Abstract
Reactive oxygen species (ROS) play crucial roles in all aspects of melanoma development, however, the source of ROS is not well defined. In this review we summarize recent advancement in this rapidly developing field. The cellular ROS pool in melanocytes can be derived from mitochondria, melanosomes, NADPH oxidase (NOX) family enzymes, and uncoupling of nitric oxide synthase (NOS). Current evidence suggests that Nox1, Nox4 and Nox5 are expressed in melanocytic lineage. While there is no difference in Nox1 expression levels in primary and metastatic melanoma tissues, Nox4 expression is significantly higher in a subset of metastatic melanoma tumors as compared to the primary tumors; suggesting distinct and specific signals and effects for NOX family enzymes in melanoma. Targeting these NOX enzymes using specific NOX inhibitors may be effective for a subset of certain tumors. ROS also play important roles in BRAF inhibitor induced drug resistance; hence identification and blockade of the source of this ROS may be an effective way to enhance efficacy and overcome resistance. Furthermore, ROS from different sources may interact with each other and interact with reactive nitrogen species (RNS) and drive the melanomagenesis process at all stages of disease. Further understanding ROS and RNS in melanoma etiology and progression is necessary for developing new prevention and therapeutic approaches.
Melanoma is a reactive oxygen species (ROS)-driven tumor based on a copious amount of work done by us and others [1–3]. Searching the Pubmed database with “reactive oxygen” and “melanoma” returned 52 publications in 2009 and 103 in 2013; within 4 years the number of publication almost doubled. With the rapid development in the field, we attempt to summarize the tremendous progress in our understanding of the role of ROS in melanoma etiology and progression.
1. Source of ROS
The term ROS includes chemically reactive molecules such as superoxide anions, peroxides and hydroxyl radicals, which can modify protein and DNA molecules, and permanently or temporally change their cellular behavior. When cells generate excessive ROS, it causes oxidative stress, which has long been recognized as an adverse event for promoting tumorigenesis and progression [4, 5]; however, mounting evidence has emerged in recent years indicating that adequate ROS, in particular superoxide and hydrogen peroxide, also serve as signal molecules for cell proliferation, vascular function and wound healing [6–9]. In contrast, extremely low levels of ROS may enable cells to undergo cell cycle arrest [10, 11]. However, there has never been a standard measure as to how much ROS is adequate and how much is excessive or insufficient. This deficiency is partially due to the complexity of ROS measurement methods, and partially due to the dynamics of ROS generation and various ROS species in cells.
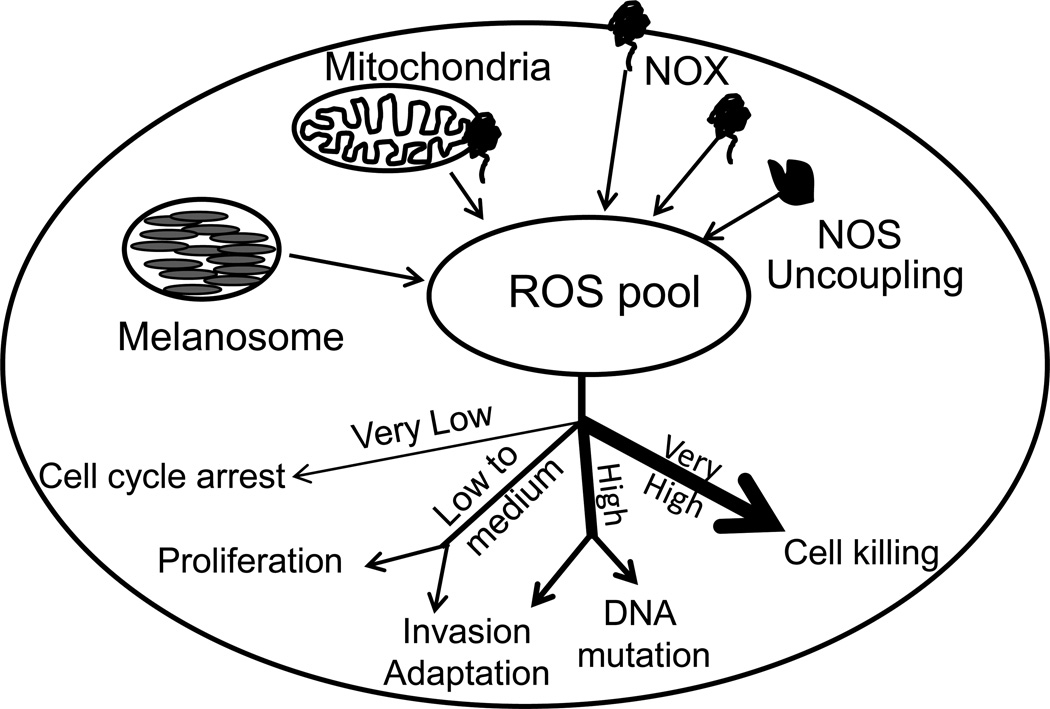
Cancer cells including melanoma cells exhibit high levels of ROS [12, 13]. The source of ROS has not been completely defined. The major source of ROS in cancer cells has traditionally been attributed to mitochondrial uncoupling and dysfunction [14]. However, emerging evidence from specific investigations of melanoma cells indicates that other cellular compartments and enzymes also contribute significantly to ROS generation, including the NADPH Oxidase (NOX) family, nitric oxide synthase (NOS) uncoupling, peroxisomes and melanosomes (Figure 1). In melanoma, the mitochondria may also generate ROS via the electron transport chain, mainly complex I and Complex III, as well as other sites [15]. How and how much each complex site generates superoxide and how much they contribute to total mitochondrial ROS is not clear. Although melanoma is a ROS-driven tumor [1], mitochondria-generated ROS currently remains as a vague and undeveloped paradigm in melanoma research; most of the studies are indirect or the signal pathways were deduced from other cancer fields. As pointed out in a recent review, mitochondrial DNA mutation is rare in cancer [16], hence, mitochondrial DNA mutation is unlikely a major cause for ROS generation and cancer development in melanoma cells. However it is now recognized that the role of mitochondria in cancer is more linked to defective metabolic regulation [17], consequently it is conceivable that mitochondria-generated ROS may also directly participate in these processes.
Figure 1. The source of ROS in melanocytes and their cellular effect.
ROS can be generated from melanosomes, mitochondria, NOX family enzymes and/or NOS uncoupling. ROS generated from these different sources may interact with each other and form a cellular ROS pool. When ROS levels are adequate, they serve as proliferation signals; when ROS is raised, they show adverse effect including promoting invasion and DNA oxidative mutations. If ROS level is beyond the cellular antioxidant buffering capacity, they can directly kill cells.
Early studies indicated that melanocytes and melanoma cells exhibited a unique redox regulation [12, 18, 19]; hence efforts on seeking a unique ROS source led to discovery of the ROS-generating roles of the melanosome and melanin [20] (Figure 1). An understanding of the melanosome and melanin-related ROS hypothesis explains how and why melanin is required for melanomagenesis [21]. The red-hair associated pheomelanin has long been assumed to have a pro-oxidant role. Recently, pheomelanin structure has been elucidated and pheomelanin was purified [22, 23]. The purified pheomelanin exhibited potent pro-oxidant characteristics in the test tube and in cells when exposed to UV radiation [24, 25]. Further investigations should lead to novel mechanistic insights about UV-induced melanomagenesis.
