Abstract
Purpose
To improve adolescent notification of positive sexually transmitted infection (STI) tests using mobile phone technology and STI information cards.
Methods
A randomized intervention among 14-21 year-olds in a pediatric emergency department (PED). A 2×3 factorial design with replication was used to evaluate the effectiveness of six combinations of two factors on the proportion of STI-positive adolescents notified within 7 days of testing. Independent factors included: method of notification (call, text message, or call + text message) and provision of an STI information card with or without a phone number to obtain results. Covariates for logistic regression included age, empiric STI treatment, days until first attempted notification and documentation of confidential phone number.
Results
Approximately half of the 383 females and 201 males enrolled were ≥ 18 years. Texting only or type of card was not significantly associated with patient notification rates, and there was no significant interaction between card and notification method. For females, successful notification was significantly greater for call + text message (OR 3.2 [95% CI 1.4, 6.9]), and documenting a confidential phone number was independently associated with successful notification (OR 3.6 [95% CI 1.7, 7.5]). We found no significant predictors of successful notification for males. Of patients with a documented confidential phone number who received a call + text message, 94% of females and 83% of males were successfully notified.
Conclusions
Obtaining a confidential phone number and using call + text message improved STI notification rates among female but not male adolescents in a PED.
Keywords: emergency medicine, healthcare quality improvement, adolescents, sexually transmitted disease, text messaging
INTRODUCTION
In the United States (US), 15-24 year olds represent half of all newly acquired sexually transmitted infections (STI), and high STI rates are seen among pediatric emergency department (PED) patients at many institutions [1-3]. Previous literature has shown that communication of positive STI test results to adolescents subsequently improved self-reported future condom use, abstinence rates and partner notification [4, 5]. However, women treated empirically with antibiotics but unaware they tested positive for STIs did not change their behavior [6]. This suggests that interventions, including improved notification of test results, are needed to decrease adolescent STI rates [7].
Despite national guidelines for STI control and treatment, emergency department (ED) clinical practices related to diagnosis, treatment, and prevention of STIs among adolescents are suboptimal [8, 9]. Often, those who have positive STI results untreated at the time of testing are lost to follow-up and remain untreated [10]. Additionally, many who test positive and were empirically treated in the ED are not routinely notified regarding their positive STI results. These deficiencies in clinical practice are often driven by barriers to effectively communicate STI results to patients. Historically, in our institution, less than half (45%) of STI positive (gonorrhea (GC), Chlamydia (CT) or trichomoniasis (trich)) female ED patients were notified and treated within 7 days [11]. With our previous interventions to improve electronic medical record (EMR) documentation of a confidential phone number, the distribution of STI patient information cards with a phone number to call for test results and a dedicated mobile phone for STI follow-up calls, we were able to increase STI positive female patients notified from 45% to 65% which was still suboptimal [11].
Text messaging is a promising method for communicating health-related information to adolescents as many report owning a cell phone and using text messaging [12-14]. Patients report that receiving text messages for sexual health care related information is highly acceptable [14, 15]. While text messaging has been used increasingly in sexual health promotion, the clinical effectiveness of text messaging to communicate STI results in the US has not been evaluated [16-18]. If text messaging is effective in improving notification of infected individuals, this contact method could lead to improved patient outcomes including decreasing rates of overtreatment and increasing rates of appropriate treatment. ED physicians routinely over treat patients for STI infections fearing they will be lost in follow-up [19]. In order to assure appropriate treatment, it is necessary to first assure that one can be contacted in follow-up to provide the appropriate prescription or appointment necessary to receive treatment. This in turn may contribute to decreasing the prevalence of STIs, and the cost of overtreatment and secondary clinical complications related to STIs [20, 21].
The specific aim of this study was to test the effectiveness of PED system interventions, including mobile phone call and texting technologies and STI information cards, in improving notification of positive STI (GC, CT or trich) test results among adolescents.
METHODS
Study Design
This study was a planned experiment with a 2x3 factorial design. Factorial design has been used successfully in healthcare research for improving complex processes and was chosen over the classic randomized controlled trial because it is an efficient methodology for studying the effect of multiple components of an intervention (factors) on an outcome as well as providing estimates of interaction effects [22, 23].
Because our previous work had focused on female adolescents, and they have significant risk for complications associated with untreated STIs, this study was initially done among females. We then obtained additional funding and included the male population in a second study using the same study design. Both studies are presented in this manuscript.
Based on our previous work, we anticipated that two factors may have an impact on results notification [11]. The first factor was the method of contact which included either: call, text message, or call + text message. The second factor was an STI patient information card given at the time of the PED visit consisting of 2 versions. Both versions (card 1 and 2) indicated the patient was tested for STIs and would be notified of positive results. Card 2 also included a mobile phone number to call for results between 9am and 5pm.
