Abstract
Fournier’s gangrene is a rapidly progressing necrotizing fasciitis involving the perineal, perianal, or genital regions and constitutes a true surgical emergency with a potentially high mortality rate. Although the diagnosis of Fournier’s gangrene is often made clinically, emergency ultrasonography and computed tomography lead to an early diagnosis with accurate assessment of disease extent. The Authors report their experience in ultrasound diagnosis of one case of Fournier’s gangrene of testis illustrating the main sonographic signs and imaging diagnostic protocol.
Keywords: Fournier's gangrene, Sonography
Riassunto
La gangrena di Fournier è una fascite necrotizzante a rapida progressione che coinvolge il perineo, le regioni perianale e genitali e costituisce una vera emergenza chirurgica con un tasso di mortalità potenzialmente elevato. Anche se la diagnosi di gangrena di Fournier è spesso fatta clinicamente, l'ecografia in emergenza e la tomografia computerizzata portano ad una diagnosi precoce, con una valutazione accurata dell'estensione della malattia. Gli Autori riportano la loro esperienza di diagnosi ecografica in un caso di gangrena di Fournier del testicolo, che illustra i principali segni ecografici ed i protocolli di diagnostica per immagini.
Introduction
Fournier’s gangrene is an acute, rapidly progressive, and potentially fatal, infective necrotizing fasciitis affecting the external genitalia, perineal or perianal regions, which commonly affects men, but can also occur in women and children [1]. Although originally thought to be an idiopathic process, Fournier’s gangrene has been shown to have a predilection for patients with state diabetes mellitus as well as long-term alcohol misuse. However, it can also affect patients with non-obvious immune compromise. Comorbid systemic disorders are being identified more and more in patients with Fournier’s gangrene. Diabetes mellitus is reported to be present in 20–70 % of patients with Fournier’s Gangrene [2] and chronic alcoholism in 25–50 % patients [3]. The nidus is usually located in the genitourinary tract, lower gastrointestinal tract, or skin. Anorectal or urogenital and perineal trauma, including pelvic and perineal injury or pelvic interventions are other causes of Fournier’s gangrene [4]. The testis, epididymis and spermatic cord are rarely involved, since this illness does not affect the internal spermatic artery [5–7]. Fournier’s gangrene is a mixed infection caused by both aerobic and anaerobic bacterial flora, which include Coliforms, Klebsiella, Streptococci, Staphylococci, Clostridia, Bacteroides, and Corynebacteria [8]. Infection represents an imbalance between host immunity and the virulence of the causative microorganisms. The compromised immunity provides a favorable environment to initiate the infection, and the virulence of the microorganism promotes the rapid spread of the disease. The development and progression of the gangrene are very often fulminating, and it can rapidly cause multiple organ failure and death. The clinical condition presents evolution from 2 to 7 days and is characterized by uneasiness, local swelling and discomfort, fever, crepitus and sometimes frank septic shock [9]. Because of its potential complications, it is important to diagnose the disease process as early as possible. Although the diagnosis of Fournier’s gangrene is often made clinically, emergency ultrasonography (US) and computed tomography (CT) lead to an early diagnosis with accurate assessment of disease extent. Early diagnosis in Fournier gangrene is crucial because immediate surgical debridement and antibiotics can reduce the high mortality [7].
Description of the case
A 63-year-old man obese and diabetic was admitted to the Emergency Department for the appearance of edema, scrotal erythema, and pain symptoms in the perianal region not responsive to the most common anti-inflammatory drugs. The patient reported a few days of queasiness with feeding difficulties. He was referred to our department for a genital ultrasound evaluation for suspected epididymo-orchitis since the patient had swelling in both testicles and low-grade fever. The US examination, performed with a high-frequency probe (10–15 MHz, Esaote MyLab70) showed thickening of the left scrotal tunica with layered look for the detection of hyperechoic–hyperreflective spots in relation to gas bubbles (Fig. 1) associated with a typical crackling during the compression of the probe suspected to be gangrenous necrotising fasciitis. At the color Doppler interrogation was noted hyperemia with dilated vessels, not normally visible. Both testes and epididymis and contralateral right scrotal tunics were normal and normo-vascularized. For further diagnosis a computed tomography (CT) iodinate contrast-enhanced scan was performed to assess the extent of the gangrene and to define the source of infection. It showed areas of fat-necrosis and gas in the subcutaneous tissue of the left scrotum and perineum extended to the ipsilateral inguinal canal (Fig. 2). The surgical operation was performed in emergency to avoid a rapid spread of tissue necrosis (Fig. 3) and a possible development towards septic shock. The recovery was completed with “restitutio ad integrum” and no relapses were recorded at follow-up.