On the other hand, recent studies reveal that NOX family genes also play an essential role in the development of non-melanoma skin cancer and melanoma, which will be discussed in detail below [26, 27]. The NOX family of enzymes includes 7 members: Nox1, Nox2 (gp91phox), Nox3, Nox4, Nox5, Duox1 and Duox2; all use NAD(P)H and oxygen as substrates and generate superoxide (except for Nox4, Duox1 and Duox2 which generates hydrogen peroxide). NOX family enzymes have not been well studied in melanoma. Early studies suggested that NADPH oxidases contributed to melanoma cell proliferation [28, 29]; although no specific isoforms were identified. Subsequently, Nox4 was discovered to play a critical role in melanoma invasion downstream of the AKT pathway [30]; Nox4 is also a target for MiTF in the B16 melanoma cell line [31]. Our data showed that among the 7 family members, only Nox1 was expressed in normal melanocytes and in all 9 melanoma cell lines examined. Nox4 was expressed in only a subset of metastatic melanoma cell lines [32], consistent with the published results showing that Nox4 is involved in cell invasion [30]. Nox5 was recently found in a melanoma cell line [33], while expression of other NOX family members has not yet been detected in cells of melanocytic cell lineage [32]. Thus, the NOX family of enzymes has emerged as a new and important source of ROS in melanoma.
2. The role of NOX family genes in melanoma etiology
NADPH oxidases are multi-subunit enzymes. Nox1, Nox2, Nox3 and Nox4 share a common membrane subunit CYBA (p22phox, Cytochrome b-245, neutrophil cytochrome b light chain) as part of their holoenzyme, but each prefers different cytoplasmic subunits [34]. Nox1 usually prefers NoxO1 and NoxA1 while Nox2 utilizes a 47-KD NCF1 (phox47) and a 67-KD NCF2 (neutrophil cytosolic factor 2, p67phox) [35, 36]. Emerging evidence indicates that Nox1, Nox4, Nox5 and NCF1 may impact melanomagenesis and progression.
As a major melanoma risk factor, skin color is regulated by a series of signaling molecules (e.g., POMC gene products, agouti protein, melanocortin receptors), transcription factors (e.g. MiTF, Sox9/Sox10) and melanin-synthesis enzymes (e.g., tyrosinase, tyrosinase-related protein 1, and tyrosinase-related protein 2) [37], among which melanocortin receptor 1 (Mc1R) transduces signals from either its agonist α-MSH or antagonist agouti to determine melanin sub-types [38, 39]. Consequently, mutations in Mc1R and agouti protein were tightly linked to melanoma risk [38, 40–42]. Although emerging evidence indicates that Mc1R can function via a UV-independent melanomagenesis signal pathway [43], it is obvious that Mc1Rmediated skin pigmentation may play a critical role in UV-induced DNA damage response. Abdel-Malek’s group showed that α-MSH treatment protected cultured human melanocytes from UV-induced oxidative stress as measured by 7,8-dihydro-8-oxyguanine (8-oxodG) levels, which was mediated by functional Mc1R as the protective effect was not observed in melanocytes carrying loss of function Mc1R alleles [44, 45]. A study of immortalized human keratinocytes HACAT cells revealed that expression of wild-type Mc1R, but not the red-hair associated loss of function Mc1R (Mc1R-R151C) gene reduced UVA-induced ROS production [46]. This study further elucidated that UVA-induced the phosphorylation of NoxA1 [46], a subunit for the Nox1 holoenzyme. Phosphorylation of NoxA1 decreases its binding to Nox1 catalytic subunit and Rac1, a key activator for Nox1 [47], hence this phosphorylation decreases Nox1 activity [48]. Thus, Nox1 seems to be responsible for ROS generation downstream of Mc1R. Interestingly, Nox2 (gp91phox) null mice showed a compromised epidermal melanocytes induction after UVB radiation in the eyes, which corresponded to compromised plasma α-MSH induction [49]. These studies suggest that NOX family genes not only regulate UV-induced melanocytes proliferation, but also play a critical role in UV-induced ROS production. Our unpublished data suggests that Nox1 protein is induced by both UVA and UVB in the melanoma cell line SK-Mel28; and more so by UVA (Liu-Smith and Meyskens, unpublished data); consequently, NOX activity assay revealed that UVA also induced higher total NOX activity as compared to UVB (Liu-Smith and Meyskens, unpublished data). These results may suggest that SK-Mel28 cells carry a non-functional MC1R allele. At the same time, this may also suggest that in normal melanocytes from individuals carrying non-functional Mc1R variants the NOX family may play an important role in UV-induced ROS production, a direct cause for UVA-induced oxidative DNA damage.
Gene knockout in mice did not reveal any tumorigenesis phenotype for NOX family genes, including Nox1, Nox2, Nox4 and CYBA/p22phox [50]. However, knockout NCF1 (neutrophil cytosolic factor 1, p47phox), a subunit for Nox2 holoenzyme, reduced xenografted tumor growth [51], suggesting that Nox2 may create a favorable environment for in vivo tumor growth. Interestingly, Nox4 knockdown in melanoma cell lines induced G2/M cell cycle arrest [52], suggesting that Nox4 is required for cell proliferation in a subset of aggressive melanomas.
3. The Role of NOX-induced ROS in melanoma progression
Advanced metastatic melanoma is difficult to treat even with the recent therapeutic breakthrough using BRAF and MEK inhibitors and immunotherapy [53–55]; hence understanding the nature of resistant metastatic cells still remains an important research focus. ROS is known to be an important component in driving cancer cell migration and invasion [5]; however, the source of this type of ROS has been rarely described. To date, few reports have investigated mitochondria-derived ROS as a driver of cancer metastasis [56, 57]. Recent research on NOX enzymes has established a new playing field for pathway-driven hypotheses focused on the role of NOX-induced ROS in cancer metastasis.
Cancer cell metastasis requires a series of regulated movements of the cytoskeleton and cell adhesive molecules. The Rho GTPase family proteins, including Rac1, RhoA and Cdc42, are essential regulators for the cytoskeleton movements and adhesion molecules, hence play pivotal roles in cancer metastasis [58–60]. Rac1 is a crucial activator for NOX enzymes [61], especially for Nox1 [62, 63]. Activated Rac1 binds NoxA1 and the C-terminal domain of NOX1 for assembly of the holoenzyme [47, 64, 65]; ectopic expression of Rac1(Q61L), a constitutively activated Rac1 mutant, enhances the cytosolic activator p67phox (NoxA1 homologue which can also bind to Nox1 and stimulate the enzymatic activity) binding to Nox1 and promotes its localization to plasma membrane, subsequently promoting Nox1 activity and induces ROS [62]. Our finding that Nox1 over-expression promoted melanoma cell invasion provides a new and complementary explanation to Rac1-Nox1 mediated cell motility [32]. Over-expression of Nox1 alone increased ROS levels in melanoma cells, induced MMP2 and MMP9 expression as well as an epithelial-mesenchymal transition (EMT), resulting in an increased invasive phenotype [32]. These results are consistent with the finding that hyaluronic acid induced Rac1 activity, resulting in increased NOX activity and ROS production, leading to increased melanoma motility [66]. Mouse B16F0 non-invasive melanoma cells, when treated with exogenous hydrogen peroxide, also became invasive due to increased Rac1 and p47phox expression [67], further affirming a role for NOX enzymes in ROS-mediated melanoma invasion.
Nox1 protein levels were reported to be associated with colon cancer progression in one report [68], but not in another [69], raising the question whether it can serve as a progression biomarker. Using the microarray data from the Gene Expression Omnibus (GEO) from National Center of Biotechnology Information initially done by Xu et al., [70], we analyzed the expression levels of Nox1 and Nox4 from 31 primary and 52 metastatic human melanoma samples. The Nox1 mRNA levels were not associated with melanoma stages (Liu-Smith and Meyskens, unpublished data). Nox1 mRNA levels are similar in metastatic melanoma samples and early stage non-invasive primary tumors (p =0.57, unpaired t-test). Our published results also showed similar Nox1 protein levels in primary melanoma and metastatic cell lines [32]. Therefore, Nox1 may not be a driving force for melanoma invasion in vivo, although it can enhance the invasion capacity in vitro. On the contrary, Nox4 seems to be a driving force for melanoma invasion in a subset of tumors. Using the same GEO dataset, we found that Nox4 expression levels were much higher in some metastatic samples as compared to the primary tumors (p=0.025, Liu-Smith and Meyskens, unpublished data). This differential expression of Nox1 and Nox4 in melanomas of different stages is further supported by publications from us and others [30, 32, 52]. Since Nox4 is required for cell cycle progression in these examples [52], Nox4 may serve as an effective therapeutic target for this subset of melanoma. On the contrary, Nox1 may not be a good biomarker for melanoma progression. Nevertheless, this does not exclude the importance of superoxide and/or hydrogene peroxide in melanoma progression because superoxide/hydrogen peroxide is the ultimate effector, not the NOX enzymes. From this point of view, activation of Rac1 may be considered as a biomarker for melanoma progression, consistent with its newly defined role as a melanoma oncogene [71]. While superoxide and hydrogen peroxide is difficult to detect after fixing procedures in biospecimens, a potential biomarker for superoxide may be Notch related ankyrin related protein (Nrarp) which was found to be down-regulated together with Nox4 in Ang2-heterozygous mice endothelial cells as compared to Ang2 null cells [72]. In this study inhibiting Nox4 by fulvene-5 blocked growth of endothelial tumors in mice [72].
