Abstract
Objectives
To understand how instructing females with patellofemoral pain to correct dynamic knee valgus affects pelvis, femur, tibia and trunk segment kinematics. To determine if pain reduction in the corrected condition was associated with improved segment kinematics.
Design
Cross-sectional.
Methods
A 3D-motion capture system was used to collect multi-joint kinematics on 20 females with dynamic knee valgus and patellofemoral pain during a single-leg squat in two conditions: usual movement pattern, and corrected dynamic knee valgus. During each condition pain was assessed using a visual analog scale (VAS). Pelvis, femur, tibia and trunk kinematics in the frontal and transverse planes were compared between conditions using a paired T-test. Pearson correlation coefficients were generated between VAS score and the kinematic variables in the corrected condition.
Results
In the corrected condition subjects had increased lateral flexion of the pelvis toward the weight-bearing limb (p<0.001), decreased femoral adduction (p=0.001) and internal rotation (p=0.01). A trend toward decreased tibial internal rotation (p=0.057) and increased trunk lateral flexion toward the weight-bearing limb (p=0.055) was also found. Lower pain levels were associated with less femoral internal rotation (p=0.04) and greater trunk lateral flexion toward the weight-bearing limb (p=0.055).
Conclusions
Decreased hip adduction after instruction was comprised of motion at both the pelvis and femur. Decreased pain levels were associated with lower extremity segment kinematics moving in the direction opposite to dynamic knee valgus. These results increase our understanding of correction strategies used by females with patellofemoral pain and provide insight for rehabilitation.
Keywords: dynamic knee valgus, single-leg squat, frontal plane, transverse plane
Introduction
Dynamic knee valgus, a faulty movement pattern where the knee collapses medially during weight-bearing, has been proposed to contribute to the development of patellofemoral pain (PFP)1, one of the most common orthopedic conditions encountered in sports medicine2. Characterized by increased hip adduction, hip internal rotation, knee abduction, and knee external rotation, dynamic knee valgus theoretically increases stress on the patellofemoral joint by decreasing the magnitude of contact area and shifting the location of contact to the lateral aspect of the joint1,3. As such, recent intervention strategies for PFP have begun to address control of the lower extremity in the frontal and transverse planes4,5.
In a study by Salsich and colleagues4 it was found that when females with PFP were instructed to intentionally alter their lower limb alignment to reduce or “correct” dynamic knee valgus, hip adduction and knee external rotation decreased, however, the contribution of individual body segments, such as pelvis, femur, and tibia to the hip and knee kinematics was not examined. The investigation of lower extremity segment kinematics could shed a light on the strategies involved in correcting the dynamic knee valgus movement pattern. For example, the reduction in hip adduction4 could have been due to a change in femur kinematics, pelvic kinematics or a combination of the two. In addition to lower extremity segments, the trunk also may play a role in the modification of dynamic knee valgus. Recent studies have documented that poor neuromuscular control of the trunk predicts knee injuries in females6,7. Other investigators have reported a negative correlation between hip abductor strength and trunk lateral flexion toward the ipsilateral side during jump landing8, and a trend toward decreased peak trunk lateral flexion toward the non-weight bearing limb during running9. Hence examining how the trunk responds to changes in lower extremity alignment could provide insight into the mechanism of PFP. To date only one study has investigated trunk and pelvis movement together with lower limb kinematics in females with PFP10. In this study, females with PFP presented with greater trunk lateral flexion toward the weight-bearing limb together with contralateral pelvic drop, greater hip adduction and knee abduction than controls during a single-leg squat10. What remains unknown is how the trunk responds when people attempt to correct a faulty lower extremity movement pattern.
The aim of this study was to determine the changes in pelvis, femur, tibia and trunk segment kinematics following instruction to correct a dynamic knee valgus pattern during a single-leg squat in females with PFP. A secondary purpose was to determine if pain reduction in the corrected condition was associated with improved segment kinematics.