Fig. 1.
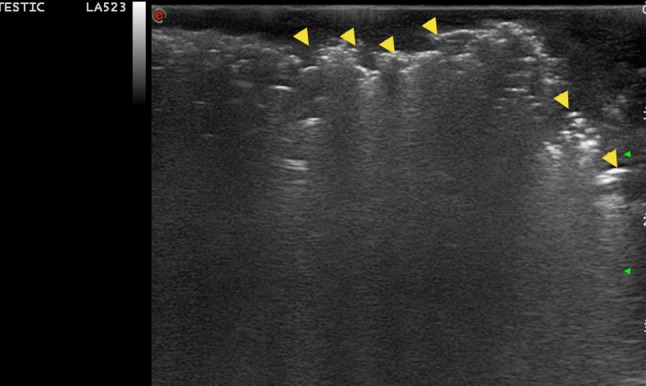
Sonographic image shows left scrotal wall thickening. Multiple echogenic foci with dirty shadowing are present, representing gas in soft tissues (yellow arrowhead)
Fig. 2.
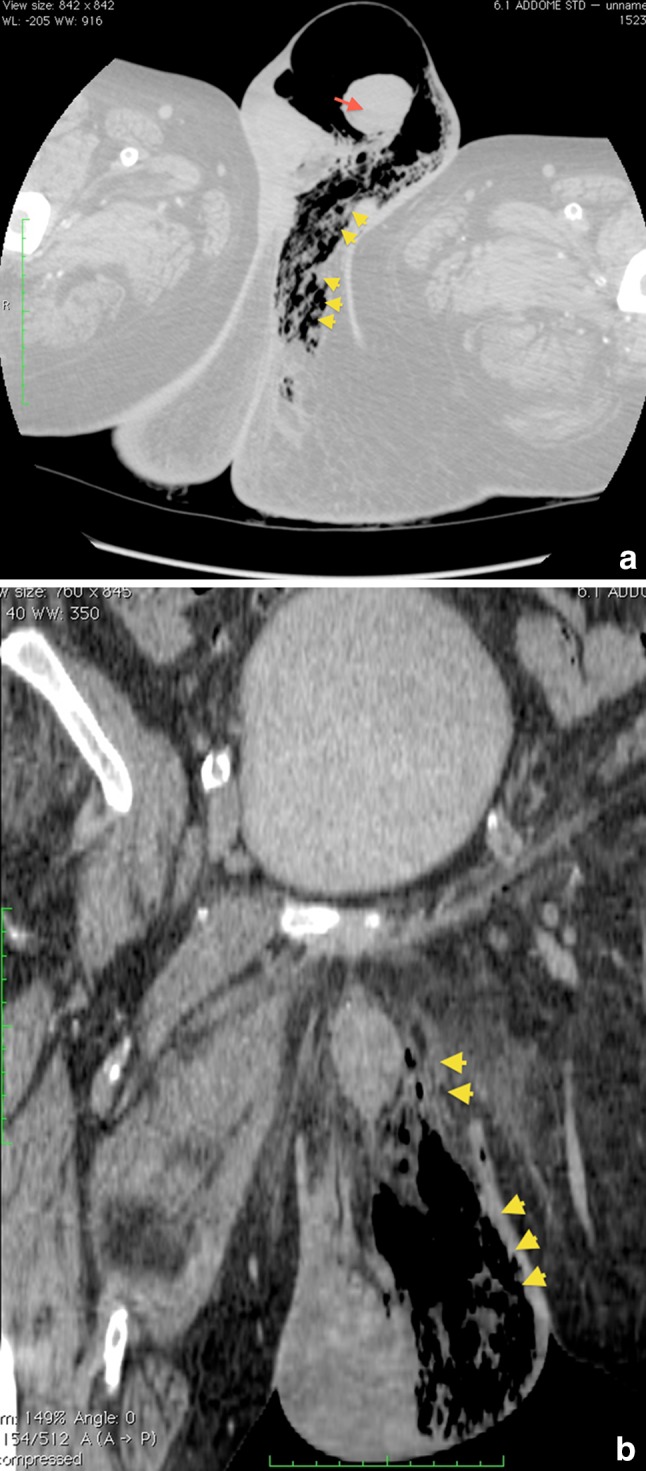
Contrast-enhanced CT a axial image magnified (WL: -205 WW: 916) and b coronal image through the scrotum confirm scrotal wall thickening and subcutaneous gas (yellow arrowhead), consistent with Fournier gangrene; Left testis (red arrow)
Fig. 3.