Furthermore, Nox1 was shown to be a downstream effector of 12-Lipoxygenase (12-LOX) signaling in colon cancer proliferation [73]. In this study, knockdown of Nox1 in colon cancer cells prevented 12-LOX mediated proliferation [73]. 12-LOX has also been reported as a biomarker for melanoma progression [74]. In this report, 12-LOX expression was not observed in human melanocytes or nevi, but 12-LOX expression was detected in dysplastic nevi and melanoma. Importantly, 12-LOX expression directly correlated with melanoma progression with melanoma displaying the highest 12-LOX expression [74]. Recent work from our lab demonstrated the opposite expression pattern for the UDP-glucuronosyltransferases (UGTs) in melanoma progression [75]. UGTs are expressed in melanocytes, but not expressed in metastatic melanoma cell lines [75]. This is intriguing since the UGTs can turn off 12-LOX signaling by metabolizing 12-HETE, the main signaling molecule generated by 12-LOX catabolism of arachidonic acid [76]. 12-HETE levels have been shown to correlate with melanoma metastatic potential in mouse models [77]. High concentrations of 12-HETE are found in highly metastatic cell lines compared to cell lines with low metastatic potential [77]. Thus, Nox1 may very well be the critical downstream effector in 12-LOX signaling in melanoma as well.
It is evident that Nox4 and Nox1 may function via different upstream signals in invasion, as Nox1 is tightly regulated by Rac1 while Nox4 has no apparent link with Rac1, rather Nox4 is downstream of the AKT pathway. Further, Nox1 participates in EMT process while Nox4 may not. The difference is also reflected by the end product of enzymatic reaction: Nox1 produces superoxide which is not membrane permeable, and which needs to be further detoxified by superoxide dismutases; Nox4 produces hydrogen peroxide which can serve as either a signaling molecule or lead to cellular damaging ROS.
4. The potential role of ROS in melanoma drug resistance
In experimental therapeutic studies, a number of drugs were reported to induce ROS, which serve as mediators for apoptosis or cell killing. For example, TRAIL (TNF-related apoptosis-inducing ligand)-induced apoptosis can be sensitized by wortmanin through a ROS-dependent phosphorylation of Bax [78]; The source of wortmanin-induced ROS seems to be Nox4 as its siRNA suppressed Bax phosphorylation and apoptosis [78]. Nox4-generated ROS also played a crucial role in proopiomelanocortin-induced apoptosis [79]. A role of Nox1 in drug response has not yet been explored.
In the clinic a significant breakthrough in melanoma treatment has been the clinical activity of BRAF inhibitor Vemurafenib (Plx4032), which has shown unprecedented efficacy (40–80% response rate) against melanoma as compared to conventional Dacarbazine treatment (~5% response rate) [80, 81]. Patients receiving Plx4032 treatment showed a progression-free survival of 5.3 months as compared to 1.6 months for those treated with Dacarbazine [53]. However, after the initial response the tumors uniformly progressed and patients quickly relapsed [54]. A combination therapy of a BRAF inhibitor and Mek1/2 inhibitor produced longer response periods, but unfortunately resistance still developed [55]. The observed Plx4032-induced resistance involved signals from NRAS, CRAF, COT, PDGFRβ, EGFR and IGF-1R [82, 83], as well as reactivation of Erk1/2 [84]. In fact, Erk1/2 seems to be at the center of this whole signal cascade because all of the listed upstream signals can be transmitted to re-activate Erk1/2. Interestingly, there have been many studies demonstrating an intrinsic link between ROS and Erk1/2 activation [85]. Hence, it is conceivable that ROS may be a key downstream effector for Plx4032-mediated Erk1/2 reactivation. This hypothesis is supported by recent observation that Plx4032 treatment induced ROS in melanoma cells ([86, 87], Liu-Smith and Meyskens, unpublished data). The ROS induction was through PGC1α-induced mitochondria biogenesis [86, 87], hence PGC1α may be a good target for developing a combination therapy with a BRAF inhibitor. In addition, considering that ROS can also serve as proliferative signals, this Vemurafenib-induced mitochondria-derived ROS may play a role in the cellular adaptation to the drug treatment; hence anti-oxidants may be useful in combination therapy with Vemurafenib in melanoma.
Emerging evidence show that mitochondria-generated ROS and cytosolic ROS (for example, NOX-generated ROS) interact with each other and may enhance the total cellular ROS production [88]; or some NOX isoforms may locate in mitochondria and become a source of mitochondrial ROS in addition to the ROS generated by electron transport complexes [89].
5. Redox balance in melanoma: co-evolution of ROS and cellular antioxidants
Numerous studies have shown that cancer cells including melanoma cells exhibit elevated ROS levels [12, 90], which led to testing of a wide range of antioxidants as potential chemotherapy drugs. However, melanoma cells also carry high levels of ROS-metabolizing enzymes including superoxide dismutases (SODs), catalase, and a series of redox-related transcription factors such as the AP-1 family, APE/Ref-1 gene and NFκB [91–95]. The two major antioxidant systems, glutathione (GSH) and thioredoxin (TRX) systems, are also up-regulated in melanoma cells as compared to normal human melanocytes [96–101]. Thus, high ROS levels and a more robust detoxifying antioxidant system seem to co-evolve and form a new balance in cancer cells in order to maintain ROS levels in the non-toxic ranges. One consequence of this new balance is that a more robust antioxidant enzyme system exists in melanoma cells, which renders tumor cells extremely adaptive to challenges like ROS-inducing chemotherapy drugs [90, 102]. We and others have discovered that APE/Ref-1 and Hif-1α genes are transcriptional targets for melanocytes master transcriptional factor MiTF [91, 103], suggesting that this redox balance may be through a currently undefined melanocyte lineage specific mechanism.
6. RNS (reactive nitrogen species) and ROS: a perspective relationship in melanoma
Reactive nitrogen species are a series of active molecules generated from nitric oxide and superoxide, and participate in essentially all aspects of cancer development. Nitric oxide is synthesized by nitric oxide synthase (NOS) which consists of three isoforms: neuronal NOS (nNOS, NOS1), inducible NOS (iNOS, NOS2 and endothelial NOS (eNOS, NOS3). iNOS has been well characterized in melanoma: its expression promotes cell proliferation; is associated with poor patient survival; and increases resistance to cisplatin [104–109]. Although an early study demonstrated nNOS expression in melanocytes and melanoma cells [110], these investigations were not followed up until we recently discovered that nNOS played a role in melanoma invasion and proliferation [111, 112]. The eNOS uncoupling is also an important source of superoxide in melanoma which drives the malignant transformation [113]. There have been large amount of data from cardiovascular research showing interactions between NOX and NOS pathways [114]. It is conceivable that the NOS product NO interacts with NOX product O2.− and generates peroxynitrite ONOO-, an extremely reactive molecule which can nitrosylate key signal molecules such as PTEN in melanoma, hence impacting melanoma development.