In this study we examined pelvis, femur, tibia, and trunk segment kinematics in the subjects who participated in the previously mentioned published study4 investigating only hip and knee kinematics during the correction of dynamic knee valgus. We compared segment kinematics in the frontal and transverse planes in two movement conditions: usual movement condition and corrected dynamic valgus condition. The hypotheses were the following. First, in the corrected condition the pelvis, femur and tibia would show a movement pattern consistent with decreased dynamic knee valgus (i.e. decreased contralateral pelvic drop, femur adduction, femur internal rotation, tibia abduction, and because segment motion is calculated relative to the laboratory, decreased tibia internal rotation). Second, we expected that trunk lateral flexion toward the weight-bearing limb would be decreased in the corrected condition compared to the usual condition. Third, decreased pain level was expected to correlate with improved segment kinematics in the corrected condition.
Methods
Twenty females with chronic PFP, who were between 18 and 40 years of age, participated in the study (mean (SD) age: 22.4 (4.3) yrs, height: 167.2 (6.5) cm; body mass: 62.5 (7.6) kg; pain duration: 4.5 (4.6) yrs; average pain in last week: 4.0 (1.3) out of 10). Fourteen subjects had bilateral PFP. The study was approved by Ethics Committee: Institutional Review Board of Saint Louis University (number 15477). All subjects read and signed an informed consent form before participating and the tenets of the Declaration of Helsinki were followed. To be included in the study, subjects needed to have: 1) pain originating from the patellofemoral articulation behind or around the patella assessed by palpation to rule out pain originating from the patellar tendon, quadriceps tendon, tibiofemoral joint, meniscii, or synovial plicae; 2) PFP of at least 2 months duration11 with average pain level during the past week being equal or above 3 on a scale where 0 represented no pain, 10 represented severe pain12; 3) pain elicited with two of three provocation tests (resisted isometric quadriceps contraction at ~10° knee flexion, squatting, prolonged sitting, stair ascent or descent)12 ; 3) presence of observable dynamic knee valgus during the descent phase of a single leg squat (visual assessment of the frontal plane knee angle (abduction) greater than 10°)13 performed with their involved or most painful limb. Exclusion criteria were: 1) BMI greater than 30 kg/m2 ; 2) a history (or current report) of knee ligament, tendon or cartilage injury, traumatic patellar dislocation, patellar instability, prior knee surgery, known pregnancy, neurological involvement that would influence coordination or balance during movement testing; 3) the absence of observable dynamic knee valgus. To confirm that all inclusion and exclusion criteria were met, subjects underwent a clinical screening examination of the knee joint by the principal investigator (a physical therapist with 24 years of experience). If inclusion criteria were met, the subject returned on a different day to complete the testing procedures.
Forty-six female subjects met the age and BMI criteria and were screened in person. Twenty-four of those screened did not meet at least one of the remaining criteria and were excluded (Supplementary material). Of the 22 remaining subjects, 2 were unable to complete the tasks as instructed during the testing procedures and were excluded. Twenty subjects completed all testing procedures.
Kinematic data (120Hz) were collected using an 8-camera 3D motion capture system (Vicon Nexus, Los Angeles, CA) and a 6-degrees-of-freedom model/marker set (Visual3D, C-motion, Inc.). For all subjects, retro-reflective markers were placed on pelvis and lower limbs as previously described4,14. Trunk markers were placed on the last 10 subjects as previously described14. Subjects wore their own running shoes, and all subjects denied wearing orthotic inserts. Before data collection a calibration trial was collected for each subject. The experimenter demonstrated the task to each subject by performing a squat with the non-weight- bearing knee flexed (lower leg behind the body). Subjects performed the squat on their involved limb (or most painful limb if bilateral PFP) while keeping their arms out to their sides. Subjects were instructed to complete each squat (from start of knee flexion back to full knee extension) in 4 seconds15. Subjects were allowed several practice trials to become comfortable with the task. Subjects started each trial with both feet on the ground (squat trials were separated by 10–15 seconds). The squat was performed under 1 additional condition: avoidance (correction) of dynamic knee valgus. For the corrected condition, subjects were instructed to “keep your knee over the middle of your foot (do not let your knee fall in)” during the descent phase of the squat4. The corrected condition was demonstrated first, and subjects were allowed several practice trials to get accustomed to the movement. The term ‘corrected’ was not verbalized to subjects in order to prevent bias in pain assessment4. Three trials of each movement condition were recorded, and between conditions subjects had 5–10 min of rest. A squat cycle was defined as the period between the start of knee flexion and the return to full knee extension. Subjects completed a visual analog scale (VAS)16 after each condition to rate their average pain during that particular condition.4.