Perineal and scrotal region after necrosectomy
Discussion
Fournier’s gangrene shows vast heterogeneity in clinical presentation, from insidious onset and slow progression to rapid onset and fulminant course, the latter being the more common presentation [10]. The infection commonly starts as a cellulitis adjacent to the portal of entry, depending on the source of infection, commonly in the perineum or perianal region. The local signs and symptoms are usually dramatic with significant pain and swelling. The patient also has pronounced systemic signs; usually out of proportion to the local extent of the disease. Crepitus of the inflamed tissues is a common feature because of the presence of gas-forming organisms [11]. As the subcutaneous inflammation worsens, necrotic patches start appearing over the overlying skin and progress to extensive necrosis [12]. Unless aggressively treated, the patient can rapidly progress to sepsis with multiple organ failure, the common cause of death in these patients [13]. The spread of infection is along the facial planes and is usually limited by the attachment of the Colles’ fascia in the perineum. Infection can spread to involve the scrotum, penis and the anterior abdominal wall, along the Scarpa fascia [14]. The testes are usually spared as their blood supply originates intra-abdominally [5]. Even though the diagnosis of Fournier’s gangrene is primarily clinical (crepitus on palpation), imaging modalities may be useful in those cases where the presentation is atypical or when there is concern regarding the true extent of the disease [6]. US is useful to differentiate intra-scrotal abnormality and usually shows thickened and swollen scrotal wall with increased flow on color Doppler interrogation. The testis and epididymis often have a normal appearance [7]. An abscess should be suspected when fluid collections with low-level internal echoes and irregular walls are present [6, 15]. Identification of subcutaneous gas in the scrotum is the key finding. On US, gas is seen as echogenic foci demonstrating posterior acoustic “dirty” shadowing [6, 7]. Evidence of gas within the scrotal wall may be seen prior to clinical crepitus. US is also useful in differentiating Fournier’s gangrene from other illnesses which involve the inguinal–scrotal region and in distinguishing subcutaneous gas from an infection disease to bowel gas of inguinal–scrotal hernia [6, 16]. CT is useful in selected cases to diagnose the exact location and cause of the scrotal gas or rule out retroperitoneal or intra-abdominal disease process [6, 18]. CT scan shows asymmetric fascial thickening, any coexisting fluid collection or abscess, fat stranding around the involved structures, and subcutaneous emphysema secondary to gas-forming bacteria [7]. The underlying cause of the Fournier’s gangrene, such as a perianal abscess, a fistulous tract, or an intra-abdominal or retroperitoneal infectious process, may also be demonstrated better at CT [17].
Conclusion
Fournier’s Gangrene is a rapidly progressing necrotizing fasciitis involving the perineal, perianal, or genital regions and constitutes a true surgical emergency with a potentially high mortality rate. Although the diagnosis of Fournier’s gangrene is often made clinically (crepitus on palpation), emergency US and, in selected cases, CT can lead to an early diagnosis with an accurate assessment of disease extent. US of testes is an useful diagnostic aid, because it is able to differentiate between the Fournier’s gangrene from other urogenital diseases with similar cause of scrotal pain, erythema and swelling, showing the presence of intra-scrotal gas which is a pathognomonic sign of this illness.
Acknowledgments
Conflict of interest
Marco Di Serafino, Chiara Gullotto, Chiara Gregorini, Claudia Nocentini declare that they have no conflict of interest.
Informed consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, and its late amendments. Additional informed consented was obtained from all patients for which identifying information is not included in this article.