7. NOX inhibitors and their potential as melanoma drugs
Recent studies of NOX enzymes in cancer development identified these enzymes as novel targets for cancer therapy [115–117]. Nox1 enzymatic activities can be inhibited by Diphenyliodonium (DPI, a classic NOX inhibitor), VAS2870 (a NOX inhibitor in clinical trial for cardiovascular conditions), apocynin (a natural compound found in the anti-inflammatory herb Picrorhiza kurroa and a potent Nox1 inhibitor), GKT137831, ML171, triphenylmethanes, Gentian violet, GKT136901 [118–124]. All these compounds inhibit NOX activity in low µM concentration range [119, 125, 126]. Our results showed that DPI, VAS2870 and apocynin are able to kill melanoma cells in vitro, with DPI as the most potent compound and apocynin the least (Liu-Smith and Meyskens, unpublished data). However due to the non-specificity of DPI and high toxicity [127], its clinical use has been limited. VAS2870 was developed as a pan-NOX inhibitor [128], but off-targets were discovered soon after [129]. ML171 showed selectivity for Nox1, as its IC50 for Nox1 is about 20 fold lower than that for Nox2 compared to Nox4 [120]. GKT137831 inhibits both Nox1 and Nox4 [121], and effectively provided renoprotection against diabetic nephropathy in mice [130, 131]. Triphenylmethanes inhibited Nox1, Nox2 and Nox4 and showed efficacy in reducing hemangiomas growth in mice model [122]. Gentian violet antagonized Nox1-induced p53 inactivation and induced cancer cell death [123]. GKT136901, similar to GKT137831, inhibits Nox1, Nox2 and Nox4, and showed renoprotective effect in diabetic mouse model [132–134]. To date validation of most of these NOX inhibitors as targeted therapy in cancer is still needed preclinically in vivo before moving them to testing in clinical trials, but the proof of principle of the use of reactive oxygen inhibitors in melanoma is demonstrated by the use of gentian violet and imiquimod in advanced melanoma of the scalp [135].
8. Summary
We summarize recent discoveries on the source of ROS in melanocytes and melanoma cells, which mainly include three types: mitochondria ROS, melanin/melanosome ROS and NOX-generated ROS. These sources of ROS may interact with each other and promote oxidative stress in cells and play causative roles in UV-dependent or UV-independent melanomagenesis and prorgression, as well as drug resistance. As the majority of single anti-oxidant therapy trials failed to show significant effect, we reason that the elevated ROS levels co-evolve with anti-oxidant levels in cancer cells, thus largely masking the exogenous anti-oxidant effects. Hence identification of specific ROS inhibitors, such as nNOS or NOX inhibitors, may prove efficacious in combination. Possibly, dual therapy with a specific ROS inhibitor and an effective chemotherapy drug such as Vemurafenib may achieve a better outcome for patients.
Highlights.
The melanocytes cellular ROS pool includes ROS from mitochondria, melanosomes, NOX and NOS.
Nox1, Nox4 and Nox5 are expressed in melanocytic lineage
Nox1 may be involved in transformation and Nox4 in metastasis
ROS plays a role in Vemurafenib resistance
ROS from different sources interact with each other to cause severe oxidative stress
Acknowledgements
This work is supported by Chao Family Cancer Center Seed Grant (CCSG, P30 CA 62230, to FLM and FLS), the Alan Hubbell Education Grant (CSUF and UCI-CFCCC Partnership for Cancer Health Disparities Research P20 CA174188 to Hubbell and subgrant to FLS), NCI K07 (CA160756 to FLS) and Waltmar Foundation (to FLM and FLS). The authors thank Dr. Sun Yang for critical scientific discussions.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Fried L, Arbiser JL. The reactive oxygen-driven tumor: relevance to melanoma. Pigment Cell Melanoma Res. 2008;21(2):117–122. doi: 10.1111/j.1755-148X.2008.00451.x. [DOI] [PubMed] [Google Scholar]
- 2.Meyskens FL, Jr, et al. New perspectives on melanoma pathogenesis and chemoprevention. Recent Results Cancer Res. 2007;174:191–195. doi: 10.1007/978-3-540-37696-5_16. [DOI] [PubMed] [Google Scholar]
- 3.Wittgen HG, van Kempen LC. Reactive oxygen species in melanoma and its therapeutic implications. Melanoma Res. 2007;17(6):400–409. doi: 10.1097/CMR.0b013e3282f1d312. [DOI] [PubMed] [Google Scholar]
- 4.Ziech D, et al. Reactive oxygen species (ROS)--induced genetic and epigenetic alterations in human carcinogenesis. Mutat Res. 2011;711(1–2):167–173. doi: 10.1016/j.mrfmmm.2011.02.015. [DOI] [PubMed] [Google Scholar]
- 5.Wu WS. The signaling mechanism of ROS in tumor progression. Cancer Metastasis Rev. 2006;25(4):695–705. doi: 10.1007/s10555-006-9037-8. [DOI] [PubMed] [Google Scholar]
- 6.Chan EC, et al. Regulation of cell proliferation by NADPH oxidase-mediated signaling: potential roles in tissue repair, regenerative medicine and tissue engineering. Pharmacol Ther. 2009;122(2):97–108. doi: 10.1016/j.pharmthera.2009.02.005. [DOI] [PubMed] [Google Scholar]
- 7.Tandara AA, Mustoe TA. Oxygen in wound healing--more than a nutrient. World J Surg. 2004;28(3):294–300. doi: 10.1007/s00268-003-7400-2. [DOI] [PubMed] [Google Scholar]
- 8.Zhang Y, et al. Redox control of the survival of healthy and diseased cells. Antioxid Redox Signal. 2011;15(11):2867–2908. doi: 10.1089/ars.2010.3685. [DOI] [PubMed] [Google Scholar]
- 9.Groeger G, Quiney C, Cotter TG. Hydrogen peroxide as a cell-survival signaling molecule. Antioxid Redox Signal. 2009;11(11):2655–2671. doi: 10.1089/ars.2009.2728. [DOI] [PubMed] [Google Scholar]
- 10.Sauer H, Wartenberg M, Hescheler J. Reactive oxygen species as intracellular messengers during cell growth and differentiation. Cell Physiol Biochem. 2001;11(4):173–186. doi: 10.1159/000047804. [DOI] [PubMed] [Google Scholar]
- 11.Ewton DZ, et al. Inactivation of mirk/dyrk1b kinase targets quiescent pancreatic cancer cells. Mol Cancer Ther. 2011;10(11):2104–2114. doi: 10.1158/1535-7163.MCT-11-0498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Meyskens FL, Jr, et al. Aberrant redox regulation in human metastatic melanoma cells compared to normal melanocytes. Free Radic Biol Med. 2001;31(6):799–808. doi: 10.1016/s0891-5849(01)00650-5. [DOI] [PubMed] [Google Scholar]
- 13.Wondrak GT. Redox-directed cancer therapeutics: molecular mechanisms and opportunities. Antioxid Redox Signal. 2009;11(12):3013–3069. doi: 10.1089/ars.2009.2541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wallace DC. Mitochondria and cancer. Nat Rev Cancer. 2012;12(10):685–698. doi: 10.1038/nrc3365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Brand MD. The sites and topology of mitochondrial superoxide production. Exp Gerontol. 2010;45(7-–8):466–472. doi: 10.1016/j.exger.2010.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Maybury BD. Mitochondrial DNA damage is uncommon in cancer but can promote aggressive behaviour. Anticancer Res. 2013;33(9):3543–3552. [PubMed] [Google Scholar]