The 6-degrees-of-freedom model incorporated the trunk, pelvis, thigh, shank and foot as previously described4,14 . Data were processed in Vicon for marker labelling and in Visual3D (C-Motion, Inc.) to apply the 6-degrees-of-freedom model. Marker trajectories were lowpass filtered (6Hz, 4th order Butterworth filter) and then imported into Matlab R2010b (The MathWorks, Inc).
Peak knee flexion (PKF) was selected as time event between the start of movement (SOM) and the end of movement (EOM). The time of peak knee flexion was chosen based on pilot data which showed that the time of peak knee flexion was coincident (within 1–2 samples) with the time of peak knee extensor moment, a point of peak patellofemoral joint stress.
The SOM was defined as the first time point at the start of the descent phase at which the angular velocity of the knee joint in the sagittal plane was greater than zero, and EOM was defined as the last time point at the end of the ascent phase at which the angular velocity of the knee joint in the sagittal plane was less than zero. Visual inspection of each repetition ensured the algorithm accuracy.
In the frontal (y) and transverse (z) planes, the following joint angles relative to lab were calculated at PKF: pelvis, femur, tibia and trunk. For the femur and tibia positive values represent adduction and medial rotation. For the trunk and pelvis, positive values represent lateral flexion toward the non-weight-bearing limb (i.e. tilt to that same side) and transverse rotation toward the non-weight-bearing limb.
The time spent to perform the squat in each condition was calculated as the difference between the knee joint EOM and the SOM time points. The dependent measures included pelvis, femur, tibia, and trunk frontal and transverse plane angles and pain (VAS scores). Dependent measures were averaged across repetitions for each subject. A 2-tailed, dependent samples T-test was performed on pelvis, femur, tibia, and trunk angles in the two planes of motion (y, z) at PKF and on the squat time. Pearson correlation coefficients were generated to determine the relationships between pain (VAS score) and the kinematic variables in the corrected condition. P-level was set at 0.05. The within-session reliability of the kinematic variables was determined by calculating the intraclass coefficient (ICC(3,1)) and the standard error of measurement (SEM) on the three repetitions of the usual condition.
Results
Dependent measures showed good to excellent17 reliability in both planes motion (Table 1), and the SEM values were less than our statistically significant differences, indicating that the differences were greater than measurements error.
Table 1.
ICC(3,1) and SEM* of the kinematics variables.
| PKF | |||
|---|---|---|---|
| ICC(3,1) | SEM(°) | ||
| Pelvis | 7 | ||
| y | 0.91 | 0.83 | |
| z | 0.79 | 2.44 | |
| Femur | |||
| y | 0.73 | 1.88 | |
| z | 0.87 | 2.74 | |
| Tibia | |||
| y | 0.68 | 1.99 | |
| z | 0.92 | 2.34 | |
| Trunk | |||
| y | 0.66 | 1.73 | |
| z | 0.69 | 2.34 | |
where σ is the pooled standard deviation of trial 1–3 (usual condition).
Compared to the usual condition, in the corrected condition subjects had increased lateral flexion of the pelvis toward the weight-bearing limb (i.e. contralateral pelvic rise) (p<0.001), decreased femoral adduction (p=0.001) and internal rotation (p=0.01). Also in the corrected condition, a non-significant trend toward decreased tibial internal rotation (p =0.057) and increased trunk lateral flexion toward the weight-bearing limb was found (p=0.055), (Figure 1). There was no differences in squat time between conditions (p=0.29). Mean and SD of the dependent measures are reported in Table 2.
Figure 1.