Human and animal rights
This article does not contain any studies with human or animal subjects performed by any of the authors.
References
- 1.Smith GL, Bunker CB, Dinneen MD. Fournier’s gangrene. Br J Urol. 1998;81(3):347–355. doi: 10.1046/j.1464-410x.1998.00532.x. [DOI] [PubMed] [Google Scholar]
- 2.Morpurgo E, Galandiuk S. Fournier’s gangrene. Surg. Clin. N. Am. 2002;821213–1224:1224. doi: 10.1016/s0039-6109(02)00058-0. [DOI] [PubMed] [Google Scholar]
- 3.Clayton MD, Fowler JE, Jr, Sharifi R, et al. Causes, presentation and survival of fifty–seven patients with necrotizing fasciitis of the male genitalia. Surg. Gynecol. Obstet. 1990;7049–55:55. [PubMed] [Google Scholar]
- 4.Eke N. Fourniers Gangrene: a review of 1726 cases. Br J Surg. 2000;87718–728:728. doi: 10.1046/j.1365-2168.2000.01497.x. [DOI] [PubMed] [Google Scholar]
- 5.Valentino M et al (2009) Dolore scrotale acuto: approccio alla diagnosi. Emergency care Journal. Anno VI Numero VI 37–38
- 6.Mirochnik B, et al. Ultrasound Evaluation of Scrotal Pathology. Radiol. Clin. N. Am. 2012;50:317–332. doi: 10.1016/j.rcl.2012.02.005. [DOI] [PubMed] [Google Scholar]
- 7.Aganovic L, et al. Imaging of the scrotum. Radiol. Clin. N. Am. 2012;50:1145–1165. doi: 10.1016/j.rcl.2012.08.003. [DOI] [PubMed] [Google Scholar]
- 8.Yaghan RJ, Al-Jaberi TM, Bani-Hani I. Fournier’s gangrene: changing face of the disease. Dis Colon Rectum. 2000;431300–1308:1308. doi: 10.1007/BF02237442. [DOI] [PubMed] [Google Scholar]
- 9.Shyam DC, Rapsang AG. Fournier’s gangrene. Surgeon. 2013;4:222–232. doi: 10.1016/j.surge.2013.02.001. [DOI] [PubMed] [Google Scholar]
- 10.Laor E, Palmer TS, Tolia BM, et al. Outcome prediction in patients with Fournier’s gangrene. J Urol. 1995;15489–92:92. [PubMed] [Google Scholar]
- 11.Patty R, Smith AD. Gangrene and Fournier’s gangrene. Urol Clin North Am . 1992;19:62–149. [PubMed] [Google Scholar]
- 12.Laucks SS. Fournier’s gangrene. Surg Clin North Am. 1994;741339–1352:1352. doi: 10.1016/s0039-6109(16)46485-6. [DOI] [PubMed] [Google Scholar]
- 13.Sutherland ME, Meyer AA. Necrotizing soft-tissue infections. Surg Clin North Am. 1994;74591–607:607. [PubMed] [Google Scholar]
- 14.Levenson RB, et al. Fournier gangrene: role of Imaging. RadioGraphics. 2008;28:519–528. doi: 10.1148/rg.282075048. [DOI] [PubMed] [Google Scholar]
- 15.Kane CJ, Nash P, McAninch JW. Ultrasonographic appearance of necrotizing gangrene: aid in early diagnosis. Urology. 1996;48142–144:144. doi: 10.1016/s0090-4295(96)00103-3. [DOI] [PubMed] [Google Scholar]
- 16.Rajan DK, Scharer KA. Radiology of Fournier’s gangrene. Am J Roentgenol. 1998;170(1):163–168. doi: 10.2214/ajr.170.1.9423625. [DOI] [PubMed] [Google Scholar]
- 17.Levenson RB, Singh AK, Novelline RA. Fournier gangrene: role of imaging. Radiographics. 2008;28(2):519–528. doi: 10.1148/rg.282075048. [DOI] [PubMed] [Google Scholar]
- 18.Amendola MA, Casillas J, Joseph R, et al. Fournier’s gangrene: CT findings. Abdom Imaging. 1994;19471–474:474. doi: 10.1007/BF00206944. [DOI] [PubMed] [Google Scholar]