- 17.Filipp FV, et al. Glutamine-fueled mitochondrial metabolism is decoupled from glycolysis in melanoma. Pigment Cell Melanoma Res. 2012;25(6):732–739. doi: 10.1111/pcmr.12000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Meyskens FL, Jr, Farmer P, Fruehauf JP. Redox regulation in human melanocytes and melanoma. Pigment Cell Res. 2001;14(3):148–154. doi: 10.1034/j.1600-0749.2001.140303.x. [DOI] [PubMed] [Google Scholar]
- 19.Meyskens FL, Jr, et al. Luminol-enhanced chemiluminescent response of human melanocytes and melanoma cells to hydrogen peroxide stress. Pigment Cell Res. 1997;10(3):184–189. doi: 10.1111/j.1600-0749.1997.tb00482.x. [DOI] [PubMed] [Google Scholar]
- 20.Farmer PJ, et al. Melanin as a target for melanoma chemotherapy: pro-oxidant effect of oxygen and metals on melanoma viability. Pigment Cell Res. 2003;16(3):273–279. doi: 10.1034/j.1600-0749.2003.00046.x. [DOI] [PubMed] [Google Scholar]
- 21.Moan J, Dahlback A, Setlow RB. Epidemiological support for an hypothesis for melanoma induction indicating a role for UVA radiation. Photochem Photobiol. 1999;70(2):243–247. [PubMed] [Google Scholar]
- 22.Greco G, et al. The fundamental building blocks of red human hair pheomelanin are isoquinoline-containing dimers. Pigment Cell Melanoma Res. 2012;25(1):110–112. doi: 10.1111/j.1755-148X.2011.00896.x. [DOI] [PubMed] [Google Scholar]
- 23.Greco G, et al. Uncovering the structure of human red hair pheomelanin: benzothiazolylthiazinodihydroisoquinolines as key building blocks. J Nat Prod. 2011;74(4):675–682. doi: 10.1021/np100740n. [DOI] [PubMed] [Google Scholar]
- 24.Panzella L, et al. Red human hair pheomelanin is a potent pro-oxidant mediating UV-independent contributory mechanisms of melanomagenesis. Pigment Cell Melanoma Res. 2013 doi: 10.1111/pcmr.12199. [DOI] [PubMed] [Google Scholar]
- 25.Panzella L, et al. Zinc-induced structural effects enhance oxygen consumption and superoxide generation in synthetic pheomelanins on UVA/visible light irradiation. Photochem Photobiol. 2010;86(4):757–764. doi: 10.1111/j.1751-1097.2010.00726.x. [DOI] [PubMed] [Google Scholar]
- 26.Valencia A, Kochevar IE. Nox1-based NADPH oxidase is the major source of UVA-induced reactive oxygen species in human keratinocytes. J Invest Dermatol. 2008;128(1):214–222. doi: 10.1038/sj.jid.5700960. [DOI] [PubMed] [Google Scholar]
- 27.Wu S, et al. IL-8 production and AP-1 transactivation induced by UVA in human keratinocytes: roles of D-alpha-tocopherol. Mol Immunol. 2008;45(8):2288–2296. doi: 10.1016/j.molimm.2007.11.019. [DOI] [PubMed] [Google Scholar]
- 28.Morre DJ, et al. Capsaicin inhibits plasma membrane NADH oxidase and growth of human and mouse melanoma lines. Eur J Cancer. 1996;32A(11):1995–2003. doi: 10.1016/0959-8049(96)00234-1. [DOI] [PubMed] [Google Scholar]
- 29.Brar SS, et al. An NAD(P)H oxidase regulates growth and transcription in melanoma cells. Am J Physiol Cell Physiol. 2002;282(6):C1212–C1224. doi: 10.1152/ajpcell.00496.2001. [DOI] [PubMed] [Google Scholar]
- 30.Govindarajan B, et al. Overexpression of Akt converts radial growth melanoma to vertical growth melanoma. J Clin Invest. 2007;117(3):719–729. doi: 10.1172/JCI30102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Liu GS, et al. Microphthalmia-associated transcription factor modulates expression of NADPH oxidase type 4: a negative regulator of melanogenesis. Free Radic Biol Med. 2012;52(9):1835–1843. doi: 10.1016/j.freeradbiomed.2012.02.040. [DOI] [PubMed] [Google Scholar]
- 32.Liu F, Gomez Garcia AM, Meyskens FL., Jr NADPH oxidase 1 overexpression enhances invasion via matrix metalloproteinase-2 and epithelial-mesenchymal transition in melanoma cells. J Invest Dermatol. 2012;132(8):2033–2041. doi: 10.1038/jid.2012.119. [DOI] [PubMed] [Google Scholar]
- 33.Antony S, et al. Characterization of NADPH oxidase 5 expression in human tumors and tumor cell lines with a novel mouse monoclonal antibody. Free Radic Biol Med. 2013;65:497–508. doi: 10.1016/j.freeradbiomed.2013.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Opitz N, et al. The 'A's and 'O's of NADPH oxidase regulation: a commentary on "Subcellular localization and function of alternatively spliced Noxo1 isoforms". Free Radic Biol Med. 2007;42(2):175–179. doi: 10.1016/j.freeradbiomed.2006.11.003. [DOI] [PubMed] [Google Scholar]
- 35.Dworakowski R, et al. Redox signalling involving NADPH oxidase-derived reactive oxygen species. Biochem Soc Trans. 2006;34(Pt 5):960–964. doi: 10.1042/BST0340960. [DOI] [PubMed] [Google Scholar]
- 36.Lambeth JD, Kawahara T, Diebold B. Regulation of Nox and Duox enzymatic activity and expression. Free Radic Biol Med. 2007;43(3):319–331. doi: 10.1016/j.freeradbiomed.2007.03.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yamaguchi Y, Hearing VJ. Physiological factors that regulate skin pigmentation. Biofactors. 2009;35(2):193–199. doi: 10.1002/biof.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Abdel-Malek Z, et al. The melanocortin-1 receptor and human pigmentation. Ann N Y Acad Sci. 1999;885:117–133. doi: 10.1111/j.1749-6632.1999.tb08669.x. [DOI] [PubMed] [Google Scholar]
- 39.Swope VB, et al. Defining MC1R regulation in human melanocytes by its agonist alpha-melanocortin and antagonists agouti signaling protein and beta-defensin 3. J Invest Dermatol. 2012;132(9):2255–2262. doi: 10.1038/jid.2012.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sturm RA. Skin colour and skin cancer - MC1R, the genetic link. Melanoma Res. 2002;12(5):405–416. doi: 10.1097/00008390-200209000-00001. [DOI] [PubMed] [Google Scholar]
- 41.Maccioni L, et al. Variants at chromosome 20 (ASIP locus) and melanoma risk. Int J Cancer. 2013;132(1):42–54. doi: 10.1002/ijc.27648. [DOI] [PubMed] [Google Scholar]
- 42.Gudbjartsson DF, et al. ASIP and TYR pigmentation variants associate with cutaneous melanoma and basal cell carcinoma. Nat Genet. 2008;40(7):886–891. doi: 10.1038/ng.161. [DOI] [PubMed] [Google Scholar]
- 43.Mitra D, et al. An ultraviolet-radiation-independent pathway to melanoma carcinogenesis in the red hair/fair skin background. Nature. 2012;491(7424):449–453. doi: 10.1038/nature11624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Song X, et al. alpha-MSH activates immediate defense responses to UV-induced oxidative stress in human melanocytes. Pigment Cell Melanoma Res. 2009;22(6):809–818. doi: 10.1111/j.1755-148X.2009.00615.x. [DOI] [PubMed] [Google Scholar]
- 45.Abdel-Malek ZA, et al. The melanocortin 1 receptor and the UV response of human melanocytes--a shift in paradigm. Photochem Photobiol. 2008;84(2):501–508. doi: 10.1111/j.1751-1097.2008.00294.x. [DOI] [PubMed] [Google Scholar]
- 46.Henri P, et al. MC1R expression in HaCaT keratinocytes inhibits UVA-induced ROS production via NADPH oxidase- and cAMP-dependent mechanisms. J Cell Physiol. 2012;227(6):2578–2585. doi: 10.1002/jcp.22996. [DOI] [PubMed] [Google Scholar]