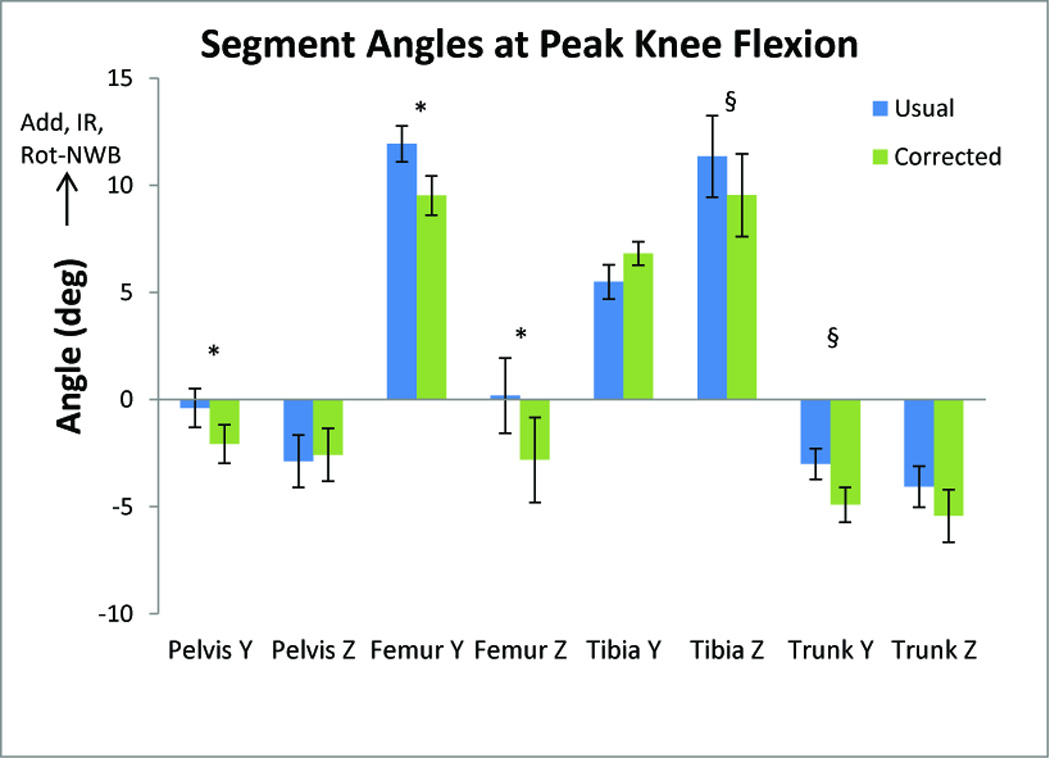
Frontal (Y) and transverse (Z) plane angles at peak knee flexion. Add = adduction, IR = internal rotation, Rot-NWB = frontal and transverse plane rotation of trunk and pelvis to the non-weight bearing limb. Error bars are 1 standard error. *p≤.05, §p<.06.
Table 2.
Kinematic variables and squat time: mean (SD). Positive values: trunk and pelvis lateral flexion, and rotation toward the non-weight-bearing limb, femur and tibia adduction and medial rotation.
| Usual | Corrected | T-test | Effect size | |
|---|---|---|---|---|
| Angles at PKF (deg) | Mean (SD) | Mean (SD) | p-value | Cohen’s d |
| Pelvis frontal | −0.39 (4.03) | −2.08 (4.00) | 0.001* | 0.34 |
| Pelvis transverse | −2.87 (5.44) | −2.58 (5.52) | 0.734 | 0.04 |
| Femur frontal | 11.93 (3.76) | 9.52 (4.08) | 0.001* | 0.51 |
| Femur transverse | 0.18 (7.85) | −2.81 (8.86) | 0.013* | 0.30 |
| Tibia frontal | 5.49 (3.59) | 6.81 (2.44) | 0.151 | 0.33 |
| Tibia transverse | 11.35 (8.51) | 9.54 (8.65) | 0.057§ | 0.17 |
| Trunk frontal | −2.99 (3.22) | −4.91 (3.66) | 0.055§ | 0.15 |
| Trunk transverse | −4.06 (4.31) | −5.43 (5.51) | 0.279 | 0.27 |
| Squat time (sec) | 3.72 (0.89) | 3.97 (0.93) | 0.292 | 0.22 |
p<0.05
p<0.06.
