Dreyer B, Bessonov S, Hilberg F, Roth GJ, Munzert G, Stefanic M, Stelljes M, Scheffold C, Muller-Tidow C, Liebisch P, Lang N, Tchinda J, Serve HL, Mesters RM, Berdel WE, Kienast J. Targeting receptor kinases by a novel indolinone derivative in multiple myeloma: abrogation of stroma-derived interleukin-6 secretion and induction of apoptosis in cytogenetically defined subgroups. Blood. 2006;107:2079–89. doi: 10.1182/blood-2004-11-4250. [DOI] [PubMed] [Google Scholar]
- 145.Golay J, Cuppini L, Leoni F, Mico C, Barbui V, Domenghini M, Lombardi L, Neri A, Barbui AM, Salvi A, Pozzi P, Porro G, Pagani P, Fossati G, Mascagni P, Introna M, Rambaldi A. The histone deacetylase inhibitor ITF2357 has anti-leukemic activity in vitro and in vivo and inhibits IL-6 and VEGF production by stromal cells. Leukemia. 2007;21:1892–900. doi: 10.1038/sj.leu.2404860. [DOI] [PubMed] [Google Scholar]
- 146.Heyer J, Kwong LN, Lowe SW, Chin L. Non-germline genetically engineered mouse models for translational cancer research. Nat Rev Cancer. 2010;10:470–80. doi: 10.1038/nrc2877. [DOI] [PMC free article] [PubMed] [Google Scholar]