- 47.Ueyama T, Geiszt M, Leto TL. Involvement of Rac1 in activation of multicomponent Nox1- and Nox3-based NADPH oxidases. Mol Cell Biol. 2006;26(6):2160–2174. doi: 10.1128/MCB.26.6.2160-2174.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kroviarski Y, et al. Phosphorylation of NADPH oxidase activator 1 (NOXA1) on serine 282 by MAP kinases and on serine 172 by protein kinase C and protein kinase A prevents NOX1 hyperactivation. Faseb J. 24(6):2077–2092. doi: 10.1096/fj.09-147629. [DOI] [PubMed] [Google Scholar]
- 49.Hiramoto K, Sato EF. Ultraviolet B radiation to the eye induces pigmentation in the epidermis via the activation of the subunit gp91 phox of reduced nicotinamide adenine dinucleotide phosphate oxidase. Clin Exp Dermatol. 2012;37(1):65–67. doi: 10.1111/j.1365-2230.2011.04149.x. [DOI] [PubMed] [Google Scholar]
- 50.Wingler K, et al. NOX1, 2, 4, 5: counting out oxidative stress. Br J Pharmacol. 2011;164(3):866–883. doi: 10.1111/j.1476-5381.2011.01249.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kelkka T, et al. Mice lacking NCF1 exhibit reduced growth of implanted melanoma and carcinoma tumors. PLoS One. 2013;8(12):e84148. doi: 10.1371/journal.pone.0084148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Yamaura M, et al. NADPH oxidase 4 contributes to transformation phenotype of melanoma cells by regulating G2-M cell cycle progression. Cancer Res. 2009;69(6):2647–2654. doi: 10.1158/0008-5472.CAN-08-3745. [DOI] [PubMed] [Google Scholar]
- 53.Chapman PB, et al. Improved survival with vemurafenib in melanoma with BRAF V600E mutation. N Engl J Med. 2011;364(26):2507–2516. doi: 10.1056/NEJMoa1103782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Flaherty KT, et al. Inhibition of mutated, activated BRAF in metastatic melanoma. N Engl J Med. 2010;363(9):809–819. doi: 10.1056/NEJMoa1002011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Flaherty KT, et al. Improved survival with MEK inhibition in BRAF-mutated melanoma. N Engl J Med. 2012;367(2):107–114. doi: 10.1056/NEJMoa1203421. [DOI] [PubMed] [Google Scholar]
- 56.Ishikawa K, Hayashi J. A novel function of mtDNA: its involvement in metastasis. Ann N Y Acad Sci. 2010;1201:40–43. doi: 10.1111/j.1749-6632.2010.05616.x. [DOI] [PubMed] [Google Scholar]
- 57.Koshikawa N, et al. Reactive oxygen species-generating mitochondrial DNA mutation up-regulates hypoxia-inducible factor-1alpha gene transcription via phosphatidylinositol 3-kinase-Akt/protein kinase C/histone deacetylase pathway. J Biol Chem. 2009;284(48):33185–33194. doi: 10.1074/jbc.M109.054221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Evers EE, et al. Rho family proteins in cell adhesion and cell migration. Eur J Cancer. 2000;36(10):1269–1274. doi: 10.1016/s0959-8049(00)00091-5. [DOI] [PubMed] [Google Scholar]
- 59.Alan JK, Lundquist EA. Mutationally activated Rho GTPases in cancer. Small GTPases. 2013;4(3) doi: 10.4161/sgtp.26530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Fukata M, Kaibuchi K. Rho-family GTPases in cadherin-mediated cell-cell adhesion. Nat Rev Mol Cell Biol. 2001;2(12):887–897. doi: 10.1038/35103068. [DOI] [PubMed] [Google Scholar]
- 61.Hordijk PL. Regulation of NADPH oxidases: the role of Rac proteins. Circ Res. 2006;98(4):453–462. doi: 10.1161/01.RES.0000204727.46710.5e. [DOI] [PubMed] [Google Scholar]
- 62.Miyano K, Sumimoto H. Role of the small GTPase Rac in p22phox-dependent NADPH oxidases. Biochimie. 2007;89(9):1133–1144. doi: 10.1016/j.biochi.2007.05.003. [DOI] [PubMed] [Google Scholar]
- 63.Miyano K, et al. Direct involvement of the small GTPase Rac in activation of the superoxide-producing NADPH oxidase Nox1. J Biol Chem. 2006;281(31):21857–21868. doi: 10.1074/jbc.M513665200. [DOI] [PubMed] [Google Scholar]
- 64.Park HS, et al. Sequential activation of phosphatidylinositol 3-kinase, beta Pix, Rac1, and Nox1 in growth factor-induced production of H2O2. Mol Cell Biol. 2004;24(10):4384–4394. doi: 10.1128/MCB.24.10.4384-4394.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Cheng G, et al. Nox1-dependent reactive oxygen generation is regulated by Rac1. J Biol Chem. 2006;281(26):17718–17726. doi: 10.1074/jbc.M512751200. [DOI] [PubMed] [Google Scholar]
- 66.Kim Y, et al. CD44-epidermal growth factor receptor interaction mediates hyaluronic acid-promoted cell motility by activating protein kinase C signaling involving Akt, Rac1, Phox, reactive oxygen species, focal adhesion kinase, and MMP-2. J Biol Chem. 2008;283(33):22513–22528. doi: 10.1074/jbc.M708319200. [DOI] [PubMed] [Google Scholar]
- 67.Park SJ, Kim YT, Jeon YJ. Antioxidant dieckol downregulates the Rac1/ROS signaling pathway and inhibits Wiskott-Aldrich syndrome protein (WASP)-family verprolin-homologous protein 2 (WAVE2)-mediated invasive migration of B16 mouse melanoma cells. Mol Cells. 2012;33(4):363–369. doi: 10.1007/s10059-012-2285-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Wang R, et al. NADPH oxidase overexpression in human colon cancers and rat colon tumors induced by 2-amino-1-methyl-6-phenylimidazo[4,5-b]pyridine (PhIP) Int J Cancer. 2011;128(11):2581–2590. doi: 10.1002/ijc.25610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Sun Z, Liu F. Association of Nox1 and vinculin with colon cancer progression. Cancer Invest. 2013;31(4):273–278. doi: 10.3109/07357907.2013.789897. [DOI] [PubMed] [Google Scholar]
- 70.Xu L, et al. Gene expression changes in an animal melanoma model correlate with aggressiveness of human melanoma metastases. Mol Cancer Res. 2008;6(5):760–769. doi: 10.1158/1541-7786.MCR-07-0344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Hodis E, et al. A landscape of driver mutations in melanoma. Cell. 2012;150(2):251–263. doi: 10.1016/j.cell.2012.06.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Bhandarkar SS, et al. Fulvene-5 potently inhibits NADPH oxidase 4 and blocks the growth of endothelial tumors in mice. J Clin Invest. 2009;119(8):2359–2365. doi: 10.1172/JCI33877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.de Carvalho DD, et al. Nox1 downstream of 12-lipoxygenase controls cell proliferation but not cell spreading of colon cancer cells. Int J Cancer. 2008;122(8):1757–1764. doi: 10.1002/ijc.23300. [DOI] [PubMed] [Google Scholar]
- 74.Winer I, et al. Expression of 12-lipoxygenase as a biomarker for melanoma carcinogenesis. Melanoma Res. 2002;12(5):429–434. doi: 10.1097/00008390-200209000-00003. [DOI] [PubMed] [Google Scholar]
- 75.Dellinger RW, et al. Anti-cancer drugs elicit re-expression of UDP-glucuronosyltransferases in melanoma cells. PLoS One. 2012;7(10):e47696. doi: 10.1371/journal.pone.0047696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Turgeon D, et al. Glucuronidation of arachidonic and linoleic acid metabolites by human UDP-glucuronosyltransferases. J Lipid Res. 2003;44(6):1182–1191. doi: 10.1194/jlr.M300010-JLR200. [DOI] [PubMed] [Google Scholar]