Lower pain levels were associated with decreased femoral internal rotation (r=0.46, p=0.04) and greater trunk lateral flexion toward the weight-bearing limb, although not statistically significant (r=0.61, p=0.055).
Discussion
The aim of this study was to understand the contribution of segment kinematics to the modification of the dynamic knee valgus movement pattern present in females with PFP. We also aimed to examine if and how instructing individuals with PFP to change their lower limb usual movement pattern influences trunk kinematics and pain level.
The results show that pelvis and femur kinematics moved in a direction opposite to dynamic knee valgus in the corrected condition: contralateral pelvis rise increased, and femur adduction and internal rotation decreased (Figure 1). These findings suggest that the reduced hip adduction previously reported4 is comprised of motion at both the pelvis and femur segments. Interestingly, our pelvis kinematics differ slightly from those reported by Nakagawa and collegues10. In the usual condition, our subjects were in slight contralateral pelvic rise, whereas in the study from Nakagawa and colleagues10 subjects demonstrated ~11° of pelvic drop. The difference might be explained by slightly different methodology and instruction. (Nakagawa and colleagues10 used electromagnetic sensors and instructed subjects to cross their arms over their chests).
Nevertheless, in the current study compared to the usual condition, in the corrected condition subjects had increased lateral flexion of the pelvis toward the weight-bearing limb (i.e. contralateral pelvic rise). This suggests that our subject were able to move away from contralateral pelvic drop in the corrected condition. The decreased tibia internal rotation suggests that the increased knee internal rotation found in the corrected condition compared to usual in the previously reported results4 may have been the result of greater relative movement of the femur segment than the tibia segment. Interestingly, the decreased femur and tibia internal rotation observed may be a secondary consequence of the movement pattern correction, as the instruction was directed toward the frontal plane position of the knee. Similar results have been reported by Olson and colleagues5. After a 4-week intervention program that emphasized proper knee positioning during movement (i.e. avoiding dynamic knee valgus), females with PFP had decreased femoral rotation during a single limb step-down. Similar to our methods, no specific instruction was given to alter transverse plane alignment5. Knowledge of the motion of the individual body segments in space, in addition to their movement relative to each other, is necessary to better understand the mechanisms used to correct dynamic knee valgus.
The results of this investigation further showed that instructing females with PFP to alter their usual lower limb movement pattern may also modify trunk kinematics. Compared to the usual condition, in the corrected condition subjects show a trend toward greater lateral flexion of the trunk toward the weight-bearing limb, although this result did not reach statistical significance. The lack of significant difference was probably due to the small sample size combined with a relatively small effect size (Table 2). The tendency to increase lateral flexion of the trunk toward the weight-bearing limb was surprising, as we expected that the trunk would respond similarly to the lower extremity segments and adopt a posture opposite to dynamic knee valgus in the corrected condition. One possible explanation is that subjects were attempting to compensate for weakness in the hip abductor muscles, a common finding in people with PFP18,19. By leaning the trunk toward the supporting limb, the trunk center of mass is closer to the hip joint center which would decrease the demand on the hip abductors. In support of this argument, Nagakawa and colleagues10 reported an association between decreased gluteus medius activity and increased trunk lateral flexion toward the weight-bearing limb during single-leg squat in females with PFP. Although the increased trunk lateral flexion toward the weight-bearing limb in the corrected condition might have decreased the demands on the hip abductors, it might have increased the lateral forces acting at the patella. Specifically trunk lateral flexion toward the weight-bearing limb may have shifted the ground reaction force vector lateral to the knee joint center creating a valgus moment at the knee20. As such, this trunk strategy may not be optimal in the long term. Although there was no difference in pain level between the usual and corrected conditions4, in the corrected condition, decreased pain was associated with decreased femoral internal rotation. As such, the secondary consequence of the frontal plane instruction (e.g. transverse plane motion of the femur) appears to be important in females with PFP. Decreased pain also was associated with increased trunk lateral flexion toward the weight-bearing limb. Given that the instructions were directed at the lower extremity, it is possible that the trunk lateral flexion was necessary to stabilize the hip to achieve the desired lower extremity movement pattern. This information may shed some light on treatment interventions for females with PFP who demonstrate dynamic knee valgus. For example, strategies may initially involve instructing patients to lean their trunk over their supporting limb to align the femur and tibia. Once limb alignment is maintained, progression to upright trunk posture might be a goal.