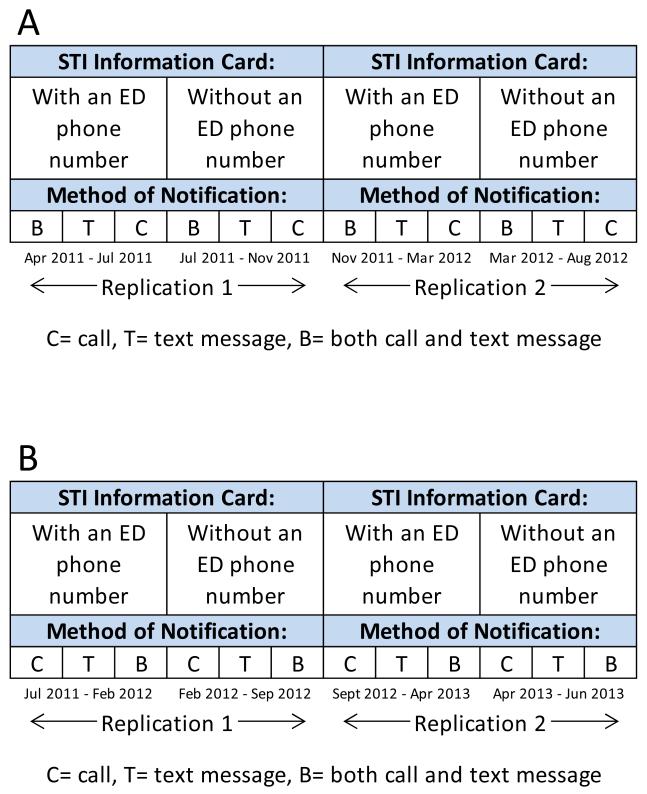
Figure 1 depicts the experimental design. The method of notification was randomized at the patient level when the tests were resulted after the patient visit. Since the card was a system level intervention that was distributed by the healthcare provider at the time of the visit, randomization at the patient level was not feasible. Thus we randomized the type of card to one of two blocks of time. As a result, the type of card would have been confounded with time. Thus, we repeated the experimental design (replications 1 and 2). Each intervention combination was tested until a sufficient sample size was obtained for each gender. The study was submitted to the Institutional Review Board (IRB) at Cincinnati Children’s Hospital Medical Center, was determined to not be human subjects research and was exempt from further IRB review.
Figure 1.
Experimental Design (A: Females, B: Males)
Based on preliminary data, we anticipated that over a 12-month time period approximately 400 females and 245 males would test STI positive. For the female population, a sample size of 420 would result in 70 patients receiving each of the 6 intervention combinations and 140 receiving each of the 3 contact methods. From our previous female studies, we anticipated that we would be able to improve the percent of successful contacts as follows: call only (65%), text only (75%), both text and call (82%).[11] We did not have previous data regarding male contact rates, but we expected that the rates would be similar. Therefore, a total sample size of 420 would result in a power of 84% to detect these differences. In the event that there would be fewer patients (n= 360), we would have a power of 78% to detect those differences.
Setting
This study was conducted in the ED of a tertiary care, urban, pediatric hospital that has 90,000 yearly visits, of which approximately 20% are adolescents. Approximately 45% of ED users are Black, 46% White and 9% other; 29% have private insurance, 66% Medicaid and the remainder are self-pay.
Selection of Participants
Our population included 14 to 21 year olds who tested positive for CT, GC or trich during their PED visit between April 2011 - August 2012 (females) and July 2011 - June 2013 (males). Those that had EMR documentation that they were unable to receive text messages were excluded; however, those with no documentation were included.
Study Protocol
In contrast to our historical ED clinical practice which involved notifying only STI positive patients who were untreated, the clinical nurse or nurse practitioner (NP) attempted to notify all STI positive patients regardless of ED treatment. The state of Ohio allows minors to consent for STI services and does not require parental notification, thus all communication was done between a healthcare provider and the adolescent. During the first half of replication 1, each patient received STI information card 2 with a dedicated mobile phone number to call for results. Female cards were pink and male cards were blue to assure the correct distribution during overlapping time periods. As soon as test results were available, notification attempts began. All positive test results were placed in chronologic order according to the date and time of ED arrival, and patients received one of the three notification methods. During the second half of replication 1, each patient received STI information card 1 without a phone number for test results. Similarly, patients with positive results during this block of time received one of the three notification methods. The study was replicated for both genders using the same methods as previously described.
Our previous improvement work had resulted in an EMR system where providers were encouraged to document a confidential phone number (provided by the adolescent to use only to relay test results) and its ability to accept text messages [11]. The confidential phone number was attempted first, but if not listed, the number given at registration was used. The nurse/NP used a designated mobile phone for all calls/texts as this was ED standard practice. For call attempts, voicemail messages were left if there was no voice-to-voice contact. Standardized text messages were sent stating “Please call (study staff name) at Children’s Hospital for your test results at (phone number).” Laboratory results or protected health information were never relayed via text message. If the patient was randomized into the call + text message group, she/he received a call followed immediately by a text message at each attempt. Similarly, patients randomized into the call group only received a call, and those in the text group only received text messages. The goal was to have voice-to-voice contact; thus, if a patient responded to a text or a call with a text message, the nurse/NP responded with a text instructing the patient to call. After three failed notification attempts on three consecutive days, a letter was mailed. If the nurse/NP made voice-to-voice contact, she followed recommended STI prevention guidelines: i.e. gave patients test results and inquired about completion of treatment, abstinence, and partner notification/treatment. If the patient had not been treated, the nurse/NP offered three options: 1) calling a prescription to a pharmacy, 2) returning to the ED, or 3) returning to her/his primary care provider or health department. The nurse/NP documented treatment and counseling information as well as the number of attempts and the date of notification on a standard follow-up form and in the EMR. The main outcome measure was the percentage of patients notified by voice-to-voice interaction within 7 days of STI testing (cervical or urine nucleic acid amplification test for GC and CT, and trichomonas antigen testing for trich). In our institution, GC and CT tests were resulted only three times a week. Thus, the time period of 7 days was based on good clinical practice, the limits of our institutional practices and previous literature [24].
Primary Data Analysis
A t-test was used to test for age differences among those who were included versus those excluded. For included patients, exploratory analyses using descriptive statistics, frequency distributions and graphical methods were conducted for all study variables. A logistic regression (LR) model was developed to estimate the main and interaction effects of the two experimental factors; type of card and method of notification. The dependent variable was the dichotomous outcome of successful notification within 7 days. The independent variables included the two experimental factors, their interaction and replication. We also included covariates to control for 1) age as a continuous variable, 2) empiric treatment in the ED, 3) number of days to first notification attempt, and 4) documentation of a confidential phone number.
RESULTS
A total of 2536 patients (1887 females and 649 males) were tested for STIs and 584 (23%) were positive. Thus, 383 female patients and 201 male patients were included in the analysis. Patient characteristics are depicted in Table 1. An additional twenty-nine females (7%) and twenty-three males (10%) were STI positive during the study period but were excluded as their phones did not receive text messages. Mean age did not differ between those included vs. those excluded in the study for females (17.6 vs. 17.3, p= 0.52) or males (17.7 vs. 17.3, p= 0.29). The average number of contact attempts among females and males respectively in each study arm included: call group = 1.80, 1.72, text group = 1.75, 1.77 and call + text group = 1.50, 1.75.
Table 1.
Demographic Characteristics and covariates by gender
| Females (n = 383) n (%) |
Males (n = 201) n (%) |
|
|---|---|---|
|
| ||
| Age (years) | ||
|
| ||
| 14 - 15 | 53 (13.8%) | 19 (9.5%) |
| 16 - 17 | 134 (35.0%) | 70 (34.8%) |
| 18 - 21 | 196 (51.2%) | 112 (55.7%) |
|
| ||
| Race | ||
|
| ||
| White | 25 (6.5%) | 8 (4.0%) |
| Black | 336 (87.7%) | 188 (93.5%) |
| Multiracial | 11 (2.9%) | 1 (0.5%) |
| Other | 11 (2.9%) | 4 (2.0%) |
|
| ||
| STI positive test results a | ||
|
| ||
| Chlamydia | 250 (65.3%) | 135 (67%) |
| Gonorrhea | 123 (32.1%) | 97 (48.3%) |
| Trichomonas | 94 (24.5%) | 0b |
|
| ||
|
Number of attempts to
successful contact |
||
|
| ||
| One attempt | 219 (57.2%) | 109 (54.2%) |
| Two attempts | 63 (16.4%) | 20 (10%) |
| Three attempts | 24 (6.3%) | 19 (9.5%) |
| Within 7 days but after third attemptc |
1 (0.3%) | 8 (4%) |
| No successful contact | 76 (19.8%) | 45 (22.3%) |
|
| ||
| Empiric treatment | 266 (69.5%) | 185 (92.0%) |
|
| ||
| Empiric treatment and successfully contacted |
225 (58.7%) | 146 (72.6%) |
|
| ||
| No empiric treatment and successfully contacted |
97 (25.3%) | 10 (5%) |
|
| ||
|
Provided a confidential
number |
334 (87.2%) | 169 (84.1%) |
|
| ||
|
Days to first contact attempt | ||
|
| ||
| Mean | 2.6 | 2.5 |
| Standard deviation | 1.4 | 1.2 |
| Min | 0 | 0 |
| Max | 6 | 6 |
Some patient were positive for more than one STI
Males were not tested for trichomonas
These patients either received a letter and contacted the nurse/NP in response to the letter or called back in response to one of the texts or voicemail messages they received.
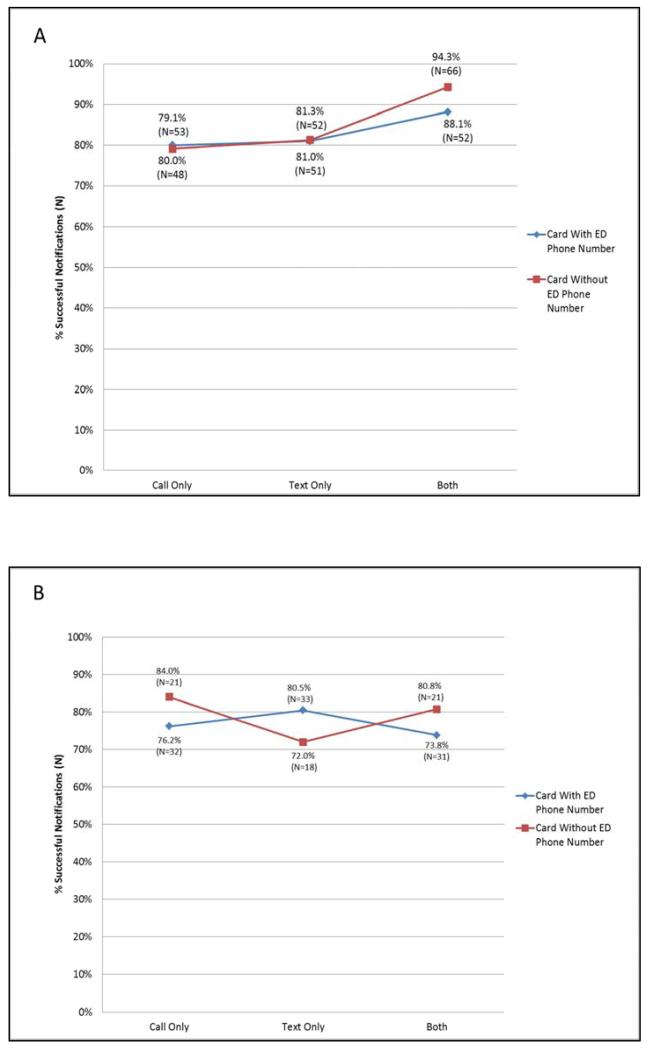
Figure 2 displays the unadjusted percentage of adolescents successfully notified in each of the six intervention combinations. There was no significant interaction (females: p=0.53; males: p=0.45) between the type of STI information card distributed and patient notification method.