- 77.Pidgeon GP, et al. Lipoxygenase metabolism: roles in tumor progression and survival. Cancer Metastasis Rev. 2007;26(3–4):503–524. doi: 10.1007/s10555-007-9098-3. [DOI] [PubMed] [Google Scholar]
- 78.Quast SA, Berger A, Eberle J. ROS-dependent phosphorylation of Bax by wortmannin sensitizes melanoma cells for TRAIL-induced apoptosis. Cell Death Dis. 2013;4:e839. doi: 10.1038/cddis.2013.344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Liu GS, et al. Proopiomelanocortin gene delivery induces apoptosis in melanoma through NADPH oxidase 4-mediated ROS generation. Free Radic Biol Med. 2014 doi: 10.1016/j.freeradbiomed.2013.12.024. [DOI] [PubMed] [Google Scholar]
- 80.Flaherty KT, Yasothan U, Kirkpatrick P. Vemurafenib. Nat Rev Drug Discov. 2011;10(11):811–812. doi: 10.1038/nrd3579. [DOI] [PubMed] [Google Scholar]
- 81.Nazarian R, et al. Melanomas acquire resistance to B-RAF(V600E) inhibition by RTK or N-RAS upregulation. Nature. 2010;468(7326):973–977. doi: 10.1038/nature09626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Corcoran RB, Settleman J, Engelman JA. Potential therapeutic strategies to overcome acquired resistance to BRAF or MEK inhibitors in BRAF mutant cancers. Oncotarget. 2011;2(4):336–346. doi: 10.18632/oncotarget.262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Prahallad A, et al. Unresponsiveness of colon cancer to BRAF(V600E) inhibition through feedback activation of EGFR. Nature. 2012 doi: 10.1038/nature10868. [DOI] [PubMed] [Google Scholar]
- 84.Hatzivassiliou G, et al. RAF inhibitors prime wild-type RAF to activate the MAPK pathway and enhance growth. Nature. 2010;464(7287):431–435. doi: 10.1038/nature08833. [DOI] [PubMed] [Google Scholar]
- 85.Mehdi MZ, Azar ZM, Srivastava AK. Role of receptor and nonreceptor protein tyrosine kinases in H2O2-induced PKB and ERK1/2 signaling. Cell Biochem Biophys. 2007;47(1):1–10. doi: 10.1385/cbb:47:1:1. [DOI] [PubMed] [Google Scholar]
- 86.Haq R, et al. Oncogenic BRAF regulates oxidative metabolism via PGC1alpha and MITF. Cancer Cell. 2013;23(3):302–315. doi: 10.1016/j.ccr.2013.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Vazquez F, et al. PGC1alpha Expression Defines a Subset of Human Melanoma Tumors with Increased Mitochondrial Capacity and Resistance to Oxidative Stress. Cancer Cell. 2013;23(3):287–301. doi: 10.1016/j.ccr.2012.11.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Daiber A. Redox signaling (cross-talk) from and to mitochondria involves mitochondrial pores and reactive oxygen species. Biochim Biophys Acta. 2010;1797(6–7):897–906. doi: 10.1016/j.bbabio.2010.01.032. [DOI] [PubMed] [Google Scholar]
- 89.Frazziano G, et al. Nox-derived ROS are acutely activated in pressure overload pulmonary hypertension: indications for a seminal role for mitochondrial Nox4. Am J Physiol Heart Circ Physiol. 2014;306(2):H197–H205. doi: 10.1152/ajpheart.00977.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Fruehauf JP, Meyskens FL., Jr Reactive oxygen species: a breath of life or death? Clin Cancer Res. 2007;13(3):789–794. doi: 10.1158/1078-0432.CCR-06-2082. [DOI] [PubMed] [Google Scholar]
- 91.Liu F, Fu Y, Meyskens FL., Jr MiTF regulates cellular response to reactive oxygen species through transcriptional regulation of APE-1/Ref-1. J Invest Dermatol. 2009;129(2):422–431. doi: 10.1038/jid.2008.255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.McNulty SE, Tohidian NB, Meyskens FL., Jr RelA, p50 and inhibitor of kappa B alpha are elevated in human metastatic melanoma cells and respond aberrantly to ultraviolet light B. Pigment Cell Res. 2001;14(6):456–465. doi: 10.1034/j.1600-0749.2001.140606.x. [DOI] [PubMed] [Google Scholar]
- 93.Meyskens FL, Jr, et al. Activation of nuclear factor-kappa B in human metastatic melanomacells and the effect of oxidative stress. Clin Cancer Res. 1999;5(5):1197–1202. [PubMed] [Google Scholar]
- 94.Yamanishi DT, Meyskens FL., Jr Alterations in gene expression and signal transductions in human melanocytes and melanoma cells. Crit Rev Oncog. 1994;5(5):429–450. doi: 10.1615/critrevoncog.v5.i5.10. [DOI] [PubMed] [Google Scholar]
- 95.Yang S, et al. Alterations in the expression of the apurinic/apyrimidinic endonuclease-1/redox factor-1 (APE/Ref-1) in human melanoma and identification of the therapeutic potential of resveratrol as an APE/Ref-1 inhibitor. Mol Cancer Ther. 2005;4(12):1923–1935. doi: 10.1158/1535-7163.MCT-05-0229. [DOI] [PubMed] [Google Scholar]
- 96.Lubos E, Loscalzo J, Handy DE. Glutathione peroxidase-1 in health and disease: from molecular mechanisms to therapeutic opportunities. Antioxid Redox Signal. 2011;15(7):1957–1997. doi: 10.1089/ars.2010.3586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Kinnula VL, Crapo JD. Superoxide dismutases in malignant cells and human tumors. Free Radic Biol Med. 2004;36(6):718–744. doi: 10.1016/j.freeradbiomed.2003.12.010. [DOI] [PubMed] [Google Scholar]
- 98.Arner ES, Holmgren A. The thioredoxin system in cancer. Semin Cancer Biol. 2006;16(6):420–426. doi: 10.1016/j.semcancer.2006.10.009. [DOI] [PubMed] [Google Scholar]
- 99.Estrela JM, Ortega A, Obrador E. Glutathione in cancer biology and therapy. Crit Rev Clin Lab Sci. 2006;43(2):143–181. doi: 10.1080/10408360500523878. [DOI] [PubMed] [Google Scholar]
- 100.Powis G, Kirkpatrick DL. Thioredoxin signaling as a target for cancer therapy. Curr Opin Pharmacol. 2007;7(4):392–397. doi: 10.1016/j.coph.2007.04.003. [DOI] [PubMed] [Google Scholar]
- 101.Ortega A, et al. Tumoricidal activity of endothelium-derived NO and the survival of metastatic cells with high GSH and Bcl-2 levels. Nitric Oxide. 2008;19(2):107–114. doi: 10.1016/j.niox.2008.04.010. [DOI] [PubMed] [Google Scholar]
- 102.Trachootham D, Alexandre J, Huang P. Targeting cancer cells by ROS-mediated mechanisms: a radical therapeutic approach? Nat Rev Drug Discov. 2009;8(7):579–591. doi: 10.1038/nrd2803. [DOI] [PubMed] [Google Scholar]
- 103.Busca R, et al. Hypoxia-inducible factor 1{alpha} is a new target of microphthalmia-associated transcription factor (MITF) in melanoma cells. J Cell Biol. 2005;170(1):49–59. doi: 10.1083/jcb.200501067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Tanese K, Grimm EA, Ekmekcioglu S. The role of melanoma tumor-derived nitric oxide in the tumor inflammatory microenvironment: its impact on the chemokine expression profile, including suppression of CXCL10. Int J Cancer. 2012;131(4):891–901. doi: 10.1002/ijc.26451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Ekmekcioglu S, et al. Inducible nitric oxide synthase and nitrotyrosine in human metastatic melanoma tumors correlate with poor survival. Clin Cancer Res. 2000;6(12):4768–4775. [PubMed] [Google Scholar]
- 106.Lopez-Rivera E, et al. Inducible Nitric Oxide Synthase Drives mTOR Pathway Activation and Proliferation of Human Melanoma by Reversible Nitrosylation of TSC2. Cancer Res. 2014;74(4):1067–1078. doi: 10.1158/0008-5472.CAN-13-0588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Sikora AG, et al. Targeted inhibition of inducible nitric oxide synthase inhibits growth of human melanoma in vivo and synergizes with chemotherapy. Clin Cancer Res. 2010;16(6):1834–1844. doi: 10.1158/1078-0432.CCR-09-3123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Godoy LC, et al. Endogenously produced nitric oxide mitigates sensitivity of melanoma cells to cisplatin. Proc Natl Acad Sci U S A. 2012;109(50):20373–20378. doi: 10.1073/pnas.1218938109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Yang Z, et al. Nitric oxide initiates progression of human melanoma via a feedback loop mediated by apurinic/apyrimidinic endonuclease-1/redox factor-1, which is inhibited by resveratrol. Mol Cancer Ther. 2008;7(12):3751–3760. doi: 10.1158/1535-7163.MCT-08-0562. [DOI] [PubMed] [Google Scholar]
- 110.Ahmed B, Van Den Oord JJ. Expression of the neuronal isoform of nitric oxide synthase (nNOS) and its inhibitor, protein inhibitor of nNOS, in pigment cell lesions of the skin. Br J Dermatol. 1999;141(1):12–19. doi: 10.1046/j.1365-2133.1999.02915.x. [DOI] [PubMed] [Google Scholar]
- 111.Huang H, et al. Potent and Selective Double-Headed Thiophene-2-carboximidamide Inhibitors of Neuronal Nitric Oxide Synthase for the Treatment of Melanoma. J Med Chem. 2014;57(3):686–700. doi: 10.1021/jm401252e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Yang Z, et al. Targeting Nitric Oxide Signaling with nNOS Inhibitors As a Novel Strategy for the Therapy and Prevention of Human Melanoma. Antioxid Redox Signal. 2013 doi: 10.1089/ars.2012.4563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Melo FH, et al. Endothelial nitric oxide synthase uncoupling as a key mediator of melanocyte malignant transformation associated with sustained stress conditions. Free Radic Biol Med. 2011;50(10):1263–1273. doi: 10.1016/j.freeradbiomed.2011.02.022. [DOI] [PubMed] [Google Scholar]
- 114.Armitage ME, et al. Translating the oxidative stress hypothesis into the clinic: NOX versus NOS. J Mol Med. 2009;87(11):1071–1076. doi: 10.1007/s00109-009-0544-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Kamata T. Roles of Nox1 and other Nox isoforms in cancer development. Cancer Sci. 2009;100(8):1382–1388. doi: 10.1111/j.1349-7006.2009.01207.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Laurent E, et al. Nox1 is over-expressed in human colon cancers and correlates with activating mutations in K-Ras. Int J Cancer. 2008;123(1):100–107. doi: 10.1002/ijc.23423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Ushio-Fukai M, Nakamura Y. Reactive oxygen species and angiogenesis: NADPH oxidase as target for cancer therapy. Cancer Lett. 2008;266(1):37–52. doi: 10.1016/j.canlet.2008.02.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Gianni D, et al. A Novel and Specific NADPH Oxidase-1 (Nox1) Small-Molecule Inhibitor Blocks the Formation of Functional Invadopodia in Human Colon Cancer Cells. ACS Chem Biol. 2010 doi: 10.1021/cb100219n. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.ten Freyhaus H, et al. Novel Nox inhibitor VAS2870 attenuates PDGF-dependent smooth muscle cell chemotaxis, but not proliferation. Cardiovasc Res. 2006;71(2):331–341. doi: 10.1016/j.cardiores.2006.01.022. [DOI] [PubMed] [Google Scholar]
- 120.Altenhofer S, et al. Evolution of NADPH oxidase inhibitors: Selectivity and mechanisms for target engagement. Antioxid Redox Signal. 2014 doi: 10.1089/ars.2013.5814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Jiang JX, et al. Liver fibrosis and hepatocyte apoptosis are attenuated by GKT137831, a novel NOX4/NOX1 inhibitor in vivo. Free Radic Biol Med. 2012;53(2):289–296. doi: 10.1016/j.freeradbiomed.2012.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Perry BN, et al. Pharmacologic blockade of angiopoietin-2 is efficacious against model hemangiomas in mice. J Invest Dermatol. 2006;126(10):2316–2222. doi: 10.1038/sj.jid.5700413. [DOI] [PubMed] [Google Scholar]
- 123.Garufi A, et al. Gentian violet induces wtp53 transactivation in cancer cells. Int J Oncol. 2014;44(4):1084–1090. doi: 10.3892/ijo.2014.2304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Garrido-Urbani S, et al. Targeting vascular NADPH oxidase 1 blocks tumor angiogenesis through a PPARalpha mediated mechanism. PLoS One. 2011;6(2):e14665. doi: 10.1371/journal.pone.0014665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Simons JM, et al. Metabolic activation of natural phenols into selective oxidative burst agonists by activated human neutrophils. Free Radic Biol Med. 1990;8(3):251–258. doi: 10.1016/0891-5849(90)90070-y. [DOI] [PubMed] [Google Scholar]
- 126.Guzik TJ, Harrison DG. Vascular NADPH oxidases as drug targets for novel antioxidant strategies. Drug Discov Today. 2006;11(11–12):524–533. doi: 10.1016/j.drudis.2006.04.003. [DOI] [PubMed] [Google Scholar]
- 127.Tazzeo T, Worek F, Janssen L. The NADPH oxidase inhibitor diphenyleneiodonium is also a potent inhibitor of cholinesterases and the internal Ca(2+) pump. Br J Pharmacol. 2009;158(3):790–796. doi: 10.1111/j.1476-5381.2009.00394.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Wingler K, et al. VAS2870 is a pan-NADPH oxidase inhibitor. Cell Mol Life Sci. 2012;69(18):3159–3160. doi: 10.1007/s00018-012-1107-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Sun QA, et al. Off-target thiol alkylation by the NADPH oxidase inhibitor 3-benzyl-7-(2-benzoxazolyl)thio-1,2,3-triazolo[4,5-d]pyrimidine (VAS2870) Free Radic Biol Med. 2012;52(9):1897–1902. doi: 10.1016/j.freeradbiomed.2012.02.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Gray SP, et al. NADPH oxidase 1 plays a key role in diabetes mellitus-accelerated atherosclerosis. Circulation. 2013;127(18):1888–1902. doi: 10.1161/CIRCULATIONAHA.112.132159. [DOI] [PubMed] [Google Scholar]
- 131.Jha JC, et al. Genetic Targeting or Pharmacologic Inhibition of NADPH Oxidase Nox4 Provides Renoprotection in Long-Term Diabetic Nephropathy. J Am Soc Nephrol. 2014 doi: 10.1681/ASN.2013070810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Briones AM, et al. Differential regulation of Nox1, Nox2 and Nox4 in vascular smooth muscle cells from WKY and SHR. J Am Soc Hypertens. 2011;5(3):137–153. doi: 10.1016/j.jash.2011.02.001. [DOI] [PubMed] [Google Scholar]
- 133.Schildknecht S, et al. The NOX1/4 inhibitor GKT136901 as selective and direct scavenger of peroxynitrite. Curr Med Chem. 2013;21(3):365–376. doi: 10.2174/09298673113209990179. [DOI] [PubMed] [Google Scholar]
- 134.Sedeek M, et al. Renoprotective effects of a novel Nox1/4 inhibitor in a mouse model of Type 2 diabetes. Clin Sci (Lond) 2013;124(3):191–202. doi: 10.1042/CS20120330. [DOI] [PubMed] [Google Scholar]
- 135.Arbiser JL, et al. Combination therapy of imiquimod and gentian violet for cutaneous melanoma metastases. J Am Acad Dermatol. 2012;67(2):e81–e83. doi: 10.1016/j.jaad.2011.10.028. [DOI] [PMC free article] [PubMed] [Google Scholar]