This study presents some limitations. We found statistically significant differences across conditions that were above the SEM, but the changes were rather small. As a result, the clinical importance of the differences is not known. Second, only a subset of subjects had trunk kinematics assessed. It is possible that with a larger sample more trunk kinematic differences would have been detected. Third, we did not measure muscle activation, and as such, cannot determine the muscle strategies used by subjects to achieve the kinematic changes we observed. Future studies should include electromyography to address this question.
Conclusion
When females with PFP were asked to correct dynamic knee valgus, they decreased femur adduction, and femur internal rotation. They also increased lateral flexion of the pelvis toward the weight-bearing limb. The correction of dynamic knee valgus may require compensatory frontal plane movement of the pelvis, perhaps to reduce the demand on the weight-bearing hip. The association between decreased pain and decreased femur internal rotation and increased trunk lateral flexion toward the weight-bearing limb may provide insight into the kinematic components that influence pain during a weight-bearing task, and provide insight for possible treatment interventions for females with PFP.
Supplementary Material
Pratical implications.
Decreased hip adduction during the modification of dynamic knee valgus was comprised of both increased lateral flexion of the pelvis toward the weight-bearing limb (i.e. contralateral pelvis rise) and decreased femur adduction.
Improvement of lower limb alignment was accompanied by lateral bending of pelvis toward the weight-bearing limb, possibly to compensate for hip muscle weakness.
Lower pain levels were associated with decreased internal rotation of the femur and increased lateral bending of the trunk toward the weight-bearing limb, providing insight for possible treatment strategies for females with patellofemoral pain.
Acknowledgements
The project described was supported by Award Number R15HD059080 from the Eunice Kennedy Shriver National Institute Of Child Health & Human Development. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Eunice Kennedy Shriver National Institute Of Child Health & Human Development or the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Powers C. The influence of altered lower-extremity kinematics on patellofemoral joint dysfunction: A theoretical perspective. J. Orthop. Sports Phys. Ther. 2003;33(11):639–646. doi: 10.2519/jospt.2003.33.11.639. [DOI] [PubMed] [Google Scholar]
- 2.Baquie P, Brukner P. Injuries presenting to an australian sports medicine centre: A 12-month study. Clin J Sport Med. 1997;7(1):28–31. doi: 10.1097/00042752-199701000-00006. [DOI] [PubMed] [Google Scholar]
- 3.Powers C. The influence of abnormal hip mechanics on knee injury: A biomechanical perspective. J. Orthop. Sports Phys. Ther. 2010;40(2):42–51. doi: 10.2519/jospt.2010.3337. [DOI] [PubMed] [Google Scholar]
- 4.Salsich GB, Graci V, Maxam DE. The effects of movement pattern modification on lower extremity kinematics and pain in women with patellofemoral pain. J Orthop Sports Phys Ther. 2012;42(12):1017–1024. doi: 10.2519/jospt.2012.4231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Olson TJ, Chebny C, Willson JD, Kernozek TW, Straker JS. Comparison of 2D and 3D kinematic changes during a single leg step down following neuromuscular training. Phys. Ther. Sport. 2011;12(2):93–99. doi: 10.1016/j.ptsp.2010.10.002. [DOI] [PubMed] [Google Scholar]
- 6.Zazulak BT, Hewett TE, Reeves NP, Goldberg B, Cholewicki J. Deficits in neuromuscular control of the trunk predict knee injury risk. Am. J. Sports Med. 2007;35(7):1123–1130. doi: 10.1177/0363546507301585. [DOI] [PubMed] [Google Scholar]