Figure 2.
Unadjusted percentage of adolescents successfully notified by notification method and card type (A: Females p=0.53, B: Males p=0.45)
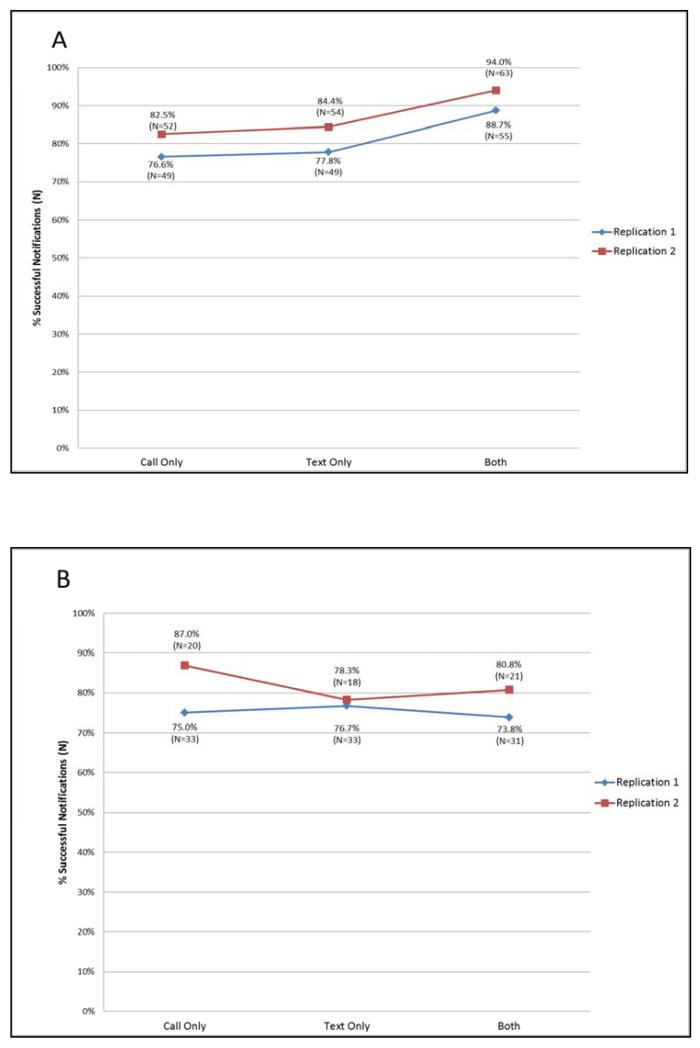
Figure 3 displays the percent of successful notification by each notification method and replication. Although notification rates were slightly higher during the second replication, the association of replication with successful notification rates was not significant for females (p=0.11) or males (p=0.26).
Figure 3.
Unadjusted percentage of adolescents successfully notified by notification method and replication (A: Females p=0.11, B: Males p=0.26)
Table 2 summarizes the adjusted and unadjusted odds ratios for the experimental factors and covariates. Because the interaction effect between card type and notification method was not significant for either gender, it was not included in the final LR models. The type of card distributed or texting alone was not significantly associated with patient notification rates. Among females, the odds of successful notification were significantly greater when notification included a call + text message compared to a call only, and documenting a confidential phone number was the only covariate that was independently associated with successful notification. There were no significant main effects for males. The unadjusted percentage of those patients who had a documented confidential phone number, received both a call + text message and were successfully notified within 7 days of their ED visit was 94.5% for females and 83.3% for males.
Table 2.
Adjusted and unadjusted odds ratios for the experimental factors
| Females: Adjusted and Unadjusted Odds Ratios | ||
|---|---|---|
|
| ||
| Experimental Factors | Unadjusted OR (95%CI) |
Adjusted OR (95% CI) |
|
| ||
| Text vs. call | 1.1 (0.6, 2.1) | 1.1 (0.6, 2.1) |
| Call + text message vs. call | 2.7 (1.3, 5.8) | 3.2 (1.4, 6.9) |
| Card (referent = no EDa phone number) | 0.9 (0.5, 1.5) | 0.9 (0.5, 1.6) |
| Replication (referent = Replication 1) | 1.6 (0.9, 2.8) | 1.5 (0.8, 2.9) |
|
| ||
| Covariates | ||
|
| ||
| Documentation of confidential phone number | - | 3.6 (1.7, 7.5) |
| Empiric treatment in the EDa | - | 0.8 (0.4, 1.6) |
| Age | - | 1.1 (0.9, 1.3) |
| Number of days to first contact attempt | - | 1.0 (0.8, 1.2) |
|
| ||
| Males: Adjusted and Unadjusted Odds Ratios | ||
|
| ||
| Experimental Factors | Unadjusted OR (95%CI) |
Adjusted OR (95% CI) |
|
| ||
| text vs. call | 0.9 (0.4, 2.0) | 0.8 (0.4, 2.0) |
| Call + text message vs. call | 0.8 (0.4, 1.9) | 0.9 (0.4, 2.1) |
| Card (referent = no EDa phone number) | 0.9 (0.4, 1.7) | 1.0 (0.5, 2.0) |
| Replication (referent = Replication 1) | 1.5 (0.7, 3.1) | 1.2 (0.6, 2.7) |
|
| ||
| Covariates | ||
|
| ||
| Documentation of confidential phone number | - | 2.2 (0.9, 5.2) |
| Empiric treatment in the EDa | - | 2.4 (0.8, 7.5) |
| Age | - | 1.1 (0.9, 1.4) |
| Number of days to first contact attempt | - | 0.9 (0.6, 1.2) |
ED- emergency department
DISCUSSION
Improving our ability to notify and appropriately treat adolescents with STIs is critical in stemming the STI epidemic in this population. In our community as well as other cities, many young men and women use the ED for primary care issues including STI evaluation [25]. Those who have positive STI results, and not treated in the ED, are often lost to follow-up and remain untreated [10, 19]. Therefore, it is important to ensure that adolescents with a positive STI result are contacted, counseled and treated. To our knowledge, this is the first study in the US to demonstrate that using a dedicated mobile phone to call and text adolescents is a successful intervention to inform female adolescents of their positive STI results.
The addition of text messaging to the continued documentation of confidential phone numbers in the EMR resulted in an almost 12% improvement in adolescent notification rates among females. Because we didn’t have previous baseline data among males, we are unable to report the change. Previous literature has suggested that text messaging among adolescents may be a contact method that would allow us to significantly improve STI notification and treatment rates [26]. Lenhart, et al. report that few adolescents have unlimited voice minute plans; however, 75% have unlimited texting plans [13]. Consequently, they choose not to check voice messages because this “wastes” minutes, and voice messages cannot be left when the phone is “out of minutes”. Skinner, et al. identified this cost as a barrier for adolescents using cell phones in the traditional way [27]. Lenhart, et al. also endorsed adolescents recognizing that receiving a text message is less expensive than voicemail [13]. Other authors have demonstrated text messaging success in managing adolescent chronic health issues and providing STI prevention and sexual health messages [28, 29]. However, previous studies examining text messaging as a notification method for positive STI testing, show mixed results with regards to notification rates and time to treatment [30-32]. These studies were conducted in sexual health clinic settings among various age groups in countries (New Zealand and the United Kingdom) with very different healthcare systems from the US. In the US, adolescent girls ages 14-17 years are most active in regards to texting, averaging 100 or more daily text messages [33]. Boys typically only average 30 daily texts [33]. This difference in use may explain in part why we demonstrated significant improvement in notification rates for females but not males. Additionally, in this ED study, patients tested for STIs all presented either due to the presence of symptoms or a possible STI exposure. A majority of the males were empirically treated with a lesser number of females receiving empiric treatment. Because many males already received treatment, perhaps they were not as concerned about knowing their STI status as compared to the females who may have had persistent symptoms thus were more interested in obtaining test results and receiving treatment. The gender differences in empiric treatment rates may have had an effect on those we were able to successfully contact. Despite ED treatment, messages need to be designed to stress the importance of follow-up with a healthcare provider. Literature has also shown that beginning in late adolescence, males have a significantly lower number of primary care visits as compared to females [34]. Our results may suggest that successful contact is a proxy for gendered socialization regarding who seeks or pursues health care.
Our demonstrated success in notifying patients through a combination of mobile phone calls and texting technology has several implications. First, inadequate systems for communicating test results often lead to STI overtreatment in ED settings where adolescents are empirically treated. Prior to our interventions, approximately 70% of our ED female patients received empiric antibiotic treatment after being tested for STIs and only 22% of those tested were STI positive, demonstrating significant overtreatment [11]. ED providers practice in this manner due to difficulty predicting who will have positive STI results, difficulty in contacting patients after ED discharge, and the presumption that a patient will not fill a prescription or receive treatment if they are not treated at the time of the visit [19]. This practice may contribute to antibiotic resistance, unnecessary antibiotic side effects, increased health care costs and adverse psychosocial consequences including stigma and shame [10]. In our institution, after information from the current study regarding our successful notification rates was communicated to ED providers, it resulted in a decrease in empiric treatment among STI patients tested in the ED [35]. Despite the decrease in overtreatment, this change has not resulted in under-treatment of true positives, but instead, more accurate treatment of true positives [35]. There are, however, some symptomatic patients who are clinically diagnosed with PID or cervicitis and may subsequently have negative test results. Thus there will always be the need for immediate treatment based on clinical findings.
Additionally, by improving post-visit contact rates, we are improving our communication with adolescents regarding their STI results. We now have increased opportunities to counsel regarding the importance of safe sex behaviors and partner notification. It has been demonstrated in previous studies that ED telephone follow-up improves patient compliance, and allows for further clarification of discharge instructions which is requested in over 40% of patients contacted [36, 37]. Perhaps this intervention should be expanded to all patients tested for STIs regardless of their results as this is an opportune teachable moment to relay further sexual prevention messages.
This intervention was low cost as we only had to pay for the cell phone and use and a dedicated NP/nurse to make follow-up phone calls/texts. Our division now has daily dedicated nurses whose sole responsibility is to contact and assure treatment among all patients with positive ED test results, including STI results. Nurses have been trained to provide confidential test results, treatment, and sexual prevention advice to the STI positive adolescents. Thus it was relatively easy to transition this care from that of the study NP/nurse to that of nurses providing this service for all ED patients.
There are several limitations to this study. Since this study was integrated into a clinical setting as a real-world effectiveness intervention, we cannot be sure that every patient received an STI patient information card at his/her ED visit. However, all staff were trained in card distribution and only one “type” of STI information card was available at any one time. Additionally, we closely monitored the number of patients tested as compared to the number of cards distributed and those numbers were similar. We did not document the number of patients calling in for their test result prior to the nurse/NP contacting them. In these cases, often patients called prior to result availability, thus the nurse/NP would have to make another contact attempt when results were available. However, these limitations are typical of real-world clinical effectiveness interventions. Although contacting adolescents for STI follow-up is a common challenge across institutions and EDs, this intervention was conducted at a single academic center, which may limit overall generalizability. Contacting patients within three days would have been preferable; however, in our institution, test results among some patients are not available until up to three days after their visit. Lastly, all adolescents in this study who were contacted and untreated at the initial visit had either a prescription called in to a pharmacy (positive for trich or CT) or were instructed to return for an intramuscular injection (positive for GC). In these patients, contact was a proxy to treatment as we were unable to assure the patient actually picked up the prescription at the pharmacy or returned to a healthcare system for treatment. Future interventions need to include further follow-up with these patients to assure appropriate outpatient treatment.
CONCLUSION
Using a combination of mobile phone call and text messaging improved our ability to notify STI positive adolescent females within 7 days of STI testing. Additionally, this study reinforced that EMR documentation of confidential phone numbers increases the likelihood of successfully notifying STI positive ED patients. Because these system changes are easily implemented and can make use of existing personnel, institutions can readily adapt these changes to improve STI care and impact the adolescent STI epidemic.
IMPLICATIONS AND CONTRIBUTION.
Communicating sexually transmitted infection (STI) results in an emergency department setting is a challenge. The addition of text messaging and confidential phone number documentation in the medical record is an effective method to notify STI positive adolescent females regarding their results. Institutions can adapt these interventions to improve STI care.
Acknowledgements
The first draft of the manuscript was written by Jennifer L. Reed, MD, and there was no payment given to anyone to produce the manuscript.
Sources of Support:
Cincinnati Hospital Research Foundation Place Outcomes Grant Award (Reed, PI)
K12 BIRCWH (Building Interdisciplinary Research Careers in Women’s Health) Award from the NICHD/NIH K12HD051953 (Tsevat, PI: Reed, Trainee)
REDCap project, Center for Clinical and Translational Science and Training Grant from NCRR/NIH UL1-RR026314-01
Previous presentations:
Ninth Annual Interdisciplinary Women’s Health Research Symposium, Bethesda, Maryland, November 2012, poster presentation
BIRCWH Scholars Annual Meeting, Bethesda, Maryland, November 2012, poster presentation
Pediatric Academic Society Annual Meeting, Washington D.C., May 2013, platform presentation
STI and AIDS World Congress, Vienna, Austria, July 2013, platform presentation
Persons who have contributed to the study:
We would like to acknowledge Mona Ho, MS for her contributions to the statistical analysis. (Ms. Ho is affiliated with Cincinnati Children’s Hospital Medical Center and does not have any financial disclosures nor does she report any conflicts of interest. Ms. Ho has provided written permission to be included in the acknowledgement section of this manuscript.)
Abbreviations
- STI
sexually transmitted infection
- PED
pediatric emergency department
- ED
emergency department
- EMR
electronic medical record
- US
United States
- NP
nurse practitioner
- LR
logistic regression
- OR
odds ratio
- IRB
Institutional Review Board
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Clinical Trial Registry:
Name: Improving sexually transmitted infection (STI) results notification and partner services
Clinicaltrials.gov ID: NCTO1938053
Conflict of Interest: There are no conflicts of interests to report among any of the authors.
Financial Disclosures: There are no financial disclosures to report among any of the authors. There was no study sponsor involved in this study.
REFERENCES
- 1.Centers for Disease Control and Prevention (CDC) [Accessed April 21, 2014];Sexually Transmitted Diseases Surveillance. 2012 Available at: http://www.cdc.gov/std/stats12/default.htm.
- 2.Goyal M, Hayes K, Mollen C. Sexually transmitted infection prevalence in symptomatic adolescent emergency department patients. Pediatr Emerg Care. 2012;28:1280. doi: 10.1097/PEC.0b013e3182767d7c. DOI:10.1097/PEC.0b013e3182767d7c. [DOI] [PubMed] [Google Scholar]
- 3.Miller MK, Harrison CJ, Mollen CJ, et al. Prevalence of Three Sexually Transmitted Infections in a Pediatric Emergency Department. Pediatr Emerg Care. 2013 doi: 10.1097/PEC.0000000000000284. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Crosby RA, DiClemente RJ, Wingood GM, et al. Associations between sexually transmitted disease diagnosis and subsequent sexual risk and sexually transmitted disease incidence among adolescents. Sex Transm Dis. 2004;31:205–208. doi: 10.1097/01.olq.0000114940.07793.20. DOI:00007435-200404000-00002 [pii] [DOI] [PubMed] [Google Scholar]
- 5.Fortenberry JD, Brizendine EJ, Katz BP, et al. Post-treatment sexual and prevention behaviours of adolescents with sexually transmitted infections. Sex Transm Infect. 2002;78:365–368. doi: 10.1136/sti.78.5.365. DOI:DOI:10.1136/sti.78.5.365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Reed JL, Simendinger L, Griffeth S, et al. Point-of-care testing for sexually transmitted infections increases awareness and short-term abstinence in adolescent women. The Journal of adolescent health: official publication of the Society for Adolescent Medicine. 2010;46:270–277. doi: 10.1016/j.jadohealth.2009.08.003. DOI:10.1016/j.jadohealth.2009.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Batteiger BE, Tu W, Ofner S, et al. Repeated Chlamydia trachomatis genital infections in adolescent women. J Infect Dis. 2010;201:42–51. doi: 10.1086/648734. DOI:10.1086/648734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Beckmann KR, Melzer-Lange MD, Gorelick MH. Emergency department management of sexually transmitted infections in US adolescents: results from the National Hospital Ambulatory Medical Care Survey. Ann Emerg Med. 2004;43:333–338. doi: 10.1016/j.annemergmed.2003.10.034. DOI:10.1016/S0196064403011119. [DOI] [PubMed] [Google Scholar]
- 9.Kane BG, Degutis LC, Sayward HK, et al. Compliance with the Centers for Disease Control and Prevention recommendations for the diagnosis and treatment of sexually transmitted diseases. Acad Emerg Med. 2004;11:371–377. doi: 10.1197/j.aem.2003.11.016. DOI:10.1197/j.aem.2003.11.016. [DOI] [PubMed] [Google Scholar]
- 10.Levitt MA, Johnson S, Engelstad L, et al. Clinical management of chlamydia and gonorrhea infection in a county teaching emergency department--concerns in overtreatment, undertreatment, and follow-up treatment success. J Emerg Med. 2003;25:7–11. doi: 10.1016/s0736-4679(03)00131-8. DOI:S0736467903001318 [pii] [DOI] [PubMed] [Google Scholar]
- 11.Huppert JS, Reed JL, Munafo JK, et al. Improving notification of sexually transmitted infections: a quality improvement project and planned experiment. Pediatrics. 2012;130:e415–422. doi: 10.1542/peds.2011-3326. DOI:10.1542/peds.2011-3326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Divecha Z, Divney A, Ickovics J, et al. Tweeting about testing: do low-income, parenting adolescents and young adults use new media technologies to communicate about sexual health? Perspect Sex Reprod Health. 2012;44:176–183. doi: 10.1363/4417612. DOI:10.1363/4417612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lenhart A, Purcell K, Smith A, et al. [Accessed April 25, 2013];Social media and mobile internet use among teens and young adults. Available at: http://www.pewinternet.org/~/media//Files/Reports/2010/PIP_Social_Media_and_Young_Adults_Report_Final_with_toplines.pdf.
- 14.Selkie EM, Benson M, Moreno M. Adolescents’ Views Regarding Uses of Social Networking Websites and Text Messaging for Adolescent Sexual Health Education. Am J Health Educ. 2011;42:205–212. doi: 10.1080/19325037.2011.10599189. DOI:DOI:10.1080/19325037.2011.10599189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Perry RC, Kayekjian KC, Braun RA, et al. Adolescents’ perspectives on the use of a text messaging service for preventive sexual health promotion. The Journal of adolescent health: official publication of the Society for Adolescent Medicine. 2012;51:220–225. doi: 10.1016/j.jadohealth.2011.11.012. DOI:10.1016/j.jadohealth.2011.11.012. [DOI] [PubMed] [Google Scholar]
- 16.Lim MS, Hocking JS, Hellard ME, et al. SMS STI: a review of the uses of mobile phone text messaging in sexual health. Int J STD AIDS. 2008;19:287–290. doi: 10.1258/ijsa.2007.007264. DOI:10.1258/ijsa.2007.007264. [DOI] [PubMed] [Google Scholar]
- 17.Gold J, Lim MS, Hocking JS, et al. Determining the impact of text messaging for sexual health promotion to young people. Sex Transm Dis. 2011;38:247–252. doi: 10.1097/OLQ.0b013e3181f68d7b. DOI:10.1097/OLQ.0b013e3181f68d7b. [DOI] [PubMed] [Google Scholar]
- 18.Suffoletto B, Akers A, McGinnis KA, et al. A sex risk reduction text-message program for young adult females discharged from the emergency department. The Journal of adolescent health: official publication of the Society for Adolescent Medicine. 2013;53:387–393. doi: 10.1016/j.jadohealth.2013.04.006. DOI:10.1016/j.jadohealth.2013.04.006. [DOI] [PubMed] [Google Scholar]
- 19.Hack JB, Hecht C. Emergency physicians’ patterns of treatment for presumed gonorrhea and chlamydia in women: one center’s practice. J Emerg Med. 2009;37:257–263. doi: 10.1016/j.jemermed.2007.06.040. DOI:10.1016/j.jemermed.2007.06.040. [DOI] [PubMed] [Google Scholar]
- 20.Rein DB, Kassler WJ, Irwin KL, et al. Direct medical cost of pelvic inflammatory disease and its sequelae: decreasing, but still substantial. Obstet Gynecol. 2000;95:397–402. doi: 10.1016/s0029-7844(99)00551-7. DOI:S0029-7844(99)00551-7 [pii] [DOI] [PubMed] [Google Scholar]
- 21.Rothenberg RB, Wasserheit JN, St Louis ME, et al. Ad Hoc STD/HIV Transmission Group The effect of treating sexually transmitted diseases on the transmission of HIV in dually infected persons: a clinic-based estimate. Sex Transm Dis. 2000;27:411–416. doi: 10.1097/00007435-200008000-00006. [DOI] [PubMed] [Google Scholar]
- 22.Apfel CC, Korttila K, Abdalla M, et al. A factorial trial of six interventions for the prevention of postoperative nausea and vomiting. N Engl J Med. 2004;350:2441–2451. doi: 10.1056/NEJMoa032196. DOI:10.1056/NEJMoa032196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Moen RD, Nolan TW, Provost LP. Quality Improvement Through Planned Experimentation. 2nd edition McGraw-Hill; New York: 1999. [Google Scholar]
- 24.Wong D, Berman SM, Furness BW, et al. Time to treatment for women with chlamydial or gonococcal infections: a comparative evaluation of sexually transmitted disease clinics in 3 US cities. Sex Transm Dis. 2005;32:194–198. doi: 10.1097/01.olq.0000154494.95138.70. DOI:00007435-200503000-00011 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wilson KM, Klein JD. Adolescents who use the emergency department as their usual source of care. Arch Pediatr Adolesc Med. 2000;154:361–365. doi: 10.1001/archpedi.154.4.361. DOI:10.1001/archpedi.154.4.361. [DOI] [PubMed] [Google Scholar]
- 26.Mackenzie H. A text messaging trial in family planning clinics. Stud Health Technol Inform. 2009;146:154–159. [PubMed] [Google Scholar]
- 27.Skinner H, Biscope S, Poland B, et al. How adolescents use technology for health information: implications for health professionals from focus group studies. J Med Internet Res. 2003;5:e32. doi: 10.2196/jmir.5.4.e32. DOI:10.2196/jmir.5.4.e32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Levine D, McCright J, Dobkin L, et al. SEXINFO: a sexual health text messaging service for San Francisco youth. Am J Public Health. 2008;98:393–395. doi: 10.2105/AJPH.2007.110767. DOI:10.2105/AJPH.2007.110767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lim MS, Hocking JS, Aitken CK, et al. Impact of text and email messaging on the sexual health of young people: a randomised controlled trial. J Epidemiol Community Health. 2012;66:69–74. doi: 10.1136/jech.2009.100396. DOI:10.1136/jech.2009.100396. [DOI] [PubMed] [Google Scholar]
- 30.Dhar J, Leggat C, Bonas S. Texting--a revolution in sexual health communication. Int J STD AIDS. 2006;17:375–377. doi: 10.1258/095646206777323463. DOI:10.1258/095646206777323463. [DOI] [PubMed] [Google Scholar]
- 31.Lim EJ, Haar J, Morgan J. Can text messaging results reduce time to treatment of Chlamydia trachomatis? Sex Transm Infect. 2008;84:563–564. doi: 10.1136/sti.2008.032441. DOI:10.1136/sti.2008.032441. [DOI] [PubMed] [Google Scholar]
- 32.Menon-Johansson AS, McNaught F, Mandalia S, et al. Texting decreases the time to treatment for genital Chlamydia trachomatis infection. Sex Transm Infect. 2006;82:49–51. doi: 10.1136/sti.2004.014381. DOI:10.1136/sti.2004.014381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lenhart A, Ling R, Campbell S, et al. [Accessed April 25, 2013];Teens and Mobile Phones. Available at: http://www.pewinternet.org/Reports/2010/Teens-and-Mobile-Phones.aspx.
- 34.Ziv A, Boulet JR, Slap GB. Utilization of physician offices by adolescents in the United States. Pediatrics. 1999;104:35–42. doi: 10.1542/peds.104.1.35. [DOI] [PubMed] [Google Scholar]
- 35.Huppert JS, Taylor RG, St Cyr S, et al. Point-of-care testing improves accuracy of STI care in an emergency department. Sex Transm Infect. 2013;89:489–494. doi: 10.1136/sextrans-2012-050994. DOI:10.1136/sextrans-2012-050994. [DOI] [PubMed] [Google Scholar]
- 36.Jones J, Clark W, Bradford J, et al. Efficacy of a telephone follow-up system in the emergency department. J Emerg Med. 1988;6:249–254. doi: 10.1016/0736-4679(88)90336-8. DOI:10.1016/0736-4679. [DOI] [PubMed] [Google Scholar]
- 37.Ritchie PD, Jenkins M, Cameron PA. A telephone call reminder to improve outpatient attendance in patients referred from the emergency department: a randomised controlled trial. Aust N Z J Med. 2000;30:585–592. doi: 10.1111/j.1445-5994.2000.tb00860.x. DOI:10.1111/j.1445-5994.2000.tb00860.x. [DOI] [PubMed] [Google Scholar]