- 7.Zazulak B, Cholewicki J, Reeves NP. Neuromuscular control of trunk stability: Clinical implications for sports injury prevention. J Am Acad. Orthop. Surg. 2008;16(9):497–505. [PubMed] [Google Scholar]
- 8.Boling M, Padua D. Relationship between hip strength and trunk, hip, and knee kinematics during a jump-landing task in individuals with patellofemoral pain. Int J Sports Phys Ther. 2013;8(5):661–669. [PMC free article] [PubMed] [Google Scholar]
- 9.Noehren B, Pohl MB, Sanchez Z, Cunningham T, Lattermann C. Proximal and distal kinematics in female runners with patellofemoral pain. Clin Biomech (Bristol, Avon) 2012;27(4):366–371. doi: 10.1016/j.clinbiomech.2011.10.005. doi: 10.1016/j.clinbiomech.2011.10.005; 10.1016/j.clinbiomech.2011.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nakagawa TH, Moriya ET, Maciel CD, Serrao FV. Trunk, pelvis, hip, and knee kinematics, hip strength, and gluteal muscle activation during a single-leg squat in males and females with and without patellofemoral pain syndrome. J Orthop Sports Phys Ther. 2012;42(6):491–501. doi: 10.2519/jospt.2012.3987. [DOI] [PubMed] [Google Scholar]
- 11.Kannus P, Natri A, Paakkata T, Jarvinen M. An outcome study of chronic patellofemoral pain syndrome. seven-year follow-up of patients in a randomized, controlled trial. J Bone Joint Surg Am. 1999;81:355–363. doi: 10.2106/00004623-199903000-00007. [DOI] [PubMed] [Google Scholar]
- 12.McConnell J. The management of chondromalacia patellae: A long term solution. Aust. J. Physiother. 1986;32(4):215. doi: 10.1016/S0004-9514(14)60654-1. [DOI] [PubMed] [Google Scholar]
- 13.Harris-Hayes M, Steger-May K, Koh C, Royer N, Graci V, Salsich G. Classification of lower extremity movement patterns based on visual assessment: Reliability and correlation to two dimensional video analysis. J Athl Train. doi: 10.4085/1062-6050-49.2.21. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Graci V, Van Dillen LR, Salsich GB. Gender differences in trunk, pelvis and lower limb kinematics during a single leg squat. Gait Posture. 2012;36(3):461–466. doi: 10.1016/j.gaitpost.2012.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Willson JD, Davis IS. Lower extremity mechanics of females with and without patellofemoral pain across activities with progressively greater task demands. Clin Biomech. 2008;23(2):203–211. doi: 10.1016/j.clinbiomech.2007.08.025. [DOI] [PubMed] [Google Scholar]
- 16.Carlsson A. Assessment of chronic pain. I. aspects of the reliability and validity of the visual analogue scale. Pain. 1983;16:87–101. doi: 10.1016/0304-3959(83)90088-X. [DOI] [PubMed] [Google Scholar]
- 17.Shrout PE, Fleiss JL. Intraclass correlations: Uses in assessing rater reliability. Psychol. Bull. 1979;86(2):420–428. doi: 10.1037//0033-2909.86.2.420. [DOI] [PubMed] [Google Scholar]
- 18.Dierks TA, Manal KT, Hamill J, Davis IS. Proximal and distal influences on hip and knee kinematics in runners with patellofemoral pain during a prolonged run. J Orthop Sports Phys Ther. 2008;38(8):448. doi: 10.2519/jospt.2008.2490. [DOI] [PubMed] [Google Scholar]
- 19.Souza RB, Powers CM. Differences in hip kinematics, muscle strength, and muscle activation between subjects with and without patellofemoral pain. J Orthop Sports Phys Ther. 2009;39(1):13. doi: 10.2519/jospt.2009.2885. [DOI] [PubMed] [Google Scholar]
- 20.Hewett T, Torg J, Boden B. Video analysis of trunk and knee motion during non-contact anterior cruciate ligament injury in female athletes: Lateral trunk and knee abduction motion are combined components of the injury mechanism. Br J Sports Med. 2009;43(6):417. doi: 10.1136/bjsm.2009.059162. doi: 10.1136/bjsm.2009.059162